Abstract
Study Design
Bibliometric analysis.
Objective
Anterior cervical discectomy and fusion (ACDF) is a typical surgical method in spine surgery and has progressed significantly in the last several decades. The purpose of this study is to determine how the 100 most-cited original articles on ACDF have been the most influential in this field by identifying and analyzing them.
Methods
The articles on ACDF were identified by searching the Thomson ISI Web of Science database on 30 May 2022. The 100 most-cited articles were selected according to specific criteria. The data extracted from the articles included title, publication date, total citations, journal name, first author, institutions, and keywords.
Results
The total number of citations was 13,181, with a mean number of 131.81 ± 100.18. The publication dates ranged from 1994 to 2018. Most of these articles originated in the United States (68%) and were published in the 2000s (32%) and 2010s (48%). Spine published most of the articles (30%), followed by the Journal of Neurosurgery-Spine (16%), Spine Journal (14%), and European Spine Journal (13%). The most prolific author was Dr. Todd J Albert (n = 7), with 1,312 citations. The Texas Back Institute was the most productive institution (n = 10). The keywords ACDF, cervical spine, cervical spine, and fusion showed the highest degree of centrality.
Conclusion
One hundred top-cited articles on ACDF were identified and analyzed in this study. We demonstrate that ACDF is a growing and popular area of research, with the focus of research varying through timeline trends. This will provide a comprehensive and detailed basis for spine surgeons to make clinical decisions and assimilate the research focus of cervical spine surgery.
Keywords: anterior cervical discectomy and fusion, ACDF, bibliometric analysis, most cited articles, top 100
Introduction
Degenerative Cervical Myelopathy (DCM) is the most common cervical spinal disease (1, 2). Its treatment has evolved from conservative treatment to cervical laminoplasty, posterior cervical laminotomy and fixation, and anterior cervical discectomy and fusion (ACDF), which was first reported by Cloward, Smith, and Ronbison in 1958, opening up a new frontier in cervical spine surgery (3, 4). In the subsequent 60 years, different shapes of the iliac crest bone graft were first used for interbody fusion, and as our understanding of the biomechanics of the cervical spine improved, more types of fusion devices were invited for ACDF (3–10). Since then, ACDF has been widely used in cervical spine surgeries worldwide. In the USA, the number of patients undergoing ACDF has increased from 31 per year in 2006, to 9,937 per year in 2016 (a 31,951.6% increase), and the average age of patients is on the rise (11). ACDF has been widely accepted and gained increasing attention in recent years, resulting in a plethora of research in the cervical spine field.
Reviewing past research is an important component in advancing each specific line of research. Bibliometrics is a cross-disciplinary science of quantitative analysis of all knowledge carried out through mathematical and statistical means (12, 13). Compared with traditional reviews and meta-analyses, in bibliometric analyses, quantitative analysis and statistics are used to estimate the structure and development of a specific scientific discipline (14).
In the past decades, many bibliometric analyses have been conducted to study the most cited articles and publications on ACDF or cervical spine surgery; however, the 100 most-cited articles on ACDF from 1950 to May 2022 remain to be elucidated (15, 16). In this study, we propose to use bibliometric methods to highlight the characteristics of the 100 most-cited articles on ACDF, especially in terms of research hotspots and focus. We hope that this study highlights the potential directions for future research on ACDF and cervical spine surgery.
Methods
Collection and allocation of data
We searched for all relevant articles on ACDF using the Web of Science database, including the Web of Science Core Collection, MEDLINE, KCI-Korean Journal Database, Russian Science Citation Index, BIOSIS Citation Index, and SciELO Citation Index. Two researchers independently identified articles for inclusion to enhance search sensitivity. The search terms were “anterior cervical discectomy and fusion” OR “ACDF” OR “anterior cervical and discectomy and fusion” OR “anterior cervical and discectomy and fusion” OR “anterior cervical decompression and fusion” OR “anterior cervical decompression and fusions” OR “anterior cervical disc fusion” OR “anterior cervical discectomy and interbody fusion” OR “anterior cervical discectomy fusion” OR “anterior cervical discectomy with fusion” OR “cervical discectomy with fusion”.
The search was performed on 30 May 2022. We obtained 2,900 articles in total, which contained all articles published from 1980 to the present. All results were sorted from highest to lowest number of citations. We exported articles with more than 50 citations to Endnote 20 (Thomson Corporation, USA) for further analysis. Two clinical doctors performed the review based on the inclusion criteria illustrated below, and the results were exported to an Excel spreadsheet. Each of the two reviewers identified the 100 most-cited articles by screening the full text. An experienced professor compared their results carefully screening for discrepancies, and the final results were generated after a group discussion for subsequent analysis.
Eligibility criteria
The inclusion criteria were: (1) basic science research, anatomic studies, animal research, and clinical research related to ACDF; (2) diagnosis, treatment, prognosis, or epidemiologic association with ACDF; and (3) original article, review, case report, editorial, clinical trial, and any other paper type closely connected with ACDF.
Data extraction
All the included articles were independently reviewed by the same two authors as above. The following information was recorded for all the articles: title, first author's name, journal name, year of publication, impact factor of the journal in 2021, total number of citations of the article, average citations per year, geographic origin, institutions, and author keywords.
Replicability and reproducibility
Replication means that people independent from the initial data extraction will simulate the search, while answering the same research question; whereas reproducibility means that the data analysis will be repeated by a person not involved in the first analysis to verify selection and quality of data. Both replicability and reproducibility were verified through the author not involved in the first search, and led to the same results, hence confirming the quality of the bibliometric analysis reported in this study.
Results
All the 100 most-cited articles are listed in Table 1 and arranged by citation rank. The total number of citations was 13,181 (mean ± SD, 131.81 ± 100.18). Of these, 7 articles were cited more than 300 times.
Table 1.
List of the 100 most-cited articles in anterior cervical decompression and fusion.
| Rank | Article | Country | Total citations | Citations in last 5 years |
|---|---|---|---|---|
| 1 | Silber J. S, Anderson D. G, Daffner S. D, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 2003; 28(2): 134–139. | United States | 660 | 137 |
| 2 | Fountas Kostas N, Kapsalaki Eftychia Z, Nikolakakos Leonidas G, et al. Anterior cervical Discectomy and fusion associated complications. Spine 2007; 32(21): 2310–2317. | United States | 604 | 234 |
| 3 | Mummaneni Praveen V, Burkus J, Kenneth, Haid Regis W, et al. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. Journal of Neurosurgery-Spine 2007; 6(3): 198–209. | United States | 437 | 98 |
| 4 | Murrey, Daniel, Janssen, Michael, Delamarter, Rick, et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational, device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine Journal 2009; 9(4): 275–286. | United States | 403 | 97 |
| 5 | Heller John G, Sasso, Rick C, Papadopoulos Stephen M, et al. Comparison of BRYAN Cervical Disc Arthroplasty With Anterior Cervical Decompression and Fusion Clinical and Radiographic Results of a Randomized, Controlled, Clinical Trial. Spine 2009; 34(2): 101–107. | United States | 381 | 104 |
| 6 | Kaiser M. G, Haid, R. W, Subach, B. R, et al. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 2002; 50(2): 229–236. | United States | 326 | 67 |
| 7 | Fraser. Jusun F, Haertl. Roger. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. Journal of Neurosurgery-Spine 2007; 6(4): 298–303. | United States | 312 | 104 |
| 8 | Matsunaga S, Kabayama S, Yamamoto T, et al. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine 1999; 24(7): 670–675. | Japan | 264 | 40 |
| 9 | Hacker RJ, Cauthen JC, Gilbert TJ, et al. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine 2000; 25(20): 2646–2654. | United States | 224 | 37 |
| 10 | Perri Brian, Cooper Martin, Lauryssen Carl, et al. Adverse swelling associated with use of rh-BMP-2 in anterior cervical discectomy and fusion: a case study. Spine Journal 2007; 7(2): 235–239. | United States | 193 | 30 |
| 11 | Parker Scott L, Godil Saniya S, Shah David N, et al. Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion Clinical article. Journal of Neurosurgery-Spine 2013; 18(2): 154–160. | United States | 191 | 109 |
| 12 | Gercek E, Arlet V, Delisle J, et al. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. European Spine Journal 2003; 12(5): 513–516. | Canada | 189 | 55 |
| 13 | Riley LH, Skolasky RL, Albert TJ, et al. Dysphagia after anterior cervical decompression and fusion - Prevalence and risk factors from a longitudinal cohort study. Spine 2005; 30(22): 2564–2569. | United States | 184 | 58 |
| 14 | Oglesby Matthew, Fineberg Steven J, Patel Alpesh A, et al. Epidemiological Trends in Cervical Spine Surgery for Degenerative Diseases Between 2002 and 2009. Spine 2013; 38(14): 1226–1232. | United States | 169 | 115 |
| 15 | Kim Seok Woo, Limson Marc Anthony, Kim, Soo-Bum, et al. Comparison of radiographic changes after ACDF versus Bryan disc arthroplasty in single and bi-level cases. European Spine Journal 2009; 18(2): 218–231. | South Korea | 173 | 37 |
| 16 | Samartzis D, Shen F H, Goldberg E J, et al. Is autograft the gold standard in achieving radiographic fusion in one-level anterior cervical discectomy and fusion with rigid anterior plate fixation? Spine 2005; 30(15): 1756–1761. | United States | 171 | 46 |
| 17 | Marawar Satyajit, Girardi Federico P, Sama Andrew A, et al. National Trends in Anterior Cervical Fusion Procedures. Spine 2010; 35(15): 1454–1459. | United States | 161 | 83 |
| 18 | Zigler Jack E, Delamarter Rick, Murrey Dan, et al. ProDisc-C and Anterior Cervical Discectomy and Fusion as Surgical Treatment for Single-Level Cervical Symptomatic Degenerative Disc Disease Five-Year Results of a Food and Drug Administration Study. Spine 2013; 38(3): 203–209. | United States | 161 | 69 |
| 19 | Buttermann, Glenn Robin. Prospective nonrandomized comparison of an allograft with bone morphogenic protein versus an iliac-crest autograft in anterior cervical discectomy and fusion. Spine Journal 2008; 8(3): 426–435. | United States | 157 | 32 |
| 20 | Boakye M, Mummaneni P V, Garrett M, et al. Anterior cervical discectomy and fusion involving a polyetheretherketone spacer and bone morphogenetic protein. Journal of Neurosurgery-Spine 2005; 2(5): 521–525. | United States | 155 | 22 |
| 21 | Chiles BW, Leonard MA, Choudhri HF, et al. Cervical spondylotic myelopathy: Patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurgery 1999; 44(4): 762–769. | United States | 151 | 43 |
| 22 | Matsumoto Morio, Okada Eijiro, Ichihara Daisuke, et al. Anterior Cervical Decompression and Fusion Accelerates Adjacent Segment Degeneration Comparison With Asymptomatic Volunteers in a Ten-Year Magnetic Resonance Imaging Follow-up Study. Spine 2010; 35(1): 36–43. | Japan | 149 | 52 |
| 23 | Vavruch L, Hedlund R, Javid D, et al. A prospective randomized comparison between the Cloward procedure and a carbon fiber cage in the cervical spine - A clinical and radiologic study. Spine 2002; 27(16): 1694–1701. | Sweden | 148 | 31 |
| 24 | Song Kyung-Jin, Taghavi Cyrus E, Lee Kwang-Bok, et al. The Efficacy of Plate Construct Augmentation Versus Cage Alone in Anterior Cervical Fusion. Spine 2009; 34(26): 2886–2892. | South Korea | 146 | 60 |
| 25 | Samartzis Dino, Shen Francis H, Matthews Don K, et al. Comparison of allograft to autograft in multilevel anterior cervical discectomy and fusion with rigid plate fixation. Spine Journal 2003; 3(6): 451–459. | United States | 141 | 42 |
| 26 | Sasso Rick C, Smucker Joseph D, Hacker Robert J, et al. Clinical outcomes of BRYAN cervical disc arthroplasty: A prospective, randomized, controlled, multicenter trial with 24-month follow-up. Journal of Spinal Disorders & Techniques 2007; 20(7): 481–491. | United States | 141 | 30 |
| 27 | Rihn Jeffrey A, Kane Justin, Albert Todd J, et al. What Is the Incidence and Severity of Dysphagia After Anterior Cervical Surgery? Clinical Orthopaedics and Related Research 2011; 469(3): 658–665. | United States | 135 | 65 |
| 28 | Davis Reginald J, Nunley Pierce Dalton, Kim Kee D, et al. Two-level total disc replacement with Mobi-C cervical artificial disc versus anterior discectomy and fusion: a prospective, randomized, controlled multicenter clinical trial with 4-year follow-up results. Journal of Neurosurgery-Spine 2015; 22(1): 15–25. | United States | 133 | 75 |
| 29 | Niu Chi-Chien, Liao Jen-Chung, Chen Wen-Jer. Outcomes of Interbody Fusion Cages Used in 1 and 2-levels Anterior Cervical Discectomy and Fusion Titanium Cages Versus Polyetheretherketone (PEEK) Cages. Journal of Spinal Disorders & Techniques 2010; 23(5): 310–316. | China | 133 | 52 |
| 30 | Phillips Frank M, Geisler Fred H, Gilder Kye M, et al. Long-term Outcomes of the US FDA IDE Prospective, Randomized Controlled Clinical Trial Comparing PCM Cervical Disc Arthroplasty With Anterior Cervical Discectomy and Fusion. Spine 2015; 40(10): 674–683. | United States | 130 | 89 |
| 31 | Davis Reginald J, Kim, Kee D, Hisey Michael S, et al. Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial. Journal of Neurosurgery-Spine 2013; 19(5): 532–545. | United States | 130 | 61 |
| 32 | Veeravagu Anand, Cole Tyler, Jiang Bowen, et al. Revision rates and complication incidence in single- and multilevel anterior cervical discectomy and fusion procedures: an administrative database study. Spine Journal 2014; 14(7): 1125–1131. | United States | 127 | 84 |
| 33 | Jawahar Ajay, Cavanaugh David A, Kerr Eubulus J 3rd, et al. Total disc arthroplasty does not affect the incidence of adjacent segment degeneration in cervical spine: results of 93 patients in three prospective randomized clinical trials. Spine Journal 2010; 10(12): 1043–1048. | United States | 126 | 30 |
| 34 | Samartzis Dino, Shen Francis H, Lyon Craig, et al. Does rigid instrumentation increase the fusion rate in one-level anterior cervical discectomy and fusion? Spine journal 2004; 4(6): 636–643. | United States | 126 | 27 |
| 35 | Phillips Frank M, Lee Joe Y B, Geisler Fred H, et al. A Prospective, Randomized, Controlled Clinical Investigation Comparing PCM Cervical Disc Arthroplasty With Anterior Cervical Discectomy and Fusion 2-Year Results From the US FDA IDE Clinical Trial. Spine 2013; 38(15): E907–E918. | United States | 125 | 52 |
| 36 | Shin Dong Ah, Yi Seong, Yoon Do Heum, et al. Artificial Disc Replacement Combined With Fusion Versus Two-Level Fusion in Cervical Two-Level Disc Disease. Spine 2009; 34(11): 1153–1159. | South Korea | 120 | 34 |
| 37 | Ruetten Sebastian, Komp Martin, Merk Harry. Full-endoscopic anterior decompression versus conventional anterior decompression and fusion in cervical disc herniations. International Orthopaedics 2009; 33(6): 1677–1682. | Germany | 117 | 61 |
| 38 | Lin Qiushui, Zhou Xuhui, Wang Xinwei, et al. A comparison of anterior cervical discectomy and corpectomy in patients with multilevel cervical spondylotic myelopathy. European Spine Journal 2012; 21(3): 474–481. | China | 113 | 25 |
| 39 | Delamarter Rick B, Zigler Jack. Five-Year Reoperation Rates, Cervical Total Disc Replacement Versus Fusion, Results of a Prospective Randomized Clinical Trial. Spine 2013; 38(9): 711–717. | United States | 112 | 56 |
| 40 | Hilibrand AS, Fye MA, Emery SE, et al. Impact of smoking on the outcome of anterior cervical arthrodesis with interbody or strut-grafting. Journal of Bone and Joint Surgery-American Volume 2001; 83A(5): 668–673. | United States | 111 | 42 |
| 41 | Coric Domagoj, Kim Paul K, Clemente Jonathan D, et al. Prospective randomized study of cervical arthroplasty and anterior cervical discectomy and fusion with long-term follow-up: results in 74 patients from a single site. Journal of Neurosurgery-Spine 2013; 18(1): 36–42. | United States | 109 | 42 |
| 42 | Tumialan Luis M, Pan Jeff, Rodts Gerald E, et al. The safety and efficacy of anterior cervical discectomy and fusion with polyetheretherketone spacer and recombinant human bone morphogenetic protein-2: a review of 200 patients. Journal of Neurosurgery-Spine 2008; 8(6): 529–535. | United States | 108 | 20 |
| 43 | Janssen Michael E, Zigler Jack E, Spivak Jeffrey M, et al. ProDisc-C Total Disc Replacement Versus Anterior Cervical Discectomy and Fusion for Single-Level Symptomatic Cervical Disc Disease Seven-Year Follow-up of the Prospective Randomized US Food and Drug Administration Investigational Device Exemption Study. Journal of Bone and Joint Surgery-American Volume 2015; 97A(21): 1738–1747. | United States | 106 | 79 |
| 44 | Wu Wen-Jian, Jiang Lei-Sheng, Liang Yu, et al. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. European Spine Journal 2012; 21(7): 1374–1382. | China | 104 | 52 |
| 45 | Mummaneni Praveen V, Kaiser Michael G, Matz Paul G, et al. Cervical surgical techniques for the treatment of cervical spondylotic myelopathy. Journal of Neurosurgery-Spine 2009; 11(2): 130–141. | United States | 103 | 31 |
| 46 | McAfee Paul C, Cappuccino Andrew, Cunningham Bryan W, et al. Lower Incidence of Dysphagia With Cervical Arthroplasty Compared With ACDF in a Prospective Randomized Clinical Trial. Journal of Spinal Disorders & Techniques 2010; 23(1): 1–8. | United States | 103 | 28 |
| 47 | Zhang Xuesong, Zhang Xuelian, Chen Chao, et al. Randomized, Controlled, Multicenter, Clinical Trial Comparing BRYAN Cervical Disc Arthroplasty With Anterior Cervical Decompression and Fusion in China. Spine 2012; 37(6): 433–438. | China | 102 | 29 |
| 48 | Floyd T, Ohnmeiss D. A meta-analysis of autograft versus allograft in anterior cervical fusion. European Spine Journal 2000; 9(5): 398–403. | United States | 100 | 15 |
| 49 | Shriver Michael F, Lewis Daniel J, Kshettry Varun R, et al. Pseudoarthrosis rates in anterior cervical discectomy and fusion: a meta-analysis. Spine Journal 2015; 15(9): 2016–2027. | United States | 96 | 74 |
| 50 | Valencia Maldonado Carlos, Diaz-Romero Paz Ricardo, Balhen Martin Claudia. Adjacent-level degeneration after cervical disc arthroplasty versus fusion. European Spine Journal 2011; 20: 403–407. | Spain | 95 | 36 |
| 51 | Gao Yu, Liu Ming, Li Tao, et al. A Meta-Analysis Comparing the Results of Cervical Disc Arthroplasty with Anterior Cervical Discectomy and Fusion (ACDF) for the Treatment of Symptomatic Cervical Disc Disease. Journal of Bone and Joint Surgery-American Volume 2013; 95A(6): 555–561. | China | 94 | 29 |
| 52 | Jagannathan Jay, Shaffrey Christopher L, Oskouian Rod J, et al. Radiographic and clinical outcomes following single-level anterior cervical discectomy and allograft fusion without plate placement or cervical collar. Journal of Neurosurgery-Spine 2008; 8(5): 420–428. | United States | 93 | 35 |
| 53 | Park Daniel K, Lin Eric L, Phillips Frank M. Index and Adjacent Level Kinematics After Cervical Disc Replacement and Anterior Fusion In Vivo Quantitative Radiographic Analysis. Spine 2011; 36(9): 721–730. | United States | 93 | 25 |
| 54 | Dowd GC, Wirth FP. Anterior cervical discectomy: is fusion necessary? Journal of Neurosurgery 1999; 90(1): 8–12. | United States | 92 | 21 |
| 55 | Park Dong-Hyuk, Ramakrishnan Prem, Cho Tai-Hyoung, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. Journal of Neurosurgery-Spine 2007; 7(3): 336–340. | South Korea | 92 | 19 |
| 56 | Wirth FP, Dowd GC, Sanders HF, et al. Cervical discectomy - A prospective analysis of three operative techniques. World Neurosurgery 2000; 53(4): 340–346. | United States | 91 | 26 |
| 57 | Elsawaf Ahmed, Mastronardi Luciano, Roperto Raffaelino, et al. Effect of cervical dynamics on adjacent segment degeneration after anterior cervical fusion with cages. Neurosurgical Review 2009; 32(2): 215–224. | Italy | 90 | 28 |
| 58 | Suchomel P, Barsa P, Buchvald P, et al. Autologous versus allogenic bone grafts in instrumented anterior cervical discectomy and fusion: a prospective study with respect to bone union pattern. European Spine Journal 2004; 13(6): 510–515. | Czech Republic | 89 | 27 |
| 59 | Iyer Sravisht, Kim Han Jo. Cervical radiculopathy. Current reviews in musculoskeletal medicine 2016; 9(3): 272–280. | United States | 88 | 77 |
| 60 | Cabraja Mario, Oezdemir Soner, Koeppen Daniel, et al. Anterior cervical discectomy and fusion: Comparison of titanium and polyetheretherketone cages. Bmc Musculoskeletal Disorders 2012; 13: 172. | Germany | 88 | 44 |
| 61 | Park Moon Soo, Kelly Michael P, Lee Dong-Ho, et al. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine Journal 2014; 14(7): 1228–1234. | South Korea | 87 | 64 |
| 62 | Oh Min Chul, Zhang Ho Yeol, Park Jeong Yoon, et al. Two-Level Anterior Cervical Discectomy Versus One-Level Corpectomy in Cervical Spondylotic Myelopathy. Spine 2009; 34(7): 692–696. | South Korea | 87 | 25 |
| 63 | Pollock Raymond, Alcelik Ilhan, Bhatia Chandra, et al. Donor site morbidity following iliac crest bone harvesting for cervical fusion: a comparison between minimally invasive and open techniques. European Spine Journal 2008; 17(6): 845–852. | United Kingdom | 86 | 24 |
| 64 | McAfee Paul C, Reah Chris, Gilder Kye, et al. A Meta-Analysis of Comparative Outcomes Following Cervical Arthroplasty or Anterior Cervical Fusion Results From 4 Prospective Multicenter Randomized Clinical Trials and Up to 1226 Patients. Spine 2012; 37(11): 943–952. | United States | 86 | 18 |
| 65 | Hisey Michael S, Bae Hyun W, Davis Reginald J, et al. Prospective, Randomized Comparison of Cervical Total Disk Replacement Versus Anterior Cervical Fusion Results at 48 Months Follow-up. Journal of Spinal Disorders & Techniques 2015; 28(4): E237–E243. | United States | 85 | 41 |
| 66 | Park Yung, Maeda Takeshi, Cho Woojin, et al. Comparison of anterior cervical fusion after two-level discectomy or single-level corpectomy: sagittal alignment, cervical lordosis, graft collapse, and adjacent-level ossification. Spine Journal 2010; 10(3): 193–199. | South Korea | 85 | 26 |
| 67 | McGirt Matthew J, Godil Saniya S, Asher Anthony L, et al. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurgical Focus 2015; 39(6): E9. | United States | 84 | 63 |
| 68 | Song Kyung-Jin, Lee Kwang-Bok, Song Ji-Hoon. Efficacy of multilevel anterior cervical discectomy and fusion versus corpectomy and fusion for multilevel cervical spondylotic myelopathy: a minimum 5-year follow-up study. European Spine Journal 2012; 21(8): 1551–1557. | South Korea | 83 | 36 |
| 69 | Liu Yang, Hou Yang, Yang Lili, et al. Comparison of 3 Reconstructive Techniques in the Surgical Management of Multilevel Cervical Spondylotic Myelopathy. Spine 2012; 37(23): E1450–E1458. | China | 82 | 35 |
| 70 | Fehlings Michael G, Arvin Babak. Surgical management of cervical degenerative disease: the evidence related to indications, impact, and outcome. Journal of Neurosurgery-Spine 2009; 11(2): 97–100. | Canada | 82 | 26 |
| 71 | Beaurain J, Bernard P, Dufour T, et al. Intermediate clinical and radiological results of cervical TDR (Mobi-C (R)) with up to 2 years of follow-up. European Spine Journal 2009; 18(6): 841–850. | France | 82 | 16 |
| 72 | Chang Ung-Kyu, Kim Daniel H, Lee Max C, et al. Range of motion change after cervical arthroplasty with ProDisc-C and Prestige artificial discs compared with anterior cervical discectomy and fusion. Journal of Neurosurgery-Spine 2007; 7(1): 40–46. | South Korea | 82 | 11 |
| 73 | Adamson Tim, Godil Saniya S, Mehrlich Melissa, et al. Anterior cervical discectomy and fusion in the outpatient ambulatory surgery setting compared with the inpatient hospital setting: analysis of 1000 consecutive cases. Journal of Neurosurgery-Spine 2016; 24(6): 878–884. | United States | 81 | 69 |
| 74 | Vaccaro Alexander, Beutler William, Peppelman Walter, et al. Clinical Outcomes With Selectively Constrained SECURE-C Cervical Disc Arthroplasty Two-Year Results From a Prospectivei, Randomized, Controlled, Multicenter Investigational Device Exemption Study. Spine 2013; 38(26): 2227–2239. | United States | 81 | 45 |
| 75 | Cho Samuel K, Riew K Daniel. Adjacent Segment Disease Following Cervical Spine Surgery. Journal of the American Academy of Orthopaedic Surgeons 2013; 21(1): 3–11. | United States | 81 | 31 |
| 76 | Anakwenze Okechukwu A, Auerbach Joshua D, Milby Andrew H, et al. Sagittal Cervical Alignment After Cervical Disc Arthroplasty and Anterior Cervical Discectomy and Fusion Results of a Prospective, Randomized, Controlled Trial. Spine 2009; 34(19): 2001–2007. | United States | 81 | 25 |
| 77 | Radcliff Kris, Coric Domagoj, Albert Todd. Five-year clinical results of cervical total disc replacement compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled, multicenter investigational device exemption clinical trial. Journal of Neurosurgery-Spine 2016; 25(2): 213–224. | United States | 79 | 61 |
| 78 | Verma Kushagra, Gandhi Sapan D, Maltenfort Mitchell, et al. Rate of Adjacent Segment Disease in Cervical Disc Arthroplasty Versus Single-Level Fusion Meta-analysis of Prospective Studies. Spine 2013; 38(26): 2253–2257. | United States | 79 | 38 |
| 79 | Lied Bjarne, Roenning Paal Andre, Sundseth Jarle, et al. Anterior cervical discectomy with fusion in patients with cervical disc degeneration: a prospective outcome study of 258 patients (181 fused with autologous bone graft and 77 fused with a PEEK cage). Bmc Surgery 2010; 10: 10. | Norway | 79 | 22 |
| 80 | Liao Jen-Chung, Niu Chi-Chien, Chen Wen-Jer, et al. Polyetheretherketone (PEEK) cage filled with cancellous allograft in anterior cervical discectomy and fusion. International Orthopaedics 2008; 32(5): 643–648. | China | 78 | 22 |
| 81 | van Jonbergen Hans-Peter W, Spruit Maarten, Anderson Patricia G, et al. Anterior cervical interbody fusion with a titanium box cage: early radiological assessment of fusion and subsidence. Spine Journal 2005; 5(6): 645–649. | Netherlands | 78 | 15 |
| 82 | Moreland Douglas B, Asch Harold L, Clabeaux David E, et al. Anterior cervical discectomy and fusion with implantable titanium cage: initial impressions, patient outcomes and comparison to fusion with allograft. Spine Journal 2004; 4(2): 184–191. | United States | 78 | 12 |
| 83 | Zdeblick T A, Cooke M E, Kunz D N, et al. Anterior cervical discectomy and fusion using a porous hydroxyapatite bone graft substitute. Spine 1994; 19(20): 2348–2357. | United States | 78 | 11 |
| 84 | van Eck Carola F, Regan Conor, Donaldson William F, et al. The Revision Rate and Occurrence of Adjacent Segment Disease After Anterior Cervical Discectomy and Fusion. Spine 2014; 39(26): 2143–2147. | United States | 77 | 28 |
| 85 | Nassr Ahmad, Lee Joon Y, Bashir Rubin S, et al. Does Incorrect Level Needle Localization During Anterior Cervical Discectomy and Fusion Lead to Accelerated Disc Degeneration? Spine 2009; 34(2): 189–192. | United States | 77 | 25 |
| 86 | Kelly Michael P, Mok James M, Frisch Richard F, et al. Adjacent Segment Motion After Anterior Cervical Discectomy and Fusion Versus ProDisc-C Cervical Total Disk Arthroplasty. Spine 2011; 36(15): 1171–1179. | United States | 77 | 20 |
| 87 | Liu Yang, Qi Min, Chen Huajiang, et al. Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy. European Spine Journal 2012; 21(12): 2428–2435. | China | 76 | 28 |
| 88 | Nanda Anil, Sharma Mayur, Sonig Ashish, et al. Surgical Complications of Anterior Cervical Diskectomy and Fusion for Cervical Degenerative Disk Disease: A Single Surgeon's Experience of 1576 Patients. World Neurosurgery 2014; 82(6). | United States | 75 | 43 |
| 89 | Hisey Michael S, Zigler Jack E, Jackson Robert, et al. Prospective, Randomized Comparison of One-level Mobi-C Cervical Total Disc Replacement vs. Anterior Cervical Discectomy and Fusion: Results at 5-year Follow-up. International journal of spine surgery 2016; 10: 10–10. | United States | 74 | 63 |
| 90 | Hisey Michael S, Bae Hyun W, Davis Reginald, et al. Multi-center, prospective, randomized, controlled investigational device exemption clinical trial comparing Mobi-C Cervical Artificial Disc to anterior discectomy and fusion in the treatment of symptomatic degenerative disc disease in the cervical spine. International journal of spine surgery 2014; 8: 7. | United States | 73 | 47 |
| 91 | Villavicencio Alan T, Pushchak Evan, Burneikiene, Sigita, et al. The safety of instrumented outpatient anterior cervical discectomy and fusion. Spine Journal 2007; 7(2): 148–153. | United States | 73 | 44 |
| 92 | Radcliff Kris, Davis Reginald J, Hisey Michael S, et al. Long-term Evaluation of Cervical Disc Arthroplasty with the Mobi-C© Cervical Disc: A Randomized, Prospective, Multicenter Clinical Trial with Seven-Year Follow-up. International Journal of Spine Surgery 2017; 11(4): 31. | United States | 72 | 69 |
| 93 | Gornet Matthew F, Burkus J Kenneth, Shaffrey Mark E, et al. Cervical disc arthroplasty with PRESTIGE LP disc versus anterior cervical discectomy and fusion: a prospective, multicenter investigational device exemption study. Journal of Neurosurgery-Spine 2015; 23(5): 558–573. | United States | 72 | 51 |
| 94 | Peolsson Anneli, Peolsson Michael. Predictive factors for long-term outcome of anterior cervical decompression and fusion: a multivariate data analysis. European Spine Journal 2008; 17(3): 406–414. | Sweden | 72 | 30 |
| 95 | Saifi Comron, Fein Arielle W, Cazzulino Alejandro, et al. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine Journal 2018; 18(6): 1022–1029. | United States | 71 | 71 |
| 96 | Memtsoudis Stavros G, Hughes Alexander, Ma Yan, et al. Increased In-hospital Complications After Primary Posterior versus Primary Anterior Cervical Fusion. Clinical Orthopaedics and Related Research 2011; 469(3): 649–657. | United States | 70 | 30 |
| 97 | Thorell W, Cooper J, Hellbusch L, et al. The long-term clinical outcome of patients undergoing anterior cervical discectomy with and without intervertebral bone graft placement. Neurosurgery 1998; 43(2): 268–273; discussion 273–264. | United States | 70 | 7 |
| 98 | Lovecchio Francis, Hsu Wellington K, Smith Timothy R, et al. Predictors of Thirty-Day Readmission After Anterior Cervical Fusion. Spine 2014; 39(2): 127–133. | United States | 69 | 42 |
| 99 | Peolsson A, Hedlund R, Vavruch L, et al. Predictive factors for the outcome of anterior cervical decompression and fusion. European Spine Journal 2003; 12(3): 274–280. | Sweden | 68 | 19 |
| 100 | Gruskay Jordan A, Fu, Michael, Basques Bryce A, et al. Factors Affecting Length of Stay and Complications After Elective Anterior Cervical Discectomy and Fusion A Study of 2164 Patients From The American College of Surgeons National Surgical Quality Improvement Project Database (ACS NSQIP). Clinical Spine Surgery 2016; 29(1): E34–E42. | United States | 66 | 50 |
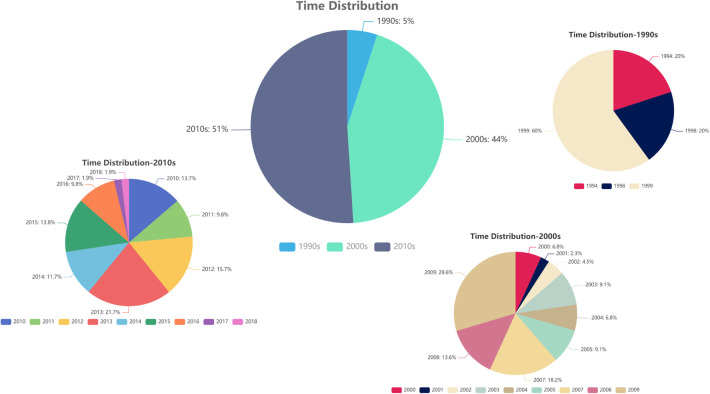
The publication time ranged from 1994 to 2018, and most articles were published in the 2010s (51%) and the 2000s (44%). Meanwhile, the articles published before 2000 only accounted for 5%, and the years with the largest number of articles were 2009 (n = 13) and 2013 (n = 11) (Figure 1).
Figure 1.
Time distribution.
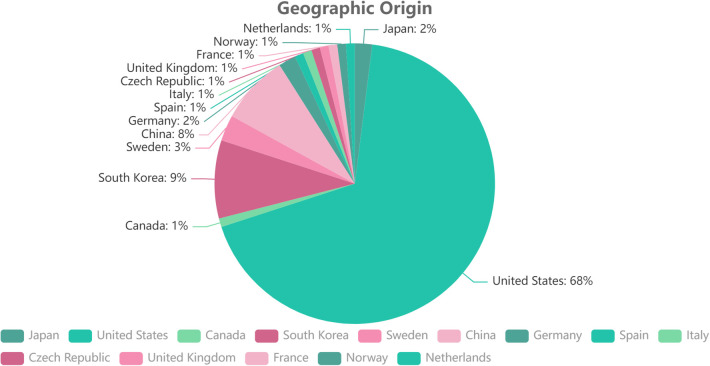
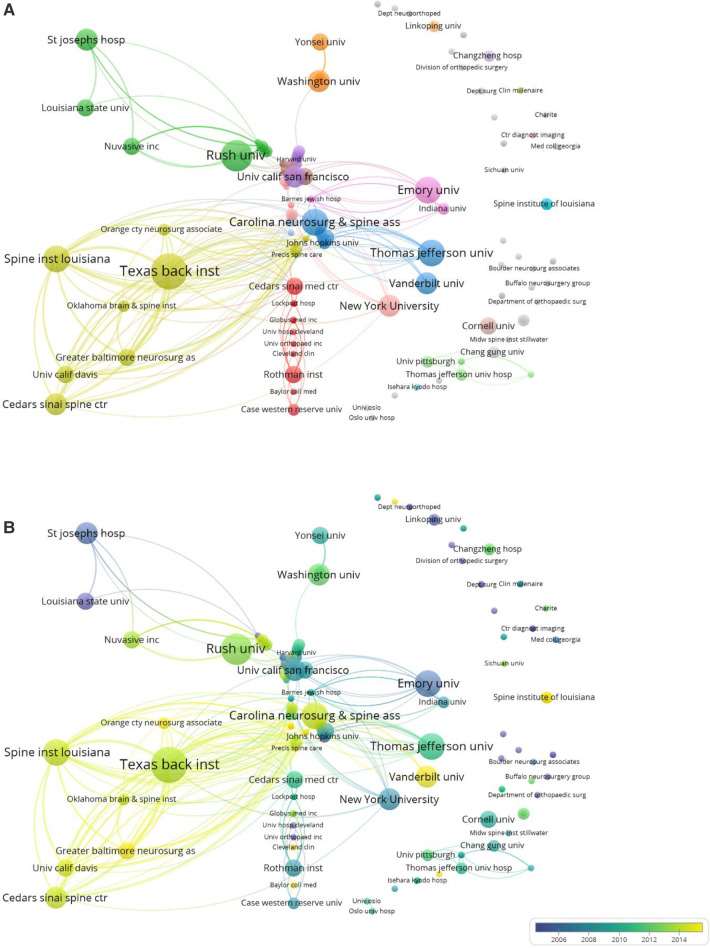
The top 100 most-cited articles originated from 14 countries. The United States has the greatest number of published articles (n = 68), followed by South Korea (n = 9), China (n = 8), Sweden (n = 3), and Japan and Germany (n = 2, each). The Czech Republic, Canada, France, Italy, the Netherlands, Norway, Spain, and the United Kingdom each contributed one article (Figure 2). Regarding the institutional information, analyzed using VOSviewer, the most productive research institutions were the Texas Back Institute (TBI) and Rush University, followed by Emory University, Spine Institute of Louisiana, Carolina Neurosurg & Spine Associates, University of California San Francisco, Thomas Jefferson University, Cedars-Sinai Spine Center, and New York University. The remaining institutions are listed in Table 2 and Figure 3 according to the number of most-cited articles and published times. The cluster analysis of institutions is shown in Figure 3A, the different colors represent different clusters and the size of the spot indicates the number of institutions. Time-dependent overlay visualization of institutions is shown in Figure 3B.
Figure 2.
Geographic distribution.
Table 2.
Institutions with multiple publications of the 100 top-cited articles on ACDF.
| Institution | Country | Publications |
|---|---|---|
| Texas Back Institute | United States | 10 |
| Rush University | United States | 9 |
| Thomas Jefferson University | United States | 8 |
| Emory University | United States | 8 |
| Spine Institute of Louisiana | United States | 7 |
| Carolina Neurosurgery & Spine Associates | United States | 7 |
Figure 3.
Degree of centrality analysis of the institutions of the whole 100 top-cited articles. (A) Overlay visualization. (B) Time-dependent overlay visualization.
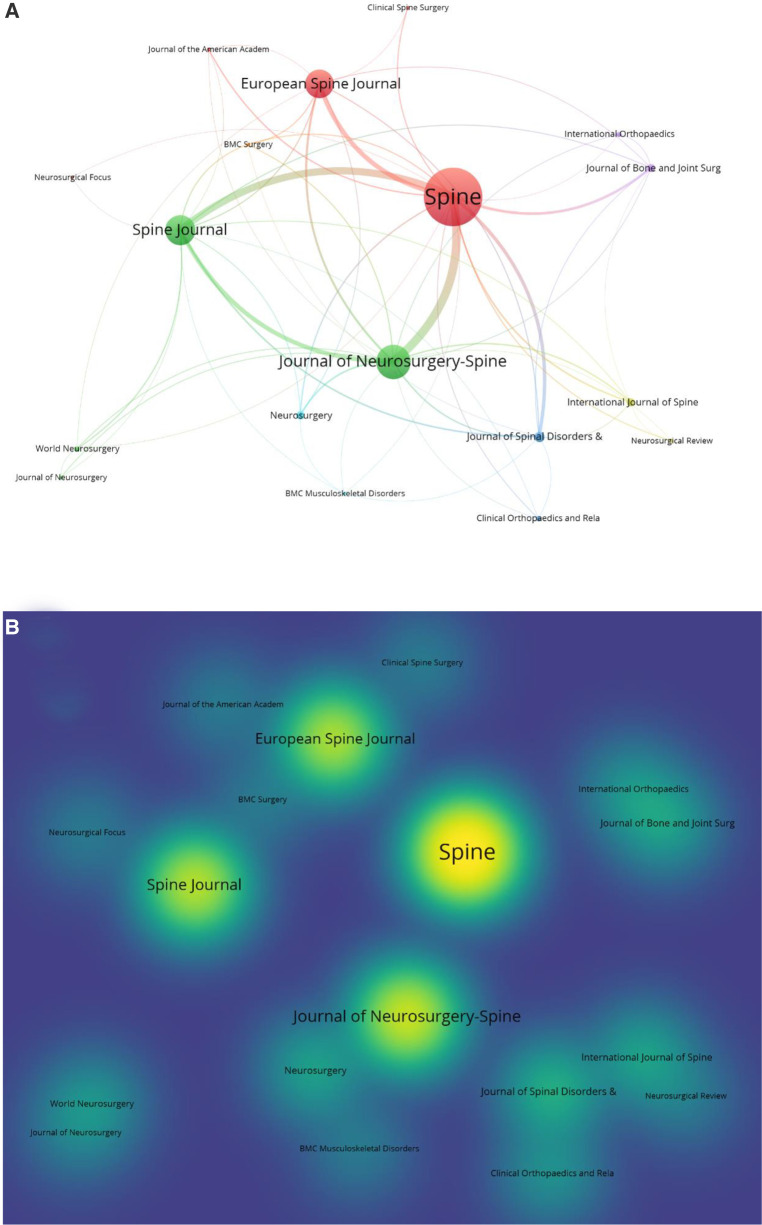
All 100 top-cited articles were published in 19 journals, led by one of the most authoritative journals, Spine, which has the most publications (n = 30), followed by Journal of Neurosurgery-Spine (n = 16), Spine Journal (n = 14), European Spine Journal (n = 13), Journal of Spinal Disorders & Techniques (n = 4), and Journal of Bone and Joint Surgery-American Volume, Neurosurgery and International journal of spine surgery (n = 3, each); the remainder are described in Table 3. The journals and hotmap of publications were also analyzed using VOSviewer. The cluster analysis of the journals is shown in Figure 4A, where different colors indicate different clusters and the size of the spot indicates the number of articles in each journal. As for the hotmap in Figure 4B, the density of the yellow color indicates the number of articles published in every journal, showing the same result as above.
Table 3.
Journals in which the top 100 cited articles were published.
| Journal | Country | IF (2021) | No. of citations | No. of articles |
|---|---|---|---|---|
| Spine | United States | 3.241 | 4,978 | 30 |
| Journal of Neurosurgery-Spine | United States | 3.467 | 2,259 | 16 |
| Spine Journal | United States | 4.297 | 1,841 | 14 |
| European Spine Journal | United States | 2.721 | 1,330 | 13 |
| Journal of Spinal Disorders & Techniques | United States | – | 462 | 4 |
| Journal of Bone and Joint Surgery-American Volume | United States | 6.558 | 311 | 3 |
| Neurosurgery | United States | 5.315 | 547 | 3 |
| International journal of spine surgery | United States | – | 219 | 3 |
| Clinical Orthopaedics and Related Research | United States | 4.755 | 205 | 2 |
| International Orthopaedics | Belgium | 3.479 | 195 | 2 |
| World Neurosurgery | Switzerland | 2.21 | 166 | 2 |
| Journal of Neurosurgery | United States | 5.408 | 92 | 1 |
| Neurosurgical Review | Germany | 2.8 | 90 | 1 |
| Bmc Musculoskeletal Disorders | United Kingdom | 2.562 | 88 | 1 |
| Current reviews in musculoskeletal medicine | United States | – | 88 | 1 |
| Neurosurgical Focus | United States | 4.332 | 84 | 1 |
| Journal of the American Academy of Orthopaedic Surgeons | United States | 4 | 81 | 1 |
| Bmc Surgery | United Kingdom | 2.03 | 79 | 1 |
| Clinical Spine Surgery | United States | 1.723 | 66 | 1 |
IF, impact factor.
Figure 4.
Degree of centrality analysis of the journals of the whole 100 top-cited articles. (A) Overlay visualization. (B) Hotmap overlay visualization.
Ten authors (first author, co-author, or corresponding author) published more than five publications within the top 100 most-cited articles (Table 4). The most prolific author was Todd J. Albert (n = 7), with a total of 1,312 citations, who is a surgeon-in-chief emeritus at the Hospital for Special Surgery and professor of orthopedic surgery at Weill Cornell Medical College (New York, NY, USA). Hyun W. Bae at the Cedars-Sinai Medical Center (Los Angeles, CA, USA) and Michael S. Hisey at the Texas Back Institute (Plano, TX, USA) were the second most prolific authors with six articles each. Alexander R. Vaccaro from the Rothman Institute, Thomas Jefferson University (Philadelphia, PA, USA) had 1,139 total citations, almost the same as Todd J Albert, who is the president of Rothman Orthopaedics and a leading doctor in spine surgery.
Table 4.
Authors with 5 or more top-cited articles.
| Author | No. of articles | Institution | Rank of articles | Total No. of citations |
|---|---|---|---|---|
| Todd J Albert | 7 | Hospital for Special Surgery and Weill Cornell Medical College, New York, NY, USA. | 1, 13, 27, 46, 77, 78, 92 | 1,312 |
| Hyun W Bae | 6 | Department of Orthopedic Surgery, Cedars-Sinai Medical Center, Los Angeles, CA, USA. | 28, 31, 65, 89, 90, 92 | 567 |
| Michael S Hisey | 6 | Department of Spine Surgery, Texas Back Institute, Plano, TX, USA. | 28, 31, 65, 89, 90, 92 | 567 |
| Alexander R Vaccaro | 5 | Department of Orthopaedic Surgery, Rothman Institute, Thomas Jefferson University, Philadelphia, PA, USA. | 1, 13, 27, 74, 78 | 1,139 |
| Jack E Zigler | 5 | Texas Back Institute and the Texas Back Institute Research Foundation, Plano, TX, USA. | 4, 18, 39, 43, 89 | 856 |
| K Daniel Riew | 5 | Department of Orthopedics, Columbia University, New York, NY, USA. | 5, 61, 66, 75, 95 | 705 |
| Frank M Phillips | 5 | Department of Orthopaedic Surgery, Rush University Medical Center, 1611 W. Harrison Street, Chicago, IL, USA. | 30, 35, 46, 53, 95 | 522 |
| Kee D Kim | 5 | Department of Neurological Surgery, UC Davis, Sacramento, CA, USA. | 28, 31, 65, 89, 90 | 495 |
| Reginald J Davis | 5 | Department of Neurosurgery, Greater Baltimore Medical Center, Baltimore, MD, USA. | 28, 31, 65,90, 92 | 493 |
| Greg Hoffman | 5 | Orthopedic North East, Fort Wayne, IN, USA. | 28, 31, 65,90, 92 | 493 |
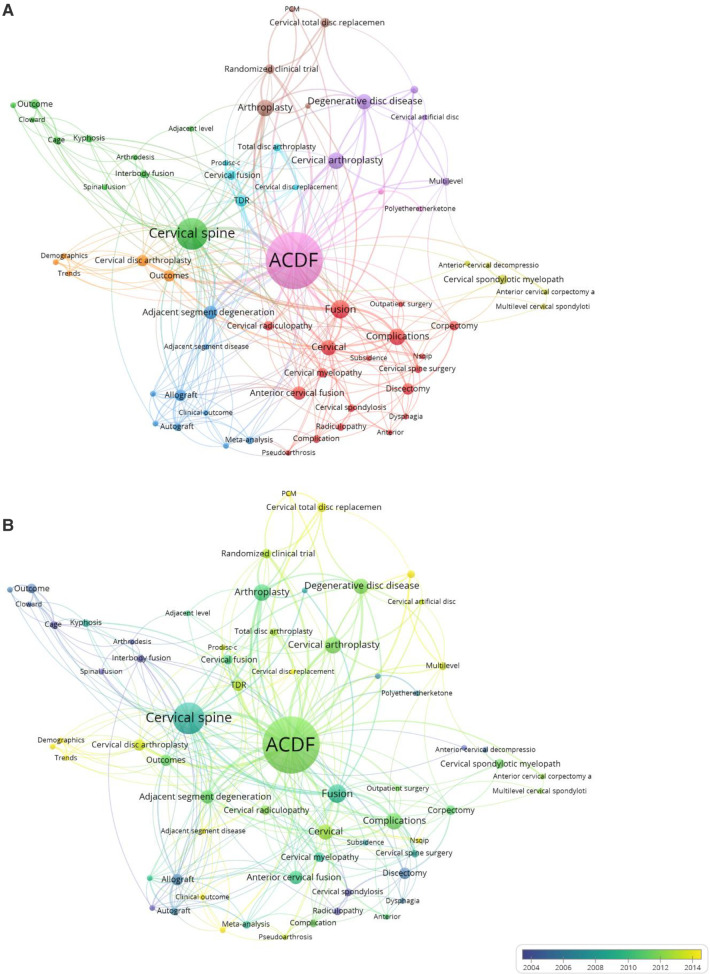
Author keywords of all 100 articles were analyzed via VOSviewer network analysis, as shown in Figure 5. The results showed that except for ACDF, cervical, cervical spine and fusion, the keywords adjacent segment degeneration, complications, cervical arthroplasty, degenerative disc disease, arthroplasty, and total disc replacement (TDR) also had a higher degree of centrality (Figure 5A). Furthermore, each node is colored based on when they occurred, in a blue-to-yellow gradient (Figure 5B); this shows that except for ACDF, cervical and complications, the keywords adjacent segment degeneration, adjacent segment disease, TDR, cervical disc replacement, cervical disc arthroplasty, cervical arthroplasty, prodisc-c, multilevel, and clinical outcome have occurred in recent years.
Figure 5.
Degree of centrality analysis of the author key words of the whole 100 top-cited articles. (A) Overlay visualization. (B) Time-dependent overlay visualization.
Discussion
The citation number is an important bibliometric indicator and a useful tool to measure the influence of publications. Many bibliometric analysis methods have also been used in various kinds of articles (17). In this study, we aimed to provide a better understanding of the historical knowledge of surgeons regarding ACDF. We also wanted to determine which articles regarding ACDF have been more impactful by identifying and analyzing the characteristics of the 100 most-cited articles.
The top 100 articles on ACDF were cited a mean of 131.81 ± 100.18 times (range, 66–660), which is more than the number of citations in other fields of spine surgery, such as endoscopic spine surgery research (mean, 84.4) (18), spinal disc arthroplasty research (mean, 115.1) (19), adult spinal deformity (mean, 34.8) (20), and idiopathic scoliosis (mean, 137.5) (21). This indicates that ACDF has been studied more frequently than other topics within the field of spine surgery.
Most of the 100 top-cited articles were published in the 2010s (51%) and the 2000s (44%), whereas only 5% were published before 2000. In our experience, older articles tend to have more citations; yet, we obtained the opposite results. This may be explained by the “obliteration by incorporation” concept, whereby a new article that originates from an early influential article gains greater popularity, reducing the citations of the original article (22). However, some researchers believe that articles may show their value 20 years after their publication (23). Moreover, some medical techniques and concepts from articles published before 2000 have been inevitably innovated by new technologies, discoveries, and views. This may explain how the 100 top-cited articles were distributed in different periods, and why the most recent article included in our list was published in 2018. Recently published research requires more time to accumulate citations and establish its significance.
As for the citations in the last five years, we found that some of the 20 top-cited articles only have a few dozen citations, such as ranks 9, 10, 15, 19, and 20 in Table 1. For several articles among the 80–100 top-cited ones, we found that the citation number for the last 5 years almost coincided with the total citation number, such as ranks 89, 90, 92, 93, 95, 98, and 100 (Table 1). Progress in academic concepts, surgical skills, and scientific research may explain this phenomenon and indicate the change in research hotspots in cervical spine surgery.
The most cited article was an investigation of donor site morbidity after anterior iliac crest bone harvest for single-level ACDF surgery by Silber Jeff S. et al. with 660 total citations after publication in 2003, which first focused on complications in the iliac crest bone graft site after single-level ACDF surgery (24). The authors found that a large percentage of patients suffered from chronic donor site pain after surgery, and long-term functional impairment could also be a significant problem. Although the study was published 20 years before, this pivotal study made surgeons aware of the need for alternative sources of graft material. Therefore, different types of interbody implants have been developed, such as hydroxyapatite (HA), polyetheretherketone (PEEK) cage, and titanium (Ti) cage, which have better shape, biomechanical function, and fusion rate (10, 25). This study greatly promoted the development of cervical interbody implants.
In 2007, Fountas Kostas et al. (26) published the second most cited article, a retrospective review, with 604 citations. This article was also about ACDF complications but focused on the ACDF surgery itself. The authors evaluated 1,015 patients undergoing first-time ACDF for cervical radiculopathy and/or myelopathy owing to degenerative disc disease and/or cervical spondylosis and analyzed the most common complications related to ACDF. This article had significant guiding significance for clinical spine surgeons in avoiding iatrogenic injury in ACDF surgery. It is worth mentioning that this article also had the most citations in the last 5 years.
The third most cited article was by Mummaneni Praveen et al. (27), which was also published in 2007. This prospective randomized multicenter study aimed to compare the clinical and radiographic outcomes between ACDF and cervical disc arthroplasty for the treatment of single-level cervical degenerative disc disease. The authors concluded that the PRESTIGE ST Cervical Disc System had more advantages in improving neurological success and clinical outcomes, as well as reducing the rate of secondary surgeries, compared with ACDF at 24 months of follow-up.
Further analysis of the articles revealed that three of the five most-cited articles were related to artificial cervical disc replacement (ADR). This kind of surgery was first proposed by Vincent E Bryan Jr in 2002 (28); since then, different kinds of movable artificial cervical discs like ProDisc-C and Mobi-C were designed and applied in clinical settings (29, 30). The Bryan disc was designed for maintaining the normal biomechanics of the cervical spine, to reduce the incidence of adjacent segment disease (ASD) and degeneration (31–33). With further research, surgeons found that the incidence of ASD was not significantly different between ACDF and ADR surgery (34, 35), but ADR surgery had the advantages of greater cervical spine mobility and less dysphagia. Moreover, the hot keywords in the 2010s were mostly about ADR surgery, which indicates that ADR surgery has huge potential in the future.
Most of the analyzed articles (68%) and journals (68.4%) originated in the United States, same as in the fields of arthroscopy (12), back pain research (36), and hand surgery (37). The inventors of ACDF, G.W. Smith, and R.B. Cloward are both from the United States, where ACDF surgery has spread worldwide. In addition, it is not unthinkable that authors from the United States are more likely to publish in US journals and usually prefer to cite US articles (38).
Regarding the journals, Spine was the most popular journal in the 100 most-cited articles, with 30 articles published in it and with 4,978 citations; three of these articles had over 300 citations. Spine is one of the most well-known and relatively older journals in the field of spine surgery, which may explain why it attracts important articles and receives more citations. The latest impact factor of Spine is 3.468, with a Q1 category quartile in the orthopedic JCR category in 2020.
The Texas Back Institute (TBI) was the most productive research institution, publishing 10 of the 100 top-cited articles. TBI was established in 1977, and surgeons have made great progress in the treatment of spinal diseases in the past 45 years. Michael S. Hisey and Jack E. Zigler, both from TBI, authored all 10 articles, making them the researchers with the most publications on the top 100 list. With their team, they have made significant achievements in cervical total disc replacement (Mobi-C from Zimmer Biomet® and ProDisc-C from Centinel Spine®) and conducted long-term follow-up studies on ACDF under many aspects (33, 39–47). Frank M. Phillips from Rush University is another ACDF pioneer, who also has advanced cervical disc replacement, and these works have made his institution productive (48–52). In addition, Thomas Jefferson University is also a productive research institution in the field of ACDF, and two of its doctors, Todd J. Albert and Alexander R. Vaccaro, are the greatest scholars in spine surgery, and their contribution to the field of ACDF relates to the most common ACDF and cervical disc replacement complications in the 100 top-cited articles (24, 34, 47, 50, 53–56). The scholars mentioned above provided great help and guidance for spine surgeons performing ACDF.
As expected, the most common keywords were ACDF, fusion, and cervical spine. Apart from these, adjacent segment degeneration, complications, cervical arthroplasty, degenerative disc disease, arthroplasty, and TDR were also frequently used keywords in the 100 top-cited articles. In chronological terms, the keywords adjacent segment degeneration, adjacent segment disease, TDR, cervical disc replacement, cervical disc arthroplasty, cervical arthroplasty, prodisc-c, multilevel, and clinical outcome were the most frequently used after 2010.
Surgery complications were always an important topic (57), and it was truly a trending research topic keyword before 2010; however, these keywords were featured relatively less often in the top 100 most-cited articles after 2010. This may be because most complications have been avoided with the directions from previous research and the development of surgical skills. The same phenomenon was observed for keywords such as cage, interbody fusion, cervical fusion, allograft, and anterior cervical decompression, likely for the same reason. In contrast, cervical disc replacement, PCM, Prodisc-c, TDR, adjacent segment disease, and multilevel became hot keywords after 2010. To our knowledge, adjacent segment degeneration after ACDF mostly depends on cervical biomechanical changes around the fusion level, and it could not be solved because of the principles of ACDF surgery (58–60), while ADR surgery can solve this problem in a targeted manner; therefore, we believe it was the reason for the change in hot keywords. The changes in other hot keywords' citation frequency, such as multilevel and clinical outcomes, may depend on the advances in diagnosis and treatment of the disease. In general, cervical disc replacement, adjacent segment disease, and clinical outcomes may be research hotspots for decades to come.
In our study, synthesis of the keywords in the top 100 most-cited articles on ACDF and all of author key words in the papers published over the last 5 years, we forecast the possible study trends in the future may include (1) new cervical interbody implants are the main objects of research, like Zero-profile intervertebral fusion system and 3D-print intervertebral fusion implants, etc.; (2) long time and large sample size follow-up research on new cervical interbody implants are needed in the future and (3) adjacent segment disease (degeneration) continues to be of interest for researchers.
This study has several limitations. First, all articles were identified according to the number of citations; therefore some new, just as relevant publications in the field did not have the same opportunity to be cited often enough to be included in this study. Second, we did not exclude self-citation, as authors prefer to cite articles from the journal with which they intend to publish (61), and the citation number may not completely reflect the research quality. Third, the geographical clustering is limited by the growing level of international collaboration. Besides, the highest quality articles are more likely to compare two techniques or provide evidence-based guidance rather than just focusing on ACDF alone (62). Then, this bibliometric analysis only included published journal articles and other materials, such as clinical guidelines, meeting notes, and textbooks. Finally, authors prefer to cite articles that already have many citations while ignoring quality or content (63).
Conclusion
This study identified and bibliometrically analyzed the 100 most-cited articles on ACDF between 1950 and 2022, including article title, authors, institutions, country, year of publication, journals, keywords, and total number of citations. Our study illustrates that ACDF is an improving and popular research field. Different types of cervical disc replacement skills, how to reduce the incidence of adjacent segment disease, and clinical outcomes may soon become research hotspots. This article provides insight into worldwide research trends and potential directions for future research on ACDF.
Acknowledgments
We thank Song Wu for his expertise in cervical spine surgery.
Funding
This study was partially supported by the National Natural Science Foundation of China (Grant Nos. 81502331) and the Natural Science Foundation of Hunan Province (Grant Nos. 2021JJ31010). The study supporters played no role in the study design, collection, analysis, and interpretation of data, in the writing of the manuscript, and in the decision to submit the manuscript for publication.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
Article review was performed by ZYD and JSL, data collection and analysis were performed by YJR and HQC. The first draft of the manuscript was written by ZYD and JSL and all the authors commented on previous versions of the manuscript. All the authors read, approved the final manuscript, and contributed to the study’s conception and design. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine. (2015) 40:E675–93. 10.1097/BRS.0000000000000913 [DOI] [PubMed] [Google Scholar]
- 2.Ganau M, Holly LT, Mizuno J, Fehlings MG. Future directions and new technologies for the management of degenerative cervical myelopathy. Neurosurg Clin N Am. (2018) 29:185–93. 10.1016/j.nec.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 3.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. (1958) 40-A:607–24. 10.2106/00004623-195840030-00009 [DOI] [PubMed] [Google Scholar]
- 4.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. (1958) 15:602–17. 10.3171/jns.1958.15.6.0602 [DOI] [PubMed] [Google Scholar]
- 5.Simmons EH, Bhalla SK. Anterior cervical discectomy and fusion. A clinical and biomechanical study with eight-year follow-up. J Bone Joint Surg Br. (1969) 51:225–37. 10.1302/0301-620X.51B2.225 [DOI] [PubMed] [Google Scholar]
- 6.Bailey RW, Badgley CE. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg Am. (1960) 42-A:565–94. 10.2106/00004623-196042040-00001 [DOI] [PubMed] [Google Scholar]
- 7.Bagby GW. Arthrodesis by the distraction-compression method using a stainless steel implant. Orthopedics. (1988) 11:931–4. 10.3928/0147-7447-19880601-13 [DOI] [PubMed] [Google Scholar]
- 8.Matgé G. Cervical cage fusion with 5 different implants: 250 cases. Acta Neurochir (Wien). (2002) 144(6):539–49. 10.1007/s00701-002-0939-0 [DOI] [PubMed] [Google Scholar]
- 9.Scholz M, Schnake KJ, Pingel A, Hoffmann R, Kandziora F. A new zero-profile implant for stand-alone anterior cervical interbody fusion. Clin Orthop Relat Res. (2011) 469:666–73. 10.1007/s11999-010-1597-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chong E, Pelletier MH, Mobbs RJ, Walsh WR. The design evolution of interbody cages in anterior cervical discectomy and fusion: a systematic review. BMC Musculoskelet Disord. (2015) 16:99. 10.1186/s12891-015-0546-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiss HK, Yamaguchi JT, Garcia RM, Hsu WK, Smith ZA, Dahdaleh NS. Trends in national use of anterior cervical discectomy and fusion from 2006 to 2016. World Neurosurg. (2020) 138:e42–51. 10.1016/j.wneu.2020.01.154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang N, Zhang W, George DM, Wei C, Su Y, Huang T. The top 100 most-cited articles on arthroscopy: most popular topic is rotator cuff rather than cartilage in the last 5 years. Arthroscopy. (2021) 37(6):1779–97. 10.1016/j.arthro.2021.01.039 [DOI] [PubMed] [Google Scholar]
- 13.Tang N, Zhang W, George DM, Su Y, Huang T. The top 100 most cited articles on anterior cruciate ligament reconstruction: a bibliometric analysis. Orthop J Sports Med. (2021) 9:2325967120976372. 10.1177/2325967120976372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yin M, Xu C, Mo W. The 100 most cited articles on lumbar spinal stenosis: a bibliometric analysis. Global Spine J. (2022) 12:381–91. 10.1177/2192568220952074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sinha A, Dheerendra S, Munigangaiah S. One hundred top cited articles in cervical myelopathy: a bibliographic analysis. Spine. (2021) 46:E1353–8. 10.1097/BRS.0000000000004100 [DOI] [PubMed] [Google Scholar]
- 16.Xie L, Chen Z, Wang H, Zheng C, Jiang J. Bibliometric and visualized analysis of scientific publications on atlantoaxial spine surgery based on web of science and VOSviewer. World Neurosurg. (2020) 137:435–42. 10.1016/j.wneu.2020.01.171. [DOI] [PubMed] [Google Scholar]
- 17.Zupic I, Cater T. Bibliometric methods in management and organization. Organ Res Methods. (2015) 18:429–72. 10.1177/1094428114562629 [DOI] [Google Scholar]
- 18.Zhao T, Shen J, Zheng B, Huang Y, Jin M, Morizane K, et al. The 100 most-cited publications in endoscopic spine surgery research. Global Spine J. (2021) 11:587–96. 10.1177/2192568220934740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhao T, Shen J, Zhang J, Hu X, Morizane K, Huang Y, et al. Top 100 cited articles on spinal disc arthroplasty research. Spine. (2020) 45:1530–6. 10.1097/BRS.0000000000003608 [DOI] [PubMed] [Google Scholar]
- 20.Liu P-C, Lu Y, Lin H-H, Yao Y-C, Wang S-T, Chang M-C, et al. Classification and citation analysis of the 100 top-cited articles on adult spinal deformity since 2011: a bibliometric analysis. J Chin Med Assoc. (2022) 85:401–8. 10.1097/JCMA.0000000000000642 [DOI] [PubMed] [Google Scholar]
- 21.Gambín-Botella J, Ayala M, Alfonso-Beltrán J, Barrios C. Predominance of studies with poor level of evidence among the top 100 most cited studies on idiopathic scoliosis: a bibliometric and content analysis. Spine Deform. (2018) 6:373–83. 10.1016/j.jspd.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Wumaier M, He D, Xiao B, Zhang J. The 100 top-cited articles on spinal deformity: a bibliometric analysis. Spine. (2020) 45:275–83. 10.1097/BRS.0000000000003247 [DOI] [PubMed] [Google Scholar]
- 23.Baltussen A, Kindler CH. Citation classics in anesthetic journals. Anesth Analg. (2004) 98:443–51. 10.1213/01.ANE.0000096185.13474.0A [DOI] [PubMed] [Google Scholar]
- 24.Silber JS, Anderson DG, Daffner SD, Brislin BT, Leland JM, Hilibrand AS, et al. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine. (2003) 28:134–9. 10.1097/00007632-200301150-00008 [DOI] [PubMed] [Google Scholar]
- 25.Muthiah N, Yolcu YU, Alan N, Agarwal N, Hamilton DK, Ozpinar A. Evolution of polyetheretherketone (PEEK) and titanium interbody devices for spinal procedures: a comprehensive review of the literature. Eur Spine J. (2022) 10.1007/s00586-022-07272-1 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine. (2007) 32:2310–7. 10.1097/BRS.0b013e318154c57e [DOI] [PubMed] [Google Scholar]
- 27.Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA. Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine. (2007) 6:198–209. 10.3171/spi.2007.6.3.198 [DOI] [PubMed] [Google Scholar]
- 28.Bryan VE. Cervical motion segment replacement. Eur Spine J. (2002) 11(Suppl 2):S92–7. 10.1007/s00586-002-0437-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DiAngelo DJ, Foley KT, Morrow BR, Schwab JS, Song J, German JW, et al. In vitro biomechanics of cervical disc arthroplasty with the ProDisc-C total disc implant. Neurosurg Focus. (2004) 17:E7. [PubMed] [Google Scholar]
- 30.Kim SH, Shin HC, Shin DA, Kim KN, Yoon DH. Early clinical experience with the mobi-C disc prosthesis. Yonsei Med J. (2007) 48:457–64. 10.3349/ymj.2007.48.3.457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gandhi AA, Kode S, DeVries NA, Grosland NM, Smucker JD, Fredericks DC. Biomechanical analysis of cervical disc replacement and fusion using single level, two level, and hybrid constructs. Spine. (2015) 40:1578–85. 10.1097/BRS.0000000000001044 [DOI] [PubMed] [Google Scholar]
- 32.Lei T, Liu Y, Wang H, Xu J, Ma Q, Wang L, et al. Clinical and radiological analysis of Bryan cervical disc arthroplasty: eight-year follow-up results compared with anterior cervical discectomy and fusion. Int Orthop. (2016) 40:1197–203. 10.1007/s00264-015-3098-7 [DOI] [PubMed] [Google Scholar]
- 33.Murrey D, Janssen M, Delamarter R, Goldstein J, Zigler J, Tay B, et al. Results of the prospective, randomized, controlled multicenter Food and Drug Administration investigational, device exemption study of the ProDisc-C total disc replacement versus anterior discectomy and fusion for the treatment of 1-level symptomatic cervical disc disease. Spine Journal. (2009) 9:275–86. 10.1016/j.spinee.2008.05.006 [DOI] [PubMed] [Google Scholar]
- 34.Verma K, Gandhi SD, Maltenfort M, Albert TJ, Hilibrand AS, Vaccaro AR, et al. Rate of adjacent segment disease in cervical disc arthroplasty versus single-level fusion: meta-analysis of prospective studies. Spine. (2013) 38:2253–7. 10.1097/BRS.0000000000000052 [DOI] [PubMed] [Google Scholar]
- 35.Dong L, Xu Z, Chen X, Wang D, Li D, Liu T, et al. The change of adjacent segment after cervical disc arthroplasty compared with anterior cervical discectomy and fusion: a meta-analysis of randomized controlled trials. Spine J. (2017) 17:1549–58. 10.1016/j.spinee.2017.06.010 [DOI] [PubMed] [Google Scholar]
- 36.Huang W, Wang L, Wang B, Yu L, Yu X. Top 100 cited articles on back pain research: a citation analysis. Spine. (2016) 41:1683–92. 10.1097/BRS.0000000000001736 [DOI] [PubMed] [Google Scholar]
- 37.Joyce CW, Kelly JC, Carroll SM. The 100 top-cited classic papers in hand surgery. J Plast Surg Hand Surg. (2014) 48:227–33. 10.3109/2000656X.2013.840640 [DOI] [PubMed] [Google Scholar]
- 38.Campbell FM. National bias: a comparison of citation practices by health professionals. Bull Med Libr Assoc. (1990) 78:376–82. PMID: [PMC free article] [PubMed] [Google Scholar]
- 39.Zigler JE, Delamarter R, Murrey D, Spivak J, Janssen M. ProDisc-C and anterior cervical discectomy and fusion as surgical treatment for single-level cervical symptomatic degenerative disc disease five-year results of a food and drug administration study. Spine. (2013) 38:203–9. 10.1097/BRS.0b013e318278eb38 [DOI] [PubMed] [Google Scholar]
- 40.Davis RJ, Nunley PD, Kim KD, Hisey MS, Jackson RJ, Bae HW, et al. Two-level total disc replacement with Mobi-C cervical artificial disc versus anterior discectomy and fusion: a prospective, randomized, controlled multicenter clinical trial with 4-year follow-up results. J Neurosurg Spine. (2015) 22:15–25. 10.3171/2014.7.SPINE13953 [DOI] [PubMed] [Google Scholar]
- 41.Davis RJ, Kim KD, Hisey MS, Hoffman GA, Bae HW, Gaede SE, et al. Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial. J Neurosurg Spine (2013) 19:532–45. 10.3171/2013.6.SPINE12527 [DOI] [PubMed] [Google Scholar]
- 42.Delamarter RB, Zigler J. Five-year reoperation rates, cervical total disc replacement versus fusion, results of a prospective randomized clinical trial. Spine. (2013) 38:711–7. 10.1097/BRS.0b013e3182797592 [DOI] [PubMed] [Google Scholar]
- 43.Janssen ME, Zigler JE, Spivak JM, Delamarter RB, Darden BV, II, Kopjar B. ProDisc-C total disc replacement versus anterior cervical discectomy and fusion for single-level symptomatic cervical disc disease seven-year follow-up of the prospective randomized US food and drug administration investigational device exemption study. J Bone Jt Surg Am Vol. (2015) 97A:1738–47. 10.2106/JBJS.N.01186 [DOI] [PubMed] [Google Scholar]
- 44.Hisey MS, Bae HW, Davis RJ, Gaede S, Hoffman G, Kim KD, et al. Prospective, randomized comparison of cervical total disk replacement versus anterior cervical fusion results at 48 months follow-up. J Spinal Disord Tech. (2015) 28:E237–43. 10.1097/BSD.0000000000000185 [DOI] [PubMed] [Google Scholar]
- 45.Hisey MS, Zigler JE, Jackson R, Nunley PD, Bae HW, Kim KD, et al. Prospective, randomized comparison of one-level Mobi-C cervical total disc replacement vs. anterior cervical discectomy and fusion: results at 5-year follow-up. Int J Spine Surg. (2016) 10:10. 10.14444/3010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hisey MS, Bae HW, Davis R, Gaede S, Hoffman G, Kim K, et al. Multi-center, prospective, randomized, controlled investigational device exemption clinical trial comparing Mobi-C Cervical Artificial Disc to anterior discectomy and fusion in the treatment of symptomatic degenerative disc disease in the cervical spine. Int J Spine Surg. (2014) 8:7. 10.14444/1007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Radcliff K, Davis RJ, Hisey MS, Nunley PD, Hoffman GA, Jackson RJ, et al. Long-term evaluation of cervical disc arthroplasty with the Mobi-C(C) cervical disc: a randomized, prospective, multicenter clinical trial with seven-year follow-up. Int J Spine Surg. (2017) 11(4):31. 10.14444/4031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Phillips FM, Geisler FH, Gilder KM, Reah C, Howell KM, McAfee PC. Long-term outcomes of the US FDA IDE prospective, randomized controlled clinical trial comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. Spine. (2015) 40:674–83. 10.1097/BRS.0000000000000869 [DOI] [PubMed] [Google Scholar]
- 49.Phillips FM, Lee JYB, Geisler FH, Cappuccino A, Chaput CD, DeVine JG, et al. A prospective, randomized, controlled clinical investigation comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion 2-year results from the US FDA IDE clinical trial. Spine. (2013) 38:E907–18. 10.1097/BRS.0b013e318296232f [DOI] [PubMed] [Google Scholar]
- 50.McAfee PC, Cappuccino A, Cunningham BW, Devine JG, Phillips FM, Regan JJ, et al. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech. (2010) 23:1–8. 10.1097/BSD.0b013e31819e2ab8 [DOI] [PubMed] [Google Scholar]
- 51.Park DK, Lin EL, Phillips FM. Index and adjacent level kinematics after cervical disc replacement and anterior fusion in vivo quantitative radiographic analysis. Spine. (2011) 36:721–30. 10.1097/BRS.0b013e3181df10fc [DOI] [PubMed] [Google Scholar]
- 52.Saifi C, Fein AW, Cazzulino A, Lehman RA, Phillips FM, An HS, et al. Trends in resource utilization and rate of cervical disc arthroplasty and anterior cervical discectomy and fusion throughout the United States from 2006 to 2013. Spine Journal. (2018) 18:1022–9. 10.1016/j.spinee.2017.10.072 [DOI] [PubMed] [Google Scholar]
- 53.Riley LH, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG. Dysphagia after anterior cervical decompression and fusion - prevalence and risk factors from a longitudinal cohort study. Spine. (2005) 30:2564–9. 10.1097/01.brs.0000186317.86379.02 [DOI] [PubMed] [Google Scholar]
- 54.Rihn JA, Kane J, Albert TJ, Vaccaro AR, Hilibrand AS. What is the incidence and severity of dysphagia after anterior cervical surgery? Clin Orthop Relat Res. (2011) 469:658–65. 10.1007/s11999-010-1731-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Radcliff K, Coric D, Albert T. Five-year clinical results of cervical total disc replacement compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled, multicenter investigational device exemption clinical trial. J. Neurosurg Spine. (2016) 25:213–24. 10.3171/2015.12.SPINE15824 [DOI] [PubMed] [Google Scholar]
- 56.Vaccaro A, Beutler W, Peppelman W, Marzluff JM, Highsmith J, Mugglin A, et al. Clinical outcomes with selectively constrained SECURE-C cervical disc arthroplasty two-year results from a prospectivei, randomized, controlled, multicenter investigational device exemption study. Spine. (2013) 38:2227–39. 10.1097/BRS.0000000000000031 [DOI] [PubMed] [Google Scholar]
- 57.Ratliff JK, Lebude B, Albert T, Anene-Maidoh T, Anderson G, Dagostino P, et al. Complications in spinal surgery: comparative survey of spine surgeons and patients who underwent spinal surgery. J Neurosurg Spine. (2009) 10:578–84. 10.3171/2009.2.SPINE0935 [DOI] [PubMed] [Google Scholar]
- 58.Hashimoto K, Aizawa T, Kanno H, Itoi E. Adjacent segment degeneration after fusion spinal surgery-a systematic review. Int Orthop. (2019) 43:987–93. 10.1007/s00264-018-4241-z [DOI] [PubMed] [Google Scholar]
- 59.Helgeson MD, Bevevino AJ, Hilibrand AS. Update on the evidence for adjacent segment degeneration and disease. Spine J. (2013) 13:342–51. 10.1016/j.spinee.2012.12.009 [DOI] [PubMed] [Google Scholar]
- 60.Hilibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. (2004) 4:190S–4S. 10.1016/j.spinee.2004.07.007 [DOI] [PubMed] [Google Scholar]
- 61.Mavrogenis AF, Ruggieri P, Papagelopoulos PJ. Self-citation in publishing. Clin Orthop Relat Res. (2010) 468:2803–7. 10.1007/s11999-010-1480-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kato S, Ganau M, Fehlings MG. Surgical decision-making in degenerative cervical myelopathy - anterior versus posterior approach. J Clin Neurosci. (2018) 58:7–12. 10.1016/j.jocn.2018.08.046 [DOI] [PubMed] [Google Scholar]
- 63.Lefaivre KA, Shadgan B, O’Brien PJ. 100 Most cited articles in orthopaedic surgery. Clin Orthop Relat Res. (2011) 469:1487–97. 10.1007/s11999-010-1604-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.