Abstract
Pulmonary hypertension (PH) is a major complication of several haematological disorders. Chronic myeloproliferative diseases (CMPDs) associated with pulmonary hypertension have been included in group five of the clinical classification for pulmonary hypertension, corresponding to pulmonary hypertension for which the aetiology is unclear and/or multifactorial. The aim of this review is to discuss the epidemiology, pathogenic mechanism and treatment approaches of the more common forms of pulmonary hypertension in the context of CMPD's: chronic thromboembolic pulmonary hypertension, precapillary pulmonary hypertension and drug-induced PH.
Short abstract
Epidemiology, pathogenic mechanism and treatment approach of PH in patients with chronic myeloproliferative diseases http://ow.ly/Q1QX4
Introduction
Pulmonary hypertension (PH), which is defined as an elevated mean pulmonary artery pressure ≥25 mmHg at rest [1–3], is a major complication of several haematological disorders. Chronic myeloproliferative diseases (CMPDs) associated with PH are included in group five of the most recent clinical classification (from the fifth World Symposium on PH, Nice, 2013), corresponding to PH with an unclear and/or multifactorial aetiology (table 1) [3]. An improvement in the characterisation of this group of diseases should be encouraged in order to support clinicians in the management of these patients with severe comorbidities, as emphasised by Simonneau et al. [2].
TABLE 1.
Updated clinical classification of pulmonary hypertension (from the fifth World Symposium on pulmonary hypertension, Nice, 2013)
| Disease | Classification |
| Pulmonary arterial hypertension (PAH) | 1 |
| Idiopathic PAH | 1.1 |
| Heritable | 1.2 |
| BMPR2 | 1.2.1 |
| ALK1, endoglin (with or without hereditary haemorrhagic telangiectasia), SMAD9, CAV1, KCNH3 | 1.2.2 |
| Unknown | 1.2.3 |
| Drug and toxin-induced | 1.3 |
| Associated with: | 1.4 |
| Connective tissue diseases | 1.4.1 |
| HIV infection | 1.4.2 |
| Portal hypertension | 1.4.3 |
| Congenital heart diseases | 1.4.4 |
| Schistosomiasis | 1.4.5 |
| Pulmonary veno-occlusive disease and/or pulmonary capillary haemangiomatosis | 1′ |
| Persistent pulmonary hypertension of the newborn | 1″ |
| Pulmonary hypertension owing to left heart disease | 2 |
| Left ventricular systolic dysfunction | 2.1 |
| Left ventricular diastolic dysfunction | 2.2 |
| Valvular disease | 2.3 |
| Congenital/acquired left heart inflow/outflow tract obstruction and congenital cardiomyopathies | 2.4 |
| Pulmonary hypertension owing to lung diseases and/or hypoxia | 3 |
| Chronic obstructive pulmonary disease | 3.1 |
| Interstitial lung disease | 3.2 |
| Other pulmonary diseases with mixed restrictive and obstructive pattern | 3.3 |
| Sleep disordered breathing | 3.4 |
| Alveolar hypoventilation disorders | 3.5 |
| Chronic exposure to high altitude | 3.6 |
| Developmental abnormalities | 3.7 |
| Chronic thromboembolic pulmonary hypertension | 4 |
| Pulmonary hypertension with unclear multifactorial mechanisms | 5 |
| Haematological disorders: chronic haemolytic anaemia, myeloproliferative disorders, splenectomy | 5.1 |
| Systemic disorders: sarcoidosis, pulmonary Langerhans cell histocytosis, lymphangioleiomyomatosis, neurofibromatosis, vasculitis | 5.2 |
| Metabolic disorders: glycogen storage disease, Gaucher disease, thyroid disorders | 5.3 |
| Others: tumoral obstruction, fibrosing mediastinitis, chronic renal failure, segmental PH | 5.4 |
BMPR2: bone morphogenetic protein receptor protein type 2; ALK1: activin receptor-like kinase type 1; CAV1: caveolin-1. Reproduced from [4] with permission from the publisher.
The haematopoietic pluripotent stem cell is capable of both self-renewal and a stepwise differentiation, after a stochastic determination, into either the lymphoid or myeloid lineage. An operational classification of haematological malignancies separates lymphoid from myeloid processes and divides them into acute or chronic according to rate of progression. The chronic myeloid disorders encompass several clinical–pathological entities including the myelodysplastic syndromes and myeloproliferative disorders, which are gathered into seven disorders in the World Health Organization (WHO) classification of the CMPDs (table 2) [5].
TABLE 2.
World Health Organization classification of the chronic myeloproliferative diseases
| Myeloproliferative neoplasms (MPN) | 1 |
| Chronic myelogenous leukaemia, BCR-ABL1 positive | 1.1 |
| Polycythaemia vera | 1.2 |
| Essential thrombocythaemia | 1.3 |
| Primary myelofibrosis | 1.4 |
| Chronic neutrophilic leukaemia | 1.5 |
| Chronic eosinophilic leukaemia, not otherwise specified | 1.6 |
| Mast cell disease | 1.7 |
| Unclassifiable myeloproliferative neoplasms | 1.8 |
| Myeloid and lymphoid neoplasms with eosinophilia and abnormalities of PDGFRA, PDGFRB and FGFR1 | 2 |
| Myelodysplastic syndromes/myeloproliferative neoplasms | 3 |
| Chronic myelomonocytic leukaemia | 3.1 |
| Juvenile myelomonocytic leukaemia | 3.2 |
| Atypical chronic myeloid leukaemia, BCR-ABL-negative | 3.3 |
| Unclassifiable myelodysplastic syndromes/myeloproliferative neoplasms | 3.4 |
| Myelodysplastic syndromes | 4 |
| Acute myeloid leukaemia | 5 |
PDGFRA: platelet-derived growth factor receptor α; PDGFRB: platelet-derived growth factor receptor β; FGFR1: fibroblast growth factor receptor 1. Information from [5].
The pathogenesis of CMPDs involves a multipotent haemopoietic progenitor cell overproducing one or more of the elements that form the blood without significant dysplasia. CMPDs are a heterogeneous group of disorders with a different genetic basis. Disorders with primary expression of a myeloid phenotype include chronic neutrophilic leukaemia (CNL), chronic eosinophilic leukaemia (CEL) and chronic myelogenous leukaemia (CML), as they are the consequence of the balanced translocation between chromosomes 9 and 22 (the Philadelphia chromosome) [6]. By contrast, in essential thrombocytosis, polycythaemia vera and idiopathic myelofibrosis erythroid or megakaryocytic hyperplasia predominates with a different rate of expression of a JAK2 (Janus kinase 2) mutation, V617F [7]. The difference between the two groups is also reflected in the natural history of the diseases. CML, CNL and CEL have a high rate of transformation into acute leukaemia, while polycythaemia vera, idiopathic myelofibrosis and essential thrombocytosis have relatively indolent clinical courses even though they may show recurrent thrombo-haemorrhagic complications. The annual incidence of CMPDs is estimated at 6–9 new cases per 100 000 population, occurring most commonly between 40 and 60 years of age. The most frequent pulmonary complications are caused either by infection or by venous thromboembolic events. Pulmonary or pleural extramedullary haematopoiesis is a rare complication that may be associated with myelofibrosis [8, 9].
Epidemiology
The possible association between PH and CMPDs has been suggested by several case reports and small case series. However, the prevalence and incidence of PH in the context of CMPDs may be underestimated since the clinical signs of disease appear at an advanced stage of the disease and, in some cases, the diagnosis of CMPDs is difficult to establish in the context of chronic hypoxaemia.
To evaluate cardiac involvement in CMPDs, Reisner et al. [10] performed two-dimensional and Doppler echocardiographic studies in 30 patients (18 women and 12 men): 18 patients had polycythaemia vera, eight had essential thrombocytosis and four had angiogenic myeloid metaplasia. Four (13%) out of 30 were diagnosed with PH unrelated to valvular disease [10]. In another study, a cohort of 24 patients, the majority of whom were affected by essential thrombocytosis (14 out of 24), underwent an echocardiographic study [11]. PH, defined by right ventricular systolic pressure (RVSP >35 mmHg), was found in 10 (41.7%) patients, four males and six females, with a mean RVSP of 42 mmHg (range 37–70 mmHg). Age, sex, presence of splenomegaly, type of CMPD, duration of CMPD, age at diagnosis of CMPD, presence of symptoms, haemoglobin levels, and white blood cell or platelet count were not predictive of the presence of PH [11]. Altintas et al. [12] found PH in 22 (47.8%) patients out of 46 affected by essential thrombocytosis in an echocardiographic study (PH was defined as RVSP >35 mmHg). In this group of patients significantly higher platelets counts were observed. Another group [13], without confirmation of right heart catheterisation, described PH in 12 (48%) out of 25 patients with CMPDs. No relationship between PH and age at diagnosis, duration of disease, platelet count and haematocrit level was described.
The association between PH and primary myelofibrosis, since angiogenesis is believed to contribute to the pathogenesis of both conditions, was investigated in a group of 36 patients, of whom 22 were affected by primary myelofibrosis, seven by myelofibrosis developing from polycythaemia vera and seven by myelofibrosis progressing from essential thrombocytosis [14]. PH, in this case evaluated by means of transthoracic echocardiography, was found in 13 (36%) patients.
Roach et al. [15] evaluated cardiac function by means of echocardiography in 19 patients with myelofibrosis, 30 patients with aplastic anaemia and 82 patients with chronic myelogenous leukaemia. They found a higher level of estimated RVSP in patients with myelofibrosis when compared with the other patients [15].
Unpublished data from our group at the Carmel Medical Center (Haifa, Israel) showed that 22 out of 49 patients had PH, as determined by a RVSP>35 mmHg (mean 55.23±12.29 mmHg) in an echocardiographic study. In 13 out of the 22 patients, the elevated pulmonary artery pressure related to heart disease. No obvious reason for the increased pulmonary artery pressure was found in only nine (18.4%) out of the 49 patients. None of the clinical characteristics of the patients was able to identify those at risk for the development of PH. A recent, larger study by Chebrek et al. [16] evaluated 103 patients with CMPDs (including 32 patients with CML, 27 patients with essential thrombocytosis and 15 patients with myelofibrosis) and found rather a low prevalence of PH. Only five patients were found to have increased pulmonary artery pressure (<5%). Again, PH in this study was defined by echocardiography (RVSP >35 mmHg) [16].
Increased pulmonary artery pressure in patients with CMPDs may result from various mechanisms including anaemia, and a hypermetabolic state with high cardiac output and left ventricular dysfunction. Therefore, transthoracic Doppler echocardiography can only be used as a screening tool and may overestimate the prevalence of PH. This implies that a right heart study with full haemodynamic evaluation is mandatory for the correct diagnosis of PH [17–19].
Three major distinct clinical forms of PH have been described in patients with CMPDs: chronic thromboembolic PH (CTEPH), precapillary PH and drug-induced PH. Although a thrombophilic state is common in CMPDs, the clinical data on CTEPH and CMPDs is scarce. A previous clinical series described six patients with CTEPH (five presented with polycythaemia vera and one with essential thrombocytosis) [20]. Interestingly the diagnosis of CTEPH and CMPD was made simultaneously in all patients, suggesting that CTEPH could be the first manifestation of myeloproliferative disease. By contrast, precapillary PH associated with CMPD is diagnosed late in the course of the disease [20–22]. In the report by Dingli et al. [20], precapillary PH was diagnosed on average 8 years after recognition of the myeloproliferative disorder (range: 0–26 years); while in the study by Guilpain et al. [21], precapillary PH occurred later in the evolution of the CMPDs, at a median of 162 months (13.5 years), and was associated with myeloid metaplasia.
Chronic thromboembolic pulmonary hypertension
Aetiology
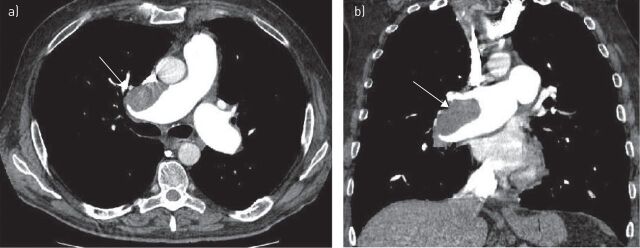
CMPDs, particularly polycythaemia vera and essential thrombocytosis, are characterised by a thrombophilic state, which may lead to microcirculatory disturbances, and arterial and venous thrombosis [23] (fig. 1). In polycythaemia vera the majority of the thrombotic events are arterial, in fact only about one third correspond to venous thrombosis, while in essential thrombocytosis there is a predominance of the arterial ones [24].
FIGURE 1.
Contrast enhanced computed tomography of a mural thrombus in the main pulmonary artery trunk (arrow) in a patient with chronic thromboembolic pulmonary hypertension. a) Coronal view and b) axial view.
Unfortunately the incidence of thrombosis in polycythaemia vera and essential thrombocytosis has been difficult to establish; however, at presentation the reported incidence of thrombosis in essential thrombocytosis and polycythaemia vera varied from 11% to 25% and from 12% to 39%, respectively [23–27]. More recent series tend to describe lower incidence figures that are probably a result of both a lead time bias in diagnosis and improved therapy. The incidence of thrombotic events during follow up remains substantial. Cortelazzo et al. [28] reported that the overall risk of thrombosis in essential thrombocytosis was 6.6% per patient-year versus 1.2% per patient-year in a controlled population. The risk factors for thrombotic events include elevated red blood cell counts, higher haemoglobin levels, an increased percentage of nucleated neutrophils at the time of diagnosis, older age and a history of thrombosis.
The pathogenesis of thrombotic events in these diseases is multifactorial. Increased blood hyperviscosity, due to high haematocrit values in polycythaemia vera, causes a major disturbance to blood flow, increasing platelet activation and platelet–platelet interactions with an higher risk of thrombosis [29]. In addition, the formation of red blood cell aggregates, induced by the red blood cell abnormalities occurring in polycythaemia vera and essential thrombocytosis, directly contribute to flow disturbance, thrombosis and platelet activation, especially in small vessels [23, 30, 31].
Erythropoietin-independent erythroid colony (EEC) formation, which is considered to be among the criteria for polycythaemia vera diagnosis, is also considered to be a surrogate marker for increased thrombotic risk. Spontaneous EEC formation may be associated with thrombosis, particularly of hepatic veins, in the absence of other peripheral blood abnormalities. The presence of EEC formation leads to the diagnosis of a primary myeloproliferative disorder in 78% of cases with apparent idiopathic Budd–Chiari syndrome and in about half of patients with portal, splenic and/or mesenteric venous thrombosis [32, 33]. It seems that the EEC formation test might be of interest in order to unmask as yet unrecognised CMPDs in CTEPH patients. The platelet count per se has not been significantly correlated with thrombosis risk in either polycythaemia vera or essential thrombocytosis. However, in high-risk patients, lowering the platelet count to below 400×109 L−1 might reduce the incidence of thrombotic events [23, 25, 34, 35].
Patients with CMPDs manifest abnormal in vivo platelet activation with resultant granule release and shortened platelet survival [24]. In polycythaemia vera associated with thrombocythaemia, hyperviscosity aggravates the platelet-mediated microvascular disturbances of thrombocythaemia and may cause major arterial and venous thrombotic complications. Thrombocythaemia persists even after correction of hyperviscosity by phlebotomy [23, 36]. However, no correlation was found in other studies between the degree of thrombocytosis, the presence of platelet dysfunction and the risk of thrombosis in polycythaemia vera [26, 35].
As they are disorders of haematopoietic stem cells, the potential role of clonal leukocytes in the pathogenesis of thrombosis in polycythaemia vera and essential thrombocytosis is supported by several studies and would be consistent with the well-established anti-thrombotic effect of myelosuppressive therapy. An ongoing state of polymorphonuclear leukocyte (PMN) activation, related to increased plasma level markers of clotting activation, has been demonstrated [23, 27, 37].
The presence of the acquired gain-of-function V617F mutation in the tyrosine kinase JAK2 gene has been demonstrated in PMNs and platelets of patients with CMPDs [37, 38]. Furthermore, patients affected by essential thrombocytosis harbouring a JAK2 mutation show a “polycythaemia vera-like” phenotype with an increased rate of venous thrombosis [39]. In addition, the association between JAK2 mutation and thrombosis at uncommon sites with no relation to the CMPD has been described in several studies. Patients with the JAK2 mutation have increased PMN activation, with platelet aggregation and activation, contributing to the increase in the susceptibility to thrombotic events in patients with CMPDs [23, 40, 41].
Splenectomy is considered a risk factor for the development of CTEPH. Thromboembolic complications following splenectomy for haematological diseases occur in up to 10% of patients and may range from portal vein thrombosis to pulmonary embolism and deep vein thrombosis [42–44]. However, Bonderman et al. [45] conducted a prospective case–control study of 109 patients and did not find any relationship between splenectomy and CTEPH.
Thrombocytosis per se, following splenectomy, is not thought to be the major factor predisposing patients to thrombosis. Loss of the filtering function of the spleen, which allows abnormal red cells to remain in the peripheral circulation, may lead to activation of the coagulation system.
A worsening extramedullary haematopoiesis is seen in patients with CMPDs after splenectomy, with the potential for pulmonary infiltration. In addition, the functional abnormal platelets in CMPDs, together with the marked elevations in their counts, may explain the difference in the interval before the development of PH, which is shorter in patients with CMPDs [23]. In a case series of 10 patients with CMPDs and PH, the platelet count was not different between patients with CTEPH and pulmonary arterial hypertension (PAH) associated with CMPDs [21]. Elevated haematocrit was significantly associated with CTEPH compared with the four patients with precapillary PH, suggesting that elevated haematocrit may contribute to the development of pulmonary artery thrombosis. Interestingly, none of the patients with CTEPH had undergone a splenectomy.
Treatment
The management of arterial and venous thrombosis in polycythaemia vera and essential thrombocytosis patients should be the same as that recommended in the general population [46, 47].
Pulmonary endarterectomy is the first choice treatment in patients with CTEPH [47]. However, in inoperable cases, due to a personal choice, the anatomic distribution of their disease, the extent of their disease or their comorbidities, medical therapy including diuretics, anticoagulants and specific PAH therapy should be considered. Several small studies in patients with CTEPH have shown that the endothelin receptor antagonists, particularly oral bosentan, improve symptoms and exercise capacity [48]. In the only randomised placebo-controlled trial (BENEFIT trial), 157 patients (WHO functional class II–IV, mild to severe disease) with inoperable CTEPH (or persistent CTEPH after thromboendarterectomy) were randomly assigned to receive oral placebo or bosentan for 16 weeks. Compared with placebo, bosentan therapy was associated with improved pulmonary vascular resistance and cardiac index. However, bosentan therapy did not improve exercise capacity in this population [49].
Recently, in patients with inoperable CTEPH (WHO functional class II–III, mild to moderate disease) riociguat, a guanylate cyclase stimulator, was shown to improve exercise capacity and pulmonary haemodynamics [50]. In a multicentre, randomised placebo-controlled trial of 261 patients with either inoperable CTEPH (189 patients) or persistent PH (72 patients) following pulmonary thromboendarterectomy (CHEST-1 trial) riociguat improved 6-min walking distance and pulmonary vascular resistance [51]. Currently, no data specific to CTEPH-associated with CMPDs are available.
Hydroxyurea has been found to reduce the risk of thrombosis in high risk patients [23], possibly due to its effect on leukocyte count and leukocyte activation [52]. For this reason cytoreductive therapy with hydroxyurea is recommended [53, 54]. The effectiveness of antiplatelet agents in reducing the incidence of vascular events is of value in patients with polycythaemia vera [54], while the use of aspirin in essential thrombocytosis is controversial and there is a potential increased risk of bleeding [23, 56].
Precapillary pulmonary hypertension
Aetiology
Precapillary PH in patients affected by CMPDs may be caused by several factors. First, portal hypertension, a well-known complication of myeloid metaplasia with myelofibrosis, may cause PAH [57, 58]. However, although portal hypertension is seen in up to 17% of patients with myeloid metaplasia and myelofibrosis, the coexistence of both PH and portal hypertension is rare [20, 21].
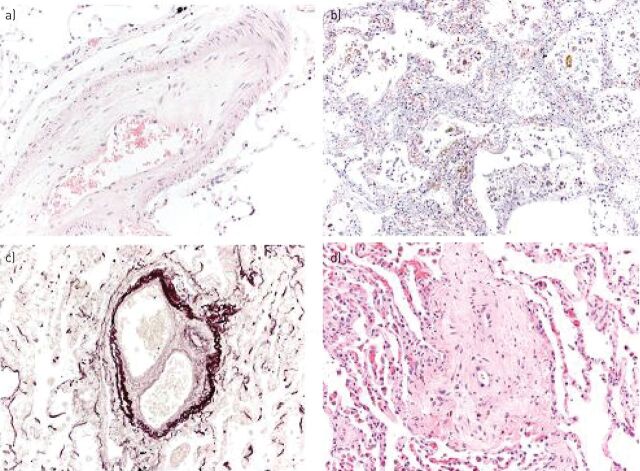
Another cause of PH during cytotoxic chemotherapy and haematopoietic stem cell transplantation is pulmonary veno-occlusive disease (fig. 2) [59]. Willems et al. [60] have described a case of veno-occlusive disease, diagnosed by means of a biopsy, as a cause of severe PH in a patient suffering from a CMPD. In this case, the use of anagrelide several weeks before the manifestation of the symptoms may suggest this treatment has a role in the pathogenesis of a pulmonary veno-occlusive disease. Moreover, in six patients with CMPDs and echocardiographic findings of PH [61], the presence of clinical signs, such as the presence of low oxygen saturation at rest and a low diffusing capacity of the lung for carbon monoxide, as well as radiological manifestations, such as centrilobular ground-glass opacities, septal lines and lymph node enlargement on high-resolution computed tomography of the chest, suggested the diagnosis of pulmonary veno-occlusive disease with a high probability. However, the diagnosis of pulmonary veno-occlusive disease was achieved late in the course of the disease with a poor prognosis [62].
FIGURE 2.
a) Pulmonary veno-occlusive disease (PVOD) with partial thrombotic occlusion of the lumen of a medium-sized vein (haematoxylin and eosin stain, 200× original magnification). b) An area simulating a capillary haemangiomatosis in a patient with PVOD, showing capillary proliferation with interstitial thickening and hemosiderin deposits (haematoxylin and eosin stain, 200× original magnification). c) Thrombotic occlusion of medium-sized veins (Weigert's elastic stain 100×). d) Almost complete thrombotic occlusion of the lumen of a small vein (haematoxylin and eosin stain, 200× original magnification). Figure courtesy of Dr. A. Cavazza (Unit of Pathology, IRCCS-Arcispedale S. Maria Nuova di Reggio Emilia, Reggio Emilia, Italy).
Another explanation for the pathogenesis of PH during the course of a myeloproliferative disorder may be the presence of a tumour microembolism, as found in various tumours. In patients affected by progressive myeloproliferative syndrome, translocation of megakaryocytes from the bone marrow, spleen or liver to the lungs may produce megakaryocyte embolism of pulmonary vessels, eventually leading to PH [63]. In fact, an increase in circulating megakaryocytes and myeloid progenitor cells, which are poorly deformable and larger than the alveolar capillary diameter, was observed in myelofibrosis and myeloid metaplasia. As a consequence, these cells may occlude the pulmonary microvasculature and secrete vasoactive cytokines, leading to the development of PH. The case of a patient with myeloid metaplasia, PH and right heart failure, with thrombocytosis and circulating megakaryocytes after splenectomy has been described [64]. The obstruction caused by megakaryocytes with stasis and secondary microthrombosis was thought to lead to the PH. Furthermore, many cases of CMPDs and PH have been described. Histological examination of the lung showed the presence of an obstruction of the small vessels by conglomerates of megakaryocytes [62, 63, 65].
A causal relationship between pulmonary myeloid infiltration during the chronic phase of agnogenic myeloid metaplasia and leukaemic infiltration during the acute transformation of the disease and the development of PH has been suggested. Steensma et al. [66] described four patients with myelofibrosis with myeloid metaplasia who developed severe PH. Technetium-99m sulfur colloid scintigraphy demonstrated diffuse pulmonary uptake, showing extramedullary haematopoiesis. Furthermore, in another case report an open lung biopsy demonstrated the presence of extramedullary haematopoiesis in an elderly woman with myelofibrosis and PH [67].
Although no clear association was found between platelet count and the risk of thrombosis, a correlation between elevated pulmonary artery pressure and platelet count was reported in patients with myeloid metaplasia and essential thrombocytosis, and with haemoglobin levels in patients with polycythaemia vera. Platelets seem to play a central role in the aetiology of PH; in fact, platelet-derived growth factor released from activated platelets is a strong stimulus for smooth muscle hyperplasia [68, 69] and in an animal model of PH the control of the platelet count delays the development of PH [70].
Marvin and Spellberg [64] reported that cytoreductive therapy, by decreasing the platelet count, reversed PH and right heart failure in a 72-year-old patient with myeloid metaplasia; however, the effect of the cytoreductive therapy may have been related to its effect on white blood cells. In a study by Dingli et al. [20], 12 out of 26 patients were treated with aspirin before PH was diagnosed suggesting that antiaggregant agents, as opposed to cytoreductive therapy, probably have no effect in preventing or reversing PH.
Finally, a possible pathogenic link between CMPDs and PH has been found in the peripheral blood and bone marrow, because of an enhanced angiogenesis. In this study, patients with primary myelofibrosis and PH had higher bone marrow microvessel density and vascular endothelial growth factor levels, suggesting the presence of a pro-angiogenic phenomenon [14, 71]. Other studies demonstrated that distinctive features of myelofibrosis associated with PH include normal or low circulating CD34 cell count, polyclonal platelets and granulocytes, the absence of peripheral blood dacrocytes and the JAK2 1849G>T(V617F) mutation [72, 73].
Treatment
Currently there is no effective treatment for PH associated with CMPDs. Cytoreductive therapy may have a role but the evidence is anecdotal. A previous study reported that, despite good CMPD control, there was no improvement in PH over time [20], while another case study described reversibility of PH with cytoreductive therapy and reduction of platelet counts, or due to therapeutic phlebotomies [64].
A treatment trial using whole-lung low-dose external beam radiotherapy has been suggested for patients with CMPDs and PH and evidence of extramedullar myelofibrosis as a palliative measure [66, 67]. There is no data on the role of anticoagulation and antiaggregants in patients with precapillary PH associated with CMPDs.
Dysregulation of JAK family kinases, specifically JAK1 and JAK2, contributes to the pathogenesis of myelofibrosis. Ruxolitinib, an oral JAK1/JAK2 inhibitor, is used for the treatment of intermediate-to-high risk myelofibrosis patients. Tabarroki et al. [74] described 15 patients with myelofibrosis and PH treated with ruxolitinib, in 66% of the patients an improvement of pulmonary artery pressure and right ventricle function measured by echocardiography was observed. Furthermore, ruxolitinib also decreased plasma levels of N-terminal pro-brain natriuretic peptide, von Willebrand antigen, ristocetin-cofactor activity and uric acid, and increased nitric oxide levels. This study suggests that aberrant JAK signal transducer and activator of transcription signalling in myelofibrosis may mediate PH through dysregulation of nitric oxide and cytokine levels, which can be restored by therapy with JAK inhibitors [74].
However, recently an association between worsening PAH and ruxolitinib, with improvement on withdrawal of the drug on two separate occasions, has been described in a 57-year-old woman with progressive myelofibrosis, testing positive for the JAK2 V617F mutation [75].
The effectiveness of pulmonary vasodilators used for PAH, including endothelin receptor antagonists, prostacyclin analogues and phosphodiesterase-type 5 inhibitors, should be further studied.
Drug-induced PH
Tyrosine kinase inhibitors (TKIs), such as imatinib, dasatinib and nilotinib, have recently being used as a therapy for CML with improved prognosis. Although TKIs are usually well tolerated, these agents are nevertheless associated with certain systemic side-effects such as oedema, musculoskeletal pain, diarrhoea, rash and cardiac toxicity, especially with imatinib. Pulmonary complications and specifically pleural effusions have been reported more frequently with dasatinib.
Several case reports have suggested that PH may be a potential specific complication of dasatinib use [76, 77]. The evaluation of the French registry data suggests that the lowest estimated incidence of dasatinib-associated PAH is 0.45% and dasatinib is considered a probable cause of PAH in the last updated PH classification [78]. Symptoms generally appear after 8–48 months of therapy and reported mean pulmonary artery pressures by right heart catheterization are 25–50 mmHg. Although a few patients have experienced full clinical and haemodynamic recovery, the majority have not recovered completely after a follow-up that ranges from 3 to 36 months (median 9 months) [76–78]. Montani et al. [78] described subsequent administration of an endothelin receptor antagonist in two patients and a calcium channel blocker to a third patient; it is not clear whether any subsequent improvement was related to these therapies, dasatinib discontinuation, or both.
No other PH cases were reported with the use of other TKIs at the time of PH diagnosis. Interestingly, clinical and haemodynamic improvements have been reported with imatinib therapy in two patients with CML and coexistent severe precapillary PH. It was suggested that this effect could be due to inhibition of tyrosine kinase targets of imatinib such as platelet-derived growth factor receptors and c-kit. In those patients with PH probably induced by dasatinib, clinical, functional and haemodynamic improvements were observed within 4 months of dasatinib discontinuation in all but one patient. However, after a median follow-up of 9 months, most patients did not demonstrate complete recovery and two patients died [78].
Prognosis
The prognosis of patients with precapillary PH associated with CMPDs is poor [21–23]. Precapillary PH occurs late in the course of the disease and the median survival is up to several months after diagnosis. In the study by Dingli et al. [20], the median survival time was 18 months and death was mainly related to cardiopulmonary failure. Garcia-Manero et al. [22] reported that the interval between the development of dyspnoea (leading to the diagnosis of PH) and death was <7 months in five out of six patients. In patients with CTEPH, pulmonary endarterectomy, if suitable, may reverse PH and improve prognosis. Data about the use of specific therapies in this group of patients are still not available.
Conclusion
To sum up, the exact incidence and prevalence of PH in patients with CMPDs is poorly defined. Three distinct clinical forms of PH have been described in patients with CMPDs: CTEPH, precapillary PH and drug-induced PAH. Precapillary PH is usually diagnosed late in the course of the haematological disease, while CTEPH is usually diagnosed earlier and may even be concurrent with the haematological diagnosis. Dasatinib, which is used for the treatment of CML, is considered to be a probable cause of PAH. High haematocrit levels with hyperviscosity, thrombocytosis and splenectomy may contribute, among other mechanisms, to the increased rate of thrombotic events in patients with CMPDs, especially polycythaemia vera. PAH-like disease associated with CMPD was found to be related to myeloid metaplasia, suggesting that pulmonary myeloid infiltration and pulmonary capillary obstruction by megakaryocytes with stasis and secondary microthrombosis may contribute to the pulmonary vascular disease. When PH is diagnosed, secondary causes which may contribute to the elevated pulmonary pressure, such as anaemia and heart failure, should be recognised and treated. However, when PH persists, treatment is not yet established. Anticoagulant drugs should be administered carefully because of the potential risk of haemorrhagic complications. Cytoreductive treatment should be used in association with symptomatic treatment of PH, such as oxygen and diuretics. There are no data on the effectiveness of specific PAH therapies in these patients and randomised control trials are needed. The prognosis of PH associated with CMPDs remains poor. However, pulmonary endarterectomy is the treatment of choice in eligible patients with proximal CTEPH.
Supplementary Material
Footnotes
Conflict of interest: Disclosures can be found alongside the online version of this article at err.ersjournals.com
Provenance: Publication of this peer-reviewed article was sponsored by F. Hoffman-La Roche Ltd, Basel, Switzerland (principal sponsor, European Respiratory Review issue 137).
References
- 1.Rubin LJ. Primary pulmonary hypertension. N Engl J Med 1997; 336: 111–117. [DOI] [PubMed] [Google Scholar]
- 2.Simonneau G, Galie N, Rubin LJ, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol 2004; 43: Suppl. S, S5–S12. [DOI] [PubMed] [Google Scholar]
- 3.McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol 2009; 53: 1573–1619. [DOI] [PubMed] [Google Scholar]
- 4.Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2013; 62: Suppl., D34–D41. [DOI] [PubMed] [Google Scholar]
- 5.Swerdlow SH, Campo E, Harris NL, et al. , eds. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th Edn. Geneva, WHO, 2008. [Google Scholar]
- 6.Groffen J, Stephenson JR, Heisterkamp N, et al. Philadelphia chromosomal breakpoints are clustered within a limited region, bcr, on chromosome 22. Cell 1984; 36: 93–99. [DOI] [PubMed] [Google Scholar]
- 7.Kralovics R, Passamonti F, Buser AS, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 2005; 352: 1779–1790. [DOI] [PubMed] [Google Scholar]
- 8.Hellmann A. Myeloproliferative syndromes: diagnosis and therapeutic options. Pol Arch Med WeWn 2008; 118: 756–760. [PubMed] [Google Scholar]
- 9.Levine RL, Gilliland DG. Myeloproliferative disorders. Blood 2008; 112: 2190–2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reisner SA, Rinkevich D, Markiewicz W, et al. Cardiac involvement in patients with myeloproliferative disorders. Am J Med 1992; 93: 498–504. [DOI] [PubMed] [Google Scholar]
- 11.Garypidou V, Vakalopoulou S, Dimitriadis D, et al. Incidence of pulmonary hypertension in patients with chronic myeloproliferative disorders. Haematologica 2004; 89: 245–246. [PubMed] [Google Scholar]
- 12.Altintas A, Karahan Z, Pasa S, et al. Pulmonary hypertension in patients with essential thrombocythemia and reactive thrombocytosis. Leuk Lymphoma 2007; 48: 1981–1987. [DOI] [PubMed] [Google Scholar]
- 13.Gupta R, Perumandla S, Patsiornik Y, et al. Incidence of pulmonary hypertension in patients with chronic myeloproliferative disorders. J Natl Med Assoc 2006; 98: 1779–1782. [PMC free article] [PubMed] [Google Scholar]
- 14.Cortelezzi A, Gritti G, Del Papa N, et al. Pulmonary arterial hypertension in primary myelofibrosis is common and associated with an altered angiogenic status. Leukemia 2008; 22: 646–649. [DOI] [PubMed] [Google Scholar]
- 15.Roach EC, Park MM, Tang WH, et al. Impaired right ventricular-pulmonary vascular funcition in myeloproliferative neoplasm. J Heart Lung Transplant 2015; 34: 390–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chebrek S, Aïssi K, Francès Y, et al. Pulmonary hypertension in patients with chronic myeloproliferative neoplasm. Leuk Lymphoma 2014; 55: 223–225. [DOI] [PubMed] [Google Scholar]
- 17.Galiè N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2009; 34: 1219–1263. [DOI] [PubMed] [Google Scholar]
- 18.Galiè N, Hoeper MM, Humbert M, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: The Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J 2009; 30: 2493–2537. [DOI] [PubMed] [Google Scholar]
- 19.Hoeper MM, Bogaard HJ, Condliffe R, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol 2013; 62: Suppl., D42–D50. [DOI] [PubMed] [Google Scholar]
- 20.Dingli D, Utz JP, Krowka MJ, et al. Unexplained pulmonary hypertension in chronic myeloproliferative disorders. Chest 2001; 120: 801–808. [DOI] [PubMed] [Google Scholar]
- 21.Guilpain P, Montani D, Damaj G, et al. Pulmonary hypertension associated with myeloproliferative disorders: a retrospective study of ten cases. Respiration 2008; 76: 295–302. [DOI] [PubMed] [Google Scholar]
- 22.Garcia-Manero G, Schuster SJ, Patrick H, et al. Pulmonary hypertension in patients with myelofibrosis secondary to myeloproliferative diseases. Am J Hematol 1999; 60: 130–135. [DOI] [PubMed] [Google Scholar]
- 23.Landolfi R, Di Gennaro L, Falanga A. Thrombosis in myeloproliferative disorders: pathogenetic facts and speculation. Leukemia 2008; 22: 2020–2028. [DOI] [PubMed] [Google Scholar]
- 24.Marchioli R, Finazzi G, Landolfi R, et al. Vascular and neoplastic risk in a large cohort of patients with polycythemia vera. J Clin Oncol 2005; 23: 2224–2232. [DOI] [PubMed] [Google Scholar]
- 25.Jensen MK, de Nully Brown P, Nielsen OJ, et al. Incidence, clinical features and outcome of essential thrombocythaemia in well defined geographical area. Eur J Hematol 2000; 65: 132–139. [DOI] [PubMed] [Google Scholar]
- 26.Ziakas PD, Voulgarelis M, Felekouras E, et al. Myelofibrosis-associated massive splenomegaly. a cause of increased intra-abdominal pressure, pulmonary hypertension, and positional dyspnea. Am J Hematol 2005; 80: 128–132. [DOI] [PubMed] [Google Scholar]
- 27.Wolanskyj AP, Schwager SM, McClure RF, et al. Essential thrombocythemia beyond the first decade: life expectancy, long-term complication rates, and prognostic factors. Mayo Clin Proc 2006; 81: 159–166. [DOI] [PubMed] [Google Scholar]
- 28.Cortelazzo S, Viero P, Finazzi G, et al. Incidence and risk factors for thrombotic complications in a historical cohort of 100 patients with essential thrombocythemia. J Clin Oncol 1990; 8: 556–562. [DOI] [PubMed] [Google Scholar]
- 29.Kwaan HC, Wang J. Hyperviscosity in polycythemia vera and other red cell abnormalities. Semin Thromb Hemost 2003; 29: 451–458. [DOI] [PubMed] [Google Scholar]
- 30.Turitto VT, Weiss HJ. Platelet and red cell involvement in mural thrombogenesis. Ann NY Acad Sci 1983; 416: 363–376. [DOI] [PubMed] [Google Scholar]
- 31.Huang PY, Hellums JD. Aggregation and disaggregation kinetics of human blood platelets: part III. The disaggregation under shear stress of platelet aggregates. Biophys J 1993; 65: 354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Valla D, Casadevall N, Lacombe C, et al. Primary myeloproliferative disorder and hepatic vein thrombosis. A prospective study of erythroid colony formation in vitro in 20 patients with Budd–Chiari syndrome. Ann Intern Med 1985; 103: 329–334. [DOI] [PubMed] [Google Scholar]
- 33.De Stefano V, Teofili L, Leone G, et al. Spontaneous erythroid colony formation as the clue to an underlying myeloproliferative disorder in patients with Budd-Chiari syndrome or portal vein thrombosis. Semin Thromb Haemost 1997; 23: 411–418. [DOI] [PubMed] [Google Scholar]
- 34.Michiels JJ, Berneman Z, Bockstaele DV, et al. Clinical and laboratory features, pathology of platelet-mediated thrombosis and bleeding complications and the molecular etiology of essential thrombocythemia and polycythemia vera: therapeutic implications. Semin Thromb Hemost 2006; 32: 174–207. [DOI] [PubMed] [Google Scholar]
- 35.Buss DH, Stuart JJ, Lipscomb GE. The incidence of thrombotic and hemorrhagic disorders in association with extreme thrombocytosis: an analysis of 129 cases. Am J Hematol 1985; 20: 365–372. [DOI] [PubMed] [Google Scholar]
- 36.Landolfi R, Ciabattoni G, Patrignani P, et al. Increased thromboxane biosynthesis in patients with polycythemia vera: evidence for aspirin-suppressible platelet activation in vivo. Blood 1992; 80: 1965–1971. [PubMed] [Google Scholar]
- 37.Carobbio A, Finazzi G, Guerini V, et al. Leukocytosis is a risk factor for thrombosis in essential thrombocythemia: interaction with treatment, standard risk factors and Jak2 mutation status. Blood 2007; 109: 2310–2313. [DOI] [PubMed] [Google Scholar]
- 38.Baxter EJ, Scott LM, Campbell PJ, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 2005; 365: 1054–1061. [DOI] [PubMed] [Google Scholar]
- 39.Campbell PJ, Scott LM, Buck G, et al. Definition of subtypes of essential thrombocythaemia and relation to polycythaemia vera based on JAK2 V617F mutation status: a prospective study. Lancet 2005; 366: 1945–1953. [DOI] [PubMed] [Google Scholar]
- 40.Arellano-Rodrigo E, Alvarez-Larran A, Reverter JC, et al. Increased platelet and leukocyte activation as contributing mechanisms for thrombosis in essential thrombocythemia and correlation with the JAK2 mutational status. Haematologica 2006; 91: 169–175. [PubMed] [Google Scholar]
- 41.Falanga A, Marchetti M, Vignoli A, et al. V617F JAK-2 mutation in patients with essential thrombocythemia: relation to platelet, granulocyte, and plasma hemostatic and inflammatory molecules. Exp Hematol 2007; 35: 702–711. [DOI] [PubMed] [Google Scholar]
- 42.Mohren M, Markmann I, Dworschak U, et al. Thromboembolic complications after splenectomy for hematologic diseases. Am J Hematol 2004; 76: 143–147. [DOI] [PubMed] [Google Scholar]
- 43.Chaffanjon PC, Brichon PY, Ranchoup Y, et al. Portal vein thrombosis following splenectomy for hematologic disease: prospective study with Doppler color flow imaging. World J Surg 1998; 22: 1082–1086. [DOI] [PubMed] [Google Scholar]
- 44.Van't riet M, Burger JW, Van Muiswinkel JM, et al. Diagnosis and treatment of portal vein thrombosis following splenectomy. Br J Surg 2000; 87: 1229–1233. [DOI] [PubMed] [Google Scholar]
- 45.Bonderman D, Wilkens H, Wakounig S, et al. Risk factors for chronic thromboembolic pulmonary hypertension. Eur Respir J 2009; 33: 325–331. [DOI] [PubMed] [Google Scholar]
- 46.Fedullo P, Kerr KM, Kim NH, et al. Chronic thromboembolic pulmonary hypertension. Am J Respir Crit Care Med 2011; 183: 1605–1613. [DOI] [PubMed] [Google Scholar]
- 47.Piazza G, Goldhaber SZ. Chronic thromboembolic pulmonary hypertension. N Engl J Med 2011; 364: 351–360. [DOI] [PubMed] [Google Scholar]
- 48.Hughes RJ, Jais X, Bonderman D, et al. The efficacy of bosentan in inoperable chronic thromboembolic pulmonary hypertension: a 1-year follow-up study. Eur Respir J 2006; 28: 138–143. [DOI] [PubMed] [Google Scholar]
- 49.Jaïs X, D'Armini AM, Jansa P, et al. Bosentan for treatment of inoperable chronic thromboembolic pulmonary hypertension: BENEFiT (Bosentan Effects in iNopErable Forms of chronIc Thromboembolic pulmonary hypertension), a randomized, placebo-controlled trial. J Am Coll Cardiol 2008; 52: 2127–2134. [DOI] [PubMed] [Google Scholar]
- 50.Ghofrani HA, Hoeper MM, Halank M, et al. Riociguat for chronic thromboembolic pulmonary hypertension and pulmonary arterial hypertension: a phase II study. Eur Respir J 2010; 36: 792–799. [DOI] [PubMed] [Google Scholar]
- 51.Ghofrani HA, D'Armini AM, Grimminger F, et al. Riociguat for the treatment of chronic thromboembolic pulmonary hypertension. N Engl J Med 2013; 369: 319–329. [DOI] [PubMed] [Google Scholar]
- 52.Maugeri N, Giordano G, Petrilli MP, et al. Inhibition of tissue factor expression by hydroxyurea in polymorphonuclear leukocytes from patients with myeloproliferative disorders: a new effect for an old drug? J Thromb Haemost 2006; 4: 2593–2598. [DOI] [PubMed] [Google Scholar]
- 53.Cortelazzo S, Finazzi G, Ruggeri M, et al. Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N Engl J Med 1995; 332: 1132–1136. [DOI] [PubMed] [Google Scholar]
- 54.Fruchtman SM, Mack K, Kaplan ME, et al. From efficacy to safety: a polycythemia vera study group report on hydroxyurea in patients with polycythemia vera. Semin Hematol 1997; 34: 17–23. [PubMed] [Google Scholar]
- 55.Landolfi R, Marchioli R, Kutti J, et al. Efficacy and safety of low dose aspirin in polycythemia vera. N Engl J Med 2004; 350: 114–124. [DOI] [PubMed] [Google Scholar]
- 56.Van Genderen PJ, Mulder PG, Waleboer M, et al. Prevention and treatment of thrombotic complications in essential thrombocythaemia: efficacy and safety of aspirin. Br J Haematol 1997; 97: 179–184. [DOI] [PubMed] [Google Scholar]
- 57.Ito H, Adachi Y, Arimura Y, et al. A 25-year clinical history of portopulmonary hypertension associated with latent myeloproliferative disorder . J Gastroenterol 2003; 38: 488–492. [DOI] [PubMed] [Google Scholar]
- 58.Tefferi A. Myelofibrosis with myeloid metaplasia. N Engl J Med 2000; 342: 1255–1265. [DOI] [PubMed] [Google Scholar]
- 59.Montani D, Price LC, Dorfmuller P, et al. Pulmonary veno-occlusive disease. Eur Respir J 2009; 33: 189–200. [DOI] [PubMed] [Google Scholar]
- 60.Willems E, Canivet JL, Ghaye B, et al. Pulmonary veno-occlusive disease in myeloproliferative disorder. Eur Respir J 2009; 33: 213–216. [DOI] [PubMed] [Google Scholar]
- 61.Adir Y, Yigla M, Amir O, et al. Pulmonary hypertension associated with myeloproliferative disorders suggesting pulmonary veno-occlusive disease: a retrospective study of six cases. Eur Respir J 2009; 34: Suppl. 53, 319s. [Google Scholar]
- 62.Hill G, McClean D, Fraser R, et al. Pulmonary hypertension as a consequence of alveolar capillary plugging by malignant megakaryocytes in essential thrombocythaemia. Aust NZ J Med 1996; 26: 852–853. [DOI] [PubMed] [Google Scholar]
- 63.Dot JM, Sztrymf B, Yaïci A, et al. Hypertension arterielle pulmonaire postembolique tumorale [Pulmonary arterial hypertension due to tumor emboli]. Rev Mal Respir 2007; 24: 359–366. [DOI] [PubMed] [Google Scholar]
- 64.Marvin KS, Spellberg RD. Pulmonary hypertension secondary to thrombocytosis in a patient with myeloid metaplasia. Chest 1993; 103: 642–644. [DOI] [PubMed] [Google Scholar]
- 65.Halank M, Marx C, Baretton G, et al. Severe pulmonary hypertension in chronic idiopathic myelofibrosis. Onkologie 2004; 27: 472–474. [DOI] [PubMed] [Google Scholar]
- 66.Steensma DP, Hook CC, Stafford SL, et al. Low-dose, singlefraction, whole-lung radiotherapy for pulmonary hypertension associated with myelofibrosis with myeloid metaplasia. Br J Haematol 2002; 118: 813–816. [DOI] [PubMed] [Google Scholar]
- 67.Weinschenker P, Kutner JM, Salvajoli JV, et al. Whole-pulmonary low-dose radiation therapy in agnogenic myeloid metaplasia with diffuse lung involvement. Am J Hematol 2002; 69: 277–280. [DOI] [PubMed] [Google Scholar]
- 68.Neville RF, Sidawy AN. Myointimal hyperplasia: basic science and clinical considerations. Semin Vasc Surg 1998; 11: 142–148. [PubMed] [Google Scholar]
- 69.Perros F, Montani D, Dorfmüller P, et al. Platelet-derived growth factor expression and function in idiopathic pulmonary arterial hypertension. Am J Respir Crit Care Med 2008; 178: 81–88. [DOI] [PubMed] [Google Scholar]
- 70.White SM, Wagner JG, Roth RA. Effects of altered platelet number on pulmonary hypertension and platelet sequestration in monocrotaline pyrrole-treated rats. Toxicol Appl Pharmacol 1989; 99: 302–313. [DOI] [PubMed] [Google Scholar]
- 71.Zetterberg E, Popat U, Hasselbalch H, et al. Angiogenesis in pulmonary hypertension with myelofibrosis. Haematologica 2008; 93: 945–946. [DOI] [PubMed] [Google Scholar]
- 72.Popat U, Frost A, Liu E, et al. High levels of circulating CD34 cells, dacrocytes, clonal hematopoiesis, and JAK2 mutation differentiate myelofibrosis with myeloid metaplasia from secondary myelofibrosis associated with pulmonary hypertension. Blood 2006; 107: 3486–3488. [DOI] [PubMed] [Google Scholar]
- 73.Fadini GP, Schiavon M, Cantini M, et al. Circulating CD34+ cells, pulmonary hypertension, and myelofibrosis. Blood 2006; 108: 1776–1777. [DOI] [PubMed] [Google Scholar]
- 74.Tabarroki A, Lindner DJ, Visconte V, et al. Ruxolitinib leads to improvement of pulmonary hypertension in patients with myelofibrosis. Leukemia 2014; 28: 1486–1493. [DOI] [PubMed] [Google Scholar]
- 75.Low AT, Howard L, Harrison C, et al. Pulmonary arterial hypertension exacerbated by ruxolitinib. Haematologica 2015; 100: e244–e245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Orlandi EM, Rocca B, Pazzano AS, et al. Reversible pulmonary arterial hypertension likely related to long-term, low-dose desatinib treatment for chronic myeloid leukemia. Leukemia Res 2012; 36: e4–e6. [DOI] [PubMed] [Google Scholar]
- 77.Dumitrescu D, Seck C, ten Freyhaus H, et al. Fully reversible pulmonary arterial hypertension associated with dasatinib treatment for chronic myeloid leukaemia. Eur Respir J 2011; 38: 218–220. [DOI] [PubMed] [Google Scholar]
- 78.Montani D, Bergot E, Günther S, et al. Pulmonary arterial hypertension in patients treated by dasatinib. Circulation 2012; 125: 2128–2137. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.