In this Update we will discuss aspects of the definitions, epidemiology, diagnostics, asthma-associated comorbidities, assessment and treatment of asthma including a specific focus on severe asthma in school children. The Update will mainly cover data published during the last 3 yrs.
In 2009, an expert panel was tasked to propose a World Health Organization definition of asthma severity and control. The result of this Task Force was a uniform definition of asthma severity, control and exacerbation [1]. As we will discuss later in an overview of asthma outcomes [2], symptom evaluation is the key to the diagnosis and outcome measures in clinical studies.
Airway inflammation is one of the pathophysiological characteristics of asthma, which is mediated through infiltration of inflammatory cells, including mast cells, and eosinophilic and neutrophilic granulocytes in the airway wall. This cell infiltration subsequently leads to bronchial hyperresponsiveness (BHR) and, in the case of chronic inflammation, persistent changes of the airways, i.e. airway remodelling [3, 4].
Immunoglobulin (Ig)E-mediated allergy leading to allergic inflammation is common among children with persistent asthma. There are ongoing studies worldwide (the MeDALL initiative) aiming to identify allergic phenotypes [5] and understand the complexity of the IgE related phenotypes in children and adults [6].
The purpose of paediatric asthma treatment is for the child to control symptoms, to be able to lead a normal active life, to have normal lung function and to prevent asthma exacerbations [7, 8]. The care of asthmatic children does not only include the prescription of asthma medication. The families need to be convinced and educated to actually make the parents give the medication as prescribed and in a proper manner [9]. Furthermore, healthcare providers must teach the families how to avoid or handle triggering factors, including exercise; recognise signs that asthma is worsening; and seek medical advice when needed [10].
NOTES ON EPIDEMIOLOGY
Wide variations exist in the symptom prevalence of children with asthma. While severe symptoms among children in less affluent countries are more common, there are more children with any symptoms of asthma in wealthy countries [11]. In a systematic analysis of the global burden of disease in people aged 10–24 yrs [12], where the disease risk was assessed by calculating years lost because of disability, respiratory disorders were the sixth main cause of disability worldwide. Most of the years lost because of disability were caused by asthma, which was the fourth most common cause of disability-adjusted life years for children aged 10–14 yrs. Another approach to estimating the burden of asthma was reported from Ontario, Canada, in a study of the lifetime risk of physician-diagnosed asthma [13]. One in three individuals had physician-diagnosed asthma. Even more interesting is that one in five was diagnosed before 20 yrs of age. This demonstrates the life-long pattern of asthma compared with other chronic diseases such as diabetes and coronary heart disease [13]. In a 5-yr follow-up study of Irish children, the prevalence of asthma remained stable in 6–9-yr-old children at 21.7% in 2002 and 23.5% in 2007 [14]. This illustrates and confirms the findings of the International Study of Asthma and Allergies in Childhood (ISAAC) study of the varying prevalence of asthma in Europe.
DEFINITIONS AND DIAGNOSIS OF SEVERE ASTHMA
Problematic severe asthma
The majority of children with asthma have mild or moderate disease and can obtain adequate control of symptoms through avoidance of triggering factors and/or with the help of medications, such as inhaled short-acting β2-receptor agonists (SABA), inhaled corticosteroids (ICS) and, when needed, the addition of long-acting β2-receptor agonists (LABA) and leukotriene receptor antagonists (LTRA) [15, 16]. Asthma control is defined as “to which extent the manifestations of asthma have been reduced or removed by treatment” [17], a concept that not only includes assessment of daytime and nocturnal symptoms and need for reliever medication, but also an estimation of future risk of severe exacerbations. However, ∼5% of all asthmatic children have chronic symptoms and/or recurrent exacerbations despite maximum treatment with conventional medications [18]. These children are referred to as severe asthmatics, and due to the lack of specific biomarkers of this disease, severe asthma is currently being defined on the basis of the intensity of treatment required to improve asthma control, and the level of control achieved [7, 17, 19]. Thus, the definition of severe asthma combines evaluation of medication, chronic symptoms and exacerbations. These criteria are developed from the Global Initiative for Asthma (GINA) guidelines and other studies or reviews on severe childhood asthma [20–22]. Children with such severe and therapy resistant symptoms are heterogeneous with respect to triggering factors, pulmonary function, inflammatory pattern and clinical symptoms [22–25]. These children have a reduced quality of life [26] and represent a continuous clinical challenge to the paediatrician [24, 27].
A Global Allergy and Asthma European Network (GA2LEN) Task Force, the Problematic Severe Asthma Initiative, has proposed the term problematic severe asthma to define all children who suffer from chronic symptoms and/or severe exacerbations despite prescription of high doses of ICS with additional LABA and/or LTRA [21, 22]. This concept has been incorporated in the recent WHO definition of severe asthma [1]. The concept is a reflection of how children with problematic severe asthma are presented to the paediatric allergist, i.e. having troublesome symptoms despite maximum conventional medications, step 4 and 5 according to GINA.
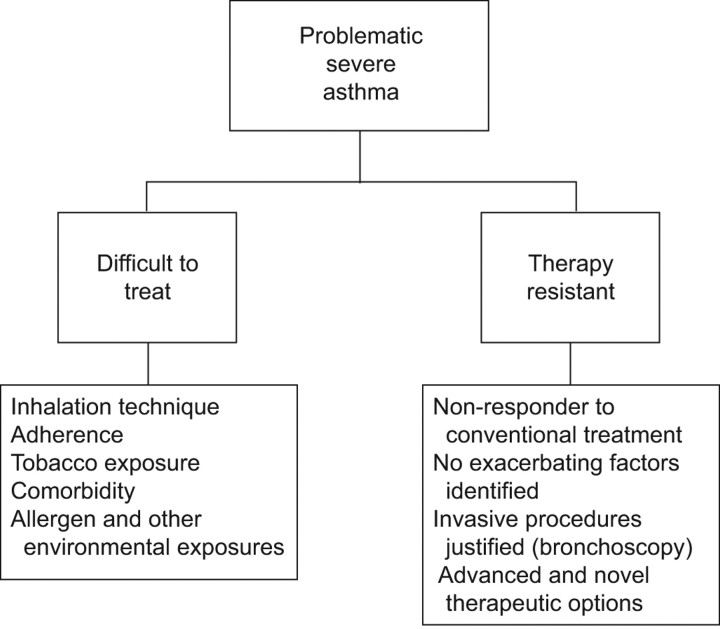
The advantage of the newly introduced term problematic severe asthma is that it encompasses two groups of children: 1) children who, after a thorough work-up, can be classified as difficult to treat because of identified exacerbating factors; and 2) children who, following a thorough work-up, do not have any identifiable aggravating factors but are still severely resistant to therapy (fig. 1).
Figure 1.
Clinical classification of children presenting with problematic severe asthma.
Clinical presentation of problematic severe asthma in school-age children
We diagnose severe therapy-resistant asthma when differential diagnosis is excluded (table 1), and we cannot identify factors that make the child “difficult-to-treat”. Severe therapy-resistant asthma may take a number of different forms that are not mutually exclusive.
Table 1. Possible differential diagnosis in a child presenting with severe asthma.
| Tracheomalacia |
| Congenital disorders |
| Primary ciliary dyskinesia |
| Oesophageal fistula |
| Foreign body |
| Bronchiolitis |
| Immunodeficiency |
| Cardiac disease |
Exacerbation phenotype
Exacerbation phenotype refers to children with problematic severe asthma who have received more than one burst of oral corticosteroids in the preceding 12 months, without experiencing daytime or night-time symptoms between exacerbations.
Chronic symptoms phenotype
Chronic symptoms phenotype refers to children with problematic severe asthma that have experienced daytime and/or night-time symptoms more than twice per week in the preceding 3 months.
We diagnose difficult-to-treat-asthma when poor control is due to one or more of the following: associated diagnoses (comorbidities), poor adherence to treatment regimens, or adverse psychological and environmental factors.
Difficult-to-treat asthma versus therapy resistant asthma
In a study of Swedish school children with problematic severe asthma, 39% of the children with problematic severe asthma were exposed to exacerbating factors that could be treated or at least partially eliminated. This finding provides support for the clinical utility of the definition of problematic severe asthma [23]. Moreover, these exacerbating factors were not disclosed in connection with routine care by experienced paediatric allergists, emphasising the usefulness of an extensive and standardised clinical protocol. Home visits [28] and assessment of steroid response with, for example, triamcinolone injection [20, 29] could have further improved the classification of children with problematic severe asthma.
The Swedish results and the results from other studies indicate that children with problematic severe asthma who have a low socioeconomic background and a high exhaled nitric oxide fraction (FeNO) have an increased probability of having asthma that is difficult to treat because of identifiable aggravating factors [23, 30]. This finding suggests a shortcoming of the profession to educate these families on how to avoid or handle triggering factors. Furthermore, although impaired asthma control and risk of exacerbations are related, the respective predictors are different [31].
ASTHMA COMORBIDITIES AND/OR ASSOCIATED DIAGNOSIS
Other conditions may co-exist with asthma, and continuing respiratory symptoms may be wrongly attributed to asthma alone. These children may be difficult to treat. The most common comorbidities are chronic rhinosinusitis, gastro-oesophageal reflux and obesity.
Rhinitis and rhinosinusitis
It has long been recognised that diseases of upper and lower airways may co-exist. The co-morbidity between childhood asthma and rhinoconjunctivitis is well established. The relationship between the nose and the lung, however, is complex and it has been reviewed in several studies [32, 33]. 76% of patients with asthma have rhinitis and up to 15% of patients with allergic rhinitis have asthma [34]. Chawes et al. [35] further report that children with allergic and non-allergic rhinitis have a similar risk of asthma. It is still unclear whether sinusitis worsens asthma, or whether both are manifestations of the same underlying disease process. However, the observation that patients with problematic severe asthma report clinical symptoms of rhinoconjunctivitis more often than those with controlled asthma was found in a Swedish study [23]. The fact that untreated rhinitis contributes to reduced symptom control in asthmatic children has become increasingly evident [34]. In children, chronic rhinosinusitis is possibly also an underestimated disease [36].
Gastro-oesophageal reflux
The relationship between the oesophagus and the lung is also multifactorial [37]. Lung disease can cause gastro-oesophageal reflux, reflux can cause lung disease, or reflux may be of no clinical significance. Depending on the criteria used for diagnosis, 20–80% of children with chronic respiratory disease have gastro-oesophageal reflux [37]. To date, a precise mechanistic link between gastro-oesophageal reflux and decline in asthma control has not been established [38]. The results of trials of anti-reflux therapy are often disappointing [39], especially in older children, but an empirical trial is reasonable in younger children if the history is suggestive.
Vocal cord dysfunction
Some breathing problems can be confused with asthma. In particular, vocal cord dysfunction may co-exist with asthma and may be a differential diagnosis, leading to inappropriate asthma treatment. Low et al. [40] report a noninvasive method for quantification of laryngeal movement by using computed tomography (CT) of the larynx. A 320-slice CT was used to monitor laryngeal behaviour. A specific pattern of laryngeal dysfunction was demonstrated, which was observed in patients with difficult-to-treat asthma. The importance in the awareness of “considering the total airway”, particularly in severe asthma, is further stressed by Ayres et al. [41].
Obesity
The relationship between obesity and asthma is complex. There are a number of confounding factors, including gastro-oesophageal reflux (as mentioned previously), and the effects of obstructive sleep apnoea could be confused with asthma. The debate on obesity and asthma is about to what degree obesity has metabolic effects that contributes to airway inflammation. The latter has been shown in the Childhood Asthma Management Program (CAMP) study [42]. In addition, an association was found in the Severe Asthma Research Program study, although it was age dependent. Children with early onset asthma became obese, whereas there was no significant relationship between increasing body mass index and asthma duration among obese children with late onset asthma [43]. Furthermore, Cibella et al. [44] reported that being overweight was not a risk factor for asthma and allergic sensitisation, but was a risk factor for airway inflammation measured by FeNO. Based on a study of 32,321 children aged 5–17 yrs, Quinto et al. [45] conclude that childhood obesity is associated with worse asthma control and exacerbations. Obesity may cause steroid resistance, in part, by reducing steroid-induced mitogen activated protein kinase phosphatase-1 [46]. Finally, Cottrell et al. [47] found an association between an abnormal lipid and glucose metabolism and asthma regardless of prevalence of obesity.
Vitamin D deficiency and asthma
The impact of low serum levels of vitamin D in relation to lung disease and to asthma, in particular, is a subject of discussion. The study by Gupta et al. [48] showed that increased airway remodelling, as measured by smooth muscle in biopsies, correlated to levels of vitamin D in children with severe asthma. This relationship did not exist for children with moderate asthma and in healthy controls [48]. Other evidence of the association between vitamin D and asthma severity was reported from the CAMP study [49]. Risk of exacerbation was increased in children with low levels of vitamin D. In addition, Chinellato et al. [50] reported an association between exercise-induced asthma and vitamin D levels.
UPDATE ON MECHANISMS OF ASTHMA IN CHILDREN
Inflammation
The level of symptoms and markers of inflammation do not always correlate; some children might have persistent symptoms without any inflammatory cells on histology, whereas other children might have no symptoms between exacerbations but still have increased markers of airway inflammation [51].
The aetiology of airway inflammation in asthmatic children varies depending on age. Whereas viral infections, including rhinovirus and respiratory syncytial virus, are linked to obstructive bronchitis in infancy and early childhood, and considered by some to be a combined risk factor with allergen sensitisation [52], sensitisation and exposure to allergens is the major cause of allergic airway inflammation in older children. Interestingly, recent evidence also points to a synergistic effect between viral infections and aeroallergen exposure, and subsequent sensitisation in genetically predisposed children [53, 54]. Furthermore, viral infections have been shown to be the most important cause of asthma exacerbations in all age groups [55, 56]. Rhinovirus and respiratory syncytial virus are shown to damage the respiratory epithelium, making it less resistant to inhaled allergens and subsequently leading to enhanced T-helper (Th)2 responses in predisposed children and the development of allergic inflammation [57].
Starting with the late phase allergic reaction, airway inflammation includes recruitment and migration of inflammatory cells, eosinophils, in particular, and neutrophils to the site of allergen exposure within 4–6 h. These cells are recruited and developed from a pluritpotent stem cell in the bone marrow via the circulation to the airways. Interleukin (IL)-3, IL-5 and granulocyte-macrophage colony-stimulating factor (GM-CSF) secreted by Th2 cells and mast cells are the most important interleukins for eosinophilic development and recruitment, although only IL-5 is specifically targeted towards the eosinophils. Once matured and recruited to the circulation, eosinophils adhere to the endothelial wall, connecting with adhesion molecules expressed on the eosinophil (very late antigen-4) and endothelial cells (vascular cell adhesion molecule-1) [58–60]. After transmigration through the endothelial wall, the eosinophils are guided to the site of inflammation by chemokines and release several stored toxic mediators, including free acid radicals, eosinophilic cationic protein, eosinophilic peroxidase and eosinophilic protein X [61].
Neutrophils are attracted by GM-CSF and interferon (IFN)-γ. Neutrophilic pathogenic excretions include elastase, which causes hypersecretion and hyperreactivity. Matrix metalloproteinase-9 breaks down collagen causing hypersecretion and the release of free oxygen radicals, which also induce BHR [62]. The relative contribution of each of these cell types to asthma severity is not clear. In a recent published study on children with therapy-resistant asthma, there was a huge variability in eosinophil counts in bronchoalveolar lavage (BAL) and biopsy [4]. This important study in children with therapy-resistant asthma did not demonstrate neutrophilic airway inflammation on BAL and biopsy [4].
Airway remodelling and asthma
Airway remodelling refers to structural changes in the bronchial wall causing reduced lung function [63] in asthmatic patients. These structural changes are diagnosed by histology and are characterised by epithelial damage, thickening of reticular basement membrane and, subepithelial fibrosis, as well as mucus gland and airway smooth muscle hypertrophy and hyperplasia. Remodelling is found in the majority of school age children with problematic severe asthma [4, 20] and the progressive loss of lung function found in these patients is probably caused by remodelling [64].
Allergy and asthma
Every allergen has several epitopes, and similar epitopes might occur in allergens from different sources; this is the biological explanation behind cross-sensitisation [65, 66]. Some allergens are unique markers of a specific allergen source whereas allergens with similar structure and function are found in different species, e.g. lipocalins are a group of proteins arising from cat, dog, horse and mice, and cross-reactivity within these groups of proteins is common [67, 68].
Basophils
Basophils share important features with mast cells; however, basophil development is stimulated by IL-3, whereas mast cells are stimulated by IL-9. Basophils are a main source of IL-4 and IL-13, which are important for the production of IgE and the development of Th2 lymphocytes. Furthermore, basophils are found in the circulation, which has led them to be considered accessible surrogate makers of mast cells [69]. However, recent evidence indicates that basophils are not only markers of mast cell function, but could also function as initiators of allergic inflammation and contribute to the development of chronic allergic inflammation [70].
ASSESSMENT AND BIOMARKERS OF ASTHMA
A biomarker reveals information about the investigated disease, and can be used in one or more of the following settings to: assess the risk of morbidity; identify disease or disease phenotypes; and monitor disease activity as well as treatment effects [71]. The ideal biomarker is attained noninvasively, is reproducible, easily measured and provides information about essential pathophysiological processes with high performance characteristics including sensitivity, specificity, and negative and positive predictive values. Using biomarkers in childhood airway disease is particularly challenging. Imaging and spirometry, although providing relevant information, also have significant limitations. Biological events that occur episodically (bronchoconstriction) might not be captured and in early or mild disease these evaluations might be normal despite the patient having symptoms [71]. A US working group proposed the most relevant biomarkers for asthma outcome, namely multi-allergen screening to define atopy, blood counts to measure total eosinophils, FeNO, sputum eosinophils, urinary leukotrienes and total and allergen specific IgE. They also concluded that system-wide studies (proteomics and genomics) are emerging but are not yet ready for clinical use [72].
Pulmonary function and BHR
Reversible obstruction of the airways and BHR are characteristic features of asthma [73]. In relation to asthma severity, some studies found no difference in forced expiratory volume in 1 s (FEV1) on average [18, 20], but there were large individual variations [74] and the results from these studies implicate that the usefulness of FEV1 as an indicator of severity in childhood asthma remains questionable. BHR to methacholine has been shown to correlate with asthma in specific studies on children with problematic severe asthma [18, 75]. BHR to methacholine is reduced by anti-inflammatory treatment and has been shown to correlate with markers of airway inflammation, including nitric oxide (NO) in exhaled air in severe asthmatics [76]. However, a negative test has a greater value to rule out asthma, at least in the treatment naïve patient [73]. The clinical relevance of direct and indirect tests is still being debated [77, 78]. The direct challenge with methacholine is a sensitive test for BHR although less specific than the indirect tests such as mannitol and exercise. The latter could be considered more “real life” appropriate.
Biomarkers in BAL and sputum
Invasive methods such as biopsy and analysis of BAL are possible in specialised centres, but in most circumstances they are not considered feasible in children. Induced sputum, a semi-invasive method, has been found to be safe in children but does require specially trained staff [79]. Cross-sectional studies have shown different cell patterns in sputum from non-allergic and allergic asthmatic children [80]. Furthermore children with asthma and food allergies were demonstrated to have more eosinophils in sputum than children with asthma but without food allergies [81]. In adults, treatment guided by the presence or absence of sputum eosinophils has been shown to reduce asthma exacerbations. There is one study in severe asthmatic children in which this has not been proven effective [82]. In a recent meta-analysis the utility of sputum eosinophils was confirmed in adults but studies in children are needed [83].
Exhaled NO
NO is produced by NO synthase in airway epithelial cells. The NO that is produced easily diffuses into the airway lumen. FeNO has been established as a noninvasive biomarker in asthma. The possibility to use it as a predictor of risk has been suggested [84].
In a cross-sectional study, Zeiger and co-workers [85, 86] found that FeNO was a complement to symptom evaluation in that higher FeNO was associated with an increased use of SABA and the need for oral corticosteroids. Nevertheless, the clinical situation in which FeNO provides the most useful information is currently under debate [73] and the relationship between FeNO and asthma severity is unclear [76]. A meta-analysis [83] included three paediatric studies of the utility of FeNO in guiding treatment in children with asthma [87–89] and it was concluded that asthma treatment guided by FeNO did not improve asthma outcomes. One of the studies in which treatment was adjusted according to FeNO showed that the children in the NO-guided group increased their daily dose of ICS [89]. In the aforementioned study comparing asthmatic children with and without food allergies, FeNO was significantly higher in the children with food allergies [81] indicating increased bronchial inflammation caused by the food allergy. One could speculate that airborne food allergen exposure might be an underestimated problem in children contributing to insufficient anti-inflammatory therapy. Likewise, children who spend a lot of time indoors and are exposed to allergen like dust mite and/or dander have been shown to have increased levels of FeNO, especially if not sensitised to the allergens; thus, sedentary behaviour might increase airway inflammation as measured by FeNO. The correlation between FeNO and the evaluation of symptoms according to the Asthma Control Test can be weak or absent [26, 90]. Finally, FeNO fluctuation measurements in combination with methods that quantify cross-correlations with symptoms can be used as indicators of risk of exacerbations as opposed to the use of single measurements of FeNO [91].
Biomarkers in exhaled breath condensate
Analysis of exhaled breath condensate (EBC) is another noninvasive method that has been proposed to reflect airway inflammation. Different approaches and methods of analysis have been used during the last 3 yrs. In a review by Aujila et al. [92], EBC is mentioned as a possibility but the conclusion is that this method requires further study before it can be applied in any clinical setting. A recent study by Caballero Balanza et al. [93] found increased concentrations of leukotriene B4 and 8-isoprostane in children aged 6–14 yrs with asthma compared to healthy controls. Furthermore, children with persistent asthma had higher concentrations than children with episodic asthma. Leukotriene B4, prostaglandin E2 and 8-isoprostane in breath condensate from the nose and the mouth were analysed in an attempt to study the relationship between persistent allergic rhinitis and asthma; possible correlations were reported [94]. In two other paediatric studies, eoxin and eotaxin were measured in EBC along with 8-isoprostane, all three were significantly increased in children with problematic severe asthma [95, 96]. Finally, a new and advanced approach to utilising EBC was reported by Bloemen et al. [97]. By using a proteomics approach, the authors conclude that EBC contains proteins of interest for asthma diagnosis and follow-up, which is also supported in studies by Dompeling and Jöbsis [98] and Sinha et al. [99].
Biomarkers in urine
Urine is the most accessible noninvasive biofluid sample that can be obtained, but its utility is still questionable in diagnosing and monitoring asthma and airway inflammation. There are, however, new approaches that seem promising. For example, metabolomic profiling of asthma by magnetic resonance spectrometry of urine. Saude et al. [100] applied this technique to discriminate between acute and stable asthma in children in relation to healthy controls with some promising results. In a similar group of children with asthma, liquid chromatography coupled with mass spectrometry was used for analysis of urine samples with similar results [101]. The measurement of urinary leukotriene excretion has been investigated in order to find a marker for response to leukotriene antagonists and some promise of the utility has been found in the ratio of urinary leukotriene E4/FeNO [102]. In children with exercise-induced asthma, the change of urinary leukotriene E4 was significantly higher after an exercise test than in healthy children and tended to be higher than in mild asthmatics, thus, leukotriene E4 might have some association in controlling exercise-induced asthma [103]. At present, analysis of leukotriene E4 seems to be the most useful measurement relevant to asthma. Eosinophil activity markers such as EPX have not been shown to be useful in monitoring asthma; however, bromotyrosine, a marker of eosinophil-catalysed protein oxidation in urine, has been shown to be associated to asthma control and risk of asthma exacerbation in children [104].
Chitinases
A group of proteins recently discovered to be potential biomarkers of asthma are the chitinases. Chitin is a tough structural polysaccharide, the second most abundant biopolymer in nature after cellulose and is used by a variety of organisms including insects, crustaceans, parasites, fungi and bacteria to protect against harsh environmental conditions [105]. Although chitin is not present in the human body, we express enzymes capable of its degradation. Two members of this family, the enzymatically active chitotriosidase and the enzymatically inactive chitinase-like protein YKL-40, are increased in the serum of asthmatic patients [106, 107] and levels of YKL-40 have also been shown to correlate with markers of asthma severity [107]. It has been suggested that the chitinases may be involved in the development of fibrosis and remodelling of the airway [108]. YKL-40 has also recently been shown to increase the proliferation and migration of human bronchial smooth muscle cells [109]. Another noteworthy finding regarding the chitinases is the close correlation between YKL-40 and blood neutrophils. Previous studies have indicated that alveolar macrophages are a major source of YKL-40 in the airways [110], although it is not known whether YKL-40 can be stored in the specific granules of neutrophils and released upon activation of these cells. A recent study of sputum YKL-40 levels in adults with asthma also demonstrated a strong correlation with sputum neutrophil count [111].
Imaging
The relationship between CT findings in children with asthma and markers of remodelling has been investigated. In a report on findings when investigating wet cough by high-resolution CT (HRCT) and bronchoscopy it was concluded that HRCT detected airway wall thickening and the finding correlated with duration of clinical symptoms and neutrophilic inflammation as evaluated by BAL [112]. In adult studies of severe asthma, CT scans are suggested to demonstrate possible bronchial wall changes [113, 114]. Little is known of the possible role of magnetic resonance imaging for evaluation of airway remodelling and/or severity of asthma, although a combination of HRCT and magnetic resonance imaging could help in identifying regional distributions of asthma in the lungs [115, 116]. This could help in investigating regional effects of bronchial/small airway obstruction in children with asthma.
Diagnosing allergy
Sensitisation is usually determined by using allergen extracts to identify the disease eliciting allergen source by in vivo skin-prick testing. An update and practical guide to skin-prick testing using aeroallergens was recently published [117]. In vitro testing, i.e. measurement of specific IgE in serum, is the alternative way of diagnosing allergic sensitisation. However, some disadvantages are associated with these extract-based methods. These methods only give information about the possible sensitising allergen source, but no information about sensitisation towards specific allergens is provided. Thus, it is not possible to differentiate between the primary source of sensitisation and cross-reactivity between allergens from different allergen sources [65]. Moreover, it is not possible to determine whether the patient is sensitised to an allergen causing severe reactions or allergens causing mild reactions. In children with severe asthma the allergy diagnostic characterisation can be complex and often requires both in vivo and in vitro testing [118].
IgE component resolved diagnostics
Today, the only commercially available component-based microarray platform for allergy is the immunosolid-phase allergen chip (ISAC; Thermo Fisher Scientific, Uppsala, Sweden). Although the ISAC chip lacks some minor allergens, the most common species-specific and cross-reactive allergens are represented. Some allergens are specific markers of an allergen source [119], and by identifying these allergens it is possible to determine which are sensitising allergen sources and which are cross-reactive allergen sources [120]. Furthermore, it is possible to predict whether the patient is at risk for a severe or mild reaction, based upon which allergen the patient is sensitised to. Children allergic to peanuts and sensitised to the allergens Ara h 1, Ara h 2 and Ara h 3 are at risk for significantly more severe symptoms upon peanut exposure compared to children sensitised to Ara h 8 [121], which is a homologue to the major Birch allergen, Bet v 1. Assessment of allergic sensitisation by the established extract-based methods has diagnostic limitations with respect to concordance [11], cross-reactivity and prediction of severe allergic reactions. There can be an added value of performing this analysis in children with persistent asthma, as shown by Nordlund et al. [122] who report that children with severe asthma have higher levels of the animal-derived components lipocalin, secretoglobin and kallikrein compared to well-controlled children with asthma.
Basophil allergen threshold sensitivity
Assessment of allergen specific IgE antibodies does not necessarily predict the effector cell response and the subsequent clinical symptoms upon allergenic stimulation. For this purpose allergen provocation tests are needed but as they are potentially harmful, especially in severe asthmatic children, few studies have been performed and published on in vivo allergen challenge tests. Basophil allergen threshold sensitivity (CD-sens) is an attractive in vitro alternative to the clinical allergen provocation tests [123] and correlates well with in vivo allergen provocation [124]. CD-sens is based on the detection of CD63 on basophils following in vitro allergen titration. CD-sens is calculated from the allergen concentration causing 50% of maximum basophil activation and reflects the sensitivity of basophils to the particular allergen. This has been shown as a difference between cat allergic children with severe or mild asthma in spite of comparable levels of cat-specific IgE [125]. It may be speculated that the higher allergen sensitivity in children with problematic severe asthma could be due to skewing of a basophil phenotype, since basophils are a heterogeneous cell population with varying degranulation properties depending on the genetic background and surrounding cytokine environment at the stage of basophil precursor development [126].
RECENT ADVANCES IN THE TREATMENT OF ASTHMA IN CHILDREN
Detailed recent reviews of the treatment of pre-school wheeze and severe asthma [27, 127] have recently been published. In this section we update these publications and also discuss studies relevant to more mild asthma. A stepwise therapeutic approach is usually applied to adjust the medications to the symptoms and several guidelines have been published to support the physician in these treatment decisions [15, 128–130].
Treatment of pre-school wheeze
The European Respiratory Society Task Force [131] proposed that pre-school children with episodic viral wheeze should be treated with intermittent therapy. A more recent paper [132] randomised 278 children with a positive asthma predictive index aged 12–15 months to either 1 mg nebulised budesonide for 7 days with any clinically diagnosed viral upper respiratory tract infection (nequals;139) or 0.5 mg nebulised twice daily regular budesonide (nequals;139). Unfortunately there was no placebo limb. There was no significant difference in any outcomes, specifically including frequency of exacerbations, time to first exacerbation, frequency of treatment for respiratory illness and time to first treatment for respiratory illness. From these data, it is clear that, in the setting of episodic viral wheeze, continuous budesonide does not prevent exacerbations, does not make them any less severe and does not result in any less treatment for acute symptoms, but does lead to an increase in the steroid dose taken. Unfortunately, in the absence of a placebo group, we do not know whether either treatment was at all helpful. We can certainly use this study to refute the need for pre-school children to be treated with ICS for episodic viral wheeze.
Treatment of school-age asthma
Intermittent therapy
The clinical reality is that adherence is poor even in very severe asthma [28], and it is likely that children with mild asthma are deliberately treated intermittently at home. The TREXA (TReating Children to Prevent Exacerbations of Asthma) study assigned 288 children aged 5–18 yrs to one of four regimes in a 44-week study [133]. The children had well-controlled, mild, persistent asthma such that treatment could be discontinued. The regimes are shown in the table 2, and the primary outcome was time to first prednisolone burst. The frequency of exacerbations was lower in all three beclomethasone diproprionate groups compared with the placebo group (group 4). Linear growth was 1.1±0.3 cm less in the two continuous beclomethasone diproprionate groups (groups 1 and 3; p<0.0001), but not in the rescue group (group 2; pequals;0.26) compared with the placebo group. This study suggests that rescue therapy with ICS during tapering may be a beneficial strategy, and adds to the evidence that ICS at the time of viral infections may be beneficial in children with asthma. This study agrees with the Finnish data which suggests that intermittent ICS may be as effective, and with fewer side-effects, than continuous ICS in children with mild asthma [134–136].
Table 2. Treatment regimens for the TREXA study.
| Group | Subjects n | Regular therapy | Exacerbation therapy |
| 1 | 71 | BDP 50 μg twice a day | BDP 100 μg/β2-rescue |
| 2 | 72 | Placebo | BDP 100 μg/β2-rescue |
| 3 | 71 | BDP 50 μg twice a day | Placebo/β2-rescue |
| 4 | 74 | Placebo | Placebo/β2-rescue |
TREXA: TReating Children to Prevent Exacerbations of Asthma; BDP: beclomethasone diproprionate.
Add-on therapy
The BADGER study [129] enrolled 182 children who were symptomatic despite being prescribed fluticasone 100 μg twice daily. The investigators used a triple cross-over, unblinded design to assess whether additional therapy with high dose ICS, LABA or LTRA was better. The salient features of the results were: 1) that additional LABA therapy performed best for the group, although many children performed better with the other alternatives; 2) no biomarker predicted best response to LABA, the children who were more likely to respond had better baseline asthma control; and 3) the peak of the ICS dose response curve for most of the children was observed during administration of low dose fluticasone. So we need better biomarkers, and LABA is probably the first-line add-on therapy, but LTRA and high dose ICS can be tested in non-responders.
Beyond guidelines therapy: currently available treatment
There is increasing evidence that background eosinophilic inflammation and viral infections interact to produce acute asthma attacks [137, 138]. Two recent studies have shown that strategies likely to have reduced airway eosinophilia also reduce acute asthma attacks [139, 140]. The anti-IgE monoclonal antibody omalizumab is a well-established therapy for asthma in childhood. A randomised, double-blind, placebo-controlled study of more than 400 inner city children and young adults aged 6–20 yrs demonstrated that omalizumab did not just merely improve the number of symptom free days, but also significantly reduced the number of children having an exacerbation from 48.8% to 30.3% [139]. In a post hoc analysis, the seasonal peak of exacerbations was abolished. Response was better in the children with higher FeNO and blood eosinophils [141, 142]. A study in younger children aged 6–<12 yrs showed that omalizumab therapy led to a 31% reduction in exacerbation rates [140]. Taken together, these studies suggest that background airway eosinophilic inflammation may contribute significantly to exacerbations.
Beyond guidelines therapy: future treatment
A large adult study showed that the addition of tiotropium to the regime of patients who were symptomatic despite ICS therapy was superior to doubling the dose of ICS and equivalent to adding a LABA [143]. There is no paediatric study of tiotropium, but there is an urgent need to explore its role.
Possible new treatment alternatives
Several new treatment alternatives are in the pipeline, including pitrakinra (IL4-/IL-13 antagonist) [144], lebrikizumab (IL-13 antagonist) [145] and reslizumab (antibody against IL-5) [146], all of which predominantly target allergic asthma. As these are, or are likely to be, expensive treatment alternatives, detailed characterisation of patients in order to identify those most likely to benefit from these interventions will be increasingly important. A novel marker of potential clinical relevance is periostin, a protein suggested as a marker of excessive Th2-type inflammation in asthma [147]. The expression of periostin in airway epithelial cells is regulated by IL-13 [148]. The effect of lebrikizumab treatment has been shown to be greater in severe asthmatics with high periostin levels compared to those with low periostin levels, as demonstrated by an improvement in FEV1 and a reduction in FeNO [145], thus providing an entirely new example of biomarker-guided treatment in severe asthma.
New treatment alternatives for asthma, particularly in children, should probably not just focus on suppressing the inflammatory response. The idea of primary prevention of asthma is becoming an option [54] and in this regard combining vaccines for allergy and rhinovirus infections are a novel and interesting approach [149]. Another novel approach is intralymphatic immunotherapy which may turn out to be a “fast-track”, effective alternative to subcutaneous immunotherapy [150]. Finally, vitamin D supplementation could be a straightforward treatment alternative to strengthen the immune response in children with therapy resistant asthma [48], although more trials are needed.
ADHERENCE TO TREATMENT
Reliable assessment of adherence to prescribed treatment is a challenge in clinical practice, as well as in research on patients with asthma. Krishnan et al. [151] compared subjective and objective measurements of children's adherence to ICS therapy in a sub-study to the CAMP study [151]. They compared reported intake of ICS, as reported in diary cards, to the number of doses left in the study inhalers. The difference was striking. Adherence of <80% of the prescribed doses was seen in 75% of the children by objective measures while this lack of adherence was only reported in 6% of the children by self-report in the diary cards. The parents’ perception of the child’s asthma is crucial for adherence to recommended therapy. This has been shown in several studies from the Netherlands. Klok et al. [152] reported on the importance of follow-up and discussion with parents on their perceptions of the child’s asthma. Koster et al. [30] reported how parents concern about side-effects affected their adherence to prescribed therapy and also that under treatment was associated with lower maternal education. Caudri et al. [153] reported from the 8-yr follow-up of the PIAMA cohort that under treatment was common but also over treatment was found in children who continued regular use of ICS while symptom free for >1 yr.
CONCLUSION
We have described a number of very exciting advances in paediatric asthma. However, the overall message for clinicians is timeless: it is essential to get the basics right. More mistakes are made through neglecting this principle than by failing to deploy the latest sophisticated treatments. Finally, it should be emphasised that childhood asthma also could be treated at the community level, as shown in a study by Mackay et al. [154]. A reduction of hospital admissions because of childhood asthma was seen after smoking was prohibited in public places in Scotland, UK. Another example of the impact of air pollution on asthma morbidity was provided by Renzetti et al. [155], who report reduced markers of airway inflammation and improved pulmonary function in asthmatic children who were relocated from a highly polluted urban area to a less polluted rural area. These studies should remind all healthcare providers to take every opportunity to advocate measures to improve indoor and outdoor air quality.
Footnotes
Provenance
Submitted article, peer reviewed.
Statement of Interest
None declared.
REFERENCES
- 1.Bousquet J, Mantzouranis E, Cruz AA, et al. Uniform definition of asthma severity, control, and exacerbations: document presented for the World Health Organization Consultation on Severe Asthma. J Allergy Clin Immunol 2010; 126: 926–938. [DOI] [PubMed] [Google Scholar]
- 2.Krishnan JA, Lemanske RF, Jr, Canino GJ, et al. Asthma outcomes: symptoms. J Allergy Clin Immunol 2012; 129: Suppl. 3, S124–S135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He XY, Simpson JL, Wang F. Inflammatory phenotypes in stable and acute childhood asthma. Paediatr Respir Rev 2011; 12: 165–169. [DOI] [PubMed] [Google Scholar]
- 4.Bossley CJ, Fleming L, Gupta A, et al. Pediatric severe asthma is characterized by eosinophilia and remodeling without T(H)2 cytokines. J Allergy Clin Immunol 2012; 129: 974–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bousquet J, Anto J, Auffray C, et al. MeDALL (Mechanisms of the Development of ALLergy): an integrated approach from phenotypes to systems medicine. Allergy 2011; 66: 596–604. [DOI] [PubMed] [Google Scholar]
- 6.Anto JM, Pinart M, Akdis M, et al. Understanding the complexity of IgE-related phenotypes from childhood to young adulthood: a Mechanisms of the Development of Allergy (MeDALL) Seminar. J Allergy Clin Immunol 2012; 129: 943–954. [DOI] [PubMed] [Google Scholar]
- 7.Global Initiative for Asthma. Global strategy for asthma management and prevention. 2008. Updated December 2009. www.ginasthma.org/uploads/users/files/GINA_Report2011_May4.pdf.
- 8.Koolen BB, Pijnenburg MWH, Brackel HJL, et al. Comparing Global Initiative for Asthma (GINA) criteria with the Childhood Asthma Control Test (C-ACT) and Asthma Control Test (ACT). Eur Respir J 2011; 38: 561–566. [DOI] [PubMed] [Google Scholar]
- 9.Klok T, Kaptein AA, Duiverman EJ, et al. High inhaled corticosteroids adherence in childhood asthma: the role of medication beliefs. Eur Respir J 2012; [Epub ahead of print DOI: 10.1183/09031936.00191511]. [DOI] [PubMed] [Google Scholar]
- 10.Boyd M, Lasserson TJ, McKean MC, et al. Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev 2009; 2: CD001290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai CK, Beasley R, Crane J, et al. Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 2009; 64: 476–483. [DOI] [PubMed] [Google Scholar]
- 12.Gore FM, Bloem PJ, Patton GC, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet 2011; 377: 2093–2102. [DOI] [PubMed] [Google Scholar]
- 13.To T, Wang C, Guan J, et al. What is the lifetime risk of physician-diagnosed asthma in Ontario, Canada? Am J Respir Crit Care Med 2010; 181: 337–343. [DOI] [PubMed] [Google Scholar]
- 14.Duggan EM, Sturley J, Fitzgerald AP, et al. The 2002–2007 trends of prevalence of asthma, allergic rhinitis and eczema in Irish schoolchildren. Pediatr Allergy Immunol 2012; [Epub ahead of print DOI: 10.1111/j.1399-3038.2012.01291.x]. [DOI] [PubMed] [Google Scholar]
- 15.Thomas A, Lemanske RF, Jr, Jackson DJ. Approaches to stepping up and stepping down care in asthmatic patients. J Allergy Clin Immunol 2011; 128: 915–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonfield TL, Ross KR. Asthma heterogeneity and therapeutic options from the clinic to the bench. Curr Opin Allergy Clin Immunol 2012; 12: 60–67. [DOI] [PubMed] [Google Scholar]
- 17.Taylor DR, Bateman ED, Boulet LP, et al. A new perspective on concepts of asthma severity and control. Eur Respir J 2008; 32: 545–554. [DOI] [PubMed] [Google Scholar]
- 18.Lang A, Carlsen KH, Haaland G, et al. Severe asthma in childhood: assessed in 10 year olds in a birth cohort study. Allergy 2008; 63: 1054–1060. [DOI] [PubMed] [Google Scholar]
- 19.Bush A, Zar HJ. WHO universal definition of severe asthma. Curr Opin Allergy Clin Immunol 2011; 11: 115–121. [DOI] [PubMed] [Google Scholar]
- 20.Bossley CJ, Saglani S, Kavanagh C, et al. Corticosteroid responsiveness and clinical characteristics in childhood difficult asthma. Eur Respir J 2009; 34: 1052–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bush A, Hedlin G, Carlsen KH, et al. Severe childhood asthma: a common international approach? Lancet 2008; 372: 1019–1021. [DOI] [PubMed] [Google Scholar]
- 22.Hedlin G, Bush A, Lødrup Carlsen K, et al. Problematic severe asthma in children, not one problem but many: a GA2LEN initiative. Eur Respir J 2010; 36: 196–201. [DOI] [PubMed] [Google Scholar]
- 23.Konradsen JR, Nordlund B, Lidegran M, et al. Problematic severe asthma: a proposed approach to identifying children who are severely resistant to therapy. Pediatr Allergy Immunol 2011; 22: 9–18. [DOI] [PubMed] [Google Scholar]
- 24.Bush A, Saglani S. Management of severe asthma in children. Lancet 2010; 376: 814–825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fitzpatrick AM, Teague WG, Meyers DA, et al. Heterogeneity of severe asthma in childhood: confirmation by cluster analysis of children in the National Institutes of Health/National Heart, Lung, and Blood Institute Severe Asthma Research Program. J Allergy Clin Immunol 2011; 127: 382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nordlund B, Konradsen J, Pedroletti C, et al. The clinical benefit of evaluating health-related quality-of-life in children with problematic severe asthma. Acta Paediatr 2011; 100: 1454–1460. [DOI] [PubMed] [Google Scholar]
- 27.Bush A, Pedersen S, Hedlin G, et al. Pharmacological treatment of severe, therapy-resistant asthma in children: what can we learn from where? Eur Respir J 2011; 38: 947–958. [DOI] [PubMed] [Google Scholar]
- 28.Bracken M, Fleming L, Hall P, et al. The importance of nurse-led home visits in the assessment of children with problematic asthma. Arch Dis Child 2009; 94: 780–784. [DOI] [PubMed] [Google Scholar]
- 29.Lødrup Carlsen KC, Hedlin G, Bush A, et al. Assessment of problematic severe asthma in children. Eur Respir J 2011; 37: 432–440. [DOI] [PubMed] [Google Scholar]
- 30.Koster ES, Wijga AH, Koppelman GH, et al. Uncontrolled asthma at age 8: the importance of parental perception towards medication. Pediatr Allergy Immunol 2011; 22: 462–468. [DOI] [PubMed] [Google Scholar]
- 31.Wu AC, Tantisira K, Li L, et al. Predictors of symptoms are different from predictors of severe exacerbations from asthma in children. Chest 2011; 140: 100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bousquet J, Schunemann HJ, Zuberbier T, et al. Development and implementation of guidelines in allergic rhinitis: an ARIA-GA2LEN paper. Allergy 2010; 65: 1212–1221. [DOI] [PubMed] [Google Scholar]
- 33.Boulay ME, Boulet LP. The relationships between atopy, rhinitis and asthma: pathophysiological considerations. Curr Opin Allergy Clin Immunol 2003; 3: 51–55. [DOI] [PubMed] [Google Scholar]
- 34.de Groot EP, Nijkamp A, Duiverman EJ, et al. Allergic rhinitis is associated with poor asthma control in children with asthma. Thorax 2012; 67: 582–587. [DOI] [PubMed] [Google Scholar]
- 35.Chawes BL, Bonnelykke K, Kreiner-Moller E, et al. Children with allergic and nonallergic rhinitis have a similar risk of asthma. J Allergy Clin Immunol 2010; 126: 567–573. [DOI] [PubMed] [Google Scholar]
- 36.Hastan D, Fokkens WJ, Bachert C, et al. Chronic rhinosinusitis in Europe – an underestimated disease. A GA(2)LEN study. Allergy 2011; 66: 1216–1223. [DOI] [PubMed] [Google Scholar]
- 37.Thakkar K, Boatright RO, Gilger MA, et al. Gastroesophageal reflux and asthma in children: a systematic review. Pediatrics 2010; 125: e925–e930. [DOI] [PubMed] [Google Scholar]
- 38.Stordal K, Johannesdottir GB, Bentsen BS, et al. Acid suppression does not change respiratory symptoms in children with asthma and gastro-oesophageal reflux disease. Arch Dis Child 2005; 90: 956–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Holbrook JT, Wise RA, Gold BD, et al. Lansoprazole for children with poorly controlled asthma: a randomized controlled trial. JAMA 2012; 307: 373–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Low K, Lau KK, Holmes P, et al. Abnormal vocal cord function in difficult-to-treat asthma. Am J Respir Crit Care Med 2011; 184: 50–56. [DOI] [PubMed] [Google Scholar]
- 41.Ayres JG, Mansur AH. Vocal cord dysfunction and severe asthma: considering the total airway. Am J Respir Crit Care Med 2011; 184: 2–3. [DOI] [PubMed] [Google Scholar]
- 42.Forno E, Lescher R, Strunk R, et al. Decreased response to inhaled steroids in overweight and obese asthmatic children. J Allergy Clin Immunol 2011; 127: 741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Holguin F, Bleecker ER, Busse WW, et al. Obesity and asthma: an association modified by age of asthma onset. J Allergy Clin Immunol 2011; 127: 1486–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cibella F, Cuttitta G, La Grutta S, et al. A cross-sectional study assessing the relationship between BMI, asthma, atopy, and eNO among schoolchildren. Ann Allergy Asthma Immunol 2011; 107: 330–336. [DOI] [PubMed] [Google Scholar]
- 45.Quinto KB, Zuraw BL, Poon KY, et al. The association of obesity and asthma severity and control in children. J Allergy Clin Immunol 2011; 128: 964–969. [DOI] [PubMed] [Google Scholar]
- 46.Sutherland ER, Goleva E, Strand M, et al. Body mass and glucocorticoid response in asthma. Am J Respir Crit Care Med 2008; 178: 682–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cottrell L, Neal WA, Ice C, et al. Metabolic abnormalities in children with asthma. Am J Respir Crit Care Med 2011; 183: 441–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gupta A, Sjoukes A, Richards D, et al. Relationship between serum vitamin D, disease severity, and airway remodeling in children with asthma. Am J Respir Crit Care Med 2011; 184: 1342–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brehm JM, Schuemann B, Fuhlbrigge AL, et al. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J Allergy Clin Immunol 2010; 126: 52–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chinellato I, Piazza M, Sandri M, et al. Serum vitamin D levels and exercise-induced bronchoconstriction in children with asthma. Eur Respir J 2011; 37: 1366–1370. [DOI] [PubMed] [Google Scholar]
- 51.Chung KF, Bel EH, Wenzel S, eds. Difficult-to-Treat Severe asthma. Eur Respir Monogr 2011; 51: 1–308. [Google Scholar]
- 52.Holt PG, Strickland DH, Sly PD. Virus infection and allergy in the development of asthma: what is the connection? Curr Opin Allergy Clin Immunol 2012; 12: 151–157. [DOI] [PubMed] [Google Scholar]
- 53.Jackson DJ, Evans MD, Gangnon RE, et al. Evidence for a causal relationship between allergic sensitization and rhinovirus wheezing in early life. Am J Respir Crit Care Med 2012; 185: 281–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martinez FD. New insights into the natural history of asthma: primary prevention on the horizon. J Allergy Clin Immunol 2011; 128: 939–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Busse WW, Lemanske RF, Jr, Gern JE. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet 2010; 376: 826–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jackson DJ, Sykes A, Mallia P, et al. Asthma exacerbations: origin, effect, and prevention. J Allergy Clin Immunol 2011; 128: 1165–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Strickland DH, Holt PG. T regulatory cells in childhood asthma. Trends Immunol 2011; 32: 420–427. [DOI] [PubMed] [Google Scholar]
- 58.Kim HY, DeKruyff RH, Umetsu DT. The many paths to asthma: phenotype shaped by innate and adaptive immunity. Nat Immunol 2010; 11: 577–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Locksley RM. Asthma and allergic inflammation. Cell 2010; 140: 777–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ramakrishna L, de Vries VC, Curotto deLafaille MA. Cross-roads in the lung: immune cells and tissue interactions as determinants of allergic asthma. Immunol Res 2012; [Epub ahead of print DOI: 10.1007/s12026-012-8296-4]. [DOI] [PubMed] [Google Scholar]
- 61.Gaston B. The biochemistry of asthma. Biochim Biophys Acta 2011; 1810: 1017–1024. [DOI] [PubMed] [Google Scholar]
- 62.Monteseirin J. Neutrophils and asthma. J Investig Allergol Clin Immunol 2009; 19: 340–354. [PubMed] [Google Scholar]
- 63.Durrani SR, Viswanathan RK, Busse WW. What effect does asthma treatment have on airway remodeling? Current perspectives. J Allergy Clin Immunol 2011; 128: 439–448. [DOI] [PubMed] [Google Scholar]
- 64.Fitzpatrick AM, Teague WG. Progressive airflow limitation is a feature of children with severe asthma. J Allergy Clin Immunol 2011; 127: 282–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Borres MP, Ebisawa M, Eigenmann PA. Use of allergen components begins a new era in pediatric allergology. Pediatr Allergy Immunol 2011; 22: 454–461. [DOI] [PubMed] [Google Scholar]
- 66.Larche M. T cell epitope-based allergy vaccines. Curr Top Microbiol Immunol 2011; 352: 107–119. [DOI] [PubMed] [Google Scholar]
- 67.Madhurantakam C, Nilsson OB, Uchtenhagen H, et al. Crystal structure of the dog lipocalin allergen Can f 2: implications for cross-reactivity to the cat allergen Fel d 4. J Mol Biol 2010; 401: 68–83. [DOI] [PubMed] [Google Scholar]
- 68.Saarelainen SA, Kinnunen TT, Buhot C, et al. Immunotherapeutic potential of the immunodominant T-cell epitope of lipocalin allergen Bos d 2 and its analogues. Immunology 2008; 123: 358–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Voehringer D. Basophils in allergic immune responses. Curr Opin Immunol 2011; 23: 789–793. [DOI] [PubMed] [Google Scholar]
- 70.Karasuyama H, Obata K, Wada T, et al. Newly appreciated roles for basophils in allergy and protective immunity. Allergy 2011; 66: 1133–1141. [DOI] [PubMed] [Google Scholar]
- 71.Taylor DR. Using biomarkers in the assessment of airways disease. J Allergy Clin Immunol 2011; 128: 927–934. [DOI] [PubMed] [Google Scholar]
- 72.Szefler SJ, Wenzel S, Brown R, et al. Asthma outcomes: biomarkers. J Allergy Clin Immunol 2012; 129: Suppl. 3, S9–S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Busse WW. Asthma diagnosis and treatment: filling in the information gaps. J Allergy Clin Immunol 2011; 128: 740–750. [DOI] [PubMed] [Google Scholar]
- 74.van Dalen C, Harding E, Parkin J, et al. Suitability of forced expiratory volume in 1 second/forced vital capacity vs percentage of predicted forced expiratory volume in 1 second for the classification of asthma severity in adolescents. Arch Pediatr Adolesc Med 2008; 162: 1169–1174. [DOI] [PubMed] [Google Scholar]
- 75.Fitzpatrick AM, Gaston BM, Erzurum SC, et al. Features of severe asthma in school-age children: atopy and increased exhaled nitric oxide. J Allergy Clin Immunol 2006; 118: 1218–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dweik RA, Sorkness RL, Wenzel S, et al. Use of exhaled nitric oxide measurement to identify a reactive, at-risk phenotype among patients with asthma. Am J Respir Crit Care Med 2010; 181: 1033–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cockcroft DW. Direct challenge tests: airway hyperresponsiveness in asthma: its measurement and clinical significance. Chest 2010; 138: Suppl. 2, 18S–24S. [DOI] [PubMed] [Google Scholar]
- 78.Anderson SD. Indirect challenge tests: airway hyperresponsiveness in asthma: its measurement and clinical significance. Chest 2010; 138: Suppl. 2, 25S–30S. [DOI] [PubMed] [Google Scholar]
- 79.Lex C, Payne DN, Zacharasiewicz A, et al. Sputum induction in children with difficult asthma: safety, feasibility, and inflammatory cell pattern. Pediatric Pulmonol 2005; 39: 318–324. [DOI] [PubMed] [Google Scholar]
- 80.Drews AC, Pizzichini MM, Pizzichini E, et al. Neutrophilic airway inflammation is a main feature of induced sputum in nonatopic asthmatic children. Allergy 2009; 64: 1597–1601. [DOI] [PubMed] [Google Scholar]
- 81.Kulkarni N, Ragazzo V, Costella S, et al. Eosinophilic airway inflammation is increased in children with asthma and food allergies. Pediatr Allergy Immunol 2012; 23: 28–33. [DOI] [PubMed] [Google Scholar]
- 82.Fleming L, Wilson N, Regamey N, et al. Use of sputum eosinophil counts to guide management in children with severe asthma. Thorax 2012; 67: 193–198. [DOI] [PubMed] [Google Scholar]
- 83.Petsky HL, Cates CJ, Lasserson TJ, et al. A systematic review and meta-analysis: tailoring asthma treatment on eosinophilic markers (exhaled nitric oxide or sputum eosinophils). Thorax 2012; 67: 199–208. [DOI] [PubMed] [Google Scholar]
- 84.van de Kant KD, Jansen MA, Klaassen EM, et al. Elevated inflammatory markers at preschool age precede persistent wheezing at school age. Pediatr Allergy Immunol 2012; 23: 259–264. [DOI] [PubMed] [Google Scholar]
- 85.Zeiger RS, Schatz M, Zhang F, et al. Association of exhaled nitric oxide to asthma burden in asthmatics on inhaled corticosteroids. J Asthma 2011; 48: 8–17. [DOI] [PubMed] [Google Scholar]
- 86.Zeiger RS, Schatz M, Zhang F, et al. Elevated exhaled nitric oxide is a clinical indicator of future uncontrolled asthma in asthmatic patients on inhaled corticosteroids. J Allergy Clin Immunol 2011; 128: 412–414. [DOI] [PubMed] [Google Scholar]
- 87.Pijnenburg MW, Bakker EM, Hop WC, et al. Titrating steroids on exhaled nitric oxide in children with asthma: a randomized controlled trial. Am J Respir Crit Care Med 2005; 172: 831–836. [DOI] [PubMed] [Google Scholar]
- 88.de Jongste JC, Carraro S, Hop WC, et al. Daily telemonitoring of exhaled nitric oxide and symptoms in the treatment of childhood asthma. Am J Respir Crit Care Med 2009; 179: 93–97. [DOI] [PubMed] [Google Scholar]
- 89.Szefler SJ, Mitchell H, Sorkness CA, et al. Management of asthma based on exhaled nitric oxide in addition to guideline-based treatment for inner-city adolescents and young adults: a randomised controlled trial. Lancet 2008; 372: 1065–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Waibel V, Ulmer H, Horak E. Assessing asthma control: symptom scores, GINA levels of asthma control, lung function, and exhaled nitric oxide. Pediatric Pulmonol 2012; 47: 113–118. [DOI] [PubMed] [Google Scholar]
- 91.Stern G, de Jongste J, van der Valk R, et al. Fluctuation phenotyping based on daily fraction of exhaled nitric oxide values in asthmatic children. J Allergy Clin Immunol 2011; 128: 293–300. [DOI] [PubMed] [Google Scholar]
- 92.Aujla SJ, Ross KR, Chmiel JF, et al. Airway molecular phenotypes in pediatric asthma. Curr Opin Allergy Clin Immunol 2011; 11: 122–126. [DOI] [PubMed] [Google Scholar]
- 93.Caballero Balanza S, Martorell Aragones A, Cerda Mir JC, et al. Leukotriene B4 and 8-isoprostane in exhaled breath condensate of children with episodic and persistent asthma. J Investig Allergol Clin Immunol 2010; 20: 237–243. [PubMed] [Google Scholar]
- 94.Profita M, Montuschi P, Bonanno A, et al. Novel perspectives in the detection of oral and nasal oxidative stress and inflammation in pediatric united airway diseases. Int J Immunopathol Pharmacol 2010; 23: 1211–1219. [DOI] [PubMed] [Google Scholar]
- 95.Sachs-Olsen C, Sanak M, Lang AM, et al. Eoxins: a new inflammatory pathway in childhood asthma. J Allergy Clin Immunol 2010; 126: 859–867. [DOI] [PubMed] [Google Scholar]
- 96.Carraro S, Cogo PE, Isak I, et al. EIA and GC/MS analysis of 8-isoprostane in EBC of children with problematic asthma. Eur Respir J 2010; 35: 1364–1369. [DOI] [PubMed] [Google Scholar]
- 97.Bloemen K, Van Den Heuvel R, Govarts E, et al. A new approach to study exhaled proteins as potential biomarkers for asthma. Clin Exp Allergy 2011; 41: 346–356. [DOI] [PubMed] [Google Scholar]
- 98.Dompeling E, Jöbsis Q. Proteomics of exhaled breath condensate: a realistic approach in children with asthma? Clin Exp Allergy 2011; 41: 299–301. [DOI] [PubMed] [Google Scholar]
- 99.Sinha A, Krishnan V, Sethi T, et al. Metabolomic signatures in nuclear magnetic resonance spectra of exhaled breath condensate identify asthma. Eur Respir J 2012; 39: 500–502. [DOI] [PubMed] [Google Scholar]
- 100.Saude EJ, Skappak CD, Regush S, et al. Metabolomic profiling of asthma: diagnostic utility of urine nuclear magnetic resonance spectroscopy. J Allergy Clin Immunol 2011; 127: 757–764. [DOI] [PubMed] [Google Scholar]
- 101.Mattarucchi E, Baraldi E, Guillou C. Metabolomics applied to urine samples in childhood asthma: differentiation between asthma phenotypes and identification of relevant metabolites. Biomed Chromatogr 2012; 26: 89–94. [DOI] [PubMed] [Google Scholar]
- 102.Rabinovitch N, Graber NJ, Chinchilli VM, et al. Urinary leukotriene E4/exhaled nitric oxide ratio and montelukast response in childhood asthma. J Allergy Clin Immunol 2010; 126: 545–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Brockmann PE, Castro-Rodriguez JA, Holmgren NL, et al. Urinary leukotriene excretion profile in children with exercise-induced asthma compared with controls: a preliminary study. Allergol Immunopathol (Madr) 2011; 40: 181–186. [DOI] [PubMed] [Google Scholar]
- 104.Wedes SH, Wu W, Comhair SA, et al. Urinary bromotyrosine measures asthma control and predicts asthma exacerbations in children. J Pediatr 2011; 159: 248–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Bussink AP, Speijer D, Aerts JM, et al. Evolution of mammalian chitinase(-like) members of family 18 glycosyl hydrolases. Genetics 2007; 177: 959–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bargagli E, Olivieri C, Margollicci M, et al. Serum chitotriosidase levels in patients with allergic and non-allergic asthma. Respiration 2010; 79: 437–438. [DOI] [PubMed] [Google Scholar]
- 107.Chupp GL, Lee CG, Jarjour N, et al. A chitinase-like protein in the lung and circulation of patients with severe asthma. N Engl J Med 2007; 357: 2016–2027. [DOI] [PubMed] [Google Scholar]
- 108.Lee CG, Da Silva CA, Dela Cruz CS, et al. Role of chitin and chitinase/chitinase-like proteins in inflammation, tissue remodeling, and injury. Annu Rev Physiol 2011; 73: 479–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bara I, Ozier A, Girodet PO, et al. Role of YKL-40 in bronchial smooth muscle remodeling in asthma. Am J Respir Crit Care Med 2012; 185: 715–722. [DOI] [PubMed] [Google Scholar]
- 110.Letuve S, Kozhich A, Arouche N, et al. YKL-40 is elevated in patients with chronic obstructive pulmonary disease and activates alveolar macrophages. J Immunol 2008; 181: 5167–5173. [DOI] [PubMed] [Google Scholar]
- 111.Otsuka K, Matsumoto H, Niimi A, et al. Sputum YKL-40 levels and pathophysiology of asthma and chronic obstructive pulmonary disease. Respiration 2012; 83: 507–519. [DOI] [PubMed] [Google Scholar]
- 112.Douros K, Alexopoulou E, Nicopoulou A, et al. Bronchoscopic and high-resolution CT scan findings in children with chronic wet cough. Chest 2011; 140: 317–323. [DOI] [PubMed] [Google Scholar]
- 113.Gupta S, Siddiqui S, Haldar P, et al. Qualitative analysis of high-resolution CT scans in severe asthma. Chest 2009; 136: 1521–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gupta S, Siddiqui S, Haldar P, et al. Quantitative analysis of high-resolution computed tomography scans in severe asthma subphenotypes. Thorax 2010; 65: 775–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tashkin DP, de Lange EE. Imaging of the distal airways. J Allergy Clin Immunol 2009; 124: Suppl. 6, S78–S83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Aysola R, de Lange EE, Castro M, et al. Demonstration of the heterogeneous distribution of asthma in the lungs using CT and hyperpolarized helium-3 MRI. J Magn Reson Imaging 2010; 32: 1379–1387. [DOI] [PubMed] [Google Scholar]
- 117.Bousquet J, Heinzerling L, Bachert C, et al. Practical guide to skin prick tests in allergy to aeroallergens. Allergy 2012; 67: 18–24. [DOI] [PubMed] [Google Scholar]
- 118.Frith J, Fleming L, Bossley C, et al. The complexities of defining atopy in severe childhood asthma. Clin Exp Allergy 2011; 41: 948–953. [DOI] [PubMed] [Google Scholar]
- 119.Gronlund H, Adedoyin J, Reininger R, et al. Higher immunoglobulin E antibody levels to recombinant Fel d 1 in cat-allergic children with asthma compared with rhinoconjunctivitis. Clin Exp Allergy 2008; 38: 1275–1281. [DOI] [PubMed] [Google Scholar]
- 120.Sastre J. Molecular diagnosis in allergy. Clin Exp Allergy 2010; 40: 1442–1460. [DOI] [PubMed] [Google Scholar]
- 121.Asarnoj A, Moverare R, Ostblom E, et al. IgE to peanut allergen components: relation to peanut symptoms and pollen sensitization in 8-year-olds. Allergy 2010; 65: 1189–1195. [DOI] [PubMed] [Google Scholar]
- 122.Nordlund B, Konradsen JR, Kull I, et al. IgE antibodies to animal-derived lipocalin, kallikrein and secretoglobin are markers of bronchial inflammation in severe childhood asthma: airway diseases. Allergy 2012; 67: 661–669. [DOI] [PubMed] [Google Scholar]
- 123.Johansson SG, Nopp A, van Hage M, et al. Passive IgE-sensitization by blood transfusion. Allergy 2005; 60: 1192–1199. [DOI] [PubMed] [Google Scholar]
- 124.Dahlen B, Nopp A, Johansson SG, et al. Basophil allergen threshold sensitivity, CD-sens, is a measure of allergen sensitivity in asthma. Clin Exp Allergy 2011; 41: 1091–1097. [DOI] [PubMed] [Google Scholar]
- 125.Konradsen JR, Nordlund B, Nilsson OB, et al. High basophil allergen sensitivity (CD-sens) is associated with severe allergic asthma in children. Pediatr Allergy Immunol 2012; 23: 376–384. [DOI] [PubMed] [Google Scholar]
- 126.Siracusa MC, Saenz SA, Hill DA, et al. TSLP promotes interleukin-3-independent basophil haematopoiesis and type 2 inflammation. Nature 2011; 477: 229–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bush A, Frey U, Teague WG. Special problems of severe asthma in childhood. Eur Respir Monogr 2011; 51: 59–81. [Google Scholar]
- 128.Boulet LP, Fitzgerald JM, Levy ML, et al. A guide to the translation of Global Initiative for Asthma (GINA) strategy into improved care. Eur Respir J 2012; 39: 1220–1229. [DOI] [PubMed] [Google Scholar]
- 129.Lemanske RF, Jr, Mauger DT, Sorkness CA, et al. Step-up therapy for children with uncontrolled asthma receiving inhaled corticosteroids. N Engl J Med 2010; 362: 975–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Levy ML, Thomas M, Small I, et al. Summary of the 2008 BTS/SIGN British Guideline on the management of asthma. Prim Care Respir J 2009; 18: Suppl. 1, S1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Brand PLP, Baraldi E, Bisgaard H, et al. Definition, assessment and treatment of wheezing disorders in preschool children: an evidence-based approach. Eur Respir J 2008; 32: 1096–1110. [DOI] [PubMed] [Google Scholar]
- 132.Zeiger RS, Mauger D, Bacharier LB, et al. Daily or intermittent budesonide in preschool children with recurrent wheezing. N Engl J Med 2011; 365: 1990–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Martinez FD, Chinchilli VM, Morgan WJ, et al. Use of beclomethasone dipropionate as rescue treatment for children with mild persistent asthma (TREXA): a randomised, double-blind, placebo-controlled trial. Lancet 2011; 377: 650–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Turpeinen M, Nikander K, Pelkonen AS, et al. Daily versus as-needed inhaled corticosteroid for mild persistent asthma (The Helsinki early intervention childhood asthma study). Arch Dis Child 2008; 93: 654–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Turpeinen M, Pelkonen AS, Nikander K, et al. Bone mineral density in children treated with daily or periodical inhaled budesonide: the Helsinki Early Intervention Childhood Asthma study. Pediatr Res 2010; 68: 169–173. [DOI] [PubMed] [Google Scholar]
- 136.Turpeinen M, Raitio H, Pelkonen AS, et al. Skin thickness in children treated with daily or periodical inhaled budesonide for mild persistent asthma. The Helsinki early intervention childhood asthma study. Pediatr Res 2010; 67: 221–225. [DOI] [PubMed] [Google Scholar]
- 137.Murray CS, Poletti G, Kebadze T, et al. Study of modifiable risk factors for asthma exacerbations: virus infection and allergen exposure increase the risk of asthma hospital admissions in children. Thorax 2006; 61: 376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Subrata LS, Bizzintino J, Mamessier E, et al. Interactions between innate antiviral and atopic immunoinflammatory pathways precipitate and sustain asthma exacerbations in children. J Immunol 2009; 183: 2793–2800. [DOI] [PubMed] [Google Scholar]
- 139.Busse WW, Morgan WJ, Gergen PJ, et al. Randomized trial of omalizumab (anti-IgE) for asthma in inner-city children. N Engl J Med 2011; 364: 1005–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lanier B, Bridges T, Kulus M, et al. Omalizumab for the treatment of exacerbations in children with inadequately controlled allergic (IgE-mediated) asthma. J Allergy Clin Immunol 2009; 124: 1210–1216. [DOI] [PubMed] [Google Scholar]
- 141.Pavord ID, Bush A. Anti-IgE for asthma in inner-city children. N Engl J Med 2011; 364: 2556–2557. [DOI] [PubMed] [Google Scholar]
- 142.Busse WW, Gergen PJ, Calatroni A. Anti IgE for asthma in inner-city children: authors response. N Engl J Med 2011; 364: 2557–2558. [DOI] [PubMed] [Google Scholar]
- 143.Peters SP, Kunselman SJ, Icitovic N, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med 2010; 363: 1715–1726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wenzel S, Wilbraham D, Fuller R, et al. Effect of an interleukin-4 variant on late phase asthmatic response to allergen challenge in asthmatic patients: results of two phase 2a studies. Lancet 2007; 370: 1422–1431. [DOI] [PubMed] [Google Scholar]
- 145.Corren J, Lemanske RF, Hanania NA, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med 2011; 365: 1088–1098. [DOI] [PubMed] [Google Scholar]
- 146.Castro M, Mathur S, Hargreave F, et al. Reslizumab for poorly controlled, eosinophilic asthma: a randomized, placebo-controlled study. Am J Respir Crit Care Med 2011; 184: 1125–1132. [DOI] [PubMed] [Google Scholar]
- 147.Woodruff PG, Modrek B, Choy DF, et al. T-helper type 2-driven inflammation defines major subphenotypes of asthma. Am J Respir Crit Care Med 2009; 180: 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Woodruff PG, Boushey HA, Dolganov GM, et al. Genome-wide profiling identifies epithelial cell genes associated with asthma and with treatment response to corticosteroids. Proc Natl Acad Sci USA 2007; 104: 15858–15863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Edlmayr J, Niespodziana K, Linhart B, et al. A combination vaccine for allergy and rhinovirus infections based on rhinovirus-derived surface protein VP1 and a nonallergenic peptide of the major timothy grass pollen allergen Phl p 1. J Immunol 2009; 182: 6298–6306. [DOI] [PubMed] [Google Scholar]
- 150.Senti G, Crameri R, Kuster D, et al. Intralymphatic immunotherapy for cat allergy induces tolerance after only 3 injections. J Allergy Clin Immunol 2012; 129: 1290–1296. [DOI] [PubMed] [Google Scholar]
- 151.Krishnan JA, Bender BG, Wamboldt FS, et al. Adherence to inhaled corticosteroids: an ancillary study of the Childhood Asthma Management Program clinical trial. J Allergy Clin Immunol 2012; 129: 112–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Klok T, Brand PL, Bomhof-Roordink H, et al. Parental illness perceptions and medication perceptions in childhood asthma, a focus group study. Acta Paediatr 2011; 100: 248–252. [DOI] [PubMed] [Google Scholar]
- 153.Caudri D, Wijga AH, Smit HA, et al. Asthma symptoms and medication in the PIAMA birth cohort: evidence for under and overtreatment. Pediatr Allergy Immunol 2011; 22: 652–659. [DOI] [PubMed] [Google Scholar]
- 154.Mackay D, Haw S, Ayres JG, et al. Smoke-free legislation and hospitalizations for childhood asthma. N Engl J Med 2010; 363: 1139–1145. [DOI] [PubMed] [Google Scholar]
- 155.Renzetti G, Silvestre G, D'Amario C, et al. Less air pollution leads to rapid reduction of airway inflammation and improved airway function in asthmatic children. Pediatrics 2009; 123: 1051–1058. [DOI] [PubMed] [Google Scholar]