Key Points
Question
Are state child abuse policies and mandated reporting policies for prenatal substance use associated with receipt of prenatal and postpartum care?
Findings
In this cross-sectional study of 4155 pregnant women who engaged in substance use during pregnancy, women who delivered in states with a child abuse policy, a mandated reporting policy, or both policies initiated prenatal care later and had a lower likelihood of adequate prenatal care and a postpartum health care visit compared with those who delivered in states with neither policy.
Meaning
These results suggest that programmatic and policy strategies that emphasize supportive, nonstigmatizing approaches to substance use during pregnancy are needed.
This cross-sectional study uses Pregnancy Risk Assessment Monitoring System survey data to evaluate the association of substance use with prenatal and postpartum care in states with a child abuse policy and/or mandated reporting policy.
Abstract
Importance
Some states have implemented policies that consider substance use during pregnancy as child abuse and require mandated reporting of substance use during pregnancy. Implications of these policies for health care receipt among pregnant people who engage in substance use are unknown.
Objective
To examine the association of state child abuse policies and mandated reporting policies with prenatal and postpartum care among women who engaged in substance use during pregnancy.
Design, Setting, and Participants
In this cross-sectional study, data from the 2016-2019 Pregnancy Risk Assessment Monitoring System survey were analyzed. The study population included 4155 women from 23 states who reported substance use during pregnancy. Data were analyzed between August and November 2021.
Exposures
Delivery in a state with a child abuse policy only (n = 6), a mandated reporting policy only (n = 4), both policies (n = 7), or neither policy (n = 5). One state switched from a mandated reporting policy only to having both policies.
Main Outcomes and Measures
Month of gestation at prenatal care initiation (ie, months 1-10, with a higher number of months indicating later initiation), receipt of adequate prenatal care, and receipt of a postpartum health care visit 4 to 6 weeks after delivery. Sample characteristics were calculated using unweighted frequencies and weighted percentages and means. Associations of state policies with the outcomes were examined using generalized linear regression with generalized estimating equations, adjusting for potential confounders and accounting for the complex sampling design of the Pregnancy Risk Assessment Monitoring System survey.
Results
The study sample included 4155 women who reported substance use during pregnancy; 33.9% of these women delivered in states with a child abuse policy only, 16.4% in states with a mandated reporting policy only, 32.9% in states with both policies, and 16.8% in states with neither policy. Overall, 14.7% of women were Black, 69.0% were White, and 64.6% were aged 18 to 29 years at delivery. Women who delivered in states with a child abuse policy only, mandated reporting policy only, or both policies initiated prenatal care at a later month of gestation (β = 0.44 [95% CI, 0.10-0.78], 0.32 [95% CI, 0.04-0.59], and 0.40 [95% CI, 0.09-0.72], respectively) and had a lower likelihood of adequate prenatal care (risk ratio, 0.85 [95% CI, 0.79-0.91], 0.94 [95% CI, 0.87-1.01], and 0.95 [95% CI, 0.89-1.03], respectively) and a postpartum health care visit (risk ratio, 0.89 [95% CI, 0.82-0.96], 0.89 [95% CI, 0.80-0.98], and 0.92 [95% CI, 0.83-1.02], respectively) compared with women who delivered in states with neither policy.
Conclusions and Relevance
The results indicate that state child abuse policies and mandated reporting policies are associated with reduced receipt of prenatal and postpartum care among women who engage in substance use during pregnancy.
Introduction
Substance use during pregnancy remains a persistent concern in the context of the US overdose crisis. According to the 2020 National Survey on Drug Use and Health, 8% of pregnant people reported recent illicit drug use, and the incidence of opioid- and amphetamine-affected births has increased substantially in recent years.1,2,3 Existing evidence indicates that substance use during pregnancy is associated with an increased risk of adverse outcomes, including preterm birth, low birth weight, and severe maternal morbidity and mortality.3,4,5 States have implemented policies specific to prenatal substance use, including policies that consider substance use during pregnancy to be child abuse under civil child welfare statutes (hereafter referred to as child abuse policies) and policies that require health care professionals to report suspected or identified substance use during pregnancy to child welfare agencies (hereafter referred to as mandated reporting policies). Currently, 23 states and the District of Columbia have a child abuse policy, and 26 states and the District of Columbia have a mandated reporting policy.6
Leading medical and public health organizations, including the American Public Health Association, American Medical Association, American College of Obstetricians and Gynecologists, and American Academy of Pediatrics, have recommended against child abuse policies and mandated reporting policies, stating that these policies may undermine caregiver and infant health by discouraging pregnant people who use substances from engaging in prenatal care and substance use disorder (SUD) treatment in order to avoid punitive responses to their substance use.7,8 Previous research has shown that child abuse policies and mandated reporting policies are associated with reductions in SUD treatment admissions and receipt of medication for opioid use disorder among pregnant people9,10,11 and lower rates of family reunification among infants in foster care because of parental substance use.12 Although no studies have specifically examined the association of these policies with health care use, qualitative studies have indicated that pregnant people with SUD delay or avoid prenatal and postpartum care because of fear of detection and legal consequences, including loss of infant custody, suggesting that these policies may contribute to decreased receipt of prenatal and postpartum care.13,14 This is important because early and consistent prenatal care is critical to ensuring healthy outcomes, particularly in the context of prenatal substance use.15,16,17,18,19
A comprehensive understanding of the association of child abuse policies and mandated reporting policies with health care use is key to informing empirically driven policy making and supporting healthy outcomes. The aim of this study was to examine the association of state child abuse policies and mandated reporting policies with prenatal and postpartum care among women who engaged in substance use during pregnancy.
Methods
Design and Data Sources
In this cross-sectional study, we used 2016-2019 survey data from the Pregnancy Risk Assessment Monitoring System (PRAMS), a population-based surveillance system conducted by state and local health departments in partnership with the Centers for Disease Control and Prevention (CDC). Each year, states use their birth certificate files to select a systematic, stratified sample of women who delivered a live birth in that year, with stratification by factors such as maternal race and ethnicity and infant birth weight to ensure sufficient sample sizes for subgroup analyses.20 Participating women complete a mail or telephone survey 2 to 6 months post partum, with survey questions specific to the preconception, prenatal, and postpartum periods.20
We used PRAMS data from states and survey years that included a question about prenatal substance use and had a 55% or greater response rate for the overall survey, in accordance with CDC guidelines20 (eTable 1 in the Supplement). Because prenatal substance use policies should affect health care use among only those with substance use during pregnancy, we restricted our sample to women who reported use of prescription opioids (eg, hydrocodone, oxycodone), marijuana, synthetic marijuana, heroin, amphetamines (eg, speed, crystal meth [methamphetamine]), cocaine, tranquilizers (eg, downers, quaaludes), or hallucinogens (eg, LSD/acid [lysergic acid diethylamide], Ecstasy [3,4-methylenedioxymethamphetamine]) during pregnancy. We also restricted our sample to women aged 18 years or older because some survey questions are not asked of female respondents younger than 18 years. Our final sample included 4155 women across 23 states and 45 state-years.
This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines. The institutional review board of the University of North Carolina at Chapel Hill considered this study exempt because it used secondary, deidentified data.
Measures
State Policy Categories
We identified the year in which states first implemented child abuse policies and mandated reporting policies through state policy documents from the Guttmacher Institute,21 reports from the Children’s Bureau,6 and other peer-reviewed studies9,10,11 (eTable 1 in the Supplement). We categorized each state-year as having a child abuse policy only, a mandated reporting policy only, both policies, or neither policy.
Prenatal Care
We examined 2 measures of prenatal care: timing of prenatal care initiation and prenatal care adequacy. We measured the timing of prenatal care initiation as the month of gestation at the first prenatal care visit as recorded on the birth certificate (ie, months 1-10, with a higher number of months indicating later initiation). We measured the adequacy of prenatal care using the Kotelchuck Index, which uses the timing of prenatal care initiation and the total number of prenatal visits received to calculate a ratio of expected to received visits.22 On the basis of the Kotelchuck Index, we categorized prenatal care as adequate (adequate or adequate plus) or not adequate (intermediate or inadequate). Data for prenatal care outcomes were missing for less than 4% of observations.
Postpartum Care
We examined 1 measure of postpartum care, receipt of a postpartum health care visit, using women’s self-report of whether they had a postpartum visit for themselves 4 to 6 weeks after delivery. Data for receipt of a postpartum health care visit were missing for less than 1% of observations.
Covariates
We identified potential confounders using a conceptual diagram (eFigure in the Supplement). On the basis of our conceptual diagram, we included several variables in multivariable models to minimize bias due to confounding (eTable 2 in the Supplement). Variables included measures of the underlying state policy context specific to substance use and maternal health care use (priority access to SUD treatment and targeted SUD treatment programs for pregnant people, medical marijuana legalization, Medicaid expansion, Medicaid Family Planning expansion, presumptive eligibility for Medicaid, and number of obstetricians and gynecologists per 100 000 female population), maternal demographic characteristics (age, self-reported race and ethnicity, per capita household income, and education), and women’s experiences and behaviors before pregnancy (mental health, experiences of violence, and pregnancy intention). Data for maternal demographic characteristics and prepregnancy experiences and behaviors were missing for 0% to 6% of observations.
Statistical Analysis
Data were analyzed between August and November 2021. We described characteristics of our sample by the 4 state policy categories, calculating unweighted frequencies and weighted percentages and means with corresponding 95% CIs, with weighting used to account for the complex sampling design of PRAMS. We did not conduct statistical tests for comparisons in accordance with recommendations to avoid an overemphasis on P values and to place greater emphasis on the actual size of observed differences.23
To examine associations of child abuse policies and mandated reporting policies with prenatal care initiation, we conducted generalized linear regression with an identity link and normal distribution to calculate differences in average month of gestation at initiation and corresponding 95% CIs. To examine associations with the adequacy of prenatal care and receipt of a postpartum health care visit, we conducted generalized linear regression with a log link and Poisson distribution with a robust error variance to calculate risk ratios (RRs) and 95% CIs.24 In all models, we included a linear time trend and compared outcomes for women who delivered in states with a child abuse policy only, a mandated reporting policy only, and both policies with outcomes for women who delivered in states with neither policy. We used generalized estimating equations and an independent working correlation matrix to account for repeated measures within states over time. We weighted the analyses to account for the complex sampling design of PRAMS. To interpret results from multivariable analyses, we relied on the magnitude of point estimates and the width and location of the corresponding 95% CIs. We did not rely on P values in accordance with guidance from the American Statistical Association.25
Because the mandated reporting policies in Kentucky and Massachusetts require reporting only if maltreatment is suspected, we conducted sensitivity analyses classifying Kentucky and Massachusetts as not having a mandated reporting policy. Results were unchanged. Statistical analyses were conducted using SAS, version 9.4 (SAS Institute Inc) software.
Results
Our study sample included a total of 4155 women aged 18 years or older across 23 states. From 2016 to 2019, 6 of the included states had a child abuse policy only, 4 states had a mandated reporting policy only, 7 states had both policies, 5 states had neither policy, and 1 state switched from a mandated reporting policy only from 2017 to 2018 to both policies in 2019. A total of 33.9% of women delivered in states with a child abuse policy only, 16.4% delivered in states with a mandated reporting policy only, 32.9% delivered in states with both policies, and 16.8% delivered in states with neither policy. Overall, 14.7% of women were non-Hispanic Black, 6.8% were Hispanic, 69.0% were non-Hispanic White, and 64.6% were aged 18 to 29 years at delivery. There was a higher percentage of births to non-Hispanic Black women in states with a child abuse policy only (19.6%; 95% CI, 16.3%-22.9%), a mandated reporting policy only (16.3%; 95% CI, 11.0%-21.5%), or both policies (15.0%; 95% CI, 13.1%-17.0%) than in states with neither policy (5.9%; 95% CI, 3.9%-8.0%) (Table). There was also a higher percentage of unintended pregnancies in states with a child abuse policy only (63.1%; 95% CI, 58.9%-67.3%) compared with states with neither policy (56.6%; 95% CI, 52.2%-61.0%). More women had adequate prenatal care in states with both policies (75.1%; 95% CI, 71.0%-79.2%) or neither policy (75.0%; 95% CI, 71.2%-78.8%) than those in states with a child abuse policy only (64.1%; 95% CI, 59.8%-68.4%) or a mandated reporting policy only (66.4%; 95% CI, 59.1%-73.7%). The mean gestational month of prenatal care initiation was later among women in states with a child abuse policy only (3.3 months; 95% CI, 3.1-3.5 months) or a mandated reporting policy only (3.1 months; 95% CI, 2.8-3.5 months) than in states with neither policy (2.8 months; 95% CI, 2.7-3.0 months).
Table. Characteristics of Women Reporting Prenatal Substance Use by State Prenatal Substance Use Policies for 4155 Birthsa.
| Characteristic | Child abuse policy only (n = 987 births) | Mandated reporting policy only (n = 610 births) | Both policies (n = 1276 births) | Neither policy (n = 1282 births) | ||||
|---|---|---|---|---|---|---|---|---|
| No. | % (95% CI) | No. | % (95% CI) | No. | % (95% CI) | No. | % (95% CI) | |
| Age, y | ||||||||
| 18-24 | 298 | 32.2 (28.1-36.4) | 166 | 31.6 (24.3-38.9) | 407 | 31.0 (26.7-35.4) | 408 | 35.9 (31.6-40.2) |
| 25-29 | 331 | 34.3 (30.2-38.4) | 213 | 36.2 (28.9-43.5) | 436 | 31.9 (27.4-36.4) | 407 | 30.9 (26.9-35.0) |
| 30-34 | 243 | 23.0 (19.5-26.6) | 143 | 16.7 (12.0-21.4) | 289 | 23.4 (19.4-27.3) | 298 | 22.4 (18.8-26.1) |
| ≥35 | 115 | 10.5 (7.9-13.0) | 88 | 15.5 (9.9-21.1) | 144 | 13.7 (10.3-17.2) | 169 | 10.7 (8.2-13.3) |
| Education | ||||||||
| <High school | 172 | 17.8 (14.3-21.3) | 92 | 20.4 (13.3-27.5) | 208 | 13.7 (10.5-16.9) | 184 | 14.0 (10.9-17.2) |
| High school diploma or GED | 335 | 38.7 (34.4-42.9) | 204 | 32.6 (25.7-39.4) | 442 | 36.7 (31.9-41.4) | 476 | 37.8 (33.5-42.1) |
| Some college or more | 475 | 43.5 (37.1-50.0) | 305 | 47.1 (35.8-58.3) | 607 | 49.6 (41.6-57.7) | 613 | 48.2 (41.1-55.3) |
| Per capita household income (quartiles) | ||||||||
| <$4000 | 223 | 21.6 (18.0-25.2) | 98 | 15.3 (9.4-21.2) | 248 | 16.1 (12.4-19.7) | 240 | 21.7 (17.9-25.5) |
| $4000 to <$8000 | 218 | 23.1 (19.3-26.8) | 163 | 31.9 (24.6-39.3) | 319 | 24.0 (20.0-28.0) | 316 | 26.6 (22.5-30.7) |
| $8000 to <$15 000 | 244 | 28.5 (24.5-32.5) | 150 | 26.4 (19.5-33.3) | 345 | 30.1 (25.6-34.6) | 319 | 25.2 (21.3-29.1) |
| ≥$15 000 | 235 | 26.8 (23.0-30.7) | 180 | 26.4 (20.6-32.2) | 277 | 29.9 (25.3-34.4) | 328 | 26.5 (22.5-30.4) |
| Race and ethnicity | ||||||||
| Non-Hispanic Black | 192 | 19.6 (16.3-22.9) | 115 | 16.3 (11.0-21.5) | 401 | 15.0 (13.1-17.0) | 80 | 5.9 (3.9-8.0) |
| Hispanic | 71 | 6.9 (5.0-8.8) | 44 | 6.6 (2.6-10.5) | 131 | 7.4 (5.8-9.1) | 78 | 5.9 (3.7-8.0) |
| Non-Hispanic White | 500 | 64.5 (60.6-68.3) | 259 | 68.5 (62.5-74.5) | 346 | 65.6 (63.1-68.2) | 929 | 80.7 (77.4-84.0) |
| Other or multiple raceb | 222 | 9.0 (7.0-11.1) | 185 | 8.7 (6.5-10.9) | 385 | 11.9 (10.5-13.3) | 188 | 7.5 (5.5-9.5) |
| Pregnancy intention | ||||||||
| Not intended | 606 | 63.1 (58.9-67.3) | 351 | 59.3 (52.3-66.4) | 745 | 54.0 (49.2-58.9) | 719 | 56.6 (52.2-61.0) |
| Intended | 357 | 36.9 (32.7-41.1) | 245 | 40.7 (33.6-47.7) | 512 | 46.0 (41.1-50.8) | 545 | 43.4 (39.0-47.8) |
| Felt down or depressed before pregnancy | ||||||||
| No | 632 | 65.4 (61.3-69.5) | 376 | 61.0 (53.5-68.5) | 847 | 64.1 (59.3-68.9) | 764 | 62.3 (58.0-66.6) |
| Yes | 348 | 34.6 (30.5-38.7) | 229 | 39.0 (31.5-46.5) | 417 | 35.9 (31.1-40.7) | 514 | 37.7 (33.4-42.0) |
| Experienced violence before pregnancy | ||||||||
| No | 819 | 83.5 (80.2-86.8) | 522 | 84.3 (78.3-90.4) | 1097 | 89 (86.4-91.6) | 1111 | 87.3 (84.2-90.3) |
| Yes | 165 | 16.5 (13.2-19.8) | 86 | 15.7 (9.6-21.7) | 176 | 11.0 (8.4-13.6) | 157 | 12.7 (9.7-15.8) |
| Month of prenatal care initiation, mean (95% CI) | 3.3 | 3.1-3.5 | 3.1 | 2.8-3.5 | 2.9 | 2.8-3.1 | 2.8 | 2.7-3.0 |
| Adequacy of prenatal care | ||||||||
| Not adequate | 336 | 35.9 (31.6-40.2) | 202 | 33.6 (26.3-40.9) | 385 | 24.9 (20.8-29.0) | 319 | 25.0 (21.2-28.8) |
| Adequate | 594 | 64.1 (59.8-68.4) | 376 | 66.4 (59.1-73.7) | 827 | 75.1 (71.0-79.2) | 955 | 75.0 (71.2-78.8) |
| Postpartum health care visit | ||||||||
| No | 216 | 21.0 (17.5-24.6) | 112 | 19.2 (12.8-25.6) | 245 | 14.5 (11.3-17.6) | 213 | 16.4 (13.1-19.7) |
| Yes | 765 | 79.0 (75.4-82.5) | 495 | 80.8 (74.4-87.2) | 1027 | 85.5 (82.4-88.7) | 1060 | 83.6 (80.3-86.9) |
Abbreviation: GED, General Educational Development.
All numbers are weighted and all percentages and means are weighted to account for the complex sampling design of the Pregnancy Risk Assessment Monitoring System survey.
Includes women who self-reported multiple races and women who self-reported their race as Alaska Native, American Indian, Chinese, Filipino, Hawaiian, Japanese, other Asian, race other than White, or mixed race.
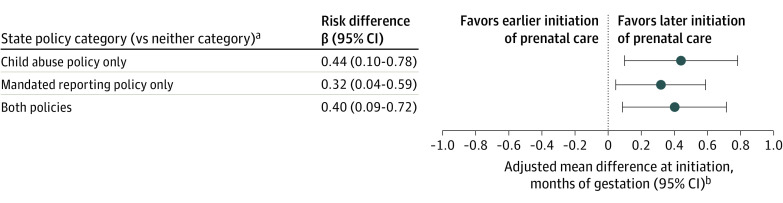
In adjusted models, women who delivered in states with a child abuse policy only (β = 0.44; 95% CI, 0.10-0.78), a mandated reporting policy only (β = 0.32; 95% CI, 0.04-0.59), or both policies (β = 0.40; 95% CI, 0.09-0.72) initiated prenatal care, on average, at a later month of gestation than women who delivered in states with neither policy (Figure 1 and eTable 3 in the Supplement). On average, women who delivered in states with a child abuse policy only initiated prenatal care at 2.6 months of gestation (95% CI, 1.6-3.5 months of gestation), in states with a mandated reporting policy only at 2.4 months of gestation (95% CI, 1.7-3.2 months of gestation), in states with both policies at 2.5 months of gestation (95% CI, 1.8-3.2 months of gestation), and in states with neither policy at 2.1 months of gestation (95% CI, 1.3-3.0 months of gestation).
Figure 1. Mean Difference in Month of Gestation at Prenatal Care Initiation by State Prenatal Substance Use Policies.
aAmong 4155 births to women who reported substance use during pregnancy.
bAdjusted for maternal age, education, race and ethnicity, per capita household income, pregnancy intention, mental health prior to pregnancy, and experiences of violence prior to pregnancy and for state-level Presumptive Eligibility for Medicaid, Expanded Family Planning under Medicaid, Medicaid expansion, priority access to substance use disorder treatment for pregnant people, targeted substance use disorder treatment programs for pregnant people, medical marijuana legalization, and number of obstetricians/gynecologists per 100 000 female population.
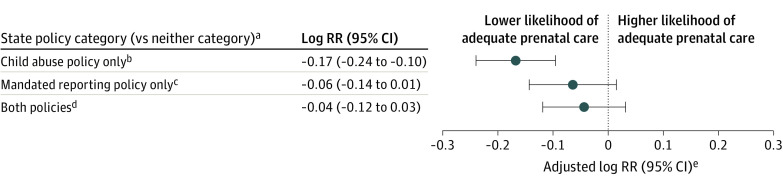
Women who delivered in states with a child abuse policy only (RR, 0.85; 95% CI, 0.79-0.91), a mandated reporting policy only (RR, 0.94; 95% CI, 0.87-1.01), or both policies (RR, 0.95; 95% CI, 0.89-1.03) had a lower likelihood of adequate prenatal care than women who delivered in states with neither policy (Figure 2 and eTable 4 in the Supplement). Women in states with a child abuse policy only, mandated reporting policy only, and both policies were 17.6%, 6.4%, and 5.2% less likely to receive adequate prenatal care than those who delivered in states with neither policy (as determined by the equation [(1 / RR) − 1] × 100).
Figure 2. Risk Ratios (RRs) Comparing Adequacy of Prenatal Care by State Prenatal Substance Use Policies.
aAmong 4155 births to women who reported substance use during pregnancy.
bRR, 0.85 (95% CI, 0.79-0.91).
cRR, 0.94 (95% CI, 0.87-1.01).
dRR, 0.95 (95% CI, 0.89-1.03).
eAdjusted for maternal age, education, race and ethnicity, per capita household income, pregnancy intention, mental health prior to pregnancy, and experiences of violence prior to pregnancy and for state-level Presumptive Eligibility for Medicaid, Expanded Family Planning under Medicaid, Medicaid expansion, priority access to substance use disorder treatment for pregnant people, targeted substance use disorder treatment programs for pregnant people, medical marijuana legalization, and number of obstetricians/gynecologists per 100 000 female population.
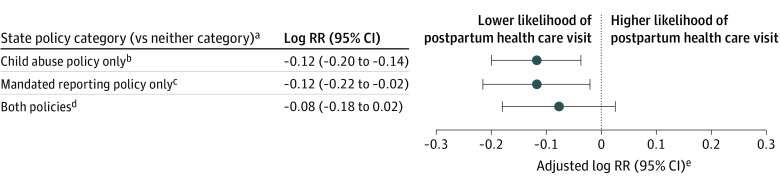
Women who delivered in states with a child abuse policy only (RR, 0.89; 95% CI, 0.82-0.96), a mandated reporting policy only (RR, 0.89, 0.80-0.98), and both policies (RR, 0.92; 95% CI, 0.82-1.02) had a lower likelihood of a postpartum health care visit than women who delivered in states with neither policy (Figure 3 and eTable 4 in the Supplement). Women in these states were 8.7% to 12.4% less likely to have a postpartum visit 4 to 6 weeks after delivery than those who delivered in states with neither policy.
Figure 3. Risk Ratios (RRs) Comparing Receipt of a Postpartum Health Care Visit by State Prenatal Substance Use Policies.
aAmong 4155 births to women who reported substance use during pregnancy.
bRR, 0.89 (95% CI, 0.82-0.96).
cRR, 0.89 (95% CI, 0.80-0.98).
dRR, 0.92 (95% CI, 0.83-1.02).
eAdjusted for maternal age, education, race/ethnicity, per capita household income, pregnancy intention, mental health prior to pregnancy, and experiences of violence prior to pregnancy and state-level Presumptive Eligibility for Medicaid, Expanded Family Planning under Medicaid, Medicaid expansion, priority access to substance use disorder treatment for pregnant people, targeted substance use disorder treatment programs for pregnant people, medical marijuana legalization, and number of obstetricians/gynecologists per 100 000 female population.
Although some 95% CIs overlapped with the null value of 1.0 for RRs, the overlap was small, and the location of the 95% CIs was consistent with a decreased likelihood of adequate prenatal care for women who delivered in states with a mandated reporting policy only or both policies and a decreased likelihood of a postpartum health care visit for women who delivered in states with both policies compared with those who delivered in states with neither policy.
Discussion
Overall, the results of this cross-sectional study indicate that child abuse policies and mandated reporting policies are associated with reduced receipt of prenatal and postpartum care among women who engaged in substance use during pregnancy according to data from the 2016-2019 PRAMS surveys. Specifically, we found that women who reported prenatal substance use and delivered in states with a child abuse policy only, a mandated reporting policy only, or both policies initiated prenatal care later, were less likely to receive adequate prenatal care, and were less likely to have a postpartum health care visit than those who delivered in states with neither policy. These results are consistent with previous research that showed reduced admissions to SUD treatment among pregnant people in states with these policies.9,10,11 Our research supports statements issued by leading public health and medical organizations,7,8 suggesting that child abuse policies and mandated reporting policies may deter pregnant people who engage in substance use from receiving essential care and treatment.
In adjusted analyses, results indicated that initiation of prenatal care was latest among women who reported substance use during pregnancy and delivered in states with a child abuse policy only or both policies, with those who delivered in these states initiating prenatal care on average at 2.6 and 2.5 months of gestation, respectively, compared with 2.1 months of gestation among women who reported substance use during pregnancy and delivered in states with neither policy. Although the absolute difference in the month of gestation at prenatal care initiation was small between these groups, previous research has shown that women who engage in substance use during pregnancy initiate prenatal care later than those who do not.26,27 Our results indicate that child abuse policies and mandated reporting policies are associated with further delays in prenatal care in this population.
Similarly, results from adjusted analyses indicated that the likelihood of adequate prenatal care was lowest for women who reported substance use during pregnancy and delivered in states with a child abuse policy only, with women in these states being 18% less likely to receive adequate prenatal care than those who delivered in states with neither policy. These results suggest that even if people who engage in substance use during pregnancy initiate prenatal care, they are less likely to receive the recommended number of visits under these policies, particularly in states with child abuse policies.
For postpartum health care, results from adjusted analyses showed that women who reported substance use during pregnancy and delivered in states with a child abuse policy only, a mandated reporting policy only, or both policies were 9% to 12% less likely to have a postpartum health care visit 4 to 6 weeks after delivery than those who delivered in states with neither policy. As with prenatal care, previous studies have shown that people who engage in substance use during pregnancy are less likely to receive timely postpartum care than those who do not,26 and our results indicate that these policies are associated with further reductions in postpartum care in this population.
Prenatal and postpartum care are critical to healthy outcomes, with previous research demonstrating multiple benefits for caregivers and infants in the context of prenatal substance use. In this population, early and consistent prenatal care is associated with a reduced risk of preterm birth and low birth weight.15 Prenatal and postpartum care also offer opportunities for health care professionals to make referrals to evidence-based SUD treatment and harm reduction services to further promote healthy outcomes and prevent harms, including overdose and acquisition and transmission of infectious diseases.16,17,18,19,28,29 However, qualitative studies have consistently indicated that delayed or inconsistent prenatal and postpartum care among pregnant people who engage in substance use is tied to the role of health care professionals as mandated reporters and caregivers’ fears of loss of infant custody, with child abuse policies and mandated reporting policies amplifying these fears and hindering engagement in care.14,30,31 These fears have been supported by recent research showing that child abuse policies and mandated reporting policies are associated with lower rates of family reunification among infants in foster care because of parental substance use.12 Importantly, our results showing a higher percentage of births to non-Hispanic Black women in states with a child abuse policy only, mandated reporting policy only, or both policies than in states with neither policy indicate that these policies have the potential to exacerbate the effects of structural racism and worsen existing inequities in prenatal and postpartum care,32 SUD treatment,16,33 and child welfare involvement34 by race and ethnicity.
Limitations
This study has several limitations. First, information on substance use during pregnancy was based on women’s self-report at 2 to 6 months post partum. Although PRAMS survey responses are confidential, because of social desirability, some women may not have disclosed substance use during pregnancy and thus been excluded from our analyses. This limitation could potentially result in selection bias if women who did and did not disclose substance use differed with respect to prenatal and postpartum care and whether they delivered in states with child abuse policies and mandated reporting policies. Specifically, if women who did not disclose prenatal substance use were less likely to engage in prenatal and postpartum care and were more likely to deliver in states with child abuse policies and mandated reporting policies, this would have biased our results toward the null. Of note, previous studies have indicated that self-reported data from the PRAMS survey, particularly for sensitive topics such as smoking during pregnancy, result in improved ascertainment compared with other data sources, including birth certificate data,35,36 because PRAMS responses are confidential. Second, given sample size limitations, we were unable to conduct analyses by type of prenatal substance use (eg, prescription opioids, marijuana, illicit drugs). Results may differ depending on the types of substances used prenatally. We also did not have data on the timing, quantity, and duration of prenatal substance use, which may provide more nuanced insights. Third, although we adjusted the multivariable analyses for a comprehensive set of confounders, unmeasured confounding may exist, specifically confounding due to unmeasured differences between states. To assess the potential for unmeasured confounding to bias results, we calculated E-values (eTable 5 in the Supplement), which indicate the strength of an association on the RR scale that an unmeasured confounder would need to have with the exposure and outcome to account for observed associations.37 The association of an unmeasured confounder with all policy categories and the outcomes would need to be moderate or strong to fully explain the results. Finally, although states may adopt similar policies, there is often variation in policy implementation. We did not have data on how child abuse policies and mandated reporting policies are implemented across states. Future qualitative research is needed to explore variation in policy implementation from the perspective of health care professionals, child welfare social workers, and pregnant people and how these variations affect care.
Conclusions
A recent report from the CDC on state strategies to address substance use and SUD among pregnant and postpartum populations found that only 2 of 12 states were considering strategies to address ethical, legal, and social factors, including child abuse policies and mandated reporting policies, that affect engagement in treatment and care.38 Our results underscore the importance of more widespread consideration of these strategies, specifically strategies that take a more supportive, nonstigmatizing approach to addressing the needs of pregnant people who engage in substance use.
eTable 1. State Prenatal Substance Use Policy Categorization
eFigure. Conceptual Diagram
eTable 2. Data Sources for State-Level Covariates
eTable 3. Mean Difference in Month of Gestation at Prenatal Care Initiation by State Prenatal Substance Use Policies
eTable 4. Risk Ratios Comparing Adequacy of Prenatal Care and Receipt of a Postpartum Health Care Visit by State Prenatal Substance Use Policies
eTable 5. E-Values for Observed Associations
References
- 1.2020 National Survey on Drug Use and Health (NSDUH) Releases. Substance Abuse and Mental Health Services Administration . 2021. Accessed May 6, 2022. https://www.samhsa.gov/data/release/2020-national-survey-drug-use-and-health-nsduh-releases
- 2.Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA. 2021;325(2):146-155. doi: 10.1001/jama.2020.24991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Admon LK, Bart G, Kozhimannil KB, Richardson CR, Dalton VK, Winkelman TNA. Amphetamine- and opioid-affected births: incidence, outcomes, and costs, United States, 2004–2015. Am J Public Health. 2019;109(1):148-154. doi: 10.2105/AJPH.2018.304771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baer RJ, Chambers CD, Ryckman KK, Oltman SP, Rand L, Jelliffe-Pawlowski LL. Risk of preterm and early term birth by maternal drug use. J Perinatol. 2019;39(2):286-294. doi: 10.1038/s41372-018-0299-0 [DOI] [PubMed] [Google Scholar]
- 5.Jarlenski M, Krans EE, Chen Q, et al. Substance use disorders and risk of severe maternal morbidity in the United States. Drug Alcohol Depend. 2020;216:108236. doi: 10.1016/j.drugalcdep.2020.108236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parental substance use as child abuse. Child Welfare Information Gateway . July 2019. Accessed November 3, 2021. https://www.childwelfare.gov/topics/systemwide/laws-policies/statutes/parentalsubstanceuse
- 7.Loertscher v Anderson and Schimel, case 14-cv-870, document 47. American Public Health Association . July 28, 2017. Accessed November 3, 2021. https://www.apha.org/-/media/files/pdf/advocacy/briefs/170728_loertscher_7circuit.ashx
- 8.Substance abuse reporting and pregnancy: the role of the obstetrician–gynecologist. American College of Obstetricians and Gynecologists Committee on Health Care for Underserved Women . January 2011. Accessed November 3, 2021. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2011/01/substance-abuse-reporting-and-pregnancy-the-role-of-the-obstetrician-gynecologist
- 9.Atkins DN, Durrance CP. State policies that treat prenatal substance use as child abuse or neglect fail to achieve their intended goals. Health Aff (Millwood). 2020;39(5):756-763. doi: 10.1377/hlthaff.2019.00785 [DOI] [PubMed] [Google Scholar]
- 10.Kozhimannil KB, Dowd WN, Ali MM, Novak P, Chen J. Substance use disorder treatment admissions and state-level prenatal substance use policies: evidence from a national treatment database. Addict Behav. 2019;90:272-277. doi: 10.1016/j.addbeh.2018.11.019 [DOI] [PubMed] [Google Scholar]
- 11.Gressler LE, Shah S, Shaya FT. Association of criminal statutes for opioid use disorder with prevalence and treatment among pregnant women with commercial insurance in the United States. JAMA Netw Open. 2019;2(3):e190338-e190338. doi: 10.1001/jamanetworkopen.2019.0338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanmartin MX, Ali MM, Lynch S, Aktas A. Association between state-level criminal justice–focused prenatal substance use policies in the US and substance use–related foster care admissions and family reunification. JAMA Pediatr. 2020;174(8):782-788. doi: 10.1001/jamapediatrics.2020.1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice. 2015;3(1):2. doi: 10.1186/s40352-015-0015-5 [DOI] [Google Scholar]
- 14.Syvertsen JL, Toneff H, Howard H, Spadola C, Madden D, Clapp J. Conceptualizing stigma in contexts of pregnancy and opioid misuse: a qualitative study with women and healthcare providers in Ohio. Drug Alcohol Depend. 2021;222:108677. doi: 10.1016/j.drugalcdep.2021.108677 [DOI] [PubMed] [Google Scholar]
- 15.El-Mohandes A, Herman AA, Nabil El-Khorazaty M, Katta PS, White D, Grylack L. Prenatal care reduces the impact of illicit drug use on perinatal outcomes. J Perinatol. 2003;23(5):354-360. doi: 10.1038/sj.jp.7210933 [DOI] [PubMed] [Google Scholar]
- 16.Austin AE, Bona VD, Cox ME, Proescholdbell S, Fliss MD, Naumann RB. Prenatal use of medication for opioid use disorder and other prescription opioids in cases of neonatal opioid withdrawal syndrome: North Carolina Medicaid, 2016–2018. Am J Public Health. 2021;111(9):1682-1685. doi: 10.2105/AJPH.2021.306374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nielsen T, Bernson D, Terplan M, et al. Maternal and infant characteristics associated with maternal opioid overdose in the year following delivery. Addiction. 2020;115(2):291-301. doi: 10.1111/add.14825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tuten M, Fitzsimons H, Hochheimer M, Jones HE, Chisolm MS. The impact of early substance use disorder treatment response on treatment outcomes among pregnant women with primary opioid use. J Addict Med. 2018;12(4):300-307. doi: 10.1097/ADM.0000000000000397 [DOI] [PubMed] [Google Scholar]
- 19.Wright TE, Schuetter R, Fombonne E, Stephenson J, Haning WF III. Implementation and evaluation of a harm-reduction model for clinical care of substance using pregnant women. Harm Reduct J. 2012;9(1):5. doi: 10.1186/1477-7517-9-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shulman HB, D’Angelo DV, Harrison L, Smith RA, Warner L. The Pregnancy Risk Assessment Monitoring System (PRAMS): overview of design and methodology. Am J Public Health. 2018;108(10):1305-1313. doi: 10.2105/AJPH.2018.304563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Substance use during pregnancy. Guttmacher Institute . Updated October 1, 2021. Accessed November 3, 2021. https://www.guttmacher.org/state-policy/explore/substance-use-during-pregnancy
- 22.Kotelchuck M. An evaluation of the Kessner adequacy of prenatal care index and a proposed adequacy of prenatal care utilization index. Am J Public Health. 1994;84(9):1414-1420. doi: 10.2105/AJPH.84.9.1414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hayes-Larson E, Kezios KL, Mooney SJ, Lovasi G. Who is in this study, anyway? guidelines for a useful Table 1. J Clin Epidemiol. 2019;114:125-132. doi: 10.1016/j.jclinepi.2019.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702-706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 25.Statement on statistical significance and P values. American Statistical Association . 2016. Accessed November 3, 2021. https://www.amstat.org/asa/files/pdfs/P-ValueStatement.pdf
- 26.Simmons E, Austin AE. Association of prenatal substance use with prenatal and postpartum care: evidence from the Pregnancy Risk Assessment Monitoring System, 2016-2019. Prev Med. 2022;159:107065. doi: 10.1016/j.ypmed.2022.107065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schempf AH, Strobino DM. Drug use and limited prenatal care: an examination of responsible barriers. Am J Obstet Gynecol. 2009;200(4):412.e1-412.e10. doi: 10.1016/j.ajog.2008.10.055 [DOI] [PubMed] [Google Scholar]
- 28.Schiff DM, Nielsen T, Terplan M, et al. Fatal and nonfatal overdose among pregnant and postpartum women in Massachusetts. Obstet Gynecol. 2018;132(2):466-474. doi: 10.1097/AOG.0000000000002734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smid MC, Stone NM, Baksh L, et al. Pregnancy-associated death in Utah: contribution of drug-induced deaths. Obstet Gynecol. 2019;133(6):1131-1140. doi: 10.1097/AOG.0000000000003279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Renbarger KM, Shieh C, Moorman M, Latham-Mintus K, Draucker C. Health care encounters of pregnant and postpartum women with substance use disorders. West J Nurs Res. 2020;42(8):612-628. doi: 10.1177/0193945919893372 [DOI] [PubMed] [Google Scholar]
- 31.Paris R, Herriott AL, Maru M, Hacking SE, Sommer AR. Secrecy versus disclosure: women with substance use disorders share experiences in help seeking during pregnancy. Matern Child Health J. 2020;24(11):1396-1403. doi: 10.1007/s10995-020-03006-1 [DOI] [PubMed] [Google Scholar]
- 32.Gadson A, Akpovi E, Mehta PK. Exploring the social determinants of racial/ethnic disparities in prenatal care utilization and maternal outcome. Semin Perinatol. 2017;41(5):308-317. doi: 10.1053/j.semperi.2017.04.008 [DOI] [PubMed] [Google Scholar]
- 33.Peeler M, Gupta M, Melvin P, et al. Racial and ethnic disparities in maternal and infant outcomes among opioid-exposed mother–infant dyads in Massachusetts (2017–2019). Am J Public Health. 2020;110(12):1828-1836. doi: 10.2105/AJPH.2020.305888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim H, Wildeman C, Jonson-Reid M, Drake B. Lifetime prevalence of investigating child maltreatment among US children. Am J Public Health. 2017;107(2):274-280. doi: 10.2105/AJPH.2016.303545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allen AM, Dietz PM, Tong VT, England L, Prince CB. Prenatal smoking prevalence ascertained from two population-based data sources: birth certificates and PRAMS questionnaires, 2004. Public Health Rep. 2008;123(5):586-592. doi: 10.1177/003335490812300508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tong VT, Dietz PM, Farr SL, D’Angelo DV, England LJ. Estimates of smoking before and during pregnancy, and smoking cessation during pregnancy: comparing two population-based data sources. Public Health Rep. 2013;128(3):179-188. doi: 10.1177/003335491312800308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 38.Kroelinger CD, Rice ME, Cox S, et al. State strategies to address opioid use disorder among pregnant and postpartum women and infants prenatally exposed to substances, including infants with neonatal abstinence syndrome. MMWR Morb Mortal Wkly Rep. 2019;68(36):777-783. doi: 10.15585/mmwr.mm6836a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. State Prenatal Substance Use Policy Categorization
eFigure. Conceptual Diagram
eTable 2. Data Sources for State-Level Covariates
eTable 3. Mean Difference in Month of Gestation at Prenatal Care Initiation by State Prenatal Substance Use Policies
eTable 4. Risk Ratios Comparing Adequacy of Prenatal Care and Receipt of a Postpartum Health Care Visit by State Prenatal Substance Use Policies
eTable 5. E-Values for Observed Associations