Abstract
Aim
To validate the PAWPER tape and assess its inter-observer reliability in children accessing a Paediatric Emergency Department (PED). As secondary outcome we compared the accuracy of the PAWPER tape with that of parents’ estimation, the Broselow tape and the European Paediatric Life Support (EPLS) formula.
Methods
This was a cross-sectional study of children (0–12 years) enrolled in a tertiary Paediatric Emergency Department in Italy. Children’s weight was estimated by parents and by trained healthcare providers using the PAWPER tape, the Broselow tape and the EPLS formula. The root mean squared percentage error (RMSPE) for the estimation of precision was calculated. Overall accuracy was evaluated using the percentage of weight estimation falling within 10% (PW10) and 20% (PW20) of real weight.
Results
The study included 2060 children. Parental estimation was the most accurate and precise method. The PAWPER tape was accurate throughout all habitus sizes except for extreme underweight and overweight categories. Furthermore, it was more accurate and more precise than the Broselow tape and the EPLS formula (p adjusted <0.001).
Conclusions
The PAWPER tape served as an accurate method for weight estimation in children accessing a Paediatric Emergency Department, with excellent inter-rater reliability. It performed significantly better than other length or age-based tools, showing good accuracy and precision except for very extreme weights. Whilst parents’ estimation yielded to be the most accurate and precise method, the age-based EPLS formula was not reliable for estimating weight in all subcategories of habitus.
Keywords: Weight-estimation, Children, Resuscitation, Broselow tape, PAWPER tape
Introduction
Knowledge of patient’s body weight is essential in several paediatric critical settings1, 2 since it may determine drug dosage, intravenous fluid volumes, defibrillator joules and choice of equipment size. However, in emergency situations, such as during resuscitation, children cannot be weighed easily, while parents may not be immediately available to provide such essential information. Therefore, accurate, simple and quick weight estimation methods can be necessary to ensure the safety and efficacy of numerous emergency therapeutic interventions.3
To date, several tools have been developed to quickly achieve acceptable accuracy and precision in estimating weight in children.4 The Broselow tape is still among the most used, even though it approximates the weight considering one parameter only the patient’s length.5 Similarly, other methods consider the patient’s age as the only parameter to roughly calculate weight, such as the European Paediatric Life Support (EPLS) formula. However, children’s weight is not strictly related to length or age only, as other variables may be implicated, including the body mass. Indeed, the weight of children of the same height (length) or age can grossly vary due to different body habitus, and some studies found low accuracy of one-dimensional systems for weight estimation in over- and under-weighted children. In particular, ideal body weight (IBW) and total body weight (TBW) can differ greatly in obese children, making it problematic to calculate the correct dosage of any emergency drug in this population, as both hydrophilic and lipophilic agents may be required.
Of note, the incidence of obesity is increasing all over the world while underweight/unnourished children in low-income countries may not fit weight prediction tools developed for wealthy populations.6, 7, 8
The PAWPER (Paediatric Advanced Weight Prediction in the Emergency Room) tape is a two-dimensional system that accounts both for the length and child’s habitus, aiming to provide a more accurate weight estimation.1, 9
In 2012, Wells et al. developed and validated the PAWPER tape in a South African population.6 The accuracy of the PAWPER has been confirmed in a small sample of 199 Australian children,10 while it has not been confirmed in a larger sample in the United States.1 To our knowledge, the PAWPER tape has not yet been validated in any European centre. Furthermore, few studies have directly compared different methods of estimating weight in the same sample of children.
The primary objectives of our study were to validate the PAWPER tape in a large paediatric cohort and evaluate its inter-observer reliability in children visiting our Paediatric Emergency Department (PED) in Verona.
As a secondary result we directly compared the accuracy of the PAWPER tape with that of parents' estimation and two other weight estimation tools, namely the Broselow tape and the European Paediatric Life Support (EPLS) formula.14
Methods
Study design and study population
We conducted a cross-sectional study at the Paediatric Emergency Department (PED) of the Verona University Hospital, Italy, over 4 years (November 2015–November 2019). All patients aged 0–12 years who attended our PED, whose height (length) was within the PAWPER tape range, i.e. from 46 to 150 cm, were eligible for the study. We excluded all children who required emergency procedures, could not be positioned for their actual weight estimation, had congenital or acquired conditions that caused severe skeletal deformities, or were not accompanied by at least one parent.
A convenience sample of 2060 participants was predicted to be sufficient to detect a 0.1 kg (1.4 SD) difference between the actual weight and the PAWPER estimated weight with a 95% confidence limit. This sample size was adequate also for analysing the Broselow tape, the EPLS formula and the parental weight estimation methods.
Ethics statement
The study was approved by the local Ethical Committee (number of approval: 672CESC), and was conducted in accordance with the Good Practice Guidelines, the Declaration of Helsinki and current laws, ethics, and regulations. All parents signed informed consent, and assent was also obtained from children over six years of age.
Study procedure
Data were collected in our PED by physicians or certified nurses trained in the use of different tape devices and body habitus estimation.
We asked parents to report their child’s weight. The investigator visually estimated the patient body habitus and assigned a habitus score according to the PAWPER method (HS1 to HS5, HS3 being the average weight), as previously reported.6 Then, the patient’s weight was estimated using the PAWPER tape and the Broselow Paediatric Emergency tape (2011A, Edition Armstrong Medical Industries, Illinois, USA) according to the specific instructions of each tool. The child’s weight was eventually measured on a calibrated scale (SECA 769 COLUMN SCALE) to the nearest 0.1 kg after removing outer clothing and shoes to assess reference weight. Height was measured to the nearest 0.1 cm using a standard tape measure.
The EPLS weight was computed: weight (kg) = (age in years + 4) × 2.14
To assess inter-observer agreement, two different operators assessed body habitus and weight estimation with both PAWPER and Broselow methods, independently and blindly, on a subsample of 51 patients.
Statistical analysis
All analyses were performed using R statistical software version 3.6.3 (R Foundation, Vienna, Austria). The Shapiro-Wilk test was used to check the normality of the distributions. Continuous variables were analysed using nonparametric test and expressed as median and inter-quantile ranges (IQR).
Children were categorised for subgroup analysis based on their habitus score (HS). The results from the four weight estimation tools (estimated weight) were compared to the reference standard weight (true weight) using methods that analysed the bias, precision and overall accuracy of the systems.1 Bias was determined using the mean percentage error (MPE), where a negative value would be indicative of an underestimation of weight. The precision was determined using the Bland & Altman 95% limits of agreement of the MPE as well as the root mean square percentage error (RMSPE). The overall accuracy of each weight estimation system was determined by calculating the proportion of weight estimations falling within 10% (PW10) and 20% (PW20) of actual, measured weight.15 The mean percentage error (MPE) for overall estimation bias, limits of agreement (LOA), and the root mean squared percentage error (RMSPE) for the estimation of precision were calculated. Negative values indicate weight underestimation while positive values overestimation. Comparisons in terms of bias and absolute differences were done using Friedman test and multiple pairwise comparison with Wilcoxon rank sum test for paired data using Bonferroni correction.
According to previous studies, a weight estimation system was considered to perform with acceptable accuracy if it achieved PW10 > 70% and PW20 > 95%.8, 15 Difference between achieved accuracy was explored using McNemar test with Bonferroni correction. Accuracy best reflects the global performance of the weight estimation system, while the measures of bias and precision are more statistically valid for refining and calibrating it.15
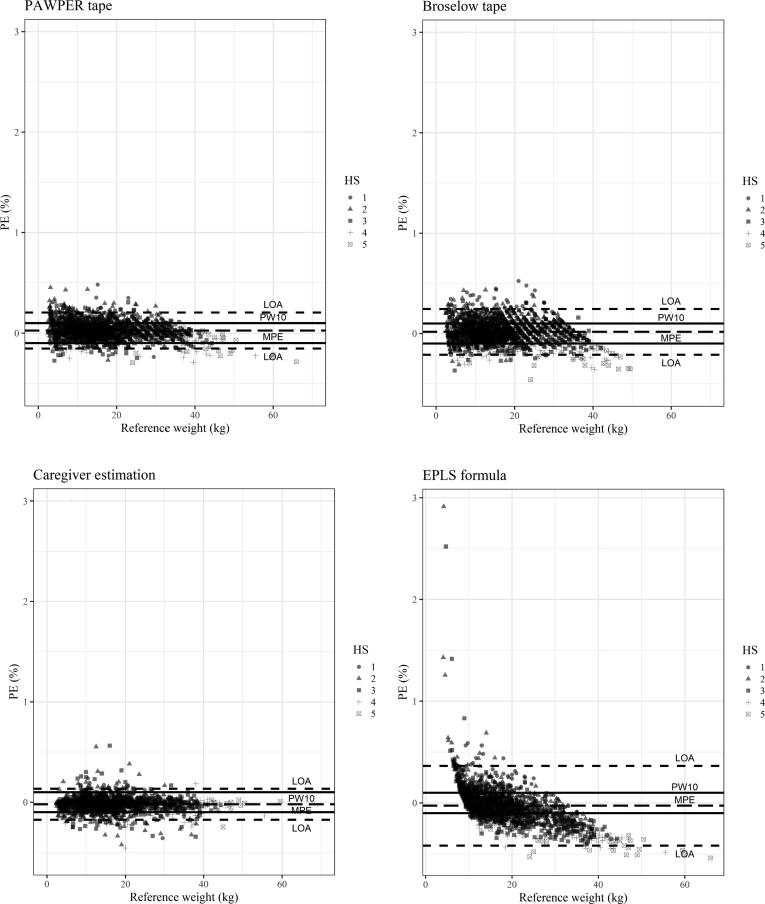
Modified Bland-Altman plots were constructed to further assess the agreement between each estimation method and the actual weight.
We used linear regression to assess the direction of the bias over the weight range.
Inter-observer agreement analysis was assessed on a subsample of 51 patients to check the agreement on assigned HS and PAWPER and Broselow tape estimated weight. Unweighted Cohen’s kappa was used to test agreement on HS, and Intra Class Correlation Coefficient (ICC) based on a single-rating, absolute-agreement, 2-way mixed-effects was used otherwise. Two-sided P < 0.05 was considered statistically significant.
Results
A total of 2060 paediatric patients were enrolled in the study.
Characteristics of the population are summarised in Table 1. Median age and weight were 3.15 years (IQR 1.08–6) and 14.9 kg (IQR 10–21.5), respectively. The length was within the PAWPER tape range in 2060 patients (100%) and within the Broselow tape range in 2019 (98%). The parental weight estimation was available for 1855 children (90%). The EPLS formula was usable only for children older than one year, including 1798 patients (87.3%).
Table 1.
Characteristics of study population in each habitus score (HS) category.
| Assigned habitus score (HS) | 1 | 2 | 3 | 4 | 5 | All |
|---|---|---|---|---|---|---|
| N (%) | 161 (7.8) | 798 (38.7) | 870 (42.2) | 185 (9.0) | 46 (2.2) | 2060 |
| Age, Median (y) (IQR) | 5 (2; 8) |
4 (1; 6) |
3 (1; 5) |
2 1; 7) |
6 (1; 9) |
3 (1; 6) |
| Height, Median (cm) (IQR) | 110 (89.7; 125.5) |
100.2 (80; 117) |
93 (76; 112) |
93 (75.8; 126) |
126 (80.2; 137.1) |
98 (78; 118) |
| Scale weight, Median (kg) (IQR) | 16.5 (11; 21.8) |
15 (9.7; 20.9) |
13.7 (9.8; 20.4) |
16 (10.4; 30) |
33.5 (10.8; 45.1) |
14.9 (10; 21.5) |
Abbreviations: N, number of non-missing value; HS, Habitus Score; BMI, Body Mass Index; IQR, Interquartile Range.
Eight hundred seventy (42.2%) patients were classified as average habitus (HS3), 959 (46.6%) as underweight (HS1 and HS2) and 231 (11.2%) as overweight (HS4 and HS5). Data on each HS category are reported in Table 1.
Measures of bias (MPE), precision (RMSPE), and accuracy (PW10, PW20) for all four weight estimation systems, both for the whole population and each habitus category subgroup, are shown in Table 2 and in the Supplemental Figure.
Table 2.
Bias and precision measures according to different weight estimation methods.
| PAWPER tape | Broselow tape | EPLS formula | Caregiver’s estimation | |||||
|---|---|---|---|---|---|---|---|---|
| All (N) | 2060 | 2019 | 1798 | 1855 | ||||
| MPE, % (LOA) | 2.6 (−15.4; 20.5) | 1.7 (−21.1; 24.4) | −2.6 (−41.6; 36.4) | −2.0 (−17.3; 13.3) | ||||
| RMSPE, % | 9.5 | 11.7 | 18.8 | 8.1 | ||||
| PW10, % (95% CI) | 75.0 | (73.0; 76.8) | 64.7 | (62.2; 66.8) | 49.9 | (47.6; 52.3) | 86.1 | (84.4; 87.6) |
| PW20, % (95% CI) | 95.0 | (93.8; 95.8) | 90.2 | (88.9; 91.5) | 78.3 | (76.3; 80.1) | 96.7 | (95.8; 97.5) |
| HS 1 | ||||||||
| MPE, % (LOA %) | 5.7 | (−13.6; 25.1) | 17.3 | (−5.0; 39.6) | 12.2 | (−20.9; 45.3) | −1.3 | (−16.6; 14.0) |
| RMSPE, % | 11.4 | 20.7 | 20.8 | 7.9 | ||||
| PW10, % (95% CI) | 69.6 | (61.8; 76.6) | 23.0 | (14.0; 27.2) | 43.5 | (29.4; 45.7) | 87.0 | (77.2; 90.1) |
| PW20, % (95% CI) | 91.3 | (85.8; 95.2) | 59.0 | (49.2; 65.3) | 70.2 | (58.6; 74.5) | 98.1 | (93.6; 99.5) |
| N | 161 | 155 | 145 | 135 | ||||
| HS 2 | ||||||||
| MPE, % (LOA %) | 4.5 | (−12.8; 21.8) | 5.3 | (−12.9; 23.6) | 2.6 | (−35.1; 40.2) | −1.9 | (−16.4; 12.7) |
| RMSPE, % | 9.9 | 10.7 | 19.4 | 7.7 | ||||
| PW10, % (95% CI) | 73.8 | (70.6; 76.8) | 66.4 | (63.0; 69.7) | 58.7 | (54.9; 62.4) | 86.5 | (83.8; 88.9) |
| PW20, % (95% CI) | 94.4 | (92.5; 95.9) | 92.2 | (90.1; 94.0) | 87.5 | (84.8; 89.9) | 96.8 | (95.3; 98.0) |
| N | 798 | 786 | 690 | 726 | ||||
| HS 3 | ||||||||
| MPE, % (LOA %) | 1.6 | (−14.7; 17.8) | −1.2 | (−18.5; 16.1) | −5.4 | (−40.3; 29.5) | −1.9 | (−18.1; 14.2) |
| RMSPE, % | 8.4 | 8.9 | 18.6 | 8.5 | ||||
| PW10, % (95% CI) | 78.5 | (75.6; 81.2) | 76.7 | (73.7; 79.5) | 51.4 | (47.8; 55) | 86.3 | (83.7; 88.6) |
| PW20, % (95% CI) | 96.6 | (95.1; 97.7) | 97.1 | (95.7; 98.1) | 80.7 | (77.7; 83.5) | 96.7 | (95.2; 97.8) |
| N | 870 | 858 | 753 | 788 | ||||
| HS 4 | ||||||||
| MPE, % (LOA %) | −1.7 | (−20.7; 17.3) | −9.6 | (−27.8; 8.6) | −16.8 | (−47.7; 14.1) | −3.0 | (−18.0; 11.9) |
| RMSPE, % | 9.8 | 13.3 | 23.0 | 8.2 | ||||
| PW10, % (95% CI) | 71.4 | (64.3; 77.7) | 50.8 | (41.9; 57.0) | 33.5 | (21.9; 40.8) | 84.9 | (78.9; 89.7) |
| PW20, % (95% CI) | 95.1 | (91.0; 97.7) | 88.1 | (82.5; 92.4) | 56.2 | (48.7; 63.5) | 96.2 | (92.3; 98.5) |
| N | 185 | 180 | 172 | 170 | ||||
| HS 5 | ||||||||
| MPE, % (LOA %) | −4.6 | (−28.6; 19.5) | −19.4 | (−41.9; 3.1) | −34.5 | (−62.1; 6.8) | −3.1 | (−15.4; 9.2) |
| RMSPE, % | 13.0 | 22.5 | 37.2 | 6.9 | ||||
| PW10, % (95% CI) | 60.9 | (45.4; 74.9) | 17.5 | (16.0; 43.4) | 7.9 | (1.7; 21.4) | 91.7 | (77.5; 98.2) |
| PW20, % (95% CI) | 82.6 | (68.6; 92.2) | 42.5 | (27.0; 59.1) | 18.4 | (7.7; 34.3) | 94.4 | (81.3; 99.3) |
| N | 46 | 40 | 38 | 36 | ||||
N refers to the number of non-missing values.
Abbreviations: PW10, Percentage Error Within 10%; PW20, Percentage Error Within 20%; MPE, Mean Percentage Error; LOA, Limits of Agreement; RMSPE, Root Mean Square Percentage Error; CI, Confidence Intervals.
Overall, the PAWPER tape was accurate in the study population (PW10 75%, PW20 95.0%), and it maintained its accuracy throughout all habitus sizes except for the two extreme categories (HS1 and HS5), where only one parameter of accuracy was nearly reached (PW10 69.6% for HS1, PW20 82.6% for HS5).
In the overall study population the PAWPER tape was more accurate (PW10 = 75.0% vs 64.7%; PW20 = 95.0% vs 90.4%, p adjusted <0.001) and precise (RMSPE 9.5% vs 11.7%, p adjusted <0.001) than the Broselow tape, while the MPE of PAWPER was higher (2.6 vs 1.6; p adjusted <0.001).
As for the habitus subgroups, the PAWPER’s MPE for HS3 was higher than the Broselow’s (1.6 vs −1.2, respectively), whilst the PAWPER MPE was lower in all other categories.
Overall, the parents’ weight estimation was the most accurate (PW10 87.5%, PW20 97%) and precise (RMSPE 7.7%) method compared to the other tools (p adjusted <0.001 for each comparison), also in the habitus sub-categories.
Conversely, the age-based EPLS formula was the least accurate (PW10 56.3%; PW20 81%) and precise (RMSPE 18.8%) compared to the other methods (p adjusted <0.001 for each comparison).
Bias tended to decrease in all four estimation tools as the reference weight increased, especially when using the EPLS formula (−0.38; 95% CI: −0.40, −0.37).
The inter-rater agreement for assessing the body habitus, tested in a subsample of 51 children, showed an agreement of 84.3%, with a Cohen’s kappa coefficient of 0.76 (95% CI: 0.61–0.91). There was a high degree of agreement in the assigned weight for both the PAWPER and the Broselow tape. The ICC was 0.993 (95% CI 0.995–0.998) and 0.996 (95% CI 0.993–0.998), respectively.
Fig. 1 illustrates the modified Bland-Altman representation of agreement between the actual measured weight and the estimated one, in all four systems.
Fig. 1.
Accuracy of the four weight estimation methods in the entire population and the five HS sub-categories. Modified Bland and Altman plots of Percentage Error (PE) against actual weight for each weight estimation tool. The continuous line represents the mean percentage error, and the short-dashed lines represent the 95% limits of agreement. The chart also shows the proportion of weight estimations falling within 10% of actual weight (PW10, long-dashed line).
Discussion
In 2021, the European Resuscitation Council (ERC) released the new EPLS guidelines, which report special consideration for using weight estimation tools during paediatric emergencies to facilitate accurate drug dosage calculation.16 They encourage implementing systems that correct for individual body size, a crucial factor for reliable weight estimation in children. Indeed, either over- or under-weight approximation can lead to suboptimal medication dosage and related morbidity and mortality.10, 18
Of note, EPLS guidelines indicate the PAWPER tape as a quick and easy weight estimation tool that corrects length-based approximation with body habitus assessment, possibly providing a more reliable weight estimation than mono-dimensional systems, such as the Broselow tape or age-based formulas.16
To date, the PAWPER tape has been validated in South Africa,6, 7, 8 USA,12 Nepal13 and Australia.10 To our knowledge, the present study is the first that assessed the reliability of the PAWPER tape in a European centre and in a large paediatric cohort, which included more than 2000 children, allowing us to obtain precise estimates.
In the present study, the PAWPER tape completely satisfied the overall accuracy criteria. However, accuracy benchmark was not achieved in extreme overweight habitus (HS5) while it was almost achieved in children with extreme small habitus (HS1). These findings are in line with other studies performed in populations with relatively high obesity rate, as observed in the USA and inner-cities,6, 12, 13, 19 where the studied samples reflected the general higher prevalence of overweight.1 Previous reports on the PAWPER tape showed high accuracy (PW10 > 80%) in populations with a low prevalence of obesity, but lower accuracy (PW10 60–70%) in populations with high incidence of obesity.7
As reported by Garcia et al., we observed that the PAWPER’s accuracy decreased as the reference weight increased. Indeed, weight has always been challenging to estimate in obese children and other authors confirmed obesity as the main variable influencing weight estimation and the likely cause of inaccuracy.1, 12
New versions of the PAWER tape have been developed in the last few years to overcome this critical bias, namely the PAWPER XL and the PAWPER-XL-MAC.15, 16
For the first time, our study compared the trustworthiness of the PAWPER tape, the Broselow tape, the parents’ estimation and the EPLS formula in the same cohort. Although the PAWPER tape was less reliable than the parents’ weight estimate, its accuracy was superior to mono-dimensional systems, i.e. the Broselow tape and age-based formulas, considering both the overall sample and the habitus subgroups.
The PAWPER tape outperformed the Broselow tape in the overall group and the habitus subgroups. In the whole population, the Broselow tape estimation fell within 10% of actual weight in 65.4% of cases, which is comparable to other published data.6, 8, 10 When analyzing the single subcategories, the Broselow tape performed well only in the average weight group (HS3), while it showed low accuracy and precision in under- and over-weight children.
Overall, the PAWPER method was less biased than the Broselow tool, slightly overestimating the actual weight. However, the mean difference in weight was less than 200 grams, thus scarcely affecting any drug dosage calculation in clinical practice. Conversely, the Broselow tape was significantly less precise than the PAWPER in children with different sizes from average, confirming its limited reliability in these latter categories.
In line with the ERC guidelines,17 our study confirmed that the parents’ weight estimation is the most accurate and precise method. However, since parents may not be present or easily reachable, or could not even remember their own child’s weight, particularly in emergency and stressful circumstances, it is prudent to implement alternative methods to infer this essential data reliably.
Our study suggests that the PAWPER tape may be an accurate and precise tool to assess weight in children of any size and habitus, except for obese subjects, similarly to other methods.
Conversely, the age-based EPLS formula performed the worst among the various tools, yielding the highest bias and the lowest precision, and not reaching the accuracy benchmark in any subgroups. Similarly, Wells et al. found that none of the age-based formulas could predict the actual body weight with reasonable accuracy, especially in obese subjects.18, 19 Our data reinforce the ERC guidelines that discourage using age-based formulas in paediatric clinical settings.
Similar to other methods, the PAWPER tape is a subjective tool as a single evaluator usually defines the habitus status. Nonetheless, it introduces specific criteria for different habitus categories. Furthermore, the inter-observer reliability analysis for the determination of the HS revealed an excellent value (k: 0.895; p < 0.001). This result was achieved after brief training offered to doctors, trainees and other PED health professionals. Our data indicate that the PAWPER tape is a reliable and reproducible weight estimation method to implement in ED settings, even in those with a rapid turnover of doctors and nurses.
Limitations
Our study has several limitations. First, the demographical characterization of the study population was incomplete as some data such as ethnicity and sex were missing, therefore precluding BMI-for-age centiles or z-scores calculations.
Second, as we included only subjects up to the age of 12 and 150 cm of length, i.e. the upper limit of the PAWPER tape, we cannot draw conclusions on what number of children are too tall for the tape. Recently, a newer version of the tape, namely the PAWPER XL tape, has been introduced to estimate weight in taller children (up to 180 cm) and severely obese children.11, 16
Third as the present study started in 2015, we used an old version of the Broselow tape throughout the study, for consistency reasons. Since the Broselow tape has been changed substantially in 2017 to provide heavier estimates at any length, our results may not be confirmed when considering the newer versions of the Broselow tape.
Fourth, the study population was very young, thus our results might not be generalizable to an older population.
Finally, like other authors,6 we did not enrol patients in need of emergency treatment in our study, therefore we could not assess the precision and accuracy of the PAWPER and other weight estimation methods in children presenting to our PED in critical conditions, a special population that could benefit the most from the use of these tools.
Nonetheless, we believe that comparing four different weight estimation tools in the same large cohort of children has allowed for more precise estimation and provided additional information about the reliability of each method.
Conclusions
In our study, although parental weight estimation turned out to be the most accurate and precise method, we have shown that PAWPER tape can be an accurate method for weight estimation in children visiting an Italian Paediatric Emergency Department, showing excellent inter-rater reliability. Additionally, compared with two other tools for weight estimation in the same sample (i.e. Broselow tape and age-based EPALS formula), the PAWPER tape performed significantly better than length and age-based tools, providing good accuracy and precision even in subjects with non-average habitus, with the exception of obese individuals. Of note, the age-based EPLS formula was not reliable for estimating weight in all subcategories of habitus.
Because parental estimation may not be readily available during resuscitation or emergencies, alternative and reliable weight assessment tools are needed in these situations. Our data showed that the PAWPER tape is an accurate weight estimation tool in non-critically ill children visiting an Emergency Department. However, further studies are warranted to evaluate the validity of the PAWPER tape even in emergency clinical conditions.
CRediT authorship contribution statement
Davide Silvagni: Conceptualization, Methodology, Investigation, Formal analysis, Writing – original draft, Writing – review & editing. Laura Baggio: Investigation, Methodology, Formal analysis, Writing – original draft, Writing – review & editing. Cristina Mazzi: Methodology, Formal analysis, Writing – review & editing. Giorgio Cuffaro: Investigation, Writing – review & editing. Silvia Carlassara: Investigation, Writing – review & editing. Simona Spada: Investigation, Writing – review & editing. Paolo Biban: .
Acknowledgments
Acknowledgement
We would like to thank the clinicians and staff of the Pediatric Emergency Department of the University Hospital of Verona, for indispensable time and dedication to this project.
Authors’ statement
We declare no competing interests.
Funding
No funding was received for this manuscript.
Footnotes
Supplementary material to this article can be found online at https://doi.org/10.1016/j.resplu.2022.100301.
Appendix A. Supplementary material
The following are the Supplementary material to this article:
References
- 1.Garcia C.M., Meltzer J.A., Chan K.N., Cunningham S.J. A validation study of the PAWPER (Pediatric Advanced Weight Prediction in the Emergency Room) tape-A new weight estimation tool. J Pediatr. 2015;167:173–177.e1. doi: 10.1016/j.jpeds.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 2.Remick K., Gausche-Hill M., Joseph M.M., Brown K., Snow S.K., Wright J.L. American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, Section on Surgery; American college of Emergency Physicians, Pediatric Emergency Medicine Committee; Emergency Nurses Association, Pediatric Committee; Pediatric Readiness in the Emergency Department; Policy statement; Organizational Principles to Guide and Define the Child Health Care System and/or Improve the Health of All Children. Pediatric Readiness in the Emergency Department. J Emerg Nurs. 2019;45:e3–e18. [Google Scholar]
- 3.Wells M., Goldstein L.N., Bentley A. The accuracy of paediatric weight estimation during simulated emergencies: The effects of patient position, patient cooperation, and human errors. Afr J Emerg Med. 2018;8:43–50. doi: 10.1016/j.afjem.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young K.D., Korotzer N.C. Weight estimation methods in children: A systematic review. Ann Emerg Med. 2016;68:441–451. doi: 10.1016/j.annemergmed.2016.02.043. [DOI] [PubMed] [Google Scholar]
- 5.Wells M., Goldstein L.N., Bentley A., et al. The accuracy of the Broselow tape as a weight estimation tool and a drug-dosing guide – A systematic review and meta-analysis. Resuscitation. 2017;121:9–33. doi: 10.1016/j.resuscitation.2017.09.026. [DOI] [PubMed] [Google Scholar]
- 6.Wells M., Coovadia A., Kramer E., Goldstein L. The PAWPER tape: A new concept tape-based device that increases the accuracy of weight estimation in children through the inclusion of a modifier based on body habitus. Resuscitation. 2013;84:227–232. doi: 10.1016/j.resuscitation.2012.05.028. [DOI] [PubMed] [Google Scholar]
- 7.Wells M., Goldstein L.N., Bentley A. A systematic review and meta-analysis of the accuracy of weight estimation systems used in paediatric emergency care in developing countries. Afr J Emerg Med. 2017;7(Suppl):S36–S54. doi: 10.1016/j.afjem.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wells M., Goldstein L.N., Bentley A. The accuracy of emergency weight estimation systems in children – a systematic review and meta-analysis. Int J Emerg Med. 2017;10:29. doi: 10.1186/s12245-017-0156-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells M., Goldstein L. Drug dosing errors in simulated paediatric emergencies – Comprehensive dosing guides outperform length-based tapes with precalculated drug doses. Afr J Emerg Med. 2020;10:74–80. doi: 10.1016/j.afjem.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O'Leary F., John-Denny B., McGarvey K., et al. Estimating the weight of ethnically diverse children attending an Australian emergency department: a prospective, blinded, comparison of age-based and length-based tools including Mercy, PAWPER and Broselow. Arch Dis Child. 2017;102:46–52. doi: 10.1136/archdischild-2016-310917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manyoni M.J., Goldstein L.N., Wells M. A comparison of four weight estimation systems for paediatric resuscitation. S Afr J Surg. 2019;57:40–46. [PubMed] [Google Scholar]
- 12.Chavez H., Peterson R.E., Lo K., Arel M. Weight estimation in an inner-city pediatric ED: the effect of obesity. Am J Emerg Med. 2015;33:1364–1367. doi: 10.1016/j.ajem.2015.07.040. [DOI] [PubMed] [Google Scholar]
- 13.Shrestha K., Subedi P., Pandey O., et al. Estimating the weight of children in Nepal by Broselow, PAWPER XL and Mercy method. World J Emerg Med. 2018;9:276–281. doi: 10.5847/wjem.j.1920-8642.2018.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.ERC: EPLS – European Pediatric Life Support: ERC manual for health care workers dealing with paediatric resuscitation; 2015 Edition.
- 15.Wells M. A validation of the PAWPER XL-MAC tape for total body weight estimation in preschool children from low- and middle-income countries. PLoS One. 2019;14:e0210332. doi: 10.1371/journal.pone.0210332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells M., Goldstein L., Bentley A. A validation study of the PAWPER XL tape: accurate estimation of both total and ideal body weight in children up to 16 years of age. Trauma Emergency Care. 2017;2:1–8. [Google Scholar]
- 17.Van de Voorde P., Turner N.M., Djakow J., et al. European resuscitation council guidelines 2021: Paediatric life support. Resuscitation. 2021;161:327–387. doi: 10.1016/j.resuscitation.2021.02.015. [DOI] [PubMed] [Google Scholar]
- 18.Wells M., Goldstein L.N. How and why paediatric weight estimation systems fail – A body composition study. Cureus. 2020;12:e7198. doi: 10.7759/cureus.7198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wells M., Goldstein L.N. Optimising emergency weight estimation in underweight and obese children: the accuracy of estimations of total body weight and ideal body weight. Eur J Emerg Med. 2019;26:301–307. doi: 10.1097/MEJ.0000000000000561. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.