Abstract
Background
Periprosthetic fractures of the distal femur remain a challenge to treat due to variations in both patient- and fracture-specific factors. This study was designed to analyze the outcomes of different subtypes of periprosthetic distal femur fractures based on the Su et al. classification system.
Methods
Thirty-six patients were classified with Su et al. system. All Type I and II fractures were managed with a locking plate. Most Type III fractures were managed with locking plate, while two were managed with long-stem revision arthroplasty due to evidence of implant loosening. Outcomes were measured and analyzed based on healing time, revision rate, and complication rate.
Results
Of the 36 patients, 30 (83.3%) achieved acceptable fracture union, while the remaining 6 (16.7%) experienced either delayed union or non-union. Type I fractures showed a significantly lower healing time than Type II and III fractures managed by locking plate. Delayed union was present in the Type II group, while non-union was recorded for two Type III fractures. Need for revision was more prevalent in fracture Types II and III.
Conclusion
The Su et al. system of classification for periprosthetic fractures of the distal femur matches the clinical outcomes of this study and would seem to be useful in the approach to the treatment of these fractures. The majority of these fractures can be managed with locking plate with reasonable results. However, if the implant is loosened in Type III fractures, revision arthroplasty is suggested.
Keywords: Distal femur, Periprosthetic fractures, Classification system, Outcomes, Subtypes, Total knee arthroplasty
1. Introduction
Total knee arthroplasty (TKA) can alleviate pain, restore function, and help patients with severe osteoarthritis maintain quality of life.1 A majority of the estimated 500,000 TKA procedures performed annually in the United States involve patients above 70 years old.2 Despite the procedure's utility, it carries a 0.3–2.5% risk of periprosthetic femur fracture, most frequently involving the distal femur.3, 4, 5 These fractures can reach a >20% 1-year mortality risk,5 making them a clinically significant problem. Risk factors for these fractures include this population's propensity for falls, medical comorbidities, and poor bone quality.6 Periprosthetic fractures of the distal femur remain difficult to treat due to variations in patient- and fracture-specific factors. As a result, each case requires careful consideration for proper management in order to satisfy each patient.7
Periprosthetic distal femur fractures usually require operative management which is commonly achieved by use of locked plating, intramedullary nailing, or revision arthroplasty. Retrograde supracondylar intramedullary nailing has shown high success rates, but its use is limited in certain scenarios.8 Locked plating has also shown promising results, demonstrating healing rates similar to intramedullary nailing.9 Despite its successes, there is still debate about strategies to decrease rates of non-union and complications with the use of locked plating.10 Finding a universal treatment method for periprosthetic femur fractures may not be feasible due to differences in fracture type and health status. Therefore, identifying select patient-specific factors that influence clinical outcome of these fractures may be an effective approach in helping determine the best surgical management for each patient.
The Su et al.11 classification system organizes periprosthetic distal femur fractures based on their location relative to the femoral implant and suggests surgical management options for each. The value of assessing a fracture based on location has been proven in the setting of hip arthroplasty, periprosthetic humerus fractures with shoulder and elbow arthroplasty, periprosthetic tibia fractures,12, 13, 14 and may prove to be useful here as well. Su et al. dictates that Type I injuries contain fracture lines entirely proximal to the femoral component. This makes these fractures mostly suitable for use of intramedullary nail, but a fixed-angle plate may sometimes be needed. Type II injuries have fracture lines arising at the level of the proximal aspect of the femoral component and continue proximally. These are best addressed with a fixed-angle plate, though a retrograde supracondylar intramedullary nail may be considered if an open femoral box is present. Injuries are classified as Type III when the fracture line extends distally past the upper edge of the femoral component. These may be treated with a fixed-angle plate if the prosthesis is intact. Otherwise, revision arthroplasty is indicated.11 Currently, outcomes based on the Su et al. classification system have not been thoroughly investigated. This study investigates outcomes of the Su et al. system, specifically in regard to its approach of classifying fractures by anatomic location, and if different fracture locations (Su et al. classification) are associated with different outcomes. The goal is to determine this system's clinical utility in formulating a reliable and straightforward approach to treating periprosthetic distal femur fractures after TKA which can lead to significantly improved treatment outcomes.
2. Materials and methods
This study was an Institutional Review Board-approved retrospective study of patients with a TKA who were treated for a distal femur fracture between the years of 2008 and 2016. Patient medical records and radiographs were viewed using the electronic medical record of a university hospital level I trauma center based on cases relating to the “femur.” Informed consent was given at time of treatment/prior to inclusion in the study. This search criterion identified patients treated operatively for extra-articular distal femur fractures above a TKA. Patients were included if treatment included use of locked plating or revision arthroplasty. Exclusion criteria included use of other surgical methods, follow-up of less than 6 months, and insufficient electronic medical or radiographic data. Patient X-rays were examined by two senior authors and supplemented with written records and descriptions. Data on age, treatment method, complications, etc. were collected from patient charts and organized using Microsoft Excel spreadsheets.
At least two X-ray views of the injured femur were initially obtained for each patient. Fractures were classified retrospectively from these pre-operative X-rays, based on the Su et al. system for supracondylar periprosthetic distal femur fractures. An approach to each operation was formulated based on the individual patient's scenario regarding fracture quality and location, as well as any relevant complications. The decision to treat surgically with locking plate was made for all patients except when the implant was loosened; revision arthroplasty was selected in these patients. Postoperative antibiotics and deep vein thrombosis prophylaxis were given in all cases. Patients were allowed to sit up in the bed following surgery, with toe-touch weight bearing and range of motion exercises performed on an appropriate timeline under the guidance of physical therapists and approval of physicians. The amount of weight-bearing was gradually increased and patients were made weight-bearing as tolerated at 2 weeks post-operatively, unless the fracture was severely comminuted and the surgeon specifically requested a longer timeline. Patients followed up within 2, 6, 12, 24, and 48 weeks, with additional visits at the discretion of the patient and/or surgeon.
Outcomes were measured and recorded based on the patient's healing status, radiologic presentation, weight-bearing status, need for revision, and complication(s). Fracture union was defined as the ability to bear weight without pain at the fracture site, or the presence of callus bridging at least 1 cortex on both the anteroposterior and lateral radiographic views. The two Type III fractures treated with revision arthroplasty were considered clinically healed immediately after surgery (healing time <1 month). Delayed union was defined as healing that extended beyond 6 months from the time of surgery. Nonunion was defined as the absence of progressive signs of healing for 3 months after a period of 6 months had elapsed from the date of the surgery.
Data were analyzed using SPSS® software. Fisher's exact test, t-test, and ANOVA with Tukey post hoc test were used to compare rates of union vs. non-union, complications, need for revision, and healing times between groups within the Su et al. classification system. Four unique groups were compared for the purpose of statistical analysis. Type I and Type II fractures were individual groups, while Type III fractures were separated into two groups: those managed with locked plating, and those managed with revision arthroplasty.
3. Results
Thirty-six patients met inclusion criteria and were evaluated for the purpose of this study. Average participant age was 71.2 (range 50–92) years. Gender breakdown of the study population was 32 females (88.9%) and 4 males (11.1%). All fractures were considered low-energy, mostly sustained after a fall at ground level. Average time between injury and surgery was 2.79 days. Average length of follow-up was >12 months. Thirty-three (91.7%) fractures were considered displaced on presentation. Fractures were comminuted in eight (22.2%) patients: four each of Type II and III. Poor bone quality, seen as osteopenia/osteoporosis was noted in 28 (77.8%) cases [Table 1].
Table 1.
Demographic data by Su et al. sub-classification.
| Classification | Patients (N) | Average Age (years) | Gender | Cases with Fracture Comminution (n, [n/N]) |
|---|---|---|---|---|
| OVERALL | 36 | 71.2 | F: 32 M: 4 |
8 [23.5%] |
| Type I | 9 | 73.6 | F: 9 M: 0 |
0 |
| Type II | 15 | 68.8 | F: 12 M: 3 |
4 [26.7%] |
| Type III (locking plate) | 10 | 73.7 | F: 9 M: 1 |
4 [40%] |
| Type III (revision arthroplasty) | 2 | 66.5 | F: 2 M: 0 |
0 |
Clinical characteristics of fractures were identified based on classification within the Su et al. system. There were nine Type I fractures [Fig. 1], 15 Type II fractures [Fig. 2], and 12 Type III fractures. All Type I and Type II fractures (34) were managed with locking plate. Of the 12 Type III fractures, 10 were initially managed with locking plate [Fig. 3], while two were managed with long-stem revision arthroplasty due to evidence of significant implant loosening [Fig. 4].
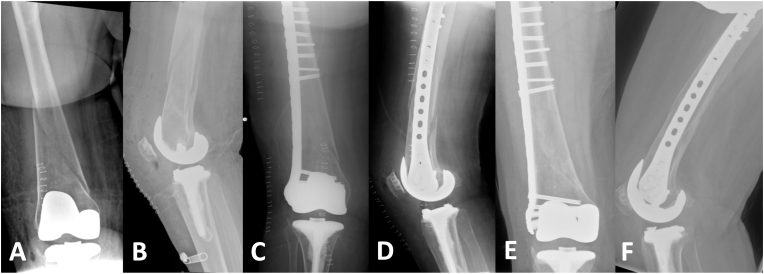
Fig. 1.
Type I fracture, 70-year-old female; (A) Anterior/Posterior (A/P) view preoperatively; (B) Lateral view preoperatively; (C) A/P view 2 weeks postoperatively, (D) Lateral view 2 weeks postoperatively; (E) A/P view 3 months post-operatively; (F) Lateral view 3 months postoperatively.
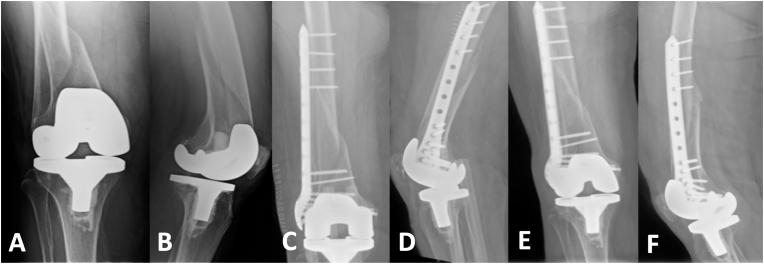
Fig. 2.
Type II fracture, 90-year-old female; (A) A/P view preoperatively; (B) Lateral view preoperatively; (C) A/P view 2 weeks postoperatively; (D) Lateral view 2 weeks postoperatively; (E) A/P view 5 months post-operatively; (F) Lateral view 5 months postoperatively.
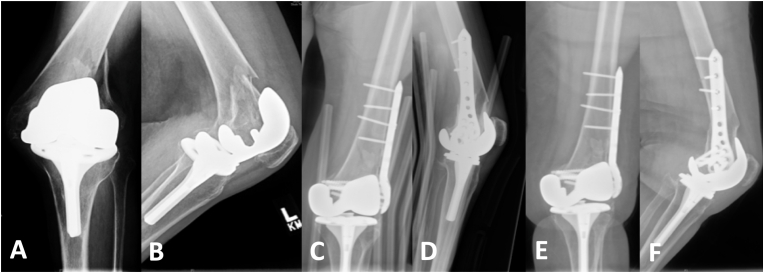
Fig. 3.
Type III fracture, 67-year-old female; (A) A/P view preoperatively; (B) Lateral view preoperatively; (C) A/P view 2 weeks postoperatively, (D) Lateral view 2 weeks postoperatively; (E) A/P view 5 months post-operatively; (F) Lateral view 5 months postoperatively.
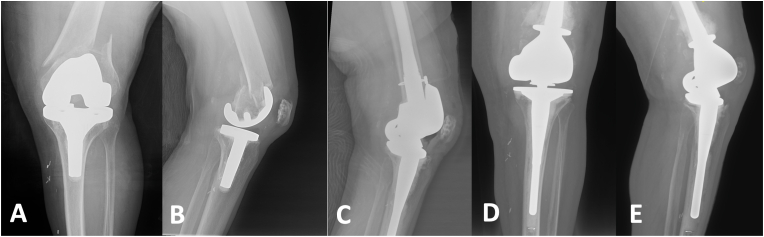
Fig. 4.
Type III fracture, 81-year-old female, revision long-stem arthroplasty; (A) A/P view preoperatively; (B) Lateral view preoperatively; (C) A/P view 2 weeks postoperatively; (D) Lateral view 2 weeks postoperatively; (E) A/P view 5 months post-operatively; (F) Lateral view 5 months postoperatively.
Of the 36 patients, 30 (83.3%) achieved acceptable fracture union, while the remaining 6 (16.7%) experienced either delayed union (1) or non-union (5). Average healing time for all patients was 3.8 months (SD = 1.95) following initial operation. Type I fractures showed a significantly lower healing time than Type II and III fractures managed by locking plate. Delayed union was present in the Type II group, while non-union was recorded for two Type III fractures. Need for revision was more prevalent in fracture Types II and III as well [Table 2].
Table 2.
Clinical healing outcomes of fractures, broken down into sub-classification within Su et al. system.
| Classification | Average Healing Time (Months) | Successful Union (n, [n/N]) | Delayed Union (n) | Non-Union (n) | Cases Requiring Revision (n, [n/N]) |
|---|---|---|---|---|---|
| OVERALL | 3.81 | 28 [82.4%] | 1 | 5 | 8 [23.5%] |
| Type I | 2.67 | 9 [100%] | 0 | 0 | 1 [11.1%] |
| Type II | 4.33 | 11 [73.3%] | 1 | 3 | 3 [20%] |
| Type III (locking plate) | 5.19 | 8 [80%] | 0 | 2 | 4 [40%] |
| Type III (revision arthroplasty) | <1 | 2 [100%] | 0 | 0 | 0 |
There was a statistically significant difference in healing time between groups as determined by one-way ANOVA (F(3,27) = 8.6; p = 0.0004). A Tukey post hoc test showed healing time for Type III fractures managed with revision arthroplasty (M = 0.25months, SD = 0) was significantly shorter than healing time for Type II (M = 4.33, SD = 2.09, p < 0.01), and Type III fractures managed with locking plate (M = 5.19, SD = 1.13, p < 0.01). There was a statistically significant difference in healing time between Type I (M = 2.67, SD = 0.35) and Type II fractures (M = 4.33, SD = 2.09) as determined by independent-samples t-test (t = −2.35, p < 0.05). There was also a statistically significant difference in healing time between Type I (M = 2.67, SD = 0.35) and Type III fractures managed with locking plate (M = 5.19, SD = 1.13) as determined by independent-samples t-test (t = −6.36, p < 0.0001). There was no statistically significant difference in rates of failed bony union between groups as determined by Fisher's Exact Test.
Post-operative alignment was evaluated and deemed to be acceptable if within 5° of angulation difference compared to the contralateral uninjured limb in all planes. Eight (22.2%) patients experienced complications following surgery: two required revision for infection at the surgical site, three experienced failed fixations, and three experienced hardware failure. Cases of failed fixation and hardware failure were managed with either revision open reduction and internal fixation (ORIF) or intramedullary nail placement, while cases of infection were managed with excision arthroplasty or placement of cement spacer and intramedullary rod. Complications and revisions occurred for all fracture types, with no significant differences between groups for either metric as determined by Fisher's Exact Test [Table 3].
Table 3.
The complications of fractures based on sub-classification within Su et al. system.
| Complication Type | Su et al. Classification Type | Revision |
|---|---|---|
| Hardware Failure | I | Implant removal; intramedullary nail |
| Hardware Failure | II | Revision ORIF with iliac crest autograft |
| Hardware Failure | II | Revision ORIF with iliac crest autograft |
| Failed Fixation | II | Revision ORIF with iliac crest autograft |
| Failed Fixation | III | Revision ORIF withcement application |
| Failed Fixation | III | Revision ORIF withcement application |
| Infected Screws | III | Excision arthroplasty |
| LKA Infection | III | Implant removal; intramedullary nail |
4. Discussion
Extra-articular, periprosthetic fractures of the distal femur in the setting of TKA remain challenging to treat. Many treatment options for these fractures are available, ranging from non-operative treatment to operative treatment with ORIF using conventional or fixed-angle locking plates, intramedullary fixation, external fixation, or revision TKA.8 Treatment choice can be dictated by several factors including fracture site, displacement, distal fragment size, bone quality, and implant stability.
This study evaluated periprosthetic distal femur fractures initially managed with locked plating, as well as two cases treated with revision arthroplasty due to a loose femoral component. Fractures were retrospectively classified within the Su et al. classification system11 of periprosthetic distal femur fractures around a TKA, allowing the evaluation of any influences fracture location may have on clinical outcomes. Each of the system's fracture types were encountered and are represented in this study, providing the opportunity for a robust outcome analysis. The average clinical healing time for Type I fractures (2.7 months) was significantly shorter than the average clinical healing time of Type II (4.3 months) and Type III (5.2 months). This may be inherently related to fracture location, as proximally located fractures have been suggested to heal faster than those which are located more distally.15 Type I fractures also generally had a satisfactory healing course, with only one case requiring revision for hardware failure and no cases of delayed or non-union. Ultimately these data suggest that Type I fractures can heal reliably well with locking plate fixation.
Outcomes for Type II and III fractures managed with locked plating were less favorable than those seen in Type I fractures. Both groups experienced an average healing time (4.3 months and 5.2 months, respectively) longer than the study's overall average, as well as some cases of delayed and/or non-union. Conversely, the Type III fractures managed initially with revision arthroplasty were considered nearly immediately healed and neither of these cases demonstrated need for revision.
It is unlikely that blood supply contributed to the sub-optimal healing course of the Type II and III fractures managed with locking plate, as the distal femur metaphyseal area is well-vascularized and known for good bone healing potential.16 These findings may instead be correlated to the proximity of these fractures to the femoral prosthesis and subsequent disruption of physiological mechanical forces, similar to the trend described for tibial periprosthetic fractures.17 These groups also had higher revision rates (20% and 40%, respectively) than the Type I group, with several instances of failed fixation (13.3% and 10%, respectively). The low trans-condylar and inter-condylar locations of the fractures that make up the Type II and III groups make distal fixation particularly difficult and significantly increase the risk of fixation failure.18 While fixed-angle plating may often be necessary and prudent for these extremely distal fractures,19 there may be ways to improve upon current methods. For example, while the prosthesis may not be overtly compromised at the time of Type II/III injury, it is possible that the prosthesis' proximity to the fracture's abnormal bony structure may cause it to experience residual aberrant mechanical forces that predispose it to loosening under normal physiologic conditions. Therefore, expanding the indications for considering revision TKA to include Type II/III fractures despite a stable prosthesis may prove to be beneficial and yield superior clinical outcomes. Judicious use of long-stem arthroplasty and cerclage wires has previously shown greater success than internal fixation in treating periprosthetic humerus fractures20 and may be a reasonable option to consider in these cases of Type II and III fractures, especially with revision more frequently necessary.
In de-classifying the fractures and taking a broader look at the data, the overall rate of delayed and non-union (16.7%) in this study is similar, but slightly lower than the non-union rate (22.2%) previously reported on systematic review of periprosthetic distal femur fractures treated with locked plate.21 While this may indicate overall advancement of surgical technique, it reiterates the need to identify fixation methods or techniques that afford greater healing potential with a rate of failed bony union closer to the estimated overall average rate (5–10%) for surgically managed fractures.22 Many factors contribute to development of non-union, including failed fixation, hardware failure, adverse fracture characteristics (comminution, openness, displacement), infection, comorbidities (diabetes, osteoporosis, chronic inflammatory state), and smoking.23 Only failed fixation has been addressed here; the remaining factors are not outright modifiable.
Patients that undergo TKA are most often elderly and at higher risk for femur fracture for several reasons. Elderly people experience a higher rate of falls than the general population, a leading cause of periprosthetic femur fractures.24 Additionally, disease processes that plague the elderly patient population (e.g. rheumatoid arthritis, osteoporotic and osteopenic bone, diabetes, and cardiovascular disease) subsequently increase the susceptibility for periprosthetic fracture.25 These factors help explain the average age of the study population being above 70 years old. It is important to point out that nearly 90% of patients in this study were female. Osteoporosis is more common in females, and the associated decrease in bone mineral density puts women at higher risk for fractures.26 Prior studies on periprosthetic fractures of the distal femur have reported rates of gender breakdown that range from nearly evenly split27 to 86% female.21 While the predominance of females experiencing periprosthetic fracture in this study is not necessarily surprising, the extreme prevalence may warrant exploring more adequate preventative measures in the future.
Several classification systems for periprosthetic distal femur fractures currently exist, each focusing on different characteristics such as location of fracture on the distal femur, bone quality, fracture displacement, prosthesis stability, and pattern complexity. The most popular of these systems was developed by Rorabeck and Taylor.28 They proposed classifying each fracture based on its relative displacement as well as stability of the prosthesis. This is useful for identifying non-displaced fractures that may be treated non-operatively, as well as those with a loose prosthesis that may require revision surgery. However, an extremely high percentage of these fractures present with displacement, as evidenced in this study and other relevant literature (91.7% and 78%, respectively).29 When managed with a locking plate, the percentage of successful healing outcomes differed between undisplaced (Rorabeck Type I) and displaced (Rorabeck Type II); undisplaced fractures occurred much less frequently (n = 2) but had successful healing outcomes of 100% whereas displaced fractures were more common (n = 180) with successful healing outcomes of 87%.30 This prevents an appropriate comparative analysis and offers limited information that would be useful for choosing a fixation method. Unlike the Rorabeck and Taylor system, Su et al. does not utilize fracture displacement as a distinguishing criterion for classification; it is purely location-based to allow for accurate comparative analysis and treatment considerations.
The Universal Classification System (UCS) has been proposed as a standardized classification system for periprosthetic fractures, incorporating numerous current classification systems into one simple one.31 The UCS has the potential to be a valuable resource for classification of periprosthetic fractures and communication between surgeons. Evaluation of clinical outcomes of the treatment suggestions associated with the Su et al. classification system may provide insight into use of the UCS in a similar way in the future.
This study had several benefits and limitations. Patient data was taken from charts in a retrospective manner, not prospectively. Grouping fractures into classification types was beneficial in allowing comparative analysis but created some notably small sample sizes that limited the study's statistical power. Additionally, follow-ups were spaced months apart which makes exact determination of clinical healing time difficult. Assessment of fracture healing on X-rays is also challenging. Different angles may be needed to determine the presence of a callus bridge at the fracture line since the implant is in the way. Radiographs were combined with the clinical examination and time elapsed since surgery to create a broader picture to determine appropriate healing. Many patients had comorbidities, which present unique challenges in treatment. It is important to address these comorbidities and recognize potential adverse outcomes, although there is no significant difference between rates of union and nonunion after lateral plate fixation of periprosthetic distal femur fractures in diabetic patients or those who smoke.32 There was no comparison to outcomes of treatment with intramedullary nail or conservative measures. More in-depth studies in the future comparing these methods would provide more insight. The results also suggest there may be benefits in further studies on periprosthetic distal femur fractures in patients on osteoporosis drug regimens.
In conclusion, the Su et al. system of classification for periprosthetic fractures of the distal femur matches the clinical outcomes of this study and would seem to be useful in the approach to treatment of these fractures. Based on the results, fractures proximal to the femoral component generally have a shorter healing time than fractures that originate from the femoral component and extend proximally or the fracture line extends distally past the component. The majority of these fractures can be managed with locking plate with reasonable results. However, if the implant is loosened in Type III fractures, revision arthroplasty is suggested.
Funding/sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Informed consent
Informed consent was obtained from all individual participants included in the study when they were admitted to our medical center.
Ethical approval
This article does contain human participants and was approved by an Institutional Review Board.
Author contribution statement
Conception and design: JL, MM & NE.
Provision of study materials or patients: All authors.
Collection and assembly of data: MM, JB, ME, DP & JL.
Data analysis and interpretation: MM, JB, ME, DP & JL.
Manuscript writing: All authors.
Final approval of manuscript: All authors.
Declaration of competing interest
All authors have nothing to disclose.
Acknowledgments
We are also grateful to Gregory Otto PA, Jared Johnson PA for assistance with double-checking fracture healing time for this study.
References
- 1.Lavernia C.J., Guzman J.F., Gachupin-Garcia A. Cost effectiveness and quality of life in knee arthroplasty. Clin Orthop Relat Res. 1997 Dec;345:134–139. [PubMed] [Google Scholar]
- 2.Jain N.B., Higgins L.D., Ozumba D., et al. Trends in epidemiology of knee arthroplasty in the United States, 1990-2000. Arthritis Rheum. 2005 Dec;52(12):3928–3933. doi: 10.1002/art.21420. [DOI] [PubMed] [Google Scholar]
- 3.Della Rocca G.J., Leung K.S., Pape H.C. Periprosthetic fractures: epidemiology and future projections. J Orthop Trauma. 2011 Jun;25(Suppl 2):S66–S70. doi: 10.1097/BOT.0b013e31821b8c28. [DOI] [PubMed] [Google Scholar]
- 4.Frenzel S., Vécsei V., Negrin L. Periprosthetic femoral fractures--incidence, classification problems and the proposal of a modified classification scheme. Int Orthop. 2015 Oct;39(10):1909–1920. doi: 10.1007/s00264-015-2967-4. [DOI] [PubMed] [Google Scholar]
- 5.Ruder J.A., Hart G.P., Kneisl J.S., Springer B.D., Karunakar M.A. Predictors of functional recovery following periprosthetic distal femur fractures. J Arthroplasty. 2017;32(5):1571–1575. doi: 10.1016/j.arth.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 6.Martinet O., Cordey J., Harder Y., Maier A., Bühler M., Barraud G.E. The epidemiology of fractures of the distal femur. Injury. 2000 Sep;31(Suppl 3):C62–C63. doi: 10.1016/s0020-1383(00)80034-0. [DOI] [PubMed] [Google Scholar]
- 7.Ebraheim N.A., Liu J., Hashmi S.Z., Sochacki K.R., Moral M.Z., Hirschfeld A.G. High complication rate in locking plate fixation of lower periprosthetic distal femur fractures in patients with total knee arthroplasties. J Arthroplasty. 2012 May;27(5):809–813. doi: 10.1016/j.arth.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 8.McGraw P., Kumar A. Periprosthetic fractures of the femur after total knee arthroplasty. J Orthop Traumatol. 2010;11(3):135–141. doi: 10.1007/s10195-010-0099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ebraheim N.A., Kelley L.H., Liu X., Thomas I.S., Steiner R.B., Liu J. Periprosthetic distal femur fracture after total knee arthroplasty: a systematic review. Orthop Surg. 2015 Nov;7(4):297–305. doi: 10.1111/os.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhattacharyya T., Chang D., Meigs J.B., Estok D.M., 2nd, Malchau H. Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am. 2007 Dec;89(12):2658–2662. doi: 10.2106/JBJS.F.01538. [DOI] [PubMed] [Google Scholar]
- 11.Su E.T., DeWal H., Di Cesare P.E. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg. 2004 Jan-Feb;12(1):12–20. doi: 10.5435/00124635-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Masri B.A., Meek R.M., Duncan C.P. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004 Mar;420:80–95. doi: 10.1097/00003086-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Gebrelul A., Green A., Schacherer T., Khazzam M. Periprosthetic humerus fractures: classification, management, and review of the literature. Ann Joint. 2018;3:49. [Google Scholar]
- 14.Stuart M.J., Hanssen A.D. Total knee arthroplasty: periprosthetic tibial fractures. Orthop Clin N Am. 1999 Apr;30(2):279–286. doi: 10.1016/s0030-5898(05)70082-1. [DOI] [PubMed] [Google Scholar]
- 15.Fayaz H.C., Giannoudis P.V., Vrahas M.S., et al. The role of stem cells in fracture healing and nonunion. Int Orthop. 2011 Nov;35(11):1587–1597. doi: 10.1007/s00264-011-1338-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freiling D., van Heerwaarden R., Staubli A., Lobenhoffer P. The medial closed-wedge osteotomy of the distal femur for the treatment of unicompartmental lateral osteoarthritis of the knee. Operat Orthop Traumatol. 2010 Jul;22(3):317–334. doi: 10.1007/s00064-010-9006-9. [DOI] [PubMed] [Google Scholar]
- 17.Schreiner A.J., Schmidutz F., Ateschrang A., et al. Periprosthetic tibial fractures in total knee arthroplasty - an outcome analysis of a challenging and underreported surgical issue. BMC Muscoskel Disord. 2018 Sep 11;19(1):323. doi: 10.1186/s12891-018-2250-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ricci W.M., Streubel P.N., Morshed S., Collinge C.A., Nork S.E., Gardner M.J. Risk factors for failure of locked plate fixation of distal femur fractures: an analysis of 335 cases. J Orthop Trauma. 2014 Feb;28(2):83–89. doi: 10.1097/BOT.0b013e31829e6dd0. [DOI] [PubMed] [Google Scholar]
- 19.Streubel P.N., Gardner M.J., Morshed S., Collinge C.A., Gallagher B., Ricci W.M. Are extreme distal periprosthetic supracondylar fractures of the femur too distal to fix using a lateral locked plate? J Bone Joint Surg Br. 2010 Apr;92(4):527–534. doi: 10.1302/0301-620X.92B3.22996. [DOI] [PubMed] [Google Scholar]
- 20.Campbell J.T., Moore R.S., Iannotti J.P., Norris T.R., Williams G.R. Periprosthetic humeral fractures: mechanisms of fracture and treatment options. J Shoulder Elbow Surg. 1998 Jul-Aug;7(4):406–413. doi: 10.1016/s1058-2746(98)90033-7. [DOI] [PubMed] [Google Scholar]
- 21.Hoffmann M.F., Jones C.B., Sietsema D.L., Koenig S.J., Tornetta P., 3rd Outcome of periprosthetic distal femoral fractures following knee arthroplasty. Injury. 2012 Jul;43(7):1084–1089. doi: 10.1016/j.injury.2012.01.025. [DOI] [PubMed] [Google Scholar]
- 22.Giannoudis P.V., Einhorn T.A., Marsh D. Fracture healing: the diamond concept. Injury. 2007 Sep;38(Suppl 4):S3–S6. doi: 10.1016/s0020-1383(08)70003-2. [DOI] [PubMed] [Google Scholar]
- 23.Santolini E., West R., Giannoudis P.V. Risk factors for long bone fracture non-union: a stratification approach based on the level of the existing scientific evidence. Injury. 2015 Dec;46(Suppl 8):S8–S19. doi: 10.1016/S0020-1383(15)30049-8. [DOI] [PubMed] [Google Scholar]
- 24.Platzer P., Schuster R., Aldrian S., et al. Management and outcome of periprosthetic fractures after total knee arthroplasty. J Trauma. 2010 Jun;68(6):1464–1470. doi: 10.1097/TA.0b013e3181d53f81. [DOI] [PubMed] [Google Scholar]
- 25.Yasen A.T., Haddad F.S. Periprosthetic fractures: bespoke solutions. Bone Joint Lett J. 2014 Nov;96-B(11 Supple A):48–55. doi: 10.1302/0301-620X.96B11.34300. [DOI] [PubMed] [Google Scholar]
- 26.Pietschmann P., Rauner M., Sipos W., Kerschan-Schindl K. Osteoporosis: an age-related and gender-specific disease--a mini-review. Gerontology. 2009;55(1):3–12. doi: 10.1159/000166209. [DOI] [PubMed] [Google Scholar]
- 27.Beals R.K., Tower S.S. Periprosthetic fractures of the femur. An analysis of 93 fractures. Clin Orthop Relat Res. 1996 Jun;327:238–246. doi: 10.1097/00003086-199606000-00029. [DOI] [PubMed] [Google Scholar]
- 28.Rorabeck C.H., Taylor J.W. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin N Am. 1999 Apr;30(2):209–214. doi: 10.1016/s0030-5898(05)70075-4. [DOI] [PubMed] [Google Scholar]
- 29.Herrera D.A., Kregor P.J., Cole P.A., Levy B.A., Jönsson A., Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981-2006) Acta Orthop. 2008 Feb;79(1):22–27. doi: 10.1080/17453670710014716. [DOI] [PubMed] [Google Scholar]
- 30.Ebraheim N.A., Kelley L.H., Liu X., Thomas I.S., Steiner R.B., Liu J. Periprosthetic distal femur fracture after total knee arthroplasty: a systematic review. Orthop Surg. 2015 Nov;7(4):297–305. doi: 10.1111/os.12199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van der Merwe J.M., Haddad F.S., Duncan C.P. Field testing the Unified Classification System for periprosthetic fractures of the femur, tibia and patella in association with knee replacement: an international collaboration. Bone Joint Lett J. 2014 Dec;96-B(12):1669–1673. doi: 10.1302/0301-620X.96B12.34103. [DOI] [PubMed] [Google Scholar]
- 32.Campbell S.T., Lim P.K., Kantor A.H., et al. Complication rates after lateral plate fixation of periprosthetic distal femur fractures: a multicenter study. Injury. 2020 Aug;51(8):1858–1862. doi: 10.1016/j.injury.2020.05.009. [DOI] [PubMed] [Google Scholar]