Abstract
The coronavirus pandemic is an ongoing global crisis that has profoundly harmed public health. Although studies found exposure to green spaces can provide multiple health benefits, the relationship between exposure to green spaces and the SARS-CoV-2 infection rate is unclear. This is a critical knowledge gap for research and practice. In this study, we examined the relationship between total green space, seven types of green space, and a year of SARS-CoV-2 infection data across 3,108 counties in the contiguous United States, after controlling for spatial autocorrelation and multiple types of covariates. First, we examined the association between total green space and SARS-CoV-2 infection rate. Next, we examined the association between different types of green space and SARS-CoV-2 infection rate. Then, we examined forest–infection rate association across five time periods and five urbanicity levels. Lastly, we examined the association between infection rate and population-weighted exposure to forest at varying buffer distances (100 m to 4 km). We found that total green space was negative associated with the SARS-CoV-2 infection rate. Furthermore, two forest variables (forest outside park and forest inside park) had the strongest negative association with the infection rate, while open space variables had mixed associations with the infection rate. Forest outside park was more effective than forest inside park. The optimal buffer distances associated with lowest infection rate are within 1,200 m for forest outside park and within 600 m for forest inside park. Altogether, the findings suggest that green spaces, especially nearby forest, may significantly mitigate risk of SARS-CoV-2 infection.
Keywords: COVID-19 pandemic, Infection risk, Green spaces, Forest, Open space, Causal mechanisms
1. Introduction
The SARS-CoV-2 pandemic has profoundly affected people’s health and well-being globally (World Health Organization, 2021). Studies have explored associations between SARS-CoV-2 infection rate and numerous social, economic, and medical factors (Badr et al., 2020, Carteni et al., 2020, Mena et al., 2021, Muller et al., 2021). Fewer studies have explored the relationship between the built environment and infection rate. We know that architectural and landscape elements, especially green spaces, profoundly impact people’s physical and mental health and well-being. And yet, we have largely overlooked the relationship between green spaces and SARS-CoV-2 infection rate (Frumkin, 2021).
Several recent studies on green space and SARS-CoV-2 infection rate in the U.S. suggest that green spaces may provide some protection against infection (Klompmaker et al., 2021, Lu et al., 2021). However, these preliminary studies were conducted before the much larger second and third waves of the pandemic hit the U.S. Furthermore, these studies used simple measures of greenness, such as the normalized difference vegetation index (NDVI) and leaf area index (LAI). Though effective at capturing the amount of greenness in an area, these measures fail to consider factors that are likely to impact the relationship between SARS-CoV-2 infection and green settings. Previous studies suggest factors such as green space type (Akpinar et al., 2016, Allard-Poesi et al., 2022), population density (Stier et al., 2020), distance to green settings (Ekkel and de Vries, 2017, Kim and Miller, 2019) exert significant impacts on health outcomes. Among all factors, park has been frequently reported as an environmental factor that has a significant relationship with the SARS-CoV-2 infection rate (Johnson et al., 2020, Ma et al., 2022).
The objective of this study is to examine the links between various types of green spaces and SARS-CoV-2 infection rate for an entire year after controlling for all covariates. Without understanding these relationships, we may lose the opportunity to build supportive environments that increase our ability to resist infection, especially in our most vulnerable communities.
1.1. Accumulating evidence: The health benefits of exposure to green spaces
There is overwhelming evidence documenting the health benefits of green space exposure at national (Lu et al., 2021, Nowak et al., 2014), city (Donovan et al., 2011), and community levels (Chang et al., 2021, Kuo and Sullivan, 2001). Contact with green spaces is associated with improved mental (Jiang et al., 2014, Jiang et al., 2018, He et al., 2022) and physical health outcomes (Lu, 2018, Mitchell and Popham, 2008), and the effects are complex and interdependent (Jiang et al., 2015, Sullivan and Bartlett, 2005). For example, green spaces significantly reduce mental stress and fatigue (Jiang, He, Chen, Larsen, & Wang, 2020, Jiang et al., 2021), which positively influence immune function and promote physical health (Kuo, 2015, Parsons et al., 1998). Many studies have found that green open spaces are negatively associated with chronic health outcomes because they facilitate physical activity and social interactions, reduce air pollution, and enhance immune function (Jiang et al., 2014, Kuo, 2015).
However, we still know little about whether green spaces impact SARS-CoV-2 infection rate. Recent studies have generated mixed results. Several studies identified negative associations between greenness and SARS-CoV-2 infection rate (Klompmaker et al., 2021, Spotswood et al., 2021). However, one study found that highly connected green spaces were associated with higher risk of SARS-CoV-2 transmission (Pan et al., 2021). Another study pointed out that although outdoor transmission of SARS-CoV-2 is less common, the risk does exist (Bulfone et al., 2021).
1.2. Necessity to compare health benefits of green spaces inside and outside park
Park is a mixture of many types of green spaces, such as open lawn, forest, and shrubs. As a critical type of public space for recreational and social activities, parks may have greater impacts on public health and well-being than private green spaces (Venter et al., 2020, Venter et al., 2021). And yet, studies exploring the association between parks and SARS-CoV-2 infection rate reveal mixed results. One study found that park use had no impact on infection rate (Kartal et al., 2021), while another study found that the availability of parks was associated with lower risk of SARS-CoV-2 transmission (Wang et al., 2021). Yet another study found park use decreased pre-peak SARS-CoV-2 infection rate (Johnson et al., 2020). Hitherto, we are not clear whether the relationships between different types of green spaces and SARS-CoV-2 infection rate are the same; or whether the effect of green spaces inside park is significantly different from green space outside park.
1.3. A critical knowledge gap: The relationship between green spaces and SARS-CoV-2 infection rate
While it is widely recognized that green spaces have a significant positive effect on human health, we know much less about how exposure to green spaces impacts infectious diseases such as SARS-CoV-2. One study examined the 135 most urbanized counties in the contiguous United States and found that a higher ratio of green space was significantly associated with lower racial disparity in SARS-CoV-2 infection rate at the county level (Lu et al., 2021). However, this study considered a relatively small number of highly urbanized counties (135) and used infection data from January through June 2020, a relatively short time period given the length of the pandemic.
Another study examined the association between county-level NDVI and SARS-CoV-2 infection and death rate for 2297 counties in the United States (Klompmaker et al., 2021). The study reported greenness was negatively associated with county-level SARS-CoV-2 infection rate. However, this study also used data from a relatively short time period (March to June 2020) and did not identify the types of green spaces that were associated with lower infection rate. The study also failed to account for important covariates, including transportation infrastructure and services (Carteni et al., 2020, Tirachini and Cats, 2020), political and administration factors (Clinton et al., 2021), human mobility (Muller et al., 2021), commuting mode (Figueroa et al., 2021), and employment status (Mena et al., 2021).
There is an urgent need for a more comprehensive assessment of the relationship between green spaces and SARS-CoV-2 infection rate. Understanding this relationship will enable planners and designers to develop appropriate environmental interventions that reduce the risk of infection for current and future airborne infectious diseases.
1.4. Research questions
In this study, we asked four layers of questions: 1) What is the association between total green space and SARS-CoV-2 infection rate? 2) What are the associations between various types of green spaces and SARS-CoV-2 infection rate and what are key green spaces that have the greatest impacts on the associations? 3) What are the relationships between key green spaces and SARS-CoV-2 infection rate across various levels of urbanicity and over distinct time periods of SARS-CoV-2 pandemic? 4) What are the optimal buffer distances of key green spaces exposure associated with reduced levels of SARS-CoV-2 infection rate?
2. Material and methods
2.1. Study design
We investigated the association between total green space, various types of green space, and SARS-CoV-2 infection rate in the contiguous United States from January 22 to December 31, 2020. We also examined associations between forest and SARS-CoV-2 infection rate in counties across five levels of urbanicity and five different time periods. To identify the optimal buffer distance, we examined the relationship between population-weighted exposure to forest within various buffer distances (100 m to 4 km) from human population distribution and the SARS-CoV-2 infection rate. We used the county as the basic unit of analysis and included a total of 3,108 counties in the contiguous United States.
2.1.1. SARS-CoV-2 infection
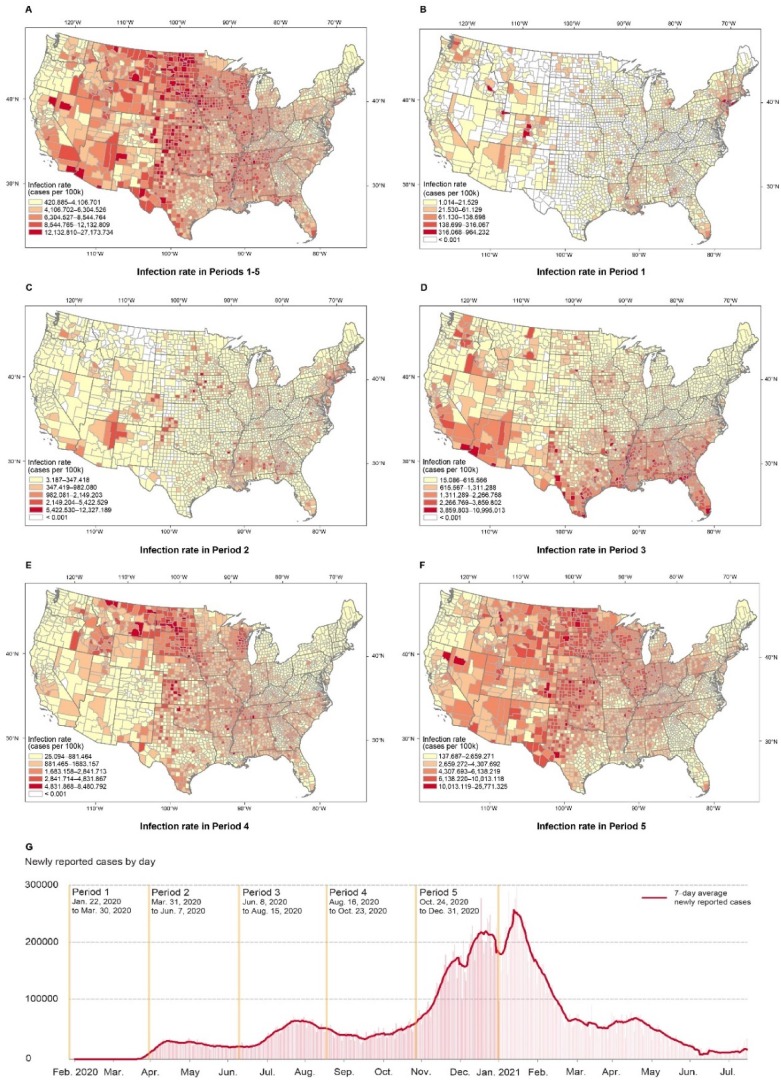
We obtained the number of positive cases of SARS-CoV-2 infection rate from January 22, 2020 to December 31, 2020 from the Centers for Disease Control and Prevention (CDC) and state- and local-level public health agencies (USAFACTS, 2021). We chose December 31 as the endpoint as the SARS-CoV-2 pandemic neared its peak at approximately this week, despite some fluctuations (Fig. 1 ). Moreover, this endpoint fell prior to the rollout of large-scale vaccination programs and the change in the U.S. presidency, allowing us to avoid the confounding effects of political and programmatic factors. The research period was divided into five periods to investigate the temporal association between SARS-CoV-2 infection rate and green spaces. We select the break point of the five time periods based on the development stage of the SARS-CoV-2 infection in 2020, as the severity of SARS-CoV-2 infection rate may affect social distancing policies and people’s mobility patterns including green space usage during the pandemic (Heo et al., 2020, Tokey, 2021). As shown in Fig. 1, period 1 included the onset and early outbreak of SARS-CoV-2 (January 22 to March 30); period 2 included the first wave of SARS-CoV-2 infection in 2020 (March 31 to June 7), period 3 included the second wave in 2020 (June 8 to August 15), period 4 included a stagnation period in 2020 (August 16 to October 23), and period 5 included the peak in 2020 (October 24 to December 31, 2020).
Fig. 1.
County-level Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection (cases per 100,000 population) in total and across the five subperiods. (A) The overall research period, from January 22 to December 31, 2020. (B) Period 1: January 22 to March 30, 2020. (C) Period 2: March 31 to June 7, 2020. (D) Period 3: June 8 to August 15, 2020. Period 4: August 16 to October 23, 2020. (F) Period 5: October 24 to December 31, 2020. (G) Diagram of cases of SARS-CoV-2 from February 2020 to July 2021 in the United States. The SARS-CoV-2 pandemic emerged out the U.S. out 2020 and comprised several different periods, with low, moderate, and high infection rates. The infection rate in 2021 was significantly attenuated due to wide-scale vaccination, so this data was not included.
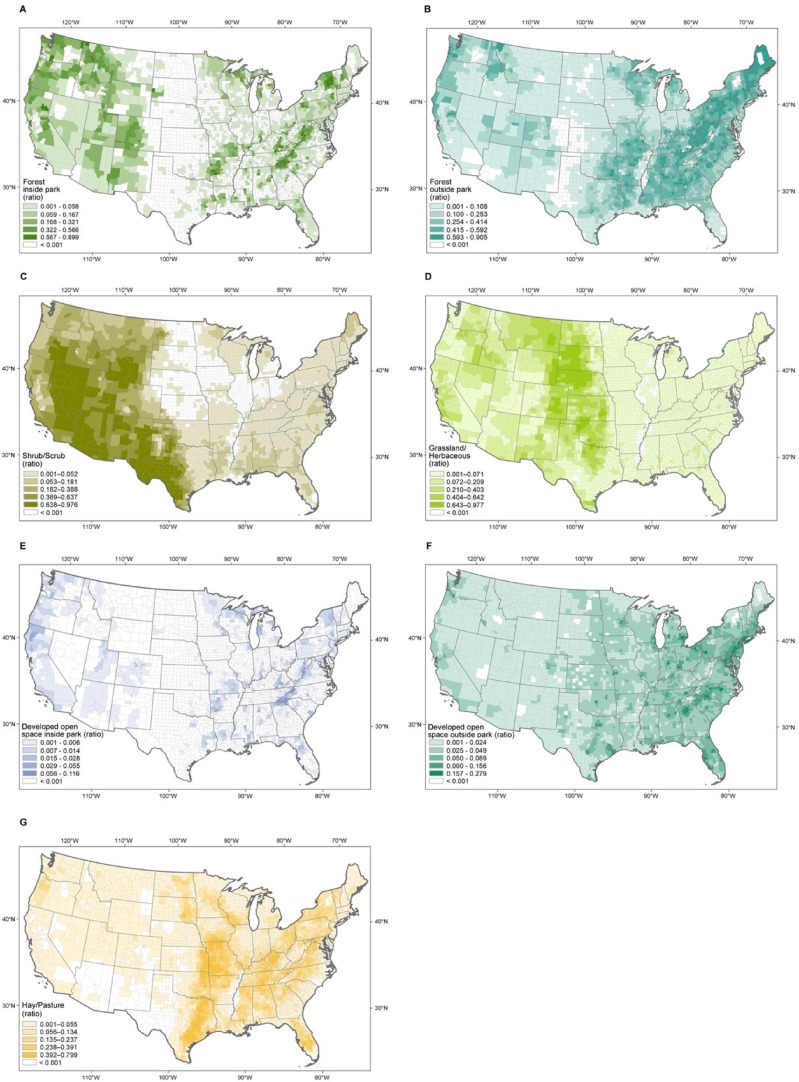
2.1.2. Green spaces
We quantified the total and seven types of green space with predominant natural elements assessed at a 30-m resolution using National Land Cover Datasets (NLCD, 2016): open space inside park, open space outside park, forest inside park, forest outside park, shrub and scrub, herbaceous, hay and pasture (Table S1). County-level open space and forest were divided into factors within and outside parks using the USA Parks dataset from Esri (Esri, 2021). The ratio of total and seven types of green space were measured as the area of total and each type of green space within a county divided by the total county area (Fig. 2 ).
Fig. 2.
Ratio of seven types of green spaces at a county level. Values represent the (A) forest inside park (B) forest outside park, (C) shrub/scrub, (D) grassland/herbaceous, (E) open space inside park, (F) open space outside park, (G) hay/pasture at the county level, calculated as the total area of each green space divided by the county area. Data were extracted from the NLCD landcover dataset.
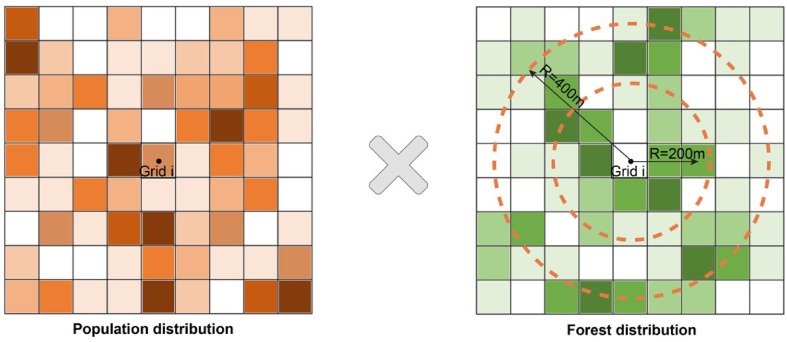
We also calculated population-weighted exposure to forest within varying buffer sizes (100 -m to 4 km) in each county in Google Earth Engine (GEE). We extracted the forest inside park and forest outside park using the NLCD 2016 and USA Parks boundary (Esri, 2021). Then, we located the population distribution of the residents in the contiguous United States from the WorldPop Global Project Population Data 2020 (Sorichetta et al., 2015). The WorldPop Global Project Population Data 2020 estimated the number of people residing in each 100x100m grid cell matched to their associated administrative units. The original 30 m NLCD 2016 land cover map was reprojected to a 100 m resolution to match the population data. The population-weighted exposure to forest within various buffer distances in each county was calculated using the following Eq. (1) (Chen et al., 2018),
| (1) |
where Pi represents the population of the i th grid, represents the forest cover of the i th grid with a buffer size of b meters, N denotes the total number of grids for a given county, and FE is the estimated forest exposure area per person for the given county.
The population-weighted exposure considers population spatial distribution in forest exposure estimates by giving proportionally greater weight to forest near densely populated areas. The forest exposure received by the population living in a grid is not only the forest cover within this grid, but also includes the forest around the living grid in a certain spatial range (e.g., 200 m, 400 m) (Fig. 3 ). In this calculation, the buffer distance is calculated from the center of the grid, a grid is included in the buffer zone if the center point of the grid falls inside the dashed-line circle. We select the 4 km threshold because most walking trips are within 4 km (Yang & Diez-Roux, 2012). We set the buffer intervals of 200 m for buffer distances less than or equal to 2 km and 500 m for buffer distances 2 to 4 km.
Fig. 3.
Conceptual diagram of population-weighted exposure to forest within a given buffer (i.e., 200 and 400 m buffer in this example). Population-weighted exposure to forest considers the relative spatial distribution of population and forest, and gives a higher weighting to forest close to densely populated area (see Equation 1). The buffer distance is calculated from the center of the grid, and a grid is included in the buffer zone if the center point of the grid falls inside the buffer zone (the dashed line circle).
2.1.3. Levels of urbanicity
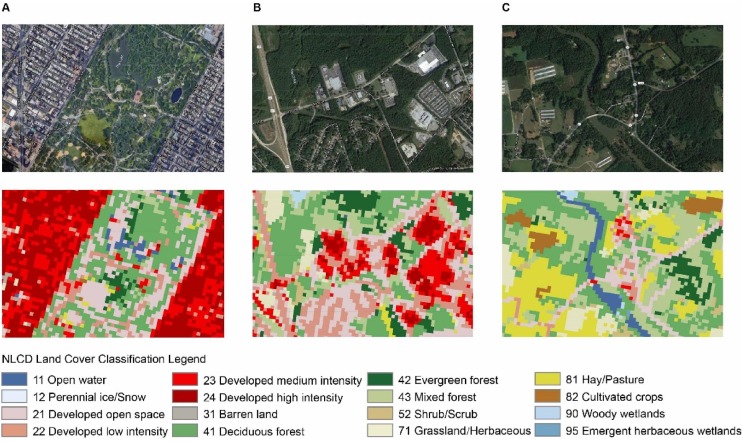
We categorized all counties into five levels of urbanicity based on the 2013 Urban-Rural Classification Scheme from the National Center for Health Statistics, which is well-suited for health analyses (NCHS, 2017). Urbanicity level 1 is the most urbanized and level 5 is the most rural (Fig. 4 & Table S2). Previous studies have identified an urban–rural disparity in the prevalence of SARS-CoV-2 infection in the United States (Huang et al., 2021, Pro et al., 2020). A recent review study also found exposure to green space has a heterogeneous effect on health outcomes across different levels of urbanicity (Browning et al., 2022).
Fig. 4.
Example of land cover distributions at three different urbanicity levels. (A) New York City, NY, urbanicity level 1. (B) Athens, GA, urbanicity level 3. (C) Coleridge, NC, urbanicity level 5. Squares marked by light, moderate, and dark green colors have been identified by NLCD as forest areas, including deciduous, evergreen, or mixed forest.
2.1.4. Covariates
Additionally, we adjusted for potential covariates which significantly impact SARS-CoV-2 infection rates, including healthcare and testing rate (Wu et al., 2020), pre-existing chronic diseases (i.e., hypertension and diabetes) (Clerkin et al., 2020, Fang et al., 2020, Sattar et al., 2020), socioeconomic and demographic factors (i.e., racial minority and elderly) (Abedi et al., 2020, Clouston et al., 2021, Karaye and Horney, 2020), politics and policy factors (i.e., political affiliation and stay-at-home orders) (Neelon et al., 2021, Fowler et al., 2021), behavioral factors (i.e., mobility pattern and social distancing) (Badr et al., 2020, McGrail et al., 2020), and environmental factors (i.e., air pollution, crowded housing, and airport density) (Chakrabarty et al., 2021, Gaskin et al., 2021, McLaughlin et al., 2020). The definition of all covariates is presented in Table S2.
2.1.5. Descriptive statistics of variables
The descriptive statistics for each variable entered in the models are presented in Table 1 (See Table S3 & S4 for the descriptive information for all variables). The correlation matrix of all variables in the final model is given in Supplementary Fig. 1.
Table 1.
Descriptive data for SARS-CoV-2 infection rate, socioeconomic and demographic, healthcare and testing, pre-existing chronic disease, policy and regulation, behavioral, environmental, and green space factors.
| Variable Categories | Variables | Min | Max | Mean | SD | Unit or Formula |
|---|---|---|---|---|---|---|
| SARS-CoV-2 Infection rate | Infection rate | 420.885 | 27173.734 | 6570.950 | 2762.664 | Cases per 100 k |
| Socio-economic and Demographic factors | Population density | 0.094 | 19625.842 | 98.221 | 559.972 | Persons per |
| Black non-Hispanic | 0.000 | 87.400 | 8.957 | 14.520 | Ratio | |
| Population aged 65 above | 3.800 | 55.600 | 18.428 | 4.542 | Ratio | |
| Gini Index | 0.257 | 0.665 | 0.446 | 0.036 | Range 0–1 | |
| Median home value | 21000.00 | 1057000.00 | 146157.40 | 89047.61 | USD$ | |
| Unemployment rate | 1.300 | 18.100 | 4.093 | 1.397 | Ratio | |
| Population without high school diploma | 1.200 | 66.300 | 13.448 | 6.342 | Ratio | |
| Healthcare and testing factors | Population without insurance | 2.300 | 33.700 | 11.418 | 5.106 | Ratio |
| COVID-19 testing rate | 0.000 | 1711.099 | 170.197 | 107.693 | Per 100 k | |
| Pre-existing chronic disease factors | Diabetes rate | 2.200 | 28.700 | 10.506 | 3.526 | Ratio |
| Obesity rate | 12.30 | 57.90 | 32.76 | 5.68 | Ratio | |
| Stroke mortality | 14.000 | 92.500 | 39.776 | 8.153 | Per 100 k | |
| Hypertension morality | 19.300 | 587.300 | 131.825 | 55.366 | Per 100 k | |
| Heart failure mortality | 19.400 | 304.300 | 108.314 | 25.488 | Per 100 k | |
| Politics and policy factors | State Governor Party | 0.000 | 1.000 | 0.435 | 0.496 | Democratic /Republican |
| Stay-at-home orders | 3.856 | 6.897 | 4.441 | 0.447 | Range 1–7 | |
| Public mask mandates | 0.000 | 1.000 | 0.497 | 0.339 | Yes/No | |
| Business closing and reopening | 4.781 | 8.233 | 6.331 | 0.683 | Range 1–5 | |
| Behavioral factors | Smoker | 5.909 | 41.491 | 17.446 | 3.554 | Ratio |
| Essential worker | 0.178 | 0.791 | 0.526 | 0.073 | Ratio | |
| Foot traffic to all points of interest (POI) | 0.000 | 10.507 | 1.505 | 0.904 | Per person | |
| Commute to work by walking or bicycle | 0.000 | 42.410 | 3.427 | 3.146 | Ratio | |
| Leisure time physical inactivity | 9.400 | 49.800 | 26.238 | 5.498 | Ratio | |
| Mobility | 0.409 | 553.723 | 8.118 | 14.190 | Km | |
| Normalized mobility index | 17.156 | 947.757 | 79.520 | 40.596 | Percentage | |
| Environmental factors | Severe housing problems | 2.700 | 39.100 | 14.308 | 4.338 | Ratio |
| Overcrowded housing | 0.000 | 16.900 | 2.314 | 1.816 | Ratio | |
| Proximity to highway | 0.000 | 16.400 | 1.943 | 1.871 | Ratio | |
| Airport density | 0.000 | 0.039 | 0.002 | 0.002 | Number per | |
| Railway density | 0.000 | 2.625 | 0.062 | 0.111 | Length of km per | |
| Highway and secondary road density | 0.000 | 1.577 | 0.105 | 0.132 | Length of km per | |
| PM2.5 | 1.500 | 16.000 | 7.640 | 1.674 |
Ug/m3 |
|
| PM10 | 7.476 | 57.922 | 17.417 | 4.755 | Ug/m3 | |
| NO2 | 2.896 | 27.402 | 13.321 | 3.337 | Ppb | |
| Average temperature | 36.809 | 79.218 | 57.687 | 7.941 | Degrees Fahrenheit | |
| Wind speed | 3.969 | 9.923 | 7.026 | 0.800 | m/s | |
| Green space factors | Total green space | 0.008 | 0.998 | 0.622 | 0.291 | ratio |
| Shrub/scrub | 0.000 | 0.976 | 0.085 | 0.181 | ratio | |
| Grassland/herbaceous | 0.000 | 0.977 | 0.094 | 0.169 | ratio | |
| Hay/pasture | 0.000 | 0.799 | 0.101 | 0.123 | ratio | |
| Open space inside park | 0.000 | 0.116 | 0.002 | 0.007 | ratio | |
| Open space outside park | 0.000 | 0.279 | 0.040 | 0.034 | ratio | |
| Forest inside park | 0.000 | 0.899 | 0.056 | 0.129 | ratio | |
| Forest outside park | 0.000 | 0.905 | 0.244 | 0.218 | ratio |
2.2. Statistical analysis
This study evaluates the association between green space and SARS-CoV-2 infection rate, with negative binomial mixed-effect models. The negative binomial model fits our overdispersion of the dependent variable, i.e., infection rate. We confirmed the spatial autocorrelation presence using Moran’s I test. The mixed-effect model can account for the clustering in the data of counties from the same state. We included a random effect of state to account for the non-independence of county-level data. The intra-class correlation coefficient (ICC) was 0.67, indicating that a 67 % variation in county-level infection rate was attributed to the clustering structure of our data. It also supports the mixed-effect model is necessary. In all models, all explanatory variables were centered and scaled; the covariates were adjusted including healthcare and testing factors, pre-existing chronic disease factors, socioeconomic and demographic factors, politics and policy factors, behavioral factors, and environmental factors.
We conduct two sets of statistical analyses. In the first set, Model 1 estimates the effect of total green space on the infection rate. Model 2 estimates the effects of seven types of green space. In the second set, Model 3 estimates the effects of forest in five time periods and five urbanicity levels using a series of separate models. The testing and regulation and policy variables (i.e., public mask mandate and stay-at-home order) were calculated in a time-sensitive way to reflect the variation in each period of time (see calculation method in Supplementary Table S2). Model 4 examines the dose–response effect of population-weighted exposure to forest at various buffer distances. This allows us to identify the optimal exposure distances from forest. In all models, we reported the effect size (β) and/or the incidence rate ratio (IRR), which compares the effect of independent variables on the SARS-CoV-2 infection rate. The IRR estimates the estimated rate ratio of SARS-CoV-2 infection rate for a one-unit increase in change of a variable, given the other variables are held constant in the model.
The variance inflation factor (VIF) test was used to identify multicollinearity between the independent variables, and variables with a VIF ≥ 4 were excluded from our models (O'Brien, 2007). All analyses were performed in R v.4.1.2 (R Core Team, 2020). Moran’s I test was performed using the package ‘spdep’ (Bivand & Wong, 2018) and negative binomial mixed effect models were performed using the package ‘lme4′ (Bates et al., 2014).
3. Results
3.1. Associations of total green space and various types of green space with SARS-CoV-2 infection rate
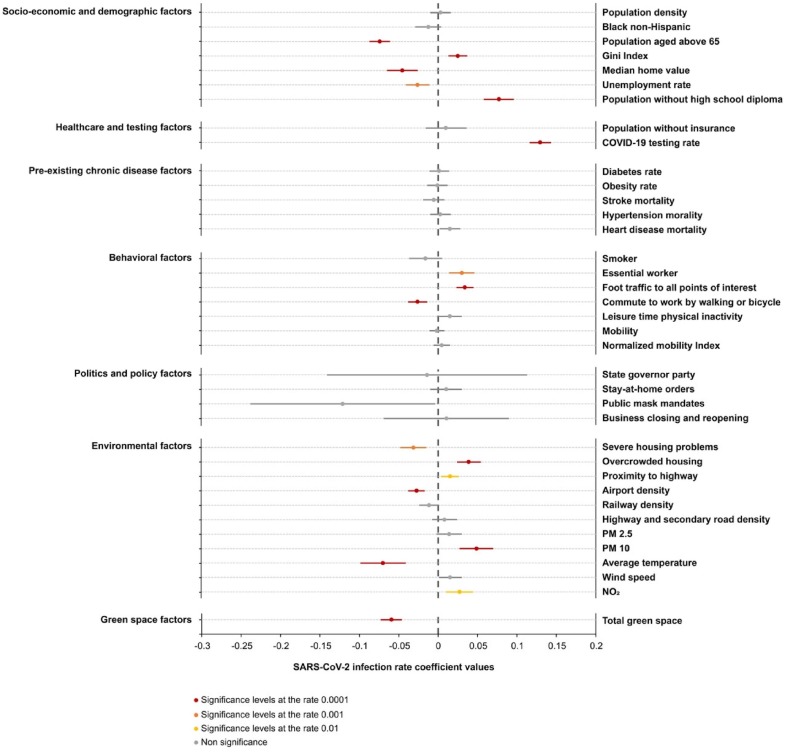
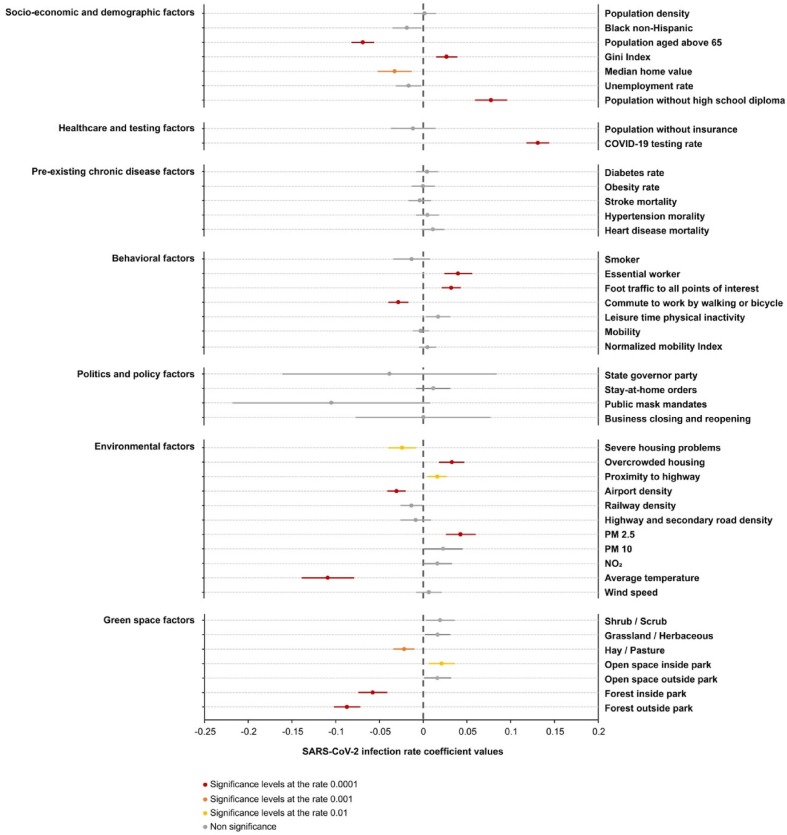
The results of the negative binominal mixed effect model for total green space, seven types of green space and SARS-CoV-2 infection rate are shown in Table 2, Table 3 , respectively. After controlling for covariates, the total green space has a significant and negative association with the SARS-CoV-2 infection rate (β = − 0.059, p < 0.0001) (Fig. 5 ). For the seven types of green spaces, forest inside park (p < 0.0001), forest outside park (p < 0.0001), and hay/pasture (p < 0.001) are significantly negatively associated with SARS-CoV-2 infection rate. Open space inside park is positively associated with SARS-CoV-2 infection rate (p < 0.001) (Fig. 6 ).
Table 2.
Estimated effect of green space on SARS-CoV-2 infection rate after controlling for all covariates in Model 1 (including state as a random effect).
| Variable Categories | Variables | Coefficient | SE | Z Value | P Value |
|---|---|---|---|---|---|
| Socioeconomic and demographic factors | Population density | 0.003 | 0.007 | 0.474 | 0.635 |
| Black non-Hispanic | −0.012 | 0.009 | −1.451 | 0.147 | |
| Population aged 65 above | −0.074 | 0.007 | −11.098 | <0.0001*** | |
| Gini Index | 0.025 | 0.006 | 4.026 | <0.0001*** | |
| Median home value | −0.045 | 0.010 | −4.604 | <0.0001*** | |
| Unemployment rate | −0.026 | 0.007 | −3.495 | <0.001** | |
| Population without high school diploma | 0.077 | 0.010 | 7.948 | <0.0001*** | |
| Healthcare and testing factors | Population without insurance | 0.010 | 0.013 | 0.738 | 0.460 |
| COVID-19 testing rate | 0.130 | 0.007 | 19.325 | <0.0001*** | |
| Pre-existing chronic disease factors | Diabetes rate | 0.001 | 0.006 | 0.174 | 0.862 |
| Obesity rate | −0.001 | 0.007 | −0.140 | 0.888 | |
| Stroke mortality | −0.005 | 0.007 | −0.794 | 0.427 | |
| Hypertension mortality | 0.003 | 0.007 | 0.424 | 0.671 | |
| Heart disease mortality | 0.015 | 0.007 | 2.232 | 0.026 | |
| Behavioral factors | Smoker | −0.016 | 0.011 | −1.470 | 0.142 |
| Essential worker | 0.030 | 0.008 | 3.754 | <0.001** | |
| Foot traffic to all POI | 0.034 | 0.006 | 5.908 | <0.0001*** | |
| Commute to work by walking or bicycle | −0.026 | 0.006 | −4.226 | <0.0001*** | |
| Leisure time physical inactivity | 0.015 | 0.007 | 2.006 | 0.045 | |
| Mobility | −0.002 | 0.005 | −0.319 | 0.750 | |
| Normalized mobility index | 0.005 | 0.005 | 0.899 | 0.368 | |
| Politics and policy factors | State governor party | −0.014 | 0.065 | −0.215 | 0.830 |
| Stay-at-home orders | 0.010 | 0.010 | 1.008 | 0.313 | |
| Public mask mandates | −0.121 | 0.060 | −2.028 | 0.043 | |
| Business closing and reopening | 0.011 | 0.041 | 0.263 | 0.793 | |
| Environmental factors | Severe housing problem | −0.031 | 0.008 | −3.824 | <0.001** |
| Overcrowded housing | 0.039 | 0.008 | 5.115 | <0.0001*** | |
| Proximity to highway | 0.015 | 0.006 | 2.630 | <0.01* | |
| Airport density | −0.027 | 0.005 | −5.069 | <0.0001*** | |
| Railway density | −0.011 | 0.007 | −1.745 | 0.081 | |
| Highway and secondary road density | 0.008 | 0.008 | 1.005 | 0.315 | |
| PM 2.5 | 0.014 | 0.008 | 1.686 | 0.092 | |
| PM 10 | 0.049 | 0.011 | 4.417 | <0.0001*** | |
| NO2 | 0.027 | 0.009 | 3.128 | <0.01* | |
| Average temperature | −0.070 | 0.015 | −4.749 | <0.0001*** | |
| Wind speed | 0.015 | 0.007 | 2.104 | 0.035 | |
| Green space factors | Total green space | −0.059 | 0.007 | −8.502 | <0.0001*** |
Note: * indicates p < 0.01; ** indicates p < 0.001; *** indicates p < 0.0001.
Table 3.
Estimated effect of seven types of green space on SARS-CoV-2 infection rate after controlling for all covariates in Model 2 (including state as a random effect).
| Variable Categories | Variables | Coefficient | SE | Z Value | p Value |
|---|---|---|---|---|---|
| Socioeconomic and demographic factors | Population density | 0.002 | 0.007 | 0.242 | 0.809 |
| Black non-Hispanic | −0.019 | 0.009 | −2.196 | 0.028 | |
| Population aged 65 above | −0.069 | 0.007 | −10.430 | <0.0001*** | |
| Gini Index | 0.027 | 0.006 | 4.375 | <0.0001*** | |
| Median home value | −0.033 | 0.010 | −3.332 | 0.001** | |
| Unemployment rate | −0.016 | 0.007 | −2.209 | 0.027 | |
| Population without high school diploma | 0.078 | 0.010 | 8.085 | <0.0001*** | |
| Healthcare and testing factors | Population without insurance | −0.012 | 0.013 | −0.868 | 0.385 |
| COVID-19 testing rate | 0.131 | 0.007 | 19.912 | <0.0001*** | |
| Pre-existing chronic disease factors | Diabetes rate | 0.004 | 0.006 | 0.697 | 0.486 |
| Obesity rate | 0.000 | 0.007 | −0.052 | 0.959 | |
| Stroke mortality | −0.004 | 0.007 | −0.570 | 0.569 | |
| Hypertension mortality | 0.005 | 0.007 | 0.753 | 0.451 | |
| Heart disease mortality | 0.011 | 0.007 | 1.706 | 0.088 | |
| Behavioral factors | Smoker | −0.013 | 0.011 | −1.220 | 0.223 |
| Essential worker | 0.040 | 0.008 | 4.977 | <0.0001*** | |
| Foot traffic to all POI | 0.032 | 0.006 | 5.650 | <0.0001*** | |
| Commute to work by walking or bicycle | −0.029 | 0.006 | −4.689 | <0.0001*** | |
| Leisure time physical inactivity | 0.017 | 0.007 | 2.319 | 0.020 | |
| Mobility | −0.003 | 0.005 | −0.597 | 0.551 | |
| Normalized mobility index | 0.005 | 0.005 | 0.980 | 0.327 | |
| Politics and policy factors | State governor party | −0.039 | 0.063 | −0.614 | 0.539 |
| Stay-at-home orders | 0.012 | 0.010 | 1.170 | 0.242 | |
| Public mask mandates | −0.105 | 0.058 | −1.815 | 0.070 | |
| Business closing and reopening | 0.000 | 0.039 | 0.006 | 0.995 | |
| Environmental factors | Severe housing problem | −0.024 | 0.008 | −2.969 | 0.003* |
| Overcrowded housing | 0.033 | 0.008 | 4.379 | <0.0001*** | |
| Proximity to highway | 0.016 | 0.006 | 2.864 | 0.004* | |
| Airport density | −0.031 | 0.005 | −5.654 | <0.0001*** | |
| Railway density | −0.013 | 0.006 | −2.079 | 0.038 | |
| Highway and secondary road density | −0.009 | 0.009 | −0.968 | 0.333 | |
| PM 2.5 | 0.043 | 0.009 | 4.909 | <0.0001*** | |
| PM 10 | 0.023 | 0.011 | 2.032 | 0.042 | |
| NO2 | 0.016 | 0.009 | 1.876 | 0.061 | |
| Average temperature | −0.109 | 0.015 | −7.105 | <0.0001*** | |
| Wind speed | 0.006 | 0.007 | 0.881 | 0.378 | |
| Green space factors | Shrub/Scrub | 0.019 | 0.009 | 2.262 | 0.024 |
| Grassland/ Herbaceous | 0.017 | 0.007 | 2.262 | 0.024 | |
| Hay/Pasture | −0.022 | 0.006 | −3.511 | 0.000** | |
| Open space inside park | 0.021 | 0.008 | 2.724 | 0.006* | |
| Open space outside park | 0.016 | 0.008 | 2.040 | 0.041 | |
| Forest inside park | −0.058 | 0.009 | −6.726 | <0.0001*** | |
| Forest outside park | −0.087 | 0.008 | −11.466 | <0.0001*** |
Note: * indicates p < 0.01; ** indicates p < 0.001; *** indicates p < 0.0001.
Fig. 5.
Relationships between total green space, covariates, and SARS-CoV-2 infection (Model 1). Coefficient values represent effect sizes from the negative binomial mixed effects model for the relationship between infection rate of SARS-CoV-2 (cases per 100,000 people) and all variables. Bars represent 95 % CIs and significant variables are shown out red, orange, and yellow. Note: * p < 0.01; ** p < 0.001; *** p < 0.0001.
Fig. 6.
Relationships between different types of green spaces, covariates, and SARS-CoV-2 infection (Model 2). Coefficient values represent effect sizes from the negative binomial mixed effects model for the relationship between infection rate of SARS-CoV-2 (cases per 100,000 people) and all variables. Bars represent 95 % CIs and significant variables are shown out red, orange, and yellow. Note: * p < 0.01; ** p < 0.001; *** p < 0.0001.
Among all green spaces, forest outside park and forest inside park have the greatest effect size on SARS-CoV-2 infection rate (β = −0.087 and β = −0.058, respectively). We found that a one-unit increase in forest inside park is associated with a 5.6 % decrease in SARS-CoV-2 infection rate (IRR 95 % CI: 4.0 %–7.5 %), and a one-unit increase in forest outside park is associated with an 8.3 % decrease in SARS-CoV-2 infection rate (IRR 95 % CI: 7.0 %–9.7 %) (Table 4 ).
Table 4.
Incident rate ratio of seven types of green spaces with SARS-CoV-2 infection rate in overall model after adjusting for covariates (Model 2).
| Green spaces | SARS-CoV-2 IRR (95 % CI) |
|---|---|
| Shrub/Scrub | 1.0195 (1.0026, 1.0367) |
| Grassland/Herbaceous | 1.0167 (1.0022, 1.0314) |
| Hay/Pasture | 0.9785 (0.9668, 0.9905) |
| Open space inside park | 1.0213 (1.0059, 1.0369) |
| Open space outside park | 1.0166 (1.0006, 1.0327) |
| Forest inside park | 0.9441 (0.9284, 0.9601) |
| Forest outside park | 0.9167 (0.9032, 0.9304) |
Note: IRR = incidence rate ratios, CI = confidence interval.
3.2. Forest-SARS-CoV-2 infection rate associations across five levels of urbanicity
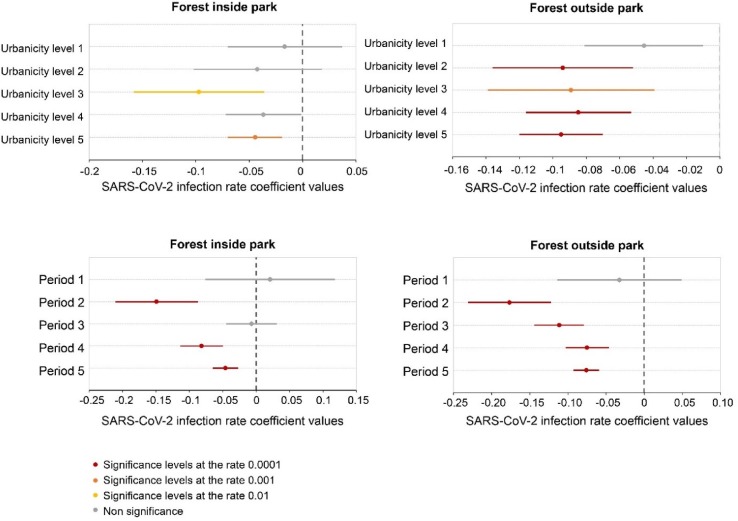
After identifying forest outside park and forest inside park as key green spaces, we further ran separate negative binomial mixed effect models to measure associations between the two forest variables and SARS-CoV-2 infection rate across five levels of urbanicity (Fig. 7 ). The descriptive data of all variables across five urbanicity levels are presented in Table S4 and results are presented in Table S5. Forest inside park is significantly negatively associated with infection rate at urbanicity levels 3 and 5; the association is strongest at level 3 (β = −0.097, p < 0.01). Forest outside park is significantly negatively associated with infection rate across urbanicity levels 2 to 5; the association is strongest at level 5 (β = −0.095, p < 0.0001).
Fig. 7.
The effects of two forest variables with SARS-CoV-2 infection across five levels of urbanicity and five time periods after accounting for other variables (Model 3). Coefficient values represent effect sizes from the negative binomial mixed effects model for the relationship between rate of SARS-CoV-2 (cases per 100,000 people) and green space variables. Bars represent 95 % CIs and significant variables are shown in red, orange, and yellow. Note: * p < 0.01; ** p < 0.001; *** p < 0.0001. The level of urbanicity decreases from level 1 to level 5: level 1 is large metro, Level 2 is medium metro, level 3 is small metro, level 4 is micropolitan, and level 5 is non-core. Period 1: January 22 to March 30, 2020. Period 2: March 31 to June 7, 2020. Period 3: June 8 to August 15, 2020. Period 4: August 16 to October 23, 2020. Period 5: October 24 to December 31, 2020.
3.3. Forest-SARS-CoV-2 infection rate associations across five time periods
Next, we examined the associations between the two forest variables and SARS-CoV-2 infection rate across five time periods. Fig. 7 and Table S6 show the effect sizes of two forest variables on SARS-CoV-2 infection rate across different time periods. Forest outside park has a significant and negative association with the infection rate from periods 2 to 5, and the association is strongest in period 2 (β = −0.177, p < 0.0001). Forest inside park has a significant and negative association in time periods 2, 4 and 5, with the largest effect size in period 2 (β = −0.149, p < 0.0001).
3.4. Associations of population-weighted exposure to forest at varying buffer distances with SARS-CoV-2 infection rate
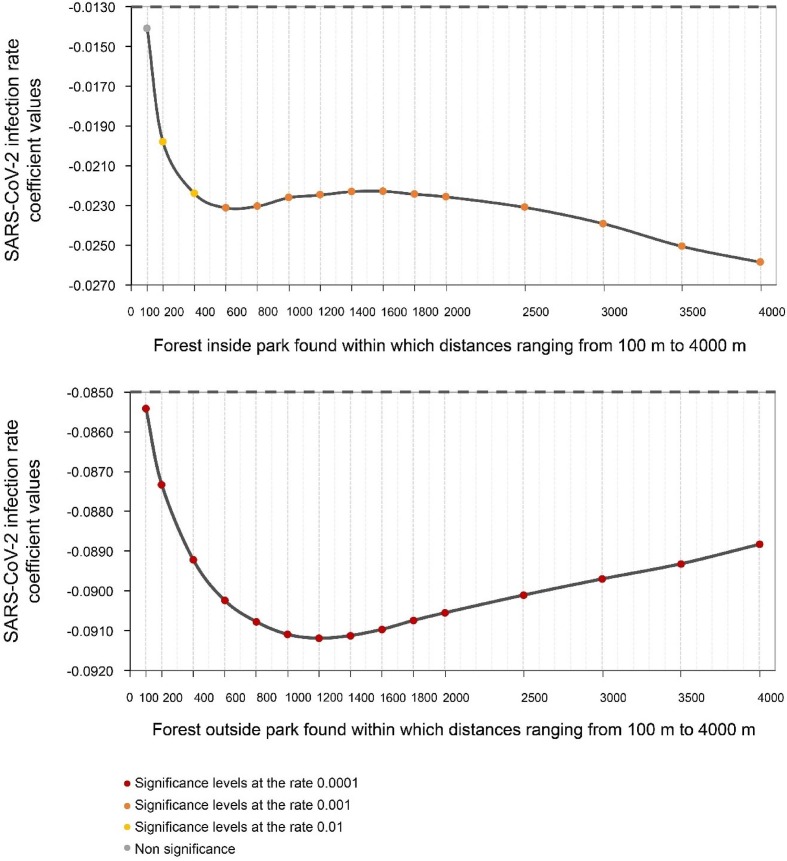
Next, we examined the association of population-weighted exposure to forest at various buffer sizes within walking distance (100 m to 4 km) with the SARS-CoV-2 infection rate. We report the standardized coefficient value representing effect sizes and the 95 % CI in Table 5 and Fig. 8 .
Table 5.
Model results from negative binomial mixed effect model relating to SARS-CoV-2 infection to fixed effect populated weighted green space exposures and all covariates at varying buffer distances, including state as a random effect (Model 4).
| Variables | Buffer size(m) | Beta | SE | z-value | p-value |
|---|---|---|---|---|---|
| Forest inside park | 100 | −0.014 | 0.010 | −1.400 | 0.161 |
| 200 | −0.020 | 0.009 | −2.119 | 0.034* | |
| 400 | −0.022 | 0.009 | −2.498 | 0.012* | |
| 600 | −0.023 | 0.009 | −2.629 | 0.009** | |
| 800 | −0.023 | 0.009 | −2.648 | 0.008** | |
| 1,000 | −0.023 | 0.009 | −2.616 | 0.009** | |
| 1,200 | −0.022 | 0.009 | −2.610 | 0.009** | |
| 1,400 | −0.022 | 0.009 | −2.597 | 0.009** | |
| 1,600 | −0.022 | 0.009 | −2.597 | 0.009** | |
| 1,800 | −0.022 | 0.009 | −2.615 | 0.009** | |
| 2,000 | −0.023 | 0.009 | −2.627 | 0.009** | |
| 2,500 | −0.023 | 0.009 | −2.679 | 0.007** | |
| 3,000 | −0.024 | 0.009 | −2.758 | 0.006** | |
| 3,500 | −0.025 | 0.009 | −2.872 | 0.004** | |
| 4,000 | −0.026 | 0.009 | −2.954 | 0.003** | |
| Forest outside park | 100 | −0.085 | 0.008 | −11.135 | <0.0001*** |
| 200 | −0.087 | 0.008 | −11.244 | <0.0001*** | |
| 400 | −0.089 | 0.008 | −11.404 | <0.0001*** | |
| 600 | −0.090 | 0.008 | −11.510 | <0.0001*** | |
| 800 | −0.091 | 0.008 | −11.578 | <0.0001*** | |
| 1,000 | −0.091 | 0.008 | −11.635 | <0.0001*** | |
| 1,200 | −0.091 | 0.008 | −11.669 | <0.0001*** | |
| 1,400 | −0.091 | 0.008 | −11.692 | <0.0001*** | |
| 1,600 | −0.091 | 0.008 | −11.701 | <0.0001*** | |
| 1,800 | −0.091 | 0.008 | −11.701 | <0.0001*** | |
| 2,000 | −0.091 | 0.008 | −11.705 | <0.0001*** | |
| 2,500 | −0.090 | 0.008 | −11.704 | <0.0001*** | |
| 3,000 | −0.090 | 0.008 | −11.694 | <0.0001*** | |
| 3,500 | −0.089 | 0.008 | −11.677 | <0.0001*** | |
| 4,000 | −0.089 | 0.008 | −11.641 | <0.0001*** |
Fig. 8.
The effects of forest exposure without comfortable walking distance (0–4 km) on infection risk (Model 4). The effects are indicated by the β values and 95 % CI. Coefficient values represent effect sizes from the negative binomial mixed effects model for the relationship between SARS-CoV-2 infection rate and green space variables.
Forest inside park is significantly negatively associated with SARS-CoV-2 infection rate from 200 m to 4 km and reaches an optimal effect at 4,000 m. The exposure buffer-response curve shows the effect size of forest inside park increases as buffer size increases to 600 m, then decreases beyond 600 m, and increase again at 2,500 m, though the increase in effect size remains limited (600 m: β = −0.023 vs 4,000 m: β = −0.026). As shown in Table S13, per one unit increase in exposure to forest in park is linked to 2.3 % decrease in infection rate within 600 m buffers (IRR 95 % CI: 0.6 %–4%) and a 2.6 % decrease at 4,000 m buffer (IRR 95 % CI: 0.9 %–4.2 %) (Table 6 ).
Table 6.
Descriptive data for green space factors at five urbanicity levels.
| Variables | Urbanicity level 1 | Urbanicity level 2 | Urbanicity level 3 | Urbanicity level 4 | Urbanicity level 5 |
|---|---|---|---|---|---|
| Forest inside park | 0.029 | 0.047 | 0.054 | 0.060 | 0.065 |
| Forest outside park | 0.264 | 0.278 | 0.244 | 0.246 | 0.226 |
| Shrub/scrub | 0.039 | 0.067 | 0.077 | 0.093 | 0.104 |
| Grassland/herbaceous | 0.044 | 0.063 | 0.069 | 0.081 | 0.132 |
| Hay/pasture | 0.115 | 0.116 | 0.105 | 0.102 | 0.091 |
| Open space inside park | 0.003 | 0.002 | 0.002 | 0.002 | 0.002 |
| Open space outside park | 0.078 | 0.055 | 0.042 | 0.034 | 0.026 |
Note: The level of urbanicity decreases from level 1 to level 5: level 1 is large metro, Level 2 is medium metro, level 3 is small metro, level 4 is micropolitan, and level 5 is non-core.
Exposure to forest outside park is significantly negatively associated with SARS-CoV-2 infection rate from 100 m to 4 km, reaching the largest effect size around 1,200 m. The exposure buffer-response curve suggests the effect size of forest outside park increases between 100 m and 1,200 m, then decreases beyond 1,200 m. With a one-unit increase in exposure to forest outside park is linked to an 8.7 % decrease in infection rate within 1,200 m buffers (IRR 95 % CI: 7.3–10.1 %).
4. Discussion
This study examines the relationship between green spaces and SARS-CoV-2 infection rate across all 3,108 counties during 2020 in the contiguous United States after controlling for multiple covariates. In the following sections, we first provide interpretations of key findings. Then, we discuss potential impacts and implications of this study. Lastly, we discuss the limitations of this study and opportunities for future research.
4.1. Interpretation of key findings
4.1.1. Why total green space has a significant and negative association with the SARS-CoV-2 infection rate?
We found that the total green space has a significant negative association with the infection rate. Although many studies have summarized that green spaces can make positive impacts on mental and physical health (Jiang et al., 2015, Labib et al., 2020, Markevych et al., 2017, Zhang et al., 2020), a comprehensive interpretation on why green spaces have positive impacts on SARS-CoV-2 infection rate is rarely presented. We argue the association can be interpreted by four causal mechanisms.
Being in green spaces allows people to have normal recreational and social life while maintaining a safer social distance than being in indoor spaces. The primary pathway of SARS-CoV-2 transmission is via aerosol particles and droplets that are exhaled by human hosts (Bourouiba, 2020, Klompas et al., 2020, Zhang et al., 2020). Hence, virus transmission is less likely to occur outdoors than indoors (Leclerc et al., 2020). Comparing to indoor spaces, green spaces can also enable people to maintain adequate physical distancing (Leclerc et al., 2020). In other words, green spaces are a relatively safer social environment than indoor spaces during the SARS-CoV-2 pandemic: they encourage people to leave indoor environments and participate in outdoor activities with other people while maintaining safe social distances (Lu et al., 2021, Schipperijn et al., 2013, Sullivan et al., 2004). Green spaces not only invite people to go outdoors more often (Coley et al., 1997), but also encourage them to stay outdoors longer, reducing their time spent indoors (Braubach et al., 2017, Coley et al., 1997, Grahn and Stigsdotter, 2003). Nevertheless, it is important to point out the “safer social distance” is not always “safe enough”. The risk of infection might be high if large gathering occur in green spaces or they have close contact during social activities, such as conversation, dance party, food-sharing party (Domènech-Montoliu et al., 2021, Peng et al., 2022).
Green spaces can promote physical activity thus enhance immune functioning. Previous studies have reported that green spaces promote physical activity (Cohen et al., 2007, Lu et al., 2019, Lu et al., 2021). Exercising while viewing green landscapes can produce synergic health outcomes, beyond those yielded by exercise alone (Pretty et al., 2005). Numerous studies have suggested that green spaces reduce the risk of obesity by promoting physical activity, making people less vulnerable to SARS-CoV-2 infection (Jia et al., 2021, Jordan and Adab, 2020, Sattar et al., 2020). Physical activities in green spaces can enhance immune functioning (Li et al., 2010, Amatriain-Fernández et al., 2020), thus strengthening resistance to SARS-CoV-2 infection.
Green spaces can reduce mental stress thus enhance immune functioning. Adverse mental state can make people more vulnerable to SARS-CoV-2 virus (Qin et al., 2020, Wang et al., 2021, Yang et al., 2020). Extensive evidence suggests viewing or being in a forest can reduce mental stress (Hunter et al., 2019, Jiang et al., 2016, Ulrich et al., 1991). Elevated stress levels were found to weaken immune functioning (Dhabhar, 2014, Marketon and Glaser, 2008). Exposure to forest enhance immune functioning by increasing the numbers of Natural Killer (NK) cells, lymphocytes, and enhances human NK activity, which would also strengthen resistance to SARS-CoV-2 infection (Li, 2010, Li et al., 2007).
Green spaces can remove ambient pollutants to reduce transmission of virus. Green spaces in urban and rural areas can improve air quality by removing particulates and absorbing aerosols through leaf stomata (Janhäll, 2015, Kumar et al., 2019, Nowak et al., 2006, Nowak et al., 2014, Nowak et al., 2013, Nowak et al., 2018). Because SARS-CoV-2 is transmitted through particles and aerosols, these green spaces may reduce SARS-CoV-2 infection risk (Bourouiba, 2020). Those who have daily exposure to green spaces are less vulnerable to SARS-CoV-2 infection (Fattorini and Regoli, 2020, Paital and Agrawal, 2020, Zhu et al., 2020).
4.1.2. Why do forests have a stronger negative association with infection rate than other green spaces?
In this study, “forest” was defined as “an area dominated by trees, generally greater than 5 m tall, and accounting for greater than 20 % of total vegetation cover” (NLCD, 2016). Forests included large natural forests in rural areas and moderate or smaller patches of trees in urban, suburban, and rural areas.
We found forests have a stronger tie with lower SARS-CoV-2 infection rate than other types of green space. We propose three reasons for that difference. First, forests are more likely to entice people outdoors than other types of green spaces. During the pandemic, more people chose to visit natural forest parks than urban parks for recreational and exercise (Lu et al., 2021). Forests create a more comfortable microclimate than other green spaces without large tree canopy (Li et al., 2019, Ziter et al., 2019). Forested areas, which in our study include lawn or grassland partially covered by tree canopy, provide a more comfortable environment for outdoor activities than a lawn or park without shade.
Second, forests are more effective to boost immune function than other green spaces because forests are more mentally restorative than other green spaces (Li, 2010, Li et al., 2007, Lyu et al., 2019). Forests have a stronger presence of “positive distractions” than other green spaces (Beil and Hanes, 2013, Jiang et al., 2019, Ulrich, 1997): Forests have a complex three-dimensional profile with trees of different sizes, type and age, and a diversity of vegetation, animals, and insects (Beil and Hanes, 2013, Brockerhoff et al., 2017, Trochta et al., 2017, Wood et al., 2018). Those positive distractions allow people to have a greater level of stress reduction, thus enhance their immune functioning to resist the risk of infection (Morey et al., 2015).
Lastly, forests are also more effective at reducing air pollutants than other green spaces, which makes forests more effective to reduce risk of SARS-CoV-2 virus transmission. Researchers found that forests capture particulate pollutants more efficiently than grassland and shrubs, as forests often have more complex foliage, a larger number of trees, more diverse tree heights and canopy sizes, and more diverse tree species (Beckett et al., 2000). A nationwide study in the contiguous United States found that trees and forests removed approximately 17.4 million tonnes of air pollution in 2010, which was estimated to lead to 850 fewer deaths and 670,000 fewer incidents of acute respiratory symptoms (Nowak et al., 2006).
4.1.3. Why does forest outside park have a stronger negative association with infection rate than forest inside park?
We found forest outside park have a greater negative association with the infection rate than the forest inside park. One possible reason is that naturalistic green spaces are more likely to be found in forest outside park. Previous studies have suggested that naturalistic green spaces are more strongly associated with health benefits than urban green spaces (Allard-Poesi et al., 2022).
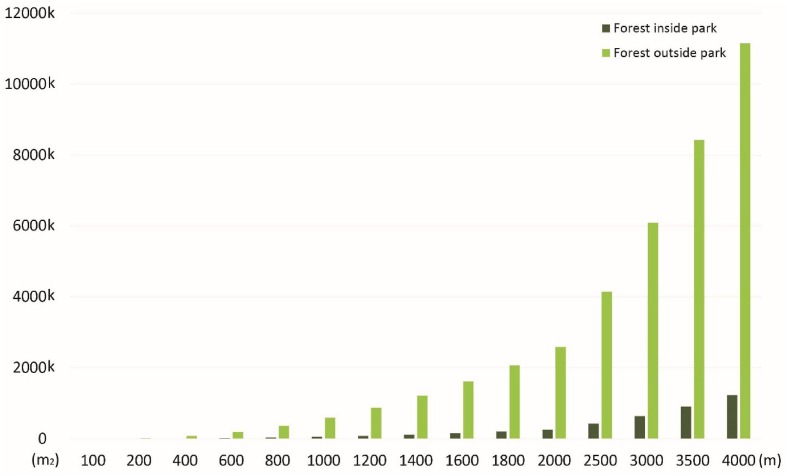
Second, US residents have much higher level of exposure to forest outside park than forest inside park. According to our calculation in this study, population-weighted exposure to forest outside park is 10 times greater than exposure to forest inside park within 4 km (Fig. 9 ). The dominating supply of forest outside park might make the forest outside park have a greater impact than forest inside park.
Fig. 9.
The population-weighted exposure to forest inside park and forest outside park within 4 km. The supply of forest outside park is much more than the supply of forest inside park and this disparity increases as the buffer distance increases.
Third, forest inside park, as a public space, might have a greater responsibility to accommodate more visitors and social gatherings than forest outside park, which makes users of forest inside park have a greater risk of infection than users of forest outside park. Mobility studies found that park visits were associated with higher SARS-CoV-2 infection rate and suggested that parks may serve as locations of virus transmission (DePhillipo et al., 2021, Praharaj and Han, 2021). Other studies suggest outdoor gatherings increase risk of respiratory disease outbreaks (Dixon et al., 2013, Domènech-Montoliu et al., 2021). Thus, increased risk social gatherings may counteract the other benefits of forest inside park.
Finally, the effect of forest inside park might be impacted by shutdown policies (Smith et al., 2021, Volenec et al., 2021). Many parks were fully or partly shut down during the pandemic (Smith et al., 2021).
4.1.4. Why do open spaces have a significantly positive and a non-significant association with SARS-CoV-2 infection rate?
We found open space inside park to be significantly associated with higher SARS-CoV-2 infection rate, and open space outside park to be non-significantly associated with infection rate. In this study, open space is defined as “…. mostly vegetation in the form of lawn grasses. Impervious surfaces account for <20 % of total cover. These areas most commonly include large-lot single-family housing units, parks, golf courses, and vegetation planted in settings for recreation, erosion control, or aesthetic purposes” (NLCD, 2016). Thus, most open space, especially those in parks, are important places for recreational and social activities.
At the first glance, these findings are surprising given that many studies have found that open spaces are benefitical for health although their effects might be smaller than those of forest (please refer to 4.1.2). The most frequently reported benefits include reducing stress, fatigue, and negative emotions (Jiang et al., 2019, Ulrich et al., 1991); promoting physical activities (Giles-Corti et al., 2005); promoting social cohesion (Jennings and Bamkole, 2019, Schmidt et al., 2019); and reducing the incidence of noninfectious chronic diseases, which mainly include cardiovascular diseases, stroke, cancers, and diabetes (Kondo et al., 2018). Open spaces, similar as other green spaces, might enhance human’s resistance to infection risk through enhancing mental health and then immunization functioning, and reduce solid aerosols (e.g., PM 2.5) in the air that might serve as a SARS-CoV-2 carrier as we discussed in 4.4.1.
However, our findings also echo many studies that reported open spaces have mixed impacts of open spaces on SARS-CoV-2 infection rate (Johnson et al., 2020, Klompmaker et al., 2021). It is possible that positive effects of open spaces have been significantly offset by their detrimental impacts. This interpretation is supported by studies that suggest that outdoor social activities, such as mass gathering, talking, or partying, can lead to higher risk of infection (Domènech-Montoliu et al., 2021, Peng et al., 2022). Although open spaces can provide a relatively larger social distancing than indoor spaces, limited supply of open spaces in urban areas may make it hard for people to maintain safe social distancing all the time (Nobajas and Casas, 2020, Shoari et al., 2020). As the pandemic lasted longer than people expected, the pandemic fatigue may also influence people’s compliance of safe social distancing when they gathered in open spaces (Franzen and Wöhner, 2021, Shearston et al., 2021).
4.1.5. How to interpret forest-infection rate associations across five levels of urbanicity?
For the forest-infection rate associations across five levels of urbanicity, we found a key pattern: both forests variables have non-significant associations with the infection rate in large metropolitan counties (Level 1) but the negative associations remain significant in many other less urbanized counties (Level 2–5).
This distinction might be caused by the low supply of green space per capita, especially forest space per capita, in those highly urbanized counties. Studies have found that green space per capita, including forest per capita, is lower in urbanized counties than in other areas (Wen et al., 2013) and social distancing is hard to remain safe when many urban dwellers have to share limited areas of forest spaces (Nobajas et al., 2020). This finding is consistent with a recent study that found population density at the county level is an effective predictor of infection rate in the United States (Wong & Li, 2020), and that severity of SARS-CoV-2 pandemic is often high in high-density cities, such as New York, London, Hong Kong, and Tokyo (Sharifi & Khavarian-Garmsir, 2020).
4.1.6. How to interpret forest-infection rate associations across five time periods?
For the associations across five time periods, we also found a key pattern: the negative associations between two forest variables and infection rate are stronger in an early time periods (period 2) but the negative associations largely remain significant in later time periods (period 3, 4, and 5).
One possible reason might be early in the pandemic, the total number of infected people was small, and the virus was largely spread via social gatherings in private or institutional places (Leclerc et al., 2020, Thakar, 2020). Therefore, the total number of infected people were relatively small in green spaces, and it was easier for people to have recreational activities in green spaces while maintaining safe social distancing. In later stages, the pandemic had widely spread. The risk of infection largely increased due to a higher proportion of infected population and harder to keep safe social distancing.
One additional reason might be the pandemic fatigue developed overtime (Haktanir et al., 2021). The fatigue was mainly due to the increasing levels of mental and physical exhaustion overtime. Recent studies found decline in protective behaviors, lower perceived severity of SARS-CoV-2, and increase in the visit of retail and recreation locations compared to the early stage of the pandemic (Franzen and Wöhner, 2021, Haktanir et al., 2021, Shearston et al., 2021, Petherick et al., 2021, MacIntyre et al., 2021).
Nevertheless, we should emphasize again that the negative associations remain significant across five periods, which suggest impacts of forest on relieving infection rate can keep being robust through a long period of time.
4.1.7. Forests within walking distance associated with reduce infection rate
In this study, we identified an optimal distance to forested areas by considering the spatial distribution of populations and forests across counties. We found that negative associations between forests and infection rate are strongest for forests within moderate walking distance (forest outside park ≤ 1,200 m and forest inside park ≤ 600 m). The radius of optimal buffer zones largely matches the most favorable walking distances in the United States (Yang & Diez-Roux, 2012). Our findings are consistent with other studies that report the significant health benefits of nearby forest and other green spaces (Corraliza and Collado, 2011, Cox et al., 2017, Lee et al., 2019, Oh et al., 2017).
The reason why nearby forest has a stronger effect of relieving infection risk can be interpret as direct and indirect reasons. For the direct reason, nearby forest is more frequently visited by residents than distant forest. More frequent visits can lead to better mental and physical health and then better immunization functioning to resist the infection risk (Kuo, 2015, Roviello et al., 2021). Past studies suggest the frequency of green space visit declines with increasing distance (Coombes et al., 2010, Žlender and Ward Thompson, 2017). An increase in people walking to nearby green space during SARS-CoV-2 pandemic was also observed (Ugolini et al., 2020). For the second reason, nearby forest has a stronger effect on reduce concentration of air pollutants in residential areas, such as PM2.5 and PM10, that might be carriers of SARS-CoV-2 virus (Czwojdzińska et al., 2021, Nor et al., 2021, Qu et al., 2019). Thus, nearby forest, no matter they are accessible or not by public, can reduce the infection risk of people who live in nearby neighborhoods.
4.2. Significance and contributions to knowledge and practice
To our best knowledge, this study is one of the first nationwide studies investigating the relationships between different types of green spaces and SARS-CoV-2 infection rate. The significance and contribution of this study mainly include the following aspects:
The control of key confounding factors in this study is more comprehensive and rigorous than in previous studies. We include socioeconomic and demographic factors, pre-existing chronic disease factors, political and policy factors, healthcare and testing factors, behavioral factors, and climate and environmental factors. In addition, control of bias caused by spatial autocorrelation can further enhance the validity of our findings. After controlling all these factors in statistical analysis, the association between green spaces and infection rate was found to be statistically independent and significant.
Numerous studies have found green space, as a general type of land cover, can be beneficial for health and society already recognized it. This type of generic finding is not informative enough to guide specific policymaking and planning interventions (Lu et al., 2021, Klompmaker et al., 2021). This study moves beyond this limitation by revealing the relationships between various types of green spaces and SARS-CoV-2 infection rate and identifying forest as the key type of green space. Further, the study reveals the relationship between forest and SARS-CoV-2 infection rate across five levels of urbanicity and five periods of time. Lastly, the study reveals the relationship between population-weighted forest and infection rate thus identifying optimal buffer zones that are associated with the lowest inflection risk. Through all these key steps, this study provides more specific evidence to guide practice to reduce the risk of airborne infectious diseases.
4.3. Limitations as future research opportunities
This study has several limitations that should be further investigated by future studies. First, this study presents correlational, rather than causal, findings. A causal relationship between green spaces and infection rate is plausible, based on the mechanisms proposed and a wealth of previous research. Future researchers should conduct experimental studies, including laboratory or natural experiments, to confirm these causal relationships (Jiang et al., 2021, Tyrvainen et al., 2014).
Second, our study focuses on investigating and interpreting the potential effects of green spaces, especially forest, on the infection rate. We find, however, that many other factors are also significantly associated with infection rate, such as the Gini index, overcrowded housing, political factors, numbers of essential workers, modes of transport used for commuting, and public mask mandates. These factors all have significant potential to be the focal point of future studies.
Third, we did not use data collected in 2021, as vaccination programs were implemented in the early months of 2021, likely confounding the relationship between green spaces and infection rate (BBC, 2020). Here again, we see this as an important opportunity for future research. It is necessary to understand the extent to which the vaccination rate alters the relationship between green spaces and the SARS-CoV-2 infection rate.
Fourth, some variables are time-sensitive, e.g., testing rate and social distancing policies. The temporal dynamics were considered by splitting the data into five time periods in this study. Future research may use longitudinal data analysis (e.g., multilevel model) to model such temporal dynamics.
Finally, although this study employed an ecological design that includes a series of population-weighted assessments, inferences cannot be made about individual levels of infection based on aggregate data gathered at the county level. This challenge is difficult to overcome, given the difficulty of acquiring personal SARS-CoV-2 data. Perhaps researchers in countries where individual data is available can address this limitation.
5. Conclusion
This one-year study is one of a few nationwide studies investigating the relationships between different types of green spaces and the SARS-CoV-2 infection rate. The consideration of spatial autocorrelation, population-weighted measure, and control of a variety of covariates adds to the study’s validity. As the whole world continue to battle the SARS-CoV-2 pandemic and prepare preventive solutions for future health crises, we urge them to prioritize equitable and accessible green spaces, especially those that contain forest, as a critical public health strategy.
Funding
This work was supported by the University of Hong Kong [grant numbers 102010054.088616.01100.302.01] and [grant numbers 104006587.088616.01100.301.01] and the Research Grants Council of the Hong Kong SAR [grant number CityU11207520].
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We are grateful that this study received enormous trust and support from the following leaders and colleagues at the University of Hong Kong: Dean Chris Webster, Associate Dean Mathew Pryor, Associate Dean Wilson W.S. Lu of the Faculty of Architecture, Head Eric H. Schuldenfrei of the Department of Architecture, Head Ivan Valin of the Division of Landscape Architecture. We appreciate valuable comments and suggestions from Chao Song, Matthew Browning, Lan Luo, and Wenyan Xu.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.landurbplan.2022.104583.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Abedi V., Olulana O., Avula V., Chaudhary D., Khan A., Shahjouei S.…Zand R. Racial, economic, and health inequality and COVID-19 infection in the United States. Journal of Racial and Ethnic Health Disparities. 2020;8:1–11. doi: 10.1007/s40615-020-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akpinar A., Barbosa-Leiker C., Brooks K.R. Does green space matter? Exploring relationships between green space type and health indicators. Urban Forestry & Urban Greening. 2016;20:407–418. [Google Scholar]
- Allard-Poesi F., Matos L.B.S., Massu J. Not all types of nature have an equal effect on urban residents’ well-being: A structural equation model approach. Health & place. 2022;74 doi: 10.1016/j.healthplace.2022.102759. [DOI] [PubMed] [Google Scholar]
- Amatriain-Fernández S., Gronwald T., Murillo-Rodríguez E., Imperatori C., Solano A.F., Latini A., Budde H. Physical exercise potentials against viral diseases like COVID-19 in the elderly. Frontiers in Medicine. 2020;7:379. doi: 10.3389/fmed.2020.00379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr H.S., Du H., Marshall M., Dong E., Squire M.M., Gardner L.M. Association between mobility patterns and COVID-19 transmission in the USA: A mathematical modelling study. The Lancet Infectious Diseases. 2020;20(11):1247–1254. doi: 10.1016/S1473-3099(20)30553-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates, D., Mächler, M., Bolker, B., & Walker, S. (2014). Fitting linear mixed-effects models using lme4. arXiv preprint:1406.5823.
- BBC. (2020). Covid-19: First vaccine given in US as roll-out begins. Retrieved 1 July 2021 from https://www.bbc.com/news/world-us-canada-55305720.
- Beckett K.P., Freer-Smith P.H., Taylor G. Particulate pollution capture by urban trees: Effect of species and windspeed. Global Change Biology. 2000;6(8):995–1003. [Google Scholar]
- Beil K., Hanes D. The influence of urban natural and built environments on physiological and psychological measures of stress-A pilot study. International Journal of Environmental Research and Public Health. 2013;10(4):1250–1267. doi: 10.3390/ijerph10041250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bivand R.S., Wong D.W. Comparing implementations of global and local indicators of spatial association. Test. 2018;27(3):716–748. [Google Scholar]
- Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID-19. JAMA. 2020;323(18):1837–1838. doi: 10.1001/jama.2020.4756. [DOI] [PubMed] [Google Scholar]
- Braubach M., Egorov A., Mudu P., Wolf T., Ward Thompson C., Martuzzi M. In: Nature-based solutions to climate change adaptation in urban areas: Linkages between science, policy and practice. Kabisch N., Korn H., Stadler J., Bonn A., editors. Springer International Publishing; 2017. Effects of urban green space on environmental health, equity and resilience; pp. 187–205. [DOI] [Google Scholar]
- Brockerhoff E.G., Barbaro L., Castagneyrol B., Forrester D.I., Gardiner B., González-Olabarria J.R.…Jactel H. Forest biodiversity, ecosystem functioning and the provision of ecosystem services. Biodiversity and Conservation. 2017;26(13):3005–3035. [Google Scholar]
- Browning M.H.E.M., Rigolon A., McAnirlin O., Yoon H. Where greenspace matters most: A systematic review of urbanicity, greenspace, and physical health. Landscape and Urban Planning. 2022;217 [Google Scholar]
- Bulfone T.C., Malekinejad M., Rutherford G.W., Razani N. Outdoor transmission of SARS-CoV-2 and other respiratory viruses: A systematic review. The Journal of Infectious Diseases. 2021;223(4):550–561. doi: 10.1093/infdis/jiaa742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carteni A., Di Francesco L., Martino M. How mobility habits influenced the spread of the COVID-19 pandemic: Results from the Italian case study. Science of the Total Environment. 2020;741 doi: 10.1016/j.scitotenv.2020.140489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarty, R. K., Beeler, P., Liu, P., Goswami, S., Harvey, R. D., Pervez, S., van Donkelaar, A., & Martin, R. V. (2021). Ambient PM2. 5 exposure and rapid spread of COVID-19 in the United States. Science of the Total Environment, 760, 143391. [DOI] [PMC free article] [PubMed]
- Chang D., H., Jiang B., Wong N., H., Wong J., J., Webster C., Lee T., M. The human posterior cingulate and the stress-response benefits of viewing green urban landscapes. NeuroImage. 2021;226(117555) doi: 10.1016/j.neuroimage.2020.117555. [DOI] [PubMed] [Google Scholar]
- Chen B., Song Y., Jiang T., Chen Z., Huang B., Xu B. Real-time estimation of population exposure to PM2. 5 using mobile-and station-based big data. International Journal of Environmental Research and Public Health. 2018;15(4):573. doi: 10.3390/ijerph15040573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clerkin K.J., Fried J.A., Raikhelkar J., Sayer G., Griffin J.M., Masoumi A.…Rabbani L. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- Clinton J., Cohen J., Lapinski J., Trussler M. Partisan pandemic: How partisanship and public health concerns affect individuals’ social mobility during COVID-19. Science Advance. 2021;7(2) doi: 10.1126/sciadv.abd7204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston S.A., Natale G., Link B.G. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: A examination of the emergence of social inequalities. Social Science & Medicine. 2021;268 doi: 10.1016/j.socscimed.2020.113554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D.A., McKenzie T.L., Sehgal A., Williamson S., Golinelli D., Lurie N. Contribution of public parks to physical activity. American Journal of Public Health. 2007;97(3):509–514. doi: 10.2105/ajph.2005.072447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coley R.L., Kuo F.E., Sullivan W.C. Where does community grow? The social context created by nature in urban public housing. Environment and Behavior. 1997;29(4):468–494. [Google Scholar]
- Coombes E., Jones A.P., Hillsdon M. The relationship of physical activity and overweight to objectively measured green space accessibility and use. Social Science & Medicine. 2010;70(6):816–822. doi: 10.1016/j.socscimed.2009.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corraliza J.A., Collado S. Nearby nature as a moderator of stress during childhood. Psicothema. 2011;23(2):221–226. [PubMed] [Google Scholar]
- Cox D.T.C., Shanahan D.F., Hudson H.L., Plummer K.E., Siriwardena G.M., Fuller R.A.…Gaston K.J. Doses of neighborhood nature: The benefits for mental health of living with nature. BioScience. 2017;67(2):147–155. [Google Scholar]
- Czwojdzińska M., Terpińska M., Kuźniarski A., Płaczkowska S., Piwowar A. Exposure to PM2.5 and PM10 and COVID-19 infection rates and mortality: A one-year observational study in Poland. Biomedical Journal. 2021 doi: 10.1016/j.bj.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePhillipo N.N., Chahla J., Busler M., LaPrade R.F. Mobile phone gps data and prevalence of covid-19 infections: Quantifying parameters of social distancing in the us. Archives of Bone and Joint Surgery. 2021;9(2):217. doi: 10.22038/abjs.2020.48515.2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhabhar F.S. Effects of stress on immune function: The good, the bad, and the beautiful. Immunologic Research. 2014;58(2):193–210. doi: 10.1007/s12026-014-8517-0. [DOI] [PubMed] [Google Scholar]
- Dixon, M., Ishola, D., & Phin, N. (2013). Impact of mass gatherings on an influenza pandemic: Scientific evidence base review.
- Domènech-Montoliu S., Pac-Sa M.R., Vidal-Utrillas P., Latorre-Poveda M., Del Rio-González A., Ferrando-Rubert S.…Badenes-Marques G. Mass gathering events and COVID-19 transmission in Borriana (Spain): A retrospective cohort study. PLoS ONE. 2021;16(8):e0256747. doi: 10.1371/journal.pone.0256747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan G.H., Michael Y.L., Butry D.T., Sullivan A.D., Chase J.M. Urban trees and the risk of poor birth outcomes. Health & Place. 2011;17(1):390–393. doi: 10.1016/j.healthplace.2010.11.004. [DOI] [PubMed] [Google Scholar]
- Ekkel E.D., de Vries S. Nearby green space and human health: Evaluating accessibility metrics. Landscape and Urban Planning. 2017;157:214–220. [Google Scholar]
- Esri. (2021). USA Parks. Retrieved July 20 2021 from https://www.arcgis.com/home/item.html?id=578968f975774d3fab79fe56c8c90941.
- Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? The lancet Respiratory Medicine. 2020;8(4):e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattorini D., Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environmental Pollution. 2020;264 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figueroa J.F., Wadhera R.K., Mehtsun W.T., Riley K., Phelan J., Jha A.K. Association of race, ethnicity, and community-level factors with COVID-19 cases and deaths across U.S. counties. Healthcare (Amst) 2021;9(1) doi: 10.1016/j.hjdsi.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fowler J.H., Hill S.J., Levin R., Obradovich N. Stay-at-home orders associate with subsequent decreases in COVID-19 cases and fatalities in the United States. PLoS ONE. 2021;16(6):e0248849. doi: 10.1371/journal.pone.0248849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzen A., Wöhner F. Fatigue during the COVID-19 pandemic: Evidence of social distancing adherence from a panel study of young adults in Switzerland. PLoS ONE. 2021;16(12):e0261276. doi: 10.1371/journal.pone.0261276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frumkin H. COVID-19, the built environment, and health. Environmental Health Perspectives. 2021;129(7) doi: 10.1289/EHP8888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskin D.J., Zare H., Delarmente B.A. Geographic disparities in COVID-19 infections and deaths: The role of transportation. Transport Policy. 2021;102:35–46. doi: 10.1016/j.tranpol.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles-Corti B., Broomhall M.H., Knuiman M., Collins C., Douglas K., Ng K.…Donovan R.J. Increasing walking: How important is distance to, attractiveness, and size of public open space? American Journal of Preventive Medicine. 2005;28(2):169–176. doi: 10.1016/j.amepre.2004.10.018. [DOI] [PubMed] [Google Scholar]
- Grahn P., Stigsdotter U.A. Landscape planning and stress. Urban Forestry and Urban Greening. 2003;2(1):1–18. [Google Scholar]
- Haktanir A., Can N., Seki T., Kurnaz M.F., Dilmaç B. Do we experience pandemic fatigue? Current state, predictors, and prevention. Current Psychology. 2021 doi: 10.1007/s12144-021-02397-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He D., Miao J., Lu Y., Song Y., Chen L., Liu Y. Urban greenery mitigates the negative effect of urban density on older adults’ life satisfaction: Evidence from Shanghai, China. Cities. 2022;124 [Google Scholar]
- Heo S., Lim C.C., Bell M.L. Relationships between Local Green Space and Human Mobility Patterns during COVID-19 for Maryland and California, USA. Sustainability. 2020;12(22):9401. [Google Scholar]
- Huang Q., Jackson S., Derakhshan S., Lee L., Pham E., Jackson A., Cutter S.L. Urban-rural differences in COVID-19 exposures and outcomes in the South: A preliminary analysis of South Carolina. PLoS ONE. 2021;16(2):e0246548. doi: 10.1371/journal.pone.0246548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter M.R., Gillespie B.W., Chen S.-Y.-P. Urban nature experiences reduce stress in the context of daily life based on salivary biomarkers. Frontiers in Psychology. 2019;10(722) doi: 10.3389/fpsyg.2019.00722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janhäll S. Review on urban vegetation and particle air pollution – Deposition and dispersion. Atmospheric Environment. 2015;105:130–137. [Google Scholar]
- Jennings V., Bamkole O. The relationship between social cohesion and urban green space: An avenue for health promotion. International Journal of Environmental Research and Public Health. 2019;16(3):452. doi: 10.3390/ijerph16030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia P., Cao X., Yang H., Dai S., He P., Huang G.…Wang Y. Green space access in the neighbourhood and childhood obesity. Obesity Reviews. 2021;22(S1):e13100. doi: 10.1111/obr.13100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang B., Chang C.-Y., Sullivan W.C. A dose of nature: Tree cover, stress reduction, and gender differences. Landscape and Urban Planning. 2014;132:26–36. [Google Scholar]
- Jiang B., He J., Chen J., Larsen L. Moderate is optimal: A simulated driving experiment reveals freeway landscape matters for driving performance. Urban Forestry & Urban Greening. 2021;58(126976) [Google Scholar]
- Jiang B., He J., Chen J., Larsen L., Wang H. Perceived green at speed: A simulated driving experiment raises new questions for attention restoration theory and stress reduction theory. Environment and Behavior. 2020 0013916520947111. [Google Scholar]
- Jiang B., Larsen L., Deal B., Sullivan W.C. A dose–response curve describing the relationship between tree cover density and landscape preference. Landscape and Urban Planning. 2015;139:16–25. [Google Scholar]
- Jiang B., Li D., Larsen L., Sullivan W.C. A dose-response curve describing the relationship between urban tree cover density and self-reported stress recovery. Environment and Behavior. 2016;48(4):607–629. [Google Scholar]
- Jiang, B., Schmillen, R., & Sullivan, W. C. (2018). How to waste a break: using portable electronic devices substantially counteracts attention enhancement effects of green spaces. Environment and Behavior, 0013916518788603.
- Jiang B., Schmillen R., Sullivan W.C. How to waste a break: Using portable electronic devices substantially counteracts attention enhancement effects of green spaces. Environment and Behavior. 2019;51(9–10):1133–1160. [Google Scholar]
- Jiang B., Shen K., Sullivan W.C., Yang Y., Liu X., Lu Y. A natural experiment reveals impacts of built environment on suicide rate: Developing an environmental theory of suicide. Science of The Total Environment. 2021;776 doi: 10.1016/j.scitotenv.2021.145750. [DOI] [PubMed] [Google Scholar]
- Jiang B., Wang H., Larsen L., Bao F., Li Z., Pryor M. Quality of sweatshop factory outdoor environments matters for workers’ stress and anxiety: A participatory smartphone-photography survey. Journal of Environmental Psychology. 2019;65 [Google Scholar]
- Johnson, T. F., Hordley, L. A., Greenwell, M. P., & Evans, L. C. (2020). Effect of park use and landscape structure on COVID-19 transmission rates. medRxiv, 2020.20215731. [DOI] [PMC free article] [PubMed]
- Jordan R.E., Adab P. Who is most likely to be infected with SARS-CoV-2? The Lancet Infectious Diseases. 2020;20(9):995–996. doi: 10.1016/S1473-3099(20)30395-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karaye I.M., Horney J.A. The impact of social vulnerability on COVID-19 in the US: An analysis of spatially varying relationships. American Journal of Preventive Medicine. 2020;59(3):317–325. doi: 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kartal M.T., Depren Ö., Depren S.K. The relationship between mobility and COVID-19 pandemic: Daily evidence from an emerging country by causality analysis. Transportation Research Interdisciplinary Perspectives. 2021;10 doi: 10.1016/j.trip.2021.100366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim G., Miller P.A. The impact of green infrastructure on human health and well-being: The example of the Huckleberry Trail and the Heritage Community Park and Natural Area in Blacksburg, Virginia. Sustainable Cities and Society. 2019;48 [Google Scholar]
- Klompas M., Baker M.A., Rhee C. Airborne transmission of SARS-CoV-2: Theoretical considerations and available evidence. JAMA. 2020;324(5):441–442. doi: 10.1001/jama.2020.12458. [DOI] [PubMed] [Google Scholar]
- Klompmaker J.O., Hart J.E., Holland I., Sabath M.B., Wu X., Laden F.…James P. County-level exposures to greenness and associations with COVID-19 incidence and mortality in the United States. Environmental Research. 2021;199 doi: 10.1016/j.envres.2021.111331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo M.C., Fluehr J.M., McKeon T., Branas C.C. Urban green space and its impact on human health. International Journal of Environmental Research and Public Health. 2018;15(3):445. doi: 10.3390/ijerph15030445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar P., Druckman A., Gallagher J., Gatersleben B., Allison S., Eisenman T.S.…Morawska L. The nexus between air pollution, green infrastructure and human health. Environment International. 2019;133 doi: 10.1016/j.envint.2019.105181. [DOI] [PubMed] [Google Scholar]
- Kuo, F., & Sullivan, W. (2001). Environment and crime in the inner city: does vegetation reduce crime? Environment and Behavior, 33. Kuo, F. E., & Sullivan, W. C. (2001). Aggression and violence in the inner city – Effects of environment via mental fatigue. Environment and Behavior, 33(4), 543-571.
- Kuo M. How might contact with nature promote human health? Promising mechanisms and a possible central pathway. Frontiers in Psychology. 2015;6:1093. doi: 10.3389/fpsyg.2015.01093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labib S.M., Lindley S., Huck J.J. Spatial dimensions of the influence of urban green-blue spaces on human health: A systematic review. Environmental Research. 2020;180 doi: 10.1016/j.envres.2019.108869. [DOI] [PubMed] [Google Scholar]
- Leclerc Q., Fuller N., Knight L., Null N., Funk S., Knight G. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Research. 2020;5(83) doi: 10.12688/wellcomeopenres.15889.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M., Kim S., Ha M. Community greenness and neurobehavioral health in children and adolescents. Science of The Total Environment. 2019;672:381–388. doi: 10.1016/j.scitotenv.2019.03.454. [DOI] [PubMed] [Google Scholar]
- Li J., Liu J., Srebric J., Hu Y., Liu M., Su L., Wang S. The effect of tree-planting patterns on the microclimate within a courtyard. Sustainability. 2019;11(6) [Google Scholar]
- Li Q. Effect of forest bathing trips on human immune function. Environmental Health and Preventive Medicine. 2010;15(1):9–17. doi: 10.1007/s12199-008-0068-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Kobayashi M., Inagaki H., Hirata Y., Li Y.J., Hirata K.…Kagawa T. A day trip to a forest park increases human natural killer activity and the expression of anti-cancer proteins in male subjects. Journal of Biological Regulators and Homeostatic Agents. 2010;24(2):157–165. [PubMed] [Google Scholar]
- Li Q., Morimoto K., Nakadai A., Inagaki H., Katsumata M., Shimizu T.…Miyazaki Y. Forest bathing enhances human natural killer activity and expression of anti-cancer proteins. International Journal of Immunopathology and Pharmacology. 2007;20(2_suppl):3–8. doi: 10.1177/03946320070200S202. [DOI] [PubMed] [Google Scholar]
- Lu Y. Using Google Street View to investigate the association between street greenery and physical activity. Landscape and Urban Planning. 2018;191 [Google Scholar]
- Lu Y., Chen L., Liu X., Yang Y., Sullivan W.C., Xu W.…Jiang B. Green spaces mitigate racial disparity of health: A higher ratio of green spaces indicates a lower racial disparity in SARS-CoV-2 infection rates in the USA. Environment International. 2021;152 doi: 10.1016/j.envint.2021.106465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y., Yang Y., Sun G., Gou Z. Associations between overhead-view and eye-level urban greenness and cycling behaviors. Cities. 2019;88:10–18. [Google Scholar]
- Lu Y., Zhao J., Wu X., Lo S.M. Escaping to nature during a pandemic: A natural experiment in Asian cities during the COVID-19 pandemic with big social media data. Science of the Total Environment. 2021;777 [Google Scholar]
- Lyu B., Zeng C., Xie S., Li D., Lin W., Li N.…Chen Q. Benefits of a three-day bamboo forest therapy session on the psychophysiology and immune system responses of male college students. International Journal of Environmental Research and Public Health. 2019;16(24):4991. doi: 10.3390/ijerph16244991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J., Zhu H., Li P., Liu C., Li F., Luo Z.…Li L. Spatial Patterns of the Spread of COVID-19 in Singapore and the Influencing Factors. ISPRS International Journal of Geo-Information. 2022;11(3):152. [Google Scholar]
- MacIntyre C.R., Nguyen P.-Y., Chughtai A.A., Trent M., Gerber B., Steinhofel K., Seale H. Mask use, risk-mitigation behaviours and pandemic fatigue during the COVID-19 pandemic in five cities in Australia, the UK and USA: A cross-sectional survey. International Journal of Infectious Diseases. 2021;106:199–207. doi: 10.1016/j.ijid.2021.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marketon J.I.W., Glaser R. Stress hormones and immune function. Cellular Immunology. 2008;252(1–2):16–26. doi: 10.1016/j.cellimm.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Markevych I., Schoierer J., Hartig T., Chudnovsky A., Hystad P., Dzhambov A.M.…Fuertes E. Exploring pathways linking greenspace to health: Theoretical and methodological guidance. Environmental Research. 2017;158:301–317. doi: 10.1016/j.envres.2017.06.028. [DOI] [PubMed] [Google Scholar]
- McGrail D.J., Dai J., McAndrews K.M., Kalluri R. Enacting national social distancing policies corresponds with dramatic reduction in COVID19 infection rates. PLoS ONE. 2020;15(7):e0236619. doi: 10.1371/journal.pone.0236619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin, J. M., Khan, F., Pugh, S., Angulo, F. J., Schmitt, H.-J., Isturiz, R. E., Jodar, L., & Swerdlow, D. L. (2020). County-level Predictors of Coronavirus Disease 2019 (COVID-19) Cases and Deaths in the United States: What Happened, and Where Do We Go from Here? Clinical Infectious Diseases, 73(7), e1814-e1821. [DOI] [PMC free article] [PubMed]
- Mena G.E., Martinez P.P., Mahmud A.S., Marquet P.A., Buckee C.O., Santillana M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago. Chile. Science. 2021;372(6545) doi: 10.1126/science.abg5298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell R., Popham F. Effect of exposure to natural environment on health inequalities: An observational population study. The lancet. 2008;372(9650):1655–1660. doi: 10.1016/S0140-6736(08)61689-X. [DOI] [PubMed] [Google Scholar]
- Morey J.N., Boggero I.A., Scott A.B., Segerstrom S.C. Current directions in stress and human immune function. Current Opinion in Psychology. 2015;5:13–17. doi: 10.1016/j.copsyc.2015.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller N.F., Wagner C., Frazar C.D., Roychoudhury P., Lee J., Moncla L.H.…Bedford T. Viral genomes reveal patterns of the SARS-CoV-2 outbreak in Washington State. Science Translational Medicine. 2021;13(595):abf0202. doi: 10.1126/scitranslmed.abf0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCHS. (2017). NCHS Urban-Rural Classification Scheme for Counties. Retrieved July 20 2021 from https://www.cdc.gov/nchs/data_access/urban_rural.htm.
- Neelon B., Mutiso F., Mueller N.T., Pearce J.L., Benjamin-Neelon S.E. Associations between governor political affiliation and COVID-19 cases, deaths, and testing in the US. American Journal of Preventive Medicine. 2021;61(1):115–119. doi: 10.1016/j.amepre.2021.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NLCD. (2016). National Land Cover Database Class Legend and Description. Retrieved July 20 2021 from https://www.mrlc.gov/data/legends/national-land-cover-database-class-legend-and-description.
- Nobajas, A., I Casas, J. G., I Agusti, D. P., & Peacock, A. J. (2020). Lack of sufficient public space can limit the effectiveness of COVID-19’s social distancing measures. medRxiv, 2020.2006.2007.20124982.
- Nor, N. S. M., Yip, C. W., Ibrahim, N., Jaafar, M. H., Rashid, Z. Z., Mustafa, N., Hamid, H. H. A., Chandru, K., Latif, M. T., Saw, P. E., Lin, C. Y., Alhasa, K. M., Hashim, J. H., & Nadzir, M. S. M. (2021, 2021/01/28). Particulate matter (PM2.5) as a potential SARS-CoV-2 carrier. Scientific Reports, 11(1), 2508. https://doi.org/10.1038/s41598-021-81935-9. [DOI] [PMC free article] [PubMed]
- Nowak D.J., Crane D.E., Stevens J.C. Air pollution removal by urban trees and shrubs in the United States. Urban Forestry and Urban Greening. 2006;4(3–4):115–123. [Google Scholar]
- Nowak D.J., Hirabayashi S., Bodine A., Greenfield E. Tree and forest effects on air quality and human health in the United States. Environmental Pollution. 2014;193:119–129. doi: 10.1016/j.envpol.2014.05.028. [DOI] [PubMed] [Google Scholar]
- Nowak D.J., Hirabayashi S., Bodine A., Hoehn R. Modeled PM2.5 removal by trees in ten U.S. cities and associated health effects. Environmental Pollution. 2013;178:395–402. doi: 10.1016/j.envpol.2013.03.050. [DOI] [PubMed] [Google Scholar]
- Nowak D.J., Hirabayashi S., Doyle M., McGovern M., Pasher J. Air pollution removal by urban forests in Canada and its effect on air quality and human health. Urban Forestry & Urban Greening. 2018;29:40–48. [Google Scholar]
- Oh, B., Lee, K. J., Zaslawski, C., Yeung, A., Rosenthal, D., Larkey, L., & Back, M. (2017). Health and well-being benefits of spending time in forests: systematic review. Environmental Health and Preventive Medicine, 22(1), 71-71. [DOI] [PMC free article] [PubMed]
- Paital B., Agrawal P.K. Air pollution by NO 2 and PM 2.5 explains COVID-19 infection severity by overexpression of angiotensin-converting enzyme 2 in respiratory cells: A review. Environmental Chemistry Letters. 2020:1–18. doi: 10.1007/s10311-020-01091-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan J., Bardhan R., Jin Y. Spatial distributive effects of public green space and COVID-19 infection in London. Urban Forestry & Urban Greening. 2021;62 doi: 10.1016/j.ufug.2021.127182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons R., Tassinary L.G., Ulrich R.S., Hebl M.R., Grossman-Alexander M. The view from the road: Implications for stress recovery and immunization. Journal of Environmental Psychology. 1998;18(2):113–140. [Google Scholar]
- Peng, Z., Rojas, A. P., Kropff, E., Bahnfleth, W., Buonanno, G., Dancer, S., Kurnitski, J., Li, Y., Loomans, M. G., & Marr, L. C. (2022). Practical indicators for risk of airborne transmission in shared indoor environments and their application to covid-19 outbreaks. Environmental science & technology. [DOI] [PMC free article] [PubMed]
- Petherick A., Goldszmidt R., Andrade E.B., Furst R., Hale T., Pott A., Wood A. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nature Human Behaviour. 2021;5(9):1145–1160. doi: 10.1038/s41562-021-01181-x. [DOI] [PubMed] [Google Scholar]
- Praharaj S., Han H. Human mobility impacts on the surging incidence of COVID-19 in India. Geographical Research. 2021 [Google Scholar]
- Pretty J., Peacock J., Sellens M., Griffin M. The mental and physical health outcomes of green exercise. International Journal of Environmental Health Research. 2005;15(5):319–337. doi: 10.1080/09603120500155963. [DOI] [PubMed] [Google Scholar]
- Pro G., Hubach R., Wheeler D., Camplain R., Haberstroh S., Giano Z.…Baldwin J.A. Differences in US COVID-19 case rates and case fatality rates across the urban-rural continuum. Rural and Remote Health. 2020;20(3):6074. doi: 10.22605/RRH6074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y.…Tian D.S. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clinical Infectious Disease. 2020;71(15):762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qu H., Lu X., Liu L., Ye Y. Effects of traffic and urban parks on PM10 and PM2.5 mass concentrations. Energy Sources, Part A: Recovery, Utilization, and Environmental Effects. 2019:1–13. [Google Scholar]
- R Core Team. (2020). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2020. Retrieved 1 July 2021 from http://www.R-project.org.
- Roviello V., Gilhen-Baker M., Vicidomini C., Roviello G.N. Forest-bathing and physical activity as weapons against COVID-19: A review. Environmental chemistry letters. 2021:1–10. doi: 10.1007/s10311-021-01321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sattar N., McInnes I.B., McMurray J.J.V. Obesity Is a Risk Factor for Severe COVID-19 Infection. Circulation. 2020;142(1):4–6. doi: 10.1161/CIRCULATIONAHA.120.047659. [DOI] [PubMed] [Google Scholar]
- Schipperijn J., Bentsen P., Troelsen J., Toftager M., Stigsdotter U.K. Associations between physical activity and characteristics of urban green space. Urban Forestry & Urban Greening. 2013;12(1):109–116. [Google Scholar]
- Schmidt T., Kerr J., Schipperijn J. Associations between neighborhood open space features and walking and social interaction in older adults—a mixed methods study. Geriatrics. 2019;4(3):41. doi: 10.3390/geriatrics4030041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifi, A., & Khavarian-Garmsir, A. R. (2020). The COVID-19 pandemic: Impacts on cities and major lessons for urban planning, design, and management. The Science of the Total Environment, 749, 142391-142391. [DOI] [PMC free article] [PubMed]
- Shearston J.A., Martinez M.E., Nunez Y., Hilpert M. Social-distancing fatigue: Evidence from real-time crowd-sourced traffic data. Science of The Total Environment. 2021;792 doi: 10.1016/j.scitotenv.2021.148336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoari N., Ezzati M., Baumgartner J., Malacarne D., Fecht D. Accessibility and allocation of public parks and gardens in England and Wales: A COVID-19 social distancing perspective. PLoS ONE. 2020;15(10):e0241102. doi: 10.1371/journal.pone.0241102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M.K.S., Smit I.P., Swemmer L.K., Mokhatla M.M., Freitag S., Roux D.J., Dziba L. Sustainability of protected areas: Vulnerabilities and opportunities as revealed by COVID-19 in a national park management agency. Biological Conservation. 2021;255 [Google Scholar]
- Sorichetta A., Hornby G.M., Stevens F.R., Gaughan A.E., Linard C., Tatem A.J. High-resolution gridded population datasets for Latin America and the Caribbean in 2010, 2015, and 2020. Scientific Data. 2015;2(1):1–12. doi: 10.1038/sdata.2015.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spotswood E.N., Benjamin M., Stoneburner L., Wheeler M.M., Beller E.E., Balk D.…McDonald R.I. Nature inequity and higher COVID-19 case rates in less-green neighbourhoods in the United States. Nature Sustainability. 2021;4(12):1092–1098. [Google Scholar]
- Stier, A. J., Berman, M. G., & Bettencourt, L. (2020). COVID-19 attack rate increases with city size. arXiv preprint arXiv:2003.10376.
- Sullivan, W. C., & Bartlett, P. F. (2005). Nature at home: an evolutionary perspective. Urban Place: Reconnecting with the Natural World, Peggy F. Bartlett, ed.(Cambridge: MIT Press, 2005), 237-252.
- Sullivan W.C., Kuo F.E., DePooter S.F. The fruit of urban nature – Vital neighborhood spaces. Environment and Behavior. 2004;36(5):678–700. [Google Scholar]
- Thakar V. Unfolding events in space and time: Geospatial insights into COVID-19 diffusion in Washington State during the initial stage of the outbreak. ISPRS International Journal of Geo-Information. 2020;9(6):382. [Google Scholar]
- Tirachini A., Cats O. COVID-19 and public transportation: Current assessment, prospects, and research needs. Journal of Public Transportation. 2020;22(1):1–21. doi: 10.5038/2375-0901.22.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokey A.I. Spatial association of mobility and COVID-19 infection rate in the USA: A county-level study using mobile phone location data. Journal of Transport & Health. 2021;22 doi: 10.1016/j.jth.2021.101135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trochta J., Krůček M., Vrška T., Král K. 3D Forest: An application for descriptions of three-dimensional forest structures using terrestrial LiDAR. PLoS ONE. 2017;12(5):e0176871–e. doi: 10.1371/journal.pone.0176871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrvainen L., Ojala A., Korpela K., Lanki T., Tsunetsugu Y., Kagawa T. The influence of urban green environments on stress relief measures: A field experiment. Journal of Environmental Psychology. 2014;38:1–9. [Google Scholar]
- Ugolini F., Massetti L., Calaza-Martínez P., Cariñanos P., Dobbs C., Ostoić S.K.…Sanesi G. Effects of the COVID-19 pandemic on the use and perceptions of urban green space: An international exploratory study. Urban Forestry & Urban Greening. 2020;56 doi: 10.1016/j.ufug.2020.126888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulrich R.S. A theory of supportive design for healthcare facilities. J Healthc Des. 1997;9:3–7. discussion 21–24. [PubMed] [Google Scholar]
- Ulrich R.S., Simons R.F., Losito B.D., Fiorito E., Miles M.A., Zelson M. Stress recovery during exposure to natural and urban environments. Journal of Environmental Psychology. 1991;11(3):201–230. [Google Scholar]
- USAFACTS. (2021). USAFACTS. Retrieved July 20 2021 from https://usafacts.org/about-usafacts/.
- Venter Z.S., Barton D.N., Gundersen V., Figari H., Nowell M.S. Back to nature: Norwegians sustain increased recreational use of urban green space months after the COVID-19 outbreak. Landscape and Urban Planning. 2021;214 [Google Scholar]
- Venter Z., Barton D., Gundersen V., Figari H., Nowell M. Urban nature in a time of crisis: Recreational use of green space increases during the COVID-19 outbreak in Oslo, Norway. Environmental Research Letters. 2020 [Google Scholar]
- Volenec Z.M., Abraham J.O., Becker A.D., Dobson A.P. Public parks and the pandemic: How park usage has been affected by COVID-19 policies. PLoS ONE. 2021;16(5):e0251799. doi: 10.1371/journal.pone.0251799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Wu X., Wang R., He D., Li D., Yang L.…Lu Y. Review of associations between built environment characteristics and severe acute respiratory syndrome coronavirus 2 infection risk. International Journal of Environmental Research and Public Health. 2021;18(14):7561. doi: 10.3390/ijerph18147561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: Analysis from electronic health records in the United States. World Psychiatry. 2021;20(1):124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen, M., Zhang, X., Harris, C. D., Holt, J. B., & Croft, J. B. (2013). Spatial disparities in the distribution of parks and green spaces in the USA. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine, 45 Suppl 1(Suppl 1), S18-S27. [DOI] [PMC free article] [PubMed]
- Wong D.W.S., Li Y. Spreading of COVID-19: Density matters. PLoS ONE. 2020;15(12):e0242398. doi: 10.1371/journal.pone.0242398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E., Harsant A., Dallimer M., Cronin de Chavez A., McEachan R.R.C., Hassall C. Not all green space is created equal: biodiversity predicts psychological restorative benefits from urban green space. Frontiers in Psychology. 2018;9(2320) doi: 10.3389/fpsyg.2018.02320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2021). Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update. Retrieved July 20 2021 from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.
- Wu S.L., Mertens A.N., Crider Y.S., Nguyen A., Pokpongkiat N.N., Djajadi S.…Reingold A. Substantial underestimation of SARS-CoV-2 infection in the United States. Nature Communications. 2020;11(1):1–10. doi: 10.1038/s41467-020-18272-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Liu S., Liu J., Zhang Z., Wan X., Huang B.…Zhang Y. COVID-19: Immunopathogenesis and Immunotherapeutics. Signal Transduction and Targeted Therapy. 2020;5(1):128. doi: 10.1038/s41392-020-00243-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Diez-Roux A.V. Walking distance by trip purpose and population subgroups. American Journal of Preventive Medicine. 2012;43(1):11–19. doi: 10.1016/j.amepre.2012.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Yu Z., Zhao B., Sun R., Vejre H. Links between green space and public health: A bibliometric review of global research trends and future prospects from 1901 to 2019. Environmental Research Letters. 2020;15(6) [Google Scholar]
- Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proceedings of the National Academy of Sciences. 2020;117(26):14857. doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Science of the Total Environment. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziter C.D., Pedersen E.J., Kucharik C.J., Turner M.G. Scale-dependent interactions between tree canopy cover and impervious surfaces reduce daytime urban heat during summer. Proceedings of the National Academy of Sciences. 2019;116(15):7575–7580. doi: 10.1073/pnas.1817561116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Žlender V., Ward Thompson C. Accessibility and use of peri-urban green space for inner-city dwellers: A comparative study. Landscape and Urban Planning. 2017;165:193–205. [Google Scholar]
Further reading
- Angulo F.J., Finelli L., Swerdlow D.L. Estimation of US SARS-CoV-2 infections, symptomatic infections, hospitalizations, and deaths using seroprevalence surveys. JAMA Network Open. 2021;4(1):e2033706–e. doi: 10.1001/jamanetworkopen.2020.33706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berman M.G., Jonides J., Kaplan S. The cognitive benefits of interacting with nature. Psychological Science. 2008;19(12):1207–1212. doi: 10.1111/j.1467-9280.2008.02225.x. [DOI] [PubMed] [Google Scholar]
- Branas C.C., South E., Kondo M.C., Hohl B.C., Bourgois P., Wiebe D.J., MacDonald J.M. Citywide cluster randomized trial to restore blighted vacant land and its effects on violence, crime, and fear. Proceedings of the National Academy of Sciences. 2018;115:2946–2951. doi: 10.1073/pnas.1718503115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulston J.W., Jacobs D.M., King C.R., Elmore I.C. The influence of multi-season imagery on models of canopy cover. Photogrammetric Engineering & Remote Sensing. 2013;79(5):469–477. [Google Scholar]
- Coulston J.W., Moisen G.G., Wilson B.T., Finco M.V., Cohen W.B., Brewer C.K. Modeling percent tree canopy cover: A pilot study. Photogrammetric Engineering & Remote Sensing. 2012;78(7):715–727. [Google Scholar]
- Helbich M., O’Connor R.C., Nieuwenhuijsen M., Hagedoorn P. Greenery exposure and suicide mortality later in life: A longitudinal register-based case-control study. Environment International. 2020;143 doi: 10.1016/j.envint.2020.105982. [DOI] [PubMed] [Google Scholar]
- Holtan M.T., Dieterlen S.L., Sullivan W.C. Social life under cover: Tree canopy and scoia capital in Baltimore, Maryland. Environment & Behavior. 2014;46(6):1–24. [Google Scholar]
- Jiang B., Mak C.N.S., Larsen L., Zhong H. Minimizing the gender difference in perceived safety: Comparing the effects of urban back alley interventions. Journal of Environmental Psychology. 2017;51:117–131. [Google Scholar]
- Kaplan R., Kaplan S. Cambridge University Press; 1989. The experience of nature: A psychological perspective. [Google Scholar]
- Kaplan S. The restorative benefits of nature – toward an integrative framework. Journal of Environmental Psychology. 1995;15(3):169–182. [Google Scholar]
- Lovasi G.S., Quinn J.W., Neckerman K.M., Perzanowski M.S., Rundle A. Children living in areas with more street trees have lower prevalence of asthma. Journal of Epidemiology and Community Health. 2008;62(7):647–649. doi: 10.1136/jech.2007.071894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang B., Zhang T., Sullivan W.C. Healthy Cities: Mechanisms and Research Questions Regarding the Impacts of Urban Green Landscapes on Public Health and Well-being. Landscape Architeture Frontiers. 2015;3(1):24–35. [Google Scholar]
- Mazumdar S., Learnihan V., Cochrane T., Davey R. The built environment and social capital: A systematic review. Environment and Behavior. 2017;50(2):119–158. [Google Scholar]
- Min K.-B., Kim H.-J., Kim H.-J., Min J.-Y. Parks and green areas and the risk for depression and suicidal indicators. International Journal of Public Health. 2017;62(6):647–656. doi: 10.1007/s00038-017-0958-5. [DOI] [PubMed] [Google Scholar]
- O’Brien R.M. A caution regarding rules of thumb for variance inflation factors. Quality & Quantity. 2007;41(5):673–690. [Google Scholar]
- Ouyang W., Morakinyo T.E., Ren C., Ng E. The cooling efficiency of variable greenery coverage ratios in different urban densities: A study in a subtropical climate. Building and Environment. 2020;174 [Google Scholar]
- Power M.C., Kioumourtzoglou M.-A., Hart J.E., Okereke O.I., Laden F., Weisskopf M.G. The relation between past exposure to fine particulate air pollution and prevalent anxiety: Observational cohort study. BMJ. 2015;350 doi: 10.1136/bmj.h1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan, W. C., & Li, D. (2021). Nature and attention. In Nature and psychology: Biological, cognitive, developmental, and social pathways to well-being. Springer Nature.
- Yu C.-P., Lee H.-Y., Luo X.-Y. The effect of virtual reality forest and urban environments on physiological and psychological responses. Urban Forestry & Urban Greening. 2018;35:106–114. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.