Abstract
Purpose
Studies in adults have reported that video laryngoscope is more useful than direct laryngoscope when training less experienced anesthesiologists. However, whether this is true for infants remains unclear. Therefore, this study aimed to evaluate whether the use of video laryngoscope would result in smaller differences in success rate according to anesthesiologists’ expertise than those in direct laryngoscope.
Methods
Medical records and video recordings from the operating room of patients aged < 1 year who underwent non-cardiac surgery between March 2019 and September 2021 were reviewed. Tracheal intubations between April 8, 2020, and June 20, 2021, were excluded due to the shortage of video laryngoscope blades during the COVID-19 pandemic. Rates of first-time tracheal intubation success were compared by years of anesthesia experience and initial intubation device.
Results
In total, 125 of 175 tracheal intubations were analyzed (direct laryngoscope group, n = 72; video laryngoscope group, n = 53). The first-time tracheal intubation success rate increased with years of experience as an anesthesiologist in the direct laryngoscope group (odds ratio OR 1.70, 95% confidence interval CI 1.15, 2.49; P = 0.0070), but not the video laryngoscope group (OR 0.99, 95% CI 0.74, 1.35; P = 0.99).
Conclusion
The differences in success rate according to the anesthesiologists’ years of experience were non-significant when using video laryngoscope in infants, compared to those in direct laryngoscope.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00540-022-03106-y.
Keywords: Infant, Tracheal intubation, Video laryngoscope
Introduction
Airway management is a fundamental technique used in anesthesia. Hypoxia due to inappropriate airway management is a potential risk leading to cardiac arrest and hypoxic brain damage; hence, safe airway management is crucial. A higher incidence of adverse respiratory events has been reported in infants than in adults [1]. Due to the differences in anatomical (e.g., different shapes of the epiglottis, larger tongue, shorter mandible, and protruding occiput) and physiological characteristics (e.g., short acceptable apnea time [2]), a longer training period is required to learn safe tracheal intubation techniques in infants than in adults [3–6]. Therefore, it is important to consider better practices when less experienced anesthesiologists perform infant tracheal intubation.
Video laryngoscope, a device with a camera attached to its distal tip, offers an indirect view of the larynx and glottis on a screen [7]. Video laryngoscopes have advantages over direct laryngoscopes for adult tracheal intubations performed by less experienced anesthesiologists [8, 9].
In infants, Garcia–Marcinkiewicz showed a higher success rate with video laryngoscope in a large randomized controlled trial that included tracheal intubation providers with a wide range of experience [10]. However, their study did not focus on the relationship between anesthesiologist’s experience and intubation success rate. It remains unknown whether a video laryngoscope is more reliable than a direct laryngoscope for tracheal intubation of infants by less experienced anesthesiologists, and thereby needs to be evaluated.
Therefore, this study aimed to investigate whether video laryngoscope would result in minimum differences in success rate according to anesthesiologist’s years of experience, compared to direct laryngoscope.
Methods
This single-center retrospective observational study adhered to the tenets of the Declaration of Helsinki. The Ethical Review Committee of Hokkaido University Hospital, Sapporo approved this study (IRB No. 021–0200) on March 25, 2022. The requirement for written informed consent was waived owing to its retrospective nature of this study. Consent was obtained through an opt-out method. Opportunity to opt-out of the study was provided through the Hokkaido University Hospital website (https://www.huhp.hokudai.ac.jp/date/rinsho-johokokai/approval/) and Department of Anesthesiology, Hokkaido University Hospital website (http://www.hokudaimasui.jp/research.html) for guardians/parents of the patients who did not wish to participate.
Patients aged < 1 year who underwent non-cardiac surgery under general anesthesia between March 2019 and September 2021 were included. Data between April 8, 2020, and June 20, 2021, were excluded due to the shortage of video laryngoscope blades during the COVID-19 pandemic. The exclusion criteria were: (1) lack of oral tracheal intubation by an anesthesiologist prior to surgery (i.e., existing tracheal intubation before entering the operating room, tracheal intubation performed after the start of surgery, nasal intubation, mask ventilation, use of supraglottic devices, or tracheal intubation by junior residents undergoing short-term training in anesthesiology) and (2) insufficient data obtained from anesthesia records or operating room videos.
No preoperative sedatives or analgesics were administered. Anesthetic and perioperative management were performed according to our institutional practices. For inhalational induction, patients are started on oxygen 6–8 L/min with sevoflurane 5–8% inhalation, and fentanyl (2–5 μg/kg) and rocuronium (0.6–0.9 mg/kg) were administered after placing the venous route; subsequently, mask ventilation was initiated. For intravenous induction, midazolam (0.2–0.3 mg/kg), fentanyl (2–5 μg/kg), and rocuronium (0.6–0.9 mg/kg) were administered, and mask ventilation was initiated with 6–8 L/min of oxygen with 3% sevoflurane. The anesthesiologist in charge determined the neuromuscular blockade achieved based on the time elapsed since rocuronium administration and subsequently performed the tracheal intubation.
The tracheal intubation devices were the Macintosh blade size 1 and Miller blades size 00, size 0, and size 1 (Welch Allyn, Tokyo, Japan) as the direct laryngoscope, and the McGRATH MAC™ blade size 2 (Covidien, Tokyo, Japan) as the video laryngoscope. The choice of tracheal intubation device and the method of using the video laryngoscope (whether to look at the screen or look directly at the glottis like with a direct laryngoscope) were at the discretion of the anesthesiologist who performed anesthesia.
The type and size of the tracheal tube, and whether with or without a cuff, were also left up to the anesthesiologist who performed anesthesia. Although there was no specific time limit for any type of tracheal intubation, the anesthesiologist who performed anesthesia made the decision based on the patient's safety as the top priority. Standard monitoring, including pulse oximetry, end-tidal capnography, electrocardiography, and noninvasive blood pressure measurements, was performed for each patient. Invasive blood pressure measurements were performed if deemed necessary by the anesthesiologist.
Data on patient background, comorbidities, tracheal intubation, and adverse events during tracheal intubation, such as decrease in transcutaneous oxygen saturation to < 95% before and after tracheal intubation, laryngospasm, bronchospasm, minor airway trauma (dental or lip), airway activation (including coughing and bucking), esophageal intubation, cardiac arrest, and laryngeal bleeding, were extracted from electronic medical records (NEC, Tokyo, Japan) and operating room databases (Fukuda Denshi, Tokyo, Japan).
The operator performing tracheal intubation and the time required for tracheal intubation were confirmed using video recordings from the operating room. The time required for tracheal intubation was defined as the amount of time from when the intubation device began to enter the oral cavity to when it completely exited the oral cavity, using the teeth or gums as the boundary line of the oral cavity.
The primary aim was to determine the relationship between years of experience as an anesthesiologist and first-time successful tracheal intubation rate for direct laryngoscope and video laryngoscope, respectively. In order to standardize performance, we used the following definitions. If the size of the tracheal intubation tube changed because the tube was too large, the next attempt was considered as the first-time tracheal intubation. An anesthesia trainee was defined as an anesthesiologist with less than 5 years of experience, and an experienced anesthesiologist was defined as an anesthesiologist with five or more years of experience. This cutoff was established based on the fact that, in Japan, a trainee must have 4 years of anesthesia experience to qualify to sit for the anesthesiologist examination.
Since this was a retrospective study, to ensure the quality of the study and retaining feasibility, the sample size was determined based on the number of patients enrolled in our hospital during the study period. Continuous variables were expressed as medians with interquartile ranges (IQR), as it require no assumption of normality and were considered an optimal description of the data. Categorical data were reported as numbers with percentages (%). Based on the logistic regression model, the effect of years of experience as an anesthesiologist on tracheal intubation success or failure was analyzed and expressed using odds ratios (OR) with 95% confidence intervals (CIs). Pearson’s Chi-squared test was used to analyze the first tracheal intubation success rate of anesthesia trainees and experienced anesthesiologists, expressed using the risk difference with 95% CIs. The least squares method was used to analyze the relationship between the years of experience as an anesthesiologist and the time required for intubation, expressed as regression coefficients and 95% CIs. The Mann–Whitney U test was used to compare tracheal intubation times between anesthesia trainees and experienced anesthesiologists. Two-sided P-values < 0.05 were considered statistically significant. Statistical analyses were performed using JMP 16 (SAS, Cary, NC, USA).
Results
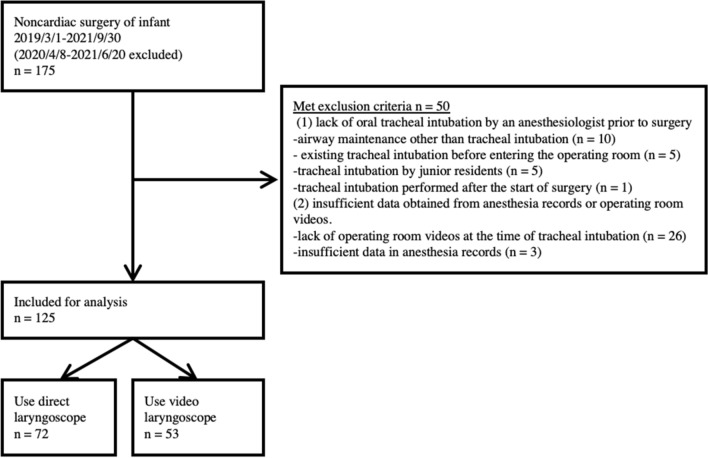
In total, 175 tracheal intubations during the study period met the inclusion criteria (Fig. 1). We excluded 50 tracheal intubations due to lack of operating room video at the time of tracheal intubation (n = 26), airway maintenance other than tracheal intubation (n = 10), existing tracheal intubation prior to entering the operating room (n = 5), tracheal intubated by junior residents (n = 5), insufficient data in anesthesia records (n = 3), and tracheal intubation performed after the start of surgery (n = 1). The remaining 125 tracheal intubations were analyzed. Of these, 72 and 53 were initially attempted using direct laryngoscope and video laryngoscope, respectively. Patient demographic data by tracheal intubation device are listed in Table 1. No adverse events occurred in either of the groups to the extent detectable from the records.
Fig. 1.
Flow diagram of the patients. In the case of multiple tracheal intubations, classification was performed based on the first tracheal intubation procedure
Table 1.
Patient demographic data by tracheal intubation device
| Characteristic | All patients (N = 125) | Direct laryngoscope group (N = 72) | Video laryngoscope group (N = 53) |
|---|---|---|---|
| Age (months) | 7 (4, 9) | 6 (4, 8) | 7 (4, 9) |
| Female/male | 47/78 | 26/46 | 21/32 |
| Weight (kg) | 7.40 (5.75, 8.10) | 7.40 (5.68, 8.40) | 7.40 (5.75, 8.00) |
| ASA-PS 1/2/3/4 | 75/39/11/0 | 49/19/4/0 | 26/20/7/0 |
| Scheduled/emergency surgery | 114/11 | 66/6 | 48/5 |
| Department | |||
| Ophthalmology | 10 | 8 | 2 |
| Plastic surgery | 41 | 31 | 10 |
| Respiratory surgery | 2 | 0 | 2 |
| Gastrointestinal surgery | 50 | 20 | 30 |
| Orthopedic surgery | 7 | 5 | 2 |
| Neurosurgery | 7 | 3 | 4 |
| Urology | 8 | 5 | 3 |
| Number of tracheal intubations (1/2/3 or > 3) | 98/21/6 | 55/14/3 | 43/7/3 |
| Experience as an anesthesiologist (years) | 5.0 (4.0, 7.0) | 5.0 (4.0, 6.8) | 6.0 (5.0, 7.5) |
| Tracheal intubation tube size (3.0/3.5/4.0/4.5 mm inner diameter) | 17/38/69/1 | 9/19/43/1 | 8/19/26/0 |
| Adverse events | 0 | 0 | 0 |
Data are presented as the median (IQR) or number of patients.
ASA-PS American society of anesthesiologists—physical status
Thirty-nine anesthesiologists intubated the patients’ tracheas. The median number of tracheal intubations performed by each anesthesiologist was two (IQR 1, 4). The number of tracheal intubations performed by anesthesia trainees and experienced anesthesiologists were 41 and 84, respectively. Direct laryngoscope was used in 78% of the tracheal intubations performed by anesthesia trainees and 48% of the tracheal intubations performed by experienced anesthesiologists (P = 0.0012; Online resource 1). Patient demographic data by tracheal intubation provider are listed in Online resource 2.
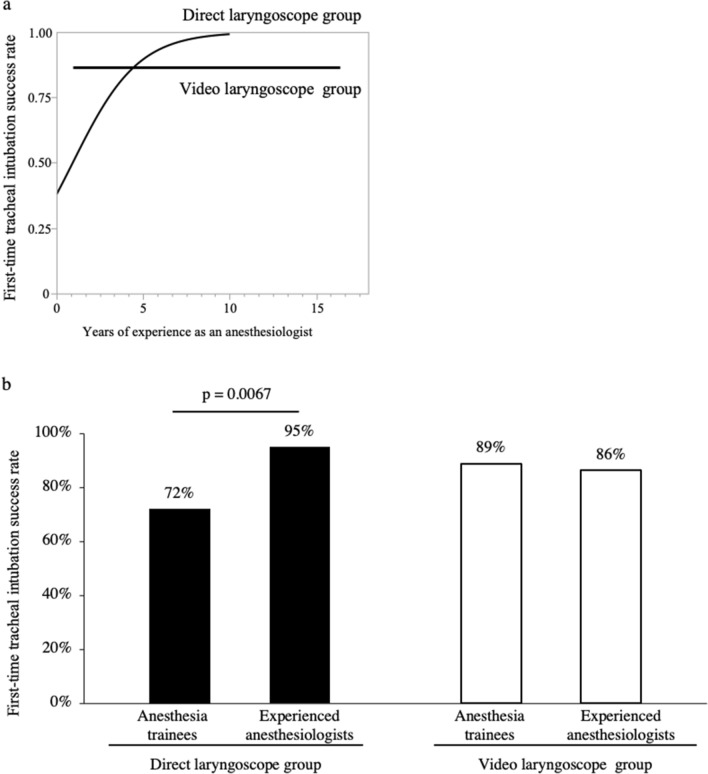
Figure 2a shows relationship between the years of experience as an anesthesiologist and first-time tracheal intubation success rate with each tracheal intubation device. In the direct laryngoscope group, the first-time tracheal intubation success rate increased with the years of experience as anesthesiologists (OR 1.70, 95% CI 1.15, 2.49; P = 0.0070). In the video laryngoscope group, there was no relationship between the years of experience as anesthesiologists and the success rate (OR 0.99, 95% CI 0.74, 1.35; P = 0.99).
Fig. 2.
First-time tracheal intubation success rate with direct laryngoscope and video laryngoscope (a). In the direct laryngoscope group, first-time successful tracheal intubation rates increase with increasing years of experience of the anesthesiologists (OR 1.70, 95% CI 1.15, 2.49; P = 0.0070). In the video laryngoscope group, there was no association between years of experience of the anesthesiologists and first-time successful tracheal intubation rate (OR 0.99, 95% CI 0.74, 1.35; P = 0.99) (b). In the direct laryngoscope group, the first-time successful tracheal intubation rate was significantly higher for experienced anesthesiologists compared with anesthesia trainees (95 vs. 72%, risk difference 23%, 95% CI 0.05, 0.39; P = 0.0067); in the video laryngoscope group, there was no significant difference (86 vs. 89%, risk difference, −3%, 95% CI −0.22, 0.28; P = 0.84)
In the direct laryngoscope group, the success rate of first tracheal intubation was significantly higher for experienced anesthesiologists than for anesthesia trainees (95% vs. 72%; risk difference, 23%; 95% CI 0.05, 0.39; P = 0.0067). In the video laryngoscope group, there was no significant difference in the success rate of the first tracheal intubation between experienced anesthesiologists and anesthesia trainees (86 vs. 89%; risk difference, − 3%; 95% CI − 0.22, 0.28; P = 0.84; Fig. 2b).
The number of first tracheal intubation successes was 61 (85%) and 46 (87%) in the direct laryngoscope and video laryngoscope groups, respectively. Figure 3 shows the relationship between years of experience as an anesthesiologist and time required for intubation. Longer years of anesthesia experience tended to result in shorter intubation times, with no significant difference in the direct laryngoscope group (regression coefficient − 1.03, 95% CI − 2.29, 0.22) and a significant difference in the video laryngoscope group (regression coefficient − 1.63, 95% CI − 2.88, – 0.37).
Fig. 3.
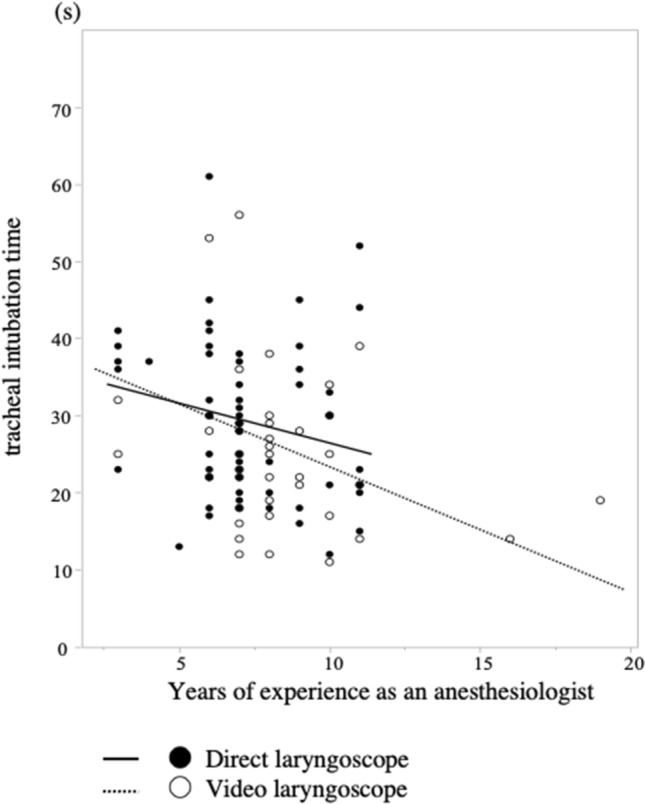
Relationship between years of anesthesiologist experience and time required for tracheal intubation. More years of anesthesia experience tended to result in shorter tracheal intubation times, with no significant difference in the direct laryngoscope group (regression coefficient −1.03, 95% CI −2.29, 0.22) and a significant difference in the video laryngoscope group (regression coefficient −1.63, 95% CI −2.88, −0.37)
In the direct laryngoscope group, tracheal intubation time was significantly shorter for experienced anesthesiologists than for anesthesia trainees [37 (23, 41 s) vs. 25 s (20, 34 s); P = 0.0471]. In the video laryngoscope group, tracheal intubation time was also significantly shorter for experienced anesthesiologists than for anesthesia trainees [30 (26, 48 s) vs. 23 s (17, 29 s); P = 0.0147] (Table 2).
Table 2.
Intubation time for anesthesia trainees and experienced anesthesiologists
| Anesthesia trainees | Experienced anesthesiologists | P value | |
|---|---|---|---|
| Direct laryngoscope group (N = 61) | 37 s (23, 41 s) | 25 s (20, 34 s) | 0.0471 |
| Video laryngoscope group (N = 46) | 30 s (26, 48 s) | 23 s (17, 29 s) | 0.0147 |
Experienced anesthesiologists had significantly shorter intubation times than anesthesia trainees in both direct laryngoscope and video laryngoscope groups. Data are presented as the median (IQR)
Discussion
This study examined the relationship between years of anesthesia experience and first-time intubation success rate in infants with direct laryngoscope and video laryngoscope, which are commonly used in the operating room. The first-time tracheal intubation success rate increased with increasing anesthesia experience while using direct laryngoscope; no significant difference between years of experience and the first-time tracheal intubation success rate was noted with video laryngoscope. This indicates that video laryngoscope may be used successfully by anesthesiologists with less experience as well as those with more experience.
To the best of our knowledge, this is the first study to evaluate whether using a video laryngoscope would result in non-significant differences in the success rate of first-time infant tracheal intubation according to the anesthesiologists’ years of experience, when compared to using a direct laryngoscope. It has been reported that the success rate of tracheal intubation with a direct laryngoscope increases with the years of experience of the anesthesiologist performing the intubation in infants [5]. In video laryngoscopy, previous reports have examined the relationship between years of experience and success rates in tracheal intubation for adults in the emergency department [11, 12], but not in the anesthesia department or for infants.
In this study, if there were changes in the size of the tracheal intubation tube, the next attempt was considered as the first-time tracheal intubation. This definition was used as it is difficult to predict the appropriate tube size for infants based on age, height, and weight. Shibasaki et al. reported that the probability of selecting the correct size with a cuffed tube was 35% in their age-based formula study [13]. It is necessary to separate the success/failure of the tracheal intubation procedure from tube size mismatch.
We also measured the tracheal intubation time only in successful initial tracheal intubation. White et al. reported a mean tracheal intubation time of 25.03 ± 1.42 s with direct laryngoscope and 25.90 ± 2.34 s with video laryngoscope [14]. Fiadjoe et al. reported a median tracheal intubation time and range of 21.4 s (9.5, 66.1 s) with direct laryngoscope and 22.6 s (13.3, 61.0 s) with video laryngoscope [15]. In these studies, tracheal intubation was performed on infants by anesthesiologists fully trained in tracheal intubation techniques. When experienced anesthesiologists performed tracheal intubation in our study, the median (IQR) tracheal intubation time was 25 s (20, 34 s) with direct laryngoscope and 23 s (17, 29 s) with video laryngoscope, which is reasonable considering previous reports.
The time required for successful first-time tracheal intubation tended to be shorter with the higher the years of anesthesia experience (Fig. 3). Furthermore, experienced anesthesiologists had shorter tracheal intubation times than did anesthesia trainees. This trend was the same for both direct laryngoscope and video laryngoscope (Table 2). The results suggest that years of experience as anesthesiologists may have a greater influence on the time required for tracheal intubation than the choice of tracheal intubation device.
A potential issue while discussing tracheal intubation time is the variation in the definitions of tracheal intubation time. Some studies defined a single tracheal intubation time as from the time the laryngoscope was placed in the oral cavity until it was removed [15, 16], whereas others defined it as the time until end-tidal carbon dioxide was detected [17–19]. In this study, the time required for tracheal intubation was defined as the time from the when the laryngoscope was placed in the oral cavity until it was removed. Furthermore, when multiple tracheal intubations were performed, one study defined the tracheal intubation time as the sum of all the tracheal intubation times [15], while another considered the time required for the final tracheal intubation which succeeded [18]. In this study, the time required for tracheal intubation was compared only in cases of first-time successful tracheal intubation.
The video laryngoscope used in this study was a McGRATH MAC ™ blade size 2. Although similar in size with the Macintosh blade size 2 and intended for children, it is large for infants; however, we used the blade safely for newborns by inserting only the tip of the blade into the mouth. The McGRATH MAC ™ blade size 1 was not available at our institution during the period covered by this study; however, we are currently using size 1 for tracheal intubation of infants. This is expected to improve the operability of video laryngoscope when tracheal intubating infants; however, this needs further investigation.
The choice of tracheal intubation device is predominantly based on two factors. The first is the prior prediction of tracheal intubation difficulties. Several congenital diseases, syndromes, and conditions are predictors of difficult tracheal intubation in infants [20]. It is possible that physical characteristics can also predict tracheal intubation difficulties for anesthesiologists [21]. The second factor is the personal preference of the operator. Although device selection varies from individual to individual, the selection of direct laryngoscope among anesthesia trainees was higher than that of experienced anesthesiologists (Online resource 2), possibly because less experienced anesthesiologists chose direct laryngoscope to improve their tracheal intubation techniques.
Limitations
This was a single-center retrospective observational study, considerably limited by the lack of a priori sample size estimation. Exceeding the outcome by < 10 times the sum of the exposure factor and covariates may reduce bias [22]. In the present study, the sample size was small; therefore, the results are likely biased and we should exercise caution when interpreting them.
The selection of operators and devices was not randomized, which may result in selection bias for tracheal intubation devices. Anesthesiologists who performed the tracheal intubation and risk factors of tracheal intubation difficulty are not independent; hence, confounding may occur.
As data in anesthesia records were written by an anesthesiologist who had performed the anesthesia after tracheal intubation was performed, some details of the procedure may have been omitted. Although no adverse events were found as far as we have examined the operating room video recordings, monitor screen recordings, and medical record entries, we cannot rule out the possibility of omissions in the medical records. Cormack classification and subjective tracheal intubation difficulty was not evaluated because of the large amount of missing data.
Conclusion
Compared to a direct laryngoscope, the use of video laryngoscope in infants resulted in non-significant differences in success rate according to years of experience as an anesthesiologist.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank Taiki Kojima for the helpful discussions and comments on the manuscript and Editage (www.editage.com) for the editing and proofreading of English language.
Author contributions
All the authors contributed to the conception and design of the study. Material preparation, data collection and analysis, and preparation of the first draft of the manuscript were performed by YU. Data collection was assisted by TA. Critical revision of the manuscript was performed by KH. The statistical analysis was supervised by IY. All the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Funding
IY reports grants from KAKENHI, AMED, and Health, Labour and Welfare Policy Research Grants, research fund by Nihon Medi-Physics, and speaker fees from Chugai Pharmaceutical Co, AstraZeneca plc and Nippon Shinyaku Co, outside the submitted work.
Declarations
Conflict of interest
All the authors declare that they have no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Morray JP, Geiduschek JM, Caplan RA, Posner KL, Gild WM, Cheney FW. A comparison of pediatric and adult anesthesia closed malpractice claims. Anesthesiology. 1993;78:461–467. doi: 10.1097/00000542-199303000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Hardman JG, Wills JS. The development of hypoxaemia during apnoea in children: a computational modelling investigation. Bja Br J Anaesth. 2006;97:564–570. doi: 10.1093/bja/ael178. [DOI] [PubMed] [Google Scholar]
- 3.Doglioni N, Cavallin F, Zanardo V, Trevisanuto D. Intubation training in neonatal patients: a review of one trainee’s first 150 procedures. J Matern-fetal Neonatal Med. 2011;25:1302–1304. doi: 10.3109/14767058.2011.632035. [DOI] [PubMed] [Google Scholar]
- 4.Reed MJ. Intubation training in emergency medicine: a review of one trainee’s first 100 procedures. Emerg Med J. 2007;24:654. doi: 10.1136/emj.2007.048678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanders RC, Giuliano JS, Sullivan JE, Brown CA, Walls RM, Nadkarni V, et al. Level of trainee and tracheal intubation outcomes. Pediatrics. 2013;131:e821–e828. doi: 10.1542/peds.2012-2127. [DOI] [PubMed] [Google Scholar]
- 6.Konrad C, Schupfer G, Wietlisbach M, Gerber H. Learning manual skills in anesthesiology. Anesth Analg. 1998;86:635–639. doi: 10.1213/00000539-199803000-00037. [DOI] [PubMed] [Google Scholar]
- 7.Chemsian R, Bhananker S, Ramaiah R. Videolaryngoscopy. Int J Crit Illn Inj Sci. 2014;4:35–41. doi: 10.4103/2229-5151.128011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayoub CM, Kanazi GE, Alami AA, Rameh C, El-Khatib MF. tracheal intubation following training with the glidescope® compared to direct laryngoscopy. Anaesthesia. 2010;65:674–678. doi: 10.1111/j.1365-2044.2010.06335.x. [DOI] [PubMed] [Google Scholar]
- 9.Nouruzi-Sedeh P, Schumann M, Groeben H. Laryngoscopy via macintosh blade versus glidescope. Anesthesiology. 2009;110:32–37. doi: 10.1097/ALN.0b013e318190b6a7. [DOI] [PubMed] [Google Scholar]
- 10.Garcia-Marcinkiewicz AG, Kovatsis PG, Hunyady AI, Olomu PN, Zhang B, Sathyamoorthy M, Gonzalez A, Kanmanthreddy S, Gálvez JA, Franz AM, Peyton J, Park R, Kiss EE, Sommerfield D, Griffis H, Nishisaki A, Ungern-Sternberg BS, Nadkarni VM, McGowan FX, Fiadjoe JE. First-attempt success rate of video laryngoscopy in small infants (VISI): a multicentre, randomised controlled trial. Lancet. 2020;396:1905–1913. doi: 10.1016/S0140-6736(20)32532-0. [DOI] [PubMed] [Google Scholar]
- 11.Schulte TE, Ringenberg KJ, Lisco SJ, Sayles H, Shillcutt SK. Trainee experience and success of urgent airway management. J Clin Anesth. 2016;35:536–542. doi: 10.1016/j.jclinane.2016.07.041. [DOI] [PubMed] [Google Scholar]
- 12.Sakles JC, Mosier J, Patanwala AE, Dicken J. Learning curves for direct laryngoscopy and glidescope® video laryngoscopy in an emergency medicine residency. West J Emerg Med. 2014;15:930–937. doi: 10.5811/westjem.2014.9.23691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, Sessler DI. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010;113:819–824. doi: 10.1097/ALN.0b013e3181ef6757. [DOI] [PubMed] [Google Scholar]
- 14.White MC, Marsh CJ, Beringer RM, Nolan JA, Choi AYS, Medlock KE, Mason DG. A randomised, controlled trial comparing the Airtraq™ optical laryngoscope with conventional laryngoscopy in infants and children. Anaesthesia. 2012;67:226–231. doi: 10.1111/j.1365-2044.2011.06978.x. [DOI] [PubMed] [Google Scholar]
- 15.Fiadjoe JE, Gurnaney H, Dalesio N, Sussman E, Zhao H, Zhang X, Stricker PA. A prospective randomized equivalence trial of the glidescope cobalt® video laryngoscope to traditional direct laryngoscopy in neonates and Infants. Anesthesiology. 2012;116:622–628. doi: 10.1097/ALN.0b013e318246ea4d. [DOI] [PubMed] [Google Scholar]
- 16.Singh R, Singh P, Vajifdar H. A comparison of Truview infant EVO2 laryngoscope with the Miller blade in neonates and infants. Pediatr Anesth. 2009;19:338–342. doi: 10.1111/j.1460-9592.2009.02929.x. [DOI] [PubMed] [Google Scholar]
- 17.Kim JE, Kwak HJ, Jung WS, Chang MY, Lee SY, Kim JY. A comparison between McGrath MAC videolaryngoscopy and macintosh laryngoscopy in children. Acta Anaesthesiol Scand. 2017;62:312–318. doi: 10.1111/aas.13043. [DOI] [PubMed] [Google Scholar]
- 18.Kaur G, Gupta S, Mehta N, Dhingra J. Comparative evaluation of mcgrath MAC, Truview video laryngoscopes and Macintosh laryngoscope for endotracheal intubation in patients undergoing surgery under general anaesthesia. Anesth Essays Res. 2020;14:20. doi: 10.4103/aer.AER_16_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manirajan M, Bidkar P, Sivakumar R, Lata S, Srinivasan G, Jha A. Comparison of paediatric King Vision™ videolaryngoscope and Macintosh laryngoscope for elective tracheal intubation in children of age less than 1 year: A randomised clinical trial. Indian J Anaesth. 2020;64:943. doi: 10.4103/ija.IJA_154_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rinaldi PA, Dogra S, Sellman GL. Difficult intubation in paediatric palatoplasty. Anaesthesia. 1993;48:358–359. doi: 10.1111/j.1365-2044.1993.tb06996.x. [DOI] [PubMed] [Google Scholar]
- 21.Aparna D, Jafra A, Bhardwaj N, Jain D, Luthra A, Malik MA. Evaluation of various anthropometric airway parameters as predictors of difficult airway in neonates: a prospective observational study. Int J Pediatr Otorhi. 2020 doi: 10.1016/j.ijporl.2020.110387. [DOI] [PubMed] [Google Scholar]
- 22.Cepeda MS, Boston R, Farrar JT, Strom BL. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;158:280–287. doi: 10.1093/aje/kwg115. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.