Abstract
Alcohol has been drunk for centuries and in the past also used as a medicine. Alcohol consumption in Poland and in the entire world has gradually increased, which is also nowadays accelerated by the ongoing COVID-19 pandemic. In 2020, the amount of alcohol consumed in Poland was 11.7 l per capita, which was a the highest level since 1961. It is estimated that global alcohol consumption will increase by 17% by the year 2030. There is also increasing alcohol consumption by children and adolescents, as well as pregnant women. Alcohol consumption as a health damaging factor is not always recognized in the general population. Additionally, numerous scientific societies in their guidelines/recommendations indicate that moderate doses of alcohol are beneficial or at least neutral for health. The question remains whether so-called “moderate doses of alcohol” really are not harmful to health. We analyze this issue in this article.
Keywords: alcohol consumption, risk of death, health
A brief history of alcohol
It is difficult to determine when mankind started making and consuming alcohol. It is thought that fermented drinks were consumed as early as the Late Neolithic. In the surviving texts, the first mentions of brewing and consuming beer date back to around 4000 BC from Mesopotamia. In turn, the first restrictions on alcohol consumption were introduced in Egypt. The ban on alcohol consumption was introduced in the temples to prevent theft, intoxication and various abuses. On the other hand, around 2000 BC a ban on drinking alcohol was introduced in the army of the pharaohs. The rulers were to lose several battles due to alcohol abuse by soldiers. The discoverer of the alcohol distillation process is considered to be the Arab alchemist Jābiribn Hayyān (around 721 – around 815 AD). This event took place around 800 AD and gave rise to the possibility of producing high-proof alcohols [1, 2].
In Poland, according to Gall Anonim, the first taverns appeared in the 11th century. Until the early Enlightenment, when alcohol began to be distilled in Poland, first of all beer was consumed. The beginning of alcohol abuse on a mass scale in Poland dates back to the 16th century, when the phenomenon of propination (a noble monopoly on the production and sale of alcoholic beverages) was formed and spread [1, 2]. Over the centuries, the statistics on the amount of alcohol consumed in Poland have changed. Historical data show that in the first half of the 19th century in the Kingdom of Poland, the amount of pure alcohol consumed per capita/year could reach up to 38 l [2].
The origin of the word “alcohol” is also interesting. The word alcohol comes from the Arabic “al-kuhl” which is a black powder used for cosmetic (as a powder blackening the skin around the eyes) and medical purposes. When Europeans encountered it in Andalusia, they began to apply the name to other powders and elixirs, eventually to volatile substances such as alcohol.
The gradual increase in the popularity of alcohol consumption was related to the attribution of medicinal properties to it. Aristotle of the island of Kos (439–377 BC) said that wine had sedative, analgesic, diuretic and antidiarrheic properties. Moreover, he found that the wine helped heal wounds. In the New Testament, in the parable of the Good Samaritan (Luke 10: 30-37), this hero dressed the wounds of the sick person with oil and wine. So, for centuries, until the 20th century, alcohol was used as a medicine.
Alcohol consumption in the general population (in the world and in Poland)
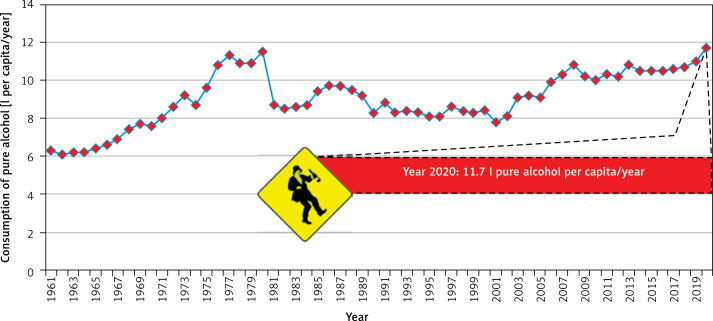
According to the data of the World Health Organization (WHO) from 2020 covering 191 countries and regions, the highest alcohol consumption was recorded in countries such as: Moldova (1st place; 17.3 l of pure alcohol per capita/year), Belarus (2nd place; 17.1 l of pure alcohol per capita/year) and Lithuania (3rd place; 16.2 l of pure alcohol per capita/year). In this ranking, Poland was 21st (11.2 l of pure alcohol per capita/year). However, these data may be understated (Figure 1: 11.2 l vs. 11.7 l of pure alcohol per capita/year).
Figure 1.
Alcohol consumption (100%) in adult population (15+) for Poland in 1961-2020. Based on: https://data.oecd.org/healthrisk/alcohol-consumption.htm and https://www.oecd.org/poland/Preventing-Harmful-Alcohol-Use-Key-Findings-POLAND.pdf
In Poland, the percentage of people who do not consume alcohol at all is changing. According to the results of a study conducted by CBOS (Public Opinion Research Center), which compared the percentage of abstainers in 2010 and 2019, it is gradually decreasing (women: 30% vs. 21%; men: 16% vs. 10% respectively) [3]. The reasons for the increase in the amount of alcohol consumed in Poland at the beginning of the 21st century are very interesting. Until the end of the 20st century, Poland, unlike the Mediterranean and Balkan countries, was one of the countries with a relatively low incidence of alcohol-related diseases [4]. In the last two decades of the 20th century, alcohol consumption in Poland was at a moderate level, i.e. 6–7 l per capita/year. These statistics resulted from the introduction of a comprehensive program limiting the health effects of alcohol consumption, which was introduced in Poland in 1982. From 2002, following the reduction of the excise duty on spirits by 30%, the return to television advertising for beer (2001) and the ongoing marketing campaign not regulated by the state since 2010, there was an increase in alcohol consumption in Poland. Changes in the structure of alcohol consumption in Poland in the years 1961–2020 are shown in Figure 1. Interestingly, in connection with the COVID-19 pandemic the alcohol industry introduced vodka in a small plastic glass for PLN 2 from 2020. The scale of the problem in Poland is shown by the sale of small bottles of vodka, commonly known as “monkeys”. Every year Poles buy 1.1 billion (3.3 million daily) “monkeys” of vodka, with 600 000 between 6 am and 12 noon [4]. The most frequently consumed alcoholic beverages in Poland include beer (39%), wine (25%) and vodka (16%) [3]. These data demonstrate that Poles drink more bottles of beer than water every year [5].
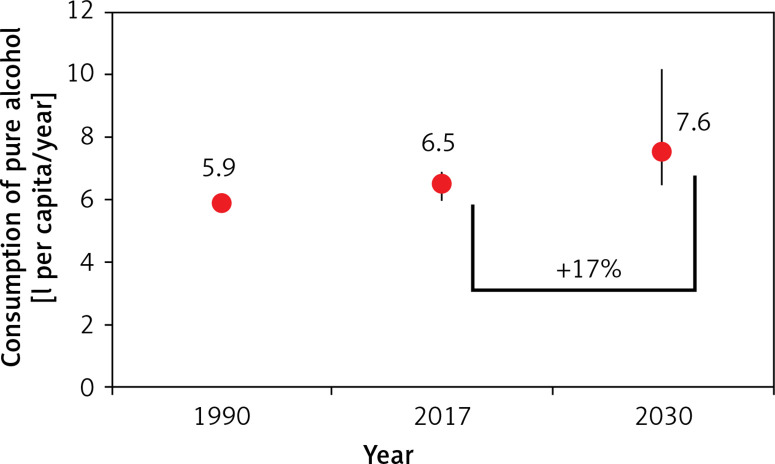
In an interesting study by Manthey et al., data on alcohol consumption in 189 countries and regions over the period 1990-2017 were summarized and forecasted until 2030. Global alcohol consumption was found to increase between 1990 and 2017. Moreover, these researchers forecast a further increase in alcohol consumption by 2030 (Figure 2) [6].
Figure 2.
World alcohol consumption in 1990 and 2017 and forecasts until 2030. Based on [6]
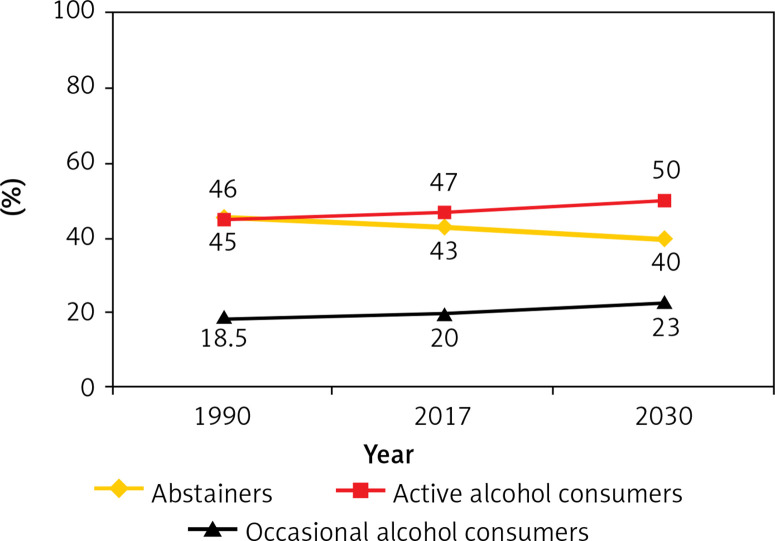
The prevalence of abstinence around the world is also gradually declining. Moreover, the percentage of people actively consuming alcohol and consuming alcohol episodically is increasing. In forecasts until 2030, these trends will be even more intensive (Figure 3) [6].
Figure 3.
Abstinence, active and occasional alcohol consumption in the world in 1990 and 2017, and forecasts until 2030. Based on [6]
Based on these results, it is unlikely that the global goals of reducing harmful effects of alcohol consumption will be achieved in the near future [6].
It should be mentioned that a large percentage of junior high school and high school students admit to alcohol consumption. In the study by Żołnierczuk-Kieliszek et al., which included 135 students of the 3rd grade of lower secondary schools, it was found that 42% of the respondents consumed alcohol several times a year, and almost 25% several times a week. What is alarming, based on the results of the Cage test, it was found that 22% of the respondents had a high probability of being addicted to alcohol [7]. In turn, the study by Wojtyła-Bucior et al. analyzed the prevalence of alcohol consumption among 1100 high school students. Fifty-three percent of respondents confirmed drinking alcohol, of which 69% consumed it less than once a week, 26% once a week, 5% several times a week and 1% every day. The most common drinks were beer (89%) and vodka (71%) [8].
It is worth mentioning that during the current COVID-19 pandemic alcohol consumption increased significantly. A study by McKetta et al. analyzed alcohol consumption by American adults during the first wave of the COVID-19 pandemic. Increased alcohol consumption (increasing the number of drinking days) was found, especially in less severe conditions of the COVID-19 pandemic (incidence risk ratio (IRR) = 1.003; 95% CI: 1.001–1.004) [9]. The study by Valente et al. found that the factors that particularly increased the risk of alcohol consumption during the COVID-19 pandemic were: male gender (AOR = 1.29; 95% CI: 1.13–1.49), higher income (AOR = 1.64; 95% CI: 1.35–1.99), and more stringent quarantine (AOR = 1.10; 95% CI: 1.04–1.16) [10]. Moreover, a study by Weerakoon et al. of 1982 Americans found that 34% reported binge drinking during the COVID-19 pandemic. Each extension of the so-called lockdown by 1 week increased the risk of binge drinking by 19% (AOR = 1.19; 95% CI: 1.06–1.34). Among people suffering from depression, the risk was as high as 77% (AOR = 1.77; 95% CI: 1.16–2.73) [11]. A study by Pollard et al. showed that from 2019 to 2020, alcohol consumption by American adults increased by 14% [12]. In Poland, the impact of the COVID-19 pandemic on trends in alcohol consumption was analyzed by Szajnoga et al. in a study involving 4072 people. It was found that the frequency of alcohol consumption increased especially in the group of men, people aged 18–24, residents of large cities and people working remotely [13].
In summary, the results of several studies indicate a high prevalence of alcohol consumption, both in Poland and in the entire world. The perspective for the next 10 years in terms of trends in alcohol consumption is unfavorable. A large percentage of adolescents have already confirmed their own experience with drinking alcohol. Since 2020 the COVID-19 pandemic has further worsened these adverse statistics.
The impact of alcohol consumption on health in social awareness
The review of the literature by Surma et al. analyzed the knowledge of younger and older people about various risk factors for cardiovascular diseases. It was found that both younger and older people were characterized by insufficient knowledge of the adverse impact of alcohol consumption on the risk of cardiovascular diseases [14, 15]. The study by Żołnierczuk-Kieliszek et al. showed that the knowledge of middle school students about the harmful effects of alcohol abuse on human health was low [7]. An interesting study by Whitman et al., involving 5582 participants of the Health eHeart Study, analyzed the perception of alcohol through its impact on human health. It was found that 30% of the respondents believed that alcohol has a pro-health effect, 39% that it is harmful to health, and 31% did not have an opinion on this subject. Moreover, 80% of those who considered that alcohol is healthy based their opinions on opinions expressed by non-specialized sources. People who believed that alcohol was beneficial to health drank about 50% more alcohol than those who did not support this position. The respondents attributed a particularly health-promoting effect to the consumption of red wine [16].
In conclusion, knowledge about the health effects of alcohol consumption is insufficient, which applies to both younger and older people. A large percentage of people consider alcohol consumption to be healthy, and draw their knowledge from non-specialized sources.
Definition of the alcohol unit and clinical recommendations for alcohol consumption
One unit of alcohol, i.e. a “drink”, usually contains 10 g of pure ethanol in its volume. For example, one unit of alcohol is 125 ml of wine or 250 ml of beer or 40 ml of vodka.
National and international scientific societies in their guidelines/recommendations indicate that in the case of people declaring the willingness to consume alcohol, it should be limited to specific doses (Table I) [17–20]. It is worth mentioning that the latest recommendations of the Polish Lipidological Association of 2021 state that patients with lipid disorders should limit their alcohol consumption to the minimal amount. It is due to, inter alia, the fact that the consumption of 10–30 g of alcohol/day significantly increases the concentration of triglycerides [21]. Moreover, alcohol consumption increases the risk of statin intolerance by 22% [22]. This is important because hypercholesterolemia is the most common cardiovascular risk factor in Poland, affecting as many as 21 million people [23].
Table I.
| Polish Society of Hypertension (2019) |
|---|
| You should limit your alcohol consumption: |
| in men, up to 20-30 g of pure alcohol per day, but not more than 140 g per week (e.g. 2 glasses of wine a day, 5 days a week) |
| in women, up to 10–20 g of pure alcohol per day, but not more than 80 g per week (e.g. one glass of wine a day, 5 days a week) |
| Getting drunk should be strictly avoided |
| Designate alcohol-free days during the week |
| Polish Society of Diabetology (2021) |
| It is not recommended for people with diabetes to consume alcohol |
| You should limit your alcohol consumption: |
| in men: ≤ 30 g/day |
| in women: ≤ 20 g/day |
| European Society of Cardiology (2021) |
| Recommended to restrict alcohol consumption to a maximum of 100 g per week |
| American Heart Association and American College of Cardiology (2019) |
| You should limit your alcohol consumption: |
| in men: ≤ 2 drinks/day |
| in women: ≤ 1 drink/day |
In the United States, a unit of alcohol (drink) contains 14 g of ethanol.
In conclusion, scientific societies allow the daily consumption of alcohol in the amount of 2 drinks for men and one drink for women. The question is whether the recommended doses of alcohol are safe for health.
Alcohol consumption and the risk of premature death
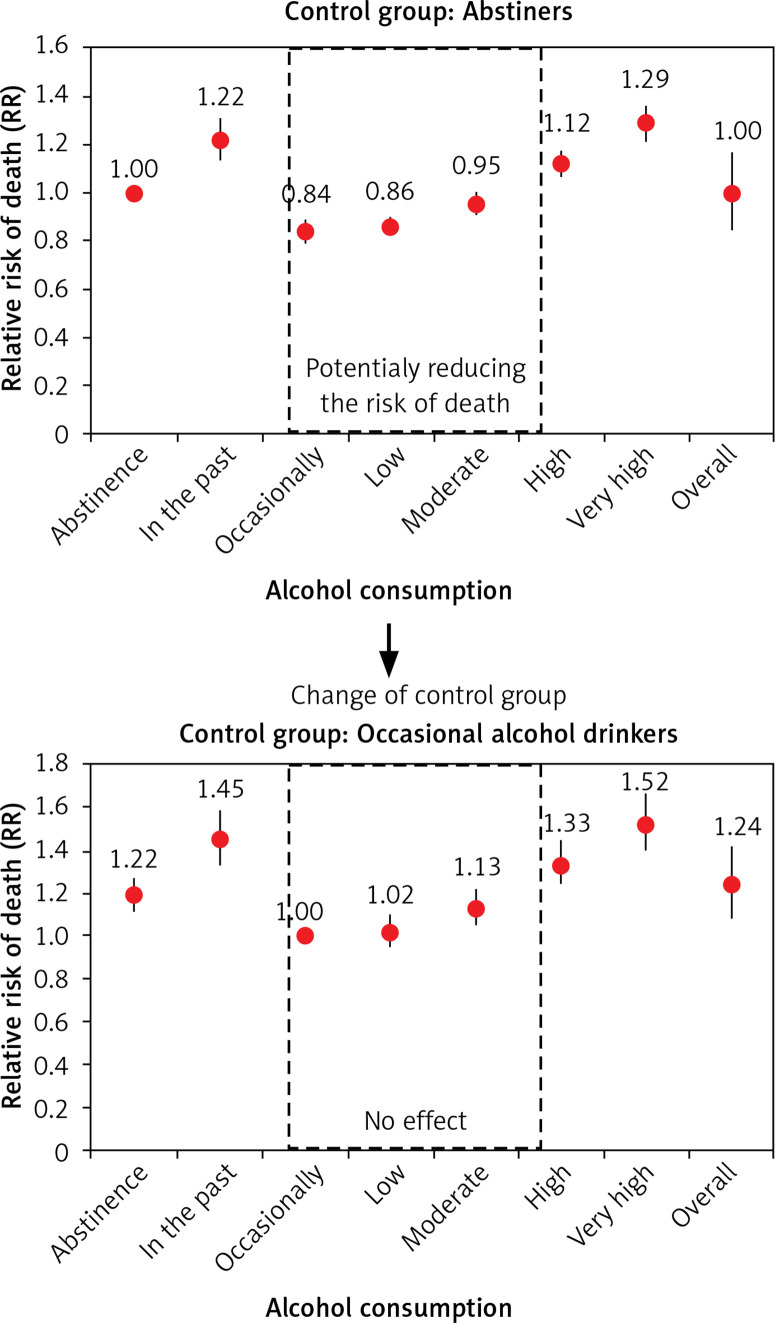
A meta-analysis of 87 studies by Stockwell et al., involving nearly 4 million people, analyzed the impact of their alcohol consumption on the risk of premature death depending on various confounding factors. Interestingly, it was found that the obtained results depended on the reference point (abstainers versus occasional alcohol users as a control group) (Figure 4) [24].
Figure 4.
The impact of alcohol consumption on the risk of premature death [24]
This study showed a significant effect of the way the data were analyzed on the relationship between alcohol consumption and the risk of premature death. The authors of the study stated that comparing people who drink alcohol with abstinent ones does not yield reliable results because the latter are characterized by a tendency towards poor health. Thus, in this study, no beneficial effect of alcohol consumption in reducing the risk of death was found, and, moreover, it was found that alcohol consumption increased this risk [24].
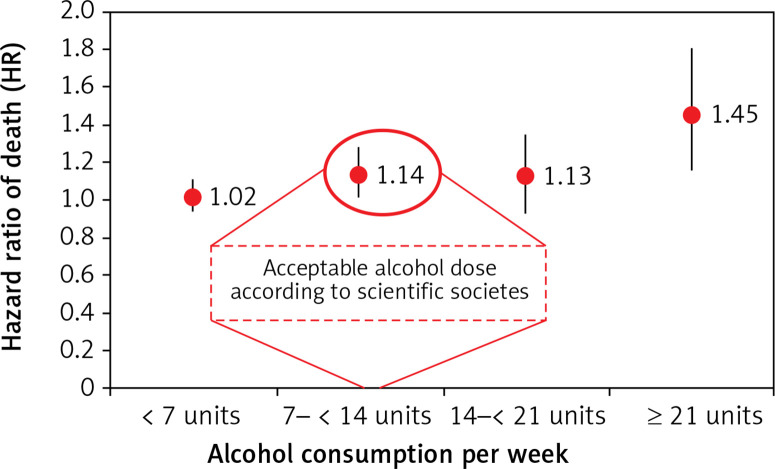
The study by Goulden also assessed the effect of alcohol consumption on the risk of premature death. The obtained results were related to people who used alcohol occasionally. The study included data from 24029 participants in the Health and Retirement Study, while alcohol consumption was assessed on the basis of data from 4 years prior to the start of follow-up. It was found that the risk of death is increased in people who consume alcohol (Figure 5) [25].
Figure 5.
Effect of alcohol consumption (compared to occasional alcohol users) on the risk of premature death [25]
Taking into account the results, alcohol consumption according to the recommendations of scientific societies (7– <14 drinks/week) was associated with an increase in the risk of death by 14% [25].
An important analysis published in 2018 in The Lancet assessed the impact of alcohol consumption on the risk of deteriorating health. The study covered data from surveys and registers from 195 countries. It was found that worldwide alcohol consumption was the seventh leading risk factor for both death and DALY (disability adjusted life-years) in 2016, accounting for 2.2% (95% CI: 1.5–3.0%) of female deaths and 6.8% (5.8–8.0%) of male deaths. A linear relationship was found between the amount of drinks consumed/day and the risk of health loss (complications from cardiovascular diseases or other diseases). The authors concluded that there is no “healthy dose” of alcohol [26]. A study by Wood et al., involving nearly 600 000 people, also showed a positive and curvilinear relationship between alcohol consumption and the risk of death [27]. In a study by Zatoński et al., the alcohol-related deaths in 2002 and 2017 in Poland were compared. It was found that in 2002, among women and men, the aforementioned ratio was 1.7/100 000 inhabitants and 13.9/100 000 inhabitants, respectively. In 2017, alcohol-related mortality in men and women was 6.4/100 000 and 28.0/100 000, respectively. Mortality rates in 2002 and 2017, for both women and men, were highest in the 45–64 age group. It was found that over the years 2002–2017, alcohol-related mortality in Poland increased significantly [28].
In summary, alcohol consumption, including in doses recommended as beneficial by scientific societies, is associated with an increased risk of premature death. The selection of the control group (abstainers versus occasional alcohol users) has a significant impact on the results of the research.
Alcohol consumption and the risk of selected diseases
Until recently, it was believed that small doses of alcohol had a beneficial effect on human health [29]. However, one has to remember that although there are studies in the literature showing, for example, cardioprotective and nephroprotective properties of consuming moderate amounts of alcohol (e.g. [30–32]), toxic effects of the alcohol may occur in other organs [33].
Table II summarizes the impact of alcohol consumption on the risk of developing selected diseases [34–43].
Table II.
Summary of research results and meta-analyses on the impact of alcohol consumption on the risk of selected diseases
| Authors; year | Type of study | Number of subjects/ studies | Analyzed relationship | Results | |
|---|---|---|---|---|---|
| Mouth | Wang J. et al.; 2016 [34] | Meta-analysis | 18 | Influence of alcohol consumption on the risk of periodontitis | Linear increase in the risk of periodontitis from the lowest daily dose of alcohol + 1 g/day → 0.4% (RR = 0.4; 95% CI: 1.002–1.007) High versus low consumption: → 59% (RR = 1.59; 95% CI: 1.37–1.85) |
| Cardiovascular system | Larsson S. et al.; 2014 [35] | Meta-analysis | 7 | Effect of alcohol consumption on the risk of atrial fibrillation |
Increased risk of developing atrial fibrillation depending on the amount of alcohol consumed: 1 unit/day → 8% (RR = 1.08; 95% CI: 1.06–1.10) 2 units/day → 17% (RR = 1.17; 95% CI: 1.13–1.21) 3 units/day → 26% (RR = 1.26; 95% CI: 1.19–1.33) 4 units/day → 36% (RR = 1.36; 95% CI: 1.27–1.46) 5 units/day → 47% (RR = 1.47; 95% CI: 1.34–1.61) |
| Liu F. et al.; 2020 [36] | Meta-analysis | 22 | Effect of alcohol consumption on the risk of arterial hypertension |
Increased risk of high blood pressure depending on the amount of alcohol consumed: < 1 unit/day → 3% (RR = 1.03; 95% CI: 1.01–1.06) 1–2 units/day → 8% (RR = 1.08; 95% CI: 1.01–1.15) > 4 units/day → 26% (RR = 1.26; 95% CI: 1.04–1.53) |
|
| Larsson S. et al.; 2020 [37] | Mendelian randomization study | 889198 subjects | Effect of alcohol consumption on the risk of stroke | Consuming more alcohol, depending on genetic factors, increases your risk of having a stroke about: 27% (OR = 1.27; 95% CI: 1.12–1.45) |
|
| 367586 subjects | Effect of alcohol consumption on the risk of peripheral artery disease |
Consuming more alcohol, taking genetic factors into account, increases the risk of developing peripheral artery disease by: 205% (OR = 3.05; 95% CI: 1.92–4.85) |
|||
| Skeletal system | Charaghi Z. et al.; 2019 [38] | Meta-analysis | 6 | Effect of alcohol consumption on the risk of osteoporosis |
Increased risk of osteoporosis depending on the amount of alcohol consumed: 1–2 units/day → 34% (RR = 1.34; 95% CI: 1.11–1.62) > 2 units/day → 63% (RR = 1.63; 95% CI: 1.01–2.65) |
| Liver | Roerecke M. et al.; 2019 [39] | Meta-analysis | 7 | Effect of alcohol consumption on the risk of cirrhosis |
Increased risk of cirrhosis depending on the amount of alcohol consumed: 1 unit/day → 40% (RR = 1.40; 95% CI: 1.00–1.97) 2 units/day → 203% (RR = 3.02; 95% CI: 1.95–4.70) 3–4 units/day → insignificant increase 5–6 units/day → 526% (RR = 6.26; 95% CI: 2.38–16.50) > 7 units/day → 970% (RR = 10.70; 95% CI: 2.95–38.78) |
| Lungs | Simou E. et al.; 2018 [40] | Meta-analysis | 17 | Effect of alcohol consumption on the risk of pneumonia | Linear increase in the risk of pneumonia from the lowest daily dose of alcohol |
| Lassen M. et al.; 2020 [41] | Cohort study | 171 patients with COVID-19 |
Effect of alcohol consumption on the risk of developing acute respiratory distress syndrome (ARDS) in the course of COVID-19 |
Each additional drink consumed/day led to an increased risk of: ARDS: + 1 unit/day → 5% (OR = 1.05, 95% CI: 1.00–1.10) Severe ARDS: + 1 unit/day → 7% (OR = 1.07, 95% CI: 1.01–1.13) |
|
| Cancers | Begnardi V. et al.; 2015 [42] | Meta-analysis | 52 | Influence of alcohol consumption on the risk of otopharyngeal cancer |
Increased risk of mouth and throat cancer depending on the amount of alcohol consumed: Low → 13% (RR = 1.13; 95% CI: 1.00–1.26) Moderate → 83% (RR = 1.83; 95% CI: 1.62–2.07) Heavy → 413% (RR = 5.13; 95% CI: 4.31–6.10) |
| 41 | Influence of alcohol consumption on the risk of laryngeal cancer |
Increased risk of laryngeal cancer depending on the amount of alcohol consumed: Low → no impact Moderate → 44% (RR = 1.44; 95% CI: 1.25–1.66) Heavy → 165% (RR = 2.65; 95% CI: 2.19–3.19) |
|||
| 54 | Effect of alcohol consumption on the risk of esophageal cancer |
Increased risk of esophageal cancer depending on the amount of alcohol consumed: Low → 26% (RR = 1.26; 95% CI: 1.06–1.50) Moderate → 123% (RR = 2.23; 95% CI: 1.87–2.65) Heavy → 395% (RR = 4.95; 95% CI: 3.86–6.34) |
|||
| 66 | Effect of alcohol consumption on the risk of rectal cancer |
Increased risk of rectal cancer depending on the amount of alcohol consumed: Low → no impact Moderate → 17% (RR = 1.17; 95% CI: 1.11–1.24) Heavy → 44% (RR = 1.44; 95% CI: 1.25–1.65) |
|||
| 14 | Effect of alcohol consumption on the risk of melanoma |
Increased risk of melanoma depending on the amount of alcohol consumed: Low → no impact Moderate → 20% (RR = 1.20; 95% CI: 1.03–1.41) Heavy → no data |
|||
| 118 | Effect of alcohol consumption on the risk of breast cancer |
Increased risk of breast cancer depending on the amount of alcohol consumed: Low → 4% (RR = 1.04; 95% CI: 1.01–1.07) Moderate → 23% (RR = 1.23; 95% CI: 1.19–1.28) Heavy → 61% (RR = 1.61; 95% CI: 1.33–1.94) |
|||
| 43 | Influence of alcohol consumption on the risk of prostate cancer |
Increased risk of prostate cancer depending on the amount of alcohol consumed: Low → 4% (RR = 1.04; 95% CI: 1.01–1.08) Moderate → 6% (RR = 1.06; 95% CI: 1.01–1.11) Heavy → no impact |
|||
| Other | Taylor B. and Rehm J.; 2012 [43] | Research analysis | 5 | Influence of alcohol consumption on the risk of a traffic accident |
Increased risk of a car accident depending on the amount of alcohol concentration in the blood: Each + 0.02% → 75% (RR = 1.75; 95% CI: 1.43–2.14) |
Very recently The Lancet published the results of a population study by Rumgay et al., assessing the influence of alcohol consumption on the risk of cancer development. The categories of alcohol consumption were divided into moderate consumption (< 20 g/day), risky consumption (20–60 g/day) and heavy consumption (> 60 g/day). It was found that in 2020, 4.1% (95% CI: 3.1–5.3%) of all cancers worldwide were caused by alcohol consumption. It was also found that, starting from moderate through risky and heavy alcohol consumption, the risk of cancer was significantly increased [44]. The study by Zatoński et al. assessed the incidence of death related to alcoholic cirrhosis in Poland in 2002 and 2017. It was found that mortality from alcoholic cirrhosis increased in both women and men aged 20–64 (respectively: 1.1/100 000 vs. 7.2/100 000 women and 6.5/100 000 vs. 20.0/100 000 men) [45]. A meta-analysis of 30 studies by Mezzano et al. showed that alcohol was the most frequently reported etiology of chronic liver disease (45%; 95% CI: 41–50) [46].
Alcohol consumption during pregnancy is an extremely important issue from a clinical point of view. Consumption of alcohol in pregnancy is highly teratogenic for the fetus and may cause congenital abdominal defects, microencephalopathy, congenital heart defects, mental retardation, and restriction of intrauterine growth [47]. The study by Wojtyła and Wojtyła analyzed the prevalence of alcohol consumption by pregnant women in Poland. The study included 3695 women, of whom 54.7% reported alcohol consumption during pregnancy. Importantly, almost 6% of them consumed alcohol twice a month on average [48]. The results of a study by Mårdby et al., involving 7905 women living in Europe, provide slightly more optimistic data. In this study, 15.8% of women reported alcohol consumption during pregnancy. The highest prevalence of alcohol consumption during pregnancy was reported by the inhabitants of the UK (28.5%), Russia (26.5%) and Switzerland (20.9%). The lowest prevalence of alcohol consumption during pregnancy was observed in women from Norway (4.1%), Sweden (7.2%) and Poland (9.7%) [49]. The results of these studies indicate that the problem of alcohol consumption during pregnancy is large and there is still a need for large-scale educational campaigns in this regard.
In summary, alcohol consumption, even in amounts permitted by scientific societies, increases the risk of disease in many organ systems.
Controversies regarding the impact of alcohol consumption on human health
The results of numerous studies examining the health effects of alcohol consumption are often inconsistent. The most important factors influencing the obtained results include incorrect selection of patients into particular groups, a control group consisting of non-drinkers but with numerous complications or former drinkers who stopped drinking alcohol due to health loss, possible variability in the amount of alcohol consumed during observation and underestimating the amount of alcohol consumed by the respondents. Moreover, people who drink small amounts of alcohol are generally wealthier, eat well and healthily, and lead a more active lifestyle. One example of the influence of the selection of the control group on the obtained results is the meta-analysis conducted by Stockwell et al. (Figure 3) [24].
The French paradox – what is its explanation?
The widespread belief that alcohol is healthy is related to the French paradox. The term “French paradox” and its meaning were published in 1991 by Serge Renaud, a scientist working at the University of Bordeaux. The reason for its introduction was the results of research conducted by the World Health Organization (WHO), in particular the MONICA project involving 41 cities in 21 countries (mostly European), which assessed the relationship between consumption of saturated fat and mortality from cardiovascular disease. It was found a relationship between the amount of saturated fat consumed and increased cardiovascular mortality. However, this rule was not confirmed everywhere. The most spectacular example was France, where very high consumption of saturated fat (higher than in the United States) was found together with a low cardiovascular mortality rate. Serge Renaud proposed that this phenomenon, which he called the French paradox, may be related to the fact that in France more alcohol is consumed, mainly red wine [50].
In recent years, it has been suggested that the explanation of the French paradox is not the health-promoting effect of alcohol (ethanol), but probably the numerous polyphenols contained in red wine (including resveratrol, flavonoids, anthocyanidins, phenolic acids, quercetin, etc.) [51]. A meta-analysis of 37 clinical trials conducted by Weaver et al. assessed the effect of red wine polyphenols (RWP) on cardiovascular function. The use of RWP was found to be associated with a reduction in systolic blood pressure (mean difference: –2.62 mm Hg (–4.81 to –0.44 mm Hg); p = 0.02) and this effect was more pronounced in people with cardiovascular risk factors (metabolic syndrome, type 2 diabetes, obesity) (mean difference: –3.24 mm Hg (95% CI: –5.71 to –0.77 mm Hg); p = 0.01 versus mean difference: 0.67 (95% CI: –2.45 to 3.80); p = 0.67). There was no significant effect on diastolic blood pressure. Moreover, the analysis with regard to the type of RWP showed that only a significant effect on the reduction of systolic blood pressure was associated with the intake of resveratrol preparations [52]. On the other hand, a meta-analysis involving 22 randomized clinical trials conducted by Huang et al. assessed the effect of consuming blueberries (rich in polyphenols, including procyanidins, quercetin, phenolic acids, anthocyanins, etc.) on cardiovascular risk factors. Blueberry consumption was found to be associated with a reduction in LDL cholesterol (WMD = –0.21 mmol/l; 95% CI: –0.34 to 0.07 mmol/l, p = 0.003), systolic blood pressure (WMD = –2.72 mm Hg; 95% CI: –5.32 to –0.12 mm Hg, p = 0.04), fasting glucose (WMD = –0.10 mmol/l; 95% CI: –0.17 to –0.03 mmol/l, p = 0.004), body mass index (WMD = –0.36 kg/m2; 95% CI: –0.54 to –0.18 kg/m2, p < 0.00001), percent glycated hemoglobin (HbA1c) (WMD = –0.20%; 95% CI: –0.39 to –0.01%, p = 0.04) and tumor necrosis factor α (TNFα) concentrations (WMD = –0.99 pg/ml; 95% CI: –1.96 to –0.02 pg/ml, p = 0.04] [53]. In a meta-analysis published very recently by Wang et al., including 38 clinical trials, the impact of habitual consumption of various fruits, juices and fruit preparations on cardiovascular risk factors was assessed. The consumption of cranberry or cherry juice was found to be associated with a reduction in systolic and diastolic blood pressure (cranberry juice: systolic blood pressure, mean difference = –1.52 mm Hg; 95% CI: –2.97 to –0.07 mm Hg, p = 0.05 and diastolic blood pressure –1.78 mm Hg; 95% CI: –3.43 to –0.12 mm Hg, p = 0.04; cherry juice: systolic blood pressure, mean difference = –3.11 mm Hg; 95% CI: –4.06 to –2.15 mm Hg, p = 0.02) [54]. A meta-analysis of 17 randomized clinical trials conducted by Sarkhosh-Khorasani et al. assessed the effect of consuming grape products on oxidative stress. There was a significant increase in total antioxidant capacity (TAC) (WMD = 1.524 mmol/l; 95% CI: 0.83–2.21 mmol/l) [55]. Moreover, in a meta-analysis of 24 randomized clinical trials conducted by Lupoli et al., the effect of consuming grape-based products on the lipid profile was assessed. It was found that people consuming grape products had lower levels of total cholesterol, LDL cholesterol, oxidized LDL lipoproteins, apolipoprotein B and triglycerides, and at the same time higher levels of HDL cholesterol. A particularly significant effect was seen in the reduction of LDL cholesterol levels (mean difference: –6.3 mg/dl; 95% CI: –9.5 to –3.0 mg/dl; p < 0.001) and oxidized LDL lipoproteins (mean difference: –4.5 U/l; 95% CI: –7.5 to –1.5 U/l; p = 0.003) [56].
Thus, the health benefits attributed to red wine to explain the French paradox are most likely due to the effects of the polyphenols (found in many fruits) and not directly due to the effects of alcohol (ethanol).
Summary and conclusions
Alcohol has been a popular medicine for centuries and has also been used externally for medical purposes.
The problem of alcohol abuse goes back to the time of ancient Egypt.
In Poland and in the entire world, an increase in the amount of alcohol consumed is observed. The current COVID-19 pandemic makes these statistics even worse.
Public awareness of the negative health impact of alcohol consumption is low.
Even in the 20th century, small doses of alcohol were believed to have a health-promoting effect (which was even related to the recommendations given by scientific societies).
The results of recent years suggested that the advantage of small doses of alcohol over abstainers may result from the selection of participants in these analyses and not taking into account confounding factors (e.g. abstainers may have health problems, and those who drink small amounts of alcohol have a better standard of life).
The French paradox is not related to the health-promoting effects of alcohol, but more likely to the polyphenols contained in red wine and fruit.
It is now believed that any amount of alcohol used long-term may have an adverse effect on recovery (the healthy dose of alcohol is zero).
Special emphasis should be placed on educating the public, including pregnant women, about the harmfulness of any amount of alcohol.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Żukowska-Łyko J. Krótka historia alkoholu – kto zawodzi w winie, zawodzi we wszystkim. https://histmag.org/Krotka-historia-alkoholu-14314/ (2016).
- 2.Wnuk M, Purandare B, Marcinkowski J. Struktura spożycia alkoholu w Polsce w ujęciu historycznym. Probl Hig Epidemiol 2013; 94: 446-50. [Google Scholar]
- 3.https://www.cbos.pl/SPISKOM.POL/2019/K_151_19.PDF (access: May 21, 2022).
- 4.Zatoński W, Janik-Koncewicz K, Zatoński M, Wojtyła A. Alkohol – ojciec polskich chorób. Menadżer Zdrowia 2021; 1-2: 82-6. [Google Scholar]
- 5.https://www.money.pl/gospodarka/wiadomosci/artykul/napoje-rynek-spozycie-napojow-cola-pepsi-ile,243,0,2159091.html (access: May 21, 2022).
- 6.Manthey Y, Shield K, Rylett M, Hasan O, Probst C, Rehm J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: a modelling study. Lancet 2019; 393: 2493-502. [DOI] [PubMed] [Google Scholar]
- 7.Żołnierczuk-Kieliszek D, Kulik T, Sidor R, et al. Zachowania zdrowotne związane ze spożyciem alkoholu i wiedza młodzieży gimnazjalnej na temat skutków nadużywania alkoholu. Medycyna Ogólna i Nauki o Zdrowiu 2013; 19: 162-7. [Google Scholar]
- 8.Wojtyła-Buciora P, Wojtyła A, Wojtyła C, Marcinkowski J. Rozpowszechnienie konsumpcji alkoholu w opinii uczniów szkół licealnych i ich rodziców. Hygiea Public Health 2012; 47: 498-504. [Google Scholar]
- 9.McKetta S, Morrison C, Keyes K. Trends in US alcohol consumption frequency during the first wave of the SARS-CoV-2 pandemic. Alcohol Clin Exp Res 2021; 45: 773-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valente J, Sohi I, Garcia-Cerde R, Monteiro M, Sanchez Z. What is associated with the increased frequency of heavy episodic drinking during the COVID-19 pandemic? Data from the PAHO regional web-based survey. Drug Alcohol Depend 2021; 221: 108621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weerakoon S, Jatelina K, Knell G. Longer time spent at home during COVID-19 pandemic is associated with binge drinking among US adults. Am J Drug Alcohol Abuse 2021; 47: 98-106. [DOI] [PubMed] [Google Scholar]
- 12.Pollard M, Tucker J, Green H Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open 2020; 3: e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Szajnoga D, Klimek-Tulwin M, Piekut A. COVID-19 lockdown leads to changes in alcohol consumption patterns. Results from the Polish national survey. J Addict Dis 2021; 39: 215-25. [DOI] [PubMed] [Google Scholar]
- 14.Surma S, Szyndler A, Narkiewicz K. Świadomość wybranych czynników ryzyka chorób układu sercowo-naczyniowego w populacji młodych osób. Choroby Serca i Naczyń 2017; 14: 186-93. [Google Scholar]
- 15.Surma S, Szyndler A, Narkiewicz K. Świadomość nadciśnienia tętniczego i innych czynników ryzyka chorób układu sercowo-naczyniowego w populacji osób dorosłych. Choroby Serca i Naczyń 2018; 15: 14-22. [Google Scholar]
- 16.Whitman I, Pletcher M, Vittinghoff E, et al. Perceptions, information sources, and behavior regarding alcohol and heart health. Am J Cardiol 2015; 116: 642-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tykarski A, Filipiak KJ, Januszewicz A, et al. Zasady postępowania w nadciśnieniu tętniczym – 2019 rok. Wytyczne Polskiego Towarzystwa Nadciśnienia Tętniczego. Nadciśnienie Tętnicze w Praktyce 2019; 5: 1-86. [Google Scholar]
- 18.Araszkiewicz A, Bandurska-Stankiewicz E, Borys S, et al. 2021 Guidelines on the management of patients with diabetes. A position of Diabetes Poland. Clin Diabetol 2021; 10: 1-113. [Google Scholar]
- 19.Visseren FLJ, Mach F, Smulders YM, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 2021; 42: 3227-37. [DOI] [PubMed] [Google Scholar]
- 20.Arnett D, Blumenthal R, Albert M, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019; 140: 596-646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Banach M, Burchardt P, Chlebus K, et al. PoLA/CFPiP/PCS/PSLD/PSD/PSH guidelines on diagnosis and therapy of lipid disorders in Poland 2021. Arch Med Sci 2021; 17: 1447-547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bytyçi I, Penson PE, Mikhailidis DP, et al. Prevalence of statin intolerance: a meta-analysis. Eur Heart J 2022: ehac015. doi: 10.1093/eurheartj/ehac015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banach M, Kaźmierczak J, Mitkowski P, et al. Which patients at risk of cardiovascular disease might benefit the most from inclisiran? Polish experts’ opinion. The compromise between EBM and possibilities in healthcare. Arch Med Sci 2022; 18: 569-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “moderate” drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. J Stud Alcohol Drugs 2016; 77: 185-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goulden R. Moderate alcohol consumption is not associated with reduced all-cause mortality. Am J Med 2016; 129: 180-6. [DOI] [PubMed] [Google Scholar]
- 26.Griswold M, Fullman N, Hawley C, et al. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018; 392: 1015-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wood A, Kaptoge S, Butterworth A, et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018; 391: 1513-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zatoński WA, Zatoński M, Janik-Koncewicz K, Wojtyła A. Alcohol-related deaths in Poland during a period of weakening alcohol control measures. JAMA 2021; 325: 1108-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Toma A, Paré G, Leong G. Alcohol and cardiovascular disease: how much is too much? Curr Atheroscler Rep 2017; 19: 13. [DOI] [PubMed] [Google Scholar]
- 30.O’Neill D, Britton A, Hanah M, et al. Association of longitudinal alcohol consumption trajectories with coronary heart disease: a meta-analysis of six cohort studies using individual participant data. BMC Med 2018; 16: 124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yuan H, Yu Q, Bai H, Xu H, Gu P, Chen L. Alcohol intake and the risk of chronic kidney disease: results from a systematic review and dose-response meta-analysis. Eur J Clin Nutr 2021; 75: 1555-67. [DOI] [PubMed] [Google Scholar]
- 32.Schaeffner E, Ritz E. Alcohol and kidney damage: a Janus-faced relationship. Kidney Int 2012; 81: 816-8. [DOI] [PubMed] [Google Scholar]
- 33.Stătescu C, Clement A, Șerban IL, Sascău R. Consensus and controversy in the debate over the biphasic impact of alcohol consumption on the cardiovascular system. Nutrients 2021; 13: 1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang J, Lv J, Wang W, Jiang X. Alcohol consumption and risk of periodontitis: a meta-analysis. J Clin Periodontol 2016; 43: 572-83. [DOI] [PubMed] [Google Scholar]
- 35.Larsson S, Drca N, Wolk A. Alcohol consumption and risk of atrial fibrillation: a prospective study and dose-response meta-analysis. J Am Coll Cardiol 2014; 64: 281-9. [DOI] [PubMed] [Google Scholar]
- 36.Liu F, Liu Y, Sun X, et al. Race- and sex-specific association between alcohol consumption and hypertension in 22 cohort studies: a systematic review and meta-analysis. Nutr Metab Cardiovasc Dis 2020; 30: 1249-59. [DOI] [PubMed] [Google Scholar]
- 37.Larsson S, Burgess S, Mason A, Michaëlsson K. Alcohol consumption and cardiovascular disease. A mendelian randomization study. Circ Genom Precis Med 2020; 13: e002814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Charaghi Z, Doosti-Irani A, Almasi-Hashiani A, et al. The effect of alcohol on osteoporosis: a systematic review and meta-analysis. Drug Alcohol Depend 2019; 197: 197-202. [DOI] [PubMed] [Google Scholar]
- 39.Roerecke M, Vafaei A, Hasan O, et al. Alcohol consumption and risk of liver cirrhosis: a systematic review and meta-analysis. Am J Gastroenterol 2019; 114: 1574-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simou E, Britton J, Leonardi-Bee J. Alcohol and the risk of pneumonia: a systematic review and meta-analysis. BMJ Open 2018; 8: e022344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lassen MCH, Skaarup KG, Sengeløv M, et al. alcohol consumption and the risk of acute respiratory distress syndrome in COVID-19. Ann Am Thorac Soc 2021; 18: 1074-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Begnardi V, Rota M, Botteri E, et al. Alcohol consumption and site-specific cancer risk: a comprehensive dose-response meta-analysis. Br J Cancer 2015; 112: 580-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taylor B, Rehm J. The relationship between alcohol consumption and fatal motor vehicle injury: high risk at low alcohol levels. Alcohol Clin Exp Res 2012; 36: 1827-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rumgay H, Shield K, Charvat H, et al. Global burden of cancer in 2020 attributable to alcohol consumption: a population-based study. Lancet Oncol 2021; 22: 1071-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zatoński WA, Zatoński M, Janik-Koncewicz K, McKee M. Alcohol-related liver cirrhosis in Poland: the reservoir effect. Lancet Gastroenterol Hepatol 2020; 5: 1035. [DOI] [PubMed] [Google Scholar]
- 46.Mezzano G, Juanola A, Cardenas A, et al. Global burden of disease: acute-on-chronic liver failure, a systematic review and meta-analysis. Gut 2022; 71: 148-55. [DOI] [PubMed] [Google Scholar]
- 47.Subramaniyan V, Chakravarthi S, Jegasothy R, et al. Alcohol-associated liver disease: a review on its pathophysiology, diagnosis and drug therapy. Toxicol Rep 2021; 8: 376-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wojtyła C, Wojtyła A. Alcohol consumption by pregnant women in Poland. J Health Inequal 2017; 3: 51-7. [Google Scholar]
- 49.Mårdby AC, Lupattelli A, Hensing G, Nordeng H. Consumption of alcohol during pregnancy – a multinational European study. Women Birth 2017; 30: 207-13. [DOI] [PubMed] [Google Scholar]
- 50.Sinkiewicz W. Francuski paradoks – czy coś więcej niż tylko potęga czerwonego wina? Kardiologia po Dyplomie 2010; 9: 91-5. [Google Scholar]
- 51.Vidavalur R, Otani H, Singal P, Maulik N. Significance of wine and resveratrol in cardiovascular disease: French paradox revisited. Exp Clin Cardiol Fall 2006; 11: 217-25. [PMC free article] [PubMed] [Google Scholar]
- 52.Weaver S, Rendeiro C, McGettrick H, Philp A, Lucas S. Fine wine or sour grapes? A systematic review and meta-analysis of the impact of red wine polyphenols on vascular health. Eur J Nutr 2021; 60: 1-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Huang H, Chen G, Liao D, Zhu Y, Xue X. Effects of berries consumption on cardiovascular risk factors: a meta-analysis with trial sequential analysis of randomized controlled trials. Sci Rep 2016; 6: 23625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang Y, Gallegos J, Haskell-Ramsay C, Lodge J. Effects of chronic consumption of specific fruit (berries, citrus and cherries) on CVD risk factors: a systematic review and meta-analysis of randomised controlled trials. Eur J Nutr 2021; 60: 615-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sarkhosh-Khorasani S, Sangsefidi Z, Hosseinzadeh M. The effect of grape products containing polyphenols on oxidative stress: a systematic review and meta-analysis of randomized clinical trials. Nutr J 2021; 20: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lupoli R, Ciciola P, Costabile G, Giacco R, Di Minno M, Capaldo B. Impact of grape products on lipid profile: a meta-analysis of randomized controlled studies. J Clin Med 2020; 9: 313. [DOI] [PMC free article] [PubMed] [Google Scholar]