Abstract
Although the main goal of asthma management guidelines is to achieve and maintain clinical control, reported levels of not well-controlled asthma remain high. The aim of this analysis was to compare the levels of asthma control and the associated impact on patients' health status in Europe in 2006, 2008 and 2010. An additional outcome was the comparison of the burden of asthma with diabetes.
Data were obtained from the cross-sectional, self-reported, European National Health and Wellness Surveys conducted in France, Germany, Italy, Spain and the UK. Asthma control (Asthma Control Test™; QualityMetric, Inc., Lincoln, RI, USA) and health status (Short Form (SF)-12 health survey and the Work Productivity Loss and Activity Impairment questionnaire) were assessed.
In 2010, the proportion of treated asthma patients assessed as having not well-controlled asthma was 53.5%, compared with 56.6% and 55.0% in 2008 and 2006, respectively. A significant reduction in not well-controlled asthma was observed in Germany between 2006 (72.3%) and 2010 (62.5%; p=0.005). Fluctuations in control levels were observed in other countries. For all surveys, having at least well-controlled asthma was associated with a significantly lower number of healthcare contacts in the previous 6 months, better mean±sd SF-12 scores for the physical (data for 2010: not well controlled 39.9±11.38, at least well-controlled 48.0±9.89; p<0.001) and mental (data for 2010: not well-controlled 40.6±10.95, at least well-controlled 45.0±10.91; p<0.001) components, and significantly less impact on Work Productivity Loss and Activity Impairment. Asthma and diabetes were associated with a similar overall negative impact on health status.
A substantial proportion of asthmatics remain not well-controlled across five European countries, resulting in a significant impact on health resources and patients' health status. The overall burden of asthma appears to be similar to that of diabetes.
Keywords: Adults, asthma control, cross-sectional surveys, Europe
Asthma is a chronic respiratory disease that affects an estimated 235 million people worldwide [1], and is associated with a significant socioeconomic burden [2]. Days lost from work and absences from school have been reported as a substantial consequence of asthma [3]. The number of disability-adjusted life years lost due to asthma worldwide has been estimated to be about 15 million per year, similar to that for other chronic diseases, such as diabetes, cirrhosis of the liver or schizophrenia [4]. The economic burden associated with asthma is substantial, due to both direct costs (such as hospital care and medications) and indirect costs (such as time lost from work and premature death) [4]. Data from patients identified in the European Community Respiratory Health Survey (ECRHS) II reported that a heavy asthma burden (reduced activity days and/or hospital services utilisation) was more common in patients with obesity, frequent respiratory symptoms, low lung function and chronic cough/phlegm, and in non-atopic females [2].
The main goal of current asthma treatment guidelines is to achieve clinical control, including control of symptoms, maintenance of normal activity levels and to prevent exacerbations [3, 5]. Previous studies have shown an association between asthma control and health-related quality of life (HRQoL) and healthcare utilisation; worse control results in worse HRQoL scores and an increased number of doctor visits and hospitalisations [6, 7]. Studies in adults and children have also shown that patients with asthma are more likely to report depressive feelings and experience negative emotions compared with non-asthmatic control subjects [8–10]. Anxiety and depression have been reported as independent risk factors for poor asthma control [11]. Poor control has also been shown to increase the costs of asthma [12, 13] and guideline-determined care can be cost-effective [3]. Having not well-controlled (NWC) asthma is common; approximately half of all treated asthmatics in Europe were reported as NWC in the 2006 and 2008 European National Health and Wellness Surveys (NHWS) [14, 15].
The aim of the current NHWS analysis was to review the level of asthma control in Europe in 2010 compared with that in 2006 and 2008, and to re-assess the effects of asthma control on HRQoL, work productivity and healthcare resource use. An additional outcome, utilising the same methodology, was the comparison of the burden of asthma with that of diabetes.
METHODS
Study design
The European NHWS is a large, self-reported patient database based on an annual cross-sectional healthcare survey in France, Germany, Italy, Spain and the UK. The methods for obtaining data have been described previously [14, 15]. For the purposes of this analysis, data were obtained from the 2006, 2008 and 2010 NHWS (Kantar Health, Princeton, NJ, USA). Each survey was taken by a largely different population; in 2006, 2008 and 2010 85%, 84% and 92% of asthma respondents, respectively, took the survey only once (table S1 of the online supplementary material). Respondents with self-reported diagnosed asthma were included in the analyses for 2006 and 2008; respondents with self-reported asthma or diabetes (type 1 and type 2) were included in the analyses for 2010.
Outcome measures
Patient characteristics
Patients answered general questions about their demographics and general health, including sex, age, employment status, weight, smoking status and self-reported experience of comorbidities including depression and anxiety. Questions specifically about asthma included duration of disease, symptoms in the previous 4 weeks and details of asthma medications. Further details have been published previously [14, 15].
Asthma control
For the respondents with asthma, asthma control was assessed using the Asthma Control Test™ (QualityMetric, Inc., Lincoln, RI, USA) [16], a self-administered questionnaire which is validated and aligned with Global Initiative for Asthma (GINA) defined levels of asthma control [3]. The Asthma Control Test scores range from 5 to 25 with a score of ≥20 denoting at least well-controlled (ALWC) asthma and a score of ≤19 denoting NWC asthma.
Healthcare resource use
For both the asthmatic and diabetic patients, information was collected about number and type of healthcare contacts over the previous 6 months including numbers of doctor visits, emergency room visits and hospitalisations.
HRoQL: Short-Form Health Survey
Generic HRQoL was assessed using the Short-Form (SF)-12 Health Survey [17]. Patients were asked to complete the questions based on the previous 4 weeks. The 12 items are used to calculate two component summary scores (physical and mental; PCS-12 and MCS-12, respectively), ranging from 0 (worst quality of life) to 100 (best). Scores are normalised so that scores above or below 50 would be considered better or worse, respectively, than the general population. A minimum clinically important difference (MCID) has been reported to be 3 to 5 units [18].
Work productivity loss and activity impairment
The effect of a patient's disease on their work and general activities was assessed using the Work Productivity Loss and Activity Impairment (WPAI) questionnaire [19]. This has four components: absenteeism (time missed from work); presenteeism (impairment while working); overall work productivity impairment (considers both absenteeism and presenteeism); and impairment in daily activities. WPAI outcomes are expressed as impairment percentages, with higher percentages indicating greater impairment and less productivity.
Statistical analyses
Prevalence estimates for the proportion of patients with ALWC and NWC asthma were computed using frequency weights, based on sex, age and country of residence, as described previously [14, 15].
Bivariate analyses were used to compare data between patients with ALWC versus NWC asthma, and between patients with asthma and diabetes, and were made using weighted data. Patients with both asthma and diabetes were excluded from the comparisons between the asthma and diabetes cohorts. Chi-squared tests were used to test for significant differences in categorical variables, and unpaired t-tests were used to test for significant differences in continuous variables. For all statistical tests, the applied comparison-wise significance level was 0.05. No adjustments were made for multiple comparisons.
RESULTS
Patient characteristics: asthma cohort
Results from the 2010 survey showed that, compared with patients with ALWC asthma, NWC patients were more likely to be female, aged >55 yrs, a current or former smoker, suffer from obesity and be unemployed (table 1). Levels of depression, anxiety and sleep problems were also higher in the patients with NWC asthma. These results are consistent with those reported in the 2006 and 2008 NHWS [14, 15].
Table 1. Characteristics of treated asthma patients by control status from the 2010 National Health and Wellness Survey.
| Not well-controlled | At least well-controlled | p-value | |
| Subjects n | 1677 | 1480 | |
| Females | 63.9 | 56.8 | <0.001 |
| Age yrs | 47.3±15.4 | 43.2±16.0 | <0.001 |
| 18–34 | 25.2 | 35.9 | |
| 35–54 | 40.1 | 38.7 | |
| >55 | 34.7 | 25.4 | |
| Current/ex-smoker | 67.3 | 56.9 | <0.001 |
| Overweight# | 33.0 | 34.2 | ns |
| Obese¶ | 33.0 | 23.0 | <0.001 |
| Asthma treatment | |||
| Controller medication | 79.9 | 66.0 | <0.001 |
| Rescue medication | 60.6 | 63.0 | ns |
| Employment status | |||
| Employed | 48.5 | 59.8 | <0.001 |
| Self-reported in the last 12 months | |||
| Depression | 28.6 | 20.6 | <0.001 |
| Anxiety | 35.8 | 27.3 | <0.001 |
| Sleep problems | 44.9 | 31.9 | <0.001 |
Data are presented as % or mean±sd, unless otherwise stated. Statistical comparisons were computed using Chi-squared tests for percentages and unpaired t-tests for mean. ns: nonsignificant. #: body mass index ≥25 and <30 kg·m−2; ¶: body mass index ≥30 kg·m−2.
Treatment patterns at the three time-points showed that there had been a significant decrease in short-acting β2-agonist use in 2010 (61.8%) compared with 2006 and 2008 (66.3% for both, p<0.05). The proportion of patients prescribed an inhaled corticosteroid (ICS) was 33.5%, 30.9% and 34.8% for 2006, 2008 and 2010, respectively; the difference between 2008 and 2010 was statistically significant (p<0.05). The use of fixed dose combination products was significantly greater in 2008 (31.3%) compared with 2006 (27.9%), and a similar usage to 2008 was reported in 2010 (31.1%). Conversely, the percentage of patients reporting treatment with a long-acting β2-agonist (LABA) showed a significant reduction between 2006 (10.9%) and 2008 (8.8%, p<0.05). There was no statistical difference between LABA use in the 2010 survey (9.8%) and either of the previous surveys.
Asthma control
In the three NHWS, the number of respondents with diagnosed asthma and the percentage of these currently using a prescription medication for their asthma were: 2006: n=2,337 (78%); 2008: n=3,619 (78%); 2010: n=3,848 (81%).
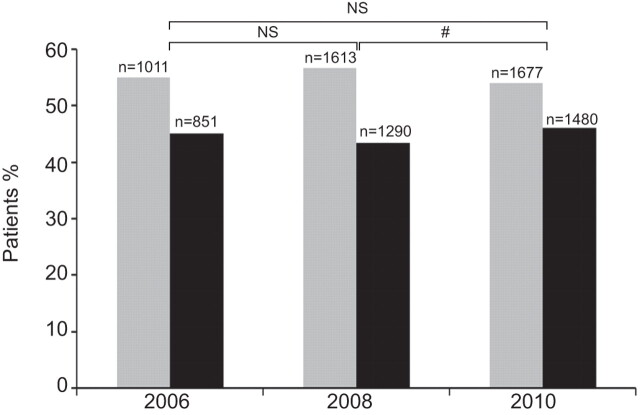
In 2010, the proportion of treated asthma patients assessed as having NWC asthma by the Asthma Control Test was 53.5%, compared with 56.6% and 55.0% in 2008 and 2006, respectively (fig. 1 and table S2). There was no statistically significant difference between reported control levels in 2006 and 2010, but a significant improvement between 2008 and 2010 was observed (p=0.035).
Figure 1.
Proportion of treated patients with not well-controlled asthma (▓) and at least well-controlled asthma (▪) in 2006, 2008 and 2010 in all countries. ns: nonsignificant. #: p=0.035.
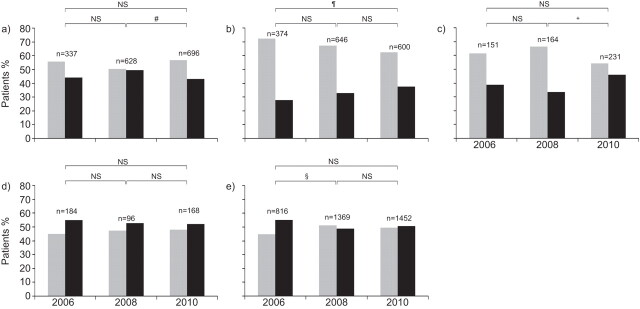
In 2010, higher levels of NWC asthma were reported in Germany compared with the other countries, agreeing with previous NHWS, but the proportion of patients with NWC asthma showed a significant improvement in this country between those reported in 2006 (72.3%) and those in 2010 (62.5%; p=0.005) (fig. 2 and table S2). For all other countries, there was no significant difference in the control levels reported in 2006 compared with 2010. For the comparison of asthma control levels in 2008 and 2010, France showed a statistically significant worsening in the proportion of patients with NWC asthma (p=0.033) whilst Italy showed a statistically significant improvement (p=0.021) (fig. 2 and table S2). Germany, Spain and the UK showed no significant changes in reported control levels between these two time-periods.
Figure 2.
Proportion of treated patients with not well-controlled asthma (▓) and at least well-controlled (▪) asthma in 2006, 2008 and 2010 in a) France, b) Germany, c) Italy, d) Spain and e) the UK. ns: nonsignificant. #: p=0.033; ¶: p=0.005; +: p=0.021; §: p=0.01.
Results from all three NHWS consistently showed that ∼75% of patients with NWC asthma reported breathlessness at least 3–6 times per week and ∼75% used their rescue medication at least 2–3 times per week compared with around 6.0% and 15%, respectively, of patients with ALWC asthma (data not shown) [14, 15]. Similarly, across all surveys, an average of 61% of NWC patients reported waking at least once a week due to asthma symptoms compared with 4% of those with ALWC. These findings were reported consistently across all countries.
Healthcare resource use and patient reported outcomes in the asthma cohorts
Healthcare resource use
Results for the 2010 NHWS showed that patients with NWC asthma spoke to their doctors more about their asthma, made more emergency room visits and were hospitalised more often compared with patients with ALWC asthma (table 2). These results agree with the findings reported in 2006 and 2008 (fig. 3a). In 2010, the results were largely consistent across all countries except for mean hospitalisations in Italy and Spain; these were not significantly different between patients according to their asthma control status (table 2). These findings are similar to those reported in 2006/2008 (tables S3a and S3b).
Table 2. Healthcare utilisation, health-related quality of life and work productivity in asthma patients by control status and country in 2010.
| All countries | France | Germany | Italy | Spain | UK | |||||||
| NWC | ALWC | NWC | ALWC | NWC | ALWC | NWC | ALWC | NWC | ALWC | NWC | ALWC | |
| Subjects n | 1875 | 1973 | 451 | 480 | 436 | 318 | 160 | 186 | 90 | 127 | 738 | 862 |
| Healthcare utilisation# | ||||||||||||
| Times spoken to doctor about asthma n¶ | 3.35±3.79 | 1.38±1.73 | 3.77±3.54 | 1.52±1.86 | 3.47±3.40 | 2.09±2.31 | 3.90±4.90 | 1.27±1.54 | 3.27±3.88 | 1.14± 1.73 | 2.79±3.60 | 1.09±1.26 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Emergency room visits | 0.53±1.50 | 0.27±1.03 | 0.33±1.01 | 0.20±0.73 | 0.36±1.32 | 0.13±0.70 | 0.80±1.92 | 0.29±1.07 | 1.34±1.84 | 0.77±1.66 | 0.49±1.50 | 0.21±1.00 |
| p-value | <0.001 | 0.036 | 0.011 | 0.003 | 0.022 | 0.001 | ||||||
| Times hospitalised n | 0.31±1.22 | 0.14±0.58 | 0.27±0.71 | 0.15±0.44 | 0.32±1.22 | 0.09±0.39 | 0.37±1.01 | 0.21±0.85 | 0.34±0.99 | 0.29±0.97 | 0.30±1.54 | 0.09±0.36 |
| p-value | <0.001 | 0.002 | 0.003 | 0.127 | 0.756 | 0.001 | ||||||
| SF-12 scores | ||||||||||||
| PCS | 39.9±11.38 | 48.0±9.89 | 41.0±11.40 | 49.9±8.41 | 39.1±10.14 | 46.7±9.63 | 40.2±9.4 | 46.5±9.27 | 41.4±9.36 | 46.51±10.0 | 39.3±13.17 | 48.8±10.67 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| MCS | 40.6±10.95 | 45.0±10.91 | 41.4±10.77 | 45.4±10.17 | 39.9±10.29 | 45.0±10.24 | 38.9±9.54 | 44.0±10.12 | 38.8±10.90 | 48.0±11.19 | 41.7±11.94 | 44.5±11.65 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
| Work productivity and activity impairment | ||||||||||||
| Work time missed due to health % | 10.4±23.59 | 7.0±22.28 | 13.3±29.51 | 6.8±23.04 | 11.9±26.08 | 9.0±25.50 | 7.0±15.49 | 5.7±16.10 | 14.4±22.69 | 6.1±19.94 | 7.8±20.47 | 6.9±22.70 |
| p-value | 0.010 | 0.019 | 0.357 | 0.655 | 0.076 | 0.671 | ||||||
| Impairment while at work due to health % | 32.5±26.99 | 18.0±23.19 | 29.1±27.20 | 15.2±20.17 | 34.5±25.55 | 22.6±25.71 | 38.9±28.47 | 25.1±26.80 | 39.9±27.49 | 17.4±23.34 | 25.9±24.86 | 15.3±21.26 |
| p-value | <0.001 | <0.001 | <0.001 | 0.005 | <0.001 | <0.001 | ||||||
| Activity impairment due to health % | 48.8±29.22 | 26.4±28.57 | 46.3±29.95 | 24.6±27.36 | 49.3±27.41 | 26.0±26.60 | 50.8±28.19 | 29.7±26.68 | 48.3±27.70 | 28.6±30.17 | 47.9±30.85 | 25.6±29.40 |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
Data are presented as mean±sd, unless otherwise stated. In the 2006 National Health and Wellness Survey (NHWS), the hospitalisation question was: “What is the total number of days you were hospitalised for your own medical condition in the past 6 months?” In the 2008 and 2010 NHWS, the question was changed to: “How many times have you been hospitalised for your own medical condition in the past 6 months?” NWC: not well-controlled; ALWC: at least well-controlled; SF-12: short-form 12; PCS: physical component summary score; MCS: mental component summary score. #: during previous 6 months; ¶: includes any form of contact, not just clinic visits.
Figure 3.
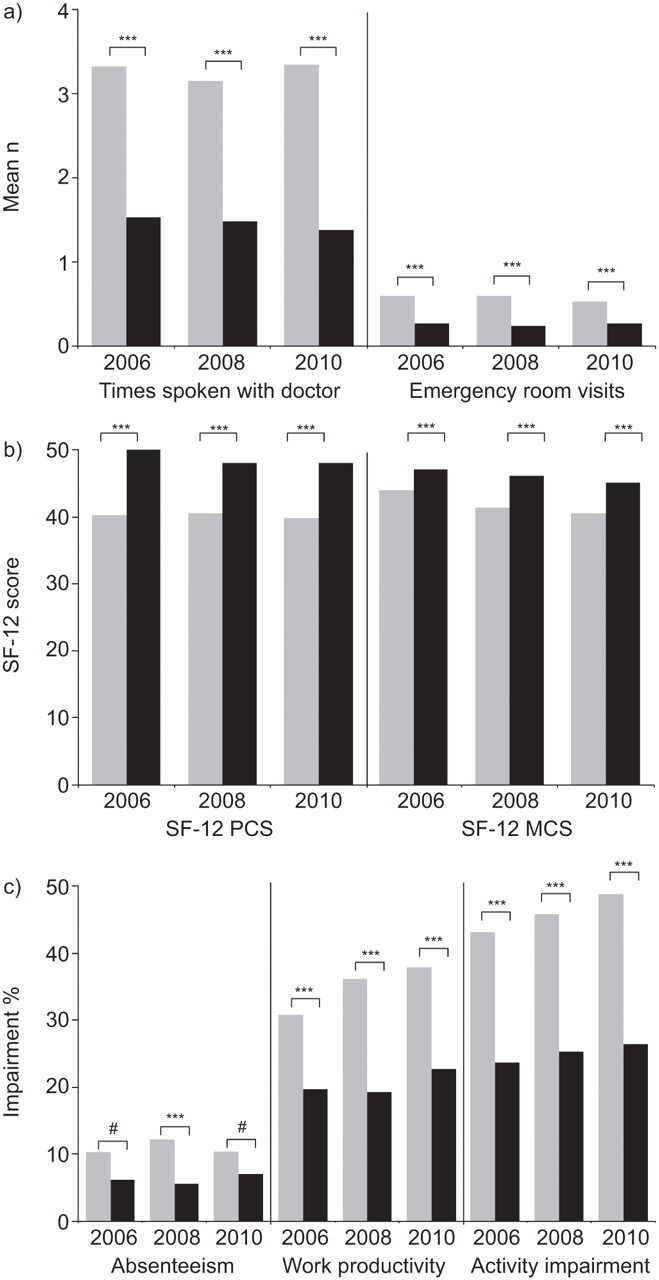
a) Healthcare utilisation, b) short form (SF)-12 scores and c) work productivity and impairment, in 2006, 2008 and 2010 in all countries. Work productivity considers both absenteeism and impairment while at work due to health. ▪. not well-controlled asthma; ▪. at least well-controlled asthma. PCS: physical component summary score; MCS: mental component summary score. ***: p<0.001; #: p=0.01.
HRQoL: Short-Form Health Survey
Results of SF-12 scores in 2010 showed significant impairment in HRQoL in patients with NWC asthma compared with ALWC patients for both the PCS (mean±sd NWC 39.9±11.38 and ALWC 48.0±9.89; p<0.001) and MCS scores (NWC 40.6±10.95 and ALWC 45.0±10.91; p<0.001) (fig. 3b). Results from the 2006 and 2008 surveys showed a similar significant impact (fig. 3b). Results were largely similar across all countries for 2010 (table 2) and 2006/2008 (tables S3a and S3b). The differences between patient groups exceeded the MCID in all comparisons with the exception of MCS-12 scores in the UK (2010), France (2006) and Italy (2006/2008). Generally, in patients with ALWC asthma, mean PCS and MCS scores were near to or approaching the normalised score of 50 for the general population whereas mean scores for patients with NWC asthma were well below this normalised score.
Work productivity and activity impairment
Having asthma that was NWC had a significant impact on work productivity and daily activities. Overall, results in 2010 showed that NWC patients missed more days from work (absenteeism), suffered more impairment whilst at work and experienced more impairment in activities than patients with ALWC asthma; which is similar to that reported in 2006 and 2008 (fig. 3c). The results for time missed from work were not consistent across countries in 2010 (table 2), 2006 or 2008 (tables S3a and S3b). In 2010, for example, significant differences between patient groups in absenteeism were observed in France (mean±sd NWC 13.26±29.51 and ALWC 6.84±23.04; p=0.019) but not in Germany, Italy, Spain or the UK (table 2). Differences between asthma control groups with respect to impairment at work and impairment of daily activities showed similar results across all countries.
Asthma versus diabetes cohorts
Patient characteristics
A total of 284 patients diagnosed with both asthma and diabetes were excluded from the asthma and diabetes cohorts considered in this analysis, comprising 4% of these patient populations. When comparing the asthma and diabetes cohorts from the 2010 NHWS, patients with diabetes were significantly older, were more likely to be current or former smokers and significantly more patients were either overweight or obese. Consistent with the age demographics, a higher proportion of patients with asthma were in employment and a higher proportion of patients with diabetes were retired (table 3).
Table 3. Demographic characteristics of patients with diagnosed asthma and diabetes.
| Asthma | Diabetes | p-value | |
| Subjects n | 3564 | 3361 | |
| Females | 58.4 | 39.0 | <0.05 |
| Age yrs | 43.3±15.5 | 59.9±12.9 | |
| 18–34 | 35.1 | 5.1 | |
| 35–54 | 38.8 | 24.3 | <0.05 |
| >55 | 26.1 | 70.6 | |
| Current/ex-smoker | 61.8 | 70.4 | <0.05 |
| Overweight# | 33.4 | 40.0 | <0.05 |
| Obese¶ | 24.9 | 41.2 | <0.05 |
| Employment status | |||
| Employed | 56.4 | 33.1 | <0.05 |
| Unemployed | 43.6 | 66.9 | <0.05 |
| Retired | 16.5 | 53.1 | <0.05 |
| Long-term disability | 4.2 | 3.8 | ns |
Data are presented as % or mean±sd, unless otherwise stated. Statistical comparisons were computed using Chi-squared test for percentages and unpaired t-tests for means. ns: nonsignificant. #: body mass index ≥25 and <30 kg·m−2; ¶: body mass index ≥30 kg·m−2.
Healthcare resource use and patient reported outcomes in the asthma versus diabetes cohorts
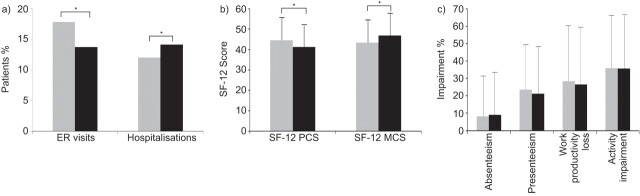
A significantly higher proportion of patients with asthma attended emergency rooms during 2010 compared with those with diabetes, whilst a significantly higher percentage of patients with diabetes were hospitalised (fig. 4a). Both asthma and diabetes were associated with impaired HRQoL; mean SF-12 PCS and MCS scores for the asthma and diabetes cohorts were below the normalised score of 50 for the general population. Patients with diabetes scored worse than patients with asthma on PCS (diabetes 41.3±10.76 and asthma 44.9±11.04; p<0.05), the reverse was true for MCS (diabetes 46.8±10.90 and asthma 43.1±11.20; p<0.05) (fig. 4b). The differences between cohorts exceeded the MCID for both the PCS and MCS scores.
Figure 4.
a) Healthcare utilisation, b) short form (SF)-12 scores and c) work productivity and activity impairment in patients with asthma (▓) and diabetes (▪) in 2010. ER: emergency room; PCS: physical component summary score; MCS: mental component summary score. *: p<0.05.
Having asthma or diabetes was associated with a similar negative impact on work productivity and activity impairment; no significant differences between diseases were observed for any WPAI parameter (fig. 4c).
DISCUSSION
The current analysis shows that over the past 5 yrs the proportion of treated asthma patients reporting their asthma as NWC has been consistently 50% or more in five European countries. The results of the three surveys, conducted in largely different populations of asthmatics, demonstrate that large numbers of patients with asthma remain uncontrolled despite the fact that most patients should be able to achieve and maintain clinical control based on a good pharmacological strategy [3]. Statistically significant fluctuations in medication treatment patterns were seen over the three time-points but they did not alter the consistent message of poor control that was observed for all surveys. Surveys conducted in primary care have reported similar levels of uncontrolled asthma (55–59%) as those reported herein [20–22].
Although there was no substantial change in asthma control prevalence in five European countries overall from 2006 to 2010, there were fluctuations at country level. The most consistent improvements were seen in Germany. However, Germany reported higher levels of NWC asthma in 2006 which may explain this finding. The remaining countries showed no significant change from 2006 to 2010 despite some positive and negative changes from 2008 to 2010. The clinical relevance of the statistically significant changes that were observed is not clear due to limitations regarding patient-reported data and the sensitivity of the Asthma Control Test. However, the observed differences at country level may be due to different healthcare organisation. The ECRHS II showed widespread variations in asthma control across countries in Europe; asthma control in ICS users ranged from 20% (Iceland) to 67% (Italy) [23]. A review of the follow-ups of the population-based Respiratory Health in Northern Europe and ECRHS studies reported that overall asthma treatments have increased over a 9-yr period but that the prevalence of asthma treatments varied across European countries, and that the strongest predictor of adherence to treatment was regular consultation with a healthcare professional [24]. Results of the International Control of Asthma Symptoms (ICAS) survey also demonstrated differences in asthma prescribing patterns, e.g. 86% of patients surveyed in Germany reported that they could obtain a repeat prescription instead of discussing symptoms with their doctor compared with 7% in France. [25]. The results of a survey conducted in Spain, France and Italy, showed poor asthma control in patients with moderate and severe persistent asthma, which was attributed, in part, to under-use of asthma medications [26]. Most patients in France and Spain (≥90%) reported use of ICS compared with ∼70% of patients in Italy. In Spain, visits to the emergency room were more frequent and the costs of emergency care in all asthma severity categories were up to 10 times higher than in Italy and France.
One possible explanation for the low levels of overall asthma control may relate to perceptions about the disease; both patients and physicians have been shown to over-estimate levels of asthma control and patients have been shown to accept a sub-optimal disease status as being normal [27, 28]. Results of the ICAS survey demonstrated that patients with asthma have low expectations about their disease with as many as 90% expecting to have symptoms as a normal part of their condition [25]. In a recent epidemiological study in Germany in patients with allergic asthma, 65% of patients were rated as controlled (GINA definition) by respiratory specialists compared with 20% by patient-rated Asthma Control Test. Although these findings are not strictly comparable to our own, as these asthma patients were all under respiratory specialist care, they do highlight the differences between patient-rated assessments and the perceptions of physicians [29]. This was also shown in a study by Juniper et al. [30] who reported that respiratory specialists overestimated improvements in asthma control, following asthma treatment modifications, compared with patient responses to the asthma control questionnaire.
A possible means to improve asthma control may include improved communication between patients and their physicians. The importance of a good patient–physician partnership was reported recently in a cross-sectional observational study conducted in the same five European countries as analysed here, and showed that the better the partnership between patient and physician, the more likely patients were to have good asthma control, fewer exacerbations and a better quality of life [31]. Kaya et al. [32] also reported that, for a group of 63 outpatients with persistent asthma, asthma self-management plans improved asthma control and quality of life. Personalised patient action plans that take into consideration the variable nature of asthma and the different responses in individual patients have also been cited as providing a possible tool for anticipating triggers of symptoms and exacerbations [33]. Soriano et al. [34] analysed predictors of asthma control, using the Asthma Insights and Reality in Europe database, and reported that poor asthma control was associated with less continuity of medical care, poor patient understanding about their disease, fears about taking ICS and an over reliance on quick relief bronchodilator and non-prescription medications. Improved monitoring of patients and a good understanding between doctor and patients may help to resolve some of these important issues.
Results from the 2010 NHWS showed that patients with NWC asthma were more likely to require a physician/emergency room visit or be hospitalised, miss time from work and have a poorer quality of life than patients with ALWC asthma. This in agreement with the results of several previous studies that show uncontrolled asthma is associated with a significant burden for patients and healthcare systems [6, 7, 35]. Most recently, in a 1-yr, prospective, longitudinal study in adults and children, Guilbert et al. [7] showed that patients with NWC asthma had significantly lower quality of life and attended more physicians’ surgeries or had more emergency room visits compared with patients with higher Asthma Control Test scores. The associated costs of the socioeconomic burden of asthma are substantial [12, 13], and this is especially pertinent in the current environment where healthcare providers are trying to allocate resources and control escalating healthcare costs.
The results of this analysis showed a similar overall burden for asthma and diabetes, which agrees with statistics published by the World Health Organization for disability-adjusted life years [4]. The negative impact on work productivity and physical impairment was very similar for the two diseases. Both asthma and diabetes were also associated with an impaired HRQoL, but the impact of diabetes was worse on the PCS whilst that of asthma was worse on the MCS. The differences in the physical component results may be related to the higher average age of the diabetes cohort compared with the asthma cohort. The impact of asthma on mental summary scores concur with previous findings that patients with asthma are more likely to report depressive feelings and experience negative emotions compared with non-asthmatic control subjects [8–10].
One of the limitations of this analysis is that the outcomes were self-reported and have not been clinically verified. However, the questionnaires used have been clinically verified and the results for asthma prevalence are consistent with the finding of other surveys in general practice [20–22], suggesting that these findings are valid. Another limitation is that this was a cross-sectional survey and therefore cause and effect relationships cannot be established. However, the results of the three surveys in largely different asthmatic populations have shown a very consistent pattern at three different time-points. Prospective, longitudinal studies are required to verify such effects. The results of the present analysis, conducted using bivariate analyses, showed that several demographic factors were associated with NWC asthma, but of additional interest would be to further explore these factors using multiple logistic regression analyses to investigate possible predictors of asthma control.
In conclusion, the overall level of asthma control in five European countries has not substantially improved in the last 5 yrs, although variations by country were observed with improvements seen in Germany. High levels of NWC asthma continue to result in a significant impact on health resource use, HRQoL and work impairment across all countries surveyed. The overall burden of asthma and diabetes was similar.
Supplementary Material
Acknowledgments
Editorial support was provided by K. Hollingworth (Continuous Improvement Ltd, Kingsbridge, UK), and was funded by GlaxoSmithKline.
Footnotes
Provenance
Publication of this peer-reviewed article was supported by GlaxoSmithKline, France (article sponsor, European Respiratory Review issue 123).
This article has supplementary material available from err.ersjournals.com
Support Statement
This analysis was funded by GlaxoSmithKline (study number: 115200).
Statement of Interest
K. Annunziata is currently an employee of Kantar Health. GlaxoSmithKline has purchased access into the EU National Health and Wellness Survey from Kantar Health. E. Gubba currently works as a contractor for GlaxoSmithKline and has previously been employed by them and holds shares in the company. L. Adamek holds shares in GlaxoSmithKline and is an employee of GlaxoSmithKline.
REFERENCES
- 1.World Health Organization Asthma fact sheet. Date last accessed: September 2011. Date last updated: May 2011. www.who.int/mediacentre/factsheets/fs307/en/index.html.
- 2.Accordini S, Corsico A, Cerveri I, et al. The socio-economic burden of asthma is substantial in Europe. Allergy 2008; 63: 116–124. [DOI] [PubMed] [Google Scholar]
- 3.Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention (updated 2010). www.ginasthma.com.
- 4.Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee Report. Allergy 2004; 59: 469–478. [DOI] [PubMed] [Google Scholar]
- 5.National Asthma Education and Prevention Program: Expert Panel Report 3. Guidelines for the Diagnosis and Management of Asthma. Bethesda, National Institutes of Health, 2007.
- 6.Vollmer W, Markson LE, O'Connor E, et al. Association of asthma control with healthcare utilisation and quality of life. Am J Respir Crit Care Med 1999; 160: 1647–1652. [DOI] [PubMed] [Google Scholar]
- 7.Guilbert TW, Garris C, Jhingran P, et al. Asthma that is not well-controlled is associated with increased healthcare utilization and decreased quality of life. J Asthma 2011; 48: 126–132. [DOI] [PubMed] [Google Scholar]
- 8.Strine TW, Mokdad AH, Balluz LS, et al. Impact of depression and anxiety on quality of life, health behaviors, and asthma control among adults in the United States with asthma, 2006. J Asthma 2008; 45: 123–133. [DOI] [PubMed] [Google Scholar]
- 9.Cluely S, Cochrane GM. Psychological disorder in asthma is associated with poor control and poor adherence to inhaled steroids. Respir Med 2001; 95: 37–39. [DOI] [PubMed] [Google Scholar]
- 10.Fernandes L, Fonseca J, Martins S, et al. Association of anxiety with asthma: subjective and objective outcome measures. Psychosomatics 2010; 51: 39–46. [DOI] [PubMed] [Google Scholar]
- 11.Di Marco, Verga M, Santus P, et al. Close correlation between anxiety, depression and asthma control. Respir Med 2010; 104: 22–28. [DOI] [PubMed] [Google Scholar]
- 12.Accordini S, Bugiani M, Arossa W, et al. Poor control increases the economic cost of asthma. A multicentre population-based study. Int Arch Allergy Immunol 2006; 141: 189–198. [DOI] [PubMed] [Google Scholar]
- 13.Van Ganse E, Laforest L, Pietri G, et al. Persistent asthma: disease control, resource utilisation and direct costs. Eur Respir J 2002; 20: 260–267. [DOI] [PubMed] [Google Scholar]
- 14.Demoly P, Paggiaro P, Plaza V, et al. Prevalence of asthma control among adults in France, Germany, Italy, Spain and the UK. Eur Respir Rev 2009; 18: 105–112. [DOI] [PubMed] [Google Scholar]
- 15.Demoly P, Gueron B, Annunziata K, et al. Update on asthma control in five European countries. Eur Respir Rev 2010; 19: 150–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nathan RA, Sorkness CA, Kosinski, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol 2004; 113: 59–65. [DOI] [PubMed] [Google Scholar]
- 17.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34: 220–233. [DOI] [PubMed] [Google Scholar]
- 18.Samsa G, Edelman D, Rothman ML, et al. Determining clinically important differences in health status measures. A general approach with illustration to the health utilities index mark II. Pharmacoeconomics 1999; 15: 141–155. [DOI] [PubMed] [Google Scholar]
- 19.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 1993; 4: 353–65. [DOI] [PubMed] [Google Scholar]
- 20.Mintz M, Gilsenan AW, Bui CL, et al. Assessment of asthma control in primary care. Curr Med Res Opin 2009; 25: 2423–2531. [DOI] [PubMed] [Google Scholar]
- 21.Peters SP, Jones CA, Haselkorn T, et al. Real-world evaluation of asthma control and treatment (REACT): findings from a national web-based survey. J Allergy Clin Immunol 2007; 119: 1454–61. [DOI] [PubMed] [Google Scholar]
- 22.Chapman KR, Boulet LP, Rea RM, et al. Suboptimal asthma control: prevalence, detection and consequences in general practice. Eur Respir J 2008; 31: 320–325. [DOI] [PubMed] [Google Scholar]
- 23.Cazzoletti L, Marcon A, Janson C, et al. Asthma control in Europe: a real-world evaluation based on an international population-based study. J Allergy Clin Immunol 2007; 120: 1360–1367. [DOI] [PubMed] [Google Scholar]
- 24.Omenaas E, Svanes C, Janson C, et al. What can we learn about asthma and allergy from the follow-up of the RHINE and the ECRHS studies? Clin Respir J 2008; 2: 45–52. [DOI] [PubMed] [Google Scholar]
- 25.Bellamy D, Harris T. Poor perceptions and expectations of asthma control: results of the International Control of Asthma Symptoms (ICAS) survey of patients and general practitioners. Prim Care Respir J 2005; 14: 252–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Van Ganse E, Antonicelli L, Zhang Q, et al. Asthma-related resource use and cost by GINA classification of severity in three European countries. Respir Med 2006; 100: 140–147. [DOI] [PubMed] [Google Scholar]
- 27.Rabe KF, Vermeire PA, Soriano JB, et al. Clinical management of asthma in 1999: the Asthma Insights and Reality in Europe (AIRE) study. Eur Respir J 2000; 16: 802–807. [DOI] [PubMed] [Google Scholar]
- 28.Prieto L, Badiola C, Villa JR, et al. Asthma control: do patients' and physicians' opinions fit in with patients' asthma control status? J Asthma 2007; 44: 461–467. [DOI] [PubMed] [Google Scholar]
- 29.Kardos P, Wittchen H-U, Mühlig S, et al. Controlled and uncontrolled allergic asthma in routine respiratory specialist care – a clinical–epidemiological study in Germany. Curr Med Res Opin 2011; 27: 1835–1847. [DOI] [PubMed] [Google Scholar]
- 30.Juniper EF, Chauhan A, Neville E, et al. Clinicians tend to overestimate improvements in asthma control: an unexpected observation. Prim Care Respir J 2004; 13: 181–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Small M, Vickers A, Anderson P, et al. The patient-physician partnership in asthma: real-world observations associated with clinical and patient-reported outcomes. Adv Ther 2010; 27: 591–599. [DOI] [PubMed] [Google Scholar]
- 32.Kaya Z, Erkan F, Ozkan M, et al. Self-management plans for asthma control and predictors of patient compliance. J Asthma 2009; 46: 270–272. [DOI] [PubMed] [Google Scholar]
- 33.Yawn BP. Factors accounting for asthma variability: achieving optimal symptom control for individual patients. Prim Care Respir J 2008; 17: 138–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Soriano JB, Rabe KF, Vermeire PA. Predictors of poor asthma control in European adults. J Asthma 2003; 40: 803–813. [DOI] [PubMed] [Google Scholar]
- 35.Pont LG, van der Molen T, Denig P, et al. Relationship between guideline treatment and health-related quality of life in asthma. Eur Respir J 2004; 23: 718–722. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.