Abstract
Objectives
Although inherited retinal disorders (IRDs) related to the gene encoding the retinal pigment epithelium 65kD protein (RPE65) significantly impact the vision-related quality of life (VRQoL), their emotional and social aspects remain poorly investigated in Italy. Narrative Medicine (NM) reveals the more intimate aspects of the illness experience, providing insights into clinical practice.
Design and setting
This NM project was conducted in Italy between July and December 2020 and involved five eye clinics specialised in IRDs. Illness plots and parallel charts, together with a sociodemographic survey, were collected through the project’s website; remote in-depth interviews were also conducted. Narratives and interviews were analysed through NVivo software and interpretive coding.
Participants
3 paediatric and 5 adult patients and eight caregivers participated in the project; 11 retinologists globally wrote 27 parallel charts; 5 professionals from hospital-based multidisciplinary teams and one patient association member were interviewed.
Results
Findings confirmed that RPE65-related IRDs impact VRQoL in terms of activities and mobility limitations. The emotional aspects emerged as crucial in the clinical encounter and as informative on IRD management challenges and real-life experiences, while psychological support was addressed as critical from clinical diagnosis throughout the care pathway for both patients and caregivers; the need for an IRDs ‘culture’ emerged to acknowledge these conditions, and therefore, promoting diversity within society.
Conclusions
The project was the first effort to investigate the impact of RPE65-related IRDs on the illness experience through NM, concomitantly addressing the perspectives of paediatric and adult patients, caregivers and healthcare professionals and provided preliminary insights for the knowledge of RPE65-related IRDs and the clinical practice.
Keywords: Paediatric ophthalmology, Medical retina, QUALITATIVE RESEARCH
STRENGTHS AND LIMITATIONS OF THIS STUDY.
Inclusion of paediatric patients’ perspectives.
Integration of patients’ and caregivers’ perspectives to that of retinologists and hospital-based multidisciplinary professionals.
Participants did not equally represent the geographical areas of Italy.
Restrictions due to Sars-CoV-2 pandemic impacted the number of patients visiting the clinics, so involved healthcare professionals had to engage them virtually.
Patients and caregivers participated in the project on a voluntary basis, and SARS-CoV-2 pandemic could have created a bias on the motivation to join the research.
Introduction
Affecting about 1 in 2–3000 people globally,1 inherited retinal disorders (IRDs) constitute a group of clinically and genetically heterogeneous degenerative conditions in which gene mutations affect the proteins necessary to functional vision.2 A progressive loss of photoreceptor cells and an impairment for visual function characterise the IRDs related to mutations involving the gene encoding the retinal pigment epithelium 65kD protein (RPE65) and gradually lead to an irreversible visual decline,3 and potentially to blindness4; Leber congenital amaurosis and retinitis pigmentosa (RP) represent the most common forms.5 6
Age of onset ranges from early childhood to middle age; visual impairment at low light levels, night blindness and nystagmus are the early symptoms, followed by an increasing deterioration of visual acuity and peripheral vision.7 While gene therapy represents a promising scenario for treating these conditions,3 8 IRDs management has been mainly support-oriented and focused on monitoring, counselling and education.3
RPE65-related IRDs significantly impact patients in daily activities,9 with implications for their sense of identity10 and autonomy management11; previous studies associate visual impairment with lower social engaging ability,12 self-confidence and vision-related quality of life (VRQoL),13 as well as with higher levels of depression.14 15
Against this backdrop, other studies and reviews16 17 suggest that a holistic and multidisciplinary approach—also addressing IRDs emotional and social aspects—is crucial to support patients and their caregivers.
The WHO has acknowledged narrative research as informative to address the illness experience18 in leading clinical practice19; a keen focus on narratives resulted in better patient care also in clinical genetics practice.20 As described in similar studies,21 Narrative Medicine (NM) is based on illness narratives22 and aims to integrate the disease-centred approach, related to the biomedical sphere, with the illness-centred and sickness-centred approaches, focusing on the individual and social experience of a condition,23 respectively. NM addresses the possible interventions on a specific disorder by integrating the perspectives of all the actors involved in the care pathway,24 and its findings have been increasingly used to improve the quality of care in clinical practice.25 26
The NM project ‘BIRDS—The Beat of IRD Stories’ investigated the RPE65-related IRDs illness experience through the analysis of narratives (1) to reveal the practical, emotional and social issues linked to these conditions as experienced by patients, caregivers and healthcare professionals, and (2) to understand the patient’s journey and expectations regarding the gene therapy, to finally provide insights to foster the knowledge on RPE65-related IRDs and clinical practice.
The present research article focuses on the first goal (1); another study addressed the second one.27 Although other studies integrated the perspectives of both patients and caregivers,28 29 to the best of our knowledge, this is the first project that also engages the retinologists and hospital-based multidisciplinary professionals (MDTs) in investigating the RPE65-related IRDs illness experience in Italy.
Methods
Research design and setting
The project was conducted in Italy between July and December 2020 and targeted paediatric and adult patients with an RPE65-related IRD, their caregivers, retinologists and MDT professionals involved in their care pathway. Participants were enrolled from five eye clinics specialised in IRDs (online supplemental file 1) across Italy. In July 2020, the steering committee—composed of five retinologists working in these centres and a patient association (PA) member—participated in an online meeting conducted by researchers from Istituto Studi Direzionali (ISTUD), Healthcare Area to be trained in NM and to discuss the project’s goals and design; the Steering Committee, together with other IRD specialists from these centres, were then invited to engage patients and caregivers in participating in the research by accessing the project’s webpage http://www.medicinanarrativa.eu/birds.
bmjopen-2022-061080supp001.pdf (44.7KB, pdf)
A clinical RPE65-related IRD diagnosis, without a minimum length of follow-up time postdiagnosis, or the caregiving of a person with an RPE65-related IRD constituted the eligibility criteria for patients and caregivers, as well as the willingness to share their illness experience; however, the ability to write or communicate in Italian was critical for the inclusion.
Data collection
Researchers followed the Web Content Accessibility Guidelines 2.130 to ensure survey accessibility. Patients were invited to share their narratives either by writing or recording an audio file; also, caregivers were allowed to support paediatric patients in writing their narratives following the project’s data collection tools. Narratives were anonymously collected through the Alchemer platform, available on the project’s webpage. Afterwards, raw narratives were downloaded as Microsoft Excel spreadsheets.
A sociodemographic survey and an illness plot,31 namely, a plot related to the illness experience, were addressed to patients and caregivers; evocative and open words characterised the illness plot to facilitate individual expression32 and chronologically guide the narrative to identify changes over time. The retinologists’ caring experience was gathered through the parallel chart,33 that is, a personal notebook, parallel to the clinical one, in which to write down thoughts and feelings in a plain language.34 The patients described in parallel charts could not coincide with patients participating in the project. Overall, these investigation tools (online supplemental file 2) addressed two common aspects: (1) the personal and social experience of RPE65-related IRDs from early symptoms onwards and (2) the VRQoL perception and the current daily life with RPE65-related IRDs.
bmjopen-2022-061080supp002.pdf (74.7KB, pdf)
Furthermore, in-depth interviews35 were conducted with MDT professionals involved in IRD care pathway and a PA member, caregiver of a person with an RPE65-related IRD, to facilitate the emergence of patient-related and care pathway-related issues further and to delve into organisational aspects without proposing to these professionals the introspective experience of writing; the interviewees approved the transcripts before the analysis.
The investigation tools were designed by two ISTUD researchers with different academic backgrounds and reviewed by the steering committee to reduce any cognitive bias.
Patient and public involvement
Researchers did not engage patients and caregivers in (1) developing the research design and tools, (2) interpreting and discussing the results and (3) contributing to the writing or editing of this document.
Analysis
Researchers analysed the sociodemographic data through descriptive statistics; answering survey questions or filling in fields in the illness plots and parallel charts was not mandatory, so sample size may vary. Narratives were entered into NVivo software36 for coding and content analysis.37 Three narratives for each group and one in-depth interview were collectively coded to assess the consistency across team members; then, each narrative and in-depth interview were separately coded and reviewed during weekly peer debriefings to limit any interpretation bias.
Open interpretive coding was employed to identify and analyse the emerging contents in all narratives and in-depth interviews. Moreover, adult patients’ and caregivers’ narratives and parallel charts were classified following: (1) Kleinman’s classification,23 which identifies disease-related, illness-related and sickness-related aspects in narratives, respectively, concerning the biomedical description of a condition, its personal and emotional experience, and its social and cultural perception; (2) Bury’s classification,38 which distinguishes among contingent narratives (concerning a condition’s immediate effects on daily life), core narratives (connecting the illness experience to deeper and cultural levels of meaning) and moral narratives (highlighting an evaluative and social dimension). Researchers did not apply retrospective classifications of narratives to paediatric patients’ narratives since their caregivers’ in-writing support could have affected the narrative style and the word choice.
Researchers asked the participants to describe RPE65-related IRDs through a metaphor to trace spontaneous meaning associations related to the illness experience through daily language.39
The steering committee discussed the results to address the emerged issues and data interpretation collectively. Researchers followed the Standards for Reporting Qualitative Research guidelines.40
Results
Three paediatric and 5 early-onset adult patients and 8 caregivers participated in the project, as well as 11 retinologists specialised in IRDs, who wrote 27 parallel charts; all patients chose to share their experience in writing. In-depth interviews were conducted with five MDT professionals—that is, two genetic counsellors, two psychologists and one orientation and mobility (O&M) instructor—and one PA member. Table 1 summarises the sociodemographic data of participants, including non-responders as a separate category.
Table 1.
Sociodemographic data of participants
| Patients (N=8) | Caregivers (N=8) | Patients in parallel charts (N=27) | Retinologists (N=11) | Participants in in-depth interviews (N=6) | |
| Gender | |||||
| Female | 6 (75%) | 6 (75%) | 12 (44%) | 5 (45%) | 5 (83%) |
| Male | 2 (25%) | 2 (25%) | 15 (56%) | 6 (55%) | 1 (17%) |
| Age (years) | |||||
| Median (range) | 26 (8–63) | 44 (31–70) | 17 (5–65) | 42 (32–64) | 54 (49–67) |
| Geographic residence | |||||
| Northern Italy | 3 (38%) | 2 (24%) | – | – | 2 (33%) |
| Central Italy | 4 (50%) | 4 (50%) | – | 8 (73%) | 4 (67%) |
| Southern Italy | 1 (12%) | 1 (13%) | – | 3 (27%) | – |
| Non-responders | – | 1 (13%) | – | – | – |
| Education | |||||
| Elementary school | 1 (12%) | – | 7 (26%) | – | – |
| Middle school | – | 1 (12%) | 4 (15%) | – | – |
| High school | 1 (12%) | 3 (38%) | 4 (15%) | – | – |
| Bachelor/master | 3 (38%) | 3 (38%) | 3 (11%) | – | – |
| Non-responders | 3 (38%) | 1 (12%) | 9 (33%) | – | – |
| Employment status | |||||
| Student | 4 (50%) | – | 16 (59%) | – | – |
| Working | 3 (38%) | 6 (76%) | 10 (37%) | – | – |
| Not working | – | – | – | – | – |
| Retired | – | 1 (12%) | 1 (4%) | – | – |
| Non-responders | 1 (12%) | 1 (12%) | – | – | – |
| Marital state | |||||
| Single | 6 (75%) | 1 (12%) | 18 (67%) | – | – |
| Married | 2 (25%) | 5 (64%) | 7 (26%) | – | – |
| Separated | – | 1 (12%) | 2 (7%) | – | – |
| Non-responders | – | 1 (12%) | – | – | – |
| Professional activity (years) | |||||
| Median (range) | – | – | – | 16 (6–41) | 23 (19–35) |
| Specialisation | |||||
| Ophthalmology | – | – | – | 8 (73%) | 1 (17%) |
| Paediatric ophthalmology | – | – | – | 1 (9%) | |
| Orthoptics | – | – | – | 2 (18%) | |
| Medical genetics | 1 (17%) | ||||
| O&M training | 1 (17%) | ||||
| Psychology | 2 (32%) | ||||
| Other | – | 1 (17%) | |||
| Workplace | |||||
| Hospital | – | – | – | 2 (18%) | |
| University Hospital | – | – | – | 9 (82%) | 2 (33%) |
| Other | 4 (67%) |
Data are presented as n (%) or median (range).
O&M, orientation and mobility.
Results are presented along four main lines: (1) the RPE65-related IRDs experience analysed through narrative classifications and metaphors; (2) the emotional issues before and on the clinical diagnosis; (3) VRQoL perception, the condition’s impact on daily life and participants’ expectations; (4) insights from in-depth interviews. Narratives informed (1) and (2), while (3) was investigated through both narratives and quantitative data from the survey; in-depth interviews alone informed (4). Figures 1–3 and tables 2–5 provide quotes from the narratives, while four narratives are available in English in online supplemental file 3; we reduced the risk of reidentification by applying different codes from those used to identify participants during data collection.
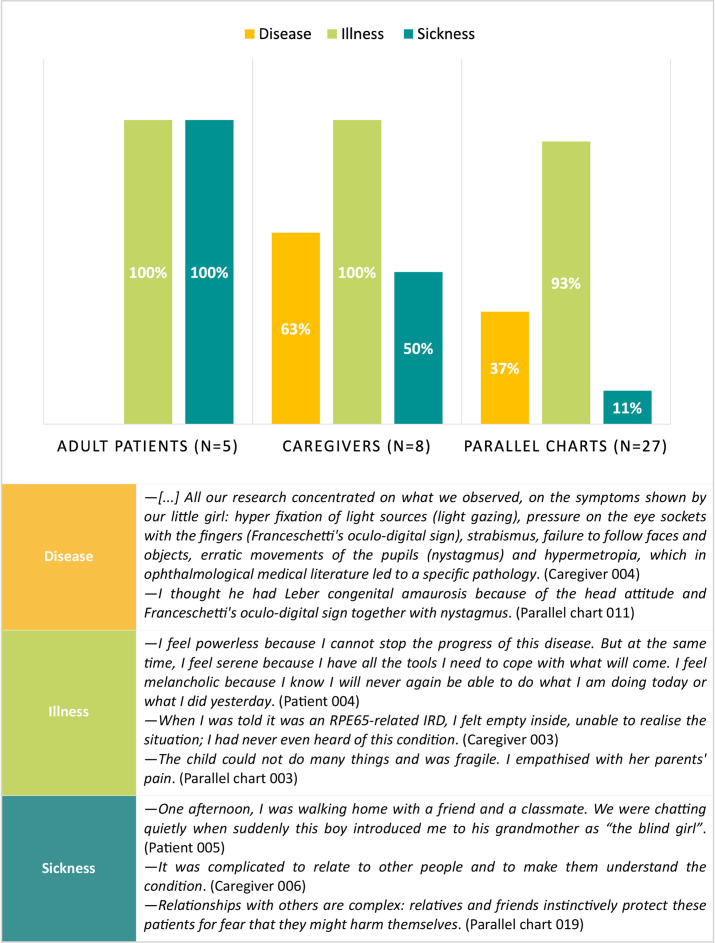
Figure 1.
Kleinman’s classification: distribution and quotes from narratives.
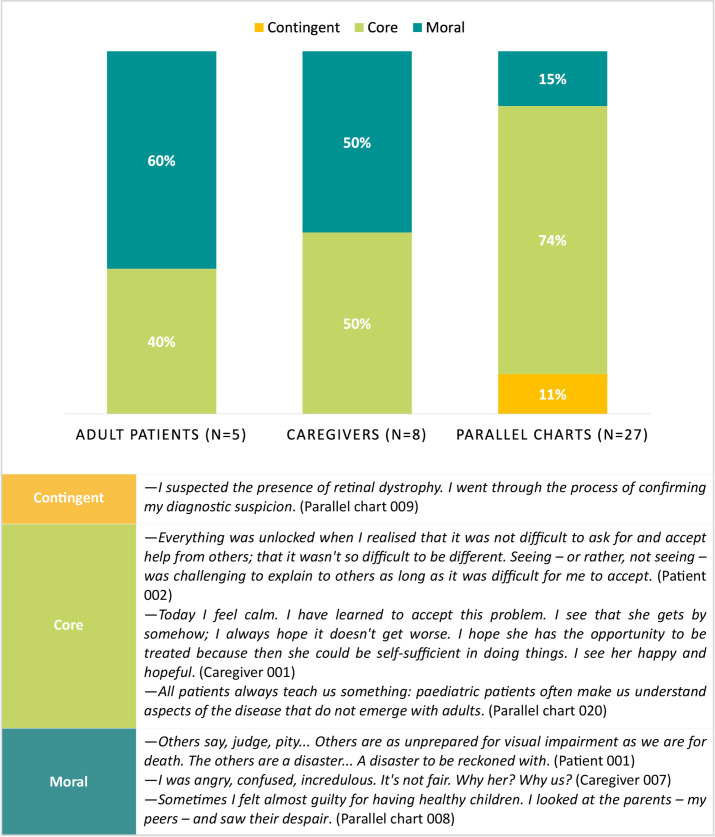
Figure 2.
Bury’s classification: distribution and quotes from narratives.
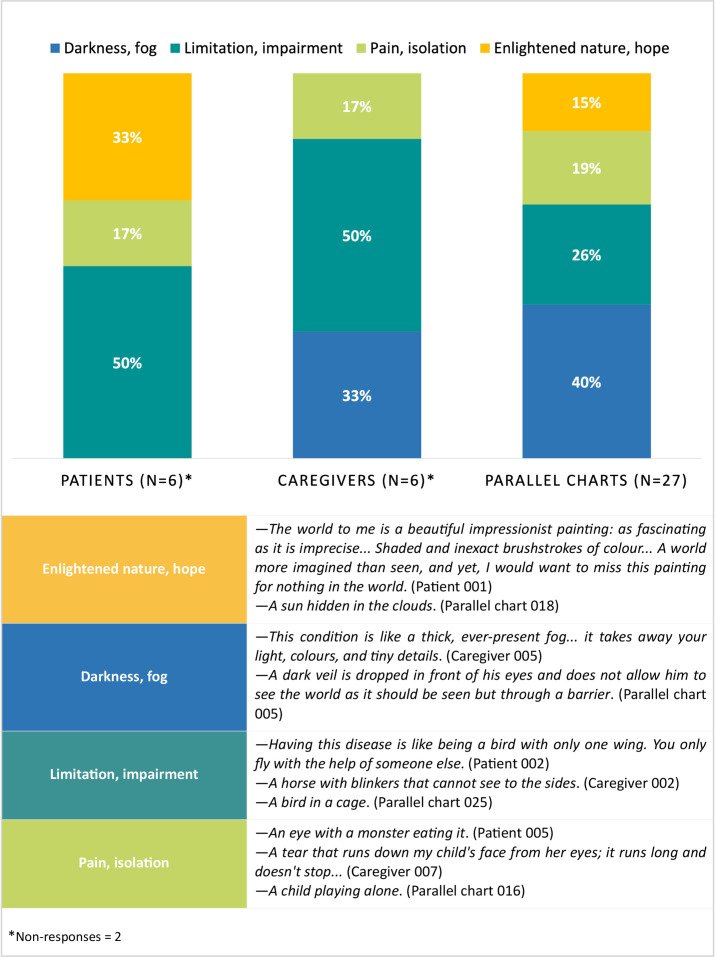
Figure 3.
Metaphors used to describe RPE65-related IRDs: distribution and examples. IRDs, inherited retinal disorders; RPE65, retinal pigment epithelium 65kD protein.
Table 2.
Patients’ and caregivers’ emotions before and at the diagnosis of RPE65-related IRD
| Patients | ||
| Before diagnosis | Normal (38%) | – I have always felt normal. I never had the feeling that the slight differences I noticed could be a problem, or part of a problem. (Patient 004) |
| Uncomfortable (62%) | – I felt their disappointment, their concern… They were not happy with me, and I felt wrong, because my answers were wrong. I couldn’t see, and I couldn’t help but guess… (Patient 002) | |
| At diagnosis | Identification (29%) | – Somehow, finally identifying the problem brought me out of my limbo: for years, I had been the child who saw little during the day and who couldn’t see at night; now I finally knew why. I became familiar with terms such as “blindness”, “low vision”, or “disability”, concepts that would later radically change my future. (Patient 001) |
| Neutral (71%) | – Honestly, I wasn’t much affected. The disease has always been part of me. I grew up with it, I gradually got used to it. (Patient 004) | |
| Caregivers | ||
| Before diagnosis | Worry 50% | – I felt helpless, terrified, and afraid. (Caregiver 003) |
| Helplessness 50% | – I felt terrible, because I understood the challenge, but I couldn’t do much, except hold her hand. (Caregiver 006) | |
| At diagnosis | Hopelessness 75% | – I felt terrible. It’s something you don’t expect: a hereditary disease of a genetic nature in a family where there were no known cases seems impossible. (Caregiver 008) |
| Fear for children 25% | – In the beginning, it scared me: the fear that our other children could suffer from a similar condition. Our anxiety decreased with time: I saw her, I saw she was restricted but not blocked, which gave me courage. (Caregiver 005) | |
IRD, inherited retinal disorder; RPE65, retinal pigment epithelium 65kD protein.
Table 3.
Retinologists’ emotions at first visit and at the beginning of the care relationship
| At the first visit | A challenge for both clinician and patient 37% | – I thought that this visit was a challenge for us both: for her, it meant undergoing new tests and knowing the results; for me, it meant dedicating myself to another person to whom I could dedicate my care. I also thought that she might have access to treatment in the future, and I was ready and willing to facilitate this.(Parallel chart 007) |
| Hope 30% | – I thought it was essential to follow her carefully from a clinical perspective, and that it was imperative to have a genetic test. When she showed it to me, I realized that she had a treatable mutation, which gave me hope.(Parallel chart 015) | |
| Sorrow 22% | – Poor child, he is not living his life like his healthy peers.(Parallel chart 002) | |
| Empathy with patient or caregiver 11% | – I thought that he was the same age as me, but that he had a completely different visual situation from mine. I stepped out of the treating doctor’s shoes, and I found myself projected into an essentially human dimension. I put myself in her shoes and listened to her story with my heart as well as my ears.(Parallel chart 006) | |
| At the beginning of the care at the beginning of the care relationship | Emotional involvement and motivation 58% | – I was impressed by what I was seeing, powerless but at the same time full of motivation and hope. I knew the child’s mutation, and I imagined that—given his young age—he might have a therapeutic chance. I leveraged this last point in my talk with his parents, trying to give them a cautious hope and making them understand that this specific genetic mutation meant being severely visually impaired, but also the possibility of being cured in a not distant future.(Parallel chart 005) |
| Helplessness 30% | – Despite my knowledge, I felt powerless, unable to give immediate and concrete answers to many of his practical problems.(Parallel chart 019) | |
| Sense of guilt 12% | – I felt ashamed… I’m lucky, I think I have a successful life, and yet I often get irritated or discouraged by stupid things, while he always seems happy to live his life, despite everything.(Parallel chart 021) |
Table 4.
The current feelings of participants: distribution and quotes from narratives
| Patients | |
| Uncertainty 25% | – Today I feel poised between light and shadow. I feel like someone who chases a ball without ever reaching it. I am 42 years old, and I have spent my life being told that science works miracles, and that life is long, and that progress for me will come soon. I am 42, though, not 10… My sight is progressively worsening. I feel tangible differences over a few months, days in some cases. I can remember things from a few months ago, visual details that I no longer see today. In fact, it’s not that I don’t see them: I perceive them as covered by a veil. Glossy… Like old photographs, but far less poetic… (Patient 001) |
| Discomfort, sadness 25% | – I feel sad: when mum or dad are driving, in the afternoon or in the evening, I do not see the road, I only notice a few lampposts. (Patient 007) |
| Serenity, hope 50% | – Today I feel hopeful for the future. I try every day to accept my challenges and to live with serenity. If the situation gets worse, I know that I will have to find different ways. It will be hard, maybe even unpleasant, but it will be possible. If the situation improves, thanks to gene therapy, I will be pleased. (Patient 002) |
| Caregivers | |
| Acceptance 38% | – I feel I am an integral part of my son’s life. I live in symbiosis with him. Everything is more manageable: I manage to find solutions quite easily to meet his needs during his constant difficulties. Let’s say that everything is always about having an obstacle to overcome… It’s never easy, and sometimes it’s mentally exhausting. (Caregiver 003) |
| More serenity 62% | – I know that we are doing our best to understand her condition better and, if possible, to start the therapy. The knowledge that we are doing our best brings me serenity. (Caregiver 005) |
| Retinologists | |
| Positive feelings 44% | —I’m feeling comfortable. Able to do my job without hiding my human side. Open to questions and ready to give competent and precise answers. Willing to help but aware of my limits, my role, and my possibilities. (Parallel chart 006) |
| Commitment 37% | —I feel obliged to give him what he hasn't had so far. (Parallel chart 012) |
| Motivation 19% | —I realize that it is a mutual gift. It reassures me to see her grow strong and able to face tomorrow despite her condition. I feel good with her, comforted by her positive attitude. (Parallel chart 010) |
Table 5.
Macrothemes (MT) reported by MT professionals and PA representative interviewed:quotes from in-depth interviews
| Managing IRDs |
|
| Communication of the diagnosis |
|
| Attention to partner and parental caregivers |
|
| Lack of knowledge of IRDs |
|
| New investigation tools |
|
IRDs, inherited retinal disorders; PA, patient association.
bmjopen-2022-061080supp003.pdf (76.5KB, pdf)
The RPE65-related IRDs experience in the narratives
Overall, almost all classified narratives highlighted illness-related aspects23 (figure 1); adult patients’ narratives lacked a clinical language, which conversely characterised 63% of the caregivers’ narratives and 37% of the parallel charts. Sickness-related issues were present in 50% of the caregivers’ narratives and in 11% of the parallel charts, while they emerged in all adult patients’ narratives.
Core narratives38 prevailed in parallel charts (74%) and were equally reported (50%) as moral narratives by caregivers (figure 2); only parallel charts presented contingent narratives (11%). Moral narratives were prevalent among adult patients (60%), while discomfort, disbelief (particularly at school) and the search for independence represented three spontaneously emerged issues in all narratives.
Metaphors were clustered into four thematic groups (figure 3): (1) those referring to light and hope, used by patients (33%) and in parallel charts (15%); (2) those concerning limitations and impairment, equally reported (50%) by patients and caregivers; (3) those related to darkness and mist, used by caregivers (33%) and in parallel charts (40%) and (4) and metaphors denoting pain and isolation, almost equally used by patients and caregivers, and in parallel charts.
Emotional issues on the clinical diagnosis and the clinical encounter
Patients reported having had the first signs of visual impairment at 2 years and 3 months of age (median value; range 0,5–6). In narratives, all patients reported issues that arose during early childhood, and that their parental caregivers identified as critical, for example, being attracted by light sources or tripping (In the evening, my parents used to cover the kitchen lamp, otherwise I would spend hours just staring at it, Patient 002). As shown in table 2, patients described early living with an RPE65-associated IRD either as uncomfortable (62%), mainly referring to the feeling of ‘being wrong’, caused by the informal tests or eye examinations they were subjected to by their parents, or—conversely—normal (38%), since they did not have any standard of comparison to evaluate their sight. Caregivers reported having felt worried (50%) or helpless (50%) in the same years. During the communication of the clinical diagnosis, 71% of patients had no reaction, while the other 29% reported that it allowed them to identify their condition; conversely, parental caregivers (75%) felt hopeless, while partner caregivers (25%) reported concern for the hereditariness of the condition.
Table 3 summarises the clinicians’ feelings the first time they met their patients and at the beginning of the care pathway. During the first visit, 37% of parallel charts reported the thought that the path would have been challenging, while 30% reported hopefulness over the care options; conversely, 22% focused on a sense of sorrow for the patient and 11% on the empathy with patients or caregivers. At the beginning of the care relationship, clinicians felt on one side emotionally involved or motivated to do their best (58%), and on the other side helpless (30%) or ‘guilty’ for being in a privileged situation compared with the patient (12%).
In addition, 33% of the parallel charts highlighted the importance of showing empathy from the very beginning of the care relationship.
As for the currently living with an RPE65-related IRD (table 4), patients reported a sense of uncertainty (25%), due to increasing visual impairment or discomfort and sadness (25%); conversely, 50% reported to feel serene or hopeful, also considering the possibility of undergoing gene therapy. Caregivers declared to have accepted the condition (38%) and to live more serenely (62%), due to the awareness of having done their best. In parallel charts, clinicians reported positive feelings (44%), dedication (37%) and motivation (19%) toward patients.
VRQoL perception and daily living with RPE65-related IRDs
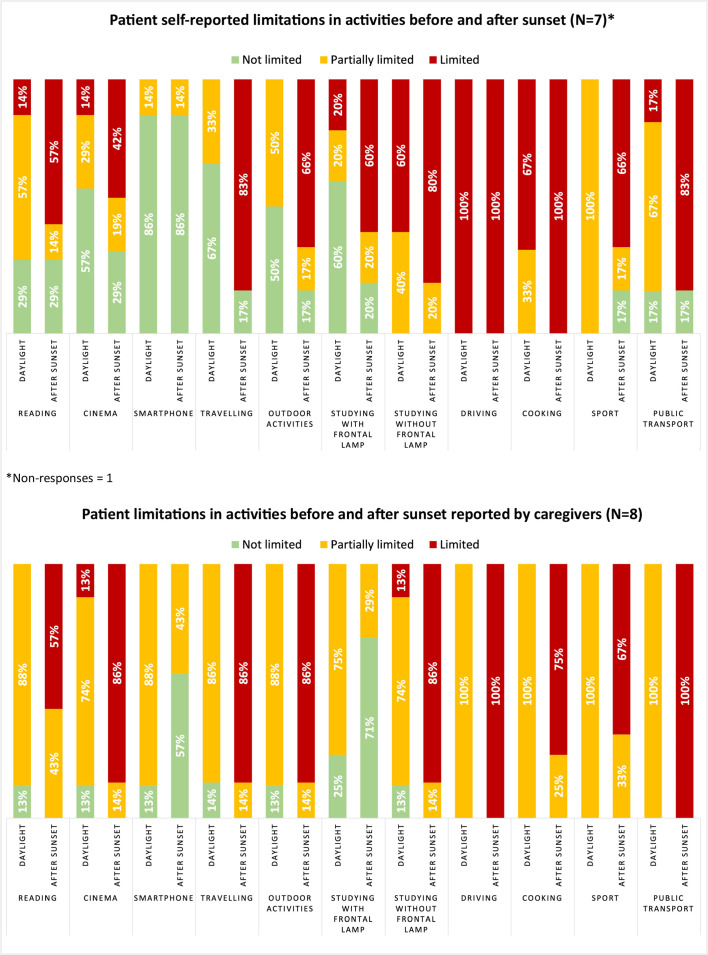
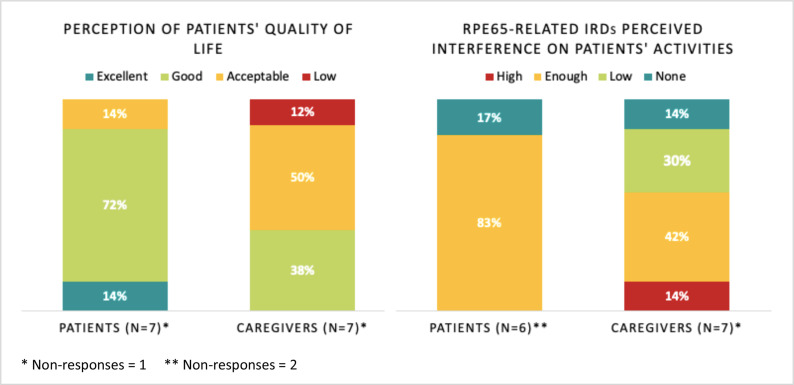
Online supplemental file 4 presents survey data on patients’ and caregivers’ evaluation of RPE65-related IRDs impact on patients and their day-to-day tasks in relation to low light conditions; figure 4 provides an overview of essential data.
Figure 4.
Reported limitations in activities by patients and caregivers: essential data.
bmjopen-2022-061080supp004.pdf (664.8KB, pdf)
Patients reported an increasing impact on main daily activities after sunset; thus, they referred both a severe impact on driving (100%) and cooking (100%), and no impact on the use of smartphones (86%) regardless of light conditions. Caregivers reported higher levels of limitation for patients in some activities even before sunset, such as reading, using digital tools or smartphones, washing, moving around; however, they reported fewer limitations in driving and cooking before sunset (100% partially limited). Considering an open coding of VRQoL domains in patient narratives, the limitation in activities was the prevalent issue, concerning 100% of patients’ narratives. Mobility limitation (–The city becomes more and more hostile. I am afraid of tripping, bumping into things, hurting myself, taking a wrong turn, being followed, and having to flee from a danger without being able to do so, Patient 001), health concerns (–I am sad and cry. I ask my mother if my eyes will ever be able to see well, Patient 007) and emotional well-being issues (–I cannot accept that I cannot do many things anymore, and I cannot admit that this leads me to close myself off, Patient 006) emerged in 75% of patients’ narratives.
Nevertheless, further survey data showed that 72% of patients considered their VRQoL good, and 14% excellent (figure 5); thus, they reported that RPE65-related IRDs have enough impact on the performance of their daily activities (83%). Fifty per cent of caregivers defined their patient’s VRQoL acceptable, and only 38% good; conversely, 30% and 14% reported that RPE65-related IRDs have a low—or no—impact on patients’ performance of daily activities, respectively.
Figure 5.
Patients’ QOL and RPE65-related IRDs overall interference on activities as perceived by patients and caregivers. IRDs, inherited retinal disorders; QOL, quality of life; RPE65, retinal pigment epithelium 65kD protein.
Addressing future perspectives, 71% of patients reported their hope to live serenely, both within their family and in the social context (–I just want my loved ones to see me calm and serene. […] I could not bear to see my relatives feeling bad for me, Patient 006), and 29% their hope to receive gene therapy (–Thinking about tomorrow, I would like to receive gene therapy, Patient 002); caregivers also stated to await gene therapy (50%). Clinicians hope to maintain a high quality of care in 41% of parallel charts, to improve their interpersonal skills and therapeutic possibilities for patients in 37%, and to be able to give them real hope in 22% (–Sometimes I think that gene therapy has already become a reality, and I feel that I am living a surreal experience. […] I wish that what I perceive as surreal today soon becomes reality, Parallel chart 007).
Overall, participants described writing as a positive experience: 80% of patients reported that narrative was a positive experience, and 20% stated to have felt a sense of freedom in sharing the illness experience. Twenty-seven per cent of the caregivers’ narratives and 21% of the parallel charts reported to consider it useful to raise awareness about these conditions; however, they also highlighted negative feelings, such as fatigue or sadness, in 14% and 8% of cases, respectively.
Insights from in-depth interviews
Five macrothemes transversely emerged from the in-depth interviews with MDT professionals and PA member (table 5):
The O&M instructor described the gap occurring between early-onset patients, who can develop compensatory strategies over time and adult-onset patients, more likely to lose their previous visual experience. Thus, early-onset patients may experience their sight as ‘normal’; in this sense, the psychologists highlighted the importance to psychologically support patients on the communication of the clinical diagnosis, when introducing the notion of ‘impairment’.
According to all interviewees, psychological support should be provided throughout the care pathway to improve communication and avoid misleading messages that could make patients feel that they ‘could do nothing more’. Furthermore, as also maintained by the genetic counsellors and the PA member, a more careful communication would allow the patient to keep an active perspective on the care pathway and early address rehabilitation programmes.
All interviewees addressed the RPE65-related IRDs impact on parental and partner caregivers. While the latter may face a couple crisis due to the progression of the impairment, the former often deal with the failure of the ‘perfect child’ dream, the hope that their children will heal and a strong sense of guilt for the inheritability of the condition. Since caregivers project these complex feelings on patients, potentially impacting their care pathway, a psychological support should be provided to help them accept this condition.
All interviewees highlighted the lack of knowledge of IRDs among the general public and society. The O&M instructor stressed that the link between visual impairment and changing light conditions is challenging for those who do not know these diseases. The psychologists confirmed that this is also critical in the school environment. One psychologist and the PA member mentioned the need to create an IRDs ‘culture’ and to address the diversity issue.
Furthermore, one psychologist focused on the need for investigation tools integrating quantitative questionnaires to address the interpersonal dimension of daily activities, especially after sunset or in low light conditions.
Discussion
The project represents the first effort to investigate RPE65-related IRDs in Italy through NM, simultaneously addressing the perspectives of patients, caregivers and treating retinologists and collecting insights from MDT professionals and PA members.
The co-presence of illness-related and sickness-related aspects23 and the lack of a clinical language in patient narratives highlighted the centrality of the personal and social dimensions of living with an RPE65-related IRD in narrating the illness experience and trying to make sense10 of the condition; the prevalence of moral narratives38 supports this suggestion. The employed classifications allowed related themes to emerge in narratives spontaneously: patients declared to have manifested the first signs of visual impairment during early childhood and reported a discomfort mainly due to the informal testing they were subjected to by their parents, together with repeated eye examinations, before the clinical diagnosis; at school, their visual impairment is misunderstood or questioned by their teachers, who are not aware of the relationship between visual impairment and changing light conditions. In-depth interviews confirm the lack of knowledge about IRDs among the general public and society, as well as at school, where patients also experience stigma41 since their visual issues are addressed like cognitive impairments. Further investigations on the school environment may integrate studies on the patients’ discrimination at their workplace42 and studies on the patients’ feeling of being often patronised.10
Early-onset patients perceive their sight as ‘normal’, finding out to be ‘impaired’ only after the clinical diagnosis or by interacting with their peers in the school environment. As emerged from the in-depth interviews, the notion of ‘impairment’ should be carefully introduced to support the patients’ awareness of their condition. This issue may be further explored and integrated with studies on making sense and coping with IRDs,10 12 while careful communication should be adopted throughout the care pathways.
The search for autonomy emerges as related to the health concerns for the progressive sight loss and the emotional well-being issues showing anxiety for the future. Findings confirm that RPE65-related IRDs significantly impact patients’ VRQoL in terms of activity and mobility limitations: while changing light conditions do not change the use of digital tools or smartphones, activities such as driving and cooking remain challenging, regardless of the light conditions; moreover, the capability to perform daily activities is compromised by low light conditions, as also shown in studies addressing IRD critical effects on lifestyle choices.11 43 Nonetheless, many patients reported having a good VRQoL, suggesting that they have found strategies to cope with the condition in the absence, so far, of a therapeutic solution; these coping strategies should be further investigated. Two considerations may be emphasised. On the one side, the narratives and survey data show misalignment between the patient’s and the caregiver’s perception of the former’s limitation in activities and in VRQoL, where patients report a higher perceived VRQoL, and conversely a lower performance while carrying out daily tasks: we remark that patients’ coping strategies may represent a possible explanation and—at the same time—not visually impaired caregivers may have a different perception of IRD impact on patients’ life; however, this issue needs further investigations. On the other side, the search for autonomy is linked with the perception that relying on others is a limitation, confirming previous studies on this topic.11
The metaphors used by patients to describe RPE65-related IRDs highlight not only limitations and pain, but also lights and hope. Conversely, the association with images recalling darkness emerges from caregiver narratives and parallel charts; in particular, caregivers do not use any positive image to describe RPE65-related IRDs.
In contrast with patients, caregiver narratives largely focus on disease-related aspects23; however, the presence of sickness-related and illness-related aspects suggests their emotional commitment to the patient’s well-being. Furthermore, moral narratives38 reveal the sense of guilt experienced by caregivers about the hereditariness of the condition, which is also addressed within in-depth interviews: while partner caregivers may face a couple crisis on the onset of the condition, parental caregivers experience the failure of the ‘perfect child’ dream and struggle to accept the condition. Misalignment in the patients’ perception of their VRQoL, metaphors and the emotional issues reported also suggest the complexity found by caregivers in coping with these conditions.
Parallel charts show that retinologists are personally and emotionally involved in the care relationship, as suggested by the prevalence of core narratives38 and reported their feelings at the beginning of the care pathway, despite being less focused on social RPE65-related IRDs aspects. Retinologists emerge as being motivated to find the most suitable therapeutic pathway, as well as emotionally committed to patients; for the first time in similar NM projects, clinicians report a clear sense of guilt for being ‘healthy’ compared with their patients.
These are only preliminary findings; however, they can provide initial insights on the importance of a multidisciplinary RPE65-related IRDs clinical practice:
RPE65-related IRDs critically impact several quality-of-life domains, while the emotional aspects of RPE65-related IRDs emerge as crucial while making sense of the condition and during the clinical encounter: the tension between the individual and the social dimensions of these conditions emerged as informative of the care pathway challenges and real-life experiences, and may be better addressed through new investigation tools, as claimed by the in-depth interviews. The NM approach has proved suitable for this purpose since sharing the illness experience by writing allows for more introspective and reflective knowledge, that may integrate the one-to-one level of in-depth interviews used in researching the living with a certain condition.
The emotional burden of caregiving remains poorly investigated. Nonetheless, narratives show that caregivers deeply participate in the patient’s illness experience, while the in-depth interviews recommend a psychological support to help them accept the condition, while potentially improving the care pathway.
The need for an RPE65-related IRDs ‘culture’ emerges as crucial to acknowledge these conditions, to avoid perpetuating the stigma and the scepticism and to foster the debate on diversity at society level.
Since narratives were anonymous, we are not able to precisely state the misalignment between patients and caregivers regarding the performance of daily activities and the perception of VRQoL; moreover, the voluntary participation in the project may have constituted a selection bias and included mostly patients more comfortable with writing. Further investigations are needed to examine in more details the issues which spontaneously emerged, also involving the work sphere. The annual incidence of RPE65-related IRDs explains the low number of participating patients44; however, the narratives collected suggest a strong dedication to the project and a relationship of trust between patients, caregivers and the retinologists from the centres involved. Finally, the data collection phase partially coincided with the local measures decided by the Italian government to contain the SARS-CoV-2 pandemic, with consequences on the clinical follow-up and the participation in the project.
Conclusion
The project investigated the practical and emotional issues of RPE65-related IRDs as experienced by patients, caregivers and retinologists, and provided insights from MDT professionals and PA members. It represented the first Italian project that simultaneously addresses and integrates these perspectives, whose comparison allowed to provide preliminary suggestions useful for the clinical practice and the knowledge of RPE65-related IRDs. NM allowed to connect the impact of RPE65-related IRDs on quality-of-life domains with real-life experiences, emerging as informative in raising suggestions to improve the care pathway for these conditions.
Supplementary Material
Acknowledgments
The authors wish to thank Novartis Farma Italia that sponsored and funded this work, especially Vincenza Vinaccia for her editorial assistance. The authors would also thank Paolo Melillo from Vanvitelli University Hospital for the support provided for the Ethical Committee’s approval of the project, as well as the researchers of Healthcare Area of ISTUD Foundation for their useful role throughout the project, as well as all the people suffering from an RPE65-related IRD, their caregivers, the healthcare professionals and the Patient Association representatives who took part in the research.
Footnotes
Contributors: FS, AS, BF, GB, GI, AA, LR, NF and MA were involved in the project’s conceptualisation. MGM, LR, and AF were involved in the methodology. FS, AS, BF, GB, GI, VDI, DG, GP, AA, GBV, AC, SDS, IDR, SF, CM, DPM, VM, IP and ST contributed to the project’s investigation. LR and MA were involved in the project’s administration. LR and AF contributed to data analysis. FS, AS, BF, GI, VDI, DG, GP, AA, LR and MA contributed to data validation. AF, LR and MA were involved in writing; all authors contributed to the manuscript review and read and approved the final draft for submission. AF is responsible for the overall content as guarantor.
Funding: Novartis Farma unconditionally supported ISTUD Foundation for the realisation of the project.
Competing interests: MA and NF are employees of Novartis Pharmaceuticals, Italy and Region Europe. FS, BF, GB and GI have received honoraria from Novartis Pharmaceuticals, Italy, for holding webinars. FS, AS, IP and IDR have received honoraria from Novartis Pharmaceuticals, Italy, for serving on advisory boards.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
BIRDS Working Group:
Giovanni Bosco Vitiello, Amelia Citro, Simona De Simone, Irene De Rienzo, Natalia Filimonova, Stefania Fortini, Cristiana Marchese, Maria Giulia Marini, Dario Pasquale Mucciolo, Vittoria Murro, Ilaria Passerini, and Simona Turco
Data availability statement
Data are available on reasonable request. The data that support the findings of this study are available from the corresponding author, LR, upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The project was performed according to the Declaration of Helsinki. Participants provided their web-based informed consent before their involvement and after being briefed on the project purposes and personal data processing procedures, according to the General Data Protection Regulation of the European Union 2016/679 and the Italian Law 196/2003. Furthermore, the IRD specialists involved obtained a written informed consent from the parents of paediatric patients during the first briefing on the project methods and purposes. The Ethical Committee of the Luigi Vanvitelli University Hospital (Naples, Italy) approved the project in September 2020 (protocol ID 20964/2020).
References
- 1. Broadgate S, Yu J, Downes SM, et al. Unravelling the genetics of inherited retinal dystrophies: past, present and future. Prog Retin Eye Res 2017;59:53–96. 10.1016/j.preteyeres.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 2. Ziccardi L, Cordeddu V, Gaddini V. Gene therapy in retinal dystrophies. Int J Mol Sci 2019;20:5722. 10.3390/ijms20225722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kang C, Scott LJ, Scoo LJ. Voretigene Neparvovec: a review in RPE65 mutation-associated inherited retinal dystrophy. Mol Diagn Ther 2020;24:487–95. 10.1007/s40291-020-00475-6 [DOI] [PubMed] [Google Scholar]
- 4. Duncan JL, Pierce EA, Laster AM, et al. Inherited retinal degenerations: current landscape and knowledge gaps. Transl Vis Sci Technol 2018;7:6. 10.1167/tvst.7.4.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tsang SH, Sharma T. Leber congenital amaurosis. Adv Exp Med Biol 2018;1085. 10.1007/978-3-319-95046-4_26 [DOI] [PubMed] [Google Scholar]
- 6. Tsang SH, Sharma T. Retinitis pigmentosa (non-syndromic). Adv Exp Med Biol 2018;1085. 10.1007/978-3-319-95046-4_25 [DOI] [PubMed] [Google Scholar]
- 7. Jacobson SG, Aleman TS, Cideciyan AV, et al. Defining the residual vision in Leber congenital amaurosis caused by RPE65 mutations. Invest Ophthalmol Vis Sci 2009;50:2368. 10.1167/iovs.08-2696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Russell S, Bennett J, Wellman JA, et al. Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial. Lancet 2017;390:849–60. 10.1016/S0140-6736(17)31868-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thompson DA, Ali RR, Banin E, et al. Advancing therapeutic strategies for inherited retinal degeneration: recommendations from the Monaciano symposium. Invest Ophthalmol Vis Sci 2015;56:918–31. 10.1167/iovs.14-16049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Thurston M, Thurston A, McLeod J. Socio-emotional effects of the transition from sight to blindness. British Journal of Visual Impairment 2010;28:90–112. 10.1177/0264619609359304 [DOI] [Google Scholar]
- 11. Prem Senthil M, Khadka J, Pesudovs K. Seeing through their eyes: lived experiences of people with retinitis pigmentosa. Eye 2017;31:741–8. 10.1038/eye.2016.315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bittner AK, Edwards L, George M. Coping strategies to manage stress related to vision loss and fluctuations in retinitis pigmentosa. Optometry 2010;81:461–8. 10.1016/j.optm.2010.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lloyd A, Piglowska N, Ciulla T, et al. Estimation of impact of RPE65-mediated inherited retinal disease on quality of life and the potential benefits of gene therapy. Br J Ophthalmol 2019;103:1610–4. 10.1136/bjophthalmol-2018-313089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chacón-López H, Pelayo FJ, López-Justicia MD, et al. Visual training and emotional state of people with retinitis pigmentosa. J Rehabil Res Dev 2013;50:1157–68. 10.1682/JRRD.2012.06.0113 [DOI] [PubMed] [Google Scholar]
- 15. Kempen GIJM, Ranchor AV, Ambergen T, et al. The mediating role of disability and social support in the association between low vision and depressive symptoms in older adults. Qual Life Res 2014;23:1039–43. 10.1007/s11136-013-0536-0 [DOI] [PubMed] [Google Scholar]
- 16. Parmeggiani F, Sato G, De Nadai K, et al. Clinical and rehabilitative management of retinitis pigmentosa: up-to-date. Curr Genomics 2011;12:250–9. 10.2174/138920211795860125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garip G, Kamal A. Systematic review and meta-synthesis of coping with retinitis pigmentosa: implications for improving quality of life. BMC Ophthalmol 2019;19:181. 10.1186/s12886-019-1169-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pierret J. The illness experience: state of knowledge and perspectives for research. Sociol Health Illn 2003;25:4–22. 10.1111/1467-9566.t01-1-00337 [DOI] [PubMed] [Google Scholar]
- 19. Greenhalgh T. Cultural contexts of health: the use of narrative research in the health sector. Copenhagen: who regional office for Europe; 2016, health evidence network (hen) synthesis report 49. Available: http://www.euro.who.int/__data/assets/pdf_file/0004/317623/HEN-synthesis-report-49.pdf, [Accessed 23 Mar 2021]. [PubMed]
- 20. Nowaczyk MJM. Narrative medicine in clinical genetics practice. Am J Med Genet A 2012;158A:1941–7. 10.1002/ajmg.a.35482 [DOI] [PubMed] [Google Scholar]
- 21. Ragusa L, Crinò A, Grugni G, et al. Caring and living with Prader-Willi syndrome in Italy: integrating children, adults and parents' experiences through a multicentre narrative medicine research. BMJ Open 2020;10:e036502. 10.1136/bmjopen-2019-036502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Marini MG. Narrative medicine: bridging the gap between evidence-based care and medical humanities. London: Springer International Publishing, 2016. [Google Scholar]
- 23. Kleinman A. The illness narrative, suffering and healing the human condition. New York: Basic Book, 1989. [Google Scholar]
- 24. Greenhalgh T, Hurwitz B. Why study narrative? BMJ 1999;318. 10.1136/bmj.318.7175.48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marini MG. Languages of care in narrative medicine. words, space and time in the healthcare ecosystem. London: Springer International Publishing, 2019. [Google Scholar]
- 26. Fioretti C, Mazzocco K, Riva S, et al. Research studies on patients' illness experience using the narrative medicine approach: a systematic review. BMJ Open 2016;6:e011220. 10.1136/bmjopen-2016-011220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Simonelli F, Sodi A, Falsini B, et al. Care pathway of RPE65-Related inherited retinal disorders from early symptoms to genetic counseling: a multicenter narrative medicine project in Italy. In Press;15:4591–605. 10.2147/OPTH.S331218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Audo I, Williamson N, Bradley H. Qualitative exploration of patient and caregiver experiences of visual function impairments and impacts on vision-dependent activities of daily living and health-related quality of life associated with retinitis pigmentosa and Leber congenital amaurosis in Germany and France. Invest. Ophthalmol. Vis. Sci 2021;62:3585. [Google Scholar]
- 29. Kay C, Williamson N, Bradley H. Qualitative interviews with patients and caregivers regarding visual function impairments and impacts on vision-dependent activities of daily living and health-related quality of life in RPE65-related retinitis pigmentosa and Leber congenital amaurosis. Invest. Ophthalmol. Vis. Sci 2021;62:3589. [Google Scholar]
- 30. Web content accessibility guidelines (WcaG) 2.1. W3C recommendations, 2018. Available: https://www.w3.org/TR/WCAG21/ [Accessed 23 Mar 2021].
- 31. Reid K, Soundy A. A qualitative study examining the illness narrative master plots of people with head and neck cancer. Behav Sci 2019;9. 10.3390/bs9100110. [Epub ahead of print: 17 10 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Peeters B, Marini M. Narrative medicine across languages and cultures: using minimal English for increased comparability of patients’ narratives. In: Goddard C, ed. Minimal English for a global world: improved communication using fewer words. Basingstoke, UK: Palgrave Macmillan, 2018: 259–86. [Google Scholar]
- 33. Charon R. The patient-physician relationship. narrative medicine: a model for empathy, reflection, profession, and trust. JAMA 2001;286:1897–902. 10.1001/jama.286.15.1897 [DOI] [PubMed] [Google Scholar]
- 34. Banfi P, Cappuccio A, Latella ME, et al. Narrative medicine to improve the management and quality of life of patients with COPD: the first experience applying parallel chart in Italy. Int J Chron Obstruct Pulmon Dis 2018;13:287–97. 10.2147/COPD.S148685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Brédart A, Marrel A, Abetz-Webb L, et al. Interviewing to develop patient-reported outcome (pro) measures for clinical research: eliciting patients' experience. Health Qual Life Outcomes 2014;12:15. 10.1186/1477-7525-12-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bazeley P, Jackson K. Qualitative data analysis with NVivo. London: SAGE, 2013. [Google Scholar]
- 37. Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 38. Bury M. Illness narratives: fact or fiction? Sociol Health Illn 2001;23:263–85. 10.1111/1467-9566.00252 [DOI] [Google Scholar]
- 39. Gibbs RW. How metaphors shape the particularities of illness and healing experiences. Transcult Psychiatry 2020:1363461520965424. 10.1177/1363461520965424 [DOI] [PubMed] [Google Scholar]
- 40. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 41. Goffman E. Stigma. London: Penguin, 1963. [Google Scholar]
- 42. Spiegel T, De Bel V, Steverink N. Keeping up appearances: the role of identity concealment in the workplace among adults with degenerative eye conditions and its relationship with wellbeing and career outcomes. Disabil Rehabil 2016;38:627–36. 10.3109/09638288.2015.1055378 [DOI] [PubMed] [Google Scholar]
- 43. Prem Senthil M, Khadka J, Gilhotra JS, et al. Exploring the quality of life issues in people with retinal diseases: a qualitative study. J Patient Rep Outcomes 2017;1:15. 10.1186/s41687-017-0023-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lorenz B, Tavares J, van den Born LI. Current management of patients with RPE65 mutation-associated inherited retinal degenerations (IRDs) in Europe. Results of a multinational survey by the European vision Institute clinical research network EVICR.net. Ophthalmic Res 2021. 10.1159/000515688 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-061080supp001.pdf (44.7KB, pdf)
bmjopen-2022-061080supp002.pdf (74.7KB, pdf)
bmjopen-2022-061080supp003.pdf (76.5KB, pdf)
bmjopen-2022-061080supp004.pdf (664.8KB, pdf)
Data Availability Statement
Data are available on reasonable request. The data that support the findings of this study are available from the corresponding author, LR, upon reasonable request.