Abstract
Objective
The aim of this work was to review the protocol of the use of silver diamine fluoride (SDF) for arresting caries, specifically the application time.
Method
Two researchers searched manufacturers’ instructions, YouTube videos, and 5 databases (Embase, Medline, PubMed, Scopus, and Web of Science). Manufacturers’ instructions, videos from national dental organisations, and peer-reviewed journal articles that published the SDF application protocol in English for arresting caries were selected.
Results
The review included 14 protocols from 15 publications from 4 manufacturers, 3 dental associations, and 7 author teams (one team had 2 articles). The American Dental Association and the British Society of Paediatric Dentistry provided their SDF application protocols on YouTube. The American Academy of Paediatric Dentistry and 7 author teams published their protocols in journal articles. Seven publications suggested an SDF application time of 60 seconds. Seven publications suggested a time range of 10 seconds to 240 seconds. Two publications suggested caries excavation, but 4 publications suggested no caries excavation before SDF application. The procedures from at least 5 publications involved protecting the gingiva with petroleum jelly, isolating the carious tooth with cotton rolls, drying the carious lesion with a 3-in-1 syringe, applying SDF solution with a micro brush for 60 seconds, removing excess SDF solution with gauze, and applying fluoride varnish to the SDF-treated lesion.
Conclusions
Although the SDF application protocol is simple and straightforward, the published protocols could be different. Most publications suggested an SDF application time of 60 seconds, which can be long, particularly for young children and older adults.
Key words: Silver diamine fluoride, Fluoride, Dentine, Caries, Arrest, Remineralisation
Introduction
The Global Burden of Disease study reported that untreated dental caries affects 573 million children1 and 2.4 billion adults.2 Treating dental caries with a dental restoration is a common job for a dentist. A survey in the United States found that a general dentist spends more than half (56%) of their clinical time providing dental restorations to their patients.3 Conventional restorative treatment requires well-trained dental personnel, sophisticated dental equipment, and a long operation time. This prevailing restorative treatment for dental caries is often neither available nor affordable in many areas of the world. Nonrestorative caries treatment can be an alternative strategy for controlling dental decay, particularly for those who cannot tolerate more involved dental treatments. Nonrestorative caries treatment enables sustainable caries control through controlling a bacterial infection and the remineralisation of teeth. Many academics and clinicians advocate that the contemporary philosophy of caries management has shifted from a surgical approach to a medical approach.4
Silver diamine fluoride (SDF) therapy is an archetypal example of nonrestorative caries treatment. SDF is a colourless solution with antimicrobial and remineralising properties. SDF is commonly available as a 38% solution containing 253,900 ppm silver and 44,800 ppm fluoride ions.5 Silver is antimicrobial and inhibits the growth of cariogenic biofilm.6 Fluoride promotes remineralisation and inhibits the demineralisation of teeth under an acid challenge.6 SDF also prevents the degradation of dentine collagen through the inhibition of proteolytic peptidases in dentine and saliva. Systematic reviews have concluded that SDF is an effective cariostatic agent for arresting caries.7,8 SDF therapy is simple, noninvasive, painless, inexpensive, and non–aerosol-generating. It can be used in people who are not a good fit for conventional restorative treatment. It can also be used to treat young children who are too young to receive conventional restorative treatment in a dental chair.9 It can furthermore be used to treat older adults who have limited access to dental clinics, as well as people with special needs who are unable to cooperate with dental treatment.
Rosenblatt et al (2009) called SDF a silver-fluoride bullet for caries management because SDF is a safe, effective, efficient, and equitable caries control agent.10 SDF therapy may meet the World Health Organization Millennium Goals and fulfil the United States Institute of Medicine's criteria for 21st-century medical care. In 2020, the British Society of Paediatric Dentistry published its support of the use of SDF to treat caries. In 2021, the World Health Organization included SDF as an essential health system medicine that meets the most important needs of adults and children. A recent bibliometric analysis found that the global interest regarding SDF exponentially increased in the 5-year period from 2016 to 2021.11 SDF has also attracted clinicians’ and researchers’ attention to its use to improve the quality of dental care.
The United States Food and Drug Administration has cleared SDF as a Class II medical device for professional use to manage dentine hypersensitivity.9 In 2017, Health Canada approved SDF for dental care. Several manufacturers developed an SDF solution with a concentration at 3.8% to 38% for dental use.12,13 Because SDF is cleared as an antihypersensitivity agent in the United States, manufacturers may target the specifications and clinical protocol of SDF use for the treatment of tooth hypersensitivity. However, based on their clinical experience, dentists often use SDF to arrest caries with different SDF application times.9 This study's objective is to review the SDF application time that provides the best practice of SDF therapy for arresting caries.
Materials and methods
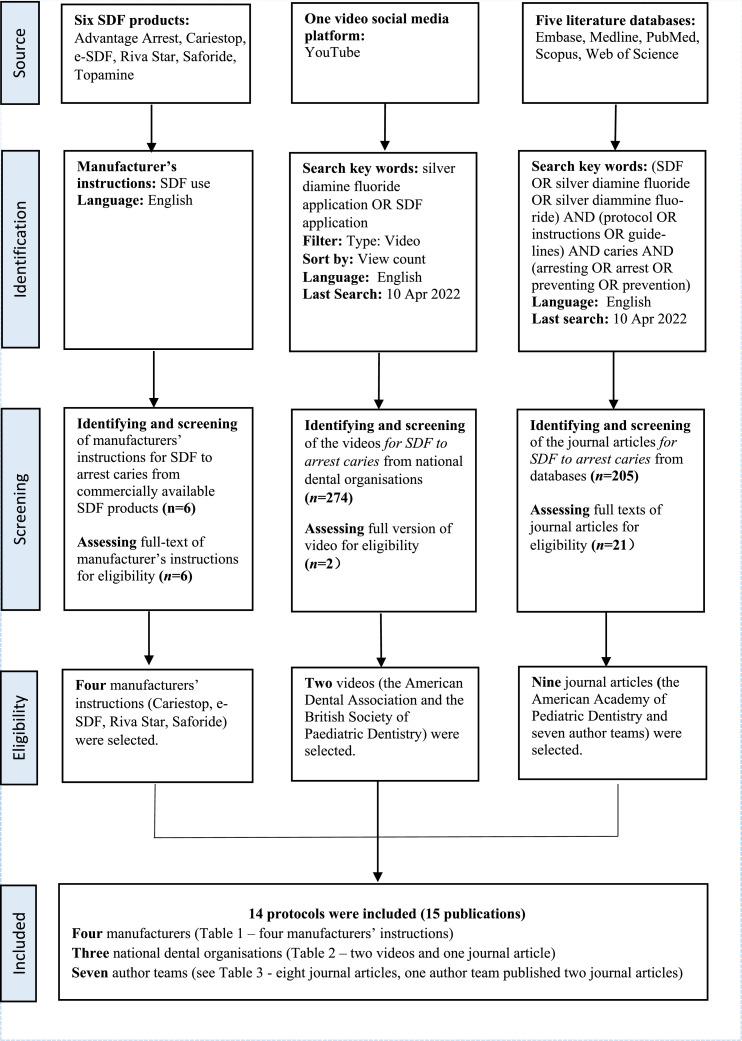
Two researchers independently reviewed the manufacturers’ instructions of the SDF products. They included publications offering protocols in English on topical SDF application for caries arrest. They also performed YouTube searches to identify videos in English from respected dental organisations, such as national dental associations. In addition, they searched through English peer-reviewed journal articles using 5 databases (Figure 1).
Fig.
Flowchart of the search strategy.
Review of the manufacturers’ instructions
The 2 researchers purchased SDF products available in Hong Kong. In addition, they sent emails to the manufacturers of the SDF products that were not available in Hong Kong asking for their SDF product or manufacturer instructions. The 2 researchers independently studied the manufacturers’ instructions of the SDF products that were purchased or received to identify their SDF application protocols for caries arrest.
YouTube search
The 2 researchers performed searches on common video search engine YouTube to identify a video (filter type: video) in English (language: English) on SDF application protocols from national dental organisations and institutions (sort by: view count). The keywords used for the search were “silver diamine fluoride application” OR “SDF application.”
Literature search
The 2 researchers independently performed a literature search to identify publications using 5 commonly used databases: Embase, Medline, PubMed, Scopus, and Web of Science. The search was restricted to publications in English. They searched through publications using the keywords (SDF OR silver diamine fluoride OR silver diammine fluoride) AND (protocol OR instructions OR guidelines) AND caries AND (arresting OR arrest OR preventing OR prevention). Journal articles published before 10 April 2022, including those which were electronically published ahead of print, were included. After excluding the duplicated publications, the researchers screened the publications’ titles and abstracts to retrieve full texts of the potentially eligible peer-reviewed publications offering guidelines on the clinical protocol of SDF for caries management. They also manually screened the references of the selected publications to identify relevant publications for inclusion.
Data analysis
The researchers reviewed the SDF application protocols for caries arrest and prevention in the selected publications, which included videos, documents that national dental associations disseminated, or peer-reviewed journal articles. They summarised the application protocol into a set of instructions and procedures that a clinician should follow, and they described each stage of the process. They also examined the evidence and justification for the recommended SDF application times on the carious lesion by studying the references that the selected publications provided. The set of instructions and procedures were tabulated according to the instructions and suggestions of the manufacturers, the national dental associations, and the author teams published in the peer-reviewed journal articles. Then, a summary of the sets of instructions on SDF therapy for arresting caries was developed.
Results
The 2 reviewers completed the search, and the last search was performed on 10 April 2022. They independently reviewed 6 manufacturers’ instructions for SDF use to arrest caries, 274 YouTube videos, and 205 journal articles. The 2 reviewers included 4 manufacturers’ instructions for the use of SDF to arrest caries, 2 YouTube videos, and 9 journal articles (15 publications in total) in this review. One author team published 2 peer-reviewed journal articles presenting the SDF application protocols. A total of 15 publications from 4 manufacturers, 3 national dental associations, and 7 author teams were included in this review (Figure 1).
Review of the manufacturers’ instructions
The 2 researchers collected 6 manufacturers’ instructions for SDF solutions: Advantage Arrest (Elevate Oral Care), Cariestop (Biodinámica), e-SDF (Kids-e-Dental), Riva Star (SDI Limited), Saforide (Toyo Seiyaku Kasei), and Topamine (DentaLife). They assessed the full text of the manufacturers’ instructions for eligibility and selected 4 manufacturers’ instructions from Cariestop (M1), e-SDF (M2), Riva Star (M3), and Saforide (M4), which provide SDF application protocols for arresting dental caries (Table 1).
Table 1.
Recommendations by the manufacturers for silver diamine fluoride (SDF) use to arrest caries.
| No. | Product information | SDF application protocol |
|---|---|---|
| M1 | Product: Cariestop 30%, Item: 30% SDF solution Manufacturer: Biodinámica Country: Brazil |
Protect gingiva and mucosa with petroleum jelly or rubber dam Clean the carious lesion with water or prophylaxes with pumice powder Dry the carious lesion Apply SDF to the carious lesion Leave the SDF-treated lesion for 120 to 180 seconds Wash |
| M2 | Product: e-SDF Item: 38% SDF solution Manufacturer: Kids-e-Dental Country: India |
Protect gingiva and mucosa with petroleum jelly Isolate the carious tooth Dry the carious lesion Apply SDF to the carious lesion using micro brush Use super floss for proximal carious lesions Leave the SDF-treated lesion for 60 to 180 seconds |
| M3 | Product: Riva Star (38%) Items: (1) 38% SDF solution and (2) Potassium iodine solution Manufacturer: SDI Limited Country: Australia |
Protect gingiva and lips with petroleum jelly, gingival barrier, or cocoa butter Isolate carious teeth with cotton roll or rubber dam Clean carious lesion with prophy paste Apply SDF to the carious lesion using micro brush Apply potassium iodide using another micro brush Dry SDF-treated carious lesion |
| M4 | Product: Saforide (38%) Item: 38% SDF solution Manufacturer: Toyo Seiyaku Kasei Country: Japan |
Protect gingiva and lips with petroleum jelly or rubber dam Isolate the carious tooth with cotton rolls Clean the carious lesion Dry the carious lesion with 3-in-1 syringe and saliva ejector (Remove carious enamel using a spoon excavator for prevention and control of incipient caries in deciduous teeth) Apply SDF to the carious lesion using a cotton pellet Leave the SDF-treated lesion for 180 to 240 seconds Rinse with water or saline |
YouTube search
The 2 researchers used YouTube to search for videos from national dental organisations. They screened 274 videos to select SDF application protocols from national dental organisations and institutions. They identified 2 videos and assessed the full versions of the 2 videos for eligibility. After their assessment, they found and included these 2 videos from the American Dental Association (ADA) and the British Society of Paediatric Dentistry (BSPD) which provided details about SDF application protocols (Table 2).
Table 2.
Recommendations by national dental organisations for silver diamine fluoride (SDF) use to arrest caries.
| No. | Organisation, year; topic [web link] | SDF application protocol |
|---|---|---|
| P1 | American Dental Association, 2018; Silver Diamine Fluoride Application: Evidence-Based Recommendations [https://www.youtube.com/watch?v=a0HH7GifdM4] |
Isolate the carious tooth with cotton roll or gauze Clean the carious lesion with cotton pellet or micro brush Dry the carious lesion with gauze or cotton Apply SDF to the carious lesion using micro brush Leave the SDF-treated lesion for 60 seconds Remove excess SDF with gauze if necessary (SDF therapy is a noninvasive way in which to treat carious lesion without drill) |
| P2 | American Academy of Pediatric Dentistry, 2018; Chairside Guide: Silver Diamine Fluoride in the Management of Dental Caries Lesions [https://www.aapd.org/globalassets/media/policies_guidelines/r_chairsideguide.pdf] |
Protect gingiva and mucosa with a protective coating Protect skin with a temporary henna-appearing tattoo Clean the carious lesion Isolate the tooth with cotton roll or other methods (Removing carious dentine prior to SDF application is not necessary) Apply SDF to the carious lesion using micro brush Leave the SDF-treated lesion for 60 seconds Dry the SDF-treated lesion with 3-in-1 syringe Leave the SDF-treated lesion up to 180 seconds Remove excess SDF with gauze, cotton roll, or cotton pellet Cover the entire dentition with fluoride varnish |
| P3 | British Society of Paediatric Dentistry, 2020; How to Apply Silver Diamine Fluoride, [https://www.youtube.com/watch?v=tELmH9jRvv8&t=17s] | Protect any exposed gingival tissues and lips with petroleum jelly Isolate the carious tooth with cotton roll Clean the carious lesion with cotton roll Dry the carious lesion with cotton roll or 3-in-1 syringe Apply SDF to the carious lesion using micro brush Leave the SDF-treated lesion for 60 seconds (best for 180 seconds) Remove excess SDF with gauze or micro brush if necessary Cover the SDF-treated lesion with toothpaste or fluoride varnish |
Literature search
The initial literature search revealed 205 potentially eligible publications (44 articles in Embase, 37 articles in Medline, 69 articles in PubMed, 5 articles in Scopus, and 50 articles in Web of Science). A total of 117 duplicated records of publications were removed. Another 56 irrelevant publications, such as those for laboratory studies, were removed following the screening of the titles and abstracts. The 2 researchers retrieved the remaining 21 full-text articles plus 2 articles identified from the references of the 21 articles. They then discussed the selected publications with another investigator to achieve an agreement on the list of publications included in this study. They included a publication by the American Academy of Pediatric Dentistry (AAPD; Table 2) and 8 articles by 7 author teams (T1 to T7; Figure). One author team (T2), which Crystal led, published their SDF application protocol in 2 articles in the same dental journal. Thus, one national dental association (Table 2) and 7 author teams were included in this study (Table 3). The author teams were mainly from the United States (5/7, T1–T4, and T7).
Table 3.
Recommendations by author teams for silver diamine fluoride (SDF) use to arrest caries.
| No. | Authors, primary affiliation, reference | SDF application protocol |
|---|---|---|
| T1 | Burgette JM, Weintraub JA, Birken SA, Lewis TA, White BA University of Pittsburgh and University of North Carolina, USA Journal of Dentistry for Children 2019;86:32–9 |
Protect gingiva and mucosa with petroleum jelly Isolate the carious tooth with cotton roll, gauze, cotton pellet, or dry angle Clean the carious lesion with power washing, gauze, micro brush, cotton roll, or pellet Dry the carious lesion with 3-in-1 syringe gauze, micro brush, cotton roll, or pellet Apply SDF to the carious lesion using micro brush Leave the SDF-treated lesion for 60 to 180 seconds Dry the SDF-treated lesion with gauze, micro brush, cotton roll, or pellet Remove excess SDF with gauze, micro brush, cotton roll, or pellet Cover the entire dentition with fluoride varnish |
| T2 | Crystal YO, Niederman R New York University, USA Pediatric Dentistry 2016;38(7):466–71 Crystal YO, Marghalani AA, Sulyanto R, Divaris K, Ureles SD, Wright JT, Fontana M, Laurel Graham L New York University, USA Pediatric Dentistry 2017;39:E135–45 |
Protect gingival tissues with cocoa butter or cotton roll Clean the carious lesion (No operative intervention [eg, affected or infected dentin removal] is necessary to achieve caries arrest) Dry the carious lesion with 3-in-1 syringe Apply SDF to the carious lesion using micro sponge brush Leave the SDF-treated lesion for 10 to 180 seconds (Leave it for 60 seconds in their second article) Dry the SDF-treated lesion with 3-in-1 syringe Allow SDF to remain on lesion at least 60 seconds (Allow SDF to remain on lesion [best] for 180 seconds) Remove excess SDF with gauze, cotton roll, or pellet |
| T3 | Croll TP, Berg JH University off Washington, USA Inside Dental Hygiene Continuing Education Course 2018 https://idh.cdeworld.com/courses/5155 |
Dry the carious lesions with a cotton swab or 3-in-1 syringe Apply SDF to the carious lesion using micro brush Leave the SDF-treated lesion for 60 seconds Dry the SDF-treated lesion Remove excess SDF with cotton swab Cover the SDF-treated lesion with fluoride varnish |
| T4 | Horst JA, Ellenikiotis H, Milgrom PL University of California at San Francisco, USA Journal of California Dental Association 2016;44:16–28 |
Protect gingiva with petroleum jelly Isolate the carious tooth with cotton roll or gauze Dry the carious lesion with 3-in-1 syringe or cotton Apply SDF to the carious lesion using micro sponge Leave the SDF-treated lesion for up to 60 seconds Remove excess SDF with gauze or cotton roll Consider applying potassium iodide to minimise staining Rinse with water |
| T5 | Haq J, Khurshid Z, Santamaria RM, Abudrya M, Schmoeckel J, Zafar MS, Splieth CH University of Greifswald, Germany Fluoride 2021;54:210–8 |
Protect gingiva and mucosa with petroleum jelly Isolate the carious tooth with cotton roll or other methods Dry the carious lesion with 3-in-1 syringe Apply SDF to the carious lesion using micro brush or micro sponge brush Leave the SDF-treated lesion at least for 60 seconds Dry the SDF-treated lesion with 3-in-1 syringe for 180 seconds Remove excess SDF with gauze, cotton roll, or pellet Cover the entire dentition with fluoride varnish |
| T6 | Seifo N, Robertson M, MacLean J, Blain K, Grosse S, Milne R, Seeballuck C, Innes N University of Dundee, UK British Dental Journal 2020;228:75–81 |
Protect gingiva and lips with petroleum jelly or gingival barrier Isolate the carious tooth with cotton roll or rubber dam Clean the carious lesion Dry the carious lesion with 3-in-1 syringe or cotton roll Apply SDF to the carious lesion using micro brush Apply potassium iodide immediately if it is used Leave the SDF-treated lesion for 60 seconds Keep isolated and leave it for 180 seconds Remove excess SDF Cover the SDF-treated carious lesion with fluoride varnish |
| T7 | Young DA, Quock RL, Horst J, Kaur R, MacLean JK, Frachella JC, Duffin S, Semprum-Clavier A, Ferreira Zandona AG Tufts University, USA Compendium of Continuing Education in Dentistry 2021;42:e5–9 |
Protect soft tissue with petroleum jelly, lip balm, or toothpaste Isolate the carious tooth with cotton roll, gauze, saliva ejector, or suction Removing caries is not necessary prior to applying SDF Dry the carious lesions with high-speed vacuum, cotton, gauze or 3-in-1 syringe Apply SDF to the carious lesion using micro brush Leave the SDF-treated lesion for 60 seconds (do not rinse, light-cure, blow compressed air) Remove excess SDF with cotton Cover the SDF-treated lesion with fluoride varnish |
Recommended SDF application procedures
Table 4 summarises the recommendations for the use of SDF therapy to arrest caries from the 4 manufacturers (Table 1, M1 to M4), the 3 national dental associations (Table 2; ADA, AAPD, and BSPD) and the 7 author teams (Table 3, T1–T7).
Table 4.
Summary of the recommendations for silver diamine fluoride (SDF) therapy to arrest caries.
| Procedure (No. of protocols) | References (from Tables 1 to 3) |
|---|---|
| Protecting gingiva and lips | |
|
M1, M2, M3, M4, P3, T1, T4, T5, T6, T7 |
|
M1, M3, M4, T6 |
|
M3, P2 |
| Isolating carious tooth | |
|
M3, M4, P1, P2, P3, T1, T4, T5, T6, T7 |
|
M1, M3, M4, T6 |
|
P1, T1, T4, T7 |
| Cleaning of carious lesion | |
|
M1, M3, M4, P1, P2, P3, T1, T2, T6 |
| Removing of carious lesion | |
|
P1, P2, T2, T7 |
|
M4 |
| Drying the carious lesion | |
|
M4, P3, T1, T2, T3, T4, T5, T6, T7 |
|
P1, P3, T1, T3, T4, T6, T7 |
|
P1, T1, T7 |
| Applying SDF solution | |
|
M2, M3, P1, P2, P3, T1, T3, T5, T6, T7 |
|
T2, T4, T5 |
|
M4 |
| Application time for SDF | |
|
P1, P2, T2, T3, T4, T5, T6, T7 |
|
M2, P3, T1 |
|
T2 |
|
M1 |
|
M4 |
| Isolation time for SDF | |
|
P2, T5, T6 |
|
T2 |
| Removing excess SDF | |
|
P1, P2, P3, T1, T2, T4, T5 |
|
P2, T1, T2, T4, T5, T7 |
|
P3, T1 |
| Minimising SDF staining | |
|
M3, T4, T6 |
| Applying sodium fluoride varnish | |
|
P2, P3, T1, T3, T5, T6, T7 |
|
P2, T1, T5 |
Four manufacturers (M1–M4), the BSPD, and 5 author teams (T1, T4–T7) recommended applying petroleum jelly to protect soft tissue prior to SDF application. Others suggested protective barriers, including a rubber dam (M1–M3, T6), a gingival barrier (M3, T6), cocoa butter (M3, T2), lip balm (T7) and toothpaste (T7). Two manufacturers (M3, M4), the ADA, the AAPD, the BSPD, and 5 author teams (T1, T4–T7) recommended isolating the tooth with cotton rolls. Other isolation methods included gauze (P1, T1, T4, T7), a rubber dam (M1, M3, M4, T6), absorbent triangles (T1, T7), cotton pellets (T1), and a dental isolation device such as Isodry or Isolite(Zyris company) (T1).
Three manufacturers (M1, M3, M4), the ADA, the AAPD, the BSPD, and 3 author teams (T1, T2, T6) recommended cleaning carious lesions prior to SDF application. The ADA, the AAPD, and 2 author teams (T2, T7) mentioned that caries removal was not necessary for SDF therapy, whereas 1 manufacturer and 1 author team suggested caries removal.
One manufacturer (M4), the BSPD, and 7 author teams (T1–T7) recommended drying the carious lesion with a 3-in-1 syringe prior to SDF application. Others suggested drying the carious lesion with cotton rolls, pellets, or swabs (P1, P3, T1, T3, T4, T6, T7), gauze (P1, T1, T7), a micro brush (T1), and high-volume suction (T7). Two manufacturers (M2, M3), the ADA, the AAPD, the BSPD, and 5 author teams (T1, T3, T5, T6, T7) recommended applying an SDF solution to a carious lesion with a micro brush. Others suggested application tools such as a micro sponge (T2, T4, T5) and cotton pellets (M4).
The ADA, the AAPD, and 6 author teams (T2–T7) recommended applying SDF to a carious lesion for 60 seconds. Others recommended a range of application times. One manufacturer (M2), the BSPD, and 1 author team (T1) suggested application times of 60 seconds to 180 seconds. Others suggested application times of 10 seconds to 180 seconds (T2), 120 seconds to 180 seconds (M1) and 180 seconds to 240 seconds (M4).
Four publications (P2, T2, T5, T6) suggested allowing SDF to stay on the carious lesion following SDF application. The AAPD and 2 author team (T5, T6) recommended allowing the SDF to remain on the lesion for 180 seconds (isolation time) following SDF application. One author team (T2) suggested a range of 60 seconds to 180 seconds for the isolation time.
The ADA, the AAPD, the BSPD, and 4 author teams (T1, T2, T4, T5) recommended removing excess SDF solution with gauze. The AAPD and 5 author teams (T1, T2, T4, T5, T7) suggested using cotton rolls, pellets, or swabs. The BSPD and 1 author team (T1) suggested using a micro brush to remove excess SDF solution.
One manufacturer (M3) and 2 author teams (T4, T6) recommended applying potassium iodide solution following SDF application to minimise staining on the carious lesion. The AAPD, the BSPD, and 5 author teams (T1, T3, T5, T6, T7) suggested using sodium fluoride varnish following SDF application. The BSPD and 3 author teams (T3, T6, T7) suggested applying sodium fluoride varnish to the SDF-treated lesion, whereas the AAPD and 2 author teams (T1, T5) recommended applying fluoride varnish to the entire dentition.
Summary and instruction for SDF application protocol
Table 4 summarises the commonly recommended set of instructions and procedures according to the 4 manufacturers, the 3 national dental associations, and the 7 author teams.
Table 5 shows a set of commonly recommended instructions suggested in at least 5 of the 14 protocols. It shows step-by-step procedures of SDF therapy for caries arrest.
Table 5.
Clinical procedures for silver diamine fluoride (SDF) therapy to arrest caries.
| 1. Protecting gingiva and lips with petroleum jelly |
| 2. Isolating carious tooth with cotton roll |
| 3. Cleaning carious lesion |
| 4. Drying the carious lesion with 3-in-1 syringe or cotton roll, pellet, or swabs |
| 5. Applying SDF solution with micro brush |
| 6. Applying SDF solution on carious lesion for 60 seconds |
| 7. Removing excess SDF with gauze or cotton roll, pellet, or swabs |
| 8. Applying sodium fluoride varnish to the SDF-treated carious lesion |
At least a total of 5 manufacturers, national dental associations, and author teams in peer-reviewed journals recommended these procedures.
Discussion
In this study, we searched through not only manufacturers’ instructions but also videos and peer-reviewed journal articles on the SDF application protocol for arresting caries. This allowed for an exhaustive review of the publications. However, we could not access all commercial SDF products in the world. In addition, some SDF products are manufactured for local use in non-English-speaking countries and hence the manufacturer's instructions in English were not available. Because the United States Food and Drug Administration has cleared SDF as an antihypersensitivity agent,6 we found that 2 manufacturers did not provide instructions on the use of SDF to arrest caries.
We searched for videos on the SDF application protocol. YouTube operates as one of Google's subsidiaries and is the second-largest search engine after Google.14 YouTube is the most popular video platform, and dental professionals often use it to share their best practices in clinical care. A search of YouTube can identify SDF application protocols in English. People can upload as many videos as they wish to YouTube free of charge. The videos on SDF therapy are generally not peer-reviewed. Hence, this study included only videos which national professional organisations developed and not ones from individuals or private dental groups.
We also performed a literature search to identify peer-reviewed journal articles from the literature. To identify as many peer-reviewed journal articles in English as possible, 5 common databases were employed. We used Web of Science because it is one of the databases dominating the field of academic references. We also used PubMed because it offers an optimal update frequency and includes online early articles on medicine and biomedical sciences.15 We also searched Scopus, which covers a wide journal range, not just medicine and the biomedical sciences. Because SDF has been used in countries such as Argentina, Brazil, China, and Japan for many years,16 publications should be availble in other languages. Although we used 5 databases, we did not search through non-English-language publications, and this is a limitation of this study.
SDF has been used in dentistry for more than 50 years. SDF therapy does not require sophisticated equipment and can be used in the outreach setting.16 However, some protocols suggested using dental equipment, such as a 3-in-1 syringe and high-volume suction, which are not available in the field setting. We could not identify a protocol for SDF use in the field setting, although SDF is often recommended for use in the outreach setting. Although SDF use is simple and straightforward, we found that the published SDF application protocols were not the same. Some protocols suggested the use of protective barriers, such as petroleum jelly, to prevent soft tissue irritation and/or staining. However, Young et al17 opined that the protection of intraoral soft tissues is not necessary. On the contrary, the protective barrier could inadvertently get on the lesion or surface and inhibit SDF uptake. Fung et al found that gingival irritation was uncommon, and no staining of oral mucosa was reported after SDF application.13
Three manufacturers and an author team recommended the use of a rubber dam for teeth isolation and soft tissue protection for SDF therapy. A rubber dam is considered to be an ideal device for tooth isolation. It is essential for dental procedures that require good moisture control and high visibility. It provides a significantly higher success rate during restorative procedures and root canal treatment.18 A study showed that the average time spent placing a rubber dam was 8 minutes for children and 5 minutes for adults.19 Hence, its use for isolating teeth for a simple and moisture-tolerant procedure, such as SDF therapy, is not justified. Although a rubber dam protects the gingiva from irritation by SDF, the literature reveals that such a side effect is uncommon and self-limiting.16 Furthermore, dentists often choose SDF to arrest caries in young children and older adults who cannot cope with the conventional restorative care. The use of a rubber dam is difficult for many of these people. In addition, it limits the merits of SDF in outreach care. SDF therapy generally takes 1 to 3 minutes. The use of a rubber dam will increase the total treatment time to more than 10 minutes. It can cause discomfort and provoke anxiety in apprehensive people. In our YouTube search, we found many live videos of SDF therapy. No video showed rubber dam use, although 3 manufacturers recommend it.
One manufacturer mentioned caries removal before application. Wong et al reported that caries removal before SDF application shortened the time for caries arrest.20 Furthermore, caries excavation reduces the body of a carious lesion and hence may improve the poor aesthetics of the arrested caries.21 However, the ADA mentioned that SDF therapy is a noninvasive way in which to arrest caries without drill and fill. Caries removal requires the use of a hand instrument, such as an excavator. Caries excavation not only takes time but also can cause patient discomfort. A clinical trial showed that caries removal did not affect the caries-arresting effect of SDF.22 In this review, 4 publications suggested that caries removal is not necessary prior to SDF application. This simplifies and shortens the treatment time for SDF therapy. Moreover, it allows for SDF use in the outreach setting with inexpensive, simple, and disposable dental tools.
The ADA, the AAPD, and 6 author teams recommended an application time of 60 seconds for SDF application. Other publications suggested a wide range of application times from 10 seconds to 240 seconds. They have used arbitrary application times with no consensus. In addition, some dentists suggested isolating SDF-treated lesions for 60 seconds to 180 seconds following SDF application.17,23 However, a laboratory study found no difference in enamel remineralisation between 60 seconds and 180 seconds of SDF application.24 In addition, no literature investigated whether the 60-second application is the optimum application time. A lack of cooperation often compromises treatment or renders SDF treatment impossible or ineffective.9 The 60-second application is too long to be applied with young children, older adults, and people with special needs. In these situations, the arrest statuses of the lesions should be reevaluated during recall visits, and the possibility of reapplication should be considered. The optimal SDF application time remains unknown and requires further validation.9 A trial protocol for studying the carious lesion activity response to topical SDF therapy with increasing treatment application times was recently published.9 The work investigated the rate of caries arrest on children's carious teeth with an application time of 3 seconds to 180 seconds. The clinical trial should inform an evidence-based SDF protocol for arresting caries.
Some dentists use gauze or cotton rolls to remove excess SDF to prevent staining and aftertaste.23,25 The AAPD and 2 author teams suggested drying an SDF-treated lesion with a gentle blow of compressed air using a 3-in-1 syringe. However, an author team suggested no blowing with compressed air or rinsing while the SDF is being absorbed.17 Another author team did not recommend removing excess SDF with air or water spray because it can splash the SDF and stain the lips and face.25 In addition, compressed air may cause momentary and transient pain in the applied tooth.
One manufacturer and 2 author teams suggested applying potassium iodide solution to remove the dark staining that occurs following SDF application. A clinical trial found that the application of potassium iodide was associated with better aesthetic outcomes but poorer caries control compared with SDF application only.26 A laboratory study showed that potassium iodide application could reduce the intensity of staining in a dose-dependent manner.27 However, no significant difference was found 14 days after SDF application. A 30-month clinical trial found that potassium iodide application did not reduce the staining of SDF-treated lesions in the long term.28 A review concluded that insufficient evidence exists to support a demonstrable benefit of potassium iodide application to reduce tooth staining.29 Furthermore, the application of potassium iodine takes a further 60 seconds or until the precipitation of insoluble white silver iodide.30 It prolongs the treatment time of SDF therapy and may reduce patient cooperation.
Half of the publications in this review mentioned applying sodium fluoride varnish onto the SDF-treated lesion. Some researchers speculated that applying fluoride varnish after SDF application prevents saliva from diluting the applied SDF. However, a laboratory study found that the adjunctive application of SDF solution and sodium fluoride varnish had a similar remineralising effect to that of SDF solution alone on enamel caries.31 Another laboratory study found that a sodium fluoride varnish could reduce the antibacterial effects of SDF and might affect the arrest of dentine caries.32
Two manufacturers and 1 author team suggested rinsing the carious lesion following SDF applications with water or saline.33 Another author team mentioned that rinsing may not be necessary following SDF application.34 One author team did not recommend rinsing while the SDF is being absorbed on the lesion.17 Some dentists suggested refraining from eating or drinking for half an hour to 1 hour following SDF application.9,35 In general, manufacturers suggest washing or rinsing with water, saline solution, or hydrogen peroxide solution (Japanese pharmacopoeial term: Oxydol) immediately for the inadvertent accidental contact of SDF with the pulp, gingiva, oral mucosa, and skin. Direct application of SDF on a vital pulp is not recommended because it causes pulp necrosis.36 According to our own experience, we do not consider rinsing or washing to be necessary when SDF contacts gingivae or oral mucosa. SDF may cause gingival irritation, but the irritation is transient and will resolve without treatment. More clinical studies are needed to establish best practices.
Conclusions
Although SDF therapy is simple and straightforward, the recommended application protocols were principally based on experts’ opinions and could be different. The suggested application time for SDF is 10 seconds to 240 seconds, and many publications suggested 60 seconds, which is too long for young children, older adults, and people with special needs.
Author contributions
Chu C.H. conceived the idea. Yan I.G. collected the data. Yan I.G. and Gao S.S. analysed the data. Yan I.G. and Zheng F.M. took digital photos and prepared the figures. Yan I.G., Chu C.H., Duangthip D., and Lo E.C. prepared and revised the manuscript.
Conflict of Interest
None disclosed.
Acknowledgments
This study was supported by the General Research Fund (#17100421) of the Research Grant Council of Hong Kong.
REFERENCES
- 1.Kassebaum NJ, Smith AGC, Bernabé E, et al. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. 2017;96:380–387. doi: 10.1177/0022034517693566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kassebaum NJ, Bernabé E, Dahiya M, et al. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94:650–658. doi: 10.1177/0022034515573272. [DOI] [PubMed] [Google Scholar]
- 3.Gordan VV, Riley JL, 3rd, Geraldeli S, et al. Dental Practice-Based Research Network Collaborative Group. Repair or replacement of defective restorations by dentists in The Dental Practice-Based Research Network. J Am Dent Assoc. 2012;143:593–601. doi: 10.14219/jada.archive.2012.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yon MJY, Gao SS, Chen KJ, et al. Medical model in caries management. Dent J (Basel) 2019;7:37. doi: 10.3390/dj7020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yan IG, Zheng FM, Gao SS, et al. Ion concentration of silver diamine fluoride solutions. Int Dent J. 2022 doi: 10.1016/j.identj.2022.04.005. accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan IG, Zheng FM, Gao SS, et al. Fluoride delivered via a topical application of 38% SDF and 5% NaF. Int Dent J. 2022 doi: 10.1016/j.identj.2022.03.004. accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gao SS, Zhang S, Mei ML, et al. Caries remineralisation and arresting effect in children by professionally applied fluoride treatment - a systematic review. BMC Oral Health. 2016;16:12. doi: 10.1186/s12903-016-0171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao SS, Zhao IS, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Trans Res. 2016;1:201–210. doi: 10.1177/2380084416661474. [DOI] [PubMed] [Google Scholar]
- 9.Yan IG, Zheng FM, Gao SS, et al. Effect of application time of 38% silver diamine fluoride solution on arresting early childhood caries in preschool children: a randomised double-blinded controlled trial protocol. Trials. 2022;23:215. doi: 10.1186/s13063-022-06130-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenblatt A, Stamford TC, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet”. J Dent Res. 2009;88:116–125. doi: 10.1177/0022034508329406. [DOI] [PubMed] [Google Scholar]
- 11.Jiang CM, Duangthip D, Chan AKY, et al. Global research interest regarding silver diamine fluoride in dentistry: a bibliometric analysis. J Dent. 2021;113 doi: 10.1016/j.jdent.2021.103778. [DOI] [PubMed] [Google Scholar]
- 12.Zheng FM, Yan IG, Duangthip D, et al. Prevalence of untreated early childhood caries of 5-year-old children in Hong Kong: a cross-sectional study. Int J Environ Res Public Health. 2021;18:11934. doi: 10.3390/ijerph182211934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fung MHT, Duangthip D, Wong MCM, et al. Randomized clinical trial of 12% and 38% silver diamine fluoride treatment. J Dent Res. 2018;97:171–178. doi: 10.1177/0022034517728496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hernandez R. 11 Data-backed YouTube trends to help you grow your channel in 2022. Thehoth. Available from: https://www.thehoth.com/blog/youtube-trends/. Accessed 22 April 2022.
- 15.Falagas ME, Pitsouni EI, Malietzis GA, et al. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: strengths and weaknesses. FASEB J. 2008;22:338–342. doi: 10.1096/fj.07-9492LSF. [DOI] [PubMed] [Google Scholar]
- 16.Chu CH, Lo EC. Promoting caries arrest in children with silver diamine fluoride: a review. Oral Health Prev Dent. 2008;6:315–321. [PubMed] [Google Scholar]
- 17.Young DA, Quock RL, Horst J, et al. Clinical instructions for using silver diamine fluoride (SDF) in dental caries management. Compend Contin Educ Dent. 2021;42:e5–e9. [PubMed] [Google Scholar]
- 18.Goldfein J, Speirs C, Finkelman M, et al. Rubber dam use during post placement influences the success of root canal-treated teeth. J Endod. 2013;39:1481–1484. doi: 10.1016/j.joen.2013.07.036. [DOI] [PubMed] [Google Scholar]
- 19.Ryan W, O'Connel A. The attitudes of undergraduate dental students to the use of the rubber dam. J Ir Dent Assoc. 2007;53:87–91. [PubMed] [Google Scholar]
- 20.Wong MC, Lam KF, Lo EC. Bayesian analysis of clustered interval-censored data. J Dent Res. 2005;84:817–821. doi: 10.1177/154405910508400907. [DOI] [PubMed] [Google Scholar]
- 21.Chairside guide: silver diamine fluoride in the management of dental caries lesions. Pediatr Dent. 2018;40:492–517. [PubMed] [Google Scholar]
- 22.Chu CH, Lo EC, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81:767–770. doi: 10.1177/0810767. [DOI] [PubMed] [Google Scholar]
- 23.Seifo N, Robertson M, MacLean J, et al. The use of silver diamine fluoride (SDF) in dental practice. Br Dent J. 2020;228:75–81. doi: 10.1038/s41415-020-1203-9. [DOI] [PubMed] [Google Scholar]
- 24.Punhagui MF, Jussiani EI, Andrello AC, et al. Effect of application time and concentration of silver diamine fluoride on the enamel remineralization. J Clin Exp Dent. 2021;13:e653–e658. doi: 10.4317/jced.58318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burgette JM, Weintraub JA, Birken SA, et al. Development of a silver diamine fluoride protocol in safety net dental settings. J Dent Child (Chic) 2019;86:32–39. [PubMed] [Google Scholar]
- 26.Turton B, Horn R, Durward C. Caries arrest and lesion appearance using two different silver fluoride therapies on primary teeth with and without potassium iodide: 12-month results. Clin Exp Dent Res. 2021;7:609–619. doi: 10.1002/cre2.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Detsomboonrat P, Thongmak P, Lertpayab P, et al. Optimal concentration of potassium iodide to reduce the black staining of silver diamine fluoride. J Dent Sci. 2022;17:300–307. doi: 10.1016/j.jds.2021.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li R, Lo EC, Liu BY, et al. Randomized clinical trial on arresting dental root caries through silver diammine fluoride applications in community-dwelling elders. J Dent. 2016;51:15–20. doi: 10.1016/j.jdent.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 29.Roberts A, Bradley J, Merkley S, et al. Does potassium iodide application following silver diamine fluoride reduce staining of tooth? A systematic review. Aust Dent J. 2020;65:109–117. doi: 10.1111/adj.12743. [DOI] [PubMed] [Google Scholar]
- 30.Yawary R, Hegde S. Silver diamine fluoride protocol for reducing preventable dental hospitalisations in Victorian children. Int Dent J. 2021 doi: 10.1016/j.identj.2021.05.009. S0020-6539(21)00105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yu OY, Mei ML, Zhao IS, et al. Remineralisation of enamel with silver diamine fluoride and sodium fluoride. Dent Mater. 2018;34:e344–e352. doi: 10.1016/j.dental.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 32.Yu OY, Zhao IS, Mei ML, et al. Caries-arresting effects of silver diamine fluoride and sodium fluoride on dentine caries lesions. J Dent. 2018;78:65–71. doi: 10.1016/j.jdent.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 33.Horst JA, Ellenikiotis H, Milgrom PL. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications and consent. J Calif Dent Assoc. 2016;44:16–28. [PMC free article] [PubMed] [Google Scholar]
- 34.Crystal YO, Marghalani AA, Ureles SD, et al. Use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatr Dent. 2017;39:135–145. [PubMed] [Google Scholar]
- 35.Gao SS, Chen KJ, Duangthip D, et al. Preventing early childhood caries with silver diamine fluoride: study protocol for a randomised clinical trial. Trials. 2020;4:140. doi: 10.1186/s13063-020-4088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zaeneldin A, Yu OY, Chu CH. Effect of silver diamine fluoride on vital dental pulp: a systematic review. J Dent. 2022;119 doi: 10.1016/j.jdent.2022.104066. [DOI] [PubMed] [Google Scholar]