During a routine check-up, retro-pneumoperitoneum was discovered on the lowest slices of a computed tomography (CT) chest scan in a 77-year-old female patient who was known to have Sjögren’s syndrome with lymphocytic interstitial pneumonia (fig. 1a). She had initially been treated with prednisolone that improved sicca signs and cough. The patient, who had no prior history of digestive problems, complained of abdominal discomfort and distension. She was afebrile, haemodynamically stable and bowel movement was unchanged. Abdominal examination eliminated signs of peritonism.
Figure 1.
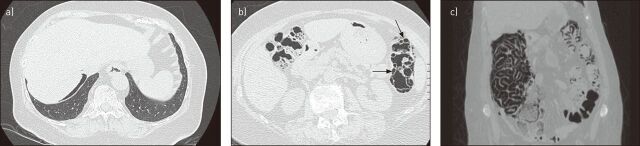
a) Computed tomography (CT) chest scan showing retro-pneumoperitoneum. b) Abdominal CT scan showing thickening of the wall of the descending colon, which contained multiple air-filled cysts (black arrows). c) Coronal CT reconstruction showing free air in the wall of the caecum, colon and adjacent mesos.
The abdominal CT scan, which showed thickening of the wall of the descending colon, contained multiple air-filled cysts (black arrows) consistent with pneumatosis cystoides intestinalis (PCI) (fig. 1b). There was free air in the wall of the caecum, colon and adjacent mesos (fig. 1c).
PCI is a rare condition characterised by multilocular pneumatocysts within the wall of the lower digestive tract. To date, association with a systemic connective tissue disease (CTD) such as Sjögren’s syndrome has only been reported twice [1]. Previous studies have mostly been of scleroderma-related conditions [2]. Corticosteroids are often used in CTD and appear to increase the risk of PCI [3]. Conservative treatment is often sufficient in stable patients with limited symptoms. Antibiotic agents (e.g. metronidazole) and the tapering of immunosuppressive drugs seem to improve clinical and radiological findings. Intestinal rest, parenteral nutrition, electrolyte supplementation and inhaled oxygen are also recommended [3]. Unnecessary surgery can be avoided through better knowledge of PCI and its complications. Surgical intervention should only be considered in severe or life-threatening cases.
Footnotes
Provenance: Submitted article, peer reviewed.
Conflict of interest: None declared.
References
- 1.Vandergheynst F, Van Gansbeke D, Steinfeld S. Primary Sjögren’s syndrome associated with pneumatosis cystoides coli. Eur J Intern Med 2006; 17: 57–58. [DOI] [PubMed] [Google Scholar]
- 2.Balbir-Gurman A, Brook OR, Chermesh I, et al. Pneumatosis cystoides intestinalis in scleroderma-related conditions. Intern Med J 2012; 42: 323–329. [DOI] [PubMed] [Google Scholar]
- 3.Zhang H, Jun SL, Brennan TV. Pneumatosis intestinalis: not always a surgical indication. Case Rep Surg 2012; 2012: 719713. [DOI] [PMC free article] [PubMed] [Google Scholar]