Abstract
Background
Neonatal hypothermia at delivery, during transport and in the postnatal wards is common, under-recognized and infrequently monitored with prevalence ranging from 32% to 85%. This study compared conductive thermal mattress to routine care for prevention of hypothermia among low-birthweight (LBW) neonates during transport.
Methods
From July 2015 to November 2016 (historical controls), all eligible LBW neonates (1500–2499 g) were transported from the labour room/operation theatre to the neonatal intensive care unit (NICU)/postnatal wards using routine care (towels, blankets, cap, mittens and socks) and from December 2016 to December 2018 using conductive thermal mattress (EMBRACETM) Axillary temperature was measured before transport and at arrival in the NICU/postnatal wards using a digital thermometer.
Results
A total of 154 and 102 neonates were transported using conductive thermal mattress and routine care, respectively. The mean standard deviation (SD) axillary temperature at arrival in the postnatal wards in conductive thermal mattress and routine care group was 36.6 (0.6) ⁰C and 36.4 (0.5) ⁰C, respectively (p-value 0.005). Relative Risk (RR) of mild and moderate neonatal hypothermia among neonates transported using conductive thermal mattress compared to routine care group was 0.59 (0.33,1.07), number needed to treat (NNT) of 13 and 0.22 (0.04,1.07), NNT 22 respectively.
Conclusions
Use of conductive thermal mattress for transport among LBW neonates led to a significant, although clinically small improvement in admission temperatures at the NICU/postnatal ward and non-significant decrease in the incidence of hypothermia.
Keywords: Conductive thermal mattress, EMBRACETM warmer, Neonatal hypothermia
Introduction
Neonatal hypothermia is a common, under-recognized and infrequently monitored condition in the delivery room and postnatal wards. The period of greatest risk is at delivery, during transport and in the postnatal wards.1 The reported prevalence varies widely from 32% to 85% among hospitalized neonates and 11%–92% among neonates in community-based studies from Nepal and India,2 due to varying definitions of neonatal hypothermia, time of measurement, and settings (hospital-based, community, postnatal wards).
Laptook et al, in 2007 found a 28% increase in the odds of mortality and a 11% increase in late-onset sepsis with each 1 °C decrease in admission temperature below 36.5 °C.3 Large observational studies have found similar results; however, the evidence for a causal association is limited and hypothermia may be an indicator of the level of sickness and a marker for poor outcome in these neonates.
Thermoregulation among neonates is a delicate balance between mechanisms of heat production and loss. Neonates are at risk due to their large body surface area, lack of subcutaneous and brown fat and immature heat production mechanisms. This risk is higher among preterm and LBW neonates owing to decreased glycogen stores, immature skin and poor vascular control and is inversely proportional to gestational age and birth weight.
The World Health Organization (WHO)4 defines neonatal hypothermia as a core body temperature < 36.5 °C and classifies its severity as follows:
-
a)
Mild hypothermia/cold stress: 36.0 °C to 36.4 °C
-
b)
Moderate hypothermia: 32.0 °C to 35.9 °C
-
c)
Severe hypothermia: < 32.0 °C
Thermoregulation is a key component of essential newborn care. The admission temperature in the neonatal intensive care unit (NICU) is a quality indicator of the processes of care and an outcome measure.5
In Armed Forces hospitals, with a wide geographic distribution and extreme winter conditions for four to five months in several locations, neonates, especially preterm/and LBW are at risk of cold stress/hypothermia during the process of transport after delivery from the labour room or operation theatre to the NICU/postnatal wards. The routine care of neonates involves delivery on the mother's abdomen or receiving them on a prewarmed towel, immediate drying, discarding the wet towel and swaddling in towels or blankets before transport. Skin-to-skin care although recommended and encouraged, is not practised widely immediately after birth, and transport incubators are expensive and not available at all hospitals or are difficult to use due to road conditions and different locations of the labour room, operation theatres and NICU. The period during transport remains a critical risk period for hypothermia.
The present study planned to demonstrate if the conductive thermal mattress was a feasible and effective method of preventing hypothermia among LBW neonates during transport in our setting. Given its easy availability and low cost (approx. Rs 25,000/- per unit), it could be used in the service hospitals to enable stable thermoregulation during the critical and vulnerable period following delivery and transport.
Materials and methods
Study design, site and time frame
The design was an experimental study (with historical controls) conducted at a tertiary referral hospital of the Armed Forces with cases enrolled from December 2016 to December 2018. The historical controls were included from July 2015 to November 2016.
Inclusion criteria
All stable LBW (1500–2499 g) intramural neonates delivered by normal vaginal delivery/caesarean section were included in the study.
Exclusion criteria
The exclusion criteria were as follows:
-
1.
Neonates with birth asphyxia requiring resuscitation
-
2.
Neonates with birth weight <1500 g
-
3.
Any sick neonate
-
4.
Neonates with major congenital malformations
Sample size
Assuming the prevalence of mild/moderate hypothermia with routine care to be around 15%, a sample size of 300 neonates would be required (150 in each group) to determine if the conductive thermal mattress is able to reduce this to 5%, with a power of 80% and alpha error of 5%.
Ethical clearance
The study was approved by the institutional ethics committee. Informed parental consent was taken from parents of all neonates enrolled in the study.
Methods
Study site: location and care procedures
The study site was a tertiary referral hospital with many high-risk pregnancies which were referred in-utero. The number of deliveries at the study site were around 1100 per year, with approximately 600 deliveries by caesarean section and 500 by the vaginal route. The annual NICU admissions were around 160 per year.
The labour room was located on the first floor with a 1st stage room and two delivery tables with air-conditioning. There was a wall mounted thermometer which displayed the room air temperature and relative humidity. The routine deliveries were conducted by nursing officers with the obstetrician available on-call as required. The operation theatre was located on the second floor and had eight theatres which were centrally air conditioned. A wall mounted thermometer displayed the room air temperature and relative humidity. All caesarean deliveries were attended by a nursing officer along with the paediatrician, if required.
Immediately after delivery, neonates were delivered on the mother's abdomen or received on prewarmed towels and placed under the radiant warmer on manual mode (with 100% heater output) for immediate drying, cord clamping and stabilization. The weight was checked on a digital weighing scale and intramuscular injection Vitamin K given on the anterolateral aspect of the thigh. After initial stabilization, the neonate was transported to the NICU/postnatal wards on the first floor by the nursing officer or ward sahayika, along with the mother.
Education of care providers
Beginning in July 2015 and continuing till December 2018, all nursing officers and other care providers were sensitised at regular intervals (quarterly) to the dangers of neonatal hypothermia by short group teaching sessions, interactive discussions and video/webinar learning modules, regarding the technique of axillary temperature measurement in neonates and essential newborn care practices including the warm chain after birth. Adequate attention was given to the availability of prewarmed towels, disposables and sterile sheets for receiving the neonates after birth, which was ensured for each shift by the nursing officer on duty.
Temperature measurement
Digital thermometers (OMRON MC 246 digital thermometer) with accuracy of 0.1 °C were purchased and placed as part of the neonatal resuscitation tray at the delivery room, operation theatre and NICU/postnatal wards, and all nursing officers were instructed to be meticulous in recording the axillary temperature of the neonate before transport from the labour room/operation theatre and at arrival in the NICU/postnatal wards. The thermometers were replaced after 3 months of continuous use, and regular checking of accuracy and reliability was carried out at the different locations of their use.
Historical controls: July 2015 to November 2016
From July 2015 to November 2016, till the procurement of the conductive thermal mattress, all eligible neonates were transported after initial stabilization in the labour room/operation theatre to the NICU/postnatal wards using routine care (n = 102). This included the use of towels, blankets, cap and mittens and socks to swaddle the neonates. The axillary temperature was measured before transport and at arrival in the NICU/postnatal wards by the nursing officer. Standard guidelines were followed for treatment and management of mild or moderate hypothermia, if encountered.
Cases: December 2016 to December 2018
From December 2016, once the conductive thermal mattress (EMBRACE™ warmers) were procured, till December 2018, all eligible neonates were transported after initial stabilization in the labour room/operation theatre by using the conductive thermal mattress (n = 154). The axillary temperature was measured before transport and at arrival in the NICU/postnatal wards by the nursing officer.
Conductive thermal mattress
The EMBRACE™ warmer, based on a novel Phase Changing Material (PCM) is an easy-to-use, portable infant warmer that once charged, maintains a temperature of around 37 °C for at least 4 h. The PCM consists of paraffin-based material (melting point 37 °C, latent heat capacity ∼200 J/g) encased within a flattened medical-grade polyurethane pouch which serves as an external heat source. Individual PCM pouches are cleansed with soap and water or alcohol-based disinfectants between babies. There is no direct contact with the skin of the neonates, thus avoiding any risk of skin injury. It is intended for use as an infant warmer for clinically stable newborns from 1500 to 2500 g in the hospital, community or during transport.
Statistical analysis
Descriptive statistics were represented as number and percentage, mean and standard deviation (SD) or median and interquartile range (IQR) as appropriate. Chi-square test was used for categorical variables, Student's t-test for normally distributed continuous variables and Mann–Whitney test for non-normally distributed continuous variables. All the statistical analyses were carried out using Graph Pad Prism software (Graph Pad Software Inc. USA). A p value of <0.05 was considered statistically significant.
Results
The study was conducted from December 2016 to December 2018 with data for the historical controls collected from July 2015 to November 2016.
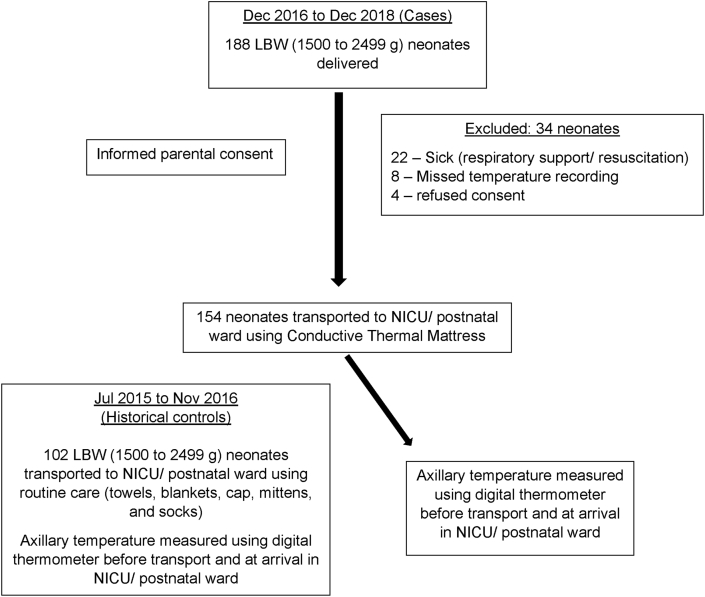
A total of 188 LBW (1500–2499 g) neonates were born during the period of the study. A total of 34 neonates were excluded, including 22 who required resuscitation/respiratory support, 8 who did not have the axillary temperature measured by the nursing officer due to oversight and 4 whose parents refused consent for the study. A total of 154 neonates were transported from the labour room/operation theatre to the NICU/postnatal wards using the conductive thermal mattress (Fig. 1).
Fig. 1.
Study flow diagram.
The data for the historical controls were collected from July 2015 to November 2016 by the principal investigator from the labour room and NICU/postnatal ward medical records. A total of 102 LBW (1500–2499 g) neonates were transported from the labour room/operation theatre to the NICU/postnatal wards using routine care (towels, blankets, caps, mittens and socks).
The baseline characteristics of the neonates were comparable (Table 1).
Table 1.
Baseline characteristics.
| Conductive thermal mattress group (n = 154) | Routine care group (n = 102) | P value | |
|---|---|---|---|
| Gestational age (wks); mean (SD) | 33.2 (1.6) | 33.6 (1.8) | 0.063 |
| Birthweight (g); mean (SD) | 2020 (264) | 2050 (248) | 0.36 |
| Intrauterine growth restriction (IUGR), n (%) | 52 (33.76) | 35 (34.31) | 1.00 |
| Gender, male; n (%) | 76 (49.35) | 43 (42.15) | 0.31 |
| Mode of delivery; n (%) | |||
| Vaginal | 53 (34.42) | 32 (31.38) | 0.71 |
| LSCS | 101 (65.58) | 70 (68.62) | 0.71 |
| Apgar Score; median (IQR) | |||
| 1 min | 8 (7,8) | 8 (7,8) | 1.00 |
| 5 min | 9 (8,9) | 9 (8,9) | 1.00 |
| Delivery room temperature (⁰C); mean (SD) | |||
| Vaginal (labour room) | 24.4 (0.8) | 24.6 (0.8) | 0.05 |
| LSCS (operation theatre) | 23.2 (0.9) | 23.4 (0.7) | 0.05 |
| Time of reaching postnatal ward (min); mean (SD) | 34 (12) | 36 (14) | 0.22 |
The mean (SD) labour room temperature in the conductive thermal mattress and routine care group was 24.4 (0.8) ⁰C and 24.6 (0.8) ⁰C, respectively. The mean (SD) operation theatre temperature in the conductive thermal mattress and routine care group was 23.2 (0.9) ⁰C and 23.4 (0.7) ⁰C, respectively.
The mean (SD) time of axillary temperature measurement in the NICU/postnatal wards in the conductive thermal mattress and routine care group was 34 (12) min and 36 (14) min, respectively.
The mean (SD) axillary temperature of neonates in the delivery room (labour room/operation theatre) in the conductive thermal mattress and routine care group was 36.3 (0.8)⁰C and 36.2 (0.6)⁰C, respectively, (p-value 0.28). The mean (SD) axillary temperature of the neonates at arrival in the NICU/postnatal wards in the conductive thermal mattress and routine care group was 36.6 (0.6)⁰C and 36.4 (0.5)⁰C, respectively, which was statistically significant (p-value 0.005) (Table 2).
Table 2.
Outcome measurements.
| Conductive thermal mattress group (n = 154) | Routine care group (n = 102) | P value | Relative risk (RR), 95% CI | Number needed to treat (NNT) | |
|---|---|---|---|---|---|
| Axillary temperature in the delivery room (labour room/operation theatre) ⁰C; mean (SD) | 36.3 (0.8) | 36.2 (0.6) | 0.28 | – | – |
| Axillary temperature in the NICU/postnatal ward ⁰C mean (SD) | 36.6 (0.6) | 36.4 (0.5) | 0.005 | – | – |
| Incidence of mild hypothermia ⁰C; n (%) | 18 (11.68) | 20 (19.60) | 1.00 | 0.59 (0.33,1.07) | 13 |
| Incidence of moderate hypothermia ⁰C; n (%) | 2 (1.29) | 6 (5.80) | 0.55 | 0.22 (0.04,1.07) | 22 |
Relative risk (RR): The ratio of the probability of neonatal hypothermia in the conductive thermal mattress group to the probability of neonatal hypothermia occurring in the routine care group.
Number needed to treat (NNT): The number of neonates that must be transported using conductive thermal mattress over a given period of time to prevent one adverse outcome (mild/moderate hypothermia).
The relative risk (RR, 95% CI) of mild hypothermia (temperature 36.0 °C to 36.4 °C) in the conductive thermal mattress versus the routine care group was 0.59 (0.33,1.07) with a number needed to treat (NNT) of 13. The relative risk (RR, 95% CI) of moderate hypothermia (temperature 32.0 °C to 35.9 °C) in the conductive thermal mattress versus the routine care group was 0.22 (0.04,1.07) with a NNT of 22, both of which were not statistically significant.
There was no occurrence of hyperthermia (core temperature > 37.5 °C) among any of the neonates in either the conductive thermal mattress or the routine care group during the study period. There was also no incidence of local skin injury with the use of the conductive thermal mattress.
Discussion
Our study shows that the use of conductive thermal mattress for transport of LBW (1500–2499 g) neonates led to an improvement in the admission temperature of neonates in the NICU/postnatal wards compared with routine care. Although the absolute difference between the two groups was only 0.2 °C, which may not be clinically meaningful, this could be due to the small sample size of the study and education/sensitization of the healthcare providers.
The LBW neonates in the study were born moderate/late preterm or term SGA and were transported after initial stabilization in the delivery room (labour room/operation theatre) by the nursing officers or ward sahayika to the NICU/postnatal wards. They were cared for in the NICU/postnatal ward by attention to thermoregulation, katori and spoon feeding, early skin-to-skin care and blood sugar monitoring as per unit protocols.
The majority of the previous studies using a self-heating sodium acetate gel mattress have been carried out among preterm (<32 weeks), VLBW (<1500 g) neonates and have shown a significant benefit in admission NICU temperatures and decreasing the incidence of hypothermia among these neonates.6, 7, 8, 9 The present study did not include this subset of neonates as there are standard guidelines for thermoregulation among these VLBW neonates and the challenge at many places is in successful and consistent implementation of the same.
Since 2012, the conductive thermal mattress (EMBRACE™) has been available as a portable, easy-to-use, external heat source for LBW neonates during transport and stabilization. A survey by Nimbalkar et al10 in Gujarat in 2014 showed widespread use by paediatricians. In a large multicentre trial by Bhat et al11, in 2015, the conductive thermal mattress was shown to be non-inferior to standard of care for thermoregulation of LBW neonates.
Our study showed a non-significant reduction in the incidence of mild and moderate hypothermia with the use of the conductive thermal mattress. The findings of our study are in contrast to a recent trial by Shabeer et al12, in 2018, who showed that the conductive thermal mattress significantly reduced the incidence and duration of hypothermia in neonates >1500 g as compared with standard of care or the use of plastic bags. Our results could be due to education and sensitization of the care providers to the dangers of neonatal hypothermia and improvement in care practices, as well as a small sample size.
The delivery room temperatures in the labour room and operation theatre was in the range recommended by WHO (23 °C to 25 °C) in the vast majority of cases.4 However, this remains a constant challenge for most hospitals if the air-conditioning is centrally controlled or an emergency delivery is conducted.
There was no occurrence of hyperthermia (core temperature > 37.5 °C) among any of the neonates using the conductive thermal mattress during the study period. Previous studies have reported this as a side effect and have advised caution in the use of the exothermic mattress as an external heat source.13
The strengths of our study include a representative sample with precise inclusion/exclusion criteria and robust methodology.
The limitations include a small sample size, no long term follow-up and an experimental study design with historical controls, due to logistic reasons.
Conclusion
Use of the conductive thermal mattress for transport of stable LBW (1500–2499 g) neonates showed a significant, although clinically small improvement in the admission temperature at NICU/postnatal ward as compared with routine care. There was also a trend (not statistically significant) towards reduction in the incidence of mild and moderate hypothermia at admission to the NICU/postnatal ward.
Disclosure of competing interest
The authors have none to declare.
Acknowledgements
(a) This article is based on Armed Forces Medical Research Committee Project No 4805/2016, granted and funded by the Office of the Directorate General Armed Forces Medical Services and Defence Research Development Organization, Government of India.
(b) The authors are grateful to the administration and staff of Command Hospital (Western Command), Chandimandir for their support in conduct of this study.
References
- 1.Kumar V., Shearer J.C., Kumar A., Darmstadt G.L. Neonatal hypothermia in low resource settings: a review. J Perinatol. 2009 Jun;29(6):401–412. doi: 10.1038/jp.2008.233. [DOI] [PubMed] [Google Scholar]
- 2.Lunze K., Bloom D.E., Jamison D.T., Hamer D.H. The global burden of neonatal hypothermia: systematic review of a major challenge for newborn survival. BMC Med. 2013 Jan 31;11:24. doi: 10.1186/1741-7015-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laptook A.R., Salhab W., Bhaskar B., Neonatal Research Network Admission temperature of low birth weight infants: predictors and associated morbidities. Pediatrics. 2007 Mar;119(3):643–649. doi: 10.1542/peds.2006-0943. [DOI] [PubMed] [Google Scholar]
- 4.Organization WH . World Health Organization; Geneva: 1997. Thermal Protection of the Newborn: A Practical Guide. [Google Scholar]
- 5.Perlman J.M., Wyllie J., Kattwinkel J., et al. Part 7: neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2015 Oct 20;132(16 Suppl 1):S204–S241. doi: 10.1161/CIR.0000000000000276. [DOI] [PubMed] [Google Scholar]
- 6.Almeida P.G., Chandley J., Davis J., Harrigan R.C. Use of the heated gel mattress and its impact on admission temperature of very low birth-weight infants. Adv Neonatal Care. 2009 Feb;9(1):34–39. doi: 10.1097/01.ANC.0000346094.28110.11. [DOI] [PubMed] [Google Scholar]
- 7.Ibrahim C.P.H., Yoxall C.W. Use of self-heating gel mattresses eliminates admission hypothermia in infants born below 28 weeks gestation. Eur J Pediatr. 2010 Jul;169(7):795–799. doi: 10.1007/s00431-009-1113-y. [DOI] [PubMed] [Google Scholar]
- 8.Singh A., Duckett J., Newton T., Watkinson M. Improving neonatal unit admission temperatures in preterm babies: exothermic mattresses, polythene bags or a traditional approach? J Perinatol. 2010 Jan;30(1):45–49. doi: 10.1038/jp.2009.94. [DOI] [PubMed] [Google Scholar]
- 9.Simon P., Dannaway D., Bright B., et al. Thermal defense of extremely low gestational age newborns during resuscitation: exothermic mattresses vs polyethylene wrap. J Perinatol. 2011 Jan;31(1):33–37. doi: 10.1038/jp.2010.56. [DOI] [PubMed] [Google Scholar]
- 10.Nimbalkar S., Patel H., Dongara A., Patel D.V., Bansal S. Usage of EMBRACE(TM) in Gujarat, India: survey of paediatricians. Adv Prev Med. 2014;2014:415301. doi: 10.1155/2014/415301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhat S.R., Meng N.F., Kumar K., Nagesh K.N., Kawale A., Bhutani V.K. Keeping babies warm: a non-inferiority trial of a conductive thermal mattress. Arch Dis Child Fetal Neonatal Ed. 2015 Jul;100(4):F309–F312. doi: 10.1136/archdischild-2014-306269. [DOI] [PubMed] [Google Scholar]
- 12.Shabeer M.P., Abiramalatha T., Devakirubai D., Rebekah G., Thomas N. Standard care with plastic bag or portable thermal nest to prevent hypothermia at birth: a three-armed randomized controlled trial. J Perinatol. 2018;38(10):1324–1330. doi: 10.1038/s41372-018-0169-9. [DOI] [PubMed] [Google Scholar]
- 13.McCarthy L.K., Molloy E.J., Twomey A.R., Murphy J.F.A., O'Donnell C.P.F. A randomized trial of exothermic mattresses for preterm newborns in polyethylene bags. Pediatrics. 2013 Jul;132(1):135–141. doi: 10.1542/peds.2013-0279. [DOI] [PubMed] [Google Scholar]