Abstract
Background
Dysmenorrhea refers to a cyclical lower abdomen or pelvic discomfort
that commonly radiates to the back or thighs. It has a significant influence on women's quality of life (QOL), social duties, and career roles. As pain relief without or with minimal use of medication is a primary health care target, usage of non-pharmacological measures is the most prominent way of managing dysmenorrhea. In this study, we explored the quality of life and the importance of non-pharmacological treatment of dysmenorrhea.
Materials & methods
A prospective, cross-sectional, and interventional study was conducted on general residents of India for six months. Women who gave consent to participate in the study and were suffering from primary dysmenorrhea were included in the study. All relevant and necessary information was collected using online questionnaire forms and interviews with the subjects.
Results
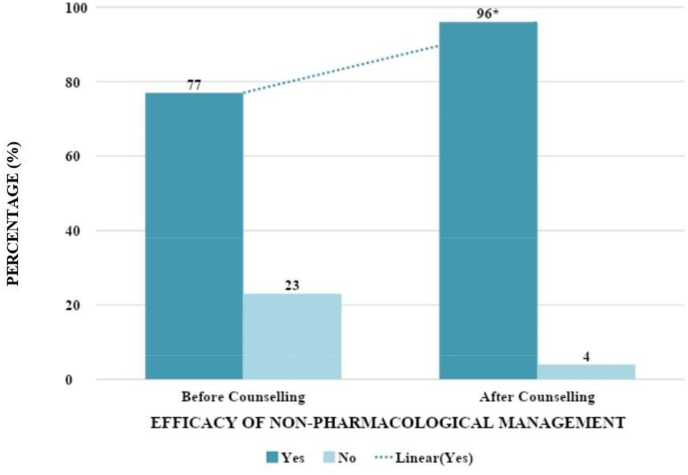
Out of a total of 517 individuals, 348 completed the study, with 51.1% having an average QOL, 33.3% having a bad QOL, and 14.9% having a good QOL. After the intervention, individuals' attitudes toward the role of non-pharmacological care in dysmenorrhea shifted significantly, with 96% of subjects believing that the actions taken were beneficial, compared to just 77% previously.
Conclusion
The current study suggests that the negative effect on health-related problems can be managed by following non-pharmacological measures regularly. Further research is needed to uncover new alternatives and offer a wider choice of treatments.
Keywords: Dysmenorrhea, Menstrual pain, Non-pharmacological management, Primary dysmenorrhea, Quality of life
Highlights
-
•
This study outlines the effect of dysmenorrhea by assessing factors contributing to discomfort and pain during menstruation.
-
•
It also adds to the literature by proving that dysmenorrhea affects the quality of life.
-
•
It indicates that non-pharmacological measures are both safe and effective in treating dysmenorrhea.
-
•
It reflects the need for more research and the application of alternate approaches for alleviating menstrual pain.
-
•
This research also aided in educating young generations on the myths and truths surrounding menstruation and its management.
1. Introduction
Dysmenorrhea refers to a medical condition characterized by severe uterine pain around the time of menstruation, manifesting as pelvic or cyclic lower abdominal pain radiating to the back and thighs [1]. The most prevalent gynecological condition in women is dysmenorrhea, which many women fail to report in medical interviews. Its frequency in the general population ranges from 16.8% to 81%, with rates as high as 90% [2]. Besides gynecological issues, primary dysmenorrhea is a significant problem in regards to public health, occupational health, and family concerns as it has a bad impact on quality of life as well as the economy due to recurrent absenteeism from school and work [3].
Nearly 10% of dysmenorrheic women have severe symptoms, which can leave them bedridden for a minimum of one to three days during each menstruation. This condition not only has a huge influence on human health but also on their quality of life. Despite its widespread prevalence and the resulting considerable impairment in quality of life, including school and work absences, this illness has gotten remarkably little scientific attention. The theological and traditional attitudes concerning menstruation could be at the core of the two-way failure of omission or lack of communication. One possible clinical aspect of its underestimation is that because dysmenorrhea is so widespread, many adolescent and adult women regard it as a “normal” ailment that they do not need to disclose, while their physician does not inquire [4].
Dysmenorrhea is categorized as primary and secondary dysmenorrhea. Primary dysmenorrhea occurs during menstruation in the absence of any other pelvic disease, whereas secondary dysmenorrhea involves pelvic pathologies such as fibroids, adenomyosis, and pelvic inflammatory disease [5]. It is commonly associated with psychological fear, heavy menstrual flow, and longer menstrual periods [6].
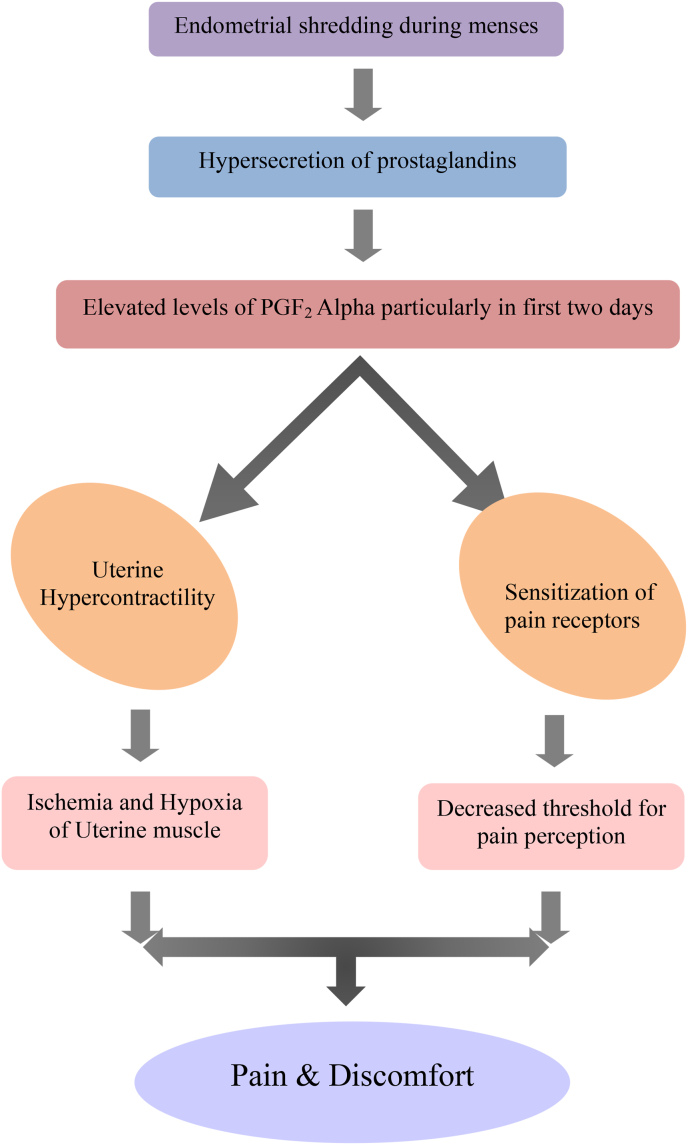
Early menarche, a favorable family history, higher or lower BMI, nulliparity, smoking, and psychological conditions such as depression and anxiety are all risk factors for dysmenorrhea [4]. The hypersecretion of uterine prostaglandins is the most widely acknowledged explanation for the pathology of primary dysmenorrhea. Myometrial hypercontractility is thought to be caused by increased production of prostaglandins from disintegrating cells during endometrial shredding, which further results in ischemia and hypoxia of the uterine muscle, and eventually pain and discomfort (Fig. 1) [7]. Common symptoms of dysmenorrhea include severe, intermittent painful spasms, typically in the suprapubic area. It is usually associated with other systematic symptoms sudich as backache, nausea, vomiting, diarrhea, sweating, syncope, tachycardia, malaise, exhaustion, and headache [8].
Fig. 1.
Pathophysiology of primary dysmenorrhea..
Primary dysmenorrhea can be treated pharmacologically as well as non-pharmacologically. Pharmacological treatment involves non-hormonal therapy and hormonal therapy. Non-hormonal medical therapy consists of acetaminophen, pamabrom, and non-steroidal anti-inflammatory drugs (NSAIDs) [9]. Hormonal therapy is composed of Combined Oral Contraceptives (COC) and progestin regimens. Both hormonal and non-hormonal pharmacological therapies can produce a variety of adverse effects [10]. None of these treatments are extremely successful. Instead, some of them may cause addiction or have an impact on cognitive function [11]. Non-pharmacological treatments should be emphasized more because they are simple to use and have no negative health effects [12]. Primary dysmenorrhea can be treated with a variety of alternative nonpharmacological methods, including self-care strategies such as exercise, rest, dietary modifications, and cold and heat therapy, which can ease menstrual pain. Acupuncture and aromatherapy have also been employed as supplementary alternative medical therapies for primary dysmenorrhea. However, there is limited evidence to support their effectiveness [13]. The current study highlights the effect of dysmenorrhea on individuals’ quality of life and evaluates the efficacy of non-pharmacological management in managing menstrual aches.
2. Methods
A randomized cross-sectional study was conducted on the general population of India. Based on the literature review of previous studies, a sample size of 250–300 was considered enough to obtain a valid result. In order to increase the study validity, we included as many respondents as possible. The total sample size was 348 participants. It was a prospective study that included 348 women in the age group of 12–40 years. Participants with primary dysmenorrhea who were willing to sign the consent form were included in the study, while those who did not complete the form or disagreed with the suggested interventions were excluded.
This internet-medicated interventional study follows the guidelines and ethical principles of the British Psychological Society [14]. This study was reported in line with the STROCSS criteria [15]. The study was registered and approved by the institutional human ethical committee of St. Pauls College of Pharmacy, Hyderabad, Telangana, India (UIN: SPCP/2020-21/IHEC/001).
Data was collected using a self-designed questionnaire that included questions about demographics, menstruation, and dysmenorrhea patterns, as well as management. Menstruation patterns, dietary habits, the types of symptoms experienced during menstruation, and the measures taken to alleviate them, as well as pharmacological and non-pharmacological treatment patterns, were all evaluated. The subjects were divided into four groups based on the World Health Organization's BMI criteria: underweight, normal, overweight, and obese. Intervention regarding non-pharmacological management was provided verbally and through patient information leaflets.
3. Statistics
The statistical analysis was performed using Statistical Package for Social Sciences (SPSS) software for Windows (version 27.0, 2021; SPSS, Inc., Chicago, IL). The Chi-square (χ2) test, McNemar's, and independent t-test were used for the analysis. A p-value of less than 0.05 was considered to be significant.
4. Results
In the current study, out of 517 participants, 348 met inclusion criteria, and the remaining were excluded as they were either categorized as non-dysmenorrheic or secondary dysmenorrheic. The subjects who were not in compliance with the study or non-cooperative during or at any step of the study were also excluded.
The mean age of the subjects who participated in the study was found to be 21.99 ± 3.75 years (12–45). The mean height and weight of the subjects were found to be 158.6 ± 7.5 and 53.1 ± 9.9, respectively. The results were overwhelming that more than half of the subjects had normal BMI and only 41% were with abnormal, among which 25% were underweight, 14% were overweight, and 2% accounted for the obese category. Almost all of those who took part were in their graduation or higher, 4% were in intermediate school, and less than 2% were in secondary school. When the participants were evaluated in terms of dietary habits and area of living, individuals with a mixed diet were way more than that vegetarians. Nearly three fourth of the subjects were from urban areas, and the rest were from rural areas.
The age of menarche was <12 years in more than ten percent of subjects, 12–15 years in maximum participants, and less than 10% of subjects who experienced their menarche over 15 years of age. The duration of the menstrual cycle was 15–20 days in some of the individuals, 21 to 35 in most of the subjects, and >35 days in just about 10%. In more than two third of the participants, menstruation was found to last for 3–5 days, whereas it lasted for <3 days or >6 days in the remaining population.
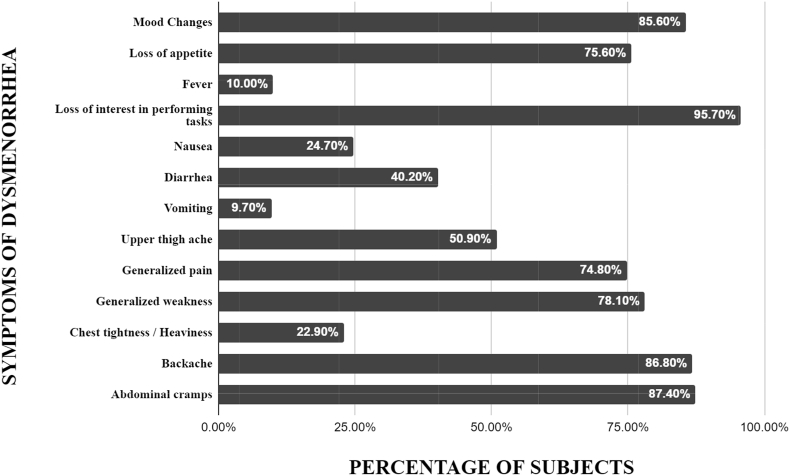
When enquired about comorbidities, 86.8% had no concomitant illness, whereas 13.2% were suffering from chronic diseases such as anemia, thyroid disorders 5.2% each, and others (2.9%). Others here include diabetes mellitus, depression, autoimmune diseases, and rheumatoid arthritis. In the study group, 67.2% of individuals were subjected to dysmenorrhea every month and 32.8% experienced it only in certain months of the year (such as 1–4 months or 5–6 months). From the start to the end of menstruation, most of the subjects reported a decreasing pattern of pain severity, 7.0% an increasing pattern, and 4.0% a fluctuating pattern. Almost half of the participants started experiencing dysmenorrhea from 1st menstruation onwards, 15.2% experienced it within a year after menarche, 12.1% after 1 year, and 31.3% experienced it after 2 or more years. When asked about possible causes of dysmenorrhea, participants chose unhealthy eating habits, stress, sedentary lifestyle, and physiological processes which accounted equally as the most likely reasons. Some think that dysmenorrhea is hereditary, and irregular sleep patterns are also a possible cause. Abdominal cramps, backaches, generalized weakness, generalized pain, upper thigh aches, nausea, vomiting, diarrhea, headaches, loss of appetite, loss of interest in daily activity, mood swings, chest tightness, and fever were reported as the symptoms of dysmenorrhea. Maximum individuals selected loss of interest in performing the task, abdominal cramps, backaches, mood changes, and generalized weakness, as these were the symptoms experienced by most of the subjects, and their frequencies are shown in Fig. 2. On evaluating participants for the effect of dysmenorrhea on QOL, only 14.9% fell under the good QOL category, whereas 51.1% and 33.3% had average and bad QOL, respectively. 21.6% of participants were taking medicine to manage their dysmenorrhea, whereas 86.2% preferred to rest, watching TV, mobile phones, and favorite shows (45.6%), dietary modifications (19.3%), hot and cold patches (18.7%), exercise (10.3%), and aromatherapy (3.7%). When investigated about pharmacological measures and their safety, 41.1% mentioned they were currently using medicines, of which 25.5% used dicyclomine, 7.75% used paracetamol, whereas 29% were in favor of NSAIDs like mefenamic acid (24.4%), diclofenac (2.87%), aceclofenac (1.14%), and piracetam (0.57%), and 0.57% of subjects mentioned tramadol will also help in managing dysmenorrhea. Subjects received information regarding various medicines from sources like elderly people at home (29%), doctors (21.2%), pharmacists (16.3%), friends (16%), and the internet (9.1%). 77.3% of participants said using medicines for menstrual aches is harmful, and 51.4% mentioned they will use non-pharmacological measures before taking pain relievers, whereas 29.3% use non-pharmacological measures less frequently, and 19.3% choose pharmacological measures without even trying non-pharmacological measures once.
Fig. 2.
Prevalence of symptoms of dysmenorrhea..
After the intervention, many of them opted for rest (79.9%) to manage their menstrual pain, followed by dietary modifications (50.8%), exercise (34.6%), hot and cold patches (32.4%), and aromatherapy (5.2%). The education level and presence of comorbidities are significantly associated with the efficacy of non-pharmacological measures. Table 1. The perspective toward the role of non-pharmacological management in dysmenorrhea notably changed after the intervention, as shown in Fig. 3.
Table 1.
Relation between various factors and effectiveness of non-pharmacological measures.
|
VARIABLES |
Non-Pharmacological Management Efficacy Before Counseling |
Non-Pharmacological Management Efficacy After Counseling |
||
|---|---|---|---|---|
| EFFECTIVE | NON-EFFECTIVE | EFFECTIVE | NON-EFFECTIVE | |
| HIGHEST EDUCATION LEVEL | ||||
| Secondary School | 0.4% | 5.0% | 0.9% | 14.3% |
| Intermediate | 4.5% | 2.5% | 4.2% | 0.0% |
| Under Graduate | 61.9% * | 76.3% | 65.3% | 64.3% |
| Post Graduate | 33.2% | 16.3% | 21.4% | 21.4% |
| DIETARY HABITS | ||||
| Mixed | 82.8% | 82.5% | 83.5% | 64.3% |
| Vegetarian | 17.2% | 17.5% | 16.5% | 35.7% |
| COMORBIDITIES | ||||
| No | 88.8% ** | 80.0% | 86.8% | 85.7% |
| Anemia | 4.9% | 6.3% | 5.1% | 7.1% |
| Thyroid | 3.7% | 10.0% | 5.1% | 7.1% |
| Others | 2.6% | 3.8% | 3.0% | 0.0% |
*p value = <0.01.
**p value = <0.05 (0.04).
Fig. 3.
Efficacy of non-pharmacological management among subjects..
The counseling provided was regarded as 99% efficient. After counseling and non-pharmacological measures, the percentage of subjects who felt their dysmenorrhea was out of control decreased from 37.9 to 13.2, with 86.8% (p 0.05) believing it was controllable. The feedback collected from participants after the intervention showed that 71.6% were very satisfied with the counseling, 28.2% were satisfied, and only 0.3% were not satisfied. 77.3% have reported that their knowledge and perception of dysmenorrhea have improved to a greater extent.
5. Discussion
This study was intended to evaluate the effect of dysmenorrhea on QOL and the role of non-pharmacological measures in the management of dysmenorrhea. Subjects of this study had varied beliefs about the causes of dysmenorrhea, where the physiological process and stress are the most possible causes, according to participants. This result is as per the study conducted by Chen X Chen et al. [16] to measure the symptoms of dysmenorrhea, where the loss of interest in performing tasks, mood disturbances, and abdominal cramps were the most prevalent symptoms among the study group, in compliance with Dawood, 1981, 1984; and [6] Kinch, 1985 [17].
This study did not show any significant association between BMI and dysmenorrhea. However, several observational studies such as a cross-sectional survey conducted on a sample of 2718 women to assess the relationship between body weight and menstrual pain [18], and a descriptive study conducted on 789 Thailand adolescents to determine the prevalence of dysmenorrhea [19], have found that BMI is related to dysmenorrhea QOL. Our study demonstrated that factors like educational level and the presence of comorbidities are associated with subjects’ perspectives on the efficacy of non-pharmacological management. Non-pharmacological management is particularly efficient in the treatment of dysmenorrhea, according to those with higher educational levels. However, non-pharmacological methods are ineffective in the treatment of menstrual discomfort, according to those with concurrent disorders. Prior literature on a correlational study among 531 school girls to test the relation between self-care behaviors and dysmenorrhea conducted in Hong Kong demonstrated that characteristics such as age, educational attainment, and menstrual health can influence how women manage dysmenorrhea [20]. The degree of discomfort could be due to the underlying illness state as well.
The current study showed a significant improvement in subjects' perspectives on the effectiveness of non-pharmacological measures in managing primary dysmenorrhea. This result is on par with other studies like a cross-sectional one, conducted with 2555 college girls to analyze the prevalence of dysmenorrhea against its management strategies, where the researchers found higher use of non-pharmacological measures was observed in severe dysmenorrhea and was effective [21]. In contrast, one observational study by Maria Laura Parra-Fernandez, et, al. which was conducted on 224 women to assess the management of dysmenorrhea, found no relation between the use of non-pharmacological management and pain intensity [22]. On follow-up, rest, physical activity, heat therapy, and dietary modifications were found to be more efficient among all the non-pharmacological measures suggested. This result is in agreement with Abbaspour et al., Noorbaksh mahvash et al., that physical activity is thought to be more effective in managing dysmenorrhea by students of the universities where these studies were conducted [22]. It is also in line with those of O'Connell et al. and Midilli et al., regarding the common non-pharmacological methods, especially local heat as a method of pain relief [23,24].
The low accessibility of the internet and other social media platforms to the general public remained the main limitation of the study. Measures were taken by approaching the people from different places in the country. Other limitations were the duration and sample size of the study. Extensive multicenter studies are necessary to obtain a better understanding of the management of dysmenorrhea and its effect on daily life activities.
6. Conclusion
Dysmenorrhea is a prominent concern among women today and is a highly prevalent gynecological problem. Changes in the regular menstrual patterns of women may have an impact on both physical and psychological well-being. The present study suggests that dysmenorrhea has a negative effect on the health-related quality of life. The results showed that following non-pharmacological measures regularly alleviated primary dysmenorrhea. Further research is necessary to identify new alternatives to offer a wider choice of treatments without overlooking the short and long-term implications for patients’ symptoms.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Ethical approval
This internet-medicated interventional study follows the guidelines and ethical principles of the British Psychological Society.
The study was registered and approved by the institutional ethical committee of St. Pauls College of Pharmacy, Hyderabad, Telangana, India (UIN: SPCP/2020-21/IHEC/001).
Consent
Participants have given their consent through an online procedure during data collection.
Author contribution
All the authors have contributed to the study equally.
Registration of research studies
-
1.
Name of the registry: Institutional human ethical committee of St. Pauls College of Pharmacy, Hyderabad, Telangana, India
-
2.
Unique Identifying number or registration ID: SPCP/2020-21/IHEC/001
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://drive.google.com/file/d/10D49jtk3bTSDqu2ROMWetVgAcQCan4Dz/view?usp=sharing
Guarantor
Dr. Keerthi Thatikonda, Ms. Prathiba Annam.
Declaration of competing interest
The authors have no relevant financial or non-financial interests to disclose.
Acknowledgements
The authors are grateful for the cooperation and help received from the management and students of St. Pauls College of Pharmacy, Hyderabad, Telangana, India.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.104407.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Deb S., Raine-Fennin Dysmenorrhoea N. Obstet. Gynaecol. Reprod. Med. 2008;18(11):294–299. [Google Scholar]
- 2.Ryan S.A. The treatment of dysmenorrhea. Pediatr. Clin. 2017;64(2):331–342. doi: 10.1016/j.pcl.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Polat A., Celik H., Gurates B., Kaya D., Nalbant M., Kavak E., et al. Prevalence of primary dysmenorrhea in young adult female university students. Arch. Gynecol. Obstet. 2009;279(4):527–532. doi: 10.1007/s00404-008-0750-0. [DOI] [PubMed] [Google Scholar]
- 4.Ballantyne J.C., CousinsPrimary Dysmenorrhea M. 2013. An Urgent Mandate. [Google Scholar]
- 5.Mohapatra D., Mishra T., Behera M., Panda P. A study of relation between body mass index and dysmenorrhea and its impact on daily activities of medical students. Asian J. Pharmaceut. Clin. Res. 2016;9(9):297–299. doi: 10.22159/ajpcr.2016.v9s3.14753. [DOI] [Google Scholar]
- 6.Dawood M.Y. In: Dysmenorrhea. Dawood M.Y., editor. Williams & Wilkins; Baltimore: 1981. Prostaglandins, hormones and dysmenorrhea; pp. 21–52. [Google Scholar]
- 7.Iacovides S., Avidon I., Baker F.C. What we know about primary dysmenorrhea today: a critical review. Hum. Reprod. Update. 2015;21(6):762–778. doi: 10.1093/humupd/dmv039. [DOI] [PubMed] [Google Scholar]
- 8.Mahvash N., Eidy A., Mehdi K. The effect of physical activity on primary dysmenorrhea of female university students. World Appl. Sci. J. 2012;17(10):1246–1252. [Google Scholar]
- 9.Burnett M., Lemyre M. No. 345-Primary dysmenorrhea consensus guideline. J. Obstet. Gynaecol. Can. 2017;39(7):585–595. doi: 10.1016/j.jogc.2016.12.023. [DOI] [PubMed] [Google Scholar]
- 10.Schrager S. Abnormal uterine bleeding associated with hormonal contraception. Am. Fam. Physician. 2002;65(10):2073–2080. [PubMed] [Google Scholar]
- 11.S Han S.H., Hur M.H., Buckle J., Choi J., Lee M.S. Effect of aromatherapy on symptoms of dysmenorrhea in college students: a randomized placebo-controlled clinical trial. J. Alternative Compl. Med. 2006;12(6):535–541. doi: 10.1089/acm.2006.12.535. [DOI] [PubMed] [Google Scholar]
- 12.Aboualsoltani F., et al. Non-pharmacological treatments of primary dysmenorrhea: a systematic review. Arch. Pharm. Pract. 2020;11(1):136–142. [Google Scholar]
- 13.Iacovides S., Avidon I., Baker F.C. What we know about primary dysmenorrhea today: a critical review. Hum. Reprod. Update. 2015;21(6):762–778. doi: 10.1093/humupd/dmv039. [DOI] [PubMed] [Google Scholar]
- 14.Ethics Guidelines for Internet-Mediated Research. British Psychological Society BPS; 7 Jan 2021. [Google Scholar]
- 15.Mathew G., Agha R., for the STROCSS Group Strocss 2021: strengthening the Reporting of cohort, cross-sectional and case-control studies in Surgery. Int. J. Surg. 2021;96 doi: 10.1016/j.ijsu.2021.106165. [DOI] [PubMed] [Google Scholar]
- 16.Chen C.X., Kwekkeboom K.L., Ward S.E. Self-report pain and symptom measures for primary dysmenorrhea: a critical review. Eur. J. Pain. 2015;19(3):377–391. doi: 10.1002/ejp.556. [DOI] [PubMed] [Google Scholar]
- 17.Kinch R. In: Premenstrual Syndrome and Dysmenorrhea. Dawood M.Y., McGuire J.L., Demers L.M., editors. Urban & Schwarzenberg; Baltimore: 1985. Dysmenorrhea: a historical perspective; pp. 79–85. [Google Scholar]
- 18.Hirata M., Kumabe K., Inove Y. Study of relation between frequency of menstrual pain and body weight in female adolescents. Nippon Koshu Eisei Zasshi. 2002;49:516–524. [PubMed] [Google Scholar]
- 19.Tangchai K., Titapant V., Boriboonhirunsarn D. Dysmenorrhea in Thai adolescents: prevalence, impact and knowledge of treatment. J. Med. Assoc. Thai. 2004;87(3):69–73. [PubMed] [Google Scholar]
- 20.Wong C.L., Ip W.Y., Choi K.C., Lam L.W. Examining self-care behaviors and their associated factors among adolescent girls with dysmenorrhea: an application of orem's self-care deficit nursing theory. J. Nurs. Scholarsh. 2015;47:219–227. doi: 10.1111/jnu.12134. [DOI] [PubMed] [Google Scholar]
- 21.Chen L., Tang L., Guo S., Kaminga A.C., Xu H. Primary dysmenorrhea and self-care strategies among Chinese college girls: a cross-sectional study. BMJ Open. 2019;9(9) doi: 10.1136/bmjopen-2018-026813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parra-Fernández M.L., Onieva-Zafra M.D., Abreu-Sánchez A., Ramos-Pichardo J.D., Iglesias-López M.T., Fernández-Martínez E. Management of primary dysmenorrhea among university students in the south of Spain and family influence. Int. J. Environ. Res. Publ. Health. 2020;17(15):5570. doi: 10.3390/ijerph17155570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O'Connell K., Davis A.R., Westhoff C. Self-treatment patterns among adolescent girls with dysmenorrhea. J. Pediatr. Adolesc. Gynecol. 2006;19:285–289. doi: 10.1016/j.jpag.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Midilli T.S., Yasar E., Baysal E. Dysmenorrhea characteristics of female Students of health school and affecting factors and their knowledge and use of complementary and alternative medicine methods. Holist. Nurs. Pract. 2015;29:194–204. doi: 10.1097/HNP.0000000000000091. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.