Abstract
Background
Verruca vulgaris is a viral infection with high recurrence rates and is very difficult to treat. It occurs due to the ability of the virus to evade immune recognition. This immune evasion by the human papillomavirus (HPV) can be circumvented by injecting HPV antigens subcutaneously and inducing inflammation and a systemic immune response. Falkner technique is an approved technique for the treatment of warts. In this observational study, we analyzed the recovery rate among patients undergoing this technique as part of their routine treatment. The aim of this study is to study the clinical outcome of Falkner's needling technique that is being used for the treatment of verruca vulgaris.
Methods
Under local anaesthesia, only a single wart was vertically punctured using a 26-gauge needle up till the subcutis multiple times till bleeding was observed. No treatment was done for other warts. Patients were advised not to take any anti-inflammatory medications for pain and were observed for responses after 1 week as well as 1 and 3 months.
Results
Of 41 patients included in this study, the total resolution of both the punctured and distant warts occurred in 28 patients (68.29%) and partial response in 7 patients (17.1%) by the end of 3 months. Interestingly, individual warts that were subjected to needling showed complete resolution in 35 patients (85.4%).
Conclusion
Falkner's needling method provides a high rate of complete resolution of multiple warts at both the needled and distant sites after a single treatment session of only a single lesion. This modality has a high cure rate, is easy to perform, requires minimal infrastructure support, is cost-effective, and can be undertaken at most peripheral settings with minimal training.
Keywords: Warts, Needling, Falkner's technique
Introduction
Warts are mucocutaneous infections caused by the human papillomavirus (HPV), with a variable prevalence across ages in school children, which varies from 0.84% to 24%.1 Despite a wide array of techniques described in the literature, no single technique is known to provide satisfactory remission of the disease. Surgical removal/cautery achieves a cure rate of 65–85%2 with a single sitting, but post-operative morbidity and scarring limits its usage, especially in multiple warts and warts over the feet. Cryotherapy provides a cure rate of about 44–92.5% after multiple sessions; however, a single session cure rate is 83.5%.3,4 Requirement of sophisticated equipment, cryogen, post-operative pain and hypopigmentation limits its usage. Salicylic acid is known to achieve cure in 75%2 of patients with the daily application, but hyperkeratotic warts, especially over the feet require frequent paring before application for better penetration, besides daily application carries risk of salicylism in children. Immunotherapy with modalities such as injection measles, mumps and rubella (MMR) vaccine, injection vitamin D, injection Mycobacterium indicus pranii, provide complete resolution in 30–87% of patients, but again require multiple sessions.5
Despite numerous available treatment modalities, frequent recurrences can be frustrating to patients and physicians alike. The recurrence rates range from 20% to 80% according to various studies.5, 6, 7 Despite a plethora of medical, surgical procedures and miscellaneous therapies like hypnotherapy, recurrences continue to be high, primarily due to failure to induce a natural immune response against the pathogen.
Viral infection–induced cell damage stimulates the production of cytotoxic T-cells, which destroys the virus-infected cells. However, owing to the inherent ability of the HPV to resist cell lysis, the antigens are never presented to the antigen-presenting cells, resulting in minimal or no immune activation. Furthermore, HPV uses T-suppressor cell anti-inflammatory mechanisms to inhibit immune responses.
This immune evasion by the HPV can be circumvented by iatrogenically inducing inflammation over the lesions or by injecting HPV antigens into the subcutaneous tissue to induce a systemic immune response.
Materials and methods
Falkner's needling technique is an approved modality for the treatment of warts. In this observational study, we analyzed the recovery rate among patients undergoing treatment of warts by this technique as part of routine treatment in the Dermatology OPD of a tertiary care hospital in Western Maharashtra. The sample size was calculated based on a similar study by Longhurst et al.7 Minimum required sample size was 37, with 95% confidence interval and 15% absolute error. Considering a dropout rate of 20%, a total of 47 patients were included in the study. However, 41 patients completed the study and hence outcome was analyzed accordingly.
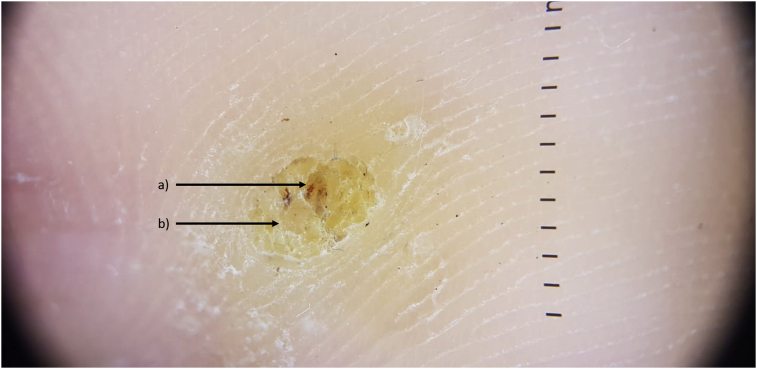
Verruca vulgaris was defined as single or multiple flesh-coloured firm papules over body showing verrucous surface not present since birth and gradually increasing in number in a nearby or distant location in the body since the acquisition of first such papule. The diagnosis was confirmed using dermoscopy (DermLite DL4) by the presence of thrombosed vessels and loss of dermatoglyphics (Fig. 1).
Fig. 1.
Dermoscopy of warts showing (a) thrombosed vessels and (b) loss of dermatoglyphics.
Inclusion and exclusion criteria
Patients of both sexes older than 12 years with a diagnosis of verruca vulgaris who reported to the Dermatology OPD during the 1-year study period were included in the study. A written informed consent was obtained from the patients/guardian. Pregnant, lactating mothers, immune-deficient individuals (including HIV) or those on immunosuppressants, those with keloidal tendency, bleeding diathesis or patients treated with any other modalities in the last 3 months were excluded from the study.
Examination protocol and study technique
After explaining the procedure and obtaining a written informed consent from the patient/guardian (in case of minor), a single sitting of Falkner's needling was performed on a single wart. No procedure was performed on any other warts.
The largest wart was chosen. Under strict aseptic precautions, the area was infiltrated with 2% lignocaine injection with an insulin syringe. The wart was repeatedly punctured using a 26-gauge disposable needle about 20–30 times depending on the size and location of the lesion, up to the level of subcutaneous tissue. The entry into the subcutaneous plane was characterized by a give-way sensation. The appearance of multiple pinpoint bleeding points over the wart was considered to be the end point (Fig. 2). A pressure dressing was applied over the site and the patient instructed to keep the dressing dry for 48 h. Patients were also advised not to take any anti-inflammatory medications though the use of tablet paracetamol was permitted in case of severe pain. A representative video clip of the procedure is also uploaded (Video 1).
Fig. 2.
Falkner's needling technique.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.mjafi.2020.07.009.
The following are the supplementary data related to this article:
Procedure of Falkner's technique.
Patients were reviewed at 3 follow-up visits at 1 week, as well as 1 and 3 months, during which patients were inspected for resolution of lesions or side-effects. The resolution in the number of warts was graded as follows: no response (0% resolution), minimal resolution (1–49% of lesions), near-total resolution (50–99% of lesions) and total response (100% resolution of lesions). Minimal resolution and near-total resolution were clubbed together under partial resolution for further analysis.
Alternative treatments were offered to patients in whom an incomplete resolution of warts occurred at the end of the follow-up period of 3 months.
Statistical analysis
Categorical variables were summarized by calculating proportions, and numerical variables were summarized by calculating median and inter-quartile range. The Mann–Whitney test was used to compare differences in numerical variables in two groups, whereas the Fisher's exact test was used to compare categorical variables. Two-tailed tests were used and p <0.05 was considered to be statistically significant. R software version 3.6.0 was used for the statistical analysis.
Results
Of the total of 47 patients who were included in the study, 41 patients completed the study successfully and the rest were lost to follow-up. In these 41 patients, 28 were men and 13 were women. The age group of the patients ranged from 12 to 68 years, with a median age of 26 years. The median duration of symptoms was 6 months, with range varying from 0.5 to 60 months. Feet were involved exclusively in 33 patients, followed by hands exclusively in 4 patients, whereas both hands and feet were involved in 3 patients. One patient had facial warts.
All 41 patients underwent needling and 28 patients (68.29%) achieved complete resolution of warts. Three patients had minimal resolution (<50%), 4 patients showed near-total resolution (50–99%), whereas 6 patients (14.6%) did not have any resolution of the wart (Table 1). Temporally, complete resolution appeared in 1 of 28 patients (3.6%) at 1 month of follow-up and 27 of 28 patients (96.4%) at 3 months of follow-up.
Table 1.
Resolution criteria.
| Category | Number (%) |
|---|---|
| No resolution | 6 (14.63%) |
| Minimal resolution (<50%) | 3 (7.32%) |
| Near-total resolution (50–99%) | 4 (9.76%) |
| Complete resolution | 28 (68.29%) |
| Total | 41 |
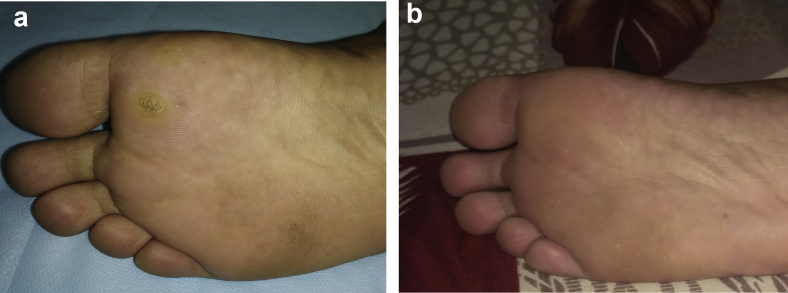
Inflammation around warts occurred 1 week after injection in 32 of 41 patients (78%). Among these 32 patients, total or partial resolution of warts was observed in 31 patients (96.8%). Of the 31 patients who responded, 24 patients had resolution of all warts, whereas 7 patients had a partial response. Despite inflammation, no resolution was observed in 1 of 31 patients (3.2%). Nine patients showed no sign of inflammation after needling, and only 4 patients (44.44%) in this group showed total or partial resolution (Table 2). There was a statistically significant association between inflammation at the needling site and resolution of warts (p < 0.001). Of the 31 patients who developed inflammation at the injected site, 20 had multiple warts (64.5%) and 11 patients had a single wart (35.5%). Complete resolution of the wart at the site of needling was observed in 35 of 41 patients (85.4%; Fig. 3, Fig. 4).
Table 2.
Inflammation at injection site and resolution of warts.
| Resolution present | Resolution absent | Total | |
|---|---|---|---|
| Inflammation present | 31 (96.88%) | 1 (3.12%) | 32 |
| Inflammation absent | 4 (44.44%) | 5 (55.56%) | 9 |
| Total | 35 | 6 | 41 |
Fisher test p < 0.001.
Fig. 3.
a) Plantar warts before the procedure. b) Plantar warts have resolved completely at 3 months after the procedure.
Fig. 4.
a) Facial warts before the procedure. b) Facial warts have resolved completely at 3 months after the procedure.
The age of the patients who showed resolution with the needling technique was lesser than patients who did not show the resolution (p = 0.046) (Table 3), although the duration of warts prior to treatment showed no such association (p = 0.31). No association was observed between the sex of the patient and resolution of warts (p = 0.361; Table 4) Resolution of warts was also not associated with the number of warts in a patient (p = 0.662; Table 5).
Table 3.
Association of age of the patient and duration of symptoms with resolution of warts.
| Age in years, median (IQR) | Duration of symptoms in months, median (IQR) | |
|---|---|---|
| Resolution Present | 26.0 (23.0–28.5) | 6 (2.0–6.25) |
| Resolution absent | 32.0 (26.0–48.0) | 6 (3.0–7.0) |
| p Value (Mann–Whitney test) | 0.046 | 0.319 |
Table 4.
Sex of the patient and resolution of warts.
| Resolution present | Resolution absent | Total | |
|---|---|---|---|
| Male | 25 (89.29%) | 3 (10.71%) | 28 |
| Female | 10 (76.92%) | 3 (23.08%) | 13 |
| Total | 35 | 6 | 41 |
Fisher test p = 0.361.
Table 5.
No. of warts and resolution.
| Resolution present | Resolution absent | Total | |
|---|---|---|---|
| Single wart | 13 (81.25%) | 3 (18.75%) | 16 |
| Multiple warts | 22 (88%) | 3 (12%) | 25 |
| Total | 35 | 6 | 41 |
Fisher test p = 0.662.
Minor pain with minimal swelling was the only side-effect in these patients, which lasted for a maximum of 2 weeks. None of the patients had fever or secondary bacterial infection.
Discussion
Human papillomavirus (HPV) is an extremely evolved virus having perfectly adapted to its mammalian host to reach a state of harmony to maintain its reproductive ability. It achieves this fine balance through sophisticated innate and acquired immune evasion methods tailor-made for the human immune system. The primary mechanism by which it achieves so is by avoidance of antigen presentation. The HPV undergoes its vegetative reproductive cycle in synchrony with the epithelial cells. By doing so it prevents the presentation of intra-virion components such as ds-DNA, non-structural proteins, thus evading the immune system. In turn, it spreads through shedding of the infected skin.8
Natural antibody formation occurs in only 30–50% of individuals, which is neither strong nor long-lasting.9,10 It is hypothesized that the capsid proteins are expressed only in the differentiated epithelial cells present in the superficial layers, leading to evasion of the immunogenic viral elements from the dermal blood supply.10 Apart from this, the E6 and E7 oncoproteins encode some specific functions to inhibit immune responses, for example, inhibition of IL-18–induced IFN-gamma production in human peripheral blood mononuclear and NK cells, inhibition of IL-8 and decreased expression of TLR-9.10
Many immunotherapeutic modalities are presently being used to circumvent this immune evasion. Firstly, boosting of non-specific immunity as is done by injection MMR, injection vitamin D, Bacillus Calmette–Guerin, injection Mycobacterium indicus pranii, and so on. These agents being highly antigenic generate robust cytokine [interleukin-2 (IL-2), interferon-γ (IFN-γ)] and T-cell responses.11
Secondly, by stimulating specific immune response by homologous implantation of viral components in the subcutaneous tissue.12, 13, 14, 15 Needling is one such way of homologous implantation of the virus first described by Falkner in the year 1969.16 It has the ease of achieving specific immunity with injections over only one site. It achieves this by attaining specific T-cell–mediated immunity towards the wart.
Inflammatory reaction is desirable at the site of the needling to promote the recruitment of T cells at the site of the infection, hence it is advised to avoid non-steroidal anti-inflammatory drugs post-operatively.6,17 This may result in increased morbidity in the form of pain and loss of work hours. In our study, this was circumvented by administering tablet Paracetamol 500 mg as on required basis. Paracetamol is a central analgesic acting through the COX-3 pathway and has minimal activity in peripheral inflammation, which acts through COX1/2 pathways.18 Non-specific inflammatory agents like diphencyprone have also been tried to induce delayed-type hypersensitivity reactions to haptens formed because of its application to warts.19
Autoinoculation achieves specific immunity to the wart and has a cure rate of about 34–75% according to various studies.12,15,20, 21, 22 In our study, complete resolution of the needled wart occurred in 35 of 41 patients (85.4%), whereas the complete resolution of multiple warts occurred in 16 of 24 patients (64%), which was comparable with autoinoculation. It is noteworthy that 23 of 25 patients (92%) with multiple warts showed complete/partial response after needling. The high cure rate in needling compared to autoinoculation can be attributed to local inflammatory response at the site of needled warts. Multiple warts are generally co-located at a defined anatomical location, hence inflammatory reaction in and around that region as with needling is more efficacious than distant implantation in autoinoculation. The flip side of autoinoculation is that it creates two surgical sites, one for excision and another for implantation, which leads to more morbidity in patients.
In our study, complete resolution was observed in 68.29% of patients and 17.1% of patients had a partial response. This corroborated well with the previous studies on Falkner's needling technique for warts. In a study done by Kumari et al on palmoplantar warts, resolution was observed in 70.7%, partial response in 6.1% and no response in 23.1% patients.16 Another study by Longhurst et al showed resolution in 69%, partial response in 7% and no response in 31% of the patients.7
Single session of cryotherapy done along with debulking of warts has a cure rate of 83.5%.4 Interestingly, our study showed complete resolution of the wart at the site of needling in 85.4% patients after a single session without the requirement of debulking. Falkner's needing is a minimalistic technique requiring minimal infrastructural support in comparison to cryotherapy that requires sophisticated equipment and liquid nitrogen. In addition, Falkner's needling technique not only treats the clinically apparent warts but also helps in treating subclinical lesions as against cryotherapy where only visible lesions can be treated, which can be safely presumed by the fact that the distant site warts also regressed after the procedure.
The resolution was observed in a significantly higher proportion of patients who had inflammation at the site of needling compared with those patients who did not have inflammation at the injection site (96.88% vs 44.44%). Inflammation at the site of injection and/or distant sites within 1 week of surgery was a good prognostic indicator of the outcome at the end of 3 months.
In our study, resolution of warts occurred in 76.9% of women as compared with 89% of men who underwent the procedure. Though this difference was not significant (p = 0.361), probably a study with a larger sample size may yield a significant difference. A possible explanation to this effect could be that the female sex steroids (oestrogen and progesterone) are linked with the development of Th2 responses as compared to male sex steroids (testosterone) that are linked with Th1 responses.23
Patients who did not show resolution after needling in our study had a significantly higher age than those who showed resolution. Increasing age is associated with diminished phagocytic activity of the dendritic cells and hence decreased antigen presentation. Therefore, the chances of success of the procedure is more likely in younger individuals.23
The cure rates achieved in this technique are better than those achieved by existing standard of care where multiple treatments may be required (surgical removal/cautery: 65–85%, chemical cautery: 43%, salicylic acid: 75%, cantharidin: 80%, cryotherapy: 92.5%, bleomycin: 16–94% and injection MMR: 74%).2
Advantage
This modality is easy to perform, requires minimal infrastructure support, is cost-effective, a single procedure results in a better outcome than the existing standard of care and can be undertaken at most peripheral settings such as rural primary health care facilities or for treatment of soldiers who are deployed in far-flung areas where expert dermatological care may not be easily available and referral is difficult because of inclement weather or terrain. In large warts where excision surgeries would lead to a large tissue defect, needling can be done before excision to reduce the size of the lesion. Other advantages of this method are the absence of scarring or any hazardous plumes as in the ablative modalities.
Limitations
The long time for clearance of warts (3 months in 60.8% of patients) is one downside of this technique in people who want rapid clearance of the warts. Initial pain at the site of injection with advise to avoid painkillers in these patients can be tricky. A study with a longer follow-up period would be required to understand recurrence rates post-procedure.
Further scope
Multiple sittings of needling, especially in those patients in whom there was a lack of inflammation after 1 week, can be tried. Interestingly, it was also noticed that the warts closer to the site of needling appeared to heal better (depending on their size) as compared with those that were distant, though this could not be quantified in the present study. Owing to the small number of patients with facial wart and palmar warts, it is difficult to comment on site-specific responses in the study. A further study in this regard would reveal more information about these observations.
Conclusion
Falkner's needling is an easy, economical and highly effective modality for the treatment of both single and multiple verrucae vulgaris.
What's new?
Falkner's needling technique provides a high cure rate of the needled wart in 87.8% of patients. The pain over the lesion post-procedure can be managed using the tablet Paracetamol without quenching the desirable local inflammatory response as against non-steroidal anti-inflammatory drugs. Inflammation at the site of needling at 1-week post-procedure is a good prognostic indicator of the outcome at the end of 3 months.
Ethical issues
Ethical clearance for this study was obtained from the institutional ethics committee. A written informed consent was obtained from the patients/guardian.
Disclosure of competing interest
All authors have none to declare.
References
- 1.Loo S.K., Tang W.Y. Warts(non-genital) BMJ Clin Evid2009. 2009:1710. [PMC free article] [PubMed] [Google Scholar]
- 2.Lipke M.M. An armamentarium of wart treatments. Clin Med Res. 2006 Dec 1;4:273–293. doi: 10.3121/cmr.4.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baumbach J.L., Sheth P.B. In: Comprehensive Dermatologic Drug Therapy. Wolverton S., editor. W. B. Saunders Company; Philadelphia, PA: 2001. Topical and intralesional antiviral agents; pp. 524–536. [Google Scholar]
- 4.Buckley D. Cryosurgery treatment of plantar warts. Ir Med J. 2000;93:140–143. [PubMed] [Google Scholar]
- 5.Thappa D.M., Chiramel M.J. Evolving role of immunotherapy in the treatment of refractory warts. Indian Dermatol Online J. 2016 Sep;7:364. doi: 10.4103/2229-5178.190487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gibbs S. Needling warts: are we any further forward? Br J Dermatol. 2017 Nov;177:1154–1155. doi: 10.1111/bjd.15977. [DOI] [PubMed] [Google Scholar]
- 7.Longhurst B., Bristow I. The treatment of verrucae pedis using Falknor's needling method: a review of 46 cases. J Clin Med. 2013 Jun;2:13–21. doi: 10.3390/jcm2020013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frazer I.H. Interaction of human papillomaviruses with the host immune system: a well evolved relationship. Virology. 2009 Feb 20;384:410–414. doi: 10.1016/j.virol.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Cubie H.A. Disease associated with human papillomavirus infection. Virol J. 2013;445:21–34. doi: 10.1016/j.virol.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 10.Lee S.J., Cho Y.S., Cho M.C., et al. Both E6 and E7 oncoproteins of human papillomavirus 16 inhibit IL-18-induced IFN-gamma production in human peripheral blood mononuclear and NK cells. J Immunol. 2001;167:497–504. doi: 10.4049/jimmunol.167.1.497. [DOI] [PubMed] [Google Scholar]
- 11.Singh S., Chouhan K., Gupta S. Intralesional immunotherapy with killed Mycobacterium indicus pranii vaccine for the treatment of extensive cutaneous warts. Indian J Dermatol, Venereology Leprology. 2014 Nov 1;80:509. doi: 10.4103/0378-6323.144145. [DOI] [PubMed] [Google Scholar]
- 12.Shivakumar V, Okade R, Rajkumar V. Autoimplantation therapy for multiple warts. Indian J Dermatol Venereol;75:593-595. [DOI] [PubMed]
- 13.Nischal KC, Sowmya CS, Swaroop MR, et al. A novel modification of the autoimplantation therapy for the treatment of multiple, recurrent and palmoplantar warts.J Cutan Aesthet Surg 2012;5:26-29. [DOI] [PMC free article] [PubMed]
- 14.Srivastava P.K., Bajaj A.K. Autowart injection therapy for recalcitrant warts. Indian J Dermatol. 2010;55:367–369. doi: 10.4103/0019-5154.74548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Das P., Sood A., Bhatnagar A., Verma R., Baveja S., Vashisht D. Clinical outcomes and recurrences after homologous autoimplantation therapy for warts: a prospective study. J Marine Medical Society. 2017 Jul 1;19:103. [Google Scholar]
- 16.Falknor G.W. Needling--a new technique in verruca therapy. J Am Podiatry Assoc. 1969 Feb;59:51. doi: 10.7547/87507315-59-2-51. [DOI] [PubMed] [Google Scholar]
- 17.Kumari P., Yadav D., Vijay A., et al. Falknor's needling method as a potential immunotherapy in palmo-plantar warts. Indian Journal of Dermatology, Venereology, and Leprology. 2019 Jan 1;85:129. doi: 10.4103/ijdvl.IJDVL_809_17. [DOI] [PubMed] [Google Scholar]
- 18.Chandrasekharan N.V., Dai H., Roos K.L., et al. COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression. Proc Natl Acad Sci Unit States Am. 2002 Oct 15;99:13926–13931. doi: 10.1073/pnas.162468699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vivier D. Recalcitrant viral warts treated by diphencyprone immunotherapy. Br J Dermatol. 1999 Aug;141:292–296. doi: 10.1046/j.1365-2133.1999.02978.x. [DOI] [PubMed] [Google Scholar]
- 20.Swaroop M.R., Sathyanarayana B.D., Vasudevan P., Kumari P., Raghavendra J. Evaluation of efficacy and safety of modified technique of auto wart implantation in the treatment of multiple, recurrent and recalcitrant warts. Indian J Clin Exp Dermatol. 2016;2:27–31. [Google Scholar]
- 21.Usman N., Udayashankar K., Subramanian S., Thyagarajan S.P. Autoimplantation technique in the treatment of anogenital warts: A clinico-immunological study. Int J STD AIDS. 1996;7:55–57. doi: 10.1258/0956462961917078. [DOI] [PubMed] [Google Scholar]
- 22.Gugle A.S., Jadhav V.M., Kote R.P., Deshmukh M.D., Vankawala D. Study of homologous autoimplantation therapy for treatment of multiple warts in patients attending the dermatology out patient department. MVP JMed Sci. 2015;2:110–117. [Google Scholar]
- 23.Giefing-Kröll C., Berger P., Lepperdinger G., Grubeck-Loebenstein B. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell. 2015 Jun;14:309–321. doi: 10.1111/acel.12326. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Procedure of Falkner's technique.