Abstract
Immune checkpoint inhibitor-related pneumonitis (ICI-P) during cancer treatment is rarely observed (<5%). ICI-P is more often observed in patients with nonsmall cell lung cancer (NSCLC) than in those with other cancers. Likewise, it is more common in those receiving programmed cell death (PD)-1/PD-1 ligand inhibitors rather than cytotoxic T-lymphocyte antigen (CTLA)-4 inhibitors alone. The frequency of ICI-P is higher when anti-PD-1 and anti-CTLA-4 are administered concomitantly. Despite the low fatality rate (≈13%), ICI-P is the leading cause of ICI-related deaths. This narrative review focuses on the epidemiology, clinical and radiological presentation and prognosis of ICI-P occurring in patients, especially those with advanced NSCLC. Emphasis is placed on the differences in terms of frequency or clinical picture observed depending on whether the ICI is used as monotherapy or in combination with another ICI or chemotherapy. Other pulmonary complications observed in cancer patients, yet not necessarily immune-related, are reviewed, such as sarcoid-like granulomatosis, tuberculosis or other infections. A proposal for pragmatic management, including differential diagnosis and therapeutic strategies, is presented, based on the ICI-P series reported in the literature and published guidelines.
Short abstract
Immune checkpoint inhibitor-related pneumonitis (ICI-P) is rare. Despite a low fatality rate, it is the leading cause of death in relation to ICIs. It is crucial to recognise and manage ICI-P by stopping immunotherapy and quickly starting corticosteroids. http://bit.ly/2Ldsp3n
Introduction
Over the past decade, immune checkpoint inhibitors (ICIs) have transformed the therapeutic management of numerous metastatic cancers, particularly advanced nonsmall cell lung carcinoma (NSCLC) without oncogenic addiction [1–3]. The interactions between tumour and immune system can be explained as follows. First, the tumour antigens are presented to naïve T-lymphocytes by antigen-presenting cells (APCs), whereas cytotoxic T-lymphocyte associated antigen (CTLA)-4 protein can curtail T-lymphocyte activation by competitively binding with cluster of differentiation (CD)28 for APCs costimulatory CD84/86 ligands [4]. If T-lymphocytes are activated and express the programmed cell death (PD)-1 protein, they can encounter programmed cell death ligand 1 (PD-L1)-expressing tumour cells. The PD-1/PD-L1 interaction then results in T-cell deactivation [5]. These repeated T-lymphocyte/tumour cell PD-1/PD-L1-negative interactions lead to either T-cells halting at the tumour edge or T-cell exhaustion, resulting in tumour immune escape [6]. ICIs are able to restore specific anti-tumour immunity by blocking the negative regulatory action of the immune checkpoint proteins CTLA-4 and PD-L1. In tumours with ≥1% PD-L1 expression, the PD-1 inhibitors nivolumab [7, 8] and pembrolizumab [9], as well as the anti-PD-L1 inhibitor atezolizumab [10], were proven superior in terms of overall survival and toxicity over docetaxel in the advanced NSCLC second-line setting. Pembrolizumab was demonstrated to be more effective and less toxic than platinum-doublet chemotherapy in advanced NSCLC with high (≥50%) tumour PD-L1 expression [11]. More recently, durvalumab was reported to be effective in consolidation therapy after concomitant chemoradiotherapy in patients with locally advanced NSCLC [12]. Therefore, combining an ICI and platinum doublet chemotherapy [13–15] is becoming the standard of care for advanced NSCLC without oncogenic addiction, in patients with good performance status (0–1) and without overt comorbidities such as previous autoimmune disorders. However, the role of combining anti-PD-1 or PD-L1 and CTLA-4 drug must be further confirmed [16, 17], whereas administering the anti CTLA-4 antibody alone has not been well evaluated for NSCLC.
Although ICIs have proven to be more effective and less toxic compared to chemotherapy, clinicians have reported the occurrence of unusual adverse events [18], likely to be related to the mechanisms of action of ICIs. By removing the brake on activated T-lymphocytes in the different body organs, ICIs are likely to promote T-cell attack on normal tissue cells expressing self-antigens. Clinically, this can manifest as a set of unique toxicities in terms of pattern of onset, organs concerned and severity level. These toxicities are referred to as immune-related adverse events (irAEs) [19]. The organs most frequently involved in the initial reports were the skin, joints, thyroid and digestive tract. Then, later on, the liver, non-thyroid endocrine glands (hypophysitis and adrenal insufficiency), lungs and nervous system (myasthenia gravis and encephalitis) were described as being affected by toxicities. Lastly, nephritis, myositis/myocarditis and even haematological irAEs were reported [20]. However, different ICIs and different doses of the same ICI may result in different adverse events, potentially depending on the cancer treated [21, 22]. Although these toxicities are generally well controlled by stopping the ICI and possibly adding glucocorticoids, some may be fatal, especially ICI-related pneumonitis (ICI-P) [23–25]. When the irAE affects the lung, it must be distinguished from a pseudoprogression [26, 27], hyperprogression [28] and pulmonary infection, insofar as the prognosis and therapeutic management will differ. This is particularly true in NSCLC patients who are more vulnerable, due to their age, frequency of cardiovascular and respiratory comorbidities, and tumoural lung involvement.
This narrative review focuses on the epidemiology, clinical and radiological presentation and prognosis of ICI-P observed in ICI-treated patients, especially in those with advanced NSCLC. Emphasis is placed on the differences observed in terms of frequency or clinical picture depending on whether the ICI was used as monotherapy or in combination with either another ICI or chemotherapy. Other pulmonary complications, not necessarily immune-related, are reviewed, such as sarcoid-like granulomatosis, tuberculosis (TB) or other pulmonary infections. A pragmatic management proposal, including differential diagnosis and therapeutic strategies, will be presented based on the ICI-P series reported in the literature and published guidelines.
Methods
A systematic MEDLINE search accessed through PubMed, Cochrane databases and Google Scholar was performed from inception to December 2018. All phase III trials, systematic reviews, meta-analyses, series and case reports on ICI-P were included. Bibliographies from selected articles were screened for relevant publications. However, narrative reviews and data extracted from meeting abstracts were only minimally used.
The language of published materials was restricted to English and French when searching in the electronic databases. Articles were identified using a combination of the following medical subject heading search terms: “atezolizumab” OR “durvalumab” OR “nivolumab” OR “pembrolizumab” OR “ipilimumab” OR “tremelimumab” OR “immune checkpoint inhibitor” AND “lung toxicity” OR “interstitial lung disease” OR “pneumonitis” OR “pneumonia” OR “diffuse interstitial pneumonitis, pneumonia” OR “organising pneumonia, pneumonitis” OR “sarcoidosis” OR “sarcoid-like granulomatosis” OR “tuberculosis” OR “aspergillosis” OR “pulmonary infection”. All articles were reviewed by at least two team members (JC, AC, LM or VF).
Epidemiology and risk factors of ICI-P
Several sources provide information on the epidemiology of ICI-P in ICI-treated patients with advanced NSCLC, such as safety reports from NSCLC phase III trials, systematic reviews and meta-analyses pertaining to irAEs, as well as data published by pharmacovigilance centres.
Phase III trials performed in NSCLC patients
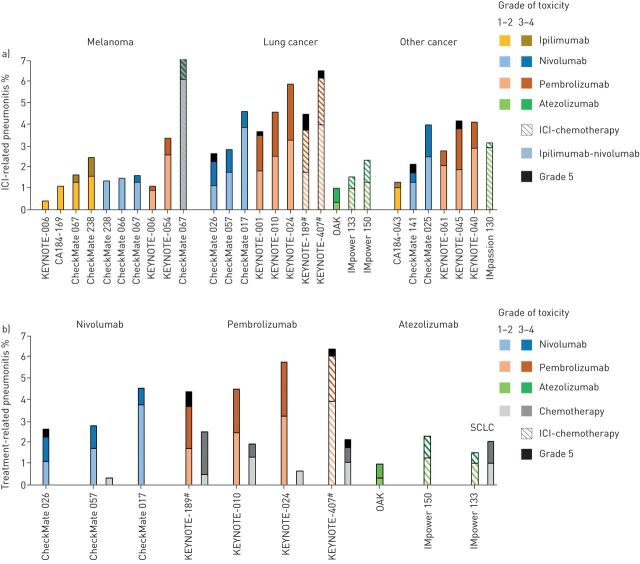
In December 2018, 30 phase III trials evaluating the efficacy of ICIs were published, of which 12 concerned lung cancer [7–15, 29–31], nine melanoma [32–40] and nine other cancer types [41–49] (figure 1a,b). All lung cancer trials concerned NSCLC, except two in small cell lung carcinoma [29, 31]. For lung cancer trials, the ICIs studied were atezolizumab [10, 13, 29], nivolumab [7, 8, 30], pembrolizumab [9, 11, 14, 15] and ipilimumab [31], given either alone or in association with chemotherapy [14, 15, 29, 31], for durvalumab in consolidation after concomitant radiochemotherapy [12].
FIGURE 1.
Frequency of immune checkpoint inhibitor (ICI)-related pneumonitis in published phase III trials. a) Frequency of ICI-related pneumonitis observed in all published phase III trials; b) frequency of pneumonitis observed in ICI and chemotherapy arms in published lung cancer phase III trials. SCLC: small cell lung carcinoma. #: pneumonitis of any cause.
The incidence of pneumonitis in phase III trials was between <0.5% and 10% for all grades, and between 0.5% and 3% for toxicity grades ≥3. The incidence was higher when an ICI was combined with chemotherapy (1.5–6.5%) or for CTLA-4 and nivolumab combinations (7%). Out of the 11 921 patients included in these trials receiving at least one ICI injection, 108 (0.9%) deaths were deemed related to drug toxicity (grade 5 event), among which 24 (0.2%) were due to respiratory adverse events. 12 (0.1%) deaths were related to ICI-P [9, 14, 15, 30, 42, 44, 47–49]; among these, five patients received either ICI with chemotherapy (n=4) [14, 15] or ipilimumab–nivolumab combination (n=1) [47]. In the one patient receiving the ipilimumab–nivolumab combination, the death was related to immune-mediated bronchitis [47]. Finally, 10 (<0.1%) deaths were related to pneumonia [9, 29, 31, 45, 47] or “lung infection” [47], of which two patients were receiving ICI with chemotherapy [29, 31] and one patient was receiving the ipilimumab–nivolumab combination [47].
Moreover, the incidence of pneumonitis was higher in lung cancer (1–6%) than in other cancers (0.1–4%). Data on treatment duration at pneumonitis onset is available from only a few studies. The median (range) time to ICI-P onset was 15.1 (2.6–85.1) weeks, 31.1 (11.7–56.9) weeks and 7.8 (3.1–48.1) weeks in patients receiving nivolumab for advanced squamous cell carcinoma (n=6) [8], advanced nonsquamous cell carcinoma (n=10) [7] and adjuvant melanoma treatment (n=6) [34], respectively. This time interval was 10.0 (1.9–14.0) weeks for the 10 patients receiving ipilimumab for adjuvant melanoma treatment [34].
Clarifications provided by systematic reviews and meta-analyses on irAEs
In December 2018, several systematic reviews conducted on irAEs [21, 22, 50–54] and, more specifically, on respiratory adverse events including ICI-P [55–60], involved nine to 48 randomised controlled prospective trials including 3500–15 000 patients. These studies involved patients with either any cancer type [22, 50–55, 57, 58, 60] or only NSCLC [21, 56, 59], treated either with any ICI [22, 50–52, 55, 57, 60] or only anti-PD-1/PD-L1 inhibitors [21, 53, 54, 56, 58, 59]. These studies present significant methodological differences, with epidemiological data on ICI-P summarised in table 1.
TABLE 1.
Epidemiology of immune-related adverse events (irAEs) and immune checkpoint inhibitor-related pneumonitis (ICI-P)
| Characteristics | Comments | References |
| Frequency of ICI-P | 5th cause of irAEs after skin toxicities, hepatitis, thyroiditis and colitis 2.6–4.8% all grades 0.6–2.0% for grades ≥3 |
[51, 57–59] |
| Increased risk of pneumonitis in NSCLC | Relative risk all grades: 1.33–1.43 | [57, 58] |
| Increased risk of pneumonitis compared to chemotherapy | Relative risk all grades: 2.35–5.17 Relative risk grades ≥3: 1–4.19 |
[55, 58–60] |
| Increased risk of ICI-P with anti-PD-1/PD-L1 versus anti-CTLA-4 inhibitors | Relative risk all grades: 3.47–6.4 Unclear difference between anti-PD-1 and PD-L1 inhibitors |
[51, 52, 55, 60] |
| Increased risk of ICI-P with ICI/ICI combotherapy vesus ICI monotherapy | 3.48–3.68 for all grades | [55, 60] |
| Fatal ICI-P | Primary cause of lethal irAEs (35% of deaths) 13% fatality rate |
[53, 55] |
NSCLC: nonsmall cell lung carcinoma; PD-1: programmed cell death protein 1; PD-L1: programmed cell death ligand 1; CTLA: cytotoxic T-lymphocyte associated antigen.
Adverse events are less common and less severe with ICI monotherapy than with chemotherapy
A recent network meta-analysis [22] involving all cancer types evaluated 15 therapeutic modalities including ICI as monotherapy at different doses, ICI combination or in association with chemotherapy. This meta-analysis did not reveal any dose-related ICI toxicity and confirmed that anti-PD-1/PD-L1 monotherapy, particularly in NSCLC patients, proves to be less toxic than ipilimumab alone, conventional chemotherapy, ICI combotherapy or ICI–chemotherapy combination. Another meta-analysis [50] of adverse events observed with nivolumab and pembrolizumab in all cancer types demonstrated a significant reduction in the risk of adverse events of all grades (0.87, 0.82–0.95), adverse events of grades 3–4 (0.39, 0.29–0.53), but no significant reduction in the risk of toxic deaths (0.45, 0.19–1.09) compared with control arms including chemotherapy, everolimus or ICI combotherapy including ipilimumab. Another systematic review [21] was focused on specifically investigating irAEs that occurred with anti-PD-1/PD-L1 drugs in NSCLC patients. In this study, irAEs of all grades were more common with anti-PD-1 drugs compared to anti-PD-L1 (16% versus 11%, p=0.07), except for grade 3–5 toxicities (≈3%); this difference was particularly relevant for ICI-P (4%, 3–5% versus 2%, 1–3%; p=0.01).
Frequency of pneumonitis in patients receiving ICIs
In a meta-analysis including all cancer types and ICIs [51], ICI-P of all grades was observed in 2.6% of patients, representing the fifth cause of irAE after cutaneous, hepatic, thyroid and colic disorders. In another study on NSCLC only [59], the ICI-P incidence was 4.8% (3.8–5.7%) for all grades and 2.0% (2–2.9%) for grades 3–5. In a third study [58], the frequency of ICI-P is 2.6% (1.7–3.8%) for all grades and all tumours.
In a meta-analysis focusing on PD-1 inhibitors, the estimated ICI-P incidence in all tumour types was 2.7% (1.9–2.6%) for all grades and 0.8% (0.4–1.2%) for ICI-P grades ≥3 [57]. In this study, the frequency was higher for NSCLC and colorectal cancer (CRC) than for melanoma. Similarly, in another meta-analysis [58], ICI-P was more common in NSCLC compared to other tumour types (melanoma, head and neck cancer and urothelial cancer) for all grades, 3.1 versus 2.01% (p=0.02), as well as for grades ≥3: 1.4% versus 0.6% (p=0.03), although there was no difference found between the PD-1 or PD-L1 inhibitor types.
Increased risk of ICI-related pneumonitis in NSCLC compared to other cancers
In the meta-analysis cited above [58], the relative risk of pneumonitis after adjusting for the ICI type received was higher in NSCLC than other cancers when administering ICIs compared to chemotherapy: 1.33 (1.01–1.76, p=0.03) for all grades and 2.08 (1.52–2.65, p=0.006) for grades ≥3. In another meta-analysis [57], the relative risk of ICI-P in NSCLC and CRC was 1.43 (1.08–1.89, p=0.005) for all grades compared to melanoma, and 2.85 (1.6–5.08, p=0.01) for grades ≥3.
Increased risk of pneumonitis in patients receiving ICIs compared to chemotherapy
Four meta-analyses focused specifically on the risk of pneumonitis with ICIs in all tumour types [55, 58, 60] and in NSCLC [59]. In the first study [55], the relative risk of pneumonitis with ICIs compared to chemotherapy was 3.96 (2.02–7.79, p=0.0001) for all toxicity grades and 2.87 (0.90–9.20, p=0.08) for grades 3–4, with no difference among cancer types, or between anti-PD-1 and ipilimumab used alone. In the second study [58], the relative risk of pneumonitis was 4.7 (2.8–7.8, p=0.0001) for all grades and 3.3 (1.68–6.5, p=0.0006) for grades ≥3, for ICIs versus chemotherapy and for all tumour types. In the third study [60], the relative risk of pneumonitis was 5.17 (2.82–9.47, p=0.001) for all grades and 4.14 (1.82–9.42, p=0.001) for grades ≥3, for anti-PD-1 versus chemotherapy and for all tumour types. In the study focusing only on NSCLC, the relative risk of pneumonitis was 4.93 (2.35–10.34, p=0.001) for all grades and 4.19 (1.50–11.76, p=0.001) for grades ≥3, for anti-PD-1 compared with chemotherapy. In the last study focusing only on NSCLC [59], a relative risk of 2.35 (1.32–4.2, p=0.004) for ICIs compared with chemotherapy for all toxicity grades was observed, yet with a similar risk for the most severe grades.
Increased risk of pneumonitis with PD-1/PD-L1 inhibitors versus CTLA-4 inhibitors, but decreased risk versus ICI/ICI combotherapy
In a meta-analysis including all cancer types and ICIs [51], the relative risk of ICI-P was 3.3 (1.2–12) with anti-PD-1/PD-L1 in comparison with anti-CTLA-4, whereas there was no difference for grade ≥3 or fatal adverse events. In a similar study [52], the relative risk of ICI-P was 6.4 (3.2–12.7) with PD-1/PD-L1 inhibitors versus CTLA-4 inhibitors, with perhaps a greater risk with anti-PD-1 drugs and in cases of NSCLC or CRC compared to melanoma. However, in two other meta-analyses [55, 60], the relative risk of ICI-P was higher with nivolumab and ipilimumab combotherapy than with nivolumab monotherapy for all toxicity grades (3.68, 1.59–8.50; p=0.001 and 3.47, 1.76–6.83; p=0.01) in both studies [55, 60], yet for ICI-P grade ≥3 only in the more recent study (3.48, 1.10–11.0; p=0.01) [60]. Another study [58] adjusted for tumour types revealed that the relative risk of ICI-P was higher for pembrolizumab than nivolumab (2.08, 1.52–2.85; p=0.0001) and atezolizumab (2.43, 1.24–4.76; p=0.07), and higher for nivolumab than atezolizumab (1.91, 0.94–3.87; p=0.09) for all toxicity grades, yet without any differences for ICI-P grade ≥3.
ICI-P associated with PD-1/PDL-1 inhibitor treatment is the leading cause of death by irAE
A recent work [53] analysed irAEs-related death cases in the VigiLyze-VigiBase database, defining the risk of irAE fatality per organ (number of deaths linked to organ toxicity/number of adverse events affecting the organ). In this study, 613 deaths were observed among the 31 059 individual case safety reports. Of these deaths, 142 (23.2%) were related to ICI-P, among which 115 (80.9%) cases were associated with PD-1/PD-L1 inhibitor monotherapy, 15 with ipilimumab monotherapy and 12 with ICI combination. ICI-P was the leading cause of irAE mortality in ICIs used as monotherapy, accounting for 35% of cases, followed by hepatitis (22%), colitis (15%), neurological disorders (15%) and cardiomyositis (8%). Nonetheless, ICI combinations were associated with death due to digestive, cardiac or hepatic disorders, with ICI-P responsible for 14% of death cases. In contrast, the fatality rate from ICI-P was 13% compared to 40% from cardiomyositis. In the same study, a meta-analysis including only irAE-related death cases was conducted. A fatal irAE was reported in 122 (0.6%) of the 19 217 patients from 112 studies. A fatal irAE was found in 0.36% and 0.38% of patients exposed to anti-PD-1 and anti-PD-L1, respectively. In these patients, 42% of deaths were caused by ICI-P, compared to 15% by cardiomyositis. A fatal irAE with anti-CTLA-4 was reported in 1.08% of patients, 5% of which were due to an ICI-P. A fatal irAE was reported in 1.23% of patients exposed to an ICI combotherapy, caused by an ICI-P in 21% of cases. Infectious pneumonia or sepsis was recorded in 10% of patients who died from irAE [53] (see later).
ICI-related pneumonitis in series and case reports
Since 2015, >200 cases of ICI-P have been reported as isolated cases [61–74] or retrospective series involving between eight and 64 patients [75–80] (tables 2 and 3). Three series only included NSCLC patients [77–79], while the others involved different cancer types and, in particular, melanomas (20–95%) [75, 76, 80]. Almost all patients (84.4%) from the reported series received ICI monotherapy, consisting of anti-PD-1 (n=133), anti-PD-L1 (n=13) or ipilimumab (n=11), while 29 patients (15.6%) were given nivolumab and ipilimumab combotherapy.
TABLE 2.
Clinical characteristics, time to onset and risk factors of immune checkpoint inhibitor-related pneumonitis (ICI-P) in published series
| First author [ref.] | Subjects | Type of cancer | ICI-P | Treatment | Patient characteristics | Time to onset | Risk factors for ICI-P |
| Abdel-Wahab [75] | 251 All irAEs |
Melanoma 95.6% NSCLC 1.2% |
10 (4%) | Ipilimumab 60% Nivolumab 30% Pembrolizumab 10% |
Male 63% (total population) Age 60 years (total population) Smokers? |
53% during 2nd and 3rd injection (total population) | |
| Naidoo [76] | 915 | Melanoma 60% NSCLC 20% Other 17% |
43 (5%) | aPD-1 93% aPD-L1 7% Combo 44% |
Male? Age 67 years Smokers 67% |
12 (1.3–82) weeks Mono 19.7 weeks Combo 11.6 weeks |
Combo versus mono, 10 versus 3% (p=0.001) aPD-1 versus aPD-L1, 4 versus 1% (p=0.13) |
| Delaunay [80] | 1828 | NSCLC 75% Melanoma 20.3% Others 4.7% |
64 (3.5%) | Ipilimumab 6.9% aPD-1 79% aPD-L1 14% Trials 9.4% |
Male 84.4% Age 59 years Smokers 83% |
9.9 (1–117) weeks | |
| Kato [78] | 111 | NSCLC 100% | 8 (7.2%) | Nivolumab 100% | Male 100% Age 65 years Smokers 100% |
5.3 (2.3–24) weeks | |
| Suresh [77] | 205 | NSCLC 100% | 39 (19%) | Nivolumab 92% Combo 21% |
Male 82% Age 68 years Smokers 95% |
2.9 (3–26) weeks | Squamous versus non-squamous RR: 2.29 (1.08 versus 4.83) Female versus male 0.25 versus 0.19 person-year Combo versus mono 0.28 versus 0.18 person-year |
| Cho [79] | 167 | NSCLC 100% | 22 (13%) | Nivolumab 59% Pembrolizumab 32% Nivolumab–iplimumab 9% |
Male 76% Age ≥70 years 30% Smokers 70% |
7.7 (2.9–139) weeks | Mono versus combo, 13.6 versus 10% Pembrolizumab versus nivolumab 12.6 versus 16.3% Age ≥70 years, 30.3% versus 54.5%; p=0.025 ILD 18.2% versus 2.8%; p=0.002 Extrathoracic metastasis 31.8% versus 58.6%; p=0.019 |
Data are presented as n or n (%), unless otherwise stated. irAE: immune-related adverse event; NSCLC: nonsmall cell lung cancer; aPD-1: antibody anti-programmed cell death-1, aPD-L1: antibody anti-programmed cell death ligand-1; combo: combination therapy; mono: monotherapy; ILD: interstitial lung disease.
TABLE 3.
Severity, treatment and follow-up of immune checkpoint inhibitor-related pneumonitis (ICI-P) in series
| First author [ref.] | Subjects n | ICI-P n | Grade | Cancer response | ICI treatment | Corticosteroids | Antibiotics | ICI-P evolution | Other treatments |
| Naidoo [76] | 915 | 43 60% ipilimumab# |
Grade 1–2: 71% Grade ≥3: 29% Grade 5: 2.3% |
CR+PR 61% SD 34% PD 5% |
Pursued 48% Suspended 28% Stopped 24% |
51.6% 50 (20–80) mg 68 (20–154) days |
ND | Resolved 74.4% Improved 11.6% Worsened 11.6% |
Yes Infliximab or CPM (n=5) |
| Delaunay [80] | 1828 | 64 | Grade 1–2: 55% Grade ≥3: 45% Grade 5: 17% |
CR+PR 36% SD 33% PD 11% Not known 20% |
Pursued 8% Suspended 17% Stopped 75% |
86.9% 80 (20–240) mg 27 (4–251) days |
66.1% | Resolved 28.6% Improved 39.7% Stable 20.6% |
No |
| Kato [78] | 111 | 8 | Grade 1–2: 75% Grade ≥3: 25% Grade 5: 13% |
ND | ND | 87.5% ND ND |
ND | Resolved 87.5 | Yes CPM (n=1) |
| Suresh [77] | 205 | 39 | Grade 1–2: 36% Grade ≥3: 64% Grade 5: 13% |
ND | ND | 100% 1 mg·kg−1 per day ND |
ND | Resolved 5.1% Improved 64% Worsened 17.9% |
Yes 2/2 MMF improved 2/3 infliximab improved |
| Cho [79] | 167 | 22 | Grade 1–2: 68% Grade ≥3: 32% Grade 5: 18% |
CR+PR 23% SD 45% PD 32% |
Pursued 5% Suspended 32% Stopped 63% |
77% 0.8 (0.4–11.7) mg·kg−1 27 (2–269) days |
59% | Resolved 22.7% Improved 27.3% Stable 4.5% |
No |
CR: complete response; PR: partial response; SD: stable disease; PD: progressive disease; ND: not done; CPM: cyclophosphamide; MMF: mycophenolate mofetil. #: in this study, 60% of subjects were melanoma patients treated using ipilimumab.
In these series, the prevalence of ICI-P was evaluated at between 3.5% and 19% of ICI-exposed patients. This higher prevalence than that reported in the phase III trials (see earlier) may reflect the increased ICI-P risk due to treatment of fewer selected patients or publication biases, since three of the reported series involved exclusively NSCLC patients, with a ICI-P risk. Indeed, ICI-P prevalence appears to be superior in the NSCLC series (7.2–19%) [77–79] than in series including different types of cancers (3.5–5%) [75, 76, 80]. Similarly, data from series seem to show a higher frequency of pneumonitis in patients receiving an ICI combination (4%) rather than a monotherapy (1%) [76]. In the Cho et al. [79] study, pneumonitis was more common in patients receiving nivolumab (16.3%) than pembrolizumab (12.6%), which is clearly not the case in the meta-analyses (see earlier).
Time to onset and risk factors
The time to onset of pneumonitis was shown to vary between 5.2 and 12 weeks in the series, being shorter in the NSCLC series (2.9–7.7 weeks) [77–79]. In the Delaunay et al. [80] series, the time to onset in NSCLC and melanoma patients was 2.1 months and 5.2 months, respectively. However, NSCLC patients were subject to other risk factors than those suffering from other cancers.
In the NSCLC only series, the proportion of patients aged >70 years or of those with prior interstitial lung disease (ILD) was higher in patients with ICI-P than those without (54.5% versus 30.3% and 18.2% versus 2.8%, respectively) [79]. In the study by Suresh et al. [77], the relative risk of pneumonitis was 1.34 (0.67–2.66) in males compared with females, with an annual pneumonitis risk of 0.25 per patient-year and 0.19 per patient year for males and females, respectively. In contrast, smoking was not a particular risk factor in these series [77, 78].
In these two series, the squamous cell histological type was more common in patients with ICI-P, with a relative risk of 2.38 (1.12–5.26) recorded in the Suresh et al. [77] series. However, in the study by Cho et al. [79], the proportion of tumours with positive PD-L1 expression did not differ between patients with ICI-P or without. In this study, the presence of extrathoracic metastases was less frequent (31.8% versus 58.6%) in patients with pneumonitis, whereas previous ILD (6.03, 1.19–30.45) and the absence of extrathoracic metastases (2.94, 1.08–7.69) were features independently associated with an increased ICI-P risk [79].
Clinical characteristics, computed tomography scan findings and pulmonary function tests at presentation
Most patients with ICI-P from the series were males aged >60 years and smokers in more than two-thirds of the cases [75–80]. The tumour was shown to be controlled in the majority of patients at the time of ICI-P diagnosis, with an objective response in 22.7–61% of cases, stable disease in 32.8–45.5%, and progression in 5–31.8% [76, 78, 80]. Fewer than one-third (7–33%) of patients were clinically asymptomatic at diagnosis [76, 79, 80], pneumonitis being identified upon computed tomography (CT) scan monitoring of cancer. The main symptoms described were dyspnoea (41–80%), followed by cough (23–53%) and more rarely, chest pain (7%) [75, 76, 78–80]. Hypoxaemia and acute respiratory distress syndrome were reported in 38% and 30% of cases, respectively [75, 79]. Fewer than one-third of patients had fever (12–33%) [76, 78, 80]. Interestingly, the frequency of other concomitant irAEs was 58% in the Naidoo et al. [76] series, particularly cutaneous signs (18%), colitis (14%) or endocrine disorders (14%).
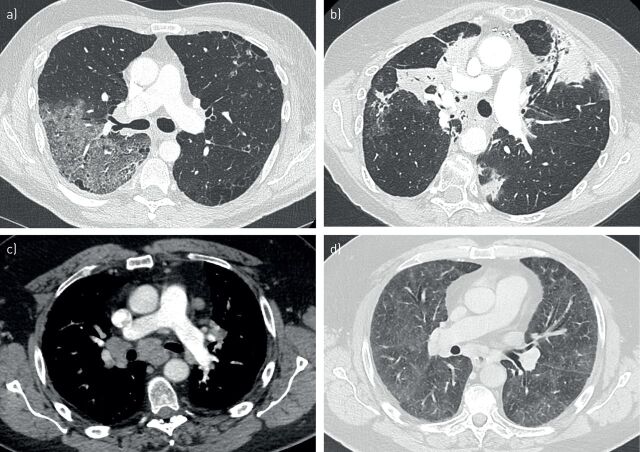
A CT scan was performed in the majority of ICI-P cases, with homogenous elementary radiological lesions detected in the 180 thoracic CT scans retrieved in the literature, 160 of which were described in the published series [75–80] and 20 in isolated case reports [61–74] (table 4). These were mainly ground-glass opacities (n=120, 66.7%) (figure 2a), consolidations (n=102, 56.6%) (figure 2b), reticular opacities (interlobular lines, interlobular septal thickenings) (n=47, 26.1%), bronchiectasis (n=19, 10.5%) and micronodules (n=7, 4%). A “crazy-paving” feature was described in one series (n=2, 1.1% of cases) [80] and bronchiolitis in two series, either alone (n=9, 5% of cases) [79, 80] or associated with ground-glass opacities and consolidations (50% of cases) [79]. An acute interstitial pneumonia pattern was suggested in one case reported in a patient presenting with respiratory failure [74]. Isolated pleural effusion was reported in two cases [81, 82]. There were no hilar or mediastinal lymphadenopathies described in ICI-P other than those related to the treated cancer or in cases of ICI-related sarcoidosis (see earlier). The lesion extent was described in two series [76, 80]. In the Naidoo et al. [76] study, three lesion categories were defined: mild (extension to a lobe or 25% of the lung parenchyma), moderate (extension >1 lobe or 25–50% of the lung parenchyma) and severe (extension to all lobes or diffuse to both lungs). In this study, 56% of pneumonitis cases were classified as mild, 22% as moderate and 22% as severe. In the study by Delaunay et al. [80], the pneumonitis was considered to be diffuse in 78.9% of patients and focal in the others. Several authors [74, 76, 77, 79, 80] have attempted to describe radiological patterns for idiopathic interstitial pneumonias [83], mostly consisting of organising pneumonia, nonspecific interstitial pneumonitis (NSIP) and hypersensitivity pneumonitis, depending on the CT scan abnormality patterns observed, and very infrequently as usual interstitial pneumonitis (UIP) or acute interstitial pneumonia with diffuse alveolar damage. The authors did not employ the same terminology for the abnormality patterns, and it is thus difficult to draw comparison between the published series. Of note, organising pneumonia (figure 2b) has been the most frequent pattern observed in 19–100% of patients from the published series [76, 77, 79, 80] and in 62.5% of the case reports [61–72].
TABLE 4.
Elementary radiological lesions observed on thoracic computed tomography scan in patients with immune checkpoint inhibitor-related pneumonitis
| Series | Case reports | Total | |
| Subjects | 160 | 20 | 180 |
| Ground glass | 105 (65.6) | 15 (75) | 120 (66.7) |
| Condensations | 92 (57.5) | 10 (50) | 102 (56.6) |
| Reticular opacities | 44 (27.5) | 3 (15) | 47 (26.1) |
| Bronchiectasis | 18 (11.3) | 1 (5) | 19 (10.5) |
| Micronodules | 6 (3.8) | 1 (5.5) | 7 (3.8) |
Data are presented as n or n (%).
FIGURE 2.
Thoracic computed tomography (CT) findings in patients with immune checkpoint inhibitor (ICI)-related pneumonitis and sarcoid-like granulomatosis. a) Transverse CT scan showing ground-glass opacity in the right upper lobe; b) transverse CT scan showing multifocal air-space consolidations with subpleural and basal distribution suggestive of an organising pneumonitis (note small ground-glass opacity surrounding consolidations); c and d) transverse CT scan in a patient with histologically proven ICI-related sarcoid-like granulomatosis showing mediastinal and bilateral and symmetric lymphadenopathies (c, mediastinal window) associated with unusual diffuse and bilateral ground-glass opacities (d, parenchymal window).
The respiratory functional impact was almost never reported in the published series and case reports. However, five out of the 10 patients in the Kato et al. [78] series received oxygen therapy at the time of ICI-P diagnosis and oxygen saturation was <90% in five out of seven isolated reported cases [61, 62, 64, 66, 67]. Moreover, eight out of 16 patients and nine out of 12 patients in the Naidoo et al. [76] series had, initially, a lowered forced expiratory volume in 1 s and diffusing capacity of the lung for carbon monoxide (DLCO), respectively. Otherwise, Franzen et al. [84] prospectively followed 71 patients with melanoma treated using ipilimumab, using pulmonary function tests. These authors reported a significant decrease in forced vital capacity (FVC) (>10%) or DLCO (>15%) after 9 weeks observed in nine (24%) out of 38 patients, with one of the patients presenting with pneumonitis in a thoracic CT scan. Therefore, the place of FVC or DLCO for the screening or the early diagnosis of ICI-P remains unclear in patients regularly assessed by thoracic CT scan upon follow-up.
Bronchoalveolar lavage and histology in ICI-P
Only a few studies have reported the results of bronchoalveolar lavage (BAL) or pulmonary biopsies. The BAL studies found lymphocyte alveolitis in six case reports [61, 62, 64–67, 71], with a lymphocyte proportion between 32.5% and 82% and no pathogens found. In four cases, transbronchial lung biopsies (TBLB) were performed [61, 64, 65, 67], with organising pneumonia lesions detected in three cases and nonspecific lesions in the last case. Likewise, a surgical lung biopsy performed in two cases revealed an organising pneumonia [66, 69]. Similar results have been described in three series. In the Naidoo et al. [76] study, pulmonary biopsy results (TBLB n=8, core biopsies n=2, surgery n=1) were available for 11 (25.5%) patients. Histopathological findings were as follows: cellular interstitial pneumonitis in four patients, organising pneumonia in three, diffuse alveolar damage in one and no abnormalities identified in three patients. In the Delaunay et al. [80] study, BAL was performed in 35 (55.6%) patients and showed T-lymphocytic alveolitis in 24 (37.5%) cases with a median of 33.5 (1–70)% lymphocytes. Microbiological evaluations (viruses, bacteria, fungi and parasites) were negative. Six patients had TBLB that showed inflammatory and lymphocytic infiltration. Finally, in the series by Cho et al. [79], BAL was performed in five patients and a median lymphocyte proportion of 14.0 (4.0–90.0)% in the lavage fluid. Altogether, these results were consistent with CT scan findings (see earlier) predominantly showing patterns of organising pneumonia and NSIP, suggesting an immuno-mediated mechanism of ICI-P, thus explaining the usual good response to corticosteroid therapy after discontinuing immunotherapy. However, it must be emphasised that no patient developed a connective tissue disorder, but none of the reported cases underwent autoimmune biological evaluation.
Grades of severity, outcomes and cancer prognosis
Most patients displayed a grade ≤2 disease severity (35.8–73%) at diagnosis in the published series [76–80], the mortality varying between 2.3% and 18%. Mortality was more marked (13–18%) in the NSCLC series [77–79]. In the Delaunay et al. [80] study, no patient died from ICI-P among melanoma patients, whereas 5% died among NSCLC patients. Conflicting data exist between series in terms of ICI-P severity in patients receiving monotherapy or ICI combotherapy [76, 79]. By contrast, while most patients (14 out of 17) were reported as isolated cases with a grade ≥3 ICI-P [61–74], only one death was observed [74].
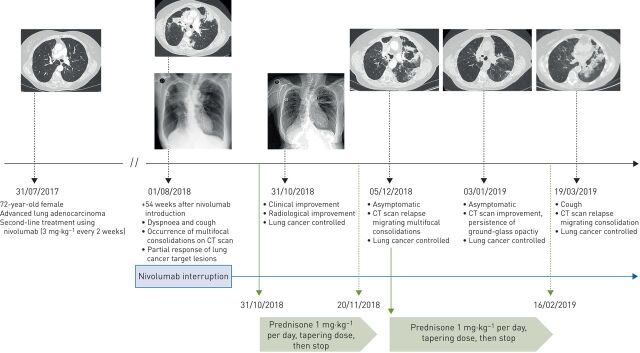
At ICI-P diagnosis, immunotherapy was halted in most (63–100%) patients and in all those with grade ≥2 toxicity [75–80]. In two series [79, 80], more than half of patients received broad-spectrum antibiotic therapy, without documented bacterial infection in almost all cases. Except in patients with grade 1 pneumonitis, all patients received corticosteroids, either orally or intravenously, at an initial daily dose ranging from 30 mg to 1000 mg prednisolone/prednisone equivalent [61, 64–74]. CT imaging resolved or remained stable in 49.6–88% and 12.8–18.8% of cases, respectively [76–80]. In the Naidoo et al. [76] series, improvement was observed in 100%, 92.8% and 58.3% of patients with grade 1 (n=17), grade 2 (n=14) and grade ≥3 (n=12) pneumonitis, respectively. The time to resolution/improvement was 27 (<7–>220) days in two different series [78, 80]. In one series, 25% of patients relapsed after steroid cessation, with two-thirds of them improving after corticosteroids were reintroduced [76] (figure 3). Initial or secondary pneumonitis worsening was observed in 11.6% and 17.9% of patients in the Naidoo et al. [76] and Suresh et al. [77] studies, respectively. In such refractory ICI-P, other immunosuppressants have been employed [76–78], including mycophenolate mofetil, with two out of two patients improving; infliximab alone, with two out of six patients improving; infliximab plus cyclophosphamide, with two out of two patients dying; cyclophosphamide alone, with the sole patient dying; as well as intravenous immunoglobulins, with the sole patient failing.
FIGURE 3.
Multiple relapsing immune checkpoint inhibitor-related pneumonitis (ICI-P) after immunotherapy cessation and corticosteroids treatment. A 72-year-old female with an advanced lung adenocarcinoma experienced an ICI-P 54 weeks after second-line treatment using nivolumab (3 mg·kg−1 every 2 weeks). She complained of dyspnoea and cough without fever. Thoracic computed tomography (CT) scanning showed bilateral multifocal air-space consolidations. Lung cancer evaluation confirmed the persistence of a partial response. Bronchioloalveolar lavage identified a CD8 T-lymphocytic alveolitis, with no pathogens identified. The diagnosis of nivolumab-related organising pneumonitis was considered. Nivolumab was interrupted, and prednisone 3 mg·kg−1 per day initiated. The patient improved clinically and radiologically. However, two attempts to discontinue corticosteroids were associated with a clinical or radiological relapse, whereas the lung cancer remained controlled.
After complete clinical and radiological resolution, ICI was reintroduced in 10 (17.2%) [80], 12 (28%) [76] and seven (31.8%) [79] patients from three series that had previously presented a grade ≤2 pneumonitis. These patients experienced pneumonitis relapses in 30%, 25% and 0% of cases, respectively.
Whereas a link between irAE occurrence and a better cancer prognosis in ICI-treated patients had previously been reported [77, 85], Suresh et al. [77] revealed a poorer prognosis in their NSCLC patients presenting with ICI-P, with a 2.7 greater risk of death than the non-ICI-P patients.
ICI-related pneumonitis in special patient groups
Two particular settings must be mentioned here, as they either expose an increased ICI-P risk in the patients or because the patients' respiratory conditions may be aggravated by ICI treatment. The first setting refers to patients who have received or must receive thoracic radiotherapy (TRT), and the second to patients with lung cancer occurring in the context of a previously-known ILD.
Radiation pneumonitis or ICI-P in cancer patients receiving TRT?
Although radiotherapy is likely to prime the immune response [86], most data on combining palliative radiation therapy (intra- and extra-cranial irradiation) with anti-PD-1 [87–92] or anti-CTLA-4 inhibitors [87, 88, 93, 94] have not revealed excessive radiation toxicity (compared to those receiving radiotherapy without immunotherapy) or excessive irAEs (compared to those receiving immunotherapy alone). In the NSCLC setting, the safety data were shown to be similar, and combining extrathoracic radiation therapy and ICIs was demonstrated to be safe [95–98]. In Lesueur et al. [96], ICI-pneumonitis of grade 1–2 occurred in three (4.6%) cases and grade 3–4 in three to four (1.5%) cases among 104 NSCLC patients administered extra-TRT in the 6 months prior, during or in the 3 months following nivolumab treatment.
Concerning conventional TRT, based on retrospective data, irAEs such as pneumonitis were demonstrated not to be common in metastatic lung cancer patients treated using both ICIs and TRT [98, 99]. However, other studies have suggested a link between prior radiation pneumonitis and increased frequency of either radiation pneumonitis or ICI-P after nivolumab exposure [100–102]. In a retrospective analysis involving 201 Asian NSCLC patients receiving nivolumab, of whom 50 had been treated with TRT, the frequency of ILD was 9.6%, 22.0% with a relative risk of 2.37 (1.15–4.88) and 26.5% with a relative risk of 2.76 (1.33–5.73) in those who had not received TRT, those who had received TRT and those who had developed radiation pneumonitis, respectively [100]. These findings support an increased ICI-P risk rather than that of radiation pneumonitis in patients previously exposed to TRT. Recently, the occurrence of radiation pneumonitis was reported at 3 and 5 months after lung stereotactic body radiotherapy in one patient previously treated with atezolizumab for a colorectal carcinoma and in another treated with pembrolizumab for a melanoma, respectively [102].
The phase III PACIFIC study revealed a light increase in radiation pneumonitis or ICI-P in unresectable stage III NSCLC patients receiving durvalumab or its placebo after concurrent chemoradiotherapy [12, 103]. Pneumonitis occurrence of all grades was higher in durvalumab (33.6%) versus placebo (24.9%) patients, whereas pneumonitis occurrence of grades 3/4 was similar in the two groups (3.4% and 2.6%, respectively). Radiation pneumonitis or ICI-P leading to durvalumab and placebo discontinuation was observed in 6.3% and 4.3% of patients, respectively. In an exploratory analysis [104], median time to pneumonitis onset from treatment start onwards did not differ between the groups (55 days), nor did pneumonitis median duration, being 64 days for durvalumab and 57 days for placebo. Pneumonitis was more commonly observed in Asian patients (47.9% versus 17.6%) or in those with epithelial growth factor receptor-driven NSCLC (11% versus 3.8%), whereas durvalumab did not seem to increase pneumonitis risk in either population. Previous respiratory disorders, radiotherapy doses or cisplatin or carboplatin use were not associated with higher pneumonitis rates.
Acute exacerbation or ICI-P in cancer patients with previous ILD?
The lung cancer risk is increased during ILD (LC-ILD), particularly in case of idiopathic pulmonary fibrosis [105–107]. In this setting, therapeutic patient management is more complex, as most patients are elderly male smokers, former smokers or patients with several comorbidities. All therapeutic approaches, such as surgery, chemotherapy or tyrosine kinase inhibitors, expose these patients to an increased risk of acute ILD exacerbation, conventional chest radiotherapy being contraindicated. The risk of exacerbation is even higher in patients with more extensive radiological involvement, a radiological pattern of UIP, or a decrease in FVC or DLCO. This increased risk has been suggested in two retrospective series focused on ICI-P [79, 80]. Therefore, the place of ICI treatment in the context of LC-ILD must be further questioned.
Very few data are currently available, except for a few clinical case reports [82, 108, 109], a prospective pilot study [110] and a retrospective Asian patient cohort [111]. All these studies concern the use of nivolumab in patients with idiopathic ILD in the majority of cases. The isolated case reports [82, 108, 109] involved five male smokers/former smokers (except one), aged 62–87 years, and with advanced NSCLC (squamous cell carcinoma n=3, adenocarcinoma n=2). The chest CTs revealed a UIP pattern. The FVC was between 74% and 101%, and DLCO between 27% and 64%. One patient was under long-term oxygen therapy [108], and one patient received pirfenidone [109]. All received nivolumab as a second-line treatment. One patient experienced a complete response for >12 months [82], one a partial response for 6 months [109], one a stabilisation for 8 months [108] and two a progressive disease [109]. None of the patients had a respiratory adverse event related to nivolumab. However, one patient died of viral pneumonia [108] and three others died of their cancer between 3 and 8 months after ICI treatment initiation [108, 109].
The Fujimoto et al. [110] pilot trial sought to investigate the safety of nivolumab as second-line treatment in six patients with advanced NSCLC and an idiopathic ILD of mild severity defined by a FVC ≥80% and absent UIP (certain) pattern at CT. All were old male smokers aged 69–81 years, with a performance status of 1 and advanced NSCLC (adenocarcinoma n=3, NSCLC otherwise specified n=3). The CT scan pattern suggested a possible UIP in five patients and an ILD inconsistent with a UIP in one; the FVC was ≥88%. None of the patients had a respiratory adverse event after 3 months of follow-up. Three partial responses and three cancer stabilisations were observed.
Finally, the largest experience reported was that of the retrospective Kanai et al. [111] cohort, involving 216 advanced NSCLC patients treated with nivolumab as second-line or more depending on the presence (n=26) or lack (n=190) of an ILD observed at the time of lung cancer diagnosis. The LC-ILD patients were had a median age of 71 (55–85) years, with 77% being male, 96% smokers/former smokers and 65% exhibiting a performance status ≤1. The histological cancer type was adenocarcinoma in 50% of cases (without oncogenic addiction) and squamous cell carcinoma in 42%. Compared to the overall cohort, the LC-ILD patients were more likely to smoke (p=0.02), with their tumours harbouring less often oncogenic addiction (p=0.003) and receiving less treatment before nivolumab (p=0.001). ILD exhibited a NSIP pattern in 54% of patients and a UIP pattern in the remaining 46%. ILD extension on CT scan was 5–25% for 77% (n=20) of the patients, <5% for 15% and 25–50% for 8% of patients. There were no data on the pulmonary function tests. ILD was associated with rheumatoid arthritis in 27% of the patients (versus 2% in the rest of the population, p<0.001). The nivolumab efficacy was similar in the LC-ILD patients compared to the overall population. The response assessment revealed objective response, stability and progression in 27%, 31% and 42% of patients, respectively. The median progression-free survival was 2.7 (1.7–5.3) months in the LC-ILD group versus 2.9 (2.1–3.4) months. Moreover, the respiratory adverse event rate was 31% (eight out of 26) in the LC-ILD group versus 12% in the remaining population (p=0.014). While the median time to onset did not differ, adverse event severity was higher in the LC-ILD group (grades 3–4 62% versus 42%, p=0.02). Nivolumab treatment was discontinued in all, and corticosteroids were given in 73% of the LC-ILD group compared to 63% in the remaining population. The only two risk factors found were male sex and concomitant rheumatoid arthritis. In contrast, no deaths related to pulmonary toxicity were reported for the entire cohort. The authors distinguished between an acute exacerbation of underlying ILD in four out of the eight cases and the occurrence of new images suggestive of ICI-P in the other four patients. In addition, the radiological pattern of worsening differed in patients with an NSIP and those with a UIP: appearance was that of an organising pneumonia in 60% of the former patients and that of an acute interstitial pneumonia in 67% of the latter.
Taken together, these results suggest that nivolumab administration is possible in LC-ILD patients, particularly in case of idiopathic ILD of mild to moderate severity. Nevertheless, despite similar efficacy, pulmonary toxicity is more common and more severe, especially in case of a UIP pattern. This toxicity may be considered either as an acute exacerbation of the underlying ILD or as ICI-P occurrence. The preventive role of antifibrotic treatments is as yet unknown.
ICI-related sarcoid-like granulomatosis
In addition to pneumonitis, the most frequently observed respiratory adverse event, 19 isolated cases of ICI-related sarcoid-like granulomatosis (ICI-SLG) were reported after ICI cancer treatment [112–128] (table 5).
TABLE 5.
Main characteristics of immune checkpoint inhibitor-related sarcoid-like granulomatosis
| Cases | 19 |
| Type of cancer | |
| Melanoma | 13 (72) |
| Nonsmall cell lung cancer/small cell lung cancer | 3/1 (22) |
| Others | 2 (6) |
| Type of immunotherapy | |
| Ipilimumab/ipilimumab+nivolumab | 7/4 (57) |
| Nivolumab/pembrolizumab/atezolizumab/durvalumab | 4/2/1/1 (43) |
| Male:female | 2:1 |
| Age at “sarcoidosis” diagnosis | 57 years (35–81) |
| Delay of “sarcoidosis” onset | 12 weeks (4–40) |
| Stage of “sarcoidosis” I/II/III/IV | 4 (21)/10 (53)/5 (26)/0 |
| Extrathoracic “sarcoidosis” involvement | |
| Skin | 5 |
| Spleen | 3 |
| Parotids/eyes | 1/1 |
| Brain | 1 |
| Diagnostic procedure | |
| Bronchial and pulmonary transbronchial biopsy | 7 (36.8) |
| Lymph node endobronchial ultrasound biopsy | 8 (42.1) |
| Extrathoracic biopsy | 7 (36.8) |
| “Sarcoidosis” treatment | |
| Immunotherapy interruption | 13 (69) |
| Corticosteroid treatment initiation | 9 (47) |
| “Sarcoidosis” follow-up | |
| Improvement | 16 (84) |
| Stabilisation | 3 (16) |
| Cancer follow-up | |
| Disease controlled | 12 (68.4) |
| Progressive disease | 4 (21.1) |
| Unknown | 3 (10.6) |
Data are presented as n, n (%) or median (range).
Most (73%) ICI-SLG cases were observed in melanoma patients (n=13). Similarly, grade 1 or 2 SLG occurred in seven (1.4%) of the 509 stage 3 melanoma patients treated with pembrolizumab, but in none of those treated with placebo [39]. Interestingly, in a recent meta-analysis, skin cancers, particularly melanomas (relative risk 1.64, 95% CI 1.16–2.31), were the commonest cancer type associated with sarcoidosis [129]. However, 10 (77%) out of 13 melanoma cases had also received ipilimumab monotherapy (n=7) or combined with nivolumab (n=3). In this manner, a CTLA-4 pathway dysregulation was suggested in sarcoidosis pathogenesis [130]. A decrease in CTLA-4 expression was shown in activated T-cells from lung-draining mediastinal lymph node sarcoidosis patients [130]. Evaluating T-helper cell subsets, the study authors revealed a significant decrease in CTLA-4 expression in sarcoidosis T-helper 17 cells, in association with their relative expansion. Furthermore, an increase in blood lymphocyte counts, especially of the T-helper 17 phenotype, was observed in a melanoma patient treated with ipilimumab, concomitantly to the occurrence of a sarcoid-like granulomatosis [113]. Therefore, sarcoidosis-like drug reactions may be more commonly observed when using anti-CTLA-4 treatments rather than anti-PD-1/PD-L1 inhibitors [130]. For patients receiving anti-PD-1/PD-L1, locally increased γ-interferon secretion was hypothesised [131, 132].
Concerning clinical presentation, the time to onset was 12 weeks, and the patients were most often asymptomatic or developed dyspnoea, cough or asthenia [112–128]. Thoracic CT scans revealed stage I–II sarcoidosis-like presentation in 14 of the 19 patients (73.6%) (figure 2c). However, atypical lesions were observed, such as ground-glass opacities (n=5) (figure 2d) and low abundance pleural effusion (n=2) [112–128]. Extrathoracic involvement was observed in 10 (52.6%) patients, of whom nine had melanoma, with lesions affecting skin (n=5), spleen (n=3), eyes and parotid gland (n=1) and brain (n=1) [114–118, 120–124], in line with sarcoidosis presentation [133]. Pulmonary function tests were normal among the few evaluated patients (n=6) [112, 113, 118, 120, 121, 123]. Granulomatosis lesions were obtained by bronchial biopsy, TBLB or mediastinal lymph nodes biopsies using endobronchial ultrasound in most cases (n=15), or by skin or other tissue biopsies in others [112–128]. BAL composition, when performed (n=6), usually showed lymphocytic alveolitis with a high CD4/CD8 ratio [112, 114, 117, 118, 121, 123, 134]. Positron emission tomography CT scans did not contribute significantly to the ICI-SLG diagnosis [113, 114, 118, 120–123, 127].
Given that ICI-SLG is usually asymptomatic, with only few lung parenchymal lesions and normal pulmonary function tests, ICI was definitively halted in 14 (77.8%) out of 18 patients, and prednisone was administered to nine of them [112–118, 121–124, 126–128]. Sarcoidosis resolved in all patients (including seven without steroids) except two, who remained stable without steroids [112–128]. Concerning cancer follow-up, ICI-SLG occurrence was observed as cancer was controlled and progressive in 11 (68.8%) [112, 113, 116, 117, 120–122, 125, 126] and three [114, 115, 123] out of 16, respectively, with no information available for three [118, 127, 128].
Tuberculosis, pneumonia and severe infections in cancer patients receiving ICI
ICI treatments were reported likely to be associated with an increased risk of pneumonitis due to infection, usually referred to as “pneumonia”, serious infections (septicaemia and opportunistic infections) and TB. However, this association remains uncertain, given that exposure to corticosteroids or associated comorbidities such as diabetes may also play a role.
Tuberculosis in cancer patients receiving ICI
Over the past 4 years, TB occurred in two out of 908 ICI-treated cancer patients in France, with an estimated TB incidence of 1/1000 treated patients per year [135]. Patients who developed pulmonary TB while receiving an ICI were mostly males treated with anti-PD-1 inhibitors for NSCLC. TB occurred relatively early after ICI initiation, with a 15 (4–33)-week median delay of onset, in the absence of any other immunosuppression agent except cancer [135–141]. This suggests reactivation of prior latent TB rather than rapid progression to TB of a recent de novo infection. PD-1 inhibition could favour an exaggerated immune response against latent TB, leading to overt TB [137, 140] as in TB/HIV-1 co-infected patients in the context of immune reconstitution inflammatory syndrome [142]. In this context, it would be of interest to perform γ-interferon release assays in at-risk TB patients before ICI introduction.
Among the nine pulmonary TB cases reported under ICI treatment [135–141], nearly half were asymptomatic, and the TB was revealed during a thoracic CT scan performed for the cancer follow-up. Clinical symptoms and radiological findings may have been confused with cancer progression. In a case report, pericardial effusion was initially considered as tumour infiltration [137]. However, thoracic CT scan imaging was as usual revealing nodules, cavitary lesions and pleural effusion [143], and positivity of direct examination or culture of sputum for Mycobacterium tuberculosis was rather common when performed. Pulmonary TB occurrence often led to ICI discontinuation (eight cases out of nine), along with anti-TB treatment [135–141]. However, two of the nine reported cases died [135, 140].
Pneumonia and serious infections in cancer patients receiving ICI
Pneumonia as a cause of death was identified in phase III trials [9, 29, 31, 45, 47], as well as in the VigiLyze-VigiBase database report [53], in patients receiving ICI, either alone or in combination for all cancer types. A meta-analysis was recently published concerning the incidence and increased risk of pneumonia observed in published phase II/III trials of cancer patients treated with anti-CTLA-4 alone, anti-PD-1, or anti-PDL-1, either alone or in combination with anti-CTLA-4 or chemotherapy [55, 60]. Compared with chemotherapy, PD-1 inhibitors did not show a significant increase in the risk of pneumonia for all cancer types. Compared with nivolumab or ipilimumab monotherapy, the nivolumab–ipilimumab combination did not show any increase in the occurrence of pneumonia. However, PD-L1 inhibitors were associated with a significantly increased risk of grade 1–5 pneumonia (2.11, 1.20–3.70; p<0.001) compared to control therapies, especially for atezolizumab (5.35, 2.61–10.96; p<0.001). However, there was no significant difference between nivolumab or pembrolizumab compared to the controls. Finally, an increase in grade 1–5 pneumonia remained significant with PD-L1 inhibitors (2.11, 1.20–3.70; p<0.001) as compared with control therapeutics in NSCLC patients.
Recently, two retrospective series [144, 145] reported the frequency, severity and characteristics of infections occurring in cancer patients receiving ICI. In both studies, the infection was defined via pathogen identification and initiation of a suitable anti-infection treatment, while the seriousness of infection was defined via hospitalisation requirement or parenteral treatment. The first study [144] reported the occurrence of infection over a 4-year period in three hospitals in New York (NY, USA): 54 cases of severe infection occurred in 740 (7.3%) melanoma patients treated with ICIs: ipilimumab (73%), nivolumab or pembrolizumab (14.9%), as well as nivolumab–ipilimumab combotherapy (8.9%). Infections occurred within a median of 19.2 (<1–70) weeks after immunotherapy initiation and were responsible for death in 17% of cases. Most infections were of bacterial origin (79.3%), primarily pneumonia (28.2%) and bloodstream infections (28.2%). There were three cases of invasive aspergillosis and two cases of pneumocystis pneumonia. Infections were more common in patients having received the ipilimumab–nivolumab combination, with a relative risk of 3.26 (1.70–6.27, p=0.0017), while the use of pembrolizumab was less associated with infection occurrence. Most strikingly, in 85% of patients who developed a serious infection, corticosteroids were received at a median dose of 40 mg of equivalent prednisone and for a median duration of 60 days. Similarly, 24% of these patients also received infliximab. Thus, the relative risk of developing a serious infection was 7.71 (3.71–16.18, p<0.0001) and 4.74 (2.27–9.45, p<0.0001) in patients exposed to corticosteroids and infliximab, respectively. Age, sex and prior receipt of chemotherapy or temozolomide were not associated with the development of serious infection.
The second study [145] reported the occurrence of 32 infections in 167 nivolumab-treated NSCLC patients from Kyoto (Japan). Infections occurred on average 12.8±10.1 weeks after immunotherapy initiation, with no reported deaths. The majority of infections were of bacterial origin (78.1%), primarily pneumonia or pulmonary abscess (76%). There was one case of pulmonary TB, one case of invasive pulmonary aspergillosis and four cases of influenza. Infections were more common in patients with type II diabetes, with an independent relative risk of 3.61 (1.14–11.4, p<0.001). In this study, except for higher age, sex, smoking habit, presence of underlying lung disease (especially chronic obstructive pulmonary disease), prior receipt of chemotherapy and duration of nivolumab treatment, previous treatment with corticosteroids were not associated with the development of infection during ICI treatment for NSCLC.
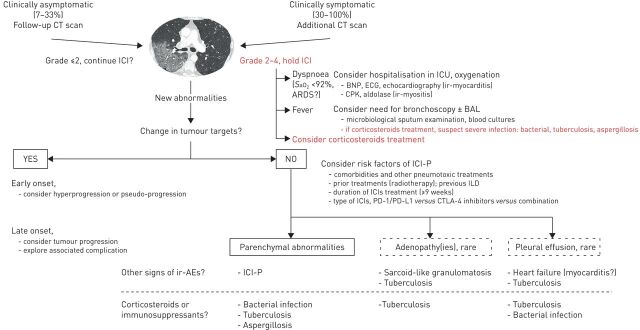
Management of pulmonary complications of ICI and suspected ICI-P
Figure 4 presents an algorithm proposal for the management of pulmonary complications in ICI-treated patients with advanced NSCLC. A multidisciplinary approach, including a pulmonologist, oncologist and radiologist, was applied to obtain the diagnosis, thus enabling the best therapeutic strategy for the patient. ICI-P diagnosis is based on the exclusion of other differential diagnoses, such as tumour progression, pulmonary infection or cardiac dysfunction. However, some risk factors were shown to increase the diagnostic probability of ICI-P (figure 4).
FIGURE 4.
Proposed algorithm for the management of suspected immune checkpoint inhibitor-related pneumonitis (ICI-P). Schematically, two settings may present in a patient treated with ICI for a nonsmall cell lung carcinoma: either new images occur on the cancer follow-up computed tomography (CT) scan or the CT scan is performed because of new respiratory (cough and dyspnoea) or general symptoms (fevers and extrathoracic signs). In each case, CT scan analysis should focus on cancer progression (probable progression) or the occurrence of new parenchymal abnormalities; particularly ground-glass opacities or condensation(s) (possible ICI-P or infection), pleurisy or mediastinal lymphadenopathy being more rarely observed. In case of respiratory or general symptoms, their severity must be graded and a hospitalisation considered in view of the appropriate diagnostic tests and symptomatic treatment initiation. In case of a fever, an extensive microbial investigation must be carried out, particularly if the patient is under immunosuppresants. ICI must be stopped and the initiation of high-dose corticosteroid therapy discussed. In the absence of tumour progression, the discussion between ICI-P or infectious pneumonia is likely to depend on concomitant respective risk factors and on the documentation of an infection. ICU: intensive care unit; BNP: bone natriuretic protein; CPK: creatine phosphokinase; BAL: bronchioloalveolar lavage; ir: immune-related; AE: adverse events; ARDS: acute respiratory distress syndrome; ILD: interstitial lung disease: SaO2: arterial oxygen saturation; PD-1: programmed cell death protein; PD-L1: programmed cell death ligand 1; CTLA: cytotoxic T-lymphocyte associated antigen.
Schematically, two situations can occur. Either radiological abnormalities are fortuitously discovered during the cancer follow-up scan [76, 80], or the CT scan is performed because of the occurrence of new respiratory (cough, dyspnoea) or general symptoms (fevers, extrathoracic signs). By definition, respiratory adverse events discovered incidentally are grade 1 toxicities, while those associated with symptoms are grade ≥2. In symptomatic patients, appropriate diagnostic tests depending on the symptoms must be performed to rule out other causes. In a case of dyspnoea, immune-related myocarditis/myositis should be ruled out, and in a case of fever, bacterial pneumonia, tuberculosis and opportunistic infections must be excluded (figure 4).
The main cause of new radiological abnormalities or respiratory symptoms is cancer progression. In the first month of ICI treatment, hyperprogressive disease was reported to occur in 4–29% of patients without any clearly identified risk factor [28, 146], while pseudoprogression occurs in <9%. The decision to pursue ICI treatment beyond progression should be made for carefully selected patients with clinical improvement yet without severe toxicities [147]. After eliminating tumour progression, an accurate analysis of radiological patterns should be performed to reinforce the ICI-P diagnosis. The most frequent abnormalities are ground-glass opacities and multifocal condensations, suggesting an organising pneumonitis pattern (see earlier). The results of a bronchoscopy with BAL is able to exclude pulmonary infection and may reveal a lymphocytic alveolitis.
ICI-P treatment differs between symptomatic and asymptomatic patients. Several oncology societies have issued recommendations with uncertain levels of evidence (table 6) [23–25]. Briefly, for asymptomatic ICI-P, ICI might be continued while monitoring the development of symptoms, pulmonary function decline (FVC and DLCO) and ILD parenchymal extension by CT scan. If symptoms appear, ICI will be interrupted, bronchoscopy with BAL will be performed and treatment with corticosteroids (see later) should be started in the absence of documented pulmonary infection. In these patients, the ICI may possibly be resumed later, especially if the cancer was well controlled at the time of the occurrence of ICI-P (see later). If no symptoms appear, but the ILD extends on lung CT and/or the pulmonary functions are deteriorating at a 4- or 6-week follow-up, our approach is to withdraw the ICI and to introduce an oral corticosteroid treatment (0.5–1 mg·kg−1 per day of prednisone/prednisolone equivalent). In this setting, provided that the cancer remains controlled and there is no sign of ILD fibrosing evolution (reticulation, honeycombing, architectural distortion/traction bronchiectasis or loss of lung volume) on the CT scan, the ICI may possibly be resumed later. However, if ICI-P does not improve, and a fortiori it worsens, ICI will be permanently discontinued and intravenous methylprednisolone therapy will be started.
TABLE 6.
Management of pneumonitis in patients treated with immune checkpoint inhibitors (ICI) according to the American Society of Clinical Oncology (ASCO), European Society For Medical Oncology (ESMO) and Society for Immunotherapy of Cancer (SITC)
| ESMO [ 23 ] | ASCO [ 24 ] | SITC [ 25 ] | |
| Grade 1 | |||
| ICI management | Consider delay of treatment | Hold ICI | Consider holding ICI |
| Treatment | No specific treatment | No specific treatment | No specific treatment |
| Patient monitoring | Monitor symptoms every 2–3 days | Monitor patients weekly clinically One CT scan to be repeated in 3–4 weeks |
Self-monitor symptoms and oxygen saturation every 2–3 days; weekly clinic visits Re-image at least prior to every cycle of ICI treatment |
| Drug re-challenge | Not specified | Yes, if radiographic evidence of improvement or resolution | Yes, with chest imaging abnormalities resolution |
| Grade 2 | |||
| ICI management | Withhold ICI | Hold ICI | Hold ICI |
| Treatment | Prednisolone 1 mg·kg−1 per day−1 orally and taper over ≥6 weeks | Prednisone 1–2 mg·kg−1 per day−1 orally and taper over 4–6 weeks | Methylprednisolone 1 mg·kg−1 per day (i.v. or oral equivalent) and taper over ⩾4 weeks |
| Patient monitoring | Bronchoscopy and bronchioloalveolar lavage: optional Monitor symptoms daily/repeat chest radiography weekly/lung function tests including TLCO |
Bronchoscopy with bronchial aspiration: optional Monitor every 3 days with history, physical examination and pulse oximetry, consider chest radiography | Bronchoscopy with bronchioloalveolar lavage: recommended Consider hospitalisation |
| Drug re-challenge | Not specified | Yes - if resolution to grade ≤1 | Yes, if symptoms and imaging abnormalities resolve |
| Grade 3/4 | |||
| ICI management | Discontinue ICI | Discontinue ICI | Discontinue ICI |
| Treatment | Empirical antibiotics/(methyl)prednisolone i.v. 2–4 mg·kg−1 per day−1; taper corticosteroids ⩾8 weeks If no improvement after 48 h, add infliximab 5 mg·kg−1 or mycophenolate mofetil |
Empirical antibiotics/(methyl)prednisolone i.v. 1–2 mg·kg−1 per day; taper corticosteroids over 4–6 weeks If no improvement after 48 h, may add infliximab 5 mg·kg−1 or mycophenolate mofetil 1 g twice a day or i.v.-immunoglobulins for 5 days or cyclophosphamide | Methylprednisolone i.v., 2 mg·kg−1 per day; taper corticosteroids ⩾8 weeks If no improvement, add infliximab or cyclophosphamide, mycophenolate mofetil or i.v. immunoglobulins |
| Patient monitoring | Bronchoscopy and bronchioloalveoar lavage: optional Hospitalisation |
Bronchoscopy with bronchioloalveolar lavage: recommended Hospitalisation |
Bronchoscopy with bronchioloalveolar lavage: recommended Hospitalisation |
| Drug re-challenge | Not specified | No | Grade 3: case-by-case; only if symptoms and imaging abnormalities resolve Grade 4: no, discontinue ICI |
CT: computed tomography; TLCO: transfer factor of the lung for carbon monoxide.
In patients with symptomatic pneumonitis, ICI should be promptly withheld, and an evaluation by a pulmonologist performed. Recommended treatment consists of ICI discontinuation, along with corticosteroid administration. In our experience, intravenous treatment with methylprednisolone 4 mg·kg−1 per day at day one, then 2 mg·kg−1 per day at days two and three, followed by an oral corticosteroid treatment with 1 mg·kg−1 per day of prednisone/prednisolone equivalent at a gradually decreasing dose is usually sufficient. A higher dose of methylprednisolone (1000 mg) has been suggested for patients with acute respiratory failure. With appropriate treatment, 70–100% of nivolumab-induced pneumonitis resolved in clinical trials, with a time to resolution of 3–6 weeks [7, 8, 32, 34, 148, 149]. In the absence of improvement within 2 days, the use of an immunosuppressive drug, such as infliximab, mycophenolate mofetil, cyclophosphamide or intravenous immunoglobulins might be considered [23–25]. Only very few data are currently available for refractory ICI-P, with a poor prognosis, given that eight out of 11 patients from a published series died, despite intensified immunosuppression [76–78].
ICI re-challenge is under discussion for grade 2 ICI-P having resolved to grade ≤1. For grade 3, there is no evidence of a safe re-challenge. Therefore, after pneumonitis has resolved, ICI reintroduction should be assessed on a case-by-case basis, along with close monitoring. For grade 4, permanent ICI discontinuation is recommended. For a second pneumonitis episode, permanent ICI discontinuation is recommended if, upon ICI re-challenge, a patient develops grade ≥2 pneumonitis.
Conclusion
ICI-P is rarely observed (<5%) during cancer treatment with immunotherapies; however, it is the most frequent pulmonary complication observed under ICI, others being ICI-SLG, TB or other infections. It is more often seen in patients with NSCLC rather than other cancers and in those receiving PD-1/PD-L1 rather than CTLA-4 inhibitors alone. Its frequency is even greater when anti-PD-1 and anti-CTLA-4 are combined. Although the fatality rate is low (≈13%), it is the leading cause (≈35%) of immune-related death under ICIs. A multidisciplinary approach involving an oncologist, pulmonologist, oncologist and radiologist is deemed necessary to obtain a diagnosis, exclude a differential diagnosis and enable the best therapeutic strategy for patients. ICI-P usually occurs in the first three treatment months, mostly reflected by respiratory symptoms, with a fever found in only one-third of cases. Risk factors for occurrence have not yet been clearly defined. In most cases, chest CT scan reveals ground-glass opacities and multifocal consolidations suggestive of organising pneumonitis, while the bronchioloalveolar scan is suggestive of lymphocyte alveolitis. ICI-P usually resolves after stopping ICI and initiating systemic corticosteroids. The role of immunosuppresants in refractory cases must be further evaluated in prospective studies. ICI re-challenge of ICI has been discussed for grade 2 ICI-P. In the near future, the ICI-P frequency and severity in the course of ICI treatment will be better defined, and its combination with chemotherapy should be quickly clarified. Additionally, prospective studies evaluating treatment strategies for ICI-P are now required to enable ICI re-challenge along with low-dose corticosteroid maintenance.
Footnotes
Provenance: Publication of this peer-reviewed article was sponsored by Boehringer Ingelheim, Germany (principal sponsor European Respiratory Review issue 153).
Conflict of interest: J. Cadranel reports grants and personal fees from AstraZeneca, Novartis and Pfizer, and personal fees from Roche, MSD and BMS, outside the submitted work.
Conflict of interest: A. Canellas reports personal fees from BMS, outside the submitted work.
Conflict of interest: L. Matton has nothing to disclose.
Conflict of interest: M. Darrason has nothing to disclose.
Conflict of interest: A. Parrot has nothing to disclose.
Conflict of interest: J-M. Naccache has nothing to disclose.
Conflict of interest: A. Lavolé has nothing to disclose.
Conflict of interest: A-M. Ruppert has nothing to disclose.
Conflict of interest: V. Fallet reports personal fees from Bristol Meyers Squib and Lilly, outside the submitted work.
References
- 1.Anagnostou VK, Brahmer JR. Cancer immunotherapy: a future paradigm shift in the treatment of non-small cell lung cancer. Clin Cancer Res 2015; 21: 976–984. [DOI] [PubMed] [Google Scholar]
- 2.Costantini A, Grynovska M, Lucibello F, et al. Immunotherapy: a new standard of care in thoracic malignancies? A summary of the European Respiratory Society research seminar of the Thoracic Oncology Assembly. Eur Respir J 2018; 51: 1702072. [DOI] [PubMed] [Google Scholar]
- 3.Berghmans T, Evison M, Blum TG, et al. New drugs in thoracic oncology: needs and knowledge – an online ERS Lung Cancer Assembly survey. ERJ Open Res 2018; 4: 00040–2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leach DR, Krummel MF, Allison JP. Enhancement of antitumor immunity by CTLA-4 blockade. Science 1996; 271: 1734–1736. [DOI] [PubMed] [Google Scholar]
- 5.Ishida Y, Agata Y, Shibahara K, et al. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J 1992; 11: 3887–3895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ribas A, Wolchok JD. Cancer immunotherapy using checkpoint blockade. Science 2018; 359: 1350–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 2015; 373: 1627–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 2015; 373: 123–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herbst RS, Baas P, Kim D-W, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016; 387: 1540–1550. [DOI] [PubMed] [Google Scholar]
- 10.Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017; 389: 255–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 2016; 375: 1823–1833. [DOI] [PubMed] [Google Scholar]
- 12.Antonia SJ, Villegas A, Daniel D, et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N Engl J Med 2017; 377: 1919–1929. [DOI] [PubMed] [Google Scholar]
- 13.Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med 2018; 378: 2288–2301. [DOI] [PubMed] [Google Scholar]
- 14.Paz-Ares L, Luft A, Vicente D, et al. Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med 2018; 379: 2040–2051. [DOI] [PubMed] [Google Scholar]
- 15.Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 2018; 378: 2078–2092. [DOI] [PubMed] [Google Scholar]
- 16.Hellmann MD, Rizvi NA, Goldman JW, et al. Nivolumab plus ipilimumab as first-line treatment for advanced non-small-cell lung cancer (CheckMate 012): results of an open-label, phase 1, multicohort study. Lancet Oncol 2017; 18: 31–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hellmann MD, Ciuleanu T-E, Pluzanski A, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med 2018; 378: 2093–2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Naidoo J, Page DB, Li BT, et al. Toxicities of the anti-PD-1 and anti-PD-L1 immune checkpoint antibodies. Ann Oncol 2015; 26: 2375–2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Postow MA, Sidlow R, Hellmann MD. Immune-related adverse events associated with immune checkpoint blockade. N Engl J Med 2018; 378: 158–168. [DOI] [PubMed] [Google Scholar]
- 20.Michot JM, Bigenwald C, Champiat S, et al. Immune-related adverse events with immune checkpoint blockade: a comprehensive review. Eur J Cancer 2016; 54: 139–148. [DOI] [PubMed] [Google Scholar]
- 21.Pillai RN, Behera M, Owonikoko TK, et al. Comparison of the toxicity profile of PD-1 versus PD-L1 inhibitors in non-small cell lung cancer. Cancer 2018; 124: 271–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu C, Chen Y-P, Du X-J, et al. Comparative safety of immune checkpoint inhibitors in cancer: systematic review and network meta-analysis. BMJ 2018; 363: k4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haanen JBAG, Carbonnel F, Robert C, et al. Management of toxicities from immunotherapy: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2017; 28: Suppl. 4, iv119–iv142. [DOI] [PubMed] [Google Scholar]
- 24.Brahmer JR, Lacchetti C, Schneider BJ, et al. Management of immune-related adverse events in patients treated with immune checkpoint inhibitor therapy: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 2018; 36: 1714–1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Puzanov I, Diab A, Abdallah K, et al. Managing toxicities associated with immune checkpoint inhibitors: consensus recommendations from the Society for Immunotherapy of Cancer (SITC) Toxicity Management Working Group. J Immunother Cancer 2017; 5: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wolchok JD, Hoos A, O'Day S, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res 2009; 15: 7412–7420. [DOI] [PubMed] [Google Scholar]
- 27.Hochmair MJ, Schwab S, Burghuber OC, et al. Symptomatic pseudo-progression followed by significant treatment response in two lung cancer patients treated with immunotherapy. Lung Cancer 2017; 113: 4–6. [DOI] [PubMed] [Google Scholar]
- 28.Champiat S, Ferrara R, Massard C, et al. Hyperprogressive disease: recognizing a novel pattern to improve patient management. Nat Rev Clin Oncol 2018; 15: 748–762. [DOI] [PubMed] [Google Scholar]
- 29.Horn L, Mansfield AS, Szczęsna A, et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N Engl J Med 2018; 379: 2220–2229. [DOI] [PubMed] [Google Scholar]
- 30.Carbone DP, Reck M, Paz-Ares L, et al. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N Engl J Med 2017; 376: 2415–2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reck M, Luft A, Szczesna A, et al. Phase III randomized trial of ipilimumab plus etoposide and platinum versus placebo plus etoposide and platinum in extensive-stage small-cell lung cancer. J Clin Oncol 2016; 34: 3740–3748. [DOI] [PubMed] [Google Scholar]
- 32.Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med 2015; 373: 23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Robert C, Schachter J, Long GV, et al. Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med 2015; 372: 2521–2532. [DOI] [PubMed] [Google Scholar]
- 34.Weber J, Mandala M, Del Vecchio M, et al. Adjuvant nivolumab versus ipilimumab in resected stage III or IV melanoma. N Engl J Med 2017; 377: 1824–1835. [DOI] [PubMed] [Google Scholar]
- 35.Ascierto PA, Del Vecchio M, Robert C, et al. Ipilimumab 10 mg/kg versus ipilimumab 3 mg/kg in patients with unresectable or metastatic melanoma: a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol 2017; 18: 611–622. [DOI] [PubMed] [Google Scholar]
- 36.Hodi FS, O'Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 2010; 363: 711–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weber JS, D'Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 2015; 16: 375–384. [DOI] [PubMed] [Google Scholar]
- 38.Robert C, Long GV, Brady B, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 2015; 372: 320–330. [DOI] [PubMed] [Google Scholar]
- 39.Eggermont AMM, Blank CU, Mandala M, et al. Adjuvant pembrolizumab versus placebo in resected stage III melanoma. N Engl J Med 2018; 378: 1789–1801. [DOI] [PubMed] [Google Scholar]
- 40.Robert C, Thomas L, Bondarenko I, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med 2011; 364: 2517–2526. [DOI] [PubMed] [Google Scholar]
- 41.Schmid P, Adams S, Rugo HS, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med 2018; 379: 2108–2121. [DOI] [PubMed] [Google Scholar]
- 42.Shitara K, Özgüroğlu M, Bang Y-J, et al. Pembrolizumab versus paclitaxel for previously treated, advanced gastric or gastro-oesophageal junction cancer (KEYNOTE-061): a randomised, open-label, controlled, phase 3 trial. Lancet 2018; 392: 123–133. [DOI] [PubMed] [Google Scholar]
- 43.Cohen EEW, Soulières D, Le Tourneau C, et al. Pembrolizumab versus methotrexate, docetaxel, or cetuximab for recurrent or metastatic head-and-neck squamous cell carcinoma (KEYNOTE-040): a randomised, open-label, phase 3 study. Lancet 2019; 393: 156–167. [DOI] [PubMed] [Google Scholar]
- 44.Ferris RL, Blumenschein G, Fayette J, et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med 2016; 375: 1856–1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kwon ED, Drake CG, Scher HI, et al. Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol 2014; 15: 700–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Motzer RJ, Escudier B, McDermott DF, et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med 2015; 373: 1803–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Motzer RJ, Tannir NM, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med 2018; 378: 1277–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Powles T, Durán I, van der Heijden MS, et al. Atezolizumab versus chemotherapy in patients with platinum-treated locally advanced or metastatic urothelial carcinoma (IMvigor211): a multicentre, open-label, phase 3 randomised controlled trial. Lancet 2018; 391: 748–757. [DOI] [PubMed] [Google Scholar]
- 49.Bellmunt J, de Wit R, Vaughn DJ, et al. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med 2017; 376: 1015–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Costa R, Carneiro BA, Agulnik M, et al. Toxicity profile of approved anti-PD-1 monoclonal antibodies in solid tumors: a systematic review and meta-analysis of randomized clinical trials. Oncotarget 2017; 8: 8910–8920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.De Velasco G, Je Y, Bossé D, et al. Comprehensive meta-analysis of key immune-related adverse events from CTLA-4 and PD-1/PD-L1 inhibitors in cancer patients. Cancer Immunol Res 2017; 5: 312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khoja L, Day D, Wei-Wu Chen T, et al. Tumour- and class-specific patterns of immune-related adverse events of immune checkpoint inhibitors: a systematic review. Ann Oncol 2017; 28: 2377–2385. [DOI] [PubMed] [Google Scholar]
- 53.Wang DY, Salem J-E, Cohen JV, et al. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol 2018; 4: 1721–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wang P-F, Chen Y, Song S-Y, et al. Immune-related adverse events associated with anti-PD-1/PD-L1 treatment for malignancies: a meta-analysis. Front Pharmacol 2017; 8: 730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Abdel-Rahman O, Fouad M. Risk of pneumonitis in cancer patients treated with immune checkpoint inhibitors: a meta-analysis. Ther Adv Respir Dis 2016; 10: 183–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Khunger M, Rakshit S, Pasupuleti V, et al. Incidence of pneumonitis with use of programmed death 1 and programmed death-ligand 1 inhibitors in non-small cell lung cancer. Chest 2017; 152: 271–281. [DOI] [PubMed] [Google Scholar]
- 57.Nishino M, Giobbie-Hurder A, Hatabu H, et al. Incidence of programmed cell death 1 inhibitor-related pneumonitis in patients with advanced cancer: a systematic review and meta-analysis. JAMA Oncol 2016; 2: 1607–1616. [DOI] [PubMed] [Google Scholar]
- 58.Ma K, Lu Y, Jiang S, et al. The relative risk and incidence of immune checkpoint inhibitors related pneumonitis in patients with advanced cancer: a meta-analysis. Front Pharmacol 2018; 9: 1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hu Y-B, Zhang Q, Li H-J, et al. Evaluation of rare but severe immune related adverse effects in PD-1 and PD-L1 inhibitors in non-small cell lung cancer: a meta-analysis. Transl Lung Cancer Res 2017; 6: Suppl 1, S8–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Su Q, Zhu EC, Wu J-B, et al. Risk of pneumonitis and pneumonia associated with immune checkpoint inhibitors for solid tumors: a systematic review and meta-analysis. Front Immunol 2019; 10: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Barjaktarevic IZ, Qadir N, Suri A, et al. Organizing pneumonia as a side effect of ipilimumab treatment of melanoma. Chest 2013; 143: 858–861. [DOI] [PubMed] [Google Scholar]
- 62.Mailleux M, Cornélis F, Colin GC, et al. Unusual pulmonary toxicity of ipilimumab treated by macrolides. Acta Clin Belg 2015; 70: 442–444. [DOI] [PubMed] [Google Scholar]
- 63.Raad RA, Kannan R, Madden K, et al. Ipilimumab-induced organizing pneumonia on 18F-FDG PET/CT in a patient with malignant melanoma. Clin Nucl Med 2017; 42: e345–e346. [DOI] [PubMed] [Google Scholar]
- 64.Nomura H, Takahashi H, Suzuki S, et al. Unexpected recalcitrant course of drug-induced erythema multiforme-like eruption and interstitial pneumonia sequentially occurring after nivolumab therapy. J Dermatol 2017; 44: 818–821. [DOI] [PubMed] [Google Scholar]
- 65.Powell CA. Pulmonary infiltrates in a patient with advanced melanoma. J Clin Oncol 2017; 35: 705–708. [DOI] [PubMed] [Google Scholar]
- 66.Sano T, Uhara H, Mikoshiba Y, et al. Nivolumab-induced organizing pneumonia in a melanoma patient. Jpn J Clin Oncol 2016; 46: 270–272. [DOI] [PubMed] [Google Scholar]
- 67.Ishiwata T, Ebata T, Iwasawa S, et al. Nivolumab-induced acute fibrinous and organizing pneumonia (AFOP). Intern Med 2017; 56: 2311–2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Koyama N, Iwase O, Nakashima E, et al. High incidence and early onset of nivolumab-induced pneumonitis: four case reports and literature review. BMC Pulm Med 2018; 18: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mahjoubi L, Gazzah A, Marabelle A, et al. Late-occurring nivolumab-induced cryptogenic organising pneumonia mimicking lung progression in a patient with metastatic non-small cell lung cancer. Eur J Cancer 2017; 85: 155–157. [DOI] [PubMed] [Google Scholar]
- 70.Teixidor E, Sais E, Vásquez CA, et al. Immune-related adverse events and atypical radiological response with checkpoint inhibitor immunotherapy in an elderly patient with high PD-L1 expressing lung adenocarcinoma. Oncotarget 2018; 9: 33043–33049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gounant V, Brosseau S, Naltet C, et al. Nivolumab-induced organizing pneumonitis in a patient with lung sarcomatoid carcinoma. Lung Cancer 2016; 99: 162–165. [DOI] [PubMed] [Google Scholar]
- 72.Nishino M, Chambers ES, Chong CR, et al. Anti-PD-1 inhibitor-related pneumonitis in non-small cell lung cancer. Cancer Immunol Res 2016; 4: 289–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nishino M, Ramaiya NH, Hatabu H, et al. PD-1 inhibitor-related pneumonitis in lymphoma patients treated with single-agent pembrolizumab therapy. Br J Haematol 2018; 180: 752–755. [DOI] [PubMed] [Google Scholar]
- 74.Akella P, Loganathan S, Jindal V, et al. Anti PD-1 immunotherapy related interstitial lung disease presenting as respiratory failure – a review with case series. Respir Med Case Rep 2018; 26: 17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Abdel-Wahab N, Shah M, Suarez-Almazor ME. Adverse events associated with immune checkpoint blockade in patients with cancer: a systematic review of case reports. PLoS One 2016; 11: e0160221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Naidoo J, Wang X, Woo KM, et al. Pneumonitis in patients treated with anti-programmed death-1/programmed death ligand 1 therapy. J Clin Oncol 2017; 35: 709–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Suresh K, Voong KR, Shankar B, et al. Pneumonitis in non-small cell lung cancer patients receiving immune checkpoint immunotherapy: incidence and risk factors. J Thorac Oncol 2018; 13: 1930–1939. [DOI] [PubMed] [Google Scholar]
- 78.Kato T, Masuda N, Nakanishi Y, et al. Nivolumab-induced interstitial lung disease analysis of two phase II studies patients with recurrent or advanced non-small-cell lung cancer. Lung Cancer 2017; 104: 111–118. [DOI] [PubMed] [Google Scholar]
- 79.Cho JY, Kim J, Lee JS, et al. Characteristics, incidence, and risk factors of immune checkpoint inhibitor-related pneumonitis in patients with non-small cell lung cancer. Lung Cancer 2018; 125: 150–156. [DOI] [PubMed] [Google Scholar]
- 80.Delaunay M, Cadranel J, Lusque A, et al. Immune-checkpoint inhibitors associated with interstitial lung disease in cancer patients. Eur Respir J 2017; 50: 1700050. [DOI] [PubMed] [Google Scholar]
- 81.Yanagihara T, Tanaka K, Ota K, et al. Tumor-infiltrating lymphocyte-mediated pleuritis followed by marked shrinkage of metastatic kidney cancer of the chest wall during nivolumab treatment. Ann Oncol 2017; 28: 2038–2039. [DOI] [PubMed] [Google Scholar]
- 82.Ide M, Tanaka K, Sunami S, et al. Durable response to nivolumab in a lung adenocarcinoma patient with idiopathic pulmonary fibrosis. Thorac Cancer 2018; 9: 1519–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 2013; 188: 733–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Franzen D, Schad K, Kowalski B, et al. Ipilimumab and early signs of pulmonary toxicity in patients with metastastic melanoma: a prospective observational study. Cancer Immunol Immunother 2018; 67: 127–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Le T, Minna JD, Gerber DE. Checkpoint inhibitor pneumonitis: too clinically serious for benefit? J Thorac Oncol 2019; 14: 332–335. [DOI] [PubMed] [Google Scholar]
- 86.Twyman-Saint Victor C, Rech AJ, Maity A, et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature 2015; 520: 373–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bang A, Wilhite TJ, Pike LRG, et al. Multicenter evaluation of the tolerability of combined treatment with PD-1 and CTLA-4 immune checkpoint inhibitors and palliative radiation therapy. Int J Radiat Oncol Biol Phys 2017; 98: 344–351. [DOI] [PubMed] [Google Scholar]
- 88.Pike LRG, Bang A, Ott P, et al. Radiation and PD-1 inhibition: favorable outcomes after brain-directed radiation. Radiother Oncol 2017; 124: 98–103. [DOI] [PubMed] [Google Scholar]
- 89.Aboudaram A, Modesto A, Chaltiel L, et al. Concurrent radiotherapy for patients with metastatic melanoma and receiving anti-programmed-death 1 therapy: a safe and effective combination. Melanoma Res 2017; 27: 485–491. [DOI] [PubMed] [Google Scholar]
- 90.Liniker E, Menzies AM, Kong BY, et al. Activity and safety of radiotherapy with anti-PD-1 drug therapy in patients with metastatic melanoma. Oncoimmunology 2016; 5: e1214788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ahmed KA, Abuodeh YA, Echevarria MI, et al. Clinical outcomes of melanoma brain metastases treated with stereotactic radiosurgery and anti-PD-1 therapy, anti-CTLA-4 therapy, BRAF/MEK inhibitors, BRAF inhibitor, or conventional chemotherapy. Ann Oncol 2016; 27: 2288–2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tallet AV, Dhermain F, Le Rhun E, et al. Combined irradiation and targeted therapy or immune checkpoint blockade in brain metastases: toxicities and efficacy. Ann Oncol 2017; 28: 2962–2976. [DOI] [PubMed] [Google Scholar]
- 93.Barker CA, Postow MA, Khan SA, et al. Concurrent radiotherapy and ipilimumab immunotherapy for patients with melanoma. Cancer Immunol Res 2013; 1: 92–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Doyen J, Picard A, Naghavi AO, et al. Clinical outcomes of metastatic melanoma treated with checkpoint inhibitors and multisite radiotherapy. JAMA Dermatol 2017; 153: 1056–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fiorica F, Belluomini L, Stefanelli A, et al. Immune checkpoint inhibitor nivolumab and radiotherapy in pretreated lung cancer patients: efficacy and safety of combination. Am J Clin Oncol 2018. In press doi: 10.1097/COC.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 96.Lesueur P, Escande A, Thariat J, et al. Safety of combined PD-1 pathway inhibition and radiation therapy for non-small-cell lung cancer: a multicentric retrospective study from the GFPC. Cancer Med 2018; 7: 5505–5513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hubbeling HG, Schapira EF, Horick NK, et al. Safety of combined PD-1 pathway inhibition and intracranial radiation therapy in non-small cell lung cancer. J Thorac Oncol 2018; 13: 550–558. [DOI] [PubMed] [Google Scholar]
- 98.Shaverdian N, Lisberg AE, Bornazyan K, et al. Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: a secondary analysis of the KEYNOTE-001 phase 1 trial. Lancet Oncol 2017; 18: 895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hwang WL, Niemierko A, Hwang KL, et al. Clinical outcomes in patients with metastatic lung cancer treated with PD-1/PD-L1 inhibitors and thoracic radiotherapy. JAMA Oncol 2018; 4: 253–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tamiya A, Tamiya M, Nakahama K, et al. Correlation of radiation pneumonitis history before nivolumab with onset of interstitial lung disease and progression-free survival of patients with pre-treated advanced non-small cell lung cancer. Anticancer Res 2017; 37: 5199–5205. [DOI] [PubMed] [Google Scholar]
- 101.Shibaki R, Akamatsu H, Fujimoto M, et al. Nivolumab induced radiation recall pneumonitis after two years of radiotherapy. Ann Oncol 2017; 28: 1404–1405. [DOI] [PubMed] [Google Scholar]
- 102.Louvel G, Bahleda R, Ammari S, et al. Immunotherapy and pulmonary toxicities: can concomitant immune-checkpoint inhibitors with radiotherapy increase the risk of radiation pneumonitis? Eur Respir J 2018; 51: 1701737. [DOI] [PubMed] [Google Scholar]
- 103.Antonia SJ, Villegas A, Daniel D, et al. Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med 2018; 379: 2342–2350. [DOI] [PubMed] [Google Scholar]
- 104.Vansteenkiste J, Naidoo J, Faivre-Finn C, et al. MA05.02 PACIFIC subgroup analysis: pneumonitis in stage III, unresectable NSCLC patients treated with durvalumab vs. placebo after CRT. J Thorac Oncol 2018; 13: S370–S371. [Google Scholar]
- 105.Naccache J-M, Gibiot Q, Monnet I, et al. Lung cancer and interstitial lung disease: a literature review. J Thorac Dis 2018; 10: 3829–3844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tzouvelekis A, Spagnolo P, Bonella F, et al. Patients with IPF and lung cancer: diagnosis and management. Lancet Respir Med 2018; 6: 86–88. [DOI] [PubMed] [Google Scholar]
- 107.King CS, Nathan SD. Idiopathic pulmonary fibrosis: effects and optimal management of comorbidities. Lancet Respir Med 2017; 5: 72–84. [DOI] [PubMed] [Google Scholar]
- 108.Khunger M, Velcheti V. A case of a patient with idiopathic pulmonary fibrosis with lung squamous cell carcinoma treated with nivolumab. J Thorac Oncol 2017; 12: e96–e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Duchemann B, Didier M, Pailler M-C, et al. Le nivolumab peut-il être utilisé dans les fibroses pulmonaires idiopathiques? [Can nivolumab be used safely in idiopathic pulmonary fibrosis?]. Rev Mal Respir 2019; 36: 209–213. [DOI] [PubMed] [Google Scholar]
- 110.Fujimoto D, Morimoto T, Ito J, et al. A pilot trial of nivolumab treatment for advanced non-small cell lung cancer patients with mild idiopathic interstitial pneumonia. Lung Cancer 2017; 111: 1–5. [DOI] [PubMed] [Google Scholar]
- 111.Kanai O, Kim YH, Demura Y, et al. Efficacy and safety of nivolumab in non-small cell lung cancer with preexisting interstitial lung disease. Thorac Cancer 2018; 9: 847–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Berthod G, Lazor R, Letovanec I, et al. Pulmonary sarcoid-like granulomatosis induced by ipilimumab. J Clin Oncol 2012; 30: e156–e159. [DOI] [PubMed] [Google Scholar]
- 113.Vogel WV, Guislain A, Kvistborg P, et al. Ipilimumab-induced sarcoidosis in a patient with metastatic melanoma undergoing complete remission. J Clin Oncol 2012; 30: e7–e10. [DOI] [PubMed] [Google Scholar]
- 114.Wilgenhof S, Morlion V, Seghers AC, et al. Sarcoidosis in a patient with metastatic melanoma sequentially treated with anti-CTLA-4 monoclonal antibody and selective BRAF inhibitor. Anticancer Res 2012; 5: 1355–1359. [PubMed] [Google Scholar]
- 115.Reule RB, North JP. Cutaneous and pulmonary sarcoidosis-like reaction associated with ipilimumab. J Am Acad Dermatol 2013; 69: e272–e273. [DOI] [PubMed] [Google Scholar]
- 116.Murphy KP, Kennedy MP, Barry JE, et al. New-onset mediastinal and central nervous system sarcoidosis in a patient with metastatic melanoma undergoing CTLA4 monoclonal antibody treatment. Oncol Res Treat 2014; 37: 351–353. [DOI] [PubMed] [Google Scholar]
- 117.Eckert A, Schoeffler A, Dalle S, et al. Anti-CTLA4 monoclonal antibody induced sarcoidosis in a metastatic melanoma patient. Dermatology 2009; 218: 69–70. [DOI] [PubMed] [Google Scholar]
- 118.Tissot C, Carsin A, Freymond N, et al. Sarcoidosis complicating anti-cytotoxic T-lymphocyte-associated antigen-4 monoclonal antibody biotherapy. Eur Respir J 2013; 41: 246–247. [DOI] [PubMed] [Google Scholar]
- 119.Koelzer VH, Rothschild SI, Zihler D, et al. Systemic inflammation in a melanoma patient treated with immune checkpoint inhibitors – an autopsy study. J Immunother Cancer 2016; 4: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Reuss JE, Kunk PR, Stowman AM, et al. Sarcoidosis in the setting of combination ipilimumab and nivolumab immunotherapy: a case report & review of the literature. J Immunother Cancer 2016; 4: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Faviez G, Bousquet E, Rabeau A, et al. Granulomatose sarcoïdosique survenant sous inhibiteurs de point de contrôle immunitaire. [Sarcoud-like granulomatosis in cancer patients treated with immune checkpoint inhibitors]. Rev Mal Respir 2018; 35: 963–967. [DOI] [PubMed] [Google Scholar]
- 122.Danlos F-X, Pagès C, Baroudjian B, et al. Nivolumab-induced sarcoid-like granulomatous reaction in a patient with advanced melanoma. Chest 2016; 149: e133–e136. [DOI] [PubMed] [Google Scholar]
- 123.Montaudié H, Pradelli J, Passeron T, et al. Pulmonary sarcoid-like granulomatosis induced by nivolumab. Br J Dermatol 2017; 176: 1060–1063. [DOI] [PubMed] [Google Scholar]
- 124.Al-dliw M, Megri M, Shahoub I, et al. Pembrolizumab reactivates pulmonary granulomatosis. Respir Med Case Rep 2017; 22: 126–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Lainez S, Tissot C, Cottier M, et al. EBUS-TBNA can distinguish sarcoid-like side effect of nivolumab treatment from tumor progression in non-small cell lung cancer. Respiration 2017; 94: 518–521. [DOI] [PubMed] [Google Scholar]
- 126.Noguchi S, Kawachi H, Yoshida H, et al. Sarcoid-like granulomatosis induced by nivolumab treatment in a lung cancer patient. Case Rep Oncol 2018; 11: 562–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cousin S, Italiano A. Molecular pathways: immune checkpoint antibodies and their toxicities. Clin Cancer Res 2016; 22: 4550–4555. [DOI] [PubMed] [Google Scholar]
- 128.Mitchell MA, Hogan K, Amjadi K. Atezolizumab-induced sarcoid-like granulomatous reaction in a patient with urothelial cell carcinoma. Immunotherapy 2018; 10: 1189–1192. [DOI] [PubMed] [Google Scholar]
- 129.Bonifazi M, Bravi F, Gasparini S, et al. Sarcoidosis and cancer risk: systematic review and meta-analysis of observational studies. Chest 2015; 147: 778–791. [DOI] [PubMed] [Google Scholar]
- 130.Broos CE, van Nimwegen M, in ‘t Veen JCCM, et al. Decreased cytotoxic T-lymphocyte antigen 4 expression on regulatory T cells and Th17 cells in sarcoidosis: double trouble? Am J Respir Crit Care Med 2015; 192: 763–765. [DOI] [PubMed] [Google Scholar]
- 131.Bristol-Meyers Squibb Pharmaceutical Research Institute . Effect of MDX-1106 on CD4+ T Cells During an Allogeneic Mixed Lymphocyte Reaction (MLR) (Medarex Study No. MDX-1106-026-R). Document Control no. 930046581. 2006.
- 132.Loke WSJ, Herbert C, Thomas PS. Sarcoidosis: immunopathogenesis and immunological markers. Int J Chronic Dis 2013; 2013: 928601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Baughman RP, Teirstein AS, Judson MA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med 2001; 164: 1885–1889. [DOI] [PubMed] [Google Scholar]
- 134.Costabel U, Bonella F, Ohshimo S, et al. Diagnostic modalities in sarcoidosis: BAL, EBUS, and PET. Semin Respir Crit Care Med 2010; 31: 404–408. [DOI] [PubMed] [Google Scholar]
- 135.Picchi H, Mateus C, Chouaid C, et al. Infectious complications associated with the use of immune checkpoint inhibitors in oncology: reactivation of tuberculosis after anti PD-1 treatment. Clin Microbiol Infect 2018; 24: 216–218. [DOI] [PubMed] [Google Scholar]
- 136.Fujita K, Terashima T, Mio T. Anti-PD1 antibody treatment and the development of acute pulmonary tuberculosis. J Thorac Oncol 2016; 11: 2238–2240. [DOI] [PubMed] [Google Scholar]
- 137.Chu Y-C, Fang K-C, Chen H-C, et al. Pericardial tamponade caused by a hypersensitivity response to tuberculosis reactivation after Anti-PD-1 treatment in a patient with advanced pulmonary adenocarcinoma. J Thorac Oncol 2017; 12: e111–e114. [DOI] [PubMed] [Google Scholar]
- 138.Takata S, Koh G, Han Y, et al. Paradoxical response in a patient with non-small cell lung cancer who received nivolumab followed by anti-Mycobacterium tuberculosis agents. J Infect Chemother 2019; 25: 54–58. [DOI] [PubMed] [Google Scholar]
- 139.He W, Zhang X, Li W, et al. Activated pulmonary tuberculosis in a patient with melanoma during PD-1 inhibition: a case report. OncoTargets Ther 2018; 11: 7423–7427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Barber DL, Sakai S, Kudchadkar RR, et al. Tuberculosis following PD-1 blockade for cancer immunotherapy. Sci Transl Med 2019; 11: eaat2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Lee JJX, Chan A, Tang T. Tuberculosis reactivation in a patient receiving anti-programmed death-1 (PD-1) inhibitor for relapsed Hodgkin's lymphoma. Acta Oncol 2016; 55: 519–520. [DOI] [PubMed] [Google Scholar]
- 142.Lai RPJ, Meintjes G, Wilkinson RJ. HIV-1 tuberculosis-associated immune reconstitution inflammatory syndrome. Semin Immunopathol 2016; 38: 185–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Beigelman C, Sellami D, Brauner M. CT of parenchymal and bronchial tuberculosis. Eur Radiol 2000; 10: 699–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Del Castillo M, Romero FA, Argüello E, et al. The spectrum of serious infections among patients receiving immune checkpoint blockade for the treatment of melanoma. Clin Infect Dis 2016; 63: 1490–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Fujita K, Kim YH, Kanai O, et al. Emerging concerns of infectious diseases in lung cancer patients receiving immune checkpoint inhibitor therapy. Respir Med 2019; 146: 66–70. [DOI] [PubMed] [Google Scholar]
- 146.Kanjanapan Y, Day D, Wang L, et al. Hyperprogressive disease in early-phase immunotherapy trials: clinical predictors and association with immune-related toxicities. Cancer 2019; 125: 1341–1349. [DOI] [PubMed] [Google Scholar]
- 147.Borcoman E, Kanjanapan Y, Champiat S, et al. Novel patterns of response under immunotherapy. Ann Oncol 2019; 30: 385–396. [DOI] [PubMed] [Google Scholar]
- 148.Overman MJ, Lonardi S, Wong KYM, et al. Durable clinical benefit with nivolumab plus ipilimumab in DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal cancer. J Clin Oncol 2018; 36: 773–779. [DOI] [PubMed] [Google Scholar]
- 149.Postow MA, Chesney J, Pavlick AC, et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med 2015; 372: 2006–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]