Key Teaching Points.
-
•
Even if high output cannot capture the His bundle, there is a possibility that a patient’s posture, heartbeat, or respiration can affect pacing.
-
•
Intermittent His bundle capture can cause inappropriate pacing. If intermittent His bundle capture is seen, the mode and post–atrial pacing ventricular blanking period of the pacemaker should be checked.
-
•
Incomplete His bundle capture might not be able to preserve left ventricular function; therefore, regular follow-up is needed, and upgrading the pacemaker to cardiac resynchronization therapy should be considered proactively.
Introduction
Right ventricular (RV) stimulations of conventional pacemakers cause ventricular dyssynchrony, in which aberrant left ventricular (LV) depolarization occurs, leading to LV remodeling and abnormalities in systolic and diastolic function, and can increase the risk of heart failure hospitalizations.1 His bundle pacing (HBP), a physiological alternative to RV pacing, has been associated with reduction in the combined endpoints of death, hospitalization owing to heart failure, and upgrade to cardiac resynchronization therapy.2 On the other hand, the HBP lead is sometimes difficult to place in the appropriate position. We present a case of inappropriate pacing owing to intermittent His bundle capture in a patient with a permanent His bundle pacemaker.
Case report
A 77-year-old Japanese woman with a history of myocardial infarction and permanent atrial fibrillation presented with dyspnea. Holter electrocardiography (ECG) during a dyspneic episode revealed complete atrioventricular block with atrial fibrillation. Transthoracic echocardiography showed severe hypokinesis of the LV posterior wall of the left ventricle; therefore, the global LV ejection fraction decreased to 47%. To avoid deterioration in this ejection fraction owing to RV pacing, we implanted a permanent HBP pacemaker, not cardiac resynchronization therapy (CRT), because previous coronary angiography showed that lateral and posterolateral veins looked too small to accommodate an LV pacing lead.
When we informed her of the risk of dislodging with an HBP lead, she requested back-up owing to her strong symptoms. Therefore, we decided to place an RV lead in addition to an HBP lead. During the procedure, we first indwelled the RV lead (3830 SelectSecure; Medtronic, Minneapolis, MN) conventionally. Subsequently, we placed the HBP lead (3830 SelectSecure; Medtronic, Minneapolis, MN) using a dedicated delivery sheath (SelectSite - C315 His; Medtronic, Minneapolis, MN) and checked the His bundle potential. A unipolar electrogram (EGM) was recorded from the lead tip and displayed on an electrophysiology recording system (Bard; Boston Scientific, Lowell, MA) and a Medtronic pacing system analyzer (model 2290). After the lead was fixed at the His bundle region, the His bundle injury current was recorded from this lead. At the end of the procedure, the HBP lead was connected to the atrial port and the RV lead to the ventricular port of the permanent pacemaker (Azure XT DR; Medtronic, Minneapolis, MN). The parameters of the electrodes were as follows: HBP threshold: 0.25 V / 0.4 ms; HBP sensing: 13.0 mV; HBP impedance: 817 Ω; RV threshold: 0.5 V / 0.4 ms; RV sensing: 4.3 mV; RV impedance: 437 Ω.
We set the pacing mode to managed ventricular pacing (MVP). This mode provides atrial-based pacing with a ventricular back-up and may reduce unnecessary RV pacing. Furthermore, if the HBP lead fails to capture, the device is designed to switch to the DDDR or DDD mode. In addition, we turned off ventricular safety pacing to avoid inappropriate pacing owing to misrecognition of cross-talk (Figure 1a).
Figure 1.
a: Pacemaker mode and settings. The pacing mode was AAI <=> DDD, which is almost equivalent to the managed ventricular pacing (MVP) mode of Medtronic’s pacemaker. “V. Safety Pacing” stands for ventricular safety pacing, which was turned off to avoid inappropriate pacing. The post–atrial pacing ventricular blanking period was fixed at 80 ms and not adjustable. b: The scheme of back-up pacing for MVP. In this patient, the ventricular sensing (VS) after a narrow waveform was within the blanking period. Therefore, the back-up atrial pacing (AP) and ventricular pacing (VP) appeared according to the interval shown because the pacemaker misread this as an atrioventricular (AV) block.
After implantation, chest radiograph showed that the HBP lead was placed in the region of the His bundle (Figure 2a). The locations of the pacemaker and its leads had not changed since the procedure was performed. However, a 12-lead ECG indicated a wide QRS complex with a left bundle branch block morphology (Figure 2c), which differed from the morphology before the implant procedure (Figure 2b). This QRS morphology was suspicious of myocardial-only capture because of notching in leads I, V1, and V5–V6. Before the patient’s discharge, she complained of palpitations. Therefore, we checked the pacemaker and found about 2% RV pacing, which was inappropriate. Furthermore, an endocardial EGM indicated that serial narrow pacing waveforms were producing inappropriate pacing (Figure 3a) and that the conduction time between the HBP and RV leads was shortened from 85–90 ms to 50–60 ms when these narrow waveforms occurred. Therefore, we inferred that the wide pacing waveforms on EGM, which accounted for the majority of HBP pacing, corresponded to the wide QRS complex with the left bundle branch block morphology and RV septal pacing (Figure 3b). On the other hand, the narrower pacing waveforms on EGM were capturing the His bundle, and had a shorter conduction time (Figure 3c). This shorter-interval pacing was suspected as the cause of the palpitations. Though MVP is designed to recognize the interval within 80 ms after atrial pacing as a post–atrial pacing ventricular blanking (PAVB) period, the EGM recorded ventricular sensing during this period. Serial His bundle captures made the pacemaker misrecognize RV sensing within the blanking period as no pulse in the ventricles or as an atrioventricular block, at which time back-up pacing occurred, with an interval consistent with back-up pacing of MVP (Figure 1b). This intermittent His bundle capture occurred regardless of the pacing amplitude or the pulse width.
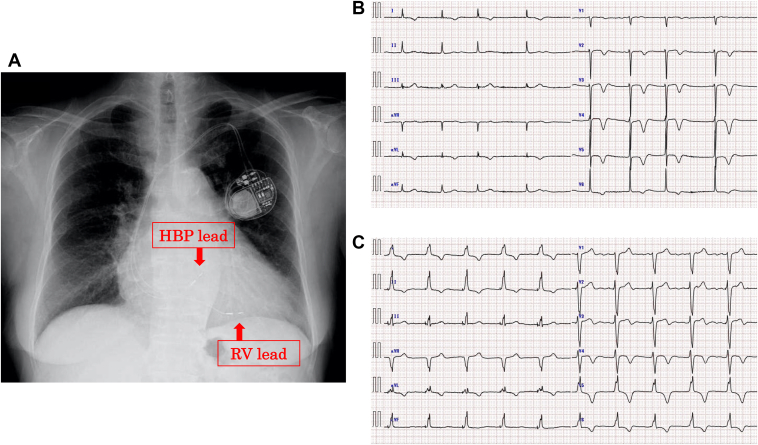
Figure 2.
a: A chest radiograph (posteroanterior projection) after implantation of the permanent pacemaker with direct His bundle pacing (HBP). RV = right ventricle. b: A 12-lead electrocardiogram (ECG) before the implantation showing atrial fibrillation and a negative T wave in leads I, aVL, and V2 owing to the previous myocardial infarction. c: A 12-lead ECG after the implantation. The QRS complex showed a left bundle branch block–type morphology and was prolonged to 142 ms. In addition, there were QRS notches in leads I and V5–V6.
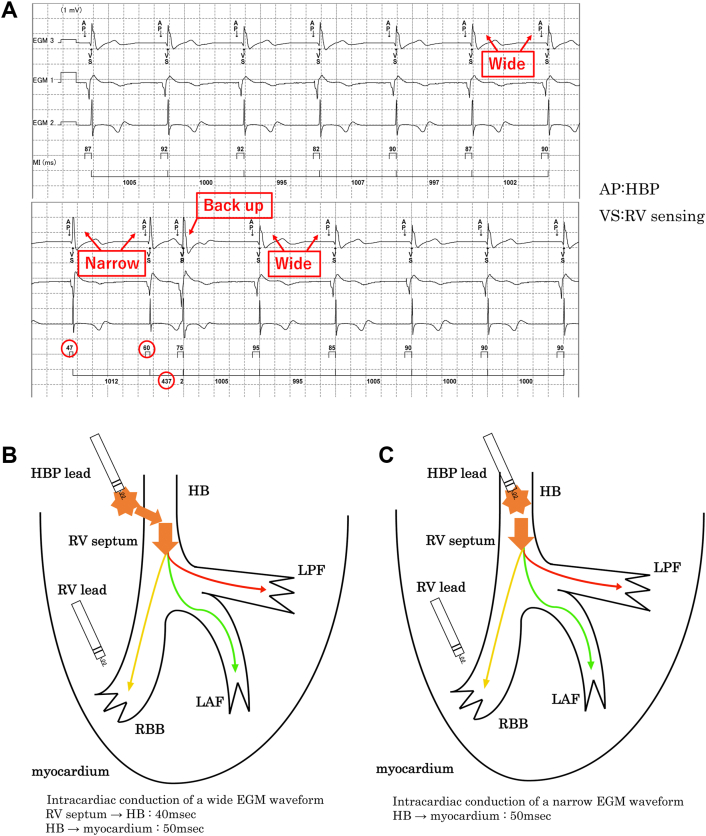
Figure 3.
a: The endocardial electrogram (EGM) during an inappropriate back-up. Inappropriate back-up pacing necessarily followed serial narrow waveforms. The interval of back-up pacing in this case corresponded to the interval of managed ventricular pacing (MVP). Subsequent back-up pacing did not occur because of right ventricular (RV) pacing after a wide waveform that occurred within 1300 ms. b: Intracardiac conduction of the wide waveforms. Wide waveforms corresponded to the left bundle branch block–type morphology of the QRS complex on the 12-lead electrocardiogram and were presumed to represent septal pacing. The conduction interval between the RV septum and the His bundle was about 40 ms because the interval of the leads with narrow waveforms, which represented the conduction interval between the His bundle and the myocardium, was 50 ms. c: Intracardiac conduction of the narrow waveforms. The narrow waveforms were presumed to represent His bundle capture; therefore, the conduction interval between the His bundle and the myocardium was 50 ms, as described. Ap = HBP pacing; HB = His bundle; HBP = His bundle pacing; LAF = left anterior fascicle; LPF = left posterior fascicle; RBB = right bundle branch; Vp = RV pacing; Vs = RV sensing.
As the PAVB period required modification, we changed the mode of the pacemaker from MVP to DDD, which is designed to shorten this period to 30 ms. After this change, the pacemaker recognized ventricular sensing correctly, even when narrow waveforms appeared, without inappropriate pacing. Three months later, we checked the pacemaker again, and there was no RV pacing. In addition, the patient’s symptoms had disappeared after the shift in the pacemaker mode.
This case report was reviewed by the Institutional Review Board and informed consent was obtained from the patient.
Discussion
This report, which presents the case of a patient with intermittent His bundle capture resulting in inappropriate back-up pacing, demonstrates 3 important points.
The first point is related to the HBP lead. We checked both the His bundle potential while detaining the HBP lead and the His bundle injury current after fixing the lead, as has been described in a previous study.3 Therefore, the HBP lead may have experienced microdislodgement after placement. A 12-lead ECG after implantation suggested that pacing was a result of myocardial-only capture owing to the presence of QRS notches in leads 1, V5, and V6 (Figure 2b). Jastrzebski and colleagues4 have shown that electrocardiographic diagnosis of a loss of nonselective His bundle capture can involve a QRS notch or a slur in these leads, with an R-wave peak time over 110 ms. High pacing output can sometimes capture the His bundle5; however, in this case, the His bundle could not be captured completely regardless of adjusting the pacemaker. Nevertheless, intermittent His bundle capture occurred spontaneously, which caused unintentional back-up pacing. This finding may be explained by changes in the HBP lead location resulting from the heartbeat or respiration. The change in the conduction time between the HBP and RV leads demonstrated that the atrial pacing of the narrow waveforms captured the His bundle directly, which shortened the conduction time between the 2 leads (Figure 3c).
The second point is related to the PAVB period, which affected this inappropriate pacing. The usual PAVB period is set to about 40–50 ms.6,7 However, when a pacemaker is set to MVP, the blanking period is fixed at 80 ms.8 As proof of this concept, the interval of back-up pacing in this case corresponded to that of the atrioventricular block for MVP (Figures 1b and 3a). In addition, subsequent back-up pacing did not occur because RV pacing occurred within 1300 ms after a wide waveform. Generally, we consider the cross-talk sensing window and escape from inappropriate ventricular safety pacing. The cross-talk sensing window depends on the pacemaker manufacturer and is usually set between 95 and 120 ms.9 Because the conduction time between the HBP and RV leads was under 95 ms, we turned off ventricular safety pacing but did not adjust the PAVB period.
The third point is related to the future treatment protocol for this patient. Though we adjusted the pacemaker settings, we could not achieve complete His bundle capture. At 5-year follow-up of 192 patients in the United States, rates of death and heart failure hospitalization have been shown to be lower in an HBP group than in an RV-pacing group.10 Because this patient had a history of ischemic heart disease and mild reduction in LV ejection fraction, we chose HBP to preserve her LV function.11 However, Lustgarten and colleagues12 have reported that the response to CRT is equivalent to HBP; therefore, we need to consider whether we should proactively upgrade her pacemaker to CRT, especially if her LV function declines or her heart failure worsens in the future. There is a case report that HBP and RV leads were simultaneously implanted.13
There have been some reports regarding pacemaker issues related to MVP14 and HBP malfunctions.15 However, to the best of our knowledge, this is the first report of inappropriate pacing due to intermittent His bundle capture.
Conclusion
We reported a case of inappropriate pacing due to intermittent His bundle capture in a patient with a permanent His bundle pacemaker.
Implantation of both HBP lead and RV lead is useful because the RV lead enables upgrading to CRT and secures back-up RV pacing if the HBP lead does not work well. This case reveals the importance of the PAVB period when implanting both HBP lead and RV lead. Usually, the PAVB period is not important when a conventional DDD pacemaker is implanted because the conduction time between the 2 leads of the pacemaker is much longer than the PAVB period. However, a permanent His bundle pacemaker has a shorter conduction time between the 2 leads; therefore, improper setting of the PAVB period may cause inappropriate pacing, such as in this case.
The PAVB period can be determined by the mode of pacemaker; therefore, both should be focused on, especially when implanting permanent HBPs.
Footnotes
Funding Sources: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures: None.
References
- 1.Sweeney M.O., Hellkamp A.S., Ellenbogen K.A., et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation. 2003;107:2932–2937. doi: 10.1161/01.CIR.0000072769.17295.B1. [DOI] [PubMed] [Google Scholar]
- 2.Abdelrahman M., Subzposh F.A., Beer D., et al. Clinical outcomes of His bundle pacing compared to right ventricular pacing. J Am Coll Cardiol. 2018;71:2319–2330. doi: 10.1016/j.jacc.2018.02.048. [DOI] [PubMed] [Google Scholar]
- 3.Vijayaraman P., Dandamudi G. How to perform permanent His bundle pacing: tips and tricks. Pacing Clin Electrophysiol. 2016;39:1298–1304. doi: 10.1111/pace.12904. [DOI] [PubMed] [Google Scholar]
- 4.Jastrzebski M., Moskal P., Curila K., et al. Electrocardiographic characterization of non-selective His-bundle pacing: validation of novel diagnostic criteria. Europace. 2019;21:1857–1864. doi: 10.1093/europace/euz275. [DOI] [PubMed] [Google Scholar]
- 5.Burri H., Jastrezebski M., Vijayaraman P. Electrocardiographic analysis for His bundle pacing at implantation and follow-up. JACC Clin Electrophysiol. 2020;6:883–900. doi: 10.1016/j.jacep.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Konishi H., Fukuzawa K., Mori S., Kiuchi K., Hirata K. The limitations and potential adverse effects of the premature ventricular contraction response. J Arrhythm. 2018;34:572–575. doi: 10.1002/joa3.12082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Do D.H., Meyer S., Bradfield J., Shivkumar K., Boyle N.G., Khakpour H. Masked premature ventricular contractions and intradevice interaction causing ventricular fibrillation. HeartRhythm Case Rep. 2021;7:69–73. doi: 10.1016/j.hrcr.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MEDTRONIC ACADEMY Managed Ventricular Pacing (MVP) Feature. https://www.medtronicacademy.com/features/managed-ventricular-pacing-mvp-feature.
- 9.Singh M., McCoy C., Daniels J. Ventricular safety pacing triggered by right ventricular lead dislodgement. Circulation. 2019;140:1766–1768. doi: 10.1161/CIRCULATIONAHA.119.043267. [DOI] [PubMed] [Google Scholar]
- 10.Vijayaraman P., Naperkowski A., Subzposh F.A., et al. Permanent His-bundle pacing: long-term lead performance and clinical outcomes. Heart Rhythm. 2018;15:696–702. doi: 10.1016/j.hrthm.2017.12.022. [DOI] [PubMed] [Google Scholar]
- 11.Zanon F., Ellenbogen K.A., Dandamudi G., et al. Permanent His-bundle pacing: a systematic literature review and meta-analysis. Europace. 2018;20:1819–1826. doi: 10.1093/europace/euy058. [DOI] [PubMed] [Google Scholar]
- 12.Lustgarten D.L., Crespo E.M., Arkhipova-Jenkins I., et al. His-bundle pacing versus biventricular pacing in cardiac resynchronization therapy patients: a crossover design comparison. Heart Rhythm. 2015;12:1548–1557. doi: 10.1016/j.hrthm.2015.03.048. [DOI] [PubMed] [Google Scholar]
- 13.Meininghaus D.G., Lengiewicz M., Biembel, et al. A case report of simultaneous His pacemaker implantation and atrioventricular junction ablation following unsuccessful treatment of atrial fibrillation. Eur Heart J Case Rep. 2020;4:1–5. doi: 10.1093/ehjcr/ytaa259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perez M.V., Al-Ahmad A.A., Wang P.J., Turakhia M.P. Inappropriate pacing in a patient with managed ventricular pacing: what is the cause? Heart Rhythm. 2010;7:1336–1337. doi: 10.1016/j.hrthm.2010.04.028. [DOI] [PubMed] [Google Scholar]
- 15.Padala S.K., Ellenbogen K.A., Koneru J.N. Intermittent loss of capture in a His bundle pacemaker: what is the cause? Heart Rhythm Case Rep. 2017;3:555–558. doi: 10.1016/j.hrcr.2017.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]