Abstract
Purpose
This study compares the functional results and survivorship of unicompartmental knee arthroplasty (UKA) and high tibial osteotomy (HTO) with an external fixator for medial compartment osteoarthritis (OA) of the knee.
Methods
Two cohorts of patients aged less than 60 years who had undergone either a cemented medial mobile-bearing UKA or an HTO with an external fixator were included in the study. The first cohort included patients undergoing a series of 197 consecutive medial UKA procedures (UKA group). The second cohort consisted of 60 consecutive patients undergoing HTO with an external fixator (HTO group). Each patient was assessed based on the Oxford Knee Score (OKS), the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the Subjective International Knee Documentation Committee (IKDC) score/questionnaire. A clinical evaluation was conducted on the day of the surgery (T0) and at the follow-up visit (T1) (minimum follow-up time was 60 months). Complications and failures resulting from the surgery were recorded for each patient.
Results
Only the age of the patients at the pre-operative time differed significantly between the two groups, with the HTO group being significantly younger (47.7 ± 8.0 versus 55.8 ± 2.2).
After the final follow-up visit, all scores improved in both groups (p < 0.05).
IKDC and Oxford scores were higher for the UKA group (p < 0.05). In the HTO group, three complications occurred (5%), including two superficial infections and one deep infection. On the other hand, the UKA group reported four complications (2%): three aseptic mobilisations and one infection requiring revision surgery. There was no difference in the complication rate between the two groups (p = 0.208).
Conclusions
In young patients (<60 years) with an isolated medial knee OA, both HTO and UKA led to good to excellent clinical results with a low rate of complications at mid-term follow-up; both surgical procedures may be considered in this patient population.
Level of evidence
Level III.
Keywords: High tibial osteotomy, Unicompartmental knee arthroplasty, Medial knee osteoarthritis, IKDC, Oxford knee score
1. Introduction
Isolated medial compartment osteoarthritis (OA) is a common condition affecting 85% of the patients with OA of the knee.1 In the case of medial compartment OA, the mechanical axis passes through the medial compartment and manifests with varus deformity.1 Both unicompartmental knee arthroplasty (UKA) and high tibial osteotomy (HTO) are two of the most common surgical treatments for OA of in varus knee.2, 3, 4
The principle of HTO is to change the load from the medial compartment to the lateral compartment and correct the alignment and varus deformity. HTO has a better indication when the varus deformity is metaphyseal.2 The different types of HTO techniques are medial opening wedge osteotomy with a plate, medial hemicallotasis with a fixator and lateral closing wedge osteotomy with a plate and staple fixation.5
The principle of UKA is to correct intraarticular deformity due to cartilage damage. A UKA is indicated when the patient has a flexion deformity of at less than 10° degrees, a varus deformity of less than 15° degrees and a low functional level.6,7
Contraindications to HTO and UKA are opposite compartment involvement, inflammatory arthritis and a flexion deformity greater than 10–15°.8,9 The present study aims to evaluate and compare the functional outcomes and survival rates of UKA and HTO with an external fixator for medial compartment OA.
2. Material and methods
The study was carried out in accordance with The Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines, and every participant provided informed consent.10
The local ethics commission provided the required ethical authorization.
Two prospective cohorts of patients younger than 60 years who had undergone either a cemented medial mobile-bearing UKA or an HTO with an external fixator were included in the study.
UKAs were performed in a specialized orthopaedic hospital in Italy (IRCCS Istituto Ortopedico Galeazzi, Milan), while HTO were performed in India in an Hopsital specialized in deformity correction and knee reconstruction (Mangal Ananad Hospital, Swastik park Chembur East, Mumbai).
The first group consisted of 197 consecutive patients (197 knees) who underwent minimally invasive mobile-bearing medial UKA (Zimmer-Biomet, Warsaw, Indiana, USA).
The second cohort consisted of 60 consecutive patients undergoing HTO with an external fixator (HTO group). The fixator was chosen because good-quality regeneration form at the osteotomy site. The fixator is removed after the healing of the osteotomy to prevent hardware-related complications. The UKA patient is from Italian tertiary care hospital and HTO patient is indian tertiary care hospital. Two senior surgeons with considerable experience in performing UKA and HTO performed all the surgeries in respective group.11,12
In both groups, surgical procedures were performed to treat isolated anteromedial OA where the Kellgren-Lawrence grade was 3.13 Clinical examinations conducted prior to surgery and magnetic resonance imaging (MRI) verified that all ligaments were healthy. Exclusion criteria were: (1) lack of data, (2) revision surgery, (3) previous surgical procedure of the interested knee (except arthroscopy for meniscal treatment [meniscectomy or meniscal suture]), (4) varus/valgus instability, (5) flexion <90°, (6) flexion deformity >10° and (7) follow-up < 60 months (8) Varus >15°.
2.1. Surgical technique
2.1.1. HTO with external fixator
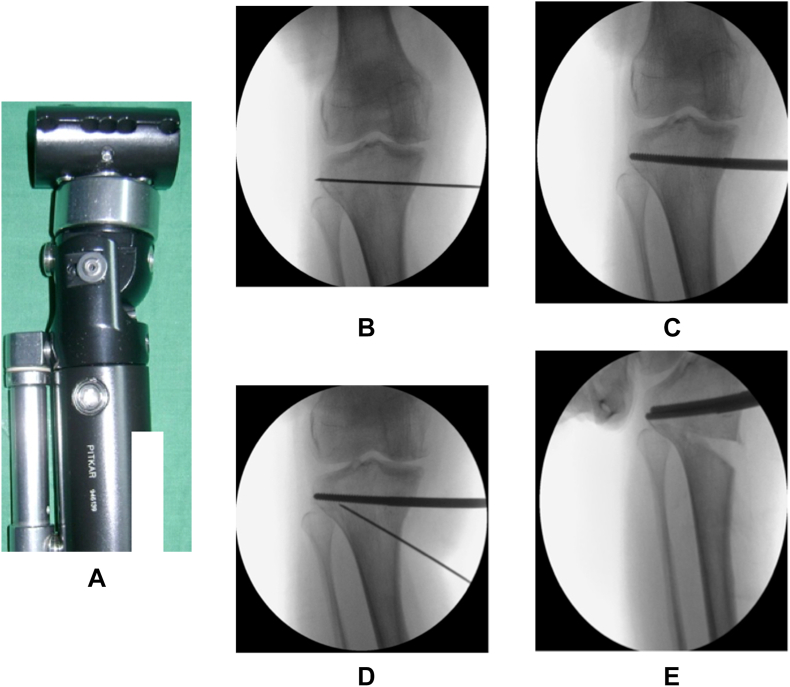
A senior surgeon in a supine position performed HTO without a tourniquet. The fixator (Dynamicfixator by S.H.Pitkar [Fig. 1A]) was applied on the anteromedial side of the limb. The guide wire was passed 2 cm underneath and parallel to the joint (Fig. 1B). The wire position is confirmed under the C arm and drill with a 4.5 mm drill bit. First, a Schanz screw was applied and the second screw was anterior to the first using a fixator as the template (Fig. 1C). Two screws were applied distally through the fixator clamp. The guide wire was passed below the tibial tuberosity from medial to lateral toward the fibula tip (Fig. 1D). Osteotome (10 mm) was passed over the guide wire up to the medial three -fourth and preserved the lateral cortex that will act as a hinge. The second and third cut was done by changing the osteotome in a different direction. Pass the fixator over the Schanz screw and apply the compression distraction unit and distract till 3–5° valgus (Fig. 1 D). Then compress the osteotomy site and start gradual distraction from the seventh postoperative day till achieving the valgus.
Fig. 1.
(1A) Dynamic axial fixator by S·H.Pitkar (1B) Guidewire in AP view aiming toward fibula tip (1C) Schanz screw passed in drilled tract (1D) Guidewire along the osteotomy track (1E) Opening of osteotomy with intact lateral hinge.
Postoperative one intravenous antibiotic shot was given and static quadriceps, knee range, and bedside mobilisation started on the same day of surgery. Following a 6-week period of partial weight-bearing, complete weight-bearing was allowed. Pin tract dressing was done with normal saline. The fixator removal was done on outpatient basis after osteotomy union. Before we discharge, patients are taught distraction on another similar fixator model. Distraction is started on eight postoperative days at a rate of 0.25 mm to be done four times a day (6 hourly intervals, the fourth one can be done before going to bed) until the planned alignment is achieved. We calculate the expected date of complete correction from preoperative planning and assess distraction with follow-up radiographs. We do the first follow-up X-ray at 2 weeks and measure the medial proximal tibial angle (MPTA) and compare with the previous radiograph to see the adequate distraction. Second, follow up at 3 weeks (2 weeks after a distraction) and measure the MPTA and distraction gap. Third, follow-up at time of expected complete correction and scannogram is done to see if planned alignment is achieved. After alignment is achieved we lock the fixator (Fig. 2, Fig. 3).
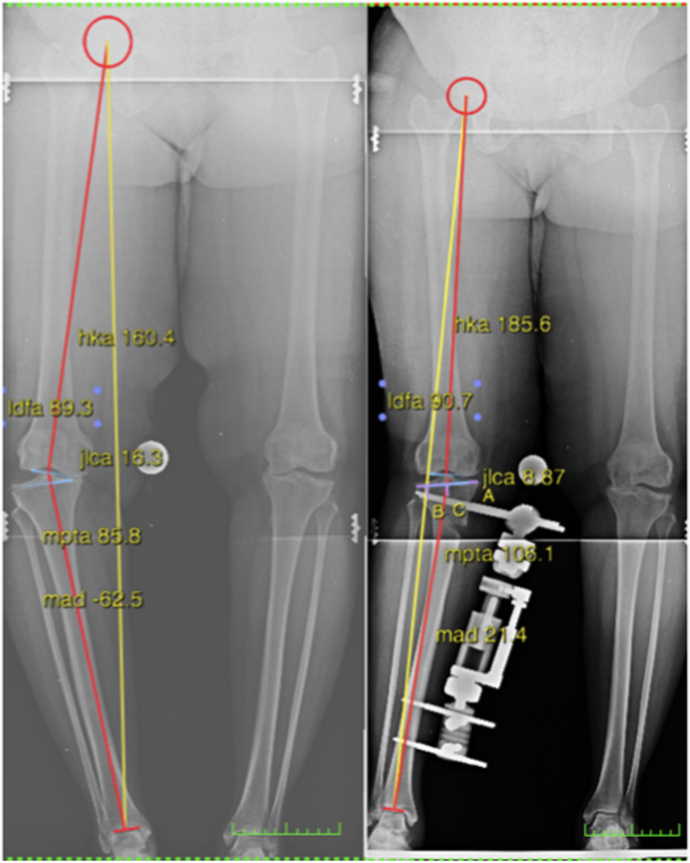
Fig. 2.
Pre- and post-operative weight-bearing showing the correction of the right leg.
Fig. 3.
Pre- and post-operative weight-bearing radiographs showing a correction of MPTA from 85.8° to 106.1° and HKA from 160.4° to 185.6°.
2.1.2. UKA
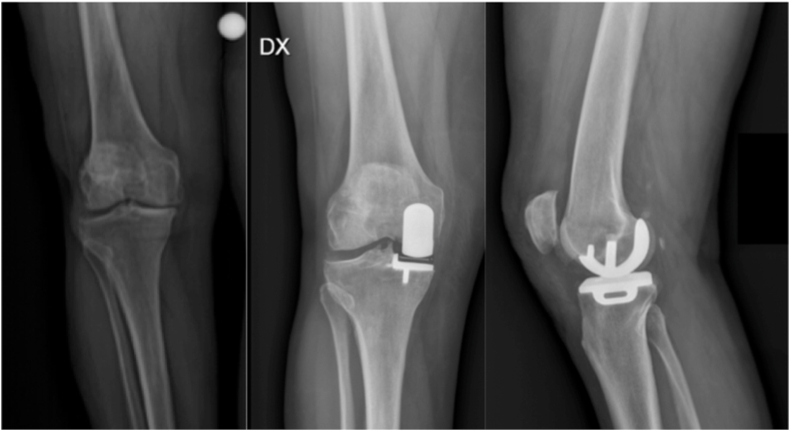
All MB-UKAs were performed with the same minimal invasive surgical approach and with Microplasty (Zimmer-Biomet). The surgical technique has been previously described in detail (Fig. 4).14
Fig. 4.
Anteroposterior pre-operative radiograph of a right knee, and antero-posteriore and lateral radiograph in a 54-year-old patient at final follow-up with Oxford UKA with no signs of aseptic loosenging or bearing dislocation.
Rehabilitation protocol started from same day of surgery involving passive mobilisation and weight-bearing as tolerated with two crutches. A gradual increasing in the load suggested in association with isometric muscle strengthening.
2.2. Clinical evaluation
Two orthopaedic surgeons who did not take part in the index operation handled the clinical follow-up. Each patient was evaluated for the Oxford Knee Score (OKS), the Knee Injury and Osteoarthritis Outcome Score (KOOS) and the Subjective International Knee Documentation Committee (IKDC). A clinical evaluation was conducted on the day of the surgery (T0) and at the follow-up visit (T1) (minimum follow-up time was 60 months).15 Complications and failures resulting from the surgery were recorded for each patient.
2.3. Statistical analysis
A mean and standard deviation are used to show a summary statistic (SD) or as percentages and absolute frequencies. We utilized the t-test and Wilcoxon-Mann-Whitney test to analyze continuous variables, and the chi-square test to analyze categorical variables. A paired t-test or a Wilcoxon signed-rank test was used to assess differences between the groups according to their written scores, while a t-test or a Wilcoxon-Mann-Whitney test was used to assess differences between the groups for each score at each time point. To evaluate the safety of the two techniques, the number of failures and the type of failures were recorded for each group and tested using a Fisher's exact test. Additionally, Pearson or Spearman correlations between the scores and the demographic and clinical factors were computed in accordance with the variable distribution. A p-value of less than 0.05 was regarded as statistically significant for two-sided testing. The analyses were carried out with R 4.1.1.
2.4. Sample size estimation
In this study, 120 subjects were required (60 for each group) to compare KOOS using a one-sided Wilcoxon-Mann-Whitney test while utilizing a 5% alpha and a mean difference of 15 and SD of 20 for both groups coefficient and 99% power. Using the same parameters, it was found that the Wilcoxon signed-rank test for comparing pre-post differences also had a power of 99% when detecting the difference. To assure statistical significance in the event of adverse events, additional individuals were recruited.
3. Results
Only the age of the patients at the pre-operative time significantly differed between the two groups, with the HTO group being significantly younger (47.7 ± 8.0 versus 55.8 ± 2.2). Table 1 summarises the results in greater detail.
Table 1.
Demographic details.
| Variables | HTO | UKA | p-value |
|---|---|---|---|
| N | 60 | 197 | |
| Age (Mean ± SD) | 47.78 ± 8.01 | 55.88 ± 2.28 | <0.001* |
| Sex, n (%) | |||
| Female | 40 (66.7) | 118 (59.9) | 0.429 |
| Male | 20 (33.3) | 79 (40.1) | |
| Side, n (%) | |||
| Left | 37 (61.7) | 94 (47.7) | 0.081 |
| Right | 23 (38.3) | 103 (52.3) | |
| Pre-operatory scores | |||
| Oxford Knee Score | 22.53 ± 6.45 | 22.77 ± 2.62 | 0.124 |
| KOOS | 45.67 ± 14.05 | 46.93 ± 13.91 | 0.392 |
| IKDC score | 36.80 ± 15.24 | 37.22 ± 15.67 | 0.982 |
* = statistical significant value (p < 0.05).
HTO = high tibial osteotomy; UKA = unicompartmental knee arthroplasty; OKS=Oxford Knee Score; KOOS=Knee Injury and Osteoarthritis Outcome Score; IKDC= Subjective International Knee Documentation Committee.
3.1. Clinical outcomes
After the final follow-up visit, all clinical scores significantly improved in both groups (p < 0.05).
IKDC and Oxford scores were higher for the UKA group (p < 0.05). See Table 2 for further details.
Table 2.
Clinical outcomes.
|
Table 2. Clinical outcomes | |||||
|---|---|---|---|---|---|
| Variables | HTO (N = 60) | UKA (N = 197) | Group comparison | Time comparison (p-value) | |
| Mean ± SD | Mean ± SD | p-value | HTO | UKA | |
| Oxford Knee Score | |||||
| T0 | 22.53 ± 6.45 | 22.77 ± 2.62 | 0.124 | <0.001* | <0.001* |
| T1 | 41.20 ± 3.71 | 44.66 ± 1.93 | <0.001* | ||
| KOOS | |||||
| T0 | 45.67 ± 14.05 | 46.93 ± 13.91 | 0.392 | <0.001* | <0.001* |
| T1 | 83.21 ± 7.85 | 82.23 ± 7.51 | 0.195 | ||
| IKDC score | |||||
| T0 | 36.80 ± 15.24 | 37.22 ± 15.67 | 0.982 | <0.001* | <0.001* |
| T1 | 66.48 ± 11.76 | 69.76 ± 10.57 | 0.044* | ||
* = statistical significant value (p < 0.05).
HTO = high tibial osteotomy; UKA = unicompartmental knee arthroplasty.
Regarding T1 scores, 194 patients were evaluated since scores could not be collected for three patients who had failed post-operatively.
3.2. Failures and complications
In the HTO group, three complications occurred (5%), including two superficial infections and one deep infection. On the other hand, the UKA group reported four complications (2%): three aseptic mobilisations and one infection requiring revision surgery. As shown in Table 3, between the two groups, there were no statistically significant differences in the complication rate (p = 0.208).
Table 3.
Complications reported.
| Parameters |
HTO (N = 60) |
UKA(N = 197) |
p-value |
|---|---|---|---|
| n (%) | n (%) | ||
| Number of complications | 3 (5.0) | 4 (2.0) | 0.208 |
| Complications | |||
| Aseptic mobilisation | 0 (0.0) | 3/4 (0.7) | 0.143 |
| Infection, any | 3/3 (100) | 1/4 (0.3) | 0.143 |
| Superficial infection | 2/3 (0.7) | 0 (0.0) | – |
| Deep infection | 1/3 (0.3) | 1/4 (0.0) | – |
* = statistical significant value (p < 0.05).
HTO = high tibial osteotomy; UKA = unicompartmental knee arthroplasty.
4. Discussion
The primary conclusions of the present study confirmed that both procedures can be considered safe with good to excellent clinical outcomes, with similar low rate of complications.
It has been shown that UKA is an effective solution for treating isolated medial compartment OA with intact knee ligaments. A learning curve is necessary for a successful UKA; indeed, the high volume centre shows a better result than the low volume centre. Robertson et al. found that a minimum of 24 UKAs per year resulted in a survival rate of 93%.16 UKAs have several benefits over total knee replacement replacements (TKRs), including less intraoperative blood loss, better function and a faster return to regular activity.17 According to the TOPKAT study, UKA was found to be cost-effective when compared to TKA for the treatment of isolated compartment disease.18
Fujisawa et al. found that fibrous cartilage could be formed inside the affected compartment of 54 knees, which had been operated on with HTO.19 Yim et al. reported the functional outcomes based on the Tegner and Lysholm knee scores and return to sports activities in patients who had received both medial opening wedge HTO and UKA. Although both groups showed good functional outcomes, there was a decrease in the level of activity for both groups. No significant difference were found in knee scores between the two groups. Three complications were reported in the HTO group (one implant failure and two iatrogenic fractures) and three in the UKA group (infection and aseptic loosening). During the follow-up, the alignments were valgus (1.8° in HTO) and varus (1.9° in UKA), but no difference was observed between the two groups in terms of OA progress.20 Tunicay et al. detailed their study of 255 knees treated with three different methods: UKA, HTO with external fixation and a medial open wedge HTO with a plate.21 The UKA group had a better SF-36 and HSS Knee Score than the other groups. The UKA group included one patient with a plateau fracture treated with a locking plate and three patients undergoing TKRs. Three patients undergoing HTO with plates had screws removed, and one patient in the HTO with external fixation group developed an infection, which was treated with a bone graft and internal fixation. A study by Takeuchi compared open wedge HTO fixed with Tomofix plate (27 knees) with UKA (30 knees) and found no significant differences in the KSS scores between the two groups. The mean age in their study was 67 ± 7 years and 77 ± 4 years for HTO & UKA respectively. At final follow up there were no difference in femoral tibial angle between two groups. HTO patients was able to continue preoperative level of sports activity and seiza style sitting. Two complications (infection & lateral tibia plateau fracture) were observed in the HTO group, while in the UKA group, two patients were treated with TKRs, and one patient with femoral component fracture was managed with component revision and polymeric exchange.22
Petersen and Metzlaff compared Open wedge HTO (Tomofix plate) with mobile bearing UKA (Oxford) in patients with medial compartment osteoarthritis. In study there was 25 patients operated wih HTO and 23 with UKA with minimum follow up of 5 years. At the time of analysis, indicated no difference in the functional scores, complications and revision rates between the two groups, but the pain scores were significantly higher in the UKA group after five years of following up.23 In a study conducted between 1998 and 2013, Krych et al. evaluated 240 patients treated with HTO (57) and UKA (183), with the mean age being 42.7 years in the HTO group and 49.2 years in the UKA group. At the final follow-up, the UKA group showed a greater Lysholm score improvement than the earlier groups. The UKA and HTO groups experienced, respectively, 6% and 23% revision TKRs. The failure occurred 42 months earlier in the UKA group than in the HTO group at 98 months.24 Jeon et al. evaluated 47 patients treated with HTO with articular cartilage surgery (26) and UKA (21) with a minimum of two years' follow-up. There was an improvement in the IKDC score in the UKA group compared to the HTO group at 6 months, but there was no difference at two years' follow-up. The mechanical axis in the HTO group achieved valgus, while in the UKA group, there was residual varus alignment.25 The early improvement in the clinical scores in the UKA group is explained by the fact that in the HTO group, full weight-bearing is possible only after osteotomy union and a long rehabilitation period.
According to Cao et al. UKA led to fewer complications and less post-operative pain compared to HTO; however, HTO led to a better range of motion. The knee function score did not differ significantly from the knee function score after revision surgery.26 Therefore, for patients with high functional demands, HTO is better than UKA.
In the present study IKDC and Oxford scores were higher for the UKA group because Indian people (HTO group) have different habits, lifestyle compared to western people (UKA group). HTO group was younger so more demanding with higher expectations.27,28
The advantage of HTO with the external fixator is good-quality regeneration at the osteotomy site and the correction of lower limb alignment. The fixator is removed after the healing of the osteotomy to prevent hardware-related complications. The external fixator is also useful in the case of large deformities when acute correction is difficult. The theoretical concern regarding the external fixator is pin tract infection, which can progress and affect future knee replacement. In this study, three infections were detected in the HTO group: two superficial infections managed with pin tract care and antibiotics and one deep infection treated with arthrotomy and wound wash. Regarding the complication rate, no statistically significant differences were seen between the two groups. The patient has to handle a fixator for around three months, which may affect their ability to wear trousers and cosmetic concerns. The timing of fixator removal should be planned after union to prevent the collapse of regeneration.
Our study had several limitations. It was conducted at only two institutions, and the findings may not be applicable to other patient populations.
In this study, other characteristics were not taken into account; only age-matched cohorts were. This study only evaluated a mid-term follow-up of five years, and further long-term studies are necessary to assess differences between these patient cohorts. Multiplane laxity measurements were not considered as a part of clinical evaluation in our study.
5. Conclusions
In young patients (<60 years) with an isolated medial knee (OA), both HTO and UKA led to good to excellent clinical results with a low rate of complications at mid-term follow-up; both surgical procedures may be considered in this patient population.
Institutional ethical committee approval (for all human studies)
Permission for the study was obtained from the local ethical committee.
Funding/sponsorship
“This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors”. *
Authors contribution
AY: writing, conceptualization, final editing; MP:supervision, surgery, final editing; IM: statistics, tables preparation; RG: writing, data collection; LM: final editing, supervion; NU: sugery, data collection; RD: writing, conceptualization, data collecting, final editing.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Declaration of competing interest
None.
Acknowledgments
This study was supported and funded by the Italian Ministry of Health – “Ricerca Corrente”.
Contributor Information
Amit Kumar Yadav, Email: amit_aur09@yahoo.com.
Mangal Parihar, Email: mangalparihar@parihar.net.
Ilaria Mariani, Email: ilaria.mariani1618@gmail.com.
Riccardo Giorgino, Email: riccardo.giorgino@unimi.it.
Laura Mangiavini, Email: laura.mangiavini@unimi.it.
Nicola Ursino, Email: nicolaursino@libero.it.
Riccardo D'Ambrosi, Email: riccardo.dambrosi@hotmail.it.
References
- 1.Lo G.H., Musa S.M., Driban J.B., et al. Running does not increase symptoms or structural progression in people with knee osteoarthritis: data from the osteoarthritis initiative. Clin Rheumatol. 2018;37:2497–2504. doi: 10.1007/s10067-018-4121-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray R., Winkler P.W., Shaikh H.S., Musahl V. High tibial osteotomy for varus deformity of the knee. J Am Acad Orthop Surg Glob Res Rev. 2021;5 doi: 10.5435/JAAOSGlobal-D-21-00141. e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D'Ambrosi R., Nuara A., Mariani I., et al. Return to physical activity and change in body mass index after hypoallergenic medial mobile-bearing unicompartmental knee arthroplasty. J Orthop Traumatol. 2021;22:36. doi: 10.1186/s10195-021-00598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.D'Ambrosi R., Anghilieri F.M., Corona K., et al. Similar rates of return to sports and BMI reduction regardless of age, gender and preoperative BMI as seen in matched cohort of hypoallergenic and standard Cobalt Chromium medial unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;30:890–898. doi: 10.1007/s00167-021-06467-1. [DOI] [PubMed] [Google Scholar]
- 5.Liu X., Chen Z., Gao Y., Zhang J., Jin Z. High tibial osteotomy: review of techniques and biomechanics. J Healthc Eng. 2019;2019 doi: 10.1155/2019/8363128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Ambrosi R., Nuara A., Mariani I., Di Feo F., Ursino N., Hirschmann M. Titanium niobium nitride mobile-bearing unicompartmental knee arthroplasty results in good to excellent clinical and radiographic outcomes in metal allergy patients with medial knee osteoarthritis. J Arthroplasty. 2021;36:140–147. doi: 10.1016/j.arth.2020.07.028. [DOI] [PubMed] [Google Scholar]
- 7.D'Ambrosi R., Ursino C., Setti S., Scelsi M., Ursino N. Pulsed electromagnetic fields improve pain management and clinical outcomes after medial unicompartmental knee arthroplasty: a prospective randomised controlled trial. J ISAKOS. 2022;S2059–7754(22) doi: 10.1016/j.jisako.2022.05.002. 00067. [DOI] [PubMed] [Google Scholar]
- 8.Mittal A., Meshram P., Kim W.H., Kim T.K. Unicompartmental knee arthroplasty, an enigma, and the ten enigmas of medial UKA. J Orthop Traumatol. 2020;21:15. doi: 10.1186/s10195-020-00551-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schuster P., Richter J. Editorial commentary: high tibial osteotomy is effective, even in patients with severe osteoarthritis: contradiction of another dogma from the past. Arthroscopy. 2021;37:645–646. doi: 10.1016/j.arthro.2020.11.025. [DOI] [PubMed] [Google Scholar]
- 10.Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):S31–S34. doi: 10.4103/sja.SJA_543_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamilton W.G., Ammeen D., Engh C.A., Jr., Engh G.A. Learning curve with minimally invasive unicompartmental knee arthroplasty. J Arthroplasty. 2010;25:735–740. doi: 10.1016/j.arth.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 12.Lee D.K., Kim K.K., Ham C.U., Yun S.T., Kim B.K., Oh K.J. The learning curve for biplane medial open wedge high tibial osteotomy in 100 consecutive cases assessed using the cumulative summation method. Knee Surg Relat Res. 2018;30:303–310. doi: 10.5792/ksrr.17.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohn M.D., Sassoon A.A., Fernando N.D. Classifications in brief: kellgren-lawrence classification of osteoarthritis. Clin Orthop Relat Res. 2016;474:1886–1893. doi: 10.1007/s11999-016-4732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ng J.P., Fan J.C.H., Lau L.C.M., Tse T.T.S., Wan S.Y.C., Hung Y.W. Can accuracy of component alignment be improved with Oxford UKA Microplasty® instrumentation? J Orthop Surg Res. 2020;15:354. doi: 10.1186/s13018-020-01868-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Collins N.J., Misra D., Felson D.T., Crossley K.M., Roos E.M. Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee Injury and osteoarthritis outcome score (KOOS), knee Injury and osteoarthritis outcome score physical function short form (KOOS-ps), knee outcome survey activities of daily living scale (KOS-adl), Lysholm knee scoring scale, Oxford knee score (OKS), western ontario and McMaster universities osteoarthritis index (WOMAC), activity rating scale (ARS), and tegner activity score (TAS) Arthritis Care Res. 2011;63:S208–S228. doi: 10.1002/acr.20632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robertsson O., Knutson K., Lewold S., Lidgren L. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br. 2001;83:45–49. doi: 10.1302/0301-620x.83b1.10871. [DOI] [PubMed] [Google Scholar]
- 17.Jones G.G., Kotti M., Wiik A.V., et al. Gait comparison of unicompartmental and total knee arthroplasties with healthy controls. Bone Joint Lett J. 2016;98-B:16–21. doi: 10.1302/0301-620X.98B10.BJJ.2016.0473.R1. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beard D.J., Davies L.J., Cook J.A., et al. TOPKAT Study Group The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet. 2019;394:746–756. doi: 10.1016/S0140-6736(19)31281-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fujisawa Y., Masuhara K., Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin N Am. 1979;10:585–608. [PubMed] [Google Scholar]
- 20.Yim J.H., Song E.K., Seo H.Y., Kim M.S., Seon J.K. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty at a minimum follow-up of 3 years. J Arthroplasty. 2013;28:243–247. doi: 10.1016/j.arth.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Tuncay İ., Bilsel K., Elmadağ M., Erkoçak Ö.F., Aşçı M., Şen C. Evaluation of mobile bearing unicompartmental knee arthroplasty, opening wedge, and dome-type high tibial osteotomies for knee arthritis. Acta Orthop Traumatol Turcica. 2015;49:280–287. doi: 10.3944/AOTT.2015.14.0320. [DOI] [PubMed] [Google Scholar]
- 22.Takeuchi R., Bito H., Akamatsu Y., et al. In vitro stability of open wedge high tibial osteotomy with synthetic bone graft. Knee. 2010;17:217–220. doi: 10.1016/j.knee.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 23.Petersen W., Metzlaff S. Open wedge high tibial osteotomy (HTO) versus mobile bearing unicondylar medial joint replacement: five years results. Arch Orthop Trauma Surg. 2016;136:983–989. doi: 10.1007/s00402-016-2465-1. [DOI] [PubMed] [Google Scholar]
- 24.Krych A.J., Reardon P., Sousa P., Pareek A., Stuart M., Pagnano M. Unicompartmental knee arthroplasty provides higher activity and durability than valgus-producing proximal tibial osteotomy at 5 to 7 years. J Bone Joint Surg Am. 2017;99:113–122. doi: 10.2106/JBJS.15.01031. [DOI] [PubMed] [Google Scholar]
- 25.Jeon Y.S., Ahn C.H., Kim M.K. Comparison of HTO with articular cartilage surgery and UKA in unicompartmental OA. J Orthop Surg. 2017;25 doi: 10.1177/2309499016684092. [DOI] [PubMed] [Google Scholar]
- 26.Cao Z., Mai X., Wang J., Feng E., Huang Y. Unicompartmental knee arthroplasty vs high tibial osteotomy for knee osteoarthritis: a systematic review and meta-analysis. J Arthroplasty. 2018;33:952–959. doi: 10.1016/j.arth.2017.10.025. [DOI] [PubMed] [Google Scholar]
- 27.Stevens K.N., Nadarajah V., Jauregui J.J., et al. Preoperative expectations of patients undergoing knee surgery. J Knee Surg. 2021;34:612–620. doi: 10.1055/s-0039-1698805. [DOI] [PubMed] [Google Scholar]
- 28.Whiting S., Mendes R., Abu-Omar K., et al. Physical inactivity in nine European and Central Asian countries: an analysis of national population-based survey results. Eur J Publ Health. 2021;31:846–853. doi: 10.1093/eurpub/ckab028. [DOI] [PMC free article] [PubMed] [Google Scholar]