Abstract
COPD is associated with a progressive loss of muscle mass and function. However, there is an unmet need to define and standardise methods to estimate the prevalence of sarcopenia in COPD patients.
We performed a systematic review and meta-analysis of the prevalence of this extrapulmonary manifestation in COPD patients. We searched Embase, Medline (Ovid), CINAHL (EBSCO), Web of Science, Scopus and Google Scholar for studies published up to January 17, 2019, assessing sarcopenia in COPD patients based on low muscle mass and decreased muscle function. Interventional studies, in vitro experiments, protocols or reviews and meta-analyses were excluded. We estimated heterogeneity (I2) and assessed significance (Q) using a Chi-squared test for estimates obtained from random-effects models.
4465 articles were initially identified. After removing the duplicates and applying the selection criteria, we reviewed 62 full-text articles. Finally, 10 articles (n=2565 COPD patients) were included in this systematic review and meta-analyses. Overall, the prevalence of sarcopenia in patients with COPD was 21.6% (95% CI 14.6–30.9%, I2=94%), ranging from 8% in population-based to 21% in clinic-based studies, and 63% in COPD patients residing in nursing homes.
Sarcopenia is frequently observed in COPD patients, with varying prevalence across population settings. Sarcopenia in COPD should be assessed using standardised tests and cut-off points from sarcopenia consensus criteria for clinical practice and international comparisons.
Short abstract
We confirmed a high prevalence of sarcopenia in COPD patients, with varying prevalence across population settings. We recommend adhering to the sarcopenia consensus criteria to systematically evaluate the muscle health of COPD patients. http://bit.ly/2KA6weh
Introduction
COPD is a heterogeneous, complex and multisystem disease, with a vast number of intra- and extrapulmonary manifestations [1–5]. The clinical assessment of COPD patients is also complicated by the presence of multi-morbid conditions due to shared risk factors with other diseases [3, 6]. The extrapulmonary manifestations are increasingly recognised as important contributors to functional decline in patients with COPD [2, 3]. Functional impairment is associated with muscle weakness and body weight loss in COPD patients [5–7]. Irrespective of the method used to assess muscle mass [8], it is well known that patients with COPD suffer from loss of muscle mass [9–29]. Indeed, loss of muscle mass and muscle strength can be greater in patients with moderate-to severe COPD [7, 30] or during acute COPD exacerbations [31], especially loss of muscle from the lower limbs [6, 7, 32].
Low muscle mass and loss of muscle function have been described as the main components of sarcopenia [33–38], which was originally defined as a multifactorial geriatric syndrome [39]. However, there has been increasing recognition of this muscle disorder as a disease-related rather than just age-related condition [40]. The 2018 European Working Group of Sarcopenia in Older People (EWGSOP2) have reinforced the importance of distinguishing “secondary sarcopenia” when factors other than ageing are involved from “primary sarcopenia” or age-related sarcopenia [38]. Sarcopenia can result from underlying diseases such as COPD or other conditions characterised by chronic inflammation [38]. Although COPD occurs mainly in middle-aged and older people, sarcopenia in COPD can occur independent of age [41]. Therefore, early detection of sarcopenia might be pivotal, given that it has therapeutic implications such as pulmonary rehabilitation and management of respiratory failure in COPD patients.
Although many aspects of the pathophysiology of sarcopenia are better understood now than a decade ago [38], the precise aetiology of sarcopenia and underlying explanatory mechanisms are still not fully established [42, 43]. However, physical inactivity, weight loss, inflammatory cytokines, inadequate energy intake, oxidative stress and reduced blood flow to muscles are common features linked with sarcopenia [43] as well as COPD [3, 5, 44]. For instance, it is well known that limb muscle dysfunction in COPD contributes to loss of muscle strength [7]. Despite the heterogeneity in the muscle fibre proportions in COPD patients [45], there is a shift from type I to II fibres, which correlates inversely with disease severity [7]. By contrast, age-related loss of muscle strength and mass are mainly attributed to muscle fibre denervation and loss of type II fibres [46].
In the last decade, different international consensus criteria of sarcopenia [33–38] have focused clinically and operationally on the measurements and thresholds of sarcopenia (table 1). For instance, five out of six sarcopenia consensus statements recommend muscle mass measurement as a first criterion to define sarcopenia. Only the updated EWGSOP2 recommends including muscle strength as the main criterion of sarcopenia, and labelling the patient as having “probable sarcopenia” [38] when muscle strength is compromised.
TABLE 1.
Criteria and cut-off points to diagnose sarcopenia according to the main consensus criteria groups
| Consensus group | Main criteria definition | Lean muscle mass | Muscle function | |||
| Handgrip strength | Gait speed m·s−1 | SPPB | TUG | |||
| ESPEN SIG [33] | Low muscle mass plus low gait speed | 2sd below mean of young adults of the same sex and ethnic background | <0.8 (4MGS) | |||
| EWGSOP [34] | Low muscle mass plus low muscle strength or low gait speed | ASMI: | Male <30 kg | <0.8 (4MGS) | ≤8 | |
| DXA score | Female <20 kg | |||||
| Male ≤7.26 kg·m−2 | ||||||
| Female ≤5.54 kg·m−2 | ||||||
| (2sd below mean of young adults) | ||||||
| BIA score: | ||||||
| Male 8.87 kg·m−2 | ||||||
| Female 6.42 kg·m−2 | ||||||
| (2sd below mean of young adults) | ||||||
| IWGS task force [35] | Low ASMI plus low gait speed | ASMI: | <1 (4MGS) | |||
| Male ≤7.23 kg·m−2 | ||||||
| Female ≤5.67 kg·m−2 | ||||||
| FNIH [36] | Low ALM/BMI plus low handgrip | ALM/BMI | Male <26 kg | <0.8 (4MGS, 6MWT) | ||
| Male <0.789 | Female <16 kg | |||||
| Female <0.512 | kg/BMI | |||||
| Male <1 | ||||||
| Female <0.56 | ||||||
| AWGS [37] | Low ASMI plus low gait speed or low handgrip | ASMI: | Male <26 kg | ≤0.8 (6MWT) | ||
| Male ≤7.0 kg·m−2 | Female <18 kg | |||||
| Female ≤5.4 kg·m−2 | ||||||
| EWGSOP2 [38] | Low muscle strength plus low muscle mass; severity of sarcopenia involve low physical performance | ASMI: | Male <27 kg | ≤0.8 | ≤8 | ≥20 s |
| Male <7.0 kg·m−2 | Female <16 kg | |||||
| Female <5.5 kg·m−2 | ||||||
SPPB: Short Physical Performance Battery; TUG: timed up and go test; ESPEN SIG: European Society of Clinical Nutrition and Metabolism Special Interest Group (“cachexia-anorexia in chronic wasting diseases”); EWGSOP: European Working Group on Sarcopenia in Older People; IWGS: International Working Group on Sarcopenia; FNIH: Foundation for the National Institutes of Health; AWGS: Asian Working Group on Sarcopenia; 4MGS: 4-min gait speed; ASMI: appendicular skeletal muscle mass index; DXA: dual-energy X-ray absorptiometry; BIA: bioelectrical impedance analysis; BMI: body mass index; ALM: appendicular lean mass; 6MWT: 6-min walk test.
Using these consensus criteria, it has recently been reported that 10% of healthy older adults have sarcopenia [47]. However, the prevalence of sarcopenia varies widely (0.9%–32.8%) among different study populations [48]. No global estimates of the prevalence of sarcopenia in COPD patients with the consensus definitions have previously been reported. Estimating the overall prevalence of sarcopenia, according to the contemporary operational definitions recommended by multidisciplinary consensus, will provide further insight into its burden in COPD.
Therefore, we conducted a systematic review and meta-analysis to appraise the best available evidence on the prevalence of sarcopenia among COPD patients based on the consensus definitions.
Methodology
Search strategy and data sources
This systematic review and meta-analysis adheres to the schema of Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) [49, 50]. We performed an electronic search of Embase.com, Medline (Ovid), CINAHL (EBSCO), Web of Science, Scopus and Google Scholar to identify all relevant articles relating to sarcopenia and COPD. We searched all records published from inception through to January 17, 2019, in collaboration with a medical information specialist (GdJ). Terms related to COPD (e.g. “chronic obstructive pulmonary disease”) and key terms were combined with synonyms of sarcopenia (e.g. “muscle atrophy”). We further hand-searched bibliographies of relevant publications to identify potential articles missed by the principal search. Full search terms are listed in supplementary table S1.
This systematic review is registered in the International Prospective Register of Systematic Reviews (PROSPERO), number CDR42018095480.
Selection criteria
For this systematic review, we used the following inclusion criteria: 1) all studies had to be case–control, longitudinal or cross-sectional designs; 2) assessment of sarcopenia had to be implemented according to the sarcopenia consensus criteria (muscle mass and muscle strength or physical performance are combined); 3) measurement of lean mass or muscle mass had to be assessed by at least one of four main methods [8] (bioelectrical impedance analysis, dual-energy X-ray absorptiometry, magnetic resonance imaging or computed tomography); 4) the prevalence of sarcopenia (primary outcome) in COPD patients had to be reported.
To provide additional insight into the prevalence of sarcopenia in COPD patients, we also investigated the associations of sarcopenia (if available in the study, e.g. odds ratio) and COPD as a secondary outcome measure.
We limited our inclusion to original publications, without language restriction, and excluded experimental studies, reviews and meta-analyses, comments, guidelines, editorials or letters and case reports. Furthermore, studies that referred to other populations were excluded (i.e. asthma or cystic fibrosis) (supplementary table S2).
Two independent co-authors (EB and KT) screened all the articles by title and abstract. Disagreements were resolved by consensus between both co-authors together with a third co-author (LL). The citations were classified as “eligible”, “uncertain about eligibility” or “excluded” and stored in an EndNote file. The full text of articles classed as “eligible” and “uncertain about eligibility” was reviewed and appraised independently by two co-authors (EB and KT), and disagreements were solved through revision and consultation with a fourth independent co-author (JDS).
Data synthesis
We used a predefined data collection form in which we summarised relevant information on characteristics of the study population (age, sex, setting), outcome assessment (prevalence of sarcopenia, definition of sarcopenia using any of the consensus criteria, cut-off points, and methods to measure handgrip and mass muscle) and the effect estimate of association (if available in the study; odds ratio adjusted for most confounders) with the corresponding precision estimate (95% confidence interval). When relevant data were not available, the corresponding authors of the selected publications were contacted to complement the electronic searches.
Risk of bias assessment
We assessed the quality of the selected studies using an adapted version of the scale developed by Hoy et al. [51] for prevalence estimates. The tool consists of 10 items addressing external and internal validity. Moreover, we used an adapted Newcastle–Ottawa Scale [52] for cross-sectional studies that measured association between prevalence of sarcopenia and COPD. Two co-authors (EB and KT) independently rated each of the items of both scales into a global score adding all the items rated as low risk. Therefore, higher scores indicated lower risk of bias (supplementary table S3).
Statistical analysis
We summarised prevalence of sarcopenia across studies as its estimator (prevalence) and confidence intervals and present data in tables of study characteristics.
Meta-analysis on the prevalence of sarcopenia in COPD patients was undertaken using a random-effects model, using the packages meta and metaprop in R (version 3.5.1; R Foundation for Statistical Computing, Vienna, Austria).
Heterogeneity across studies was defined by an I2 of >50% [53]. Given that the preliminary analyses demonstrated high heterogeneity, we stratified our analysis by population setting to explore potential sources of heterogeneity. We used a funnel plot adjusted for population setting to also measure publication bias [54].
Results
Search results
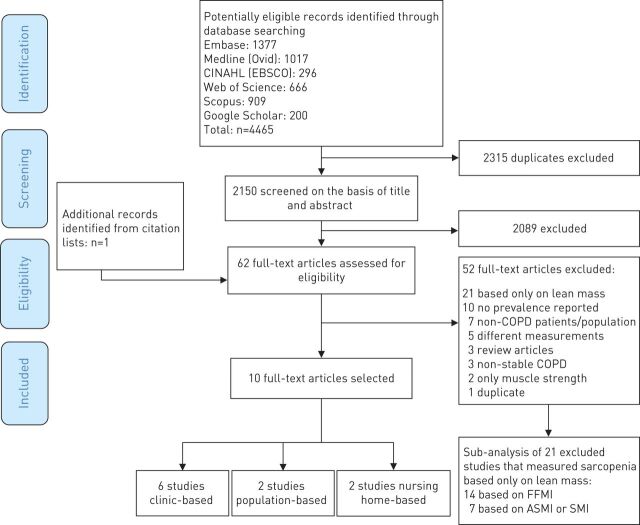
Our search yielded 4465 records, of which 2315 duplicates were removed, resulting in 2150 unique articles. We read the full text of 62 articles, and determined that 10 of them were eligible for inclusion in this meta-analysis (figure 1) [55–64].
FIGURE 1.
Flow diagram of the study selection process. FFMI: fat-free mass index; ASMI: appendicular skeletal muscle mass index; SMI: skeletal muscle mass index.
Characteristics of studies included
Among the 10 eligible studies published between 2012 and 2018, six were performed only in COPD patients without a control group [55–57, 59, 60, 63], two reported data on population-based prevalence [58, 61] and two were nursing home based [62, 64]. Four studies were from Europe [55, 58, 63, 64], four from Asia [57, 59, 60, 62] and two from South America [56, 61]. The total number of COPD participants involved in all selected studies was 2565, with a mean age ranging from 62 to 84 years at study entry (table 2).
TABLE 2.
Main characteristics of the cross-sectional selected studies in the meta-analysis
| First author [ref.] | Country | Subjects n | Male | Age years | Setting | Consensus group | Prevalence % (n) | Components of sarcopenia | |||||
| Lean mass | Muscle strength | Physical performance | |||||||||||
| Method | Cut-off | Method | Cut-off kg | Method | Cut-off m·s −1 | ||||||||
| De Blasio [55] | Italy | COPD: 263 | 70.3 | 69.8±8.0 | Clinical | EWGSOP | 24 (63) | BIA (SMI) | M: ≤8.50 kg·m−2 F: ≤5.75 kg·m−2 |
HGS | NS | 4MGS | <0.8 |
| Munhoz da Rocha Lemos Costa [56] | Brazil | COPD: 121 | 46.3 | 67.9±8.6 | Clinical | FNIH | 12.4 (15) | DXA (ALM/BMI) | M: <0.789 F: <0.512 |
NS | 6MWT | ≤0.8 | |
| Limpawattanaz [57] | Thailand | COPD: 121 | 92.6 | >65 | Clinical | AWGS | 24 (29) | DXA (ASMI) | M: ≤7.0 kg·m−2 F: ≤5.4 kg·m−2 |
HGS | M: 26 F: 18 |
6MWT | <0.8 |
| Trajanoska [58] | Netherlands | COPD: 882 All population: 5911 |
69.2±9.1 | Population | EWGSOP | COPD: 7.9 (70) All population: 4.4 (260) |
DXA (SMI) | M: ≤7.25 kg·m−2 F: ≤5.67 kg·m−2 |
HGS | M: ≤29 (if BMI ≤24) | GAITRite | M: <0.65 (if height ≤173 cm) | |
| ≤30 (if BMI ≤24.1–28) | <0.76 (if height >173 cm) | ||||||||||||
| ≤32 (if BMI >28) | F: <0.65 (if height ≤159 cm) | ||||||||||||
| F: ≤17 (if BMI ≤23) | <0.76 (if height >159 cm) | ||||||||||||
| ≤17.3 (if BMI ≤23.1–26) | |||||||||||||
| ≤18 (if BMI ≤26.1–29) | |||||||||||||
| ≤21 (if BMI >29) | |||||||||||||
| Byun [59] | Korea | COPD: 80 | 83.8 | 68.4±8.9 | Clinical | EWGSOP | 25 (20) | BIA (SMI) | Below 2sd of mean population | HGS | M: ≤30 F: ≤20 |
NS | |
| Lian [60] | China | COPD: 96 | 58.3 | 62.4±7.9 | Clinical | EWGSOP | 28.1 (27) | BIA (SMI) | M: ≤7.01 kg·m−2 F: ≤5.43 kg·m−2 |
HGS | M: ≤35.04 F: ≤21.82 |
NS | |
| Borda [61] | Colombia | COPD/asthma: 334 No COPD/asthma: 1666 |
32.9 | >60 | Population | EWGSOP | COPD/asthma: 11 (28) No COPD/asthma: 6.9 (77) |
CC | <31 cm | NS | 4MGS | ||
| Tasar# [62] | Turkey | COPD: 33 All population: 211 |
69.7 | 73.9±7.2 | Nursing home | EWGSOP | COPD: 66.7 (22) All population 33.6 (71) |
BIA (FFM/BSA) | Below the 20th percentile of mean population | HGS | M: ≤30 F: ≤20 |
6MWT | ≤0.8 |
| Jones [63] | UK | COPD: 622 | 58.8 | 73±8 | Clinical | EWGSOP | 14.5 (90) | BIA (SMI) | M: ≤8.50 kg·m−2 F: ≤5.75 kg·m−2 |
HGS | M: <30 F: <20 |
4MGS | <0.8 |
| Landi [64] | Italy | COPD: 13 All population: 122 |
68 | 84±7.3 | Nursing home | EWGSOP | COPD: 53.4 (7) All population: 32.8 (40) |
BIA (SMI) | M: <8.87 kg·m−2 F: <6.42 kg·m−2 |
HGS | M: <30 F: <20 |
4MGS | ≤0.8 |
Data are presented as % or mean±sd, unless otherwise stated. EWGSOP: European Working Group Older People; M: male; F: female; BIA: bioelectrical impedance analysis; SMI: skeletal muscle index; NS: not specified; HGS: handgrip strength; 4MGS: 4-min gait speed; FNIH: Foundation for the National Institute of Health; DXA: dual-energy X-ray absorptiometry; ALM: appendicular lean mass; BMI: body mass index; 6MWT: 6-min walk test; AWGS: Asian Working Group on Sarcopenia; ASMI: appendicular skeletal muscle mass index; GAITRite: 5.79-m-long electronic walkway; CC: calf circumference; FFM: fat-free mass; BSA: body surface area. #: data directly obtained from authors.
Eight of the selected studies used the EWGSOP definition of sarcopenia [55, 58–64], and two of them applied the Foundation for the National Institutes of Health (FNIH) and the Asian Working Group on Sarcopenia consensus (table 1) [56, 57]. When we analysed the components of sarcopenia in these 10 studies, we found large variability in the methods and cut-off points, especially for lean mass. All these studies assessed lean mass by dual-energy X-ray absorptiometry or bioelectrical impedance rather than magnetic resonance imaging or computed tomography, although one used calf circumference to measure lean mass (table 2) [61].
Quality assessment
Quality assessment scores of all included observational studies are listed according to prevalence, and two of them according to association estimators (supplementary tables S4 and S5). Regarding methodological quality of the prevalence estimator, seven (70%) had moderate risk of bias and three (30%) had low risk of bias.
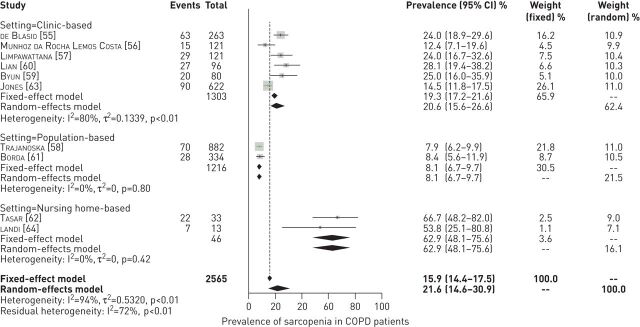
Prevalence of sarcopenia in COPD patients
The prevalence of sarcopenia in COPD patients ranged from 7.9% to 66.7%. There was substantial heterogeneity between studies (I2=94%, p<0.01), which could largely be accounted for by two studies [62, 64]. These two nursing home-based studies, which had the smallest combined sample size (n=46 COPD patients) of any study included, reported the highest prevalence of sarcopenia. When excluding these studies in a sensitivity analysis, the prevalence of sarcopenia was 16.5% (95% CI 11.4%–23.2%), with high heterogeneity (I2=92%, p<0.01) (supplementary figure S1).
Therefore, we included the 10 studies and stratified our analysis according to the three main population settings: 1) clinic based, 2) population based and 3) nursing home based. Stratifying our analysis resulted in a reduction of heterogeneity within the three population settings. Consequently, the pooled prevalence of sarcopenia was 21.6% (95% CI 14.6%–30.9%) (figure 2 and supplementary table S6). There was symmetry for the funnel plot describing publication bias in these 10 selected studies when stratified by population setting (supplementary figure S2).
FIGURE 2.
Fixed- and random-effects meta-analysis results for the prevalence of sarcopenia in patients with COPD, according to population setting. The authors directly provided the prevalence estimate for the study by Tasar et al. [62].
Additionally, we meta-analysed all the excluded studies that measured only the lean mass component of sarcopenia given that, prior to 2010, having a low lean mass was considered to represent sarcopenia (figure 1) [34, 38, 40]. These studies applied two main muscle indices: appendicular skeletal muscle mass index (ASMI), also referred as skeletal mass index (SMI) [9–15], and fat-free mass index (FFMI) [16–29]. The prevalence of low lean mass based on ASMI in COPD patients was 31.0% (95 CI 28.2%–34.2%, I2=65%, p<0.01). According to FFMI, the prevalence of low lean mass in COPD patients was 23.4% (95% CI 18.6%–29.0%, I2=96%, p<0.01) (supplementary figure S3; supplementary tables S7, S8, S9). After performing this division by index muscle, the I2 statistics (65% and 96% respectively, p<0.01), although lower than when using the sarcopenia consensus criteria, still indicated heterogeneity.
Association of sarcopenia and COPD
In addition to the prevalence of sarcopenia described in the aforementioned studies, despite the considerable variation of the cut-off points, the association of sarcopenia with COPD was tested in two studies. Borda et al. [61] investigated the association of sarcopenia in 250 COPD/asthma participants, and the odds ratio for sarcopenia was 2.01 (95% CI 1.21–3.35), independent of sex, age, educational level and body mass index (BMI). Moreover, Tasar et al. [62] reported that the odds ratio for elderly people with COPD to have sarcopenia was 1.69 (95% CI 0.83–3.43).
Factors associated with sarcopenia in COPD patients
Some of the main factors associated with sarcopenia in COPD patients were age [56, 59, 60], especially among the older group (≥75 years old) [57]; systemic inflammatory biomarkers (high-sensitivity tumour necrosis factor-α (hsTNF-α)) [59]; and BMI, either separately (both high [57] and low [59]) or as part of the BODE index (BMI, airflow obstruction, dyspnoea and exercise) [56] (supplementary table S10).
Smoking, one of the main risk factors for COPD, was associated with sarcopenia in one study [60], whereas in two other studies it was not [56, 57]. In addition, Jones et al. [63] did not find a difference in smoking status between COPD patients with and without sarcopenia.
Severity of COPD [57], severity of dyspnoea [57] and cardiovascular disease [59] were the main clinical outcomes associated with sarcopenia in COPD patients. De Blasio et al. [55] reported that 58.7% of COPD patients with sarcopenia were also malnourished. In the study of Jones et al. [63], COPD patients with sarcopenia had more severe airflow obstruction (low forced expiratory volume in 1 s (FEV1)) and reduced physical activity, functional performance and exercise capacity.
When the components of sarcopenia were analysed separately, Byun et al. [59] found that handgrip and SMI were negatively correlated with serum interleukin-6 (r= −0.27 and r= −0.23, respectively) and hsTNF-α (r= −0.35 and r= −0.25, respectively).
Discussion
Overall, we found that ∼22% of individuals with COPD had sarcopenia. The prevalence estimates of sarcopenia varied between 12.4% and 28.1% in clinical settings, and 7.9% and 8.4% in population-based settings. Prevalence was highest in nursing home settings, ranging from 53.8% to 66.7%. We observed large heterogeneity across studies, attributed to important differences in methods and cut-off points used to assess muscle mass, and particularly the distinct population settings. Therefore, differences between study settings (i.e. community dwelling versus institutionalised patients) should be considered when assessing the risk of sarcopenia in COPD patients.
In COPD patients, Bone et al. [42] have previously described the importance of sarcopenia based on consensus criteria. However, to the best our knowledge, this systematic review including a meta-analysis is the first to assess the prevalence of sarcopenia in patients with COPD. This meta-analysis notes the heterogeneity induced by the different methods used to assess sarcopenia and the type of population setting.
Clinic-based studies
The vast majority of the selected studies reporting prevalence of sarcopenia in COPD patients were clinic based, with high heterogeneity between studies (I2=80%, p<0.01). Notably, two studies using the same cut-off points and methods to measure sarcopenia in COPD patients [55, 63] reported prevalence estimates with big discrepancies (∼10% difference). However, the study by de Blasio et al. [55] (n=263) included more male COPD patients (70%), and the sarcopenic group (n=26) had more deteriorated lung function (FEV1 % pred 30.9%, 95% CI 26.1%–35.7%) than that of Jones et al. [63] (n=622) (sarcopenic group (n=90), FEV1 % pred 43.5%, 95% CI 37.4%–50.2%).
Population-based studies
The prevalence of sarcopenia in COPD population-based studies was lower than in clinical settings. This finding can be explained by the fact that COPD cases from the population are more often in an early stage of the disease or even asymptomatic. Two population-based studies reported the prevalence of sarcopenia in COPD [58, 61]; although they used the same consensus criteria [34], there was no uniformity in the measurement methods used, particularly for lean mass. Trajanoska et al. [58] performed a specific calculation of each component of sarcopenia, based on BMI and height, for male and female patients. By contrast, Borda et al. [61] calculated low lean mass based on calf circumference for both sexes in patients with COPD/asthma. This makes comparison between the two studies difficult.
Nursing home-based studies
The high prevalence of sarcopenia in COPD patients from nursing homes can be explained by two main factors. First, the selected studies had small sample sizes (<50 participants). Second, according to the mean age, these participants were older than the age range mean of the clinic- and population-based studies. However, while the prevalence of sarcopenia increases notably with ageing, the high prevalence within COPD patients is unlikely to be explained by age alone. There are biological mechanisms by which respiratory impairment contributes to muscle deterioration [7], e.g. patients with more severe emphysema have lower muscle mass [30].
Sarcopenia consensus statements
We found six international sarcopenia consensus criteria that can be applied in clinical and research fields [33–38]. All of these criteria are based on lean mass and physical performance related to muscle loss, but there is still a lack of uniformity in measurement standards, and especially in cut-off points across these criteria. However, the cut-off points for lean mass and handgrip strength measurements from two of the consensus criteria (EWGSOP2 and FNIH) are practically equivalent [36, 38].
The majority of our selected studies (n=8) [55, 58–64] applied the EWGSOP criteria to define sarcopenia in COPD patients. According to the updated EWGSOP2 [38] recommendations, muscle strength can be considered as the principal determinant of sarcopenia, mainly because it can facilitate early identification of sarcopenia in clinical practice. EWGSOP2 have modified and simplified the cut-off points to identify primary and secondary sarcopenia in a broad population [40]. Consequently, we suggest using the EWGSOP2 practical algorithm for case finding, diagnosis of sarcopenia and determining sarcopenia severity in COPD patients. We encourage clinicians to start by systematically assessing handgrip in all COPD patients, which is easily performed, rather than with other tests that can be influenced by COPD due to ventilator restrictions.
To classify the severity of sarcopenia, EWGSOP2 recommends different tests, e.g. gait speed, 400-m walk test, Short Physical Performance Battery and timed up and go test (TUG), with corresponding cut-off points. In COPD patients, an optimal test should be targeted for each case. For instance, the TUG test has not been associated with airflow limitation, in contrast to the 6-min walk distance [65]. Therefore, the TUG test could be implemented in cases of COPD with more severe ventilatory impairment. Similarly, a cut-off point (11.2 s) different from the EWGSOP2 recommendation (20 s) has been suggested for use as an abnormal TUG time for COPD patients [66]. Nevertheless, additional studies are needed to establish which functional test and cut-offs should be used across different stages of COPD. Given that these updated recommendations have only recently been introduced, their performance within COPD patients has not yet been performed and warrants future studies.
When we analysed each element of sarcopenia across studies, muscle mass was the component with most variability in its measurements, mainly due to muscle indices and cut-off points. For instance, in Asian populations, Byun et al. [59] used a SMI below 2sd of the mean of the Korean population, whereas Lian et al. [60] used cut-offs close to the ASMI. To diagnose sarcopenia in patients with COPD, dual X-ray absorptiometry and bioelectrical impedance analysis were used to measure lean mass. However, no consensus has been reached concerning cut-off points of lean mass across different international (working) groups for the diagnosis of sarcopenia. Therefore, for both SMI and ASMI, the cut-off points require further validation and standardisation. There is more consistency across the sarcopenia consensus criteria groups for assessing muscle function, although a wide range of cut-off points have been recommended (e.g. handgrip in males ranges from 26 kg to 30 kg). In addition, cut-offs for gait speed were essentially the same (≤ or <0.8 m·s−1). Only the method to measure gait speed differed across studies: some articles used the 6-min walk test and others 4-m gait speed (m·s−1). However, 4-m gait speed is significantly correlated with the 6-min walk test in COPD patients [67]. Studies are required to further establish the role and interaction of each sarcopenia component in COPD patients.
Factors associated with sarcopenia in COPD patients
We only found two studies that reported an association between sarcopenia and COPD [58, 61], even after adjustment for age, sex and BMI. Additionally, Trajanoska et al. [58] reported that the difference in sarcopenia prevalence between COPD and non-COPD individuals was independent of age, sex, smoking and corticosteroid use.
Multiple factors were associated with the presence of sarcopenia in COPD patients in the selected studies. These factors included age, severity of COPD, BMI, BODE index, dyspnoea and elevated inflammatory biomarkers, such as TNF-α [56, 57, 59, 60]. However, the direct effect of smoking on sarcopenia, an established risk factor for COPD, showed different associations across studies. For instance, only one study [60] reported an association between smoking and sarcopenia among COPD patients, whereas two other studies did not [56, 57]. Likewise, in support of a negative association, another study did not find differences in smoking across COPD patients with and without sarcopenia [63]. One explanation for these discrepancies might originate from distinct smoking classification across studies; while Lian et al. [60] used cumulative smoking exposure (i.e. a long-term history of smoking, defined as ≥10 cigarettes/day for 10 years), all other studies categorised smoking status as never, past and current.
None of these studies reported sex differences in the prevalence of sarcopenia, in contrast to what has been shown in previous studies on COPD patients that mainly focused on lean mass (and not on sarcopenia) [13, 22]. Moreover, COPD patients with sarcopenia had lower FEV1, lower exercise capacity and lower physical activity than patients without sarcopenia [63]. Therefore, in terms of sarcopenia in COPD patients, factors including age, severity of COPD, BMI, BODE index, dyspnoea and hsTNF-α might add value to preventive strategies, especially when these strategies are modifiable. Likewise, other factors such as corticosteroid use, protein intake and alcohol use were not considered and as such these should be of interest for future research.
Cruz-Jentoft et al. [38] consider sarcopenia as “secondary” when another factor besides ageing is present. They state that secondary sarcopenia can occur due to a systemic disease (i.e. COPD), physical inactivity and inadequate energy intake, among other factors [38]. However, there is not any distinction in recommendations of methods and cut-offs for distinguishing primary and secondary sarcopenia. It is important to consider that across these selected studies, age was associated with sarcopenia, which is also in line with the fact that COPD patients with sarcopenia are older. Only one study did not find age differences in COPD patients with and without sarcopenia [55]. Nevertheless, patients in all of these studies were aged >60 years. Therefore, an overlap between primary and secondary sarcopenia in COPD patients can be expected and is difficult to differentiate. Additionally, sarcopenia is increasingly recognised as a progressive and generalised muscular disorder related to long-term conditions presenting during midlife, such as COPD [40]. Nevertheless, sarcopenia in COPD patients seems to be more disease-related than age-related, as supported by distinct physiopathological processes related to ageing and COPD. With ageing there is a transition of the muscle fibres from type II to type I [68], involving intra- and inter-muscular adipose tissue [69]. In contrast, in COPD there is mainly a shift from type I to type II fibres [7] that can be responsible for dyspnoea symptomatology and/or low performance during exercise tests. Further understanding of the main molecular and cellular mechanisms underlying the onset of sarcopenia in COPD patients could support the optimisation of assessment tools for sarcopenia in COPD.
Strengths of this systematic review include the use of a predefined protocol, a comprehensive search strategy and the involvement of two independent co-authors in all stages of the process. Nevertheless, it is not free of limitations, and several topics should be taken into account when interpreting our results. First, as was previously highlighted, despite our results being centred around all sarcopenia consensus criteria, the cut-off points for its components were not uniform across studies. One explanation might be that there were different indices to measure muscle mass, and consequently there were different cut-offs. For instance, despite most of the selected studies used EWGSOP consensus criteria, they used different indices to measure lean mass (appendicular lean mass/height2, skeletal muscle mass/height2, fat-free mass/body surface area); they also applied different cut-offs even for the same muscle index. Another explanation may be that they used different dual-energy X-ray absorptiometry and bioelectrical impedance analysis devices to measure lean mass. It is well known that bioelectrical impedance analysis, an inexpensive alternative to dual-energy X-ray absorptiometry, is dependent on the formula used [70], which differed among these studies. It has also been widely reported that dual-energy X-ray absorptiometry and bioelectrical impedance measurements in healthy adults provide different estimates of fat mass and fat-free mass [71]. Second, the main aim of this systematic review and meta-analysis was to provide a comprehensive overview of the current overall prevalence of sarcopenia in COPD patients, independent of the population setting. However, the six clinic-based studies used different consensus criteria and were performed in different ethnic groups, resulting in different estimates of sarcopenia prevalence. Similarly, the two population-based studies used different cut-offs and measurements, as did the nursing home studies, and the quality assessment of the selected studies varied, affecting the external validity. Therefore, our results may not be representative for COPD patients in general. Likewise, our results highlight that population-based studies on the association of main lifestyle factors (e.g. diet, physical activity, smoking) with sarcopenia in COPD patients remain limited.
More studies are needed to identify the main characteristics of COPD patients who present with sarcopenia defined by low muscle mass and function. This is particularly the case given that the updated EWGSOP2 recommendations mention that healthcare professionals have increasing possibilities for preventing, delaying, treating and even reversing sarcopenia [38]. EWGSOP2 have described that low muscle strength should be considered as “probable sarcopenia”. Therefore, systematically measuring the handgrip of each COPD patient, independent of the clinical setting, can contribute to early detection, prevention and treatment of sarcopenia. Muscle strength is determined by the velocity and type of contraction, size and motor units activated [7], which are affected early in COPD patients [7]. However, this does not mean that we should consider only handgrip for early detection of sarcopenia in patients with COPD, because the relationship between muscle mass and muscle function is nonlinear [72]. In addition, according to new recommendations of the Global Leadership Initiative on Malnutrition [73], having low muscle mass with normal muscle strength would be considered to be a result of malnutrition rather than sarcopenia.
We propose that the EWGSOP2 algorithm be used in clinical practice [38], and muscle strength assessed in all COPD patients. We call for more research directed towards defining optimal cut-off points of tests measuring muscle mass or function in patients with COPD. Importantly, multidisciplinary interventions such as pulmonary rehabilitation, which is included in the EWGSOP2 algorithm, have been shown to improve physical performance and exercise capacity in patients with COPD. The different steps of the diagnostic approach to sarcopenia in patients with COPD, encompassing case finding, assessment, confirmation and determining its severity, are illustrated in table 3.
TABLE 3.
EWGSOP2 algorithm for case finding, making a diagnosis and quantifying severity of sarcopenia in clinical practice with clinical and research considerations for COPD patients
| Steps | Components | Response | Considerations for COPD patients |
| Step 1: Case finding | SARC-F or clinical suspicion | +: Go to step 2 | SARC-F in all COPD patients |
| −: No sarcopenia, rescreen later | |||
| Step 2: Assess | Muscle strength (grip strength or chair stand test) | +: Go to step 3 plus start intervention: “probable sarcopenia” | Call for research directed to define accurate cut-off points for low muscle strength in COPD patients |
| −: No sarcopenia, rescreen later | |||
| Step 3: Confirm | Muscle quantity or quality (DXA, BIA, CT, MRI) | +: Go to step 4 plus intervention: “sarcopenia” | Call for research directed to define accurate cut-off points for low muscle mass in COPD patients |
| −: Intervention for “probable sarcopenia” | |||
| Step 4: Severity | Physical performance (gait speed, SPPB, TUG, 400 m walk) | +: “Severe sarcopenia” | Call for research directed to define optimal physical performance tests and accurate cut-off points for COPD patients |
| −: Intervention for “sarcopenia” |
EWGSOP2: 2018 European Working Group Older People; SARC-F: questionnaire with the five components of strength, assistance with walking, rise from a chair, climb stairs and falls; DXA: dual-energy X-ray absorptiometry; BIA: bioelectrical impedance analysis; CT: computed tomography; MRI: magnetic resonance imaging; SPPB: Short Physical Performance Battery; TUG: timed up and go test.
Finally, it is important to highlight that we found the overall prevalence of sarcopenia in COPD patients to be twice as high as compared to a healthy elderly population. In conclusion, sarcopenia defined as low muscle mass plus reduced muscle function is a frequent extrapulmonary condition in COPD patients. Despite the sarcopenia consensus criteria, there is still a lack of agreement in the optimal method and cut-off points to assess sarcopenia in general and in COPD patients in particular. Therefore, it is necessary to standardise the assessment methods for clinical practice and future research in COPD patients.
Acknowledgments
The authors are grateful for the input of Alfonso J. Cruz-Jentoft (Hospital Universitario Ramon y Cajal, Madrid, Spain), primarily his information and comments regarding the search strategy. The authors also thank J. Jean Joel Bigna (Dept of Epidemiology and Public Health, Centre Pasteur of Cameroon, Yaoundé, Cameroon) and Damian Hoy (Global Musculoskeletal Alliance, University of Sydney, Sydney, Australia) for helpful advice relating to quality scoring. In addition, the authors kindly thank Jinluan Chen (Dept of Internal Medicine and Dept of Epidemiology, Erasmus MC, University Medical Center, Rotterdam, The Netherlands) for her collaboration in the Chinese translation and Joost van Rosmalen (Dept of Biostatistics, Erasmus MC, University Medical Center, Rotterdam, The Netherlands) for providing additional input in the meta-analysis.
Footnotes
This article has supplementary material available from err.ersjournals.com
This review is registered with PROSPERO with identifier CRD42018095480
Provenance: Submitted article, peer reviewed.
Author contributions: All the authors contributed their intellectual knowledge in this study. E. Benz, K. Trajanoska, L. Lahousse, J.D. Schoufour, O.H. Franco, G. Brusselle and F. Rivadeneira designed the study. E. Benz and K. Trajanoska performed all review activities including searches, study selection (including inclusion and exclusion of abstracts), data extraction and quality assessment. G.B de Jonge created the search strategies in all databases. L. Lahousse and J.D. Schoufour supervised the review activities. E. Benz, K. Trajanoska, L. Lahousse, J.D. Schoufour, G. Brusselle and F. Rivadeneira planned the analyses and E. Benz and K. Trajanoska performed the meta-analyses. E. Benz, K. Trajanoska, L. Lahousse, G. Brusselle and F. Rivadeneira wrote the first manuscript draft. E. De Roos, R. Williams and N. Terzikhan helped to critically write the first and final manuscript. All authors reviewed the study findings, and read and approved the final version before submission.
Conflict of interest: E. Benz is supported by the Netherlands Scientific Organization (NOW) and ZonMW Project number NOW/ZONMW-VIDI-016-136-367.
Conflict of interest: K. Trajanoska is supported by the Netherlands Scientific Organization (NOW) and ZonMW Project number NOW/ZONMW-VIDI-016-136-367.
Conflict of interest: L. Lahousse reports grants from AstraZeneca and Chiesi (both awards), and expert consultation for Boehringer Ingelheim GmbH and Novartis, outside the submitted work.
Conflict of interest: J.D. Schoufour is supported by the Netherlands Scientific Organization (NOW) and ZonMW Project number NOW/ZONMW-VIDI-016-136-367.
Conflict of interest: N. Terzikhan has nothing to disclose.
Conflict of interest: E. de Roos has nothing to disclose.
Conflict of interest: G.B. de Jonge has nothing to disclose.
Conflict of interest: R. Williams has nothing to disclose.
Conflict of interest: O.H. Franco has nothing to disclose.
Conflict of interest: G. Brusselle has nothing to disclose.
Conflict of interest: F. Rivadeneira is supported by the Netherlands Scientific Organization (NOW) and ZonMW Project number NOW/ZONMW-VIDI-016-136-367.
References
- 1.Celli BR, Decramer M, Wedzicha JA, et al. . An official American Thoracic Society/European Respiratory Society statement: research questions in COPD. Eur Respir Rev 2015; 24: 159–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Houben-Wilke S, Augustin IM, Vercoulen JH, et al. . COPD stands for complex obstructive pulmonary disease. Eur Respir Rev 2018; 27: 180027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J 2009; 33: 1165–1185. [DOI] [PubMed] [Google Scholar]
- 4.Jaitovich A, Barreiro E. Skeletal muscle dysfunction in chronic obstructive pulmonary disease what we know and can do for our patients. Am J Respir Crit Care Med 2018; 198: 175–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agusti A, Soriano JB. COPD as a systemic disease. COPD 2008; 5: 133–138. [DOI] [PubMed] [Google Scholar]
- 6.Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet 2017; 389: 1931–1940. [DOI] [PubMed] [Google Scholar]
- 7.Maltais F, Decramer M, Casaburi R, et al. . An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2014; 189: e15–e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buckinx F, Landi F, Cesari M, et al. . Pitfalls in the measurement of muscle mass: a need for a reference standard. J Cachexia Sarcopenia Muscle 2018; 9: 269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hwang JA, Kim YS, Leem AY, et al. . Clinical implications of sarcopenia on decreased bone density in men with COPD. Chest 2017; 151: 1018–1027. [DOI] [PubMed] [Google Scholar]
- 10.van de Bool C, Gosker HR, van den Borst B, et al. . Muscle quality is more impaired in sarcopenic patients with chronic obstructive pulmonary disease. J Am Med Dir Assoc 2016; 17: 415–420. [DOI] [PubMed] [Google Scholar]
- 11.Lee IS, Leem AY, Lee SH, et al. . Relationship between pulmonary function and bone mineral density in the Korean National Health and Nutrition Examination Survey. Korean J Intern Med 2016; 31: 899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Costa TM, Costa FM, Moreira CA, et al. . Sarcopenia in COPD: relationship with COPD severity and prognosis. J Bras Pneumol 2015; 41: 415–421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung JH, Hwang HJ, Han CH, et al. . Association between sarcopenia and metabolic syndrome in chronic obstructive pulmonary disease: the Korea National Health and Nutrition Examination Survey (KNHANES) from 2008 to 2011. COPD 2015; 12: 82–89. [DOI] [PubMed] [Google Scholar]
- 14.Koo HK, Park JH, Park HK, et al. . Conflicting role of sarcopenia and obesity in male patients with chronic obstructive pulmonary disease: Korean National Health and Nutrition Examination Survey. PLoS One 2014; 9: e110448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sergi G, Coin A, Marin S, et al. . Body composition and resting energy expenditure in elderly male patients with chronic obstructive pulmonary disease. Respir Med 2006; 100: 1918–1924. [DOI] [PubMed] [Google Scholar]
- 16.Joppa P, Tkacova R, Franssen FME, et al. . Sarcopenic obesity, functional outcomes, and systemic inflammation in patients with chronic obstructive pulmonary disease. J Am Med Dir Assoc 2016; 17: 712–718. [DOI] [PubMed] [Google Scholar]
- 17.Pothirat C, Chaiwong W, Phetsuk N, et al. . The relationship between body composition and clinical parameters in chronic obstructive pulmonary disease. J Med Assoc Thai 2016; 99: 386–393. [PubMed] [Google Scholar]
- 18.Gologanu D, Ionita D, Gartonea T, et al. . Body composition in patients with chronic obstructive pulmonary disease. Maedica (Buchar) 2014; 9: 25–32. [PMC free article] [PubMed] [Google Scholar]
- 19.Rutten EPA, Calverley PMA, Casaburi R, et al. . Changes in body composition in patients with chronic obstructive pulmonary disease: do they influence patient-related outcomes? Ann Nutr Metab 2013; 63: 239–247. [DOI] [PubMed] [Google Scholar]
- 20.Verhage TL, Heijdra Y, Molema J, et al. . Associations of muscle depletion with health status. Another gender difference in COPD? Clin Nutr 2011; 30: 332–338. [DOI] [PubMed] [Google Scholar]
- 21.van Wetering CR, van Nooten FE, Mol SJM, et al. . Systemic impairment in relation to disease burden in patients with moderate COPD eligible for a lifestyle program. Int J COPD 2008; 3: 443–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vermeeren MAP, Creutzberg EC, Schols AMWJ, et al. . Prevalence of nutritional depletion in a large out-patient population of patients with COPD. Respir Med 2006; 100: 1349–1355. [DOI] [PubMed] [Google Scholar]
- 23.Steuten LMG, Creutzberg EC, Vrijhoef HJM, et al. . COPD as a multicomponent disease: inventory of dyspnoea, underweight, obesity and fat free mass depletion in primary care. Prim Care Respir J 2006; 15: 84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vestbo J, Prescott E, Almdal T, et al. . Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med 2006; 173: 79–83. [DOI] [PubMed] [Google Scholar]
- 25.Barker BL, McKenna S, Mistry V, et al. . Systemic and pulmonary inflammation is independent of skeletal muscle changes in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 2014; 9: 975–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim SB, Kang YA, Jung JY, et al. . Body mass index and fat free mass index in obstructive lung disease in Korea. Int J Tuberc Lung Dis 2014; 18: 102–108. [DOI] [PubMed] [Google Scholar]
- 27.Andersson M, Slinde F, Grönberg AM, et al. . Physical activity level and its clinical correlates in chronic obstructive pulmonary disease: a cross-sectional study. Respir Res 2013; 14: 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Engelen MP, Schols AM, Lamers RJ, et al. . Different patterns of chronic tissue wasting among patients with chronic obstructive pulmonary disease. Clin Nutr 1999; 18: 275–280. [DOI] [PubMed] [Google Scholar]
- 29.Rutten EPA, Grydeland TB, Pillai SG, et al. . Quantitative CT: associations between emphysema, airway wall thickness and body composition in COPD. Pulm Med 2011; 2011: 419328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Celli BR, Locantore N, Tal-Singer R, et al. . Emphysema and extrapulmonary tissue loss in COPD: a multi-organ loss of tissue phenotype. Eur Respir J 2018; 51: 1702146. [DOI] [PubMed] [Google Scholar]
- 31.Spruit MA, Gosselink R, Troosters T, et al. . Muscle force during an acute exacerbation in hospitalised patients with COPD and its relationship with CXCL8 and IGF-I. Thorax 2003; 58: 752–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdulai RM, Jensen TJ, Patel NR, et al. . Deterioration of limb muscle function during acute exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2018; 197: 433–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Muscaritoli M, Anker SD, Argiles J, et al. . Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr 2010; 29: 154–159. [DOI] [PubMed] [Google Scholar]
- 34.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. . Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010; 39: 412–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fielding RA, Vellas B, Evans WJ, et al. . Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 2011; 12: 249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Studenski SA, Peters KW, Alley DE, et al. . The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 2014; 69: 547–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen LK, Liu LK, Woo J, et al. . Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 2014; 15: 95–101. [DOI] [PubMed] [Google Scholar]
- 38.Cruz-Jentoft AJ, Bahat G, Bauer J, et al. . Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019; 48: 16–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosenberg IH. Sarcopenia: origins and clinical relevance. J Nutr 1997; 127: Suppl. 5, 990S–991S. [DOI] [PubMed] [Google Scholar]
- 40.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet 2019; 393: 2636–2646. [DOI] [PubMed] [Google Scholar]
- 41.Lee LW, Lin CM, Li HC, et al. . Body composition changes in male patients with chronic obstructive pulmonary disease: aging or disease process? PLoS One 2017; 12: e0180928 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bone AE, Hepgul N, Kon S, et al. . Sarcopenia and frailty in chronic respiratory disease. Chron Respir Dis 2017; 14: 85–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marty E, Liu Y, Samuel A, et al. . A review of sarcopenia: enhancing awareness of an increasingly prevalent disease. Bone 2017; 105: 276–286. [DOI] [PubMed] [Google Scholar]
- 44.Evans RA, Morgan MDL. The systemic nature of chronic lung disease. Clin Chest Med 2014; 35: 283–293. [DOI] [PubMed] [Google Scholar]
- 45.Natanek SA, Gosker HR, Slot IGM, et al. . Heterogeneity of quadriceps muscle phenotype in chronic obstructive pulmonary disease (COPD); implications for stratified medicine? Muscle Nerve 2013; 48: 488–497. [DOI] [PubMed] [Google Scholar]
- 46.Nilwik R, Snijders T, Leenders M, et al. . The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp Gerontol 2013; 48: 492–498. [DOI] [PubMed] [Google Scholar]
- 47.Shafiee G, Keshtkar A, Soltani A, et al. . Prevalence of sarcopenia in the world: a systematic review and meta-analysis of general population studies. J Diabetes Metab Disord 2017; 16: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cruz-Jentoft AJ, Landi F, Schneider SM, et al. . Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014; 43: 748–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009; 62: e1–34. [DOI] [PubMed] [Google Scholar]
- 50.Shamseer L, Moher D, Clarke M, et al. . Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015; 350: g7647. [DOI] [PubMed] [Google Scholar]
- 51.Hoy D, Brooks P, Woolf A, et al. . Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 2012; 65: 934–939. [DOI] [PubMed] [Google Scholar]
- 52.Wells GA, Shea B, O'Connell D, et al. . The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-randomised Studies in Meta-analyses. 2014. www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Date last accessed: April 05, 2019.
- 53.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1539–1558. [DOI] [PubMed] [Google Scholar]
- 54.da Costa BR, Juni P. Systematic reviews and meta-analyses of randomized trials: principles and pitfalls. Eur Heart J 2014; 35: 3336–3345. [DOI] [PubMed] [Google Scholar]
- 55.de Blasio F, Di Gregorio A, de Blasio F, et al. . Malnutrition and sarcopenia assessment in patients with chronic obstructive pulmonary disease according to international diagnostic criteria, and evaluation of raw BIA variables. Respir Med 2018; 134: 1–5. [DOI] [PubMed] [Google Scholar]
- 56.Munhoz da Rocha Lemos Costa T, Costa FM, Jonasson TH, et al. . Body composition and sarcopenia in patients with chronic obstructive pulmonary disease. Endocrine 2018; 60: 95–102. [DOI] [PubMed] [Google Scholar]
- 57.Limpawattana P, Inthasuwan P, Putraveephong S, et al. . Sarcopenia in chronic obstructive pulmonary disease: a study of prevalence and associated factors in the Southeast Asian population. Chronic Respir Dis 2018; 15: 250–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Trajanoska K, Schoufour JD, Darweesh SKL, et al. . Sarcopenia and its clinical correlates in the general population: the Rotterdam study. J Bone Miner Res 2018; 33: 1209–1218. [DOI] [PubMed] [Google Scholar]
- 59.Byun MK, Cho EN, Chang J, et al. . Sarcopenia correlates with systemic inflammation in COPD. Int J COPD 2017; 12: 669–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lian J, Pan DZ, An XQ, et al. . Changes in body composition and associated factors for sarcopenia in patients with chronic obstructive pulmonary disease. Chinese General Practice 2017; 20: 3504–3508. [Google Scholar]
- 61.Borda MG, Celis-Preciado CA, Pérez-Zepeda MU, et al. Sarcopenia en ancianos con antecedente de EPOC/asma: resultados del estudio SABE – Bogotá [Sarcopenia in the elderly with a history of COPD/asthma: results of the SABE-Bogotá study]. Rev Esp Geriatr Gerontol 2017; 52: 313–316. [DOI] [PubMed] [Google Scholar]
- 62.Tasar PT, Sahin S, Karaman E, et al. . Prevalence and risk factors of sarcopenia in elderly nursing home residents. Eur Geriatr Med 2015; 6: 214–219. [Google Scholar]
- 63.Jones SE, Maddocks M, Kon SSC, et al. . Sarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitation. Thorax 2015; 70: 213–218. [DOI] [PubMed] [Google Scholar]
- 64.Landi F, Liperoti R, Fusco D, et al. . Sarcopenia and mortality among older nursing home residents. J Am Med Dir Assoc 2012; 13: 121–126. [DOI] [PubMed] [Google Scholar]
- 65.Al Haddad MA, John M, Hussain S, et al. . Role of the timed up and go test in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev 2016; 36: 49–55. [DOI] [PubMed] [Google Scholar]
- 66.Mesquita R, Wilke S, Smid DE, et al. . Measurement properties of the timed up & go test in patients with COPD. Chron Respir Dis 2016; 13: 344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.DePew ZS, Karpman C, Novotny PJ, et al. . Correlations between gait speed, 6-minute walk distance, physical activity, and self-efficacy in patients with severe chronic lung disease. Respir Care 2013; 58: 2113–2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ciciliot S, Rossi AC, Dyar KA, et al. . Muscle type and fiber type specificity in muscle wasting. Int J Biochem Cell Biol 2013; 45: 2191–2199. [DOI] [PubMed] [Google Scholar]
- 69.Correa-de-Araujo R, Harris-Love MO, Miljkovic I, et al. . The need for standardized assessment of muscle quality in skeletal muscle function deficit and other aging-related muscle dysfunctions: a symposium report. Front Physiol 2017; 8: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rutten EPA, Spruit MA, Wouters EFM. Critical view on diagnosing muscle wasting by single-frequency bio-electrical impedance in COPD. Respir Med 2010; 104: 91–98. [DOI] [PubMed] [Google Scholar]
- 71.Volgyi E, Tylavsky FA, Lyytikainen A, et al. . Assessing body composition with DXA and bioimpedance: effects of obesity, physical activity, and age. Obesity (Silver Spring) 2008; 16: 700–705. [DOI] [PubMed] [Google Scholar]
- 72.Shrikrishna D, Patel M, Tanner RJ, et al. . Quadriceps wasting and physical inactivity in patients with COPD. Eur Respir J 2012; 40: 1115–1122. [DOI] [PubMed] [Google Scholar]
- 73.Cederholm T, Jensen GL, Correia M, et al. . GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr 2019; 38: 1–9. [DOI] [PubMed] [Google Scholar]