Abstract
Background
Readmission rates following hospitalisation for COPD exacerbations are unacceptably high, and the contributing factors are poorly understood. Our objective was to summarise and evaluate the factors associated with 30- and 90-day all-cause readmission following hospitalisation for an exacerbation of COPD.
Methods
We systematically searched electronic databases from inception to 5 November 2019. Data were extracted by two independent authors in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Study quality was assessed using a modified version of the Newcastle–Ottawa Scale. We synthesised a narrative from eligible studies and conducted a meta-analysis where this was possible using a random-effects model.
Results
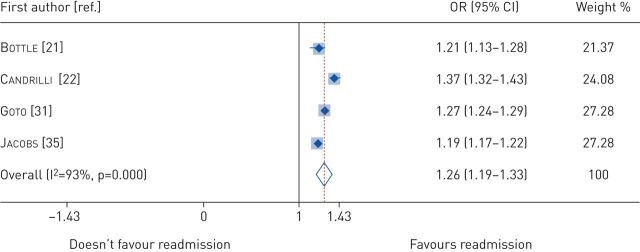
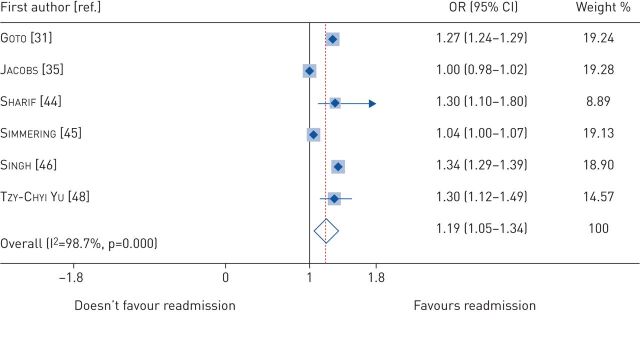
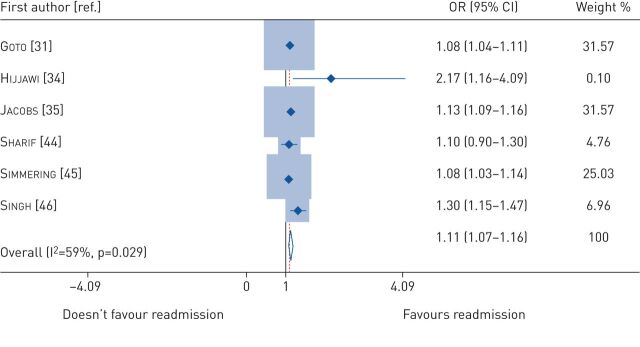
In total, 3533 abstracts were screened and 208 full-text manuscripts were reviewed. A total of 32 papers met the inclusion criteria, and 14 studies were included in the meta-analysis. The readmission rate ranged from 8.8–26.0% at 30 days and from 17.5–39.0% at 90 days. Our narrative synthesis showed that comorbidities, previous exacerbations and hospitalisations, and increased length of initial hospital stay were the major risk factors for readmission at 30 and 90 days. Pooled adjusted odds ratios (95% confidence intervals) revealed that heart failure (1.29 (1.22–1.37)), renal failure (1.26 (1.19–1.33)), depression (1.19 (1.05–1.34)) and alcohol use (1.11 (1.07–1.16)) were all associated with an increased risk of 30-day all-cause readmission, whereas being female was a protective factor (0.91 (0.88–0.94)).
Conclusions
Comorbidities, previous exacerbations and hospitalisation, and increased length of stay were significant risk factors for 30- and 90-day all-cause readmission after an index hospitalisation with an exacerbation of COPD.
Short abstract
Clinicians need to take a holistic approach including attention to comorbidities in the pre-discharge care of patients with COPD exacerbations to reduce the potential risk of readmission. http://bit.ly/2sucXKV
Introduction
Exacerbations of COPD are a major cause of hospitalisation and mortality [1, 2]. According to the Global Burden of Disease study [1], there were 251 million cases of COPD worldwide in 2016. An estimated 3.17 million deaths were caused by COPD in 2015, accounting for 5% of all global deaths, and projections suggest that COPD will soon be the third leading cause of death worldwide [1]. COPD is punctuated by periodic deteriorations in respiratory symptoms called exacerbations; exacerbations cause most of the hospitalisations, with significant effects on morbidity and mortality [3].
For patients surviving hospitalisation with a COPD exacerbation, readmission to hospital is a major problem. Identifying and mitigating risk factors for readmission is therefore important [4, 5]. In the USA, around 19% of COPD patients are readmitted within 30 days, while in the UK the all-cause readmission rates are 24% within 30 days and 43% within 90 days of discharge [5, 6]. Data from the European COPD Audit show that the risk of in-hospital mortality was substantially higher in readmitted patients compared to non-readmitted patients (13.4% versus 2.3%) [7]. Differences in readmission rates have been associated with unexplained variations in care quality [8]. In the USA, the Centers for Medicare and Medicaid Services have applied financial penalties to hospitals that have high readmission rates and have considered readmissions a marker of the quality of care [9, 10]. Similar penalties have been applied in the British NHS in an attempt to reduce readmission rates and improve quality of care [11]. Globally, preventing readmissions among patients with COPD following acute exacerbations has been recognised as a high-priority management strategy [12]. Recently, the official American Thoracic Society workshop report on reducing COPD readmission emphasised the need for improvements in identifying risk factors for COPD readmissions [13].
Reflecting the importance of readmissions to patients, clinicians and payers, there has been considerable research assessing the risk factors that lead to readmissions. However, whilst there was a 2007 systematic review examining risk factors for COPD-related readmissions [14], there is no existing review investigating risk factors for all-cause COPD readmission. Therefore, the purpose of this systematic review was to evaluate and summarise the risk factors for all-cause hospital readmissions in patients admitted for COPD exacerbations, and to identify areas of research to mitigate such risk.
Methods
Protocol and registration
This systematic review was conducted in accordance with the Preferred Reporting in Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15] and the review was prospectively registered on PROSPERO (identifier CRD42019119364).
Search strategy
We searched MEDLINE, Embase, CINAHL and Scopus from inception to 5 November 2019. We used an extensive search strategy developed for retrieving this type of evidence, which included the reference list of eligible papers (tables S1 and S2).
Inclusion criteria
The PICO framework was used in our search strategy: P: population (COPD patients admitted due to COPD exacerbation); I: intervention (not applicable); C: comparison (patients get readmitted versus not readmitted); O: outcome (readmission within 30 and 90 days). We included studies that investigated: 1) readmission/rehospitalisation after an initial admission with COPD exacerbation; 2) all-cause readmission defined as any emergency (non-elective) readmission to hospital; and 3) studies that investigated all-cause readmissions and analysed the contribution of risk factors and/or predictors associated with readmission/rehospitalisation.
Exclusion criteria
We excluded the following: 1) studies that examined readmission risk >1 year after discharge from index admission; 2) intervention studies that did not include examination of risk factors for all-cause hospital readmission for patients with COPD in the control group; 3) studies that included factors/predictors/causes for readmission but did not specifically analyse all-cause COPD readmission-related factors; 4) conference abstracts, editorial reports, correspondence, reviews, qualitative studies and theses; 5) non-English manuscripts; and 6) non-full-text articles.
Data collection
Two authors (J.S. Alqahtani and J.R. Hurst) independently screened titles and abstracts of potential studies and conflicts were resolved through a discussion with a third author (S. Mandal). Full-text articles of potential studies were then independently read by two authors (J.S. Alqahtani and C.M. Njoku) to identify studies meeting the inclusion criteria. The reference lists from all identified studies and reviews were scrutinised for eligible articles. Disagreement on selected papers was resolved through discussion with a third author (J.R. Hurst).
Quality assessment
Two authors independently evaluated the methodological quality of included studies using a modified version of the Newcastle–Ottawa Scale [16]. This scale utilises a “star” system with a maximum score of nine stars for each study. Study ratings are categorised as good (7–9 stars), fair (4–6 stars) or poor (1–3 stars). Any disagreement in the quality assessment was resolved by discussion with a third author (supplementary material).
Data synthesis
We were not able to perform a meta-analysis on all results because of the heterogeneity of included studies and inconsistencies in reporting risk factors across studies. However, we did conduct a meta-analysis using summary data from 14 studies to synthesise adjusted odds ratios for risk factors where results were reported consistently (for example, similar age ranges) and where a variable was reported in at least four studies in total. To account for study heterogeneity, we used the random-effects model in Stata 14.0 (StataCorp LLC, College Station, TX, USA). Data are displayed using forest plots. We examined between-study heterogeneity using the I2 statistic. A narrative synthesis of the results was conducted, guided by study quality.
Results
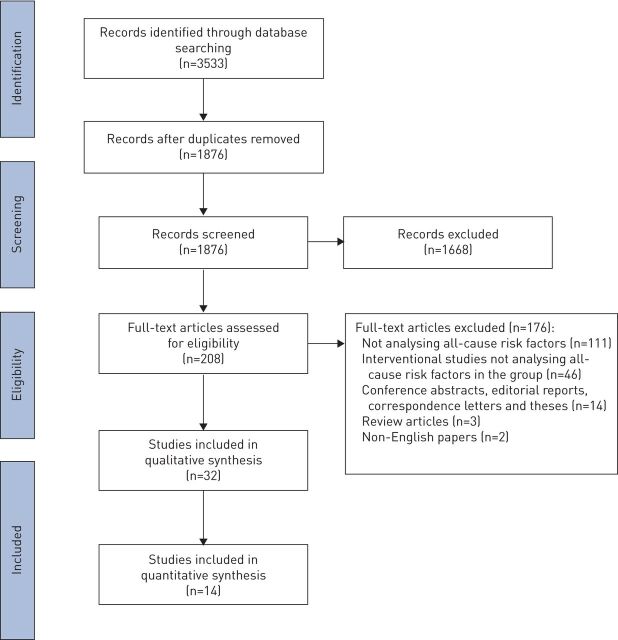
An initial search generated 3533 potentially relevant papers, of which 1657 were immediately excluded due to duplication. After the first screening of title and abstract, 208 papers were potentially relevant according to the inclusion criteria. An additional 176 papers were excluded after full-text review, which resulted in 32 studies that satisfied all criteria. The reference list of the relevant papers was also examined and did not result in any new papers (figure 1).
FIGURE 1.
Flow diagram of studies included in the review based on the Preferred Reporting Items for Systematic Review and Meta-Analysis Guidelines.
Description of included studies
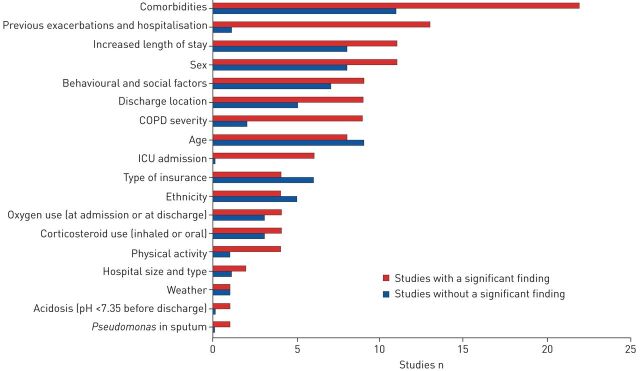
A summary of the included studies is presented in table 1, Out of 32 studies, 27 were conducted retrospectively and five were conducted prospectively; 21 studies were conducted in the USA, three in the UK, two in Canada and one each in Spain, Korea, Hong Kong, Israel, Australia and Europe. All papers were published between 2013 and 2019, and included a total of 3 982 881 patients. Among the 32 studies, three were rated as “fair” in the quality assessment. The remaining papers were ranked as “good” quality. A detailed description of the studies is presented in table S3. The all-cause readmission rates ranged from 8.8% to 26.0% at 30 days, 17.5% to 39.0% at 90 days, and from 8.8% to 65.2% at 1 year. Studies described several risk factors for all-cause COPD readmission at different time-points, the results of which are summarised in figure 2 and table S4. The details of all risk factors and the quality assessment of each study are presented in tables S3 and S5.
TABLE 1.
Characteristics of the included studies, with quality assessment
| First author [ref.] | Study design | Sample size | Age years | GOLD severity | Readmission time | Causes and rates of readmission, in order of prevalence | Study quality |
| Almagro [17] | P | Total: n=983 M: n=899 (92%) F: n=84 (8%) |
72.25±9.7 | GOLD 3 | 90 day and 1 year |
|
Good |
| Baker [18] | R | Total: n=6095 M: n=2499 (40.8%) F: n=3596 (59.2%) |
40–65 | Not reported | 1, 3 and 12 months |
|
Good |
| Bashir [19] | R | Total: n=461 M: n=311 (67.5%) F: n=150 (32.5%) |
71.7±13.3 | Not reported | 30 days | Overall rate: 16.5% | Good |
| Bollu [20] | R | Total: n=2463 M: n=1054 (43%) F: n=1409 (57%) |
72.5±12 | Not reported | 30 days | Overall rate: 20.6%
|
Good |
| Bottle [21] | R | Total: n=96 053 M: n=46 388 (48.3%) F: n=49 665 (51.7%) |
36-≥85 | Not reported | 30 days | Overall rate: 16.5%
|
Good |
| Candrilli [22] | R | Total: n=264 526 M: n=129 769 (49%) F: n=134 757 (51%) |
30 days=67.69±11.26 90 days=67.42±11.23 |
Not reported | 30 days and 90 days |
|
Good |
| Chan [23] | R | Total: n=65 497 M: n=50 456 (77%) F: n=15 041 (23%) |
76.81±9.6 | Not reported | 30 days |
|
Good |
| Chawla [24] | P | Total: n=54 M: n=30 (55%) F: n=24 (45%) |
70±12 | GOLD 3 | 30 days |
|
Fair |
| Choi [25] | R | Total: n=704 M: n=492 (70%) F: n=212 (30%) |
72.4±9.5 | GOLD 2–3 | 30 days |
|
Good |
| Couillard [26] | R | Total: n=167 M: n=86 (51.5%) F: n=81 (48.5%) |
71.4±10.3 | GOLD 2 | 1 year |
|
Good |
| Echevarria [27] | P | Total: n=2417 M: n=1119 (46%) F: n=1298 (54%) |
72.5±10.1 | GOLD 3 | 90 day |
|
Good |
| Epstein [28] | R | Total: n=539 M: n=325 (60%) F: n=214 (40%) |
69.19±11.75 | Not reported | 60 day |
|
Good |
| Ehsani [29] | P | Total: n=42 M: n=28 (66.7%) F: n=14 (33.3%) |
70±8.6 | Not reported | 30 day |
|
Fair |
| Genao [30] | R | Total: n=52 741 M: n=23 397 (44%) F: n=29 344 (56%) |
71.4±10.3 | Not reported | 30 day, 1 year and 3 years |
|
Good |
| Goto [31] | R | Total: n=845 465 M: n=350 967 (41%) F: n=494 498 (59%) |
69±0.01 | Not reported | 30 days |
|
Good |
| Gershon [32] | R | Total: n=126 013 M: not presented F: not presented |
35–85+ | Not reported | 30 days |
|
Good |
| Hakim [33] | R | Total: n=2662 M: n=1418 (53%) F: n=1244(47%) |
72.5±12 | Not reported | 30 days and 1 year |
|
Fair |
| Hijjawi [34] | P | Total: n=160 M: n=76 (47.5%) F: n=84 (52.5%) |
65.77±12.47 | GOLD 1–4 | 30 days |
|
Good |
| Jacobs [35] | R | Total: n=1 055 830 M: n=437 812 (41%) F: n=618 018 (59%) |
68 (58–77) | Not reported | 3, 7 and 30 days |
|
Good |
| Kon [36] | P | Total: n=213 M: n=111 (52%) F: n=102 (48%) |
72.1±10.8 | GOLD 3 | 90 days |
|
Good |
| Loh [37] | R | Total: n=123 M: n=65 (52.8%) F: n=58 (47.2%) |
64.9±11.3 | GOLD 3 | 30 and 90 days |
|
Good |
| Nguyen [38] | R | Total: n=4596 M: n=2040 (44%) F: n=2556 (56%) |
72.3±11 | GOLD 2 | 30 days |
|
Good |
| Nguyen [39] | R | Total: n=2910 M: n=1248 (43%) F: n=1662 (57%) |
72±11 | GOLD 2 | 30 days |
|
Good |
| Rinne [40] | R | Total: n=20 472 M: not presented F: not presented |
73 | Not reported | 30 days |
|
Good |
| Rinne [41] | R | Total: n=33 558 M: n=32 417 (96.6%) F: n=1141 (3.4%) |
68.7 | Not reported | 30 days |
|
Good |
| Roberts [42] | R | Total: n=306 M: n=135 (44%) F: n=171 (56%) |
71 | Not reported | 30 and 90 days |
|
Good |
| Shah [43] | R | Total: n=947 084 M: n=392 187 (41.41%) F: n=554 897 (58.59%) |
73.55±10.87 | Not reported | 30 days |
|
Good |
| Sharif [44] | R | Total: n=8263 M: n=3401 (41%) F: n=4862 (59%) |
56.55±5.73 | Not reported | 30 days |
|
Good |
| Simmering [45] | R | Total: n=286 313 M: n=13 0497 (45.5%) F: n=155 816 (54.5%) |
40–90+ | Not reported | 30 days |
|
Good |
| Singh [46] | R | Total: n=135 498 M: n=53 940 (38.80%) F: n=81 558 (62%) |
66–74, 75–84, ≥85 |
Not reported | 30 days |
|
Good |
| Spece [47] | R | Total: n=2391 M: n=2319 (97%) F: n=72 (3%) |
68.0±10.4 | Not reported | 30 days |
|
Good |
| Tzy-Chyi Yu [48] | R | Total: n=18 282 M: n=6869 (37.6%) F: n=11 413 (62.4%) |
56.6±5.8 | Not reported | 30 days |
|
Good |
Data are presented as mean±sd or range, unless otherwise stated. GOLD: The Global Initiative for Chronic Obstructive Lung Disease; P: prospective; R: retrospective; M: male; F: female; SABA: short-acting beta agonist; AECOPD: acute exacerbations of COPD; MI: myocardial infarction; PIF: peak inspiratory flow.
FIGURE 2.
Summary of risk/predictive factors associated with 30- and 90-day all-cause hospital readmission following a hospitalised exacerbation of COPD by order of total number of studies in which there was a significant finding. ICU: intensive care unit.
Meta-analysis results
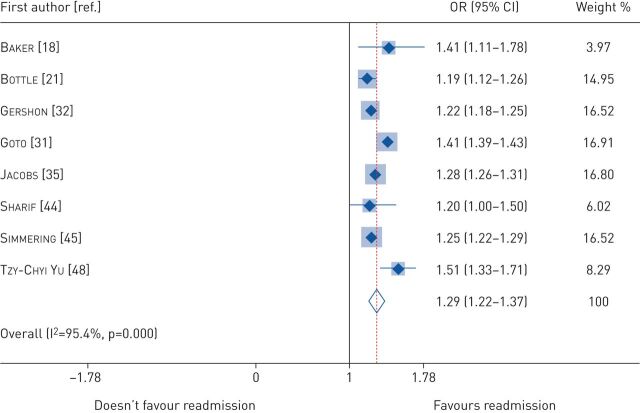
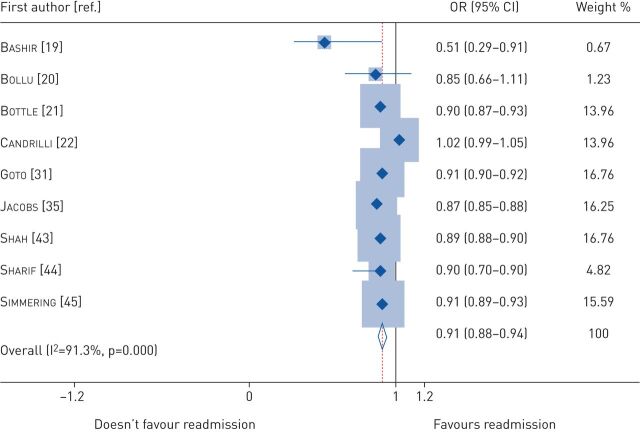
We conducted a meta-analysis on 14 studies examining five risk/protective factors associated with all-cause 30-day readmission, including a total of 3 792 506 patients, which represents ∼95% of the total sample size of the included papers. These studies were included because the reported risk factors in such studies were consistent among them. This included 2 442 314 participants in eight studies that reported heart failure as a risk factor, 2 349 651 in six studies that reported depression as a risk factor, 2 331 529 in six studies that reported alcohol use as a risk factor, 2 261 874 in four studies that reported renal failure as a risk factor and 3 506 458 in nine studies that found that female sex was a protective factor. There was heterogeneity between studies with significant I2 values that ranged from 59.8% to 96.7%; therefore, we calculated the pooled adjusted odds ratio values using a random-effect model. There was no adjustment for forced expiratory volume in 1 s in the selected odds ratios because there were no confirmatory spirometry values available to clinicians at the time of management. The pooled adjusted odds ratios for heart failure, renal failure, depression, alcohol use and female sex are presented using forest plots (figures 3–7). Heart failure was associated with the highest odds of readmission followed by renal failure, then depression.
FIGURE 3.
Pooled adjusted odds ratios (ORs) for heart failure. This is a forest plot examining eight studies and risk of 30-day readmission using random effects analysis.
FIGURE 7.
Pooled adjusted odds ratio (ORs) for female sex. This is a forest plot examining nine studies and risk of 30-day readmission using random effects analysis.
FIGURE 4.
Pooled adjusted odds ratio (ORs) for renal failure. This is a forest plot examining four studies and risk of 30-day readmission using random effects analysis.
FIGURE 5.
Pooled adjusted odds ratio (ORs) for depression. This is a forest plot examining six studies and risk of 30-day readmission using random effects analysis.
FIGURE 6.
Pooled adjusted odds ratio (ORs) for alcohol use. This is a forest plot examining six studies and risk of 30-day readmission using random effects analysis.
In general, the significant risk factors for 30- and 90-day all-cause readmission were comorbidities, previous exacerbations and hospitalisations, and increased length of initial hospital stay. A narrative synthesis of the 30-day studies appears below, with further detail on the 90-day studies included in the supplementary material.
Narrative synthesis: risk factors for all-cause readmission at 30 days
Comorbidities
Overall, 17 out of 32 studies reported various comorbidities as significant risk factors for 30-day readmission, with heart failure, depression and renal failure included in our meta-analysis. Many other comorbidities were also reported (tables S2 and S3). Four studies [22, 38, 43, 47] used the comorbidity index to assess comorbidities. Spece et al. [47] found that each one-point increase in comorbidity index was associated with a 24% increased risk of readmission or death: OR 1.24 (95% CI 1.18–1.30).
Previous COPD exacerbations and hospitalisations
Previous exacerbations and hospitalisations were risk factors for 30-day readmission in nine studies. An emergency room visit in the previous 6 months (1 versus 0) was associated with increased readmission risk with OR 1.90 (95% CI 1.01–3.58) in the study by Bashir et al. [19] and OR 1.25 (95% CI 1.21–1.29) in the study by Hakim et al. [33]. The risk of readmission increased with a greater number of previous emergency room visits (≥4 versus 0) with OR 4.37 (95% CI 1.83–10.46) and OR 2.31 (95% CI 2.23–2.39) [19, 32]. Previous COPD and non-COPD hospitalisations in the previous year also significantly increased the risk for 30-day readmission by 53% to 56% and 60% to 64%, respectively [38, 39]. Consistent with other studies, Goto et al. [31] found that frequent exacerbators (defined as two hospitalisations in the past year) had a 2.5-fold increase in odds of readmission compared to non-frequent exacerbators. Disease severity of COPD was also a risk factor for readmission and has been evaluated using different tools. These included the LACE Index [19], the 3 M™ All Patient Refined™ Diagnosis-Related Groups (APR-DRG) classification tool [20, 42] and a COPD complexity tool [22]. Using long-term systemic corticosteroids was a risk factor for readmission, with 49% increased risk in one study [38]. However, receiving oral corticosteroids at discharge decreased the odds of readmission by 72% and 30% [42, 44]. The differences between use of corticosteroids in the immediate post-discharge period and longer term requires further study. The severity of an exacerbation is the composite of the severity of the insult and the severity of the underlying COPD. Intensive care unit admission was also associated with increased risk of re-admission in six studies. These patients are also likely to have longer lengths of stay.
Patient demographics
Different age groups were found to be at different risk of readmission in six studies, but results were inconsistent. Older patients with COPD typically had a greater likelihood of being readmitted (table S3). Ethnicity was investigated in nine studies with results that were also inconsistent (table S3).
Behavioural risk factors
Physical activity was examined in four studies, and low activity was reported to be a significant risk factor for 30-day readmission in three studies. For example, Nguyen et al. [39] reported that those with low-level functioning within 24 h of discharge (levels I–III (bed bound, able to sit or can stand) versus level V (walks >50 feet)) were more likely to be readmitted with a relative risk of 2.14 and that patients who engaged in moderate to strenuous exercise with 1–149 min·week−1 or ≥150 min·week−1 post-discharge were 33–34% less at risk for readmission compared to inactive patients [38]. Alcohol use was the most frequently reported social risk factor in six papers [31, 34, 35, 44–46] and has been included in our meta-analysis. Singh et al. [46] and Gershon et al. [32] identified low socioeconomic status as a significant risk factor with a 22% and 6% increased risk of readmission, respectively.
Health system-related risk factors
Length of stay (LOS) was reported to be a significant risk factor for 30-day readmission; whilst in general a longer LOS was associated with increased risk of readmission, some studies found patients with the shortest LOS were at higher risk than those who stayed slightly longer. For example, compared to 1–3 days, Candrilli et al. [22] found patients who stayed for >10 days or for 8–10 days had increased odds of readmission by 64% and 25%, respectively, but there was 18% reduced odds of readmission for those who stayed for 4–7 days. In the study by Jacobs et al. [35], those hospitalised for >5 days versus ≤2 days had an OR of 1.32 (95% CI 1.29–1.34). Furthermore, in two studies [38, 39], LOS ≥14 days versus 1–2 days increased the relative risk of readmission 2.93-fold and 2.85-fold, respectively. Gershon et al. [32] found an OR of 1.18 when LOS was ≥14 days compared to 4–6 days but found that this risk decreased to 66% and 37% when the LOS was 7–13 and 4–6 days, respectively [38]. Rinne et al. [41] found that those with LOS of 3–4 days and >4 days had higher odds of readmission at 39% and twofold, respectively, compared to <3 days. Simmering et al. [45] found an OR of 1.16 with patients who stayed for >1 day and Singh et al. [46] found that the odds increased to 1.47 when LOS was >7 days. When >7 days was compared to 3–4 days in the study by Sharif et al. [44], the readmission OR reduced to 1.20, but the odds increased to 1.30 when 1–2 days was compared to 3–4 days.
Discharge destination was found to be a significant risk factor for readmission in nine studies but is probably complex because of confounding with disease severity and comorbidity. Compared to discharge to home with no home care, discharge to a skilled nursing facility increased readmission in three studies [19, 35, 43] by three-fold, 42% and 28%, respectively. Only one study [46] reported this as a protective factor with an OR of 0.84. Additionally, when discharged to home with care, the odds of readmission increased by 30%, 36%, 32% and 16% in four studies [32, 35, 43, 45], respectively, whereas other studies [38, 39, 46] found this to decrease the risk by 75%, 74% and 80%, respectively.
Patients' insurance was reported as a risk/protective factor in five studies: four in the USA and one in Europe [19, 31, 35, 38, 40] (tables S2 and S3). Smaller hospital size (<100 beds) and fewer doctors were reported as significant readmission risk factors with 2.27-fold and 67% increased odds of readmission, respectively [21]. Staying in medium-sized hospitals compared to large hospitals decreased the odds of readmission by 5% [35]. Those who had outpatient visits were 44% less likely to be readmitted [46].
Discussion
This study is the first to systematically examine and summarise risk factors for all-cause hospital readmission following an initial admission for exacerbation of COPD. Other reviews [14] have only considered readmissions directly due to COPD, at variance with a patient-centred and holistic approach to healthcare and clinical outcomes. Our main findings indicate that comorbidities, previous exacerbations and hospitalisations, and increased LOS were the major risk factors for both 30- and 90-day readmission.
Our meta-analysis revealed that heart failure, renal failure, depression, and alcohol use were all associated with an increased risk of 30-day all-cause COPD readmission, whereas being female was a protective factor.
Many comorbidities were significant risk factors for 30- and 90-day readmission, including mental health disorders. A possible explanation for this might be a lack of adequate interventions that extend beyond COPD-specific treatment during the initial hospitalisation. There is an ongoing debate as to whether underlying comorbidities are the main reason for higher readmission rates [13]; our results highlight that this is indeed a key risk.
Three comorbidities (heart failure, renal failure and depression) and alcohol use were found to be frequently reported risks. This differs from the findings presented in a systematic review concerning readmission due only to COPD, in which no single comorbidity was reported to be associated with readmission risk [14]. Focusing effort in addressing multi-morbidity and social determinants of health may be one method to reduce the burden of readmissions following a hospitalised exacerbation of COPD [13].
Consistently with the literature, our results show that previous exacerbations and hospitalisations are significantly associated with all-cause readmission [14]. Exacerbations have been found to negatively affect health status, increase costs and ultimately increase the risk of death [49, 50]. Indeed, frequent exacerbations have been reported as a distinct susceptibility phenotype, which may support the targeting of such patients with effective preventive strategies [51]. There are many cost-effective interventions such as inhalers and pulmonary rehabilitation that could reduce exacerbations and related hospitalisations. However, such interventions are not always effective due to inadequate inhaler technique or poor adherence [52]. A recent meta-analysis found that the frequency of COPD exacerbations has decreased over the past two decades, independently of major prognostic factors [53]. This probably indicates that healthcare improvements over time have resulted in lower rates of exacerbation in the placebo groups of clinical trials. Adopting appropriate care and preventive approaches could also have a favourable effect on COPD readmissions.
Increased LOS was found to be a significant risk factor for readmission within 30 days in nine studies, and within 90 days in two studies. This may be because of increased severity of disease or, again, the presence of comorbidities. LOS was not found to be a significant risk factor for COPD-related readmission in a previous systematic review that included 17 studies [14]. LOS could be used to recognise patients with higher readmission risk and who may benefit from supported discharge, early COPD community support and/or earlier follow-up following initial discharge. We could not perform a meta-analysis on the LOS because the reporting comparisons across the studies were inconsistent.
Different tools have been used to assess COPD severity, such as the LACE index, APR-DRG and COPD complexity tool [19, 20, 22]. As expected, patients with increased disease severity had higher odds of 30-day readmission, independently of the method of measuring disease severity. There are other scores that have been developed to assess readmission risk in COPD, such as CODEX and PEARL [17, 27]. However, there is no 30-day specific risk prediction tool to identify patients at high risk of all-cause COPD readmission. Thus, to date, there is one tool for 90-day COPD readmissions, the PEARL score (previous admissions, dyspnoea (eMRCD score), age, right-sided and left-sided heart failure) and notably this does not include comorbidities other than heart failure [27]. According to a recent systematic review on models that predict exacerbations, no existing models meet the requirements for risk-stratified treatment for personalised COPD care [54]. In order to move personalised COPD medicine forward, a more harmonised approach to developing and validating high-quality prediction models is needed.
We identified several patient, behavioural and social risk factors associated with an increased risk of 30-day readmission. Former smokers compared to those who had never smoked or were passive smokers, those with low socioeconomic status and unmarried patients were identified as at significant risk for 30-day readmission [31, 38, 46]. Underweight patients and weight loss were also found to increase the risk of readmission in two studies [31, 45]; being obese was reported to be a significant protective factor in two studies [31, 35]. Six studies discussed alcohol use [31, 34, 35, 44–46], five of which found it as a significant risk factor for all-cause COPD readmission. This was not found to be an independent marker for COPD-related readmission [14]. Our results support previous finding that identified alcohol use as a significant predictor of COPD mortality [55].
Chronic use of systemic corticosteroids was a risk factor for both 30- and 90-day readmission [18, 38]. This has been reported by Bahadori and FitzGerald [14] considering COPD-specific readmission. This might be explained by side-effects such as muscle weaknesses, or use of these drugs in people with more severe COPD. Low physical activity was found to be an important risk factor for 30-day readmission in three studies [24, 38, 39], with those who were more active being less likely to be readmitted. Indeed, physical inactivity has been associated with all-cause mortality and hospitalisation [56]. Although there is a difference between physical activity and pulmonary rehabilitation, existing research on early pulmonary rehabilitation post-exacerbation did not show a reduction in readmission risk [57]. Further research considering interventions to improve or maintain physical activity in the immediate post-discharge period following COPD exacerbation is needed to test whether this can improve outcomes and reduce the risk of readmission.
Discharge destination was associated with 30-day readmission in nine studies. When patients were discharged to a skilled nursing facility or home with care, the odds of readmission increased in five studies [19, 32, 35, 43, 45]. It is likely that those patients were more unwell or frail with more comorbidities than those discharged home and thus more likely to be readmitted. However, the quality of care could affect readmission as demonstrated in other studies [38, 39, 46]. In addition, we found that those with US Medicaid and Medicare cover had higher odds of readmission within 30 days than those with private insurance or self-funding; Medicaid and Medicare have more barriers to primary care than those with other types of insurance, which may also lead to increased readmissions [58].
Our work has a number of distinguishing aspects from existing work, which had considered only COPD-related readmission [14]. To our knowledge, the present study is the first to systematically evaluate existing literature with a focus on risk factors for all-cause readmissions. We conducted a meta-analysis using a random-effects model to calculate the adjusted odds ratios on the most frequently reported risk/protective factors to account for observed heterogeneity among studies. This increased the generalisability of our findings, as heterogeneity was addressed by incorporating between-study variability of effect sizes.
This review has some limitations. First, we excluded two non-English studies. Secondly, study heterogeneity exists in location, setting, design and reported risk factors; therefore, our meta-analysis results were restricted to 14 studies in total, but these studies were representative of the target population. Thirdly, we acknowledge the heterogeneity of the diagnosis of COPD exacerbations between studies. Exacerbation of COPD is a clinical diagnosis of exclusion and all patients were being managed by their clinicians as having that diagnosis. Despite the limitations of this approach, it remains the gold standard diagnosis. As is common in studies of hospitalised COPD exacerbations, not all patients had confirmatory spirometry available to clinicians at the time of management. Finally, our meta-analysis was conducted on summary data, not individual patient data.
Our review has important clinical implications. It summarises current evidence to inform guideline developers about the importance of carefully reviewing the discharge processes and to ensure that comorbidities are fully managed along with routine COPD management. Clinicians should devote more resources to identify and manage patients with COPD at a high risk of hospital readmission and to promote physical activity and follow-up in the immediate post-discharge period. Not all the risk factors for readmission that we have identified are modifiable and therefore future research should focus on developing robust risk models to predict patients with COPD at high risk of potentially avoidable hospital readmission, with interventions tested to mitigate modifiable risk to improve outcomes for patients and health services.
Supplementary material
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary_material ERR-0166-2019_supplementary_material (345.3KB, pdf)
Acknowledgments
We thank Jennifer Ford (Evidence Services Librarian at Royal Free Hospital Medical Library, UCL Library Services, London, UK) for her assistance and support in refining the search strategy.
Footnotes
This article has an editorial commentary https://doi.org/10.1183/16000617.0097-2020
This article has supplementary material available from err.ersjournals.com
This study is registered at www.crd.york.ac.uk/prospero/ with identifier number CRD42019119364
Provenance: Submitted article, peer reviewed
Authors contributions: J.S. Alqahtani: conception, design, data acquisition, analysis, interpretation, drafting for intellectually important content and approval of final version. C.M. Njoku: data acquisition and approval of final version. B. Bereznicki: analysis, interpretation and approval of final version. B.C. Wimmer: analysis, interpretation and approval of final version. G.M. Peterson: analysis, interpretation and approval of final version. L. Kinsman: analysis, interpretation and approval of final version. Y.S. Aldabayan: data acquisition and approval of final version. A.M. Alrajeh: interpretation and approval of final version. A.M. Aldahahir: data acquisition, analysis and approval of final version. S. Mandal: design, interpretation and approval of final version. J.R. Hurst: conception, design, data acquisition, analysis, interpretation and approval of final version.
Conflict of interest: J.S. Alqahtani has nothing to disclose.
Conflict of interest: C.M. Njoku has nothing to disclose.
Conflict of interest: B. Bereznicki has nothing to disclose.
Conflict of interest: B.C. Wimmer has nothing to disclose.
Conflict of interest: G.M. Peterson has nothing to disclose.
Conflict of interest: L. Kinsman has nothing to disclose.
Conflict of interest: Y.S. Aldabayan has nothing to disclose.
Conflict of interest: A.M. Alrajeh has nothing to disclose.
Conflict of interest: A.M. Aldahahir has nothing to disclose.
Conflict of interest: S. Mandal has nothing to disclose.
Conflict of interest: J.R. Hurst reports personal fees and non-financial support from pharmaceutical companies that make medicines to treat COPD, outside the submitted work.
Support statement: This study was supported by Prince Sultan Military College of Health Sciences through the Saudi Arabian Cultural Bureau in London. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3: e442. doi: 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of COPD. 2017. http://goldcopd.org Date last accessed: 23 October 2019.
- 3.Vogelmeier CF, Criner GJ, Martinez FJ, et al. . Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med 2017; 195: 557–582. doi: 10.1164/rccm.201701-0218PP [DOI] [PubMed] [Google Scholar]
- 4.Iacobucci G. Hospital readmissions for COPD in England are rising, audit shows. BMJ 2017; 356: j557. doi: 10.1136/bmj.j557 [DOI] [PubMed] [Google Scholar]
- 5.Stone RA, Holzhauer-Barrie J, Lowe D, et al. . COPD: who cares when it matters most? National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme: outcomes from the clinical audit of COPD exacerbations admitted to acute units in England 2014. National supplementary report. London, RCP, 2017. [Google Scholar]
- 6.Rinne ST, Castaneda J, Lindenauer PK, et al. . Chronic obstructive pulmonary disease readmissions and other measures of hospital quality. Am J Respir Crit Care Med 2017; 196: 47–55. doi: 10.1164/rccm.201609-1944OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hartl S, Lopez-Campos JL, Pozo-Rodriguez F, et al. . Risk of death and readmission of hospital-admitted COPD exacerbations: European COPD Audit. Eur Respir J 2016; 47: 113–121. doi: 10.1183/13993003.01391-2014 [DOI] [PubMed] [Google Scholar]
- 8.Hurst JR, Bafadhel M, Bolton CE, et al. . COPD exacerbations: transforming outcomes through research. Lancet Respir Med 2018; 6: 172–174. doi: 10.1016/S2213-2600(18)30049-3 [DOI] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services. Health Readmissions Reduction Program (HRRP). Baltimore, U.S. Centers for Medicare Medicaid Services, 2018. [Google Scholar]
- 10.Feemster LC, Au DH. Penalizing hospitals for chronic obstructive pulmonary disease readmissions. Am J Respir Crit Care Med 2014; 189: 634–639. doi: 10.1164/rccm.201308-1541PP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kristensen SR, Bech M, Quentin W. A roadmap for comparing readmission policies with application to Denmark, England, Germany and the United States. Health Policy 2015; 119: 264–273. doi: 10.1016/j.healthpol.2014.12.009 [DOI] [PubMed] [Google Scholar]
- 12.Reducing COPD readmissions – a personal and political priority. Lancet Respir Med 2013; 1: 347. doi: 10.1016/S2213-2600(13)70153-X [DOI] [PubMed] [Google Scholar]
- 13.Press VG, Au DH, Bourbeau J, et al. . Reducing chronic obstructive pulmonary disease hospital readmissions an official American Thoracic Society workshop report. Ann Am Thorac Soc 2019; 16: 161–170. doi: 10.1513/AnnalsATS.201811-755WS [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahadori K, FitzGerald JM. Risk factors of hospitalization and readmission of patients with COPD exacerbation: systematic review. Int J Chron Obstruct Pulmon Dis 2007; 2: 241–251. [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Shamseer L, Clarke M, et al. . Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4: 1. doi: 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells GA, Shea B, O'Connell D, et al. . The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. www.ohri.ca/programs/clinical_epidemiology/oxford.asp Date last accessed: 23 January 2019.
- 17.Almagro P, Soriano JB, Cabrera FJ, et al. . Short- and medium-term prognosis in patients hospitalized for COPD exacerbation: the CODEX index. Chest 2014; 145: 972–980. doi: 10.1378/chest.13-1328 [DOI] [PubMed] [Google Scholar]
- 18.Baker CL, Zou KH, Su J. Risk assessment of readmissions following an initial COPD-related hospitalization. Int J Chron Obstruct Pulmon Dis 2013; 8: 551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bashir B, Schneider D, Naglak MC, et al. . Evaluation of prediction strategy and care coordination for COPD readmissions. Hosp Pract (1995) 2016; 44: 123–128. doi: 10.1080/21548331.2016.1210472 [DOI] [PubMed] [Google Scholar]
- 20.Bollu V, Ernst FR, Karafilidis J, et al. . Hospital readmissions following initiation of nebulized arformoterol tartrate or nebulized short-acting beta-agonists among inpatients treated for COPD. Int J Chron Obstruct Pulmon Dis 2013; 8: 631–639. doi: 10.2147/COPD.S52557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bottle A, Honeyford K, Chowdhury F, et al. . Factors associated with hospital emergency readmission and mortality rates in patients with heart failure or chronic obstructive pulmonary disease: a national observational study. Southampton, Health Service Delivery Research, 2018. [Google Scholar]
- 22.Candrilli SD, Dhamane AD, Meyers JL, et al. . Factors associated with inpatient readmission among managed care enrollees with COPD. Hosp Pract (1995) 2015; 43: 199–207. doi: 10.1080/21548331.2015.1085797 [DOI] [PubMed] [Google Scholar]
- 23.Chan FW, Wong FY, Yam CH, et al. . Risk factors of hospitalization and readmission of patients with COPD in Hong Kong population: analysis of hospital admission records. BMC Health Serv Res 2011; 11: 186. doi: 10.1186/1472-6963-11-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chawla H, Bulathsinghala C, Tejada JP, et al. . Physical activity as a predictor of thirty-day hospital readmission after a discharge for a clinical exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc 2014; 11: 1203–1209. doi: 10.1513/AnnalsATS.201405-198OC [DOI] [PubMed] [Google Scholar]
- 25.Choi J, Oh JY, Lee YS, et al. . Pseudomonas aeruginosa infection increases the readmission rate of COPD patients. Int J Chron Obstruct Pulmon Dis 2018; 13: 3077–3083. doi: 10.2147/COPD.S173759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Couillard S, Larivée P, Courteau J, et al. . Eosinophils in COPD exacerbations are associated with increased readmissions. Chest 2017; 151: 366–373. doi: 10.1016/j.chest.2016.10.003 [DOI] [PubMed] [Google Scholar]
- 27.Echevarria C, Steer J, Heslop-Marshall K, et al. . The PEARL score predicts 90-day readmission or death after hospitalisation for acute exacerbation of COPD. Thorax 2017; 72: 686–693. doi: 10.1136/thoraxjnl-2016-209298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Epstein D, Nasser R, Mashiach T, et al. . Increased red cell distribution width: a novel predictor of adverse outcome in patients hospitalized due to acute exacerbation of chronic obstructive pulmonary disease. Respir Med 2018; 136: 1–7. doi: 10.1016/j.rmed.2018.01.011 [DOI] [PubMed] [Google Scholar]
- 29.Ehsani H, Mohler MJ, Golden T, et al. . Upper-extremity function prospectively predicts adverse discharge and all-cause COPD readmissions: a pilot study. Int J Chron Obstruct Pulmon Dis 2019; 14: 39–49. doi: 10.2147/COPD.S182802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Genao L, Durheim MT, Mi X, et al. . Early and long-term outcomes of older adults after acute care encounters for chronic obstructive pulmonary disease exacerbation. Ann Am Thorac Soc 2015; 12: 1805–1812. doi: 10.1513/AnnalsATS.201504-250OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goto T, Faridi MK, Gibo K, et al. . Trends in 30-day readmission rates after COPD hospitalization, 2006–2012. Respir Med 2017; 130: 92–97. doi: 10.1016/j.rmed.2017.07.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gershon AS, Thiruchelvam D, Aaron S, et al. . Socioeconomic status (SES) and 30-day hospital readmissions for chronic obstructive pulmonary (COPD) disease: a population-based cohort study. PLoS One 2019; 14: e0216741. doi: 10.1371/journal.pone.0216741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hakim MA, Garden FL, Jennings MD, et al. . Performance of the LACE index to predict 30-day hospital readmissions in patients with chronic obstructive pulmonary disease. Clin Epidemiol 2018; 10: 51–59. doi: 10.2147/CLEP.S149574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hijjawi SB, Minshar MA, Sharma G. Chronic obstructive pulmonary disease exacerbation: a single-center perspective on hospital readmissions. Postgrad Med 2015; 127: 343–348. doi: 10.1080/00325481.2015.1015394 [DOI] [PubMed] [Google Scholar]
- 35.Jacobs DM, Noyes K, Zhao J, et al. . Early hospital readmissions after an acute exacerbation of chronic obstructive pulmonary disease in the nationwide readmissions database. Ann Am Thorac Soc 2018; 15: 837–845. doi: 10.1513/AnnalsATS.201712-913OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kon SS, Jones SE, Schofield SJ, et al. . Gait speed and readmission following hospitalisation for acute exacerbations of COPD: a prospective study. Thorax 2015; 70: 1131–1137. doi: 10.1136/thoraxjnl-2015-207046 [DOI] [PubMed] [Google Scholar]
- 37.Loh CH, Peters SP, Lovings TM, et al. . Suboptimal inspiratory flow rates are associated with chronic obstructive pulmonary disease and all-cause readmissions. Ann Am Thorac Soc 2017; 14: 1305–1311. doi: 10.1513/AnnalsATS.201611-903OC [DOI] [PubMed] [Google Scholar]
- 38.Nguyen HQ, Chu L, Amy Liu I-L, et al. . Associations between physical activity and 30-day readmission risk in chronic obstructive pulmonary disease. Ann Am Thorac Soc 2014; 11: 695–705. doi: 10.1513/AnnalsATS.201401-017OC [DOI] [PubMed] [Google Scholar]
- 39.Nguyen HQ, Rondinelli J, Harrington A, et al. . Functional status at discharge and 30-day readmission risk in COPD. Respir Med 2015; 109: 238–246. doi: 10.1016/j.rmed.2014.12.004 [DOI] [PubMed] [Google Scholar]
- 40.Rinne ST, Elwy AR, Bastian LA, et al. . Impact of multisystem health care on readmission and follow-up among veterans hospitalized for chronic obstructive pulmonary disease. Med Care 2017; 55: Suppl. 7, S20–S25. doi: 10.1097/MLR.0000000000000708 [DOI] [PubMed] [Google Scholar]
- 41.Rinne ST, Graves MC, Bastian LA, et al. . Association between length of stay and readmission for COPD. Am J Manag Care 2017; 23: e253–e258. [PMC free article] [PubMed] [Google Scholar]
- 42.Roberts MH, Mapel DW, Von Worley A, et al. . Clinical factors, including all patient refined diagnosis related group severity, as predictors of early rehospitalization after COPD exacerbation. Drugs Context 2015; 4: 212278. doi: 10.7573/dic.212278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shah T, Churpek MM, Coca Perraillon M, et al. . Understanding why patients with COPD get readmitted: a large national study to delineate the Medicare population for the readmissions penalty expansion. Chest 2015; 147: 1219–1226. doi: 10.1378/chest.14-2181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sharif R, Parekh TM, Pierson KS, et al. . Predictors of early readmission among patients 40 to 64 years of age hospitalized for chronic obstructive pulmonary disease. Ann Am Thorac Soc 2014; 11: 685–694. doi: 10.1513/AnnalsATS.201310-358OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simmering JE, Polgreen LA, Comellas AP, et al. . Identifying patients with COPD at high risk of readmission. Chronic Obstr Pulm Dis 2016; 3: 729–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Singh G, Zhang W, Kuo YF, et al. . Association of psychological disorders with 30-day readmission rates in patients with COPD. Chest 2016; 149: 905–915. doi: 10.1378/chest.15-0449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spece LJ, Epler EM, Donovan LM, et al. . Role of comorbidities in treatment and outcomes after chronic obstructive pulmonary disease exacerbations. Ann Am Thorac Soc 2018; 15: 1033–1038. doi: 10.1513/AnnalsATS.201804-255OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yu TC, Zhou H, Suh K, et al. . Assessing the importance of predictors in unplanned hospital readmissions for chronic obstructive pulmonary disease. Clinicoecon Outcomes Res 2015; 7: 37–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Donaldson GC, Seemungal TAR, Bhowmik A, et al. . Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 2002; 57: 847–852. doi: 10.1136/thorax.57.10.847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miravitlles M, Ferrer M, Pont A, et al. . Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax 2004; 59: 387–395. doi: 10.1136/thx.2003.008730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hurst JR, Vestbo J, Anzueto A, et al. . Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med 2010; 363: 1128–1138. doi: 10.1056/NEJMoa0909883 [DOI] [PubMed] [Google Scholar]
- 52.Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of COPD. 2019. http://goldcopd.org Date last accessed: 23 October 2019.
- 53.Andreas S, Rover C, Heinz J, et al. . Decline of COPD exacerbations in clinical trials over two decades – a systematic review and meta-regression. Respir Res 2019; 20: 186. doi: 10.1186/s12931-019-1163-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guerra B, Gaveikaite V, Bianchi C, et al. . Prediction models for exacerbations in patients with COPD. Eur Respir Rev 2017; 26: 160061. doi: 10.1183/16000617.0061-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tabak C, Smit HA, Räsänen L, et al. . Alcohol consumption in relation to 20-year COPD mortality and pulmonary function in middle-aged men from three European countries. Epidemiology 2001; 12: 239–245. doi: 10.1097/00001648-200103000-00018 [DOI] [PubMed] [Google Scholar]
- 56.Garcia-Aymerich J, Lange P, Benet M, et al. . Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population-based cohort study. Thorax 2006; 61: 772–778. doi: 10.1136/thx.2006.060145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Greening NJ, Williams JE, Hussain SF, et al. . An early rehabilitation intervention to enhance recovery during hospital admission for an exacerbation of chronic respiratory disease: randomised controlled trial. BMJ 2014; 349: g4315. doi: 10.1136/bmj.g4315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cheung PT, Wiler JL, Lowe RA, et al. . National study of barriers to timely primary care and emergency department utilization among Medicaid beneficiaries. Ann Emerg Med 2012; 60: 4–10. doi: 10.1016/j.annemergmed.2012.01.035 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Please note: supplementary material is not edited by the Editorial Office, and is uploaded as it has been supplied by the author.
Supplementary_material ERR-0166-2019_supplementary_material (345.3KB, pdf)