Abstract
Cronkhite -Canada Syndrome (CCS) is a rare non-hereditary disease characterized by multiple polyps in the alimentary tract and ectoderm changes, and there is no clearly diagnostic criteria and treatment methods. A 55-year-old Chinese woman was admitted to our hospital with diarrhea. She was diagnosed with Cronkhite-Canada Syndrome (CCS). The clinical symptoms of the patient included diarrhea, nausea, retching, anorexia, weight loss, and we found that she had alopecia, onychatrophy, rampant caries and skin pigmentation from the physical examination. Gastrointestinal endoscopy revealed multiple polyps in the gastric antrum, stomach body, ileocecal part and colon, and from the microscopically the polype hyperplsique was observed. The patient was treated by eradicating Helicobacter pylori and regulating the intestinal flora disbalance and his diarrhea improved within a short period of time. We suggested that she should take glucocorticoids orally, but the patient refused. Follow-up at 1 year showed that the symptoms of the patient had recurred sometimes, and she had taken Chinese herbal medicine orally a few times. At present, the symptoms of diarrhea are relieved, the weight of the patient has increased, and the hair and nails of the patient have grown again. From this case, we learned CCS can be likely ignored and not be diagnosed promptly because the low morbidity of CCS.
Keywords: Cronkhite-Canada syndrome, Diffuse gastrointestinal polyposis, Ectodermal changes, Case report, Literature review
Highlights
-
•
The clinical manifestations of Cronkhite-Canada syndrome are diversified, including diarrhea, hyperpigmentation, hair loss, and nail malnutrition. Misdiagnosis and missed diagnosis can be caused by ignoring skin symptoms.
-
•
The patient was not treated with glucocorticoids, and symptoms resolved after 1 year.
-
•
According to the statistics of the article, there is no statistical difference in the remission rate between the use of glucocorticoid and no use.
1. Introduction
Cronkhite-Canada syndrome (CCS) is a rare, non-hereditary disease characterized by multiple polyps and ectodermal changes in the gastrointestinal tract, also known as polyp-pigmentation-alopecia- onychatrophy syndrome [1]. It was first reported by Cronkhite and Canada in 1955 [2]. There are more than 500 cases worldwide, 75% of which occurred in Japan [3]. According to the different initial symptoms, Japanese scholars divided CCS into 5 types [4]: type Ⅰ (diarrhea type), type Ⅱ (taste loss type), type Ⅲ (oral dryness type), type Ⅳ (abdominal discomfort type) and type Ⅴ (hair loss type).
CCS may be significantly underestimated in many Gastrointestinal wards. However, in recent years, there is an increasing number of cases reported due to the prompt recognition and accumulated experience of clinicians, as well as the development of lab examinations. Here we report a case of CCS and follow up 1 year the patient has a relief. Since no guideline or expert consensus has ever been achieved in CCS, it is meaningful to summarise all the related studies in order to provide more critical insight of the diagnosis, monitoring and management of this rare disorder to clinicians. This case report has been reported in line with the SCARE Criteria [5].
2. Case presentation
A 55-year-old Chinese traditional housewife was admitted to our hospital with diarrhea. This patient had no past surgical history, drug history and allergies history, and her family history was not-contributory, and she did not have bad habits, such as smoking, alcohol, and recreational drug use. About 2 months earlier, she had undergone clysis for constipation at a local hospital. After that, she suffered from severe diarrhea that the defecating frequency was greater than 10 times a day, so she had to take antidiarrheal drugs every day, but her diarrhea was not alleviated. She observed the routine stool test in the outpatient service of our hospital and the leukocytosis and fecal occult blood was in the examination.
Because of the severe diarrhea and abnormal results of the routine stool test, the patient had to be hospitalized in our hospital. After admission, the laboratory examination showed that the deficiency of serum zinc and the abnormality of Complement 3, while the infection of Helicobacter pylori and the positive fecal occult blood test and other tests were normal. And the abnormality were not observed in the computer tomography (CT) of the abdomen. While the results of gastroscopy by endoscopist with lots of years of training in our hospital showed that the mucosa edema of the cardia, gastric fundus, gastric body, gastric angle and gastric antrum was observed and the mucosa was filled with apophysis lesion with the appearance of polypuses, and the descending part of the duodenum was full of it with the appearance of polype hyperplasia. The results of colonoscopy showed that mucosa edema, scattered hemorrhage and multiple apophyses with the appearance of polypuses were observed from the ileocecal valve to 20 cm from the anus and numerous polyps were found in the ileocecal, ascending, transverse colon and other abnormality were not observed.
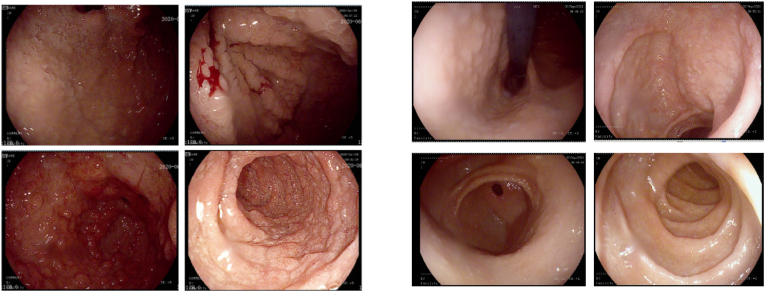
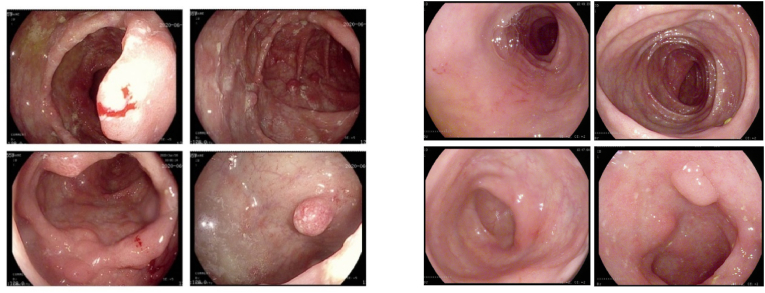
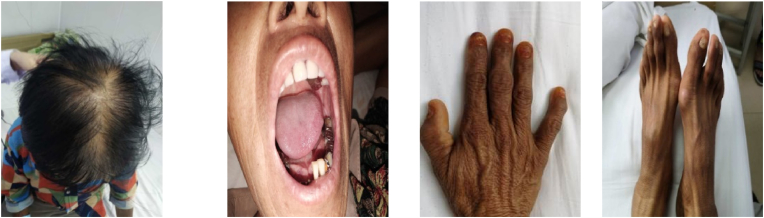
Fig. 1Awas a photograph of the tissue involving the gastric antrum and gastric body. Histopathological examination of the resected specimen showed a macroscopic appearance of grayish white tissue involving the gastric antrum and gastric body. Microscopically, polype hyperplsique was observed. Fig. 2A was a photograph of the tissue involving the ileocecal junction. Histopathological examination of the specimen showed a macroscopic appearance of grayish white tissue involving the ileocecal junction. Microscopically, acute and chronic mucosal inflammation and the expansion of the glands and crypt abscess were found. It is rare for the multiple polyps we considered the patient maybe have an immune system disease, so the patient had a tests of autoimmunity, and the index of the immunity system was normal and the serum protein electrophoresis was mildly changed. From the physical examination, we found that the patient had alopecia, onychatrophy, rampant caries, weight loss and skin pigmentation. The diagnosis of Cronkhite Canada syndrome (CCS) was established because of these physical characteristics and a related inspection. Because there is no uniform standard for the diagnosis of CCS the patient was treated with protecting the mucosal barrier and regulating the intestinal flora of disbalance, and his diarrhea improved within a short period of time. The patient accepted the treatment of supplementing trace elements because of deficiency and the patient also accepted the treatment of eradicating Helicobacter pylori because of infection. We suggested that the patient take glucocorticoids to have a relief, but she refused considering the side effects of glucocorticoids. The patient was followed up irregularly within 1 year and had not totally adhered to the advice provided by chief physician, but after 1 year she still had a hospitalization, we found the symptoms of the diarrhea are relieved, the weight of the patient is increased, and the hair and nails of the patient have grown again (see Fig. 3, Fig. 4).
Fig. 1.
A The mucosa of the cardia, gastric fundus, gastric body and antrum was extensively edematous with polypoid eminence. B Follow-up at 1 year, polyps in stomach decreased significantly.
Fig. 2.
A Extensive polyps were widely distributed in the ileocecal, ascending and transverse colon. B Follow-up at 1 year, polyps in intestinal tract decreased significantly.
Fig. 3.
Form the physical examination we found that the patient had alopecia, onychatrophy, rampant caries and skin pigmentation.
Fig. 4.
Follow-up at 1 year, the hair and nails have grown again and skin pigmentation has been relieved.
3. Discussions
The pathogen of CCS is still not clear at present. Some scholars think that the occurrence of CCS may be associated with the immune system, and a report discovered that symptoms are relived after taking corticosteroids [6]. The polyps in some CCS patients with pathological examination were found to have IgG4 plasma cells infiltrating [7]. We suggested that the patient take glucocorticoids to have a relief, but she refused considering the side effects of glucocorticoids. Some studies show that CCS is associated with genetic factors and there might be some familial aggregation [8]. Some studies have found that the occurrence of CCS may be related to infection, among which Helicobacter pylori infection is the most common, and the symptoms are improved after eradication of Helicobacter pylori treatment [9]. Some research found that the deficiency of trace elements, such as zinc and copper, may lead to the occurrence of CCS [10].
There is no uniform standard for the diagnosis of CCS, which is usually diagnosed by medical history, physical examination, endoscopic examination and pathological results. Patients are characterized by multiple polyps in the gastrointestinal tract, skin pigmentation, sparse hair, onychatrophy, diarrhea, emaciation, etc, and from this we need to consider CCS. CCS usually needs to be differentiated from familial adenomatous polyposis (FAP), Peutz-Jeghers syndrome, Turcot syndrome and other diseases. FAP is characterized by large and small adenomas in the colorectal region, and it is an autosomal inherited hereditary disease, showing multiple adenomas in the large intestine, and the incidence is more common among young people. Most polyps are adenomatous with high malignancy [[11], [12], [13]]. Peutz-Jeghers syndrome is an autosomal dominant hereditary disease characterized by dark spots on the lips and extremities, multiple hamartomatous polyps in the gastrointestinal tract, and susceptibility to highly malignant tumors and the polyp is mainly located in the small intestine and ileum and the polyp pathology is hamartomatous polyps [[14], [15], [16]]. Turcot syndrome, also known as brain-tumor-polyposis-syndrome, is a rare hereditary disease first reported by Turcot in 1959, and its clinical features are familial multiple colonic adenomas, colorectal cancer and malignant tumors of the central nervous system [17].
Chinese studies have pointed out that the typical endoscopic feature of CCS is multiple polyps or nodular eminence with the pathology of diffuse hyperemia and edema in the gastric, duodenal and colonic mucosa, which merge with lymphatic dilatation-like changes in the duodenum or terminal ileum [18]. Gastrointestinal polyps of the CCS are widely distributed with different diameters and local clusters, while some patients showed atypical endoscopic manifestations, and because the disease is rare, it is high for the misdiagnosis rate and missed diagnosis rate of diseases [6]. Proliferative polyps and hamartomatoid polyps were common histopathology in CCS and 31%–71% of patients were complicated with adenoma or adenomatoid changes in the digestive tract [19].
There is no agreed standard for the treatment of CCS in the world, and it is still in the exploratory stage. Some research has shown that oral corticosteroids have a certain efficacy in the treatment of CCS [20]. However, there is no recognized standard for the treatment of CCS in the world, and it is still in the exploratory stage. Studies have shown that oral corticosteroids have a certain efficacy in the treatment of CCS. The side effects of oral glucocorticoids, such as peptic ulcer, osteoporosis and electrolyte disorders, should not be underestimated. The use of immunosuppressants is helpful for the treatment of CCS. Some studies have pointed out that gastrointestinal polyps can disappear after the use of mesalazine [21]. Parenteral nutrition could effectively improve intestinal function and play a certain role in the recovery of diseases. Some scholars have also pointed out that the use of antibiotics is also helpful to the recovery of diseases [8].
Prognosis of CCS is related to complications. Complications of CCS include gastrointestinal bleeding with anemia, intussusception, hypoproteinemia, rectal prolapse, malabsorption, electrolyte disorder, inflammatory bowel disease and vitamin deficiency [22]. There are 383 CCS patients in Japan, of which 40 were diagnosed with gastric cancer and 51 with colon cancer [23], so endoscopic examination and pathological biopsy of CCS are particularly important. The prognosis of CCS is poor, because CCS is a rare disease and clinicians may have some misdiagnosis, what is more importantly, CCS is often associated with cancer.
We believe that there will be a great breakthrough in the treatment of CCS with the development of endoscopic technology and improvement of science and technology.
Declaration of competing interest
The authors declared that they have no conflicts of interest to this work. We declare that we do not have any commercial or associative interest that represents a conflict of interest in connection with the work submitted.
References
- 1.Slavik T., Montgomery E.A. Cronkhite-Canada syndrome six decades on: the many faces of an enigmatic disease[J] J. Clin. Pathol. 2014;67(10):891–897. doi: 10.1136/jclinpath-2014-202488. [DOI] [PubMed] [Google Scholar]
- 2.Cronkhite L.W., Jr., Canada W.J. Generalized gastrointestinal polyposis: an unusual syndrome of polyposis, pigmentation, alopecia and onychotrophia[J]. N. Engl. J. Med. 1955;252:1011–1015. doi: 10.1056/NEJM195506162522401. [DOI] [PubMed] [Google Scholar]
- 3.Matsui S., Kibi Mç, Anami E., et al. A case of Cronkhite - Canada syndrome with multiple colon adenomas and early colon cancers[J] Nihon Shokakibyo Gakkai Zasshi. 2011;108(5):778–786. [PubMed] [Google Scholar]
- 4.Goto A. Cronkhite-Canada syndrome: epidemiological study of 110 cases reported in Japan[J] Nihon Geka Hokan. 1995;64(1):3–14. [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., et al. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines[J] Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Sweetser S., Ahlquist D.A., Osborn N.K., et al. Clinicopathologic features and treatment outcomes in Cronkhite-Canada syndrome: support for autoimmunity[J]. Dig. Dis. Sci. 2012;57(2):496–502. doi: 10.1007/s10620-011-1874-9. [DOI] [PubMed] [Google Scholar]
- 7.Li Y., Luo H.Q., Wu D., et al. Cronkhite-Canada zonghezheng linchuang fenxi ji IgG4 yangxing jiangxibao jinrun de yiyi[Clinicopathologic features of Cronkhite-Canada syndrome and the significance of IgG4-positive plasma cells infiltration] Zhonghua Bing Li Xue Za Zhi. 2018;47(10):753–757. doi: 10.3760/cma.j.issn.0529-5807.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Patil V., Patil L.S., Jakareddy R., Verma A., Gupta A.B. Cronkhite-Canada syndrome: a report of two familial cases[J]. Indian J. Gastroenterol. 2013;32:119–122. doi: 10.1007/s12664-012-0296-8. [DOI] [PubMed] [Google Scholar]
- 9.Okamoto K., Isomoto H., Shikuwa S., Nishiyama H., Ito M., Kohno S. A case of Cronkhite-Canada syndrome: remission after treatment with anti-Helicobacter pylori regimen[J]. Digestion. 2008;78(2–3):82–87. doi: 10.1159/000165354. [DOI] [PubMed] [Google Scholar]
- 10.Berzin T.M., Greenberger N.J., Levy B.D., Loscalzo J. Clinical problem-solving. Worth a second look[J]. N. Engl. J. Med. 2012;366(5):463–468. doi: 10.1056/NEJMcps0907563. [DOI] [PubMed] [Google Scholar]
- 11.Lynch H.T., de la Chapelle A. Hereditary colorectal cancer[J]. N. Engl. J. Med. 2003 Mar 6;348(10):919–932. doi: 10.1056/NEJMra012242. [DOI] [PubMed] [Google Scholar]
- 12.Groen E.J., Roos A., Muntinghe F.L., et al. Extra-intestinal manifestations of familial adenomatous polyposis[J]. Ann. Surg Oncol. 2008;15(9):2439–2450. doi: 10.1245/s10434-008-9981-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Claes K., Dahan K., Tejpar S., et al. The genetics of familial adenomatous polyposis (FAP) and MutYH-associated polyposis (MAP) [J]. Acta Gastroenterol. Belg. 2011;74(3):421–426. [PubMed] [Google Scholar]
- 14.Shaco-Levy R., Jasperson K.W., Martin K., et al. Morphologic characterization of hamartomatous gastrointestinal polyps in Cowden syndrome, Peutz-Jeghers syndrome, and juvenile polyposis syndrome[J]. Hum. Pathol. 2016;49:39–48. doi: 10.1016/j.humpath.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 15.de Brabander J., Eskens F.A.L.M., Korsse S.E., et al. Chemoprevention in patients with Peutz-Jeghers syndrome: lessons learned[J]. Oncol. 2018;23(4):399. doi: 10.1634/theoncologist.2017-0682. e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rumnong V.S., Malik A.K., Kochhar R., Sakhuja V., Yadav R.V. Fatal ischaemic colitis in renal allograft recipients[J]. Indian J. Gastroenterol. 1988 Apr;7(2):117–118. [PubMed] [Google Scholar]
- 17.Ozerov S.S., Zakharov I.V., Talypov S.R., et al. Turcot syndrome. Rare observation and literature review[J]. Zh. Vopr. Neirokhir. Im. N. N. Burdenko. 2013;77(3):49–53. [PubMed] [Google Scholar]
- 18.Liu S., You Y., Wu d, et al. 24 li Cronkhite-Canada zonghezheng huanzhe de neijing tedian ji linxchuang xiangguanxing Fenxi[Endoscopic features and clinical correlation analysis of 24 patients with Cronkhite-Canada syndrome] Zhonghua Yixue Zazhi. 2020;(20):1562–1566. doi: 10.3760/cma.j.cn112137-20191125-02556. [DOI] [PubMed] [Google Scholar]
- 19.Liu Y.X., Wu D., Fei G.J., et al. 12 li Cronkhite Canada zonghezheng huanzhe linchuang ji bingli tedian[Clinical characteristics, diagnosis and therapy of 26 patients with Cronkhite-Canada syndrome] Ji Chu Yi Xue Yu Lin Chuang. 2012;(11):1349–1352. [Google Scholar]
- 20.Watanabe C., Komoto S., Tomita K., et al. Endoscopic and clinical evaluation of treatment and prognosis of Cronkhite-Canada syndrome: a Japanese nationwide survey[J]. J. Gastroenterol. 2016;51(4):327–336. doi: 10.1007/s00535-015-1107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schulte S., Kütting F., Mertens J., Kaufmann T., Drebber U., Nierhoff D., Töx U., Steffen H.M. Case report of patient with a Cronkhite-Canada syndrome: sustained remission after treatment with corticosteroids and mesalazine [J] BMC Gastroenterol. 2019;19(1):36. doi: 10.1186/s12876-019-0944-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seshadri D., Karagiorgos N., Hyser M.J. A case of cronkhite-Canada syndrome and a review of gastrointestinal polyposis syndromes. Gastroenterol. Hepatol. (N Y) 2012;8(3):197–201. [PMC free article] [PubMed] [Google Scholar]
- 23.Matsui S., Kibi M., Anammi E., et al. A case of Cronkhite - Canada syndrome with multiple colon adenomas and early colon cancers[J] Nihon Shokakibyo Gakkai Zasshi. 2011;108(5):778–786. [PubMed] [Google Scholar]