Abstract
Background
Obstructive uropathy due to stone disease is seen every day in urological practice. Percutaneous nephrostomy and double j ureteral stent procedures are used.
Methodology
A randomized controlled trial was conducted in one center from January 2021 to January 2022. A total of 104 patients of age ≥18 years who had unilateral or bilateral obstructive uropathy due to stone disease were divided into two groups. In Group A, 50 patients underwent to double j stent while in Group B, 54 patients who underwent percutaneous nephrostomy insertion tube. Under local anesthesia, the stent was inserted by cystoscopy. While the percutaneous nephrostomy was done under ultrasound guidance by using local anesthetic agent. Complications were noted in immediate postoperative period and on follow up.
Results
Mean age of Group A was 35 ± 12.7 years whereas mean age in Group B was 36.7 ± 12.5 years and 49 out of patients were male. The most common complication in double j group and nephrostomy group was hematuria (16% and 5.5% respectively). Post DJ stent, complications like septicemia, painful trigon irritation, and stent encrustation were seen in 8.0%, 10.0%, 10.0% and 4.0% patients respectively. On the other hand, post-PCN septicemia, tube dislodgment or blockage, and injury to adjacent organs were seen in 3.7%, 5.5% and 1.8% respectively. In our trial, overall success rate for double j stenting was up to 84.0% and for percutaneous nephrostomy (PCN) was 96.29% (p < 0.0001).
Conclusion
We found percutaneous nephrostomy is better and had overall higher success rate with less complications post procedure.
Keywords: Obstructive uropathy, Nephrolithiasis, Double j stent, Nephrostomy
Highlights
-
•
Obstructive uropathy is a common urological condition seen in urology.
-
•
Stone disease is the most common cause of obstructive uropathy.
-
•
Percutaneous nephrostomy and retrograde double j stent are common procedures for reliving the urological obstruction.
-
•
To these days, there is superiority of one procedure on the other.
-
•
In addition, no clear guideline support one procedure instead the other.
1. Introduction
Obstruction of urine flow could increase the pressure within the collecting system, which leads to kidney injury; this case is defined as obstructive uropathy [1].
Obstructive Uropathy is a structural or functional hindrance of normal urine flow sometimes leading to severe complications, even renal dysfunction. The cause of obstruction uropathy can be intra- or extra luminal or intramural. Among the causes, renal calculi are the main etiological factors of obstruction uropathy [2].
Drainage of the urinary tract is necessary when obstruction of the upper urinary tract causes infection, loss of renal function, or uncontrollable pain. Untreated obstruction in patients with infection may induce significant morbidity such as sepsis, pyonephrosis, and death [3].
Percutaneous nephrostomy and antegrade ureteral stenting are frequently performed, minimally invasive, imageguided procedures [4].
The efficacy, morbidities and complications of DJ stenting and PCN have been widely studied and compared in the management of obstructive uropathy. Both these procedures have been reported to present different kind of short- and long-term complications and so has been their effectiveness and usefulness in urine drainage of these procedures differs [2].
There are no clear guidelines regarding the optimal method for urinary decompression in the setting of ureteral obstruction [5].
This study aims at observing the rate of complications of each procedure conducted in this study. Furthermore, the study hopes to add more useful data that contribute to this specific aspect of urology and help make international guidelines regarding the safe method in urinary diversion.
2. Method
A randomized controlled trial was conducted at the Department of Urology, Aleppo University Hospital in Aleppo, Syria and lasted one year starting from January 2021 to January 2022.
This study aims to compare the complications rate between the double j ureteral stent and percutaneous nephrostomy in patients with acute obstructive uropathy due to stones. Inclusion criteria were all patients over 18 years old who had acute unilateral or bilateral obstructive uropathy due to lithiasis and needed urgent urinary diversion.
Exclusion criteria were patients under 18 year's old, pregnant women, non-stone renal hydronephrosis, and severe impairment coagulopathy.
Past medical history and clinical examination were done for all patients in the emergency room. Laboratory tests included complete blood count (CBC), creatinine, urea, and glucose, electrolytes, urinalysis, and coagulopathy studies. Some patients underwent renal ultrasound and KUB image; others underwent non-contrast computed tomography (NCCT) to confirm the diagnosis.
Group A or group B was allotted randomly to each of the recruiters by a biostatistician. After taking their consent, patients are divided into two groups. Group A who would undergo to double j ureteral stent and Group B who would undergo to percutaneous nephrostomy.
Firstly, we used lidocaine 2% as local anesthesia.
In Group A: we injected the lidocaine inside the urethra, then after using aseptic cystoscopy, we inserted a retrograde double j ureteral stent. All stents were 4.7fr or 6fr with open ends.
In Group B: patients underwent percutaneous nephrostomy after using lidocaine. All cases were grade 2 or grade e hydronephrosis. Ultrasound guidance was used in all patients. Nephrostomy tubes’ size was 12fr and 14fr. All patients underwent middle or lower calyx puncture by urologists only.
A single dose of prophylactic non-nephrotoxic antibiotic was given to all patients as pre-intervention procedure. Post-procedure hospitalization days were dependent mainly on the patient's status.
During hospital days, we observed any early complications that may occur.
At discharge, we performed creatinine test for all patients. A controlled follow-up for definitive treatment by ureteroscopy or extracorporeal shock wave lithotripsy [ESWL] was arranged according to the patient's status and hospital facility.
The data were analyzed via SPSS version 23. Statistical significance was accepted at P < 0.05.
3. Results
A total of 104 patients were included in this study. Patients’ characteristics are shown in Table 1.
Table 1.
Patients characteristics.
| DJ (n = 50) | PCN (n = 54) | P value | |
|---|---|---|---|
| Age (years) | 35.6 ± 12.7 | 36.7 ± 12.5 | 0.001 |
| Gender (Male) | 23 (46%) | 26(52%) | 0.826 |
| Hypertension | 13 (26%) | 15 (27.7%) | 0.838 |
| Diabetes Mellitus | 6 (12%) | 18 (33.3%) | 0.010 |
| Ischemic Heart Disease | 6 (12%) | 8 (14.8%) | 0.674 |
| Previous endourological procedures | 21 (42%) | 21 (38.8) | 0.747 |
| Scr before procedure (mg/dl) | 1.59 ± 1.37 | 1.50 ± 1.22 | 0.000 |
| Scr at discharge (mg/dl) | 1.53 ± 1.02 | 1.34 ± 1.06 | 0.000 |
| Scr at definite treatment (mg/dl) | 1.64 ± 1.35 | 1.19 ± 0.57 | 0.001 |
| Positive Urinalysis | 23 (46%) | 29 (53.7%) | 0.432 |
| Post Procedure hospitalization days | 2.67 ± 1.69 | 1.52 ± 1.37 | 0.023 |
| Days from 1st to 2nd operation | 20.17 ± 12.16 | 21.28 ± 8.94 | 0.040 |
Fifty patients (48%) underwent double j stent insertion and fifty-four patients (52%) underwent percutaneous nephrostomy. Fifty-five of the patients were female, whereas forty-nine were male. The mean age in Group A was 35.6 ± 12.7 years and 36.7 ± 12.5 years in Group B (p value = 0.001). Before the procedure, there was a statistical significance in serum creatinine between the two groups (p value < 0.001). After the procedure, serum creatinine at discharge was found significantly higher in the DJ group (ρ value = 0.000). Post-procedure hospitalization days and serum creatinine at definitive treatment were statistically significant between the two groups (p = 0.023, p = 0.001 respectively). Meantime from initial procedures to definitive treatment is 20.17 ± 12.16 days in Group A and 21.28 ± 8.94 days in Group B (p value = 0.040).
There was no statistical significance in the prevalence of ischemic heart disease, hypertension, diabetes mellitus, and previous endourological procedures in patients between the two groups Table 1.
Post-procedure complications are shown in Table 2.
Table 2.
Complications rate in both groups.
| Complications | Group A (n = 50) |
Group B (n = 54) |
||
|---|---|---|---|---|
| No of Patients | % age | No of Patients | % age | |
| Procedure Failure | 03 | 6.0 | 01 | 1.8 |
| Fever & Septicemia | 04 | 8.0 | 02 | 3.7 |
| Bleeding/Hematuria | 08 | 16.0 | 03 | 5.5 |
| Painful Trigone Irrigation | 05 | 10.0 | __ | __ |
| PCN dislodgement or blockage | __ | __ | 03 | 5.5 |
| Ureteral Perforation | 00 | 0.0 | __ | __ |
| Stent Migration | 00 | 0.0 | __ | __ |
| Injury to adjacent organs | __ | 1 | 1.8 | |
| Stent Encrustation or Stone Formation | 02 | 4.0 | __ | __ |
| Total | 22 | 44.0 | 10 | 18.3 |
Septicemia and fever occurred in 04 patients after DJ stent insertion.
They were treated conventionally by giving those I.V. antibiotics and rehydration hospitalization except one patient who needed to remove the DJ stent. Procedure failure occurred in 03 patients. Those patients were undergone to percutaneous nephrostomy later.
Hematuria was seen in 08 patients. However, three of them are managed conventionally by giving I.V fluids. Five patients complained painful trigone irrigation which was settled by α1 blocker and anticholinergic medications. Encrustation was seen in 02 patients who were late to definitive treatment. They were managed by ESWL and later the stent was removed. Overall, 22 patients had complications.
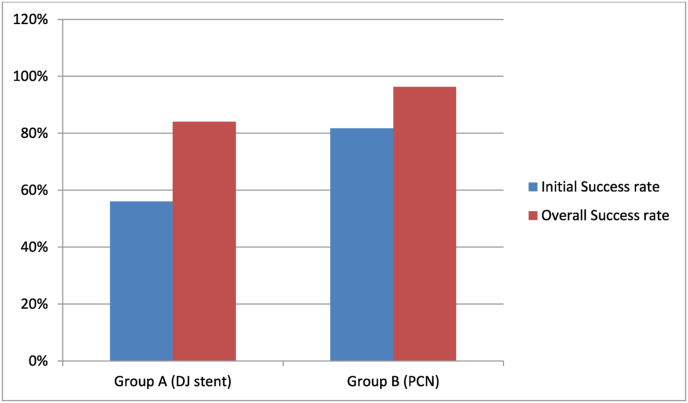
The initial success rate was 56%, but with patients who were treated conservatively, the overall success rate raised to 82% (Fig. 1).
Fig. 1.
Initial and overall success rate in both groups.
In the percutaneous nephrostomy group, procedure failure occurred in one patient. Septicemia occurred in 02 patients who were also treated conservatively according to hospital protocols. Three patients had hematuria which was treated by giving I.V. fluids.
One patient needed blood products transfusion to stop bleeding. PCN dislodgment or blockage occurred in 03 patients which were managed by re-inserting the nephrostomy tube. Only one patient had an injury to the adjacent organs (liver injury by the needle) that was treated by inserting DJ stent and being monitored in the ward. No surgical intervention was needed afterwards.
The initial success rate in the PCN group was 82%. After the management of patients who had septicemia, bleeding, and dislodgement, the overall success rate was 96.29% (Fig. 1).
4. Discussion
Obstructive Uropathy is one of the consequences of urinary tract obstruction the renal functions get deranged and the damage is caused to the urinary tract tissue. If not appropriately treated, this can become a potentially life threatening condition. Immediate decompression of the kidney is necessary to prevent the patient's condition from further deterioration before proceeding for definitive stone management [2].
The various methods of urinary diversions are retrograde double J ureteral stenting, percutaneous nephrostomy and open drainage of kidney. Clear guidelines regarding optimal urinary diversions have not been established. Most authors agreed that decisions should be individualized. Currently, retrograde double-J ureteral stenting and ultrasound guided percutaneous nephrostomy tube insertion are the most widely used techniques for relieving obstruction of the urinary tract. Both are associated with variable technical success, complication rates, and availability and quality of life issues [6].
The decision on the appropriate method of drainage is multifactorial, including factors such as stone parameters, patient's characteristics, patient's and urologist preferences.
In our study, we had 104 patients. Male patients were 47.11% and female patients were 52.88% which shows lower percentage of male patients as compared to Iftikhar Ahmad et al. [8] and Ann Pak Inst Med Sci [2] which found out male patients predominance. The mean age was 36.22 ± 12.56 years which is lower than [2] 46.27 ± 9.36.
In this study, we included patients with unilateral or bilateral obstructive uropathy. Serum creatinine prior to the procedure was 1.59 ± 1.37 mg/dl and 1.50 ± 1.22 mg/dl for Group A and Group B respectively. The p value (p = 0.000) was statistically significant between our two groups and greater than the value found in Shoshany et al. as [7] (p = 0.001).
We studied the immediate and late complications of both procedures.
DJ ureteral stent insertion was successful in 94% (procedure failure in 03 patients) while Khalid Saeed et al. [9] had 98.2%. Procedure failure in the retrograde insertion of the stent was due to benign prostatic hyperplasia or ureteral orifice malposition.
Those patients were considered to PCN for urgent diversion. On the other hand, the successful rate of PCN in our study was 96%, whereas Iftikhar Ahmad et al. [8] had a 92% overall success rate. We had one patient who had a mild grade of hydronephrosis resulted in procedure failure. Patients who had PCN procedure failure were referred to renal replacement therapy.
Post DJ stenting hematuria was observed in different studies ranged from 2 to 21% [8].
In Group A, the most common complication was bleeding and hematuria (16%). This is because we had 09 patients undergone bilateral double j stenting. One patient had to remove it to stop bleeding after we fail to treat it conventionally.
The incidence of post-PCN bleeding and hematuria in Group B was 5.5% while Jalbani MH et al. [10] reported 7.5%.
Fever and septicemia occurred in 04 patients (8%) of the DJ stent group whereas Saeed K et al. [9] and Iftikhar Ahmad et al. (80 found 26.7% and 7% respectively). Those patients are treated by giving injectable antibiotics. Two patients (3.7%) of Group B had fever and septicemia which is almost similar to Firas Al-Hammouri et al. [1] (5%). We also gave injectable antibiotics until recovery.
In our study, painful trigone irrigation occurred in 10% of Group A. However, Shao Y et al. [11] and Memon NA et al. [12] have come across this rate as 10% and 9% respectively. For this complication, we prescribed patients a1 blocker and anticholinergic drugs which improved the patients’ complaints notably.
Post PCN blockage or dislodgment of the nephrostomy tube observed in different studies range from 04 to 37% [8].
PCN dislodgment or blockage happened in 5.5% of Group B. Those patients underwent reinserting the nephrostomy tube.
In our trial, we had 02 patients (4%) who had stent encrustation and stone formation in Group A, while Iftikhar Ahmad et al. [8] pointed out 5% of the patients with stent encrustation and stone formation.
Stent encrustation occurred in patients who had a long time between the initial procedure and definite treatment (about 60 days). They were managed by ESWL successfully.
In Group B of our study, we had an injury to an adjacent organ (liver injury) in one patient (1.8%) while Saeed K et al. [13] found 14.3%. This patient was admitted to the ward for monitoring. He was managed conventionally.
Overall, PCN group patients had fewer complications and a high success rate which means that percutaneous nephrostomy is superior to DJ stent in obstructive uropathy in the field of nephrolithiasis (p value = 0.034).
Nevertheless, more data collection is needed for further studies over the world to compare the two methods and to set a guideline regarding obstructive uropathy.
5. Conclusion
We conclude that percutaneous nephrostomy is the optimal method in obstructive uropathy due to nephrolithiasis. It has less complication rate in comparison to retrograde double j ureteral stenting. More trials are needed to create clear guidelines that expect definitive approach for stone treatment and procedure availability.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Sources of funding
The article has no funding source.
Author contributions
Maher Al-Hajjaj: Project development, data collection and management, manuscript writing.
Aziz Joseph Sabbagh, Ibrahim Al-Hadid, Mohammad Nour Kazan, Hasan AL Muhammad AL Husein, Ali Alali Aljool: Data collection, manuscript writing.
Mohamed Taher Anan: Writing Statistics.
Mohamad Tallaa: manuscript writing and editing.
Registration of research studies
Name of Registry: Open Science Framwork
ID: osf.io/t6uzv.
Hyperlink: https://archive.org/details/osf-registrations-t6uzv-v1.
Guarantor
Maher Al-Hajjaj.
Consent
Written informed consent was obtained from the patients for publication of this research. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Data availability
Data are available upon request which can be directed to the corresponding author.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
We declare there is no conflict of interest.
Acknowledgment
We would like to thank Mohamad Taher Anan and Thurayya Zaitouni for their great efforts.
References
- 1.Al-Hammouri F., Abo-Qamar A., Al-Majali A. Obstructive uropathy treatment complication rate after percutaneous nephrostomy versus double J catheter insertion. JRMS. 2018;25(2):46–53. [Google Scholar]
- 2.Ali L., Khan S., Khan F.H., Orakzai N. Comparison of percutaneous nephrostomy and double j stent in early normalization of renal function tests in patients with obstructive uropathy due to urolithiasis. Ann. PIMS-Shaheed Zulfiqar Ali Bhutto Med. Univ. 2020;16(1):10–14. [Google Scholar]
- 3.Weltings S., Schout B.M., Roshani H., Kamphuis G.M., Pelger R.C. Lessons from literature: nephrostomy versus double J ureteral catheterization in patients with obstructive urolithiasis—which method is superior? J. Endourol. 2019;33(10):777–786. doi: 10.1089/end.2019.0309. [DOI] [PubMed] [Google Scholar]
- 4.Hausegger K.A., Portugaller H.R. Percutaneous nephrostomy and antegrade ureteral stenting: technique—indications—complications. Eur. Radiol. 2006;16(9):2016–2030. doi: 10.1007/s00330-005-0136-7. [DOI] [PubMed] [Google Scholar]
- 5.Tibana T.K., Grubert R.M., Santos R.F.T., Fornazari V.A.V., Domingos A.A., Reis W.T., et al. Percutaneous nephrostomy versus antegrade double-J stent placement in the treatment of malignant obstructive uropathy: a cost-effectiveness analysis from the perspective of the Brazilian public health care system. Radiol. Bras. 2019;52(5):305–311. doi: 10.1590/0100-3984.2018.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rammohan T., Panduranga R.K., Prasad D., Srinivas S., Santhosh B., Sudharshan G., et al. A comparative study of percutaneous nephrostomy versus DJ stenting in infective hydronephrosis in calculous disease. J. Evol. Med. Dent. Sci. 2015;4(18):3143–3154. [Google Scholar]
- 7.Shoshany O., Erlich T., Golan S., Kleinmann N., Baniel J., Rosenzweig B., et al. Ureteric stent versus percutaneous nephrostomy for acute ureteral obstruction-clinical outcome and quality of life: a bi-center prospective study. BMC Urol. 2019;19(1):1–7. doi: 10.1186/s12894-019-0510-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmad I., Pansota M.S., Tariq M., Saleem M.S., Tabassum S.A., Hussain A. Comparison between double J (DJ) ureteral stenting and percutaneous nephrostomy (PCN) in obstructive uropathy. Pakistan J. Med. Sci. 2013;29(3):725. doi: 10.12669/pjms.293.3563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saeed K., Hussain S.A., Kanjoo S.R., Ahmad B., Hussain M. Double-J stenting versus percutaneous nephrostomy; postoperative complications in management of ureteral obstruction. Ann. Punjab Med. Coll. (APMC) 2020;14(4):336–339. [Google Scholar]
- 10.Jalbani M.H., Deenari R.A., Dholia K.R., Oad A.K., Arbani I.A. Role of percutaneous nephrostomy (PCN) in malignant ureteral obstruction. JPMA J. Pakistan Med. Assoc. 2010;60(4):280. [PubMed] [Google Scholar]
- 11.Shao Y., Zhuo J., Sun X.W., Wen W., Liu H.T., Xia S.J. Nonstented versus routine stented ureteroscopic holmium laser lithotripsy: a prospective randomized trial. Urol. Res. 2008;36:259–263. doi: 10.1007/s00240-008-0153-5. [DOI] [PubMed] [Google Scholar]
- 12.Memon N.A., Talpur A.A., Memon J.M. Indications and complications of indwelling ureteral stenting at NMCH. Nawabshah. Pak J of Surg. 2007;23(3):187–191. [Google Scholar]
- 13.De Lorenzis E., Lievore E., Turetti M., Gallioli A., Galassi B., Boeri L., et al. Ureteral stent and percutaneous nephrostomy in managing malignant ureteric obstruction of gastrointestinal origin: a 10 Years' experience. Gastrointestinal Disorders. 2020;2(4):456–468. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon request which can be directed to the corresponding author.