Abstract
Background
Effective postoperative analgesia after lower segment caesarean section (LSCS) is very important for early ambulation and early breast feeding and has a role to play in decreasing postpartum depression. Quadratus lumborum (QL) block, a fascial plane block, is gaining popularity for pain management in lower abdominal surgeries. The aim of the present study was to compare the ultrasound-guided (USG) transversus abdominis plane (TAP) block and QL block in patients undergoing LSCS under spinal anaesthesia.
Methods
Double-blinded, randomized, controlled, single-centre study done between Aug 2019 and Oct 2019, randomised 80 patients scheduled for LSCS into two groups, QL (N = 40) and TAP (N = 40), receiving USG TAP or QL block 20 ml of 0.25% bupivacaine with 4 mg dexamethasone bilaterally, postoperatively.
Results
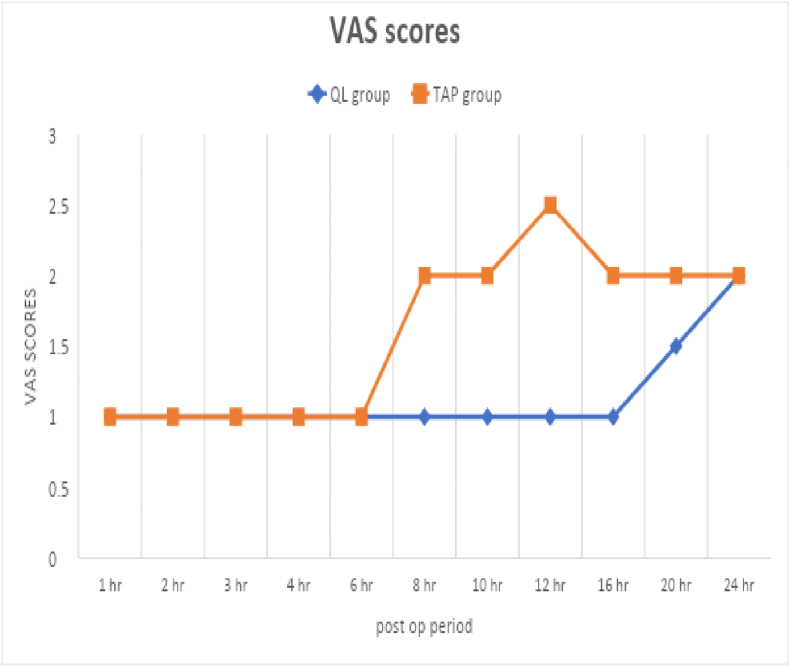
SSPS 20 was used for the statistical analysis Patients were evaluated for 24-h using visual analogue scale (VAS) for pain scores, time to rescue analgesia and the analgesic dose requirement at regular time intervals. Fifteen percent patients in QL block and 75% in TAP block required rescue analgesia (P < 0.001). Significant differences were observed in pain scores at 10 h postoperatively, VAS in QL=1.18 (0.55), TAP=3.08 (1.66) (P < 0.001). By 24 h postoperatively the difference ceased to be statistically significant. Time to rescue analgesia in QL group was 1353 min (+/−224.07) and TAP group 915 min (+/−391.62) (P < 0.001). Average requirement of rescue analgesia (paracetamol) in QL group was 153.84 mg, TAP group 756.09 mg.
Conclusions
Patients receiving QL block had prolonged analgesic effects and required less use of rescue analgesia in comparison with TAP group in the first 24 h postoperatively.
Trial number
CTRI/2019/07/020475.
Keywords: Quadratus lumborum block, Transverse abdominis plane block, Lower segment caesarean sections
Introduction
Caesarean delivery is associated with severe postoperative pain hampering early mobilisation, early breast feeding and emotional bonding with the new born. Multimodal pain therapy (regional anaesthesia blocks, paracetamol, opioids, NSAIDs) is required to control postoperative pain in caesarean delivery. Several regional blocks have been described to control postoperative pain like transversus abdominis plane (TAP) block, ilioinguinal and iliohypogastric nerve block, quadratus lumborum (QL) block, etc. Over the last 2 years, we have been practicing TAP block for providing postoperative analgesia to our lower segment caesarean section (LSCS) patients. However, the duration of analgesia was not very prolonged, and patients needed additional analgesia after 8–10 h. QL block has gained popularity in recent times as an effective method of providing postoperative analgesia in lower abdominal surgeries. There are few studies comparing the block efficacy with other modalities, and we wished to compare QL with TAP block in search for a more prolonged and better analgesia for our LSCS patients.
We performed USGQL block and USGTAP block in two groups and compared analgesic effect of both regional blocks in terms of pain-free duration and requirement of rescue analgesia. All caesarean surgeries were performed under sub-arachnoid block. We have used dexamethasone as additive to local anaesthetic drugs to extend the effect of regional blocks1,2.
Aim of the study
Aim of this study was to compare the effect of USGQL block versus TAP block for postoperative analgesia in caesarean delivery under spinal anaesthesia.
Sample size calculation
The sample size was calculated based on study of Yousef3 with α error 0.05 and power 80% and found to be 36 in each group. We have included 40 patients in each group.
Randomization
A close envelope method was used for randomization. Eighty sealed envelopes were prepared with the name of technique (40 TAP blocks and 40 QL blocks), and each patient was asked to choose one of the envelopes. These 80 patients were randomly allocated into two groups.
-
(A)
TAP block group (40 patients): Each patient received sub-arachnoid block for caesarean section followed by USGTAP block at the end of the surgery.
-
(B)
QL block group (40 patients): Each patient received sub-arachnoid block for caesarean followed by USGQL block at the end of the surgery.
Inclusion criteria
All female patients of age group 20–35 years with American Society of Anaesthesiologists (ASA) Physical status class I and class II, scheduled for LSCS were included in the study.
Exclusion criteria
Patients who had infection at injection site, refusal for procedures, allergic to local anaesthetic drugs, diabetes, coagulation disorder with INR more than 1.5 and ASA class III and class IV were excluded from this study.
Materials and Methods
This randomised controlled double-blinded trial was undertaken after approval of the Institutional Ethical Committee and obtaining written informed consent from all the subjects. The study was registered with CTRI. All patients were evaluated clinically with relevant laboratory investigations during preanaesthetic evaluation and reassessed during preoperative visit. All patients were received in preop room on the day of surgery, 18G/20G intravenous cannula was inserted, and every patient received co-loading with 500 ml of ringer lactate. After shifting to OT, baseline vital parameters were recorded before surgery, and sub-arachnoid block was performed with 2.2 ml of 0.5% bupivacaine (heavy) using 26 gauge Sprotte needle. As part of the protocol, all patients received Inj. paracetamol 1 gm intravenous over 10-min intra-operatively, and diclofenac suppository 100 mg immediately after surgery. Out of 80 patients, 40 received USG QL block, and the rest 40 patients received USG TAP block randomly. Both blocks were performed under strict aseptic precautions with 6–13 MHz linear probe (Edge Ultrasound System Sonosite Inc. Bothell WA, USA).
Transversus abdominis plane block (Fig. 1)
Fig. 1.
Transversus abdominis plane block – A picture showing the needle approaching the plane between the internal oblique and transversus abdominis muscle.
With the patient in supine position, the transducer was placed transversely in the anterior axillary line between the thoracic cage and iliac crest at the level of umbilicus, a clear view of the three layers of abdominal wall was obtained and the needle inserted in plane, directed medial to lateral. After negative aspiration 20 ml of 0.25% of bupivacaine with 4 mg dexamethasone was injected in the plane between internal oblique and transversus abdominis muscle, on each side looking for the typical spread of the drug, referred to as the Kayak Sign.
Quadratus lumborum block (Fig. 2)
Fig. 2.
Quadratus lumborum (QL) block showing the needle being advanced in the plane where transversalis fascia is merging with the fascia over quadratus lumborum. Note the hook sign.
With the patient in supine position, US probe was placed at the level of anterior superior iliac spine and moved cranially until all the three layers of abdominal wall muscles were identified. The external oblique muscle was followed till visualization of posterior border of muscle (hook sign). Drug was injected below the hook sign at the point where the transversalis fascia merged with the fascia over QL muscle. We injected 20 ml of 0.25% of bupivacaine with 4 mg dexamethasone on each side for QL block after negative aspiration.
All patients were evaluated for postoperative pain relief for the next 24 h. Visual analogue scale (VAS) was used for assessment of postoperative pain. Patients were assessed for pain at 2 h, 4 h, 6 h, 8 h, 10 h, 12 h, 16 h, 18 h, 20 h and 24 h. If patient had VAS > 4, Inj. paracetamol 1 gm was given intravenously as a rescue analgesia. The time to first rescue analgesia was noted by a blinded observer. The total dose of rescue analgesia was also documented in each patient for the first 24 h. In those patients in whom paracetamol did not provide adequate pain relief, Inj. tramadol 2 mg/kg up to 100 mg was used.
Results
Data were expressed as mean ± standard deviation, frequency and percentage. Statistical package for the Social Sciences version 20 (IBM, USA) was used for statistical analysis. Quantitative data were analysed by using independent sample t-test. Qualitative data were analysed by using independent sample median test and Chi–square test. P < 0.05 was considered to be statistically significant.
The study included 80 patients (40 patients in each group) (Fig. 3 Consort chart).
Fig. 3.
Consort diagram.
Mean age in QL group was 27.15 years (+/−4.26) and in TAP group it was 27.23 years (+/−3.63). The distribution of ASA I and II in QL group was 5% and 95%, respectively, and in TAP group it was 15% and 85%, respectively. There was also no significant difference in the operative time between the two groups. Our baseline analysis revealed that there was no statistically significant difference between the two groups regarding age, ASA status and operative time (Table 1). The indication for LSCS has been tabulated in (Table 2) and grouped into emergency and elective LSCS. There was no statistically significant difference between the two groups as regards elective and emergency cases.
Table 1.
QL – quadratus lumborum and TAP – transversus abdominis plane.
| Variable | GROUP QL (Total = 40) | GROUP TAP (Total = 40) | P value |
|---|---|---|---|
| Age in years, mean (SD) | 27.15 (4.258) | 27.23 (3.627) | 0.933 |
| Duration of surgery (min) | 48 ± 5 | 50 ± 5 | |
| ASA n (%) | 0.263 | ||
| I | 2 (5) | 06 (15) | |
| II | 38 (95) | 34 (85) | |
Table 2.
Indications for lower segment caesarean section (LSCS) in both groups. IVF – in vitro fertilisation, IUGR – intrauterine growth retardation, QL – quadratus lumborum, TAP – transversus abdominis plane.
| QL GROUP (40 cases) | TAP GROUP (40 cases) | ||
|---|---|---|---|
| Elective 21 (52.5%) | Emergency19 (47.5%) | Elective22 (55%) | Emergency18 (45%) |
| Post LSCS 18 (45%) | Non-progress of labour 07 (17.5%) | Post LSCS 17 (42.5%) | Non-progress of labour 08 (20%) |
| Post datism 01 (2.5%) | Cephalopelvic disproportion 02 (5%) | Post IVF 01 (2.5%) | Foetal distress 03 (7.5%) |
| Post IVF 02 (5%) | Oligohydramnios 01 (2.5%) | Twins with gestational diabetes mellitus 01 (2.5%) | Polyhydramnios 01 (2.5%) |
| Macrosomia 01 (2.5%) | Gestational diabetes mellitus 01 (2.5%) | Meconium-stained liquor 02 (5%) | |
| Gestational diabetes mellitus 02 (5%) | Premature rupture of membranes with IUGR 02 (5%) | Placenta previa 01 (2.5%) | |
| Pregnancy-induced hypertension 02 (5%) | Breech 01 (2.5%) | ||
| Prematurely rupture of membranes with high head 01 (2.5%) | Premature rupture of membranes 01 (2.5%) | ||
| Breech 03 (7.5%) | Pregnancy-induced hypertension 01 (2.5%) | ||
The time to rescue analgesia was the primary measurement objective, and our study showed that for Group QL patients, it was 1353 min (+/−224.07 min), whereas for TAP group it was 915 min (+/−391.62 min). This difference was highly significant with P value 0.001.
The study also tried to find out as to what percentage of patients required rescue analgesia. It was seen that 6 out of 40 in Group QL (15%), and 34 out of 40 patients in Group TAP (75%) required rescue analgesia. The difference was found to be statistically significant with P value 0.001 (Table 3). The average requirement of rescue analgesia Inj. paracetamol was less in QL group compared with TAP group (153.84 mg/756.09 mg).
Table 3.
QL – quadratus lumborum and TAP – transversus abdominis plane.
| Variable | GROUP QL | GROUP TAP | P value |
|---|---|---|---|
| Time to rescue analgesia (min), mean (SD) | 1353 (224.07) | 915 (391.62) | 0.000 |
| Rescue analgesia n (%) | 6 | 31 (77) | 0.001 |
| Average requirement of rescue analgesia (paracetamol in mg) | 153.84 | 756.09 |
For each time period independently, the postop pain VAS scores were tested using nonparametric median test. By 2 h postop interval, no statistical difference was seen inthe pain scores in the two groups (P > 0.05). However, 6 h postoperatively, significant difference was observed in the two groups; VAS pain scores with maximum difference noted at 10 h (QL 1.18(0.55) and TAP 3.08(1.66), (P < 0.05) till 20 h postop. The VAS scores were comparatively lesser in QL group compared with TAP group (Fig. 4 and Table 4). By 24 h postoperatively, the difference ceased to be statistically significant.
Fig. 4.
The VAS scores start rising 6 hrs post surgery in TAP group whereas in QL group the rise was noted at 16 h. by 24 h there was no difference between the VAS scores in both groups.
Table 4.
QL – quadratus lumborum, TAP – transversus abdominis plane and VAS – visual analog scale.
| Post Op Period (Hrs) | GROUP QL (VAS scores) |
GROUP TAP (VAS scores) |
P value | ||
|---|---|---|---|---|---|
| Mean (SD) | Median | Mean (SD) | Median | ||
| 1 | 1 (0.00) | 1 | 1.05 (0.22) | 1 | 0.474 |
| 2 | 1 (0.00) | 1 | 1.13 (0.52) | 1 | 0.239 |
| 3 | 1 (0.00) | 1 | 1.60 (2.20) | 1 | 0.034 |
| 4 | 1 (0.00) | 1 | 1.10 (0.30) | 1 | 0.124 |
| 6 | 1 (0.00) | 1 | 1.75 (1.03) | 1 | 0.000 |
| 8 | 1.05 (0.22) | 1 | 2.65 (1.72) | 2 | 0.000 |
| 10 | 1.18 (0.55) | 1 | 3.08 (1.66) | 2 | 0.000 |
| 12 | 1.65(1.35) | 1 | 2.95 (1.41) | 2.5 | 0.001 |
| 16 | 1.68 (1.27) | 1 | 2.70 (1.14) | 2 | 0.003 |
| 20 | 1.68 (0.86) | 1.5 | 2.40 (1.23) | 2 | 0.005 |
| 24 | 1.90 (1.17) | 2 | 2.10(1.36) | 2 | 0.585 |
Discussion
Postoperative analgesia in LSCS is challenging because of various reasons, including patients cultural background and expectations. Wound hyperalgesia is a known risk factor for developing chronic postsurgical pain.5,6
Intrathecal opioids, commonly morphine and fentanyl, are widely used for postoperative analgesia in Europe and North America.7 A recent review article in the Indian Journal of Anaesthesia, mentions that intrathecal opioids still remain the gold standard, but troublesome side effects have led to a search for ideal postoperative analgesia modalities and use of non-opioid methods for pain relief following LSCS.8 Another study conducted in Indian patients comparing morphine and fentanyl additives in spinal anaesthesia found morphine to be superior as an analgesic but with higher incidence of side effects although the difference was not statistically significant.9 The search continues for the ideal analgesia regimen which will have reduced side effects and extended duration of action.
There are many varieties of abdominal wall blocks available as part of multimodal analgesia, with different effects, such as paravertebral block, TAP block, rectus sheath block and QL block.9, 10, 11 Several studies showed TAP block to be effective as part of multimodal analgesic technique in the postoperative period in cases of caesarean sections.12,13 TAP block was first described by Rafi as an approach via the lumbar triangle by using a blunt needle and the ‘pop’ method14 and Hebbard et al introduced the USG technique in 2007.15 With increasing use of US in the performance of blocks, the technique became easier and frequently performed. However, in a constant search for the ideal fascial plane block providing prolonged pain relief, QL block came up as an alternative. It was first described by Blanco as a TAP block under USG, as a ‘no pops’ technique.16
Mankikar et al found that bilateral TAP block with ropivacaine in patients undergoing caesarean section under spinal anaesthesia, prolonged the time to rescue analgesia (9.53 h) compared with the control saline group.17 Neeraj et al in an RCT evaluated the analgesic efficacy of TAP block in patients undergoing open appendicectomy and found VAS scores significantly reduced immediate post-surgery and at 24 h with P < 0.001.18 In our study, the mean time to rescue analgesia in TAP group was 15.25 h with a SD of 6.52 h. We found a more prolonged analgesia with TAP probably because of dexamethasone that was used as additive. In 9 out of 40 patients in TAP group, the VAS noted at 24 h did not go beyond 3.
QL block is a relatively easy technique and gaining popularity as part of multimodal analgesia. This is more so as it can be practiced in all age groups and in various studies till date has proven to have a good safety profile. The analgesic effect of QL block is due to thoracolumbar fascia (TLF). TLF connects the lumbar paravertebral region with anterolateral abdominal wall. It is suggested that the analgesic effect is due to spread of the local anaesthetics along the TLF and the endothoracic fascia into the paravertebral space.19,21,22
Two recent RCTs (Yousef and Verma et al)3,20 have compared the effect of QL versus TAP block in total abdominal hysterectomy and LSCS, respectively. Yousef NK found that there was significantly less opioid consumption in the QL group compared with TAP group; duration of postoperative analgesia was prolonged in QL group and VAS score was higher in TAP group. Verma et al. found that there was significantly less analgesic demand (p < 0.001) of up to 72 h postoperatively in the QL group in patients undergoing LSCS. Our results were similar with those recorded by Blanco et al,12 and Yousef. We studied the results only up to 24 h postoperatively and found that by 24 h, the VAS scores ceased to be statistically significant. This is at a variance with the study by Verma et al, and the prolonged effect noticed by them might be explained by the more posterior approach to QL block used in their study.
Our results showed overall rescue analgesia given in the postoperative period was significantly less in QL group, which also indicates the prolonged duration of block effect. In our study, three patients in the TAP group continued to have pain scores more than 4 even after administering paracetamol and in these patients, injection tramadol 75 mg intravenously was used to alleviate pain, which was administered 45 min after paracetamol injection. No patients in the QL group required tramadol injection.
QL I block is technically not difficult to perform as we approach from anterolateral aspect of the abdomen. QL block does not aim to target a nerve, but it is a fascial plane block, which is identified as bright, hyperechoic and easily dissectible plane block. It has a good safety profile as does TAP block and has very rare chances of injury to any vital structures.
Three recent review articles4,21,22, have explored the anatomical concepts, mechanisms and techniques of QL blocks and commented favourably with regard to the duration and quality of analgesia in comparison with TAP block. Based on the available clinical material, they report a wider sensory blockade when performed using similar volumes of local anaesthetics compared with TAP block. They did not find any studies reporting complications after QL block. They suggest arriving at a consensus regarding the use of each type of QL block for a particular type of surgery.
Use of local anaesthetic with additive, that is, dexamethasone increased the duration of analgesic effects in the postoperative period, which was similar to findings studied earlier.23
Limitations
In the present study, we did not assess the postoperative dermatomal levels of block as part of our measurements. We also did not study pain scores in emergency LSCS and planned LSCS cases separately. There was no statistically significant difference in the type of cases in the two groups, but it will be interesting to find out if there is a difference in pain scores between the emergency and elective cases and may form a basis for another study in future. We did assess the VAS at rest and at movement but did not record them separately but only recorded the highest VAS at the assigned hour. It would be interesting to compare the two and record the findings.
Conclusion
This study comparing TAP and QL block, as a part of multimodal analgesia in patients undergoing LSCS showed both techniques to be effective. However, the duration of effect was more prolonged, and VAS scores were lower with QL block. The safety profile of both blocks and patient satisfaction was comparable.
The approach for QL block used in our study is easy and safe, with good visualisation and the ability to track the needle thereby preventing any damage to adjacent viscera. Proper implementation of the technique can significantly decrease opioid use after caesarean sections, improve bonding with the baby and promote early mobilisation, and the block has already become an integral part of multimodal analgesia after lower abdominal surgeries at our centre.
Declaration of competing interest
The authors have none to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mjafi.2020.10.009.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Br J Anaesth. March 2014;112(3):427–439. doi: 10.1093/bja/aet417. [DOI] [PubMed] [Google Scholar]
- 2.Gordon K.G., Choi S., Rodseth R.N. The role of dexamethasone inperipheral and neuraxial nerve blocks for the management ofacute pain. South Afr J Anaesth Analg. 2016;22(6):163–169. [Google Scholar]
- 3.Yousef N.K. Quadratus Lumborum Block versus Transverse Abdominis Plane Block in patients undergoing total abdominal hysterectomy: A randomized prospective controlled trial. Anesth Essays Res. 2018;12:742–747. doi: 10.4103/aer.AER_108_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ueshima H., Otake H., Lin ja. Ultrasound guided quadratuslumborum block: an updated review of anatomy andtechnique. BioMed Res Int. 2017;2017:2752876. doi: 10.1155/2017/2752876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kehlet H., Jensen T.S., Woolf C.J. Persistent postsurgical pain: riskfactors and prevention. Lancet. 2006;367:1618–1625. doi: 10.1016/S0140-6736(06)68700-X. [DOI] [PubMed] [Google Scholar]
- 6.Nikolajsen L., Jensen T.S., Kehlet H. Chronic pain following caesarean section. Acta Anaesthesiol Scand. 2004;48:111–116. doi: 10.1111/j.1399-6576.2004.00271.x. [DOI] [PubMed] [Google Scholar]
- 7.Nakamura Takako, Hase Kokichi, Fujihara Toru, et al. Combined intrathecal morphine and bupivacaine for elective post caesarian pain. Masui. 2009 Apr;58(4):416–421. [PubMed] [Google Scholar]
- 8.Kerai S., Saxena K.N., Taneja B. Post caesarian analgesia: whatis new? Indian J Anaesth. 2017;61:200–214. doi: 10.4103/ija.IJA_313_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta A., Chatterji R., Choudhary H., Chatterji C.S. Comparisonof intrathecal morphine and fentanyl in addition toropivacaine for perioperative analgesia in lower segment caesarian section. Ind J Pain. 2018;32:91–95. [Google Scholar]
- 10.Murouchi T., Iwasaki S., Yamakage M. Chronological changesin ropivacaine concentration and analgesic effects between Transverse Abdominis block and Rectus Sheath block. RegAnesth Pain Med. 2015;40:568–571. doi: 10.1097/AAP.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 11.Stoving K., Rothe C., Rosenstock C.V., et al. Cutaneous sensory block area, muscle relaxing effect, and block duration of Transverse Abdominis block: a randomized, blinded, and placebo controlled study in healthy volunteers. Reg AnesthPain Med. 2015;40:355–362. doi: 10.1097/AAP.0000000000000252. [DOI] [PubMed] [Google Scholar]
- 12.Blanco R., Ansari T., Girgis E. Quadratus Lumborum Block for postoperative pain after Caesarean Section: a randomized controlled trial. Eur J Anaesthesiol. 2015;32:812–818. doi: 10.1097/EJA.0000000000000299. [DOI] [PubMed] [Google Scholar]
- 13.McDonell J.G., Curley J., John Carney, et al. The analgesic efficacy of Transverse Abdominis Plane block after caesarean delivery: arandomized controlled study Anaesth. Analgesia. 2008;106:186–191. doi: 10.1213/01.ane.0000290294.64090.f3. [DOI] [PubMed] [Google Scholar]
- 14.Rafi A.N. Abdominal Field Block: a new approach via thelumbar triangle. Anaesthesia. 2001 Oct;56(10):1024–1026. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 15.Hebbard P., Fujiwara Y., Shibata Y., Royse C. Ultrasound guided transversus abdominis plane (TAP) block. Anaesth IntensiveCare. 2007;35:616–617. [PubMed] [Google Scholar]
- 16.Blanco R. TAP block under ultrasound guidance: thedescription of a ‘no pops’ technique. 271. Reg Anesth Pain Med. 2007;32:S130. [Google Scholar]
- 17.Gajanan Mankikar Maitreyi, Pravin Sardesai Shalini, Sachin Ghodki Poonam. Ultrasound guided Transversus Abdominis Plane block for postoperative analgesia in patients undergoing Caesarian Section. Indian J Anaesth. 2016;60:253–257. doi: 10.4103/0019-5049.179451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neeraj G., Searle A., Mathews M., et al. Analgesicefficacy of ultrasound guided Transversus Abdominis Planeblock in patients undergoing open appendicectomy. Br JAnaesth. 2009;103(4):601–605. doi: 10.1093/bja/aep175. [DOI] [PubMed] [Google Scholar]
- 19.Ueshima H., Otake H., Lin J.A. Ultrasound guided quadratuslumborum block: an updated review of anatomy andtechniques. BioMed Res Int. 2017;2017:7. doi: 10.1155/2017/2752876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Verma K., Malawat A., Jethava D., Jethava D.D. Comparison oftransversus abdominis plane block and quadratus lumborum block for post caesarian section analgesia: a randomisedclinical trial. Indian J Anaesth. 2019;63:820–826. doi: 10.4103/ija.IJA_61_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hesham Elsharkawy. Quadratus lumborum blocks. AdvAnaesth. 2017;35:145–147. doi: 10.1016/j.aan.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 22.Hesham Elsharkawy, Kariem El-Boghdady, Michael Barrington. Quadratus lumborum blocks, anatomicalconcepts, mechanisms and techniques. Anaesthesiology. 2019;130:322–335. doi: 10.1097/ALN.0000000000002524. [DOI] [PubMed] [Google Scholar]
- 23.Amany S.A., Mahmoud Khaled M. Effect of adding dexamethasone to bupivacaine on transversus abdominis plane block for abdominal hysterectomy: a prospective randomized controlled trial Saudi. J Anaesth. 2012 Jul-Sep;6(3):229–233. doi: 10.4103/1658-354X.101213. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.