Abstract
Patients with suspected pulmonary hypertension (PH) should be evaluated using a multimodality approach to ensure that they receive a correct diagnosis. The series of investigations required includes clinical evaluation, noninvasive imaging techniques and right heart catheterisation (considered to be the “gold standard” for the diagnosis of PH). Current guidelines recommend that a detailed echocardiographic assessment is performed in all patients with suspected PH.
In this review we summarise a protocol adopted by the National Pulmonary Hypertension Centres of UK and Ireland and approved by the British Society of Echocardiography for the evaluation of these patients. The views and measurements described are recommended for diagnosis, assisting in prognosis and providing a noninvasive means of following disease progression or response to therapy.
Keywords: Diagnosis, echocardiography, prognosis, pulmonary hypertension, right ventricle
Pulmonary hypertension (PH) is defined as a haemodynamic and pathophysiological condition characterised by an increase in mean pulmonary arterial pressure (Ppa) to ≥25 mmHg at rest as measured by right heart catheterisation (RHC) [1]. PH may be associated with a number of conditions displaying a range of different pathological and clinical features, despite the comparable elevations in Ppa. The clinical classification of PH aims to group together different manifestations of the disease that share similar clinical presentations and underlying pathophysiology [2], although the natural history may vary widely. In the most recent clinical classification, PH is classified into five groups. Group 1 is pulmonary arterial hypertension (PAH), which can be hereditary, idiopathic or associated with a number of underlying conditions. Group 2 includes PH due to left heart disease. Group 3 includes PH resulting from lung disease and/or hypoxaemia (e.g. interstitial lung disease and chronic obstructive pulmonary disease (COPD)). Group 4 is chronic thromboembolic PH and group 5 is made up of PH with unclear and/or multifactorial mechanisms [2]. Accurate diagnosis and classification of PH is essential as the prognostic and therapeutic implications are different between the clinical groups [1].
Patients with suspected PH must be evaluated using a multimodality approach to ensure a correct diagnosis, with a series of investigations ranging from thorough clinical evaluation through noninvasive imaging techniques to RHC, which is considered to be the “gold standard” for the diagnosis of PH [1]. Guidelines recommend that a detailed echocardiographic assessment is performed in all patients with suspected PH [1]. Transthoracic echocardiography provides a number of measures that can be used to estimate right heart haemodynamics. For example, systolic Ppa calculated from the tricuspid regurgitant velocity (TRV) is used to alert suspicion of PH, although Ppa may be underestimated by echocardiography due to an insufficient Doppler envelope or eccentric tricuspid regurgitation jet. In fact, no single echocardiographic measure is able to diagnose PH specifically and isolated abnormalities on echocardiography require cautious interpretation. Therefore, it is important that other surrogate echocardiographic measurements of PH are examined by echocardiography if PH is suspected. Further assessment of right ventricular function should be considered when one or more of these abnormalities are identified.
We have developed a protocol to describe how various echocardiographic views and measurements may be used during the initial examination and follow-up of PH. These techniques can be used to assess the severity of right ventricle (RV) dysfunction by providing prognostic information and a noninvasive means of following disease progression or response to therapy. The protocol includes only those parameters in regular clinical use, and excludes more specialised parameters such as speckle tracking and three-dimensional imaging, of which there is less experience. The procedure described in the protocol has been used successfully in the UK for the past 3 yrs, is supported by the British Society of Echocardiography and has been approved by the National Pulmonary Hypertension Centres of UK and Ireland. The aim of the protocol is to provide guidance to those undertaking echocardiographic examinations of patients, and also those interpreting the results in a clinical context, including physicians from cardiological and non-cardiological backgrounds.
RV ANATOMY AND PATHOPHYSIOLOGY
A detailed explanation of the anatomy and pathophysiology of the RV is beyond the scope of this article and has been extensively described elsewhere [3–5]. A number of anatomical and physiological features of the RV and its response to PH are important when assessing it using echocardiography. Certain anatomical features in particular make it difficult to examine the RV in detail, especially when using two-dimensional (2D) echocardiography. In particular, identifying the borders of the RV can be difficult because of the heavily trabeculated myocardium, while the available image windows can be limited because of the retrosternal position [3].
In contrast to the left ventricle (LV) and the systemic circulation, the pulmonary vascular bed is a low-resistance system in healthy individuals [3]. The RV is more compliant than the LV and adapts better to volume loading than to pressure loading. The LV and RV do not function independently of one another as the mechanics of one ventricle will impact on the other (ventricular interdependence) and this process is mediated by the interventricular septum (IVS) [6]. Ventricular septal geometry and motion are largely determined by the difference in pressure across the ventricular septum. Under normal circumstances, the higher pressures in the LV cavity mean the IVS bows into the lower pressure RV cavity. In patients with PH, pressure in the RV increases causing the septum to flatten in systole as the pressures in both ventricles begin to converge. Eventually, when the RV becomes severely pressure loaded, the septum may even bulge into the LV cavity (fig. 1) [4]. These changes also impact on both LV systolic and diastolic function.
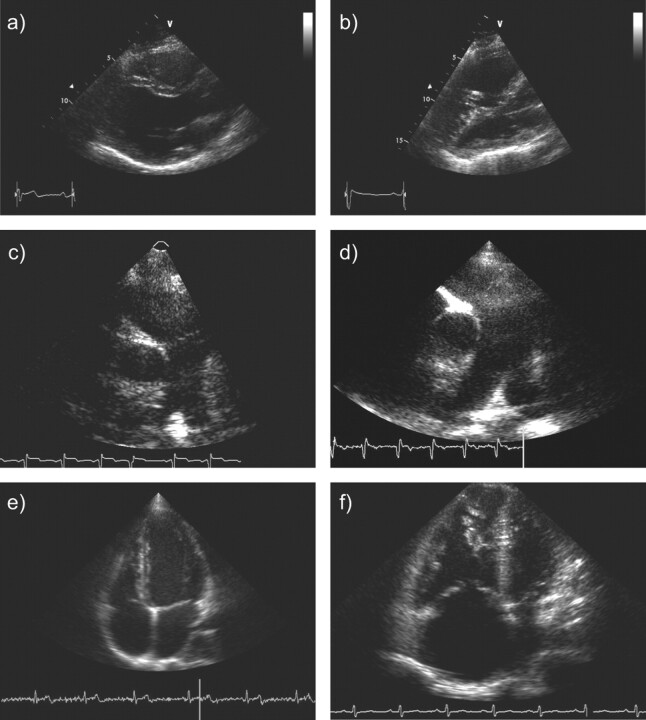
Figure 1.
a) Normal parasternal long-axis view. Note that the right ventricle is less than one third of the size of the left ventricle. b) Parasternal long-axis view in pulmonary hypertension (PH). Severely dilated right ventricle with hypertrophy of the moderator band and the right ventricular free wall. The left ventricular cavity is small due to chronic right ventricular pressure overload. c) Normal parasternal long-axis view of the right ventricular outflow tract (RVOT) showing the main pulmonary trunk, branches of the pulmonary artery and the pulmonary valve. d) Parasternal long-axis view of the RVOT in PH showing the dilated pulmonary artery and branches. e) Normal apical four-chamber view. f) Apical four-chamber view in PH showing marked right ventricular dilation and hypertrophy.
Another change seen in the RV in PH is ventricular remodelling, which is a result of chronic progressive pressure loading. This is initially in the form of hypertrophy and later as dilation [5]. The remodelling results in progressive contractile impairment, low cardiac output and, eventually, RV failure. Right ventricular dilation also leads to tricuspid annular dilation and results in significant tricuspid regurgitation [4]. When this is coupled with decreased RV systolic dysfunction and increased afterload it will further reduce stroke volume into the pulmonary circulation and resultant reduced cardiac output. The additional volume loading as a consequence of tricuspid regurgitation will further impair RV diastolic function, increasing RV end-diastolic pressure and displacing the IVS. The progressive deterioration of RV function is a determinant of exercise capacity, symptoms and prognosis and, therefore, the assessment of RV function is a key component of the assessment of a patient with PH.
RIGHT HEART IMAGING PROTOCOL
The protocol includes the measurement of a range of parameters assessed from three windows (parasternal, apical and subcostal view), which is first described using Doppler examination and secondly using M-mode examination. The aim of the measures selected is to determine the pressure within, and the capacity and function of, the RV. The technical aspects of the echocardiographic assessment have been described previously [7] and are briefly summarised here. However, the aim of this review is to highlight how the findings from the echocardiographic assessment can be interpreted clinically.
Parasternal views
In normal subjects the anterior RV wall is thin; its mass is less than one sixth and its diameter less than one third of the LV. As previously discussed, chronic pressure loading of the RV in PH leads to dilation and hypertrophy of the RV; the parasternal views of the RV allow any such changes to be viewed and various parameters to be measured (table 1).
Table 1. Parameters affected by pulmonary hypertension (PH) that can be detected by right heart imaging.
| View | Measurements | Normal range | PH |
| Long-axis view of LV or short-axis view of aorta and left atrium | LV end-diastolic diameter cm | 4.2–5.9 in males and 3.9–5.3 in females [8–10] | ↓ |
| LV end-systolic diameter cm | 2.1–4.0 in males and 2.4 in females [8–10] | ↓ | |
| Long-axis view of the RV inflow tract | Basal diameter of RV cm | 3.7–5.4 [11] | ↑ |
| Tricuspid annulus cm | 1.3–2.8 [11, 12] | ↑ | |
| Tricuspid regurgitant velocity m·s−1 | <2.6 [13] | ↑ | |
| Long- and short-axis views of RVOT or short-axis view of aorta and left atrium | RVOT cm | 1.7–2.3 [8, 11] | ↑ |
| Main pulmonary trunk cm | 1.5–2.1 [8, 11] | ↑ | |
| Right pulmonary artery cm | 0.7–1.7 [11, 14] | ↑ | |
| Left pulmonary artery cm | 0.6–1.4 [8, 11] | ↑ | |
| RV outflow acceleration time ms | >110 [8, 15, 16] | ↓ | |
| Pulmonary regurgitant velocity (beginning of diastole) m·s−1 | <1 [14, 17] | ↑ | |
| Pulmonary regurgitant velocity (end diastole) m·s−1 | <1 [14, 17] | ↑ | |
| Apical four-chamber view# | Basal diameter of RV cm | 2.0–2.8 [8, 11] | ↑ |
| RV end-diastolic area cm2 | 11–28 [8, 11] | ↑ | |
| RV end-systolic area cm2 | 7.5–16 [8, 11, 18] | ↑ | |
| Right atrial area (end-systole) cm2 | 13.5±2 cm [18] | ↑ | |
| RA volume index mL·m−2 | ≤34 in males and ≤27 in females [8, 19, 20] | ↑ | |
| Tricuspid annulus cm | 1.3–2.8 [8, 12] | ↑ | |
| Right ventricular fractional area change % | 32–60 [8, 21, 22] | ↓ | |
| Apical four-chamber view¶ | Tricuspid regurgitant velocity m·s−1 | <2.6 [13] | ↑ |
| Deceleration time–tricuspid inflow ms | 144–244 [23, 24] | ↑ | |
| RV MPI (Tei index) | <0.28 [8, 25, 26, 27] | ↑ | |
| TAPSE mm | ≥20 [8, 28–30] | ↓ | |
| IVRT (TDI RV free wall) ms | <75 [6, 8, 31, 32] | ↑ |
LV: left ventricle; RV: right ventricle; RVOT: right ventricular outflow tract; RA: right atrium; MPI: myocardial performance index; TAPSE: tricuspid annular plane systolic excursion; IVRT: isovolumic relaxation time; TDI: tissue Doppler imaging; ↓: decreased in PH; ↑: increased in PH. #: two-dimensional echocardiograph; ¶: Doppler echocardiograph.
In the parasternal long-axis view, the moderator band is usually seen close to the IVS traversing the RV and care should be taken not to include the moderator band in the measurements of the IVS. In significant PH, the LV cavity may be reduced in size in both systole and diastole, with deviation (bowing) of the septum towards the LV (fig. 1a and b).
The long-axis view of the RV inflow tract may also allow for optimal alignment for estimation of TRV when the tricuspid regurgitant jet is eccentric. Abnormalities of the leaflets and subvalvular apparatus should also be assessed to exclude primary valvular pathology. In addition, this view may be used to provide a qualitative estimate of RV systolic function.
The long- and short-axis views of the right ventricular outflow tract (RVOT) are useful for the assessment of the main pulmonary artery, which is dilated in relation to the adjacent aorta in PH, and pulmonary regurgitation (fig. 1c and d). However, we are not aware of any data to suggest that dilation of the pulmonary artery is a sensitive measurement for detection of PH using echocardiography.
As well as demonstrating the atria and RV, the short-axis view of the aorta and left atrium shows the aortic, tricuspid and pulmonary valves simultaneously, making this a useful view for the assessment of structural valvular abnormalities. It can also help to identify an atrial septal defect using a zoom view of the interatrial septum with colour Doppler imaging. RV dilation and hypertrophy, as well as dilation of the pulmonary artery, can also be seen in this view. Finally, the degree of distortion of the LV and IVS arising due to increased pressure in the RV during diastole and systole (LV eccentricity index) can be quantified using a short-axis view at the level of left ventricular papillary muscles. While in a normal situation the LV appears circular in shape, in systole and diastole dilation of the RV and increased RV pressure in severe PH shifts the IVS to the left, giving the LV a characteristic D-shape. Consequently, a RV that is dilated purely due to volume overload will deviate the septum, mainly in diastole, due to raised end-diastolic pressure and, conversely, a pressure-loaded RV will deviate the septum in systole. When pressure overload is severe the septum may even be deviated into the LV cavity itself.
Apical four-chamber views
A number of parameters influenced by the presence of PH can be assessed in this view (table 1), including RV dilation and hypertrophy, with systolic dysfunction and reduced myocardial tissue velocities being quantifiable by tissue Doppler imaging. In PH, the apex is frequently hypertrophied and akinetic, and careful examination of the apex should be performed to exclude thrombus or an apical mass [7]. Diastolic opening of the tricuspid leaflets, which can also be assessed in this view, becomes less vigorous as PH progresses. The tricuspid valve leaflet adjacent to the free wall may be either the anterior (most commonly) or posterior leaflet, depending on the exact rotation and angulation of the image plane. Tricuspid leaflets are uniformly echogenic, with normal coaptation in systole. When significant tricuspid regurgitation develops in PH, careful identification of any structural abnormalities is needed to ensure primary tricuspid incompetence is differentiated from secondary incompetence due to the annular dilation.
The interatrial and interventricular septums can be clearly delineated (fig. 1e and f). Drop-out artefact is commonly seen in the region of fossa ovalis and this should not be mistaken for an atrial septal defect. The use of tissue Doppler imaging to the septal and lateral LV walls may help to identify significant LV diastolic dysfunction (table 2).
Table 2. Effect of pulmonary hypertension (PH) on measurements from tissue Doppler imaging.
| Measurements | [Ref.] | Normal S' wave cm·s−1 | PH | Normal E' cm·s−1 | PH | Normal A' cm·s−1 | PH |
| RV free (lateral) wall | [33–35] | 12–20 | ↓ | 10.2–16.2 | ↓ | 6.2–10.9 | ↓ |
| LV septal wall | [34] | 8.1–10.9 | ↔ | 9.8–16.0 | ↔ | 9.0–13.2 | ↔ |
| LV lateral wall | [34] | 9.1–12.9 | ↔ | 12.5–20.5 | ↔ | 8.6–14.4 | ↔ |
S': systolic wave; A': late (atrial systole) myocardial diastolic wave; E': early myocardial diastolic wave; RV: right ventricle; LV: left ventricle; ↓: decreased in PH; ↔: no change.
Subcostal view
The subcostal view allows the degree of RV dysfunction and the thickness of the RV walls to be estimated. This assessment is particularly useful in patients where parasternal or apical window views are difficult to image, such as those with COPD. It provides the best view for the measurement of RV inferior wall thickness and determines the presence of an atrial septal defect. The diameter of the inferior vena cava measured at rest and during inspiration in this view can be used to provide an estimate of right atrial pressure (Pra).
Doppler examination
As part of a full echocardiographic assessment, Doppler examination should be performed in the following sequence: 1) colour Doppler in all apical projections; 2) colour Doppler in parasternal projections (long axis/short axis); 3) pulsed-wave Doppler for transmitral velocities; 4) pulsed-wave Doppler for LV outflow tract; 5) pulsed-wave Doppler for the tricuspid inflow; 6) pulsed-wave Doppler for the RVOT; 7) continuous-wave Doppler across the LV outflow aortic valve; 8) continuous-wave Doppler across the tricuspid valve (for tricuspid regurgitation); 9) continuous-wave Doppler across the pulmonary valve (for pulmonary regurgitation); and 10) tissue Doppler imaging (TDI) of the RV free wall.
QUALITATIVE ASSESSMENT OF THE RV
Dilation of the RV can be assessed in the parasternal long-axis, short-axis and the apical four-chamber views. When RV afterload becomes chronically elevated, the RV walls become hypertrophied. RV hypertrophy is defined by a free wall thickness of >5 mm on the apical four-chamber view. One of the first anatomical elements to become hypertrophied is the moderator band. In normal subjects this is thin and difficult to see, but in patients with PH it is clearly visible. In contrast to other conditions affecting the RV (e.g. RV infarction or arrhythmogenic RV cardiomyopathy) where there will be regional wall motion abnormalities, contractility assessment in PH shows global RV impairment. On the basis of these three parameters (dilation, hypertrophy and contractility), an experienced echocardiographer will be able to make a good qualitative assessment of RV function and will be able to grade it as mild, moderate or severe impairment. In patients with PAH, dilation of the RV has been shown to be linked to adverse clinical outcome (increase of >0.25 in absolute value of RV sphericity index; i.e. ratio of the short axis at the mid-ventricular level of the RV divided by the RV long axis in end-diastole [36]) and mortality (RV diameter >36.5 mm) [37].
PRESSURE MEASUREMENTS IN PH
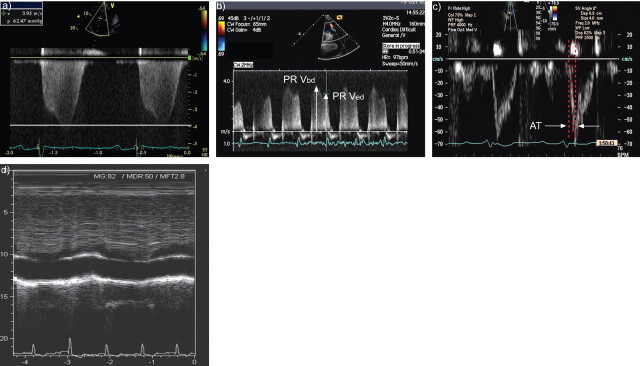
Pra can be estimated by measurement of the diameter of the inferior vena cava at end-expiration and during sharp inspiration using M-mode in the subcostal view (fig. 2d). High Pra is associated with dilation of the vena cava (normal range 1.5–2.5 cm) and/or failure of the segment adjacent to the right atrium to collapse by at least 50% with inspiration (table 3). Inferior vena cava diameter ≥20 mm with respiratory variation of diameter <50% has been shown to be significantly associated with mortality in patients with PAH [38].
Figure 2.
a) Measurement of the peak tricuspid regurgitant velocity. b) Pulmonary regurgitant velocity at the start of diastole (PRVbd) and end-diastole (PRVed). c) Acceleration time (AT) measured across the pulmonary outflow tract in the parasternal short-axis view. d) Right atrial pressure: M-mode during sniff manoeuvre.
Table 3. Estimation of right atrial pressure from the inferior vena cava [8].
| Inferior vena cava diameter | Change with respiration | Estimated right atrial pressure mmHg |
| Small <1.5 cm | Collapse | 0 |
| Normal 1.5–2.5 cm | Decrease by >50% | 5 |
| Normal | Decrease by <50% | 10 |
| Dilated >2.5 cm | Decrease by <50% | 15 |
| Dilated with dilated hepatic veins | No change | 20 |
TRV reflects the difference in pressure between the RV and the right atrium and can be measured from continuous wave Doppler of the tricuspid regurgitant jet from the apical four-chamber view, or from the parasternal RV inflow view if the regurgitant jet is eccentric (fig. 2a). When pulmonary stenosis is absent, the RV systolic pressure (RVSP) is assumed to be equivalent to the systolic Ppa and can be calculated from the TRV using the Bernoulli equation, using estimated Pra from inferior vena cava diameter (table 3) [7].
where TRVend is peak TRV at end diastole. The ability to estimate systolic Ppa represents a considerable strength of echocardiography in its role as a diagnostic tool, but with this comes limitations and there is a danger that too much weight is placed on this single measurement. Fisher et al. [39] have shown that, despite good correlation between measurements, almost 50% of patients had an estimated systolic Ppa on echocardiography that was ≥10 mmHg different from the value measured at cardiac catheterisation. Underestimation of systolic Ppa has led to frequent misclassification of PH severity or even failure to identify PH [39]. The most common causes of inaccurate estimation of systolic Ppa were an incomplete Doppler envelope resulting in underestimation of pressure or an overestimate of Pra from inferior vena cava diameter and collapsibility. With severe free-flow tricuspid regurgitation, the Bernoulli equation cannot be applied and TRV will underestimate the trans-tricuspid pressure difference. In itself, the severity of the tricuspid regurgitation is predictive of survival regardless of the systolic Ppa and irrespective of the underlying disease [37, 40]. Tricuspid regurgitation may be assessed in a number of ways, including assessment of the structure of the valve, jet area and density or measurement using continuous wave Doppler [41]. It should be emphasised that the severity of the volume of tricuspid regurgitation is distinct from the velocity. Thus, Doppler-derived estimates of RVSP/systolic Ppa must only be considered to be estimates [1, 39, 42] and cannot be used to diagnose PH. For this reason, it is often valuable to consider other surrogates for Ppa.
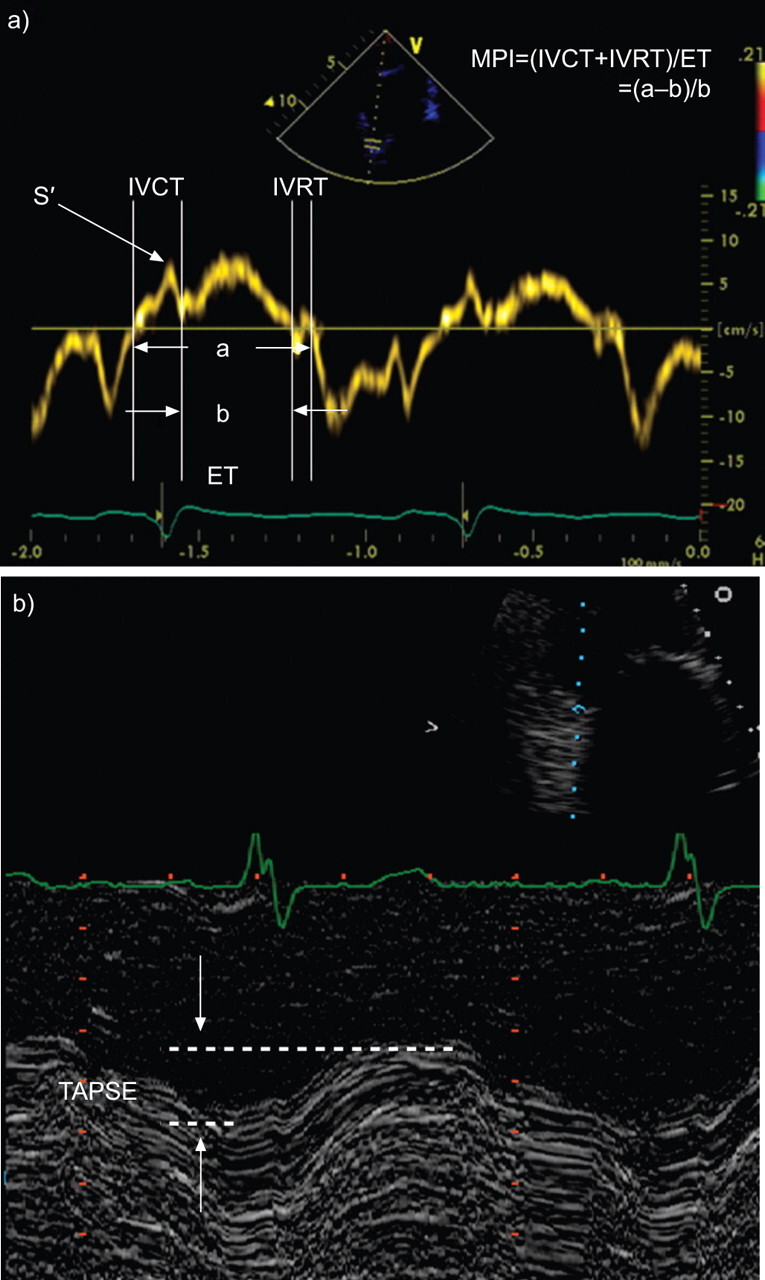
Mean Ppa and pulmonary end-diastolic pressure are not routinely used in the diagnosis or follow-up of PH, but may be useful when TRV cannot be used or is unreliable. In 2D-echocardiography, the pulmonary valve is best imaged from the parasternal short-axis at the level of the aortic valve (fig. 1c and 1d]). Pulmonary valvular motion can be determined with M-mode echocardiography and may show mid-diastolic closure. Mean Ppa and pulmonary end-diastolic pressure can be derived from the TRV at the beginning (PRVbd) and end (PRVed) of diastole, respectively (fig. 2b).
 |
RVOT acceleration time has been superseded by TRV in clinical practice, although it may be used when the tricuspid velocity cannot be measured, particularly at diagnosis. A value <105 ms is suggestive of PH. By positioning the sample volume at the centre of the pulmonary artery (ideally at the annulus) in the short-axis view, acceleration time can be measured in the parasternal short-axis view (fig. 2c). Unlike most other indices of function, which are unaffected by heart rate, RVOT acceleration time should be corrected when the heart rate is >100 bpm or <70 bpm. This is achieved by multiplying the measurement by 75 and dividing by heart rate. Notching of the flow velocity envelope may also be seen in PH. A notch seen in mid-systole is associated with severe PH and RV dysfunction [43]. Normal pressures and those in PH obtained by echocardiography are shown in table 4.
Table 4. Right ventricular pressure, cavity and functional measurements that may indicate pulmonary hypertension.
| Parameter | [Ref.] | Normal | Intermediate | Abnormal |
| Pra mmHg | [8] | <5 | 5–10 | >10 |
| TRV m·s−1 | [13] | <2.6 | ≥2.6 ≥2.8 in obese subjects ≥2.9 in patients >60 yrs |
|
| RVSP mmHg | [13] | <37 | ≥37 ≥40 in obese subjects ≥44 in patients >60 yrs |
|
| RVOT acceleration time ms | [8, 15, 16] | >110 | 105–110 | <105 |
| RA volume index mL·m−2 | [8] | ≤34 in males and ≤27 in females | >34 in males >27 in females |
|
| RV fractional area change % | [8, 21, 22] | 32–60 | ≤32 | |
| LV eccentricity index | [8, 44, 45] | 1 | >1 at end-diastole indicates volume loading of the RV >1 at end-systole indicates pressure loading of the RV |
|
| RV MPI (Tei index) | [8, 25–27] | <0.28 | 0.28–0.32 | >0.32 |
| S' wave of tricuspid annulus cm·s−1 | [33, 35] | >12 | 11.5–12 | <11.5 |
| IVRT s | [6, 8, 31, 32] | <75 | ≥75 | |
| TAPSE ms | [8, 28–30] | ≥20 | 16–20 | <16 |
| Estimated PVR Wood units | [46, 47] | <1 | 1–3 | >3 |
Pra: right atrial pressure; TRV: tricuspid regurgitant velocity; RVSP: right ventricular systolic pressure; RVOT: right ventricular outflow tract; RA: right atrium; RV: right ventricle; LV: left ventricle; MPI: myocardial performance index; S' wave: systolic wave; IVRT: isovolumic relaxation time; TAPSE: tricuspid annular plane systolic exertion; PVR: pulmonary vascular resistance.
CARDIAC CHAMBER CAVITY MEASUREMENTS IN PH
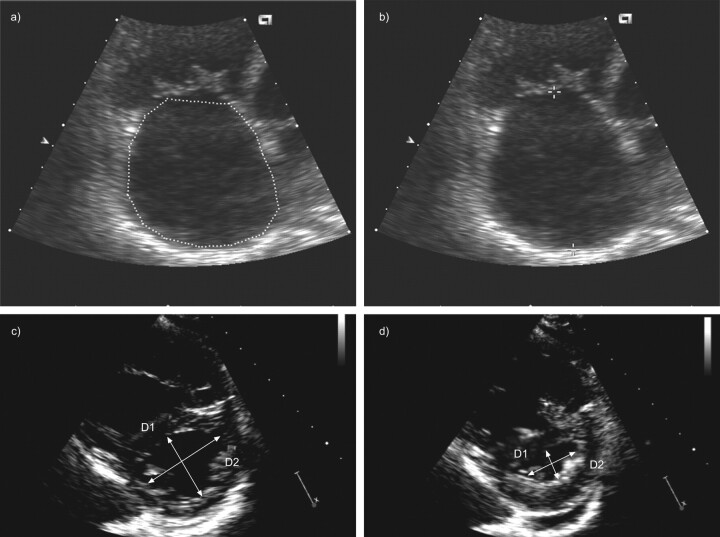
Right atrial volume index is calculated from the apical four-chamber view or from the subcostal view, and is measured at maximum atrial volume at end-systole. The single plane area–length method is used and right atrium volume is measured using the area and the long-axis length of the atrium (fig. 3a and b) [8, 19, 20].
Figure 3.
a) Measurement of the right atrial a) area and b) long axis for calculation of right atrial volume. c) Measurement of the left ventricular eccentricity index in c) end-diastole and d) end-systole. DI: minor axis perpendicular to the septum; D2: minor axis of the left ventricle parallel to the septum.
where A is the atrium area in any view (cm2), L is the long-axis atrium length (cm) and BSA is body surface area.
In a recent three-dimensional echocardiography study, while both right atrium and RV remodelling were found to be significantly associated with adverse clinical outcome, sensitivity and specificity were highest for right atrium remodelling [36]. An increase of right atrium sphericity index (ratio of the short axis of the right atrium, parallel to the tricuspid annulus, mid-cavity, divided by the long axis, perpendicular to the tricuspid annulus, in end systole) >0.24 predicted clinical deterioration with a sensitivity of 96% and a specificity of 90% [36].
RV fractional area change is calculated from end-diastolic area and end-systolic area, measured from the apical four-chamber view. It is a simple method for the assessment of RV systolic function and has been shown to correlate with prognosis and response to treatment in PH [48], and with survival [37]. However, it is limited by difficulties in endocardial definition.
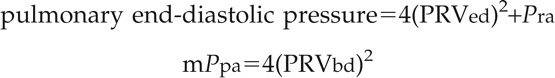
 |
LV eccentricity index is the ratio of the minor axis of the LV parallel to the septum (D2) divided by the minor axis perpendicular to the septum (D1) and is measured in the parasternal short-axis view at the level of the LV papillary muscles (fig. 3c and d) in both end diastole and end systole. In a purely pressure-loaded RV, flattening of the IVS occurs in end systole, resulting in an increased end-systolic LV eccentricity index. Conversely, the eccentricity index will be increased in end diastole in pure volume loading [8, 44, 45]. LV diastolic eccentricity index in diastole ≥1.7 has been shown to be prognostic of mortality in patients with idiopathic PAH who also have reduced RV function (tricuspid annular plane systolic exertion (TAPSE) ≤15 mm) [37]. Normal cavity measurements and those in PH as obtained by echocardiography are shown in table 4].
MEASURES OF FUNCTION IN PH
Myocardial performance index of the RV, also known as the Tei index [49], is made up of a combination of systolic and diastolic measurements. It has a number of advantages as a functional measure, including: 1) being relatively unaffected by heart rate, loading conditions or the presence and severity of tricuspid regurgitation; 2) having good reproducibility; 3) being quick to calculate; 4) not relying on the use of geometric models; and 5) being able to be applied even in the presence of a difficult acoustic window.
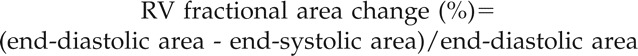
The Tei index can be measured either from colour Doppler imaging (apical four-chamber view for the tricuspid inflow pattern and the parasternal short-axis RVOT view for the determination of ejection time) or tissue Doppler imaging (fig. 4a). The Tei index should be indexed for heart rate, as described previously for RVOT acceleration time. In patients with idiopathic PAH the index correlates with symptoms and values >0.88 predict poor survival [25].
Figure 4.
a) Measurement of myocardial performance index (MPI) using tissue Doppler imaging. S’: systolic wave; IVCT: isovolumic contraction time; IVRT: isovolumic relaxation time. b) Measurement of tricuspid annular plane systolic excursion (TAPSE); ET: ejections time.
Systolic (S') wave velocity is a measure of myocardial contraction and may be determined from the average of three TDI signals from different cardiac cycles (fig. 4a). Like TAPSE, S' wave velocity is load dependent and may be pseudonormal under conditions of increased volume loading (this is discussed in more detail below). Unlike most indices of function, S' wave velocity requires correction when heart rate is >100 bpm or falls to <70 bpm. Therefore, S' wave velocity should be indexed for heart rate, as described previously for RVOT acceleration time. Normal values and those in PH obtained by echocardiography are shown in table 4].
Isovolumic relaxation time (IVRT) of the RV is defined as the time from pulmonary valve closure to tricuspid valve opening and can be measured either by pulsed-wave Doppler from tricuspid inflow or with tissue Doppler imaging of the RV free wall. Prolongation of IVRT indicates poor myocardial relaxation, which is highly suggestive of PH, although it does not provide prognostic value (fig. 4a). IVRT should be indexed for heart rate as described previously for RVOT acceleration time.
TAPSE is the reflection of the movement of base to apex shortening of the RV in systole and can be derived from the four-chamber view (fig. 4b). When measuring TAPSE, it is important to ensure that the entire RV is included in the view, in particular that there is no dropout in the endocardial outline along the IVS and RV free wall. Maximal TAPSE is defined by the total excursion of the tricuspid annulus from its highest position after atrial ascent to the peak descent during ventricular systole [29]. A TAPSE of <15 mm is associated with a significantly higher risk of mortality compared with a TAPSE of >15 mm [37] and TAPSE is recommended by treatment guidelines as a prognostic indicator in PAH for the assessment of disease severity and response to therapy [1]. A significant limitation of TAPSE is that it is highly load dependent, such that it may become pseudonormalised in the presence of significant volume loading, e.g. left-to-right shunting or severe functional tricuspid regurgitation [37]. Given that so much weight is placed on this particular measure of function in the treatment guidelines, it is important that this caveat is taken into account when interpreting TAPSE.
Stroke volume, cardiac output and pulmonary vascular resistance can be calculated from echocardiographic measurements. These parameters correlate with right and left heart function and the underlying pulmonary vascular resistance, but are not considered to be mandatory measures in PH. Normal values and those in PH obtained by echocardiography are shown in table 4].
CAUSES OF PH
Once PH has been suspected, further evaluation should be undertaken to establish any potential underlying cause. This includes assessment for congenital heart disease, valvular heart disease and left heart disease. These assessments are out of the scope of this protocol, but as the most frequent cause of PH will relate to impaired LV function, it is imperative to highlight that a detailed assessment of diastolic LV function is undertaken. In our experience this is something that is often overlooked. This should include measurement of left atrial diameter and volume (indexed for body surface area), LV hypertrophy, transmitral inflow patterns, tissue Doppler imaging of the basal lateral wall of the LV and, in some cases, pulmonary venous flow. Of note, type I diastolic dysfunction of the LV is common in pre-capillary PH and should not be considered as indicative of pulmonary venous hypertension as the cause of PH. This has been reviewed comprehensively elsewhere, with a proposed scoring system for differentiating between pulmonary venous hypertension and PAH [50].
NEW TECHNIQUES
We have presented a core clinical dataset for PH echocardiography. Outside this dataset other techniques can be applied, but these do not form part of routine investigation either as a result of complexity or because of lack of clinical validation. Exercise echocardiography has been proposed for early detection of subclinical PH, e.g. in relatives of patients with idiopathic PAH [51], but as yet no clear clinical cut-off values have been accepted. Strain and strain rate examine the deformation and rate of deformation, respectively, of the myocardial segment and, in PH, RV systolic strain and strain rate has been shown to predict morbidity and mortality [52], but at present is still considered outside the standard echocardiography protocol.
ECHOCARDIOGRAPHY REPORTING
All echocardiographic reports should include measurements, descriptions of all valves, the proximal great arteries, the heart chambers, the pericardium and Doppler findings. Where PH is the reason for the referral, the emphasis should be put on pulmonary pressures, right heart chamber size and function and any finding that may indicate a secondary cause (e.g. LV dysfunction, left heart valve disease or congenital heart disease). Where PH is confirmed, the report should also include the various parameters that provide prognostic information (e.g. right atrial volume index, inferior vena cava diameter, eccentricity index, presence of pericardial effusion and TAPSE). It is important that the reporter does not judge severity of PAH on the basis of estimated Ppa. Instead, conclusions should be drawn on the severity of RV impairment. An example report is shown in figure S1 (online supplementary data).
These criteria should be taken as guides, not rules, and have been selected by consensus: it is important not to place too much emphasis on a single value, or consider them as precise thresholds for the diagnosis of PH. It may be necessary to undertake catheterisation when clinical suspicion is high, since echocardiography may sometimes be normal even in the presence of PH. For example, in patients with a high pre-test probability of PH with unexplained breathlessness (such as those with scleroderma), as pressure can only be estimated by echocardiography, the final diagnosis of PH can only be made by cardiac catheterisation.
CONCLUSIONS
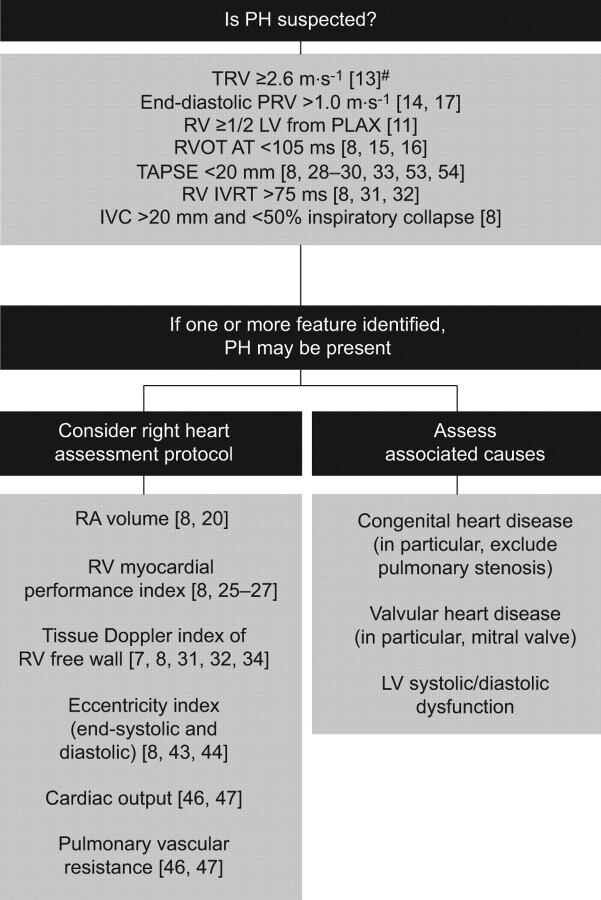
Detailed echocardiographic assessment of patients with PH allows useful diagnostic information to be collected. It can also be used to assess severity of right ventricular dysfunction, providing prognostic information and a noninvasive means of following disease progression or response to therapy. A suggested algorithm for investigating PH using transthoracic echocardiography is shown in figure 5.
Figure 5.
An algorithm for investigating pulmonary hypertension (PH) using echocardiography. TRV: tricuspid regurgitant velocity; PRV: pulmonary regurgitant velocity; RV: right ventricle; LV left ventricle; PLAX: parasternal long axis; RVOT: right ventricular outflow tract; AT: acceleration time; TAPSE: tricuspid annular plane systolic excursion; IVRT: isovolumic relaxation time; IVC: inferior vena cava; RA: right atrium. #: in patients >60 yrs of age, a TRV ≥2.9 m·s−1 is used as a cut-off value [13].
Supplementary Material
Acknowledgments
We thank A. Kenny for her comments on the standard operating procedure. Medical writing support was provided by L. Quine (Elements Communications Ltd, Westerham, UK) and funded by Actelion (Chiswick, UK).
Footnotes
This article has supplementary data available from http://err.ersjournals.com
Statement of Interest
P. Nihoyannopoulos has received research and educational grants from General Electric and from BRACCO Pharmaceuticals for organising educational meetings. He has also received fees (less than £1,000) for consulting from General Electric.
Provenance
Publication of this peer-reviewed article was supported Actelion Pharmaceuticals Ltd, Switzerland (article sponsor, European Respiratory Review issue 125).
REFERENCES
- 1.Galiè N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2009; 34: 1219–1263. [DOI] [PubMed] [Google Scholar]
- 2.Simonneau G, Robbins IM, Beghetti M, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2009; 54: Suppl. 1, S43–S54. [DOI] [PubMed] [Google Scholar]
- 3.Haddad F, Couture P, Tousignant C, et al. The right ventricle in cardiac surgery, a perioperative perspective: I. Anatomy, physiology, and assessment. Anesth Analg 2009; 108: 407–421. [DOI] [PubMed] [Google Scholar]
- 4.Haddad F, Couture P, Tousignant C, et al. The right ventricle in cardiac surgery, a perioperative perspective: II. Pathophysiology, clinical importance, and management. Anesth Analg 2009; 108: 422–433. [DOI] [PubMed] [Google Scholar]
- 5.Bogaard HJ, Abe K, Vonk Noordegraaf A, et al. The right ventricle under pressure: cellular and molecular mechanisms of right-heart failure in pulmonary hypertension. Chest 2009; 135: 794–804. [DOI] [PubMed] [Google Scholar]
- 6.Santamore WP, Dell'Italia LJ. Ventricular interdependence: significant left ventricular contributions to right ventricular systolic function. Prog Cardiovasc Dis 1998; 40: 289–308. [DOI] [PubMed] [Google Scholar]
- 7.Grapsa J, Dawson D, Nihoyannopoulos P. Assessment of right ventricular structure and function in pulmonary hypertension. J Cardiovasc Ultrasound 2011; 19: 115–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463. [DOI] [PubMed] [Google Scholar]
- 9.Ilercil A, O'Grady MJ, Roman MJ, et al. Reference values for echocardiographic measurements in urban and rural populations of differing ethnicity: the Strong Heart Study. J Am Soc Echocardiogr 2001; 14: 601–611. [DOI] [PubMed] [Google Scholar]
- 10.Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989; 2: 358–367. [DOI] [PubMed] [Google Scholar]
- 11.Foale R, Nihoyannopoulos P, McKenna W, et al. Echocardiographic measurement of the normal adult right ventricle. Br Heart J 1986; 56: 33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kitzman DW, Scholz DG, Hagen PT, et al. Age-related changes in normal human hearts during the first 10 decades of life. Part II (Maturity): a quantitative anatomic study of 765 specimens from subjects 20 to 99 years old. Mayo Clin Proc 1988; 63: 137–146. [DOI] [PubMed] [Google Scholar]
- 13.McQuillan BM, Picard MH, Leavitt M, et al. Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation 2001; 104: 2797–2802. [DOI] [PubMed] [Google Scholar]
- 14.Yoshida K, Yoshikawa J, Shakudo M, et al. Color Doppler evaluation of valvular regurgitation in normal subjects. Circulation 1988; 78: 840–847. [DOI] [PubMed] [Google Scholar]
- 15.Kitabatake A, Inoue M, Asao M, et al. Noninvasive evaluation of pulmonary hypertension by a pulsed Doppler technique. Circulation 1983; 68: 302–309. [DOI] [PubMed] [Google Scholar]
- 16.Maeba H, Nakatani S, Sugawara M, et al. Different time course of changes in tricuspid regurgitant pressure gradient and pulmonary artery flow acceleration after pulmonary thromboendarterectomy: implications for discordant recovery of pulmonary artery pressure and compliance. Circ J 2007; 71: 1771–1775. [DOI] [PubMed] [Google Scholar]
- 17.Vahanian A, Baumgartner H, Bax J, et al. Guidelines on the management of valvular heart disease: The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J 2007; 28: 230–268. [DOI] [PubMed] [Google Scholar]
- 18.Triulizi M, Gillam LD, Gentile F, et al. Normal adult cross-sectional echocardiographic values: linear dimensions and chamber areas echocardiography. Echocardiography 1984; 1: 403–426. [Google Scholar]
- 19.Schnittger I, Gordon EP, Fitzgerald PJ, et al. Standardized intracardiac measurements of two-dimensional echocardiography. J Am Coll Cardiol 1983; 2: 934–938. [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Gutman JM, Heilbron D, et al. Atrial volume in a normal adult population by two-dimensional echocardiography. Chest 1984; 86: 595–601. [DOI] [PubMed] [Google Scholar]
- 21.Anavekar NS, Skali H, Bourgoun M, et al. Usefulness of right ventricular fractional area change to predict death, heart failure, and stroke following myocardial infarction (from the VALIANT ECHO Study). Am J Cardiol 2008; 101: 607–612. [DOI] [PubMed] [Google Scholar]
- 22.Wang J, Prakasa K, Bomma C, et al. Comparison of novel echocardiographic parameters of right ventricular function with ejection fraction by cardiac magnetic resonance. J Am Soc Echocardiogr 2007; 29: 1058–1064. [DOI] [PubMed] [Google Scholar]
- 23.Appleton CP, Firstenberg MS, Garcia MJ, et al. The echo-Doppler evaluation of left ventricular diastolic function. A current perspective. Cardiol Clin 2000; 18: 513–546. [DOI] [PubMed] [Google Scholar]
- 24.Hatle L, Angelsen B. Doppler Ultrasound in Cardiology. Physical Principles and Clinical Applications. 2nd Edn. Philadelphia, Lea & Febiger, 1985. [Google Scholar]
- 25.Tei C, Dujardin KS, Hodge DO, et al. Doppler echocardiographic index for assessment of global right ventricular function. J Am Soc Echocardiogr 1996; 9: 838–847. [DOI] [PubMed] [Google Scholar]
- 26.Dujardin KS, Tei C, Yeo TC, et al. Prognostic value of a Doppler index combining systolic and diastolic performance in idiopathic-dilated cardiomyopathy. Am J Cardiol 1998; 82: 1071–1076. [DOI] [PubMed] [Google Scholar]
- 27.Yeo TC, Dujardin KS, Tei C, et al. Value of a Doppler-derived index combining systolic and diastolic time intervals in predicting outcome in primary pulmonary hypertension. Am J Cardiol 1998; 81: 1157–1161. [DOI] [PubMed] [Google Scholar]
- 28.Forfia PR, Fisher MR, Mathai SC, et al. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med 2006; 174: 1034–1041. [DOI] [PubMed] [Google Scholar]
- 29.Kaul S, Tei C, Hopkins JM, et al. Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 1984; 107: 526–531. [DOI] [PubMed] [Google Scholar]
- 30.Lee CY, Chang SM, Hsiao SH, et al. Right heart function and scleroderma: insights from tricuspid annular plane systolic excursion. Echocardiography 2007; 24: 118–125. [DOI] [PubMed] [Google Scholar]
- 31.Abbas A, Lester S, Moreno FC, et al. Noninvasive assessment of right atrial pressure using Doppler tissue imaging. J Am Soc Echocardiogr 2004; 17: 1155–1160. [DOI] [PubMed] [Google Scholar]
- 32.Stein PD, Sabbah HN, Anbe DT, et al. Performance of the failing and nonfailing right ventricle of patients with pulmonary hypertension. Am J Cardiol 1979; 44: 1050–1055. [DOI] [PubMed] [Google Scholar]
- 33.Olson JM, Samad BA, Alam M. Prognostic value of pulse-wave tissue Doppler parameters in patients with systolic heart failure. Am J Cardiol 2008; 102: 722–725. [DOI] [PubMed] [Google Scholar]
- 34.Alam M, Wardell J, Andersson E, et al. Characteristics of mitral and tricuspid annular velocities determined by pulsed wave Doppler tissue imaging in healthy subjects. J Am Soc Echocardiogr 1999; 12: 618–628. [DOI] [PubMed] [Google Scholar]
- 35.Meluzin J, Spinarova L, Bakala J, et al. Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion: a new rapid and non-invasive method of evaluating right ventricular systolic function. Eur Heart J 2001; 22: 340–348. [DOI] [PubMed] [Google Scholar]
- 36.Grapsa J, Gibbs JS, Cabrita IZ, et al. The association of clinical outcome with right atrial and ventricular remodelling in patients with pulmonary arterial hypertension: study with real-time three-dimensional echocardiography. Eur Heart J Cardiovasc Imaging 2012; [Epub ahead of print DOI: 10.1093/ehjci/jes003]. [DOI] [PubMed] [Google Scholar]
- 37.Ghio S, Klersy C, Magrini G, et al. Prognostic relevance of the echocardiographic assessment of right ventricular function in patients with idiopathic pulmonary arterial hypertension. Int J Cardiol 2010; 140: 272–278. [DOI] [PubMed] [Google Scholar]
- 38.Brierre G, Blot-Souletie N, Degano B, et al. New echocardiographic prognostic factors for mortality in pulmonary arterial hypertension. Eur J Echocardiogr 2010; 11: 516–522. [DOI] [PubMed] [Google Scholar]
- 39.Fisher MR, Forfia PR, Chamera E, et al. Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. Am J Respir Crit Care Med 2009; 179: 615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol 2004; 43: 405–409. [DOI] [PubMed] [Google Scholar]
- 41.Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003; 16: 777–802. [DOI] [PubMed] [Google Scholar]
- 42.Mukerjee D, St George D, Knight C, et al. Echocardiography and pulmonary function as screening tests for pulmonary arterial hypertension in systemic sclerosis. Rheumatology (Oxford) 2004; 43: 461–466. [DOI] [PubMed] [Google Scholar]
- 43.Arkles JS, Opotowsky AR, Ojeda J, et al. Shape of the right ventricular Doppler envelope predicts hemodynamics and right heart function in pulmonary hypertension. Am J Respir Crit Care Med 2011; 183: 268–276. [DOI] [PubMed] [Google Scholar]
- 44.Feneley M, Gavaghan T. Paradoxical and pseudoparadoxical interventricular septal motion in patients with right ventricular volume overload. Circulation 1986; 74: 230–238. [DOI] [PubMed] [Google Scholar]
- 45.Ryan T, Petrovic O, Dillon JC, et al. An echocardiographic index for separation of right ventricular volume and pressure overload. J Am Coll Cardiol 1985; 5: 918–927. [DOI] [PubMed] [Google Scholar]
- 46.Abbas AE, Fortuin FD, Schiller NB, et al. A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol 2003; 41: 1021–1027. [DOI] [PubMed] [Google Scholar]
- 47.Scapellato F, Temporelli PL, Eleuteri E, et al. Accurate noninvasive estimation of pulmonary vascular resistance by Doppler echocardiography in patients with chronic failure heart failure. J Am Coll Cardiol 2001; 37: 1813–1819. [DOI] [PubMed] [Google Scholar]
- 48.Galiè N, Hinderliter AL, Torbicki A, et al. Effects of the oral endothelin-receptor antagonist bosentan on echocardiographic and Doppler measures in patients with pulmonary arterial hypertension. J Am Coll Cardiol 2003; 41: 1380–1386. [DOI] [PubMed] [Google Scholar]
- 49.Tei C, Ling LH, Hodge DO, et al. New index of combined systolic and diastolic myocardial performance: a simple and reproducible measure of cardiac function – a study in normals and dilated cardiomyopathy. J Cardiol 1995; 26: 357–366. [PubMed] [Google Scholar]
- 50.Roberts JD, Forfia PR. Diagnosis and assessment of pulmonary vascular disease by Doppler echocardiography. Pulm Circ 2011; 1: 160–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Grünig E, Weissmann S, Ehlken N, et al. Stress Doppler echocardiography in relatives of patients with idiopathic and familial pulmonary arterial hypertension: results of a multicenter European analysis of pulmonary artery pressure response to exercise and hypoxia. Circulation 2009; 119: 1747–1757. [DOI] [PubMed] [Google Scholar]
- 52.Sachdev A, Villarraga HR, Frantz RP, et al. Right ventricular strain for prediction of survival in patients with pulmonary arterial hypertension. Chest 2011; 139: 1299–1309. [DOI] [PubMed] [Google Scholar]
- 53.Hammarstrom E, Wranne B, Pinto FJ, et al. Tricuspid annular motion. J Am Soc Echocardiogr 1991; 4: 131–139. [DOI] [PubMed] [Google Scholar]
- 54.Lopez-Candales A, Dohi K, Rajagopalan N, et al. Defining normal variables of right ventricular size and function in pulmonary hypertension: an echocardiographic study. Postgrad Med J 2008; 84: 40–45. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.