Abstract
Pulmonary hypertension (PH) is a frequent and severe complication of systemic sclerosis (SSc). PH in SSc is highly heterogeneous because of the various clinical phenotypes of SSc itself and because the mechanisms of PH can vary from one patient to another. PH in SSc may be due to vasculopathy of the small pulmonary arteries (group 1; pulmonary arterial hypertension), interstitial lung disease (group 3; PH due to lung disease or chronic hypoxia) or myocardial fibrosis leading to left ventricular systolic or diastolic dysfunction (group 2; PH due to chronic left-heart disease). Pulmonary veno-occlusive disease is not uncommon in SSc and may also cause PH in some patients (group 1′). There is a high prevalence of each of these conditions in SSc and, as such, it may be difficult to determine the dominant cause of PH in a particular patient. However, careful phenotyping of PH in SSc is important as the therapy required for each of these underlying conditions is very different. In this review, we will decipher the different phenotypes of SSc-PH.
Short abstract
Pulmonary hypertension in systemic sclerosis is heterogeneous with various possible mechanisms http://ow.ly/s98X30f0lcu
Introduction
Pulmonary hypertension (PH) is a frequent and severe complication of systemic sclerosis (SSc) [1]. The prevalence of pulmonary arterial hypertension (PAH) is around 10% and, despite recent advances in the treatment armamentarium, PAH survival is still poor with a median survival time of 3 years [2]. Moreover, SSc-PAH patients are most often less responsive than patients with idiopathic PAH and have a worse prognosis, although they present with milder haemodynamic impairment [2–5]. However, recent studies have suggested that where aggressive therapy is used, a similar reduction in event rate is achievable in SSc and idiopathic PAH populations [6, 7]. The reasons why SSc-PAH patients could exhibit different behaviour than patients with other forms of PAH is still a matter of debate. However, one major cause is probably that both SSc itself and SSc-PAH in particular are very heterogeneous diseases, which is a major difference to idiopathic PAH. In other words, the clinical phenotypes of SSc-PAH and the possible overlap of other forms of PH are numerous either because the underlying systemic disease is itself variable in its clinical characteristics [8] or because the causes and mechanisms of PH can also vary from one patient to another.
SSc is a complex disease characterised by skin involvement and a variable degree of organ involvement, including both the lungs and the heart [9]. As a consequence, PH in SSc can be due to an isolated PAH affecting small pulmonary arteries (group 1 of the updated PH classification [10]). However, in the presence of an interstitial lung disease (ILD) of different severity, PH can belong to group 3 PH (due to chronic lung disease and/or hypoxia). Moreover, as myocardial fibrosis and left-ventricular dysfunction can also exist in SSc, PH can belong to group 2 PH (due to chronic left-heart disease). Furthermore, pulmonary veno-occlusive disease (PVOD) can complicate SSc and can also explain the occurrence of PH in some patients (group 1′) [11]. Lastly, primary biliary cirrhosis is not uncommon in SSc and can lead to portopulmonary PH [10]. What is quite common and rather specific in SSc is that, in a given patient, it is highly probable that several mechanisms can work together to lead to PH. For example, a given patient can present with pre-capillary PH in a context of limited ILD and diastolic dysfunction also contributing to elevation of pulmonary artery wedge pressure (PAWP) during a fluid challenge. Careful phenotyping of PH in SSc is thus very important in that it has an impact on treatment choice as different treatments and strategies are indicated for the different subgroups of patients [10]. In the review, we will decipher the different phenotypes of SSc-PH.
Epidemiology
Right-heart catheterisation is mandatory to diagnose PH as well as to help in classifying it by measuring PAWP [10]. The definition of PH is a mean pulmonary artery pressure ≥25 mmHg. PAH is diagnosed if PAWP is ≤15 mmHg and pulmonary vascular resistance is >3 Wood units (WU) in the absence of another cause of pre-capillary PH, such as chronic thromboembolic PH (CTEPH) or PH due to chronic lung disease. SSc-PAH accounts for 15–30% of large PH registries [12] and the prevalence of PAH in large cohorts of SSc patients ranges from 5 to 12% [13]. In high risk SSc patients (for example those with a diffusing capacity of the lung for carbon monoxide (DLCO) <60%, as in the DETECT study [14]), PAH prevalence is even higher (up to 19%). Data on the incidence of PAH are scarce and a French study has estimated an incidence of 0.61 PAH cases per 100 patient-years [15]. Notably, the incidence of post-capillary PH (group 2) was in the same range [12]. Moreover, in the DETECT study, the prevalence of group 2 PH was 6%, as was that of group 3 PH [14], highlighting the importance of properly phenotyping PH in patients with SSc [7, 11, 12].
Clinical phenotypes of pulmonary hypertension in systemic sclerosis
The different clinical phenotypes of SSc-PH can be explained by different clinical phenotypes of SSc itself and by different mechanisms leading to an increase in pulmonary pressures.
Clinical phenotypes of systemic sclerosis
SSc is a complex, multi-organ connective tissue disease affecting both the skin and the organs with various degrees of severity. Among the different organs, the lungs, heart, gastro-intestinal tract, kidneys, muscles and joints are the most frequently involved. SSc is usually classified by LeRoy and Medsger subset classification as “limited cutaneous SSc” and “diffuse cutaneous SSc” [16]. This classification is based purely on skin extension and is independent of organ involvement. Therefore, a patient with diffuse cutaneous SSc can present with no organ involvement at all while a patient with limited cutaneous SSc can present with organ involvement (e.g. ILD, PH or kidney involvement). However, in a population of SSc patients, organ involvement is more frequent and occurs earlier in patients with diffuse cutaneous involvement than in patients with limited cutaneous involvement [8]. The only important exception is PAH, which is as frequently found in the limited as well as in the diffuse SSc subsets [15]. Besides the frequency of organ involvement, one major reason for classifying patients according to SSc subset is that patients with diffuse cutaneous disease have a worse prognosis than patients with limited cutaneous disease. This should be kept in mind in the context of PH, as the prognosis of patients with SSc can be altered by PH but also by the subset of SSc itself as well as the various organ involvements that this can present.
Clinical phenotypes of pulmonary hypertension
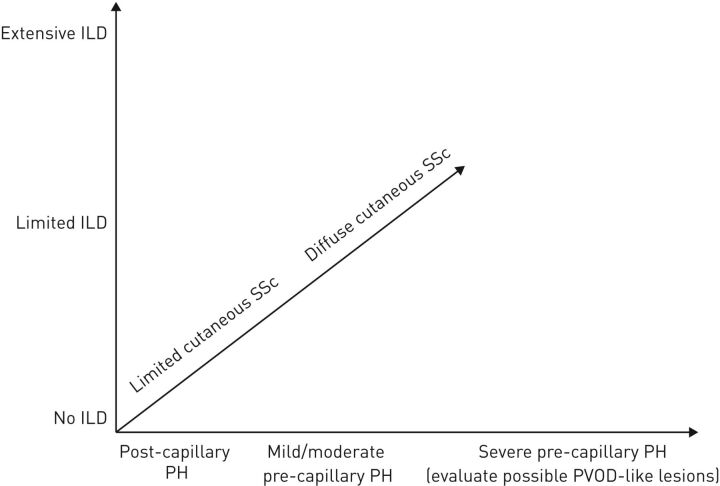
The precise phenotyping of PH in SSc remains challenging for clinicians in daily practice. We have already suggested that it can be explained by the diverse and sometimes overlapping mechanisms of PH in the setting of SSc. Indeed, SSc combines an extensive vasculopathy, inflammation, autoimmunity and fibrogenesis leading to widespread fibrosis and vascular manifestations [17]. As a consequence, PH can therefore be explained by a pulmonary arterial vasculopathy (group 1), lung fibrosis (group 3) or heart involvement (group 2) as well as by PVOD-like lesions (group 1′). However, it can be challenging to firmly distinguish the leading mechanism in a given patient while some can combine to various extents to explain the clinical presentation (figure 1).
FIGURE 1.
Clinical phenotypes of pulmonary hypertension (PH) in systemic sclerosis (SSc). PH may be heterogenous in SSc and many mechanisms can combine to produce a number of possible clinical phenotypes. A given patient can be placed somewhere on this three-axis graph with the x-axis ranging from post-capillary PH to severe pre-capillary PH, the y-axis ranging from no interstitial lung disease (ILD) to extensive ILD and the z-axis ranging from limited cutaneous SSc to diffuse cutaneous SSc. It is useful to consider possible pulmonary veno-occlusive disease (PVOD)-like conditions in patients with severe pre-capillary PH.
Interstitial lung disease
The most frequent possible confounding characteristic in SSc-PH is the presence and extension of ILD. Importantly, the presence of ILD and PH is associated with a dismal prognosis, even worse than in patients with isolated SSc-PAH [2]. In a recent meta-analysis, we showed that the pooled 3-year overall survival rate was 35% in patients with SSc-PH and ILD, as compared to 56% in SSc-PAH [2]. The prevalence of ILD in SSc ranges between 25% and 50% and is most common in the diffuse cutaneous subset [18, 19]. In SSc, ILD is usually classified as “limited ILD”, which should not be confounded with limited cutaneous SSc, or “extensive ILD” according to Goh's staging system based on high-resolution computed tomography (HRCT) of the chest as well as lung function tests [20]. Whether a SSc patient with ILD (whatever its type) and PH (whatever the haemodynamic severity) should be systematically classified in group 3 of the PH classification is not straightforward. Most authors have proposed that patients with extensive ILD and PH should be classified in group 3 [14]. By extrapolation, should patients with limited ILD all be classified in group 1, together with patients with SSc-PAH and no ILD, or should some of them be classified in group 3 when considering their haemodynamics? Alternatively, should patients with extensive ILD be classified in a single group of PH due to chronic lung disease irrespective of the haemodynamic characteristics? This is still a matter of debate; however, it is very important to try to answer this question, as PAH treatment algorithms have been built for patients without ILD [10]. Some studies have suggested that PAH-targeted therapies might improve haemodynamics but have no benefits on dyspnoea and survival and might even present an increased risk of hypoxia in SSc patients with PH and ILD [21]. This could contribute in turn to the worse results of PAH-targeted therapies in SSc-PAH patients in randomised control trials, even when patients with extensive ILD were excluded. One study suggested that survival of SSc patients with PH and ILD was modestly improved relative to historical series and, while these findings may not be generalisable, improved survival may be due partly to aggressive PAH-targeted therapy in this study [22].
Combined pulmonary fibrosis and emphysema syndrome
Combined pulmonary fibrosis and emphysema (CPFE) syndrome has recently been individualised [23]. This syndrome is characterised by the association of severe dyspnoea, paraseptal emphysema and diffuse infiltrative opacities suggestive of pulmonary fibrosis, occurring most often in smokers [23]. As a consequence spirometry is usually normal, contrasting with very severely impaired DLCO and hypoxaemia during exercise (with a major confounding effect on the forced vital capacity/DLCO ratio [24]). Interestingly, this syndrome is associated with a high risk of PH, as identified in more than 50% of patients [23, 25]. Cottin and Cordier [26] have recently described this syndrome in patients with connective tissue disease, including those with SSc. When compared to “idiopathic CPFE”, patients with comorbid connective tissue disease had a less severely impaired DLCO [26]. PH was diagnosed in 15% of patients, all of whom had SSc [26]. As lung volumes can be normal, it is possible that this syndrome is underdiagnosed in SSc. Recently, Antoniou et al. [24] showed that emphysema in patients with SSc-related ILD can also be observed in nonsmokers and smokers with a low pack-year history. The significant prevalence of emphysema in nonsmokers with SSc-related ILD provides indirect support for a pathogenetic basis for the CPFE syndrome. CPFE is an important clinical phenotype in SSc-PH as it is associated with a poor prognosis.
Pulmonary veno-occlusive disease
Idiopathic PVOD is a rare disease characterised by a diffuse obstruction of the small pulmonary veins [27–29]. Dorfmüller et al. [30] have shown that PVOD-like lesions are common in lung tissue in SSc-PH while, more recently, Günther et al. [11] have shown that 61.5% of SSc-PH patients have HRCT signs suggestive of PVOD. Moreover, the presence of these HRCT signs (lymph node enlargement, centrilobular ground-glass opacities and septal lines) is associated with worse survival rates and an increased risk of pulmonary oedema after the initiation of PAH-targeted therapies [11]. In our opinion, this difficult to diagnose PVOD-like involvement in SSc-PH patients has been overlooked, possibly due to the signs sometimes being mild or difficult to distinguish from ILD, and could play a role in the worse prognosis. It is an important phenotype to identify in SSc-PH and it should be carefully evaluated not only at baseline but also during the follow-up of patients. Clinicians have to be aware that the signs can become more obvious after the initiation of PAH-targeted therapies and should be looked at carefully in a patient who experiences an intriguing worsening after the initiation of the treatment or becomes refractory to therapy. Determining the precise prevalence of PVOD as a confounding factor is further limited by the relatively rare occurrence of pulmonary oedema in SSc when treated with prostanoids, unlike in classical descriptions of PVOD. It seems probable that the spectrum of vasculopathy present in SSc is shifted toward greater venous involvement, without necessarily leading to the overt dominance of the venous involvement seen in the typical PVOD patient.
Cardiac involvement
Cardiac involvement is very common in SSc [31] and, while it is rarely clinically obvious, myocardial fibrosis is the pathological hallmark of this complication and has been reported in 50–80% of cases in necropsy studies [32]. Recent advances in cardiac imaging, such as magnetic resonance imaging (MRI), have shown that a majority of patients have at least one abnormality on cardiac MRI [33]. We have previously shown that one third of patients have diastolic dysfunction and around 21% have myocardial delayed-contrast enhancement suggestive of myocardial fibrosis [33]. Myocardial fibrosis can lead to left-ventricular dysfunction and could either explain the development of pure post-capillary PH or contribute to a post-capillary component in SSc patients with pulmonary arteriopathy. In a recent study by Fox et al. [34], the authors assessed the prevalence of occult left-heart disease in SSc-PH. In a population of 107 patients with SSc, 53 had PH confirmed by right-heart catheterisation. Based on PAWP, 29 out of 53 had PAH and 24 had post-capillary PH. However, after fluid challenge, 11 PAH patients were reclassified as displaying occult post-capillary PH [34] although there was no follow-up data precluding any firm conclusion. Such an occult post-capillary component may explain, at least in part, the worst outcomes of SSc-associated PAH in randomised clinical trials. Moreover, this study also suggests that even if pre-capillary PH is present at rest in a SSc patient, a coexisting post-capillary component can be present due to overt or subtle diastolic left-heart dysfunction, which might be unmasked by fluid challenge or exercise testing [35]. Recently, Bourji et al. [36] showed that SSc patients with PH due to left-ventricular diastolic dysfunction had a twofold increase in the risk of death compared with SSc-PAH patients after adjusting for haemodynamics. Concomitant intrinsic pulmonary vascular disease and left-ventricular dysfunction likely contribute to very poor survival in patients with PH.
Chronic thromboembolic disease
SSc carries a higher risk of venous thromboembolic disease if antiphospholipid antibodies are present [37–39]. Therefore, a ventilation/perfusion lung scan should be performed to rule out CTEPH in the diagnosis workup of PH in SSc.
Isolated pulmonary arterial hypertension
Isolated group 1 PAH is usually presented as the most common cause of PH in SSc. However, as we have discussed, this could be only partly true as ILD, PVOD and cardiac involvement can affect virtually all SSc patients to some extent. Finding a patient solely with SSc-PAH, without any ILD, PVOD-like manifestations or diastolic dysfunction is probably not as frequent. The major problem is to determine what drives the elevation of pulmonary arterial pressure in a given patient (figure 1). As a corollary, it is also necessary to understand when ILD, PVOD-like lesions and diastolic dysfunction are sufficient to explain PH. While this issue is of utmost importance, the way to solve the question has yet to be determined.
Conclusions
PH is frequent and may be severe in SSc. The major issue is that there is not one single PH group and one single mechanism at play in SSc. Many mechanisms can overlap to explain PH in a given patient. ILD, PVOD and cardiac involvement can complicate understanding and the classification of SSc-PH and should be carefully assessed in each patient. Further studies are needed to better understand the heterogeneity of SSc-PH and better classify these patients in order to better treat them.
Disclosures
V. Sobanski V_Sobanski (1.2MB, pdf)
D. Launay D_Launay (1.2MB, pdf)
M. Humbert M_Humbert (1.2MB, pdf)
Footnotes
Conflict of interest: Disclosures can be found alongside this article at err.ersjournals.com
Provenance: Publication of this peer-reviewed article was sponsored by Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim am Rhein, Germany (principal sponsor, European Respiratory Review issue 145).
References
- 1.Le Pavec J, Launay D, Mathai SC, et al. Scleroderma lung disease. Clin Rev Allergy Immunol 2011; 40: 104–116. [DOI] [PubMed] [Google Scholar]
- 2.Lefevre G, Dauchet L, Hachulla E, et al. Survival and prognostic factors in systemic sclerosis-associated pulmonary hypertension: a systematic review and meta-analysis. Arthritis Rheum 2013; 65: 2412–2423. [DOI] [PubMed] [Google Scholar]
- 3.Clements PJ, Tan M, McLaughlin VV, et al. The pulmonary arterial hypertension quality enhancement research initiative: comparison of patients with idiopathic PAH to patients with systemic sclerosis-associated PAH. Ann Rheum Dis 2012; 71: 249–252. [DOI] [PubMed] [Google Scholar]
- 4.Sobanski V, Launay D, Hachulla E, et al. Current approaches to the treatment of systemic-sclerosis-associated pulmonary arterial hypertension (SSc-PAH). Curr Rheumatol Rep 2016; 18: 10. [DOI] [PubMed] [Google Scholar]
- 5.Shirai Y, Kuwana M. Complex pathophysiology of pulmonary hypertension associated with systemic sclerosis: potential unfavorable effects of vasodilators. J Scleroderma Relat Disord 2017; 2: 69–134. [Google Scholar]
- 6.Coghlan JG, Galie N, Barbera JA, et al. Initial combination therapy with ambrisentan and tadalafil in connective tissue disease-associated pulmonary arterial hypertension (CTD-PAH): subgroup analysis from the AMBITION trial. Ann Rheum Dis 2017; 76: 1219–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaine S, Chin K, Coghlan G,, et al. Selexipag for the treatment of connective tissue disease-associated pulmonary arterial hypertension. Eur Respir J 2017; 50: 1602493. [DOI] [PMC free article] [PubMed]
- 8.Hachulla E, Launay D. Diagnosis and classification of systemic sclerosis. Clin Rev Allergy Immunol 2011; 40: 78–83. [DOI] [PubMed] [Google Scholar]
- 9.Varga J. Systemic sclerosis: an update. Bull NYU Hosp Jt Dis 2008; 66: 198–202. [PubMed] [Google Scholar]
- 10.Galie N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2015; 46: 903–975. [DOI] [PubMed] [Google Scholar]
- 11.Günther S, Jais X, Maitre S, et al. Computed tomography findings of pulmonary veno-occlusive disease in scleroderma patients presenting with precapillary pulmonary hypertension. Arthritis Rheum 2012; 64: 2995–3005. [DOI] [PubMed] [Google Scholar]
- 12.McGoon MD, Benza RL, Escribano-Subias P, et al. Pulmonary arterial hypertension: epidemiology and registries. J Am Coll Cardiol 2013; 62: 25 Suppl, D51–D59. [DOI] [PubMed] [Google Scholar]
- 13.Avouac J, Airo P, Meune C, et al. Prevalence of pulmonary hypertension in systemic sclerosis in European Caucasians and meta-analysis of 5 studies. J Rheumatol 2010; 37: 2290–2298. [DOI] [PubMed] [Google Scholar]
- 14.Coghlan JG, Denton CP, Grunig E, et al. Evidence-based detection of pulmonary arterial hypertension in systemic sclerosis: the DETECT study. Ann Rheum Dis 2014; 73: 1340–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hachulla E, de Groote P, Gressin V, et al. The three-year incidence of pulmonary arterial hypertension associated with systemic sclerosis in a multicenter nationwide longitudinal study in France. Arthritis Rheum 2009; 60: 1831–1839. [DOI] [PubMed] [Google Scholar]
- 16.LeRoy EC, Medsger TA Jr. Criteria for the classification of early systemic sclerosis. J Rheumatol 2001; 28: 1573–1576. [PubMed] [Google Scholar]
- 17.Dumoitier N, Lofek S, Mouthon L. Pathophysiology of systemic sclerosis: state of the art in 2014. Presse Med 2014; 43: e267–e278. [DOI] [PubMed] [Google Scholar]
- 18.Launay D, Remy-Jardin M, Michon-Pasturel U, et al. High resolution computed tomography in fibrosing alveolitis associated with systemic sclerosis. J Rheumatol 2006; 33: 1789–1801. [PubMed] [Google Scholar]
- 19.Nihtyanova SI, Schreiber BE, Ong VH, et al. Prediction of pulmonary complications and long-term survival in systemic sclerosis. Arthritis Rheum 2014; 66: 1625–1635. [DOI] [PubMed] [Google Scholar]
- 20.Goh NS, Desai SR, Veeraraghavan S, et al. Interstitial lung disease in systemic sclerosis: a simple staging system. Am J Respir Crit Care Med 2008; 177: 1248–1254. [DOI] [PubMed] [Google Scholar]
- 21.Le Pavec J, Girgis RE, Lechtzin N, et al. Systemic sclerosis-related pulmonary hypertension associated with interstitial lung disease: impact of pulmonary arterial hypertension therapies. Arthritis Rheum 2011; 63: 2456–2464. [DOI] [PubMed] [Google Scholar]
- 22.Volkmann ER, Saggar R, Khanna D, et al. Improved transplant-free survival in patients with systemic sclerosis-associated pulmonary hypertension and interstitial lung disease. Arthritis Rheum 2014; 66: 1900–1908. [DOI] [PubMed] [Google Scholar]
- 23.Cottin V, Nunes H, Brillet PY, et al. Combined pulmonary fibrosis and emphysema: a distinct underrecognised entity. Eur Respir J 2005; 26: 586–593. [DOI] [PubMed] [Google Scholar]
- 24.Antoniou KM, Margaritopoulos GA, Goh NS, et al. Combined pulmonary fibrosis and emphysema in scleroderma-related lung disease has a major confounding effect on lung physiology and screening for pulmonary hypertension. Arthritis Rheum 2016; 68: 1004–1012. [DOI] [PubMed] [Google Scholar]
- 25.Cottin V, Le Pavec J, Prevot G, et al. Pulmonary hypertension in patients with combined pulmonary fibrosis and emphysema syndrome. Eur Respir J 2010; 35: 105–111. [DOI] [PubMed] [Google Scholar]
- 26.Cottin V, Cordier JF. Combined pulmonary fibrosis and emphysema in connective tissue disease. Curr Opin Pulm Med 2012; 18: 418–427. [DOI] [PubMed] [Google Scholar]
- 27.Eyries M, Montani D, Girerd B, et al. EIF2AK4 mutations cause pulmonary veno-occlusive disease, a recessive form of pulmonary hypertension. Nat Genet 2014; 46: 65–69. [DOI] [PubMed] [Google Scholar]
- 28.Montani D, Price LC, Dorfmuller P, et al. Pulmonary veno-occlusive disease. Eur Respir J 2009; 33: 189–200. [DOI] [PubMed] [Google Scholar]
- 29.Montani D, Achouh L, Dorfmuller P, et al. Pulmonary veno-occlusive disease: clinical, functional, radiologic, and hemodynamic characteristics and outcome of 24 cases confirmed by histology. Medicine (Baltimore) 2008; 87: 220–233. [DOI] [PubMed] [Google Scholar]
- 30.Dorfmüller P, Humbert M, Perros F, et al. Fibrous remodeling of the pulmonary venous system in pulmonary arterial hypertension associated with connective tissue diseases. Hum Pathol 2007; 38: 893–902. [DOI] [PubMed] [Google Scholar]
- 31.Meune C, Vignaux O, Kahan A, et al. Heart involvement in systemic sclerosis: evolving concept and diagnostic methodologies. Arch Cardiovasc Dis 2010; 103: 46–52. [DOI] [PubMed] [Google Scholar]
- 32.Follansbee WP, Miller TR, Curtiss EI, et al. A controlled clinicopathologic study of myocardial fibrosis in systemic sclerosis (scleroderma). J Rheumatol 1990; 17: 656–662. [PubMed] [Google Scholar]
- 33.Hachulla AL, Launay D, Gaxotte V, et al. Cardiac magnetic resonance imaging in systemic sclerosis: a cross-sectional observational study of 52 patients. Ann Rheum Dis 2009; 68: 1878–1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fox BD, Shimony A, Langleben D, et al. High prevalence of occult left heart disease in scleroderma-pulmonary hypertension. Eur Respir J 2013; 42: 1083–1091. [DOI] [PubMed] [Google Scholar]
- 35.D'Alto M, Romeo E, Argiento P, et al. Clinical relevance of fluid challenge in patients evaluated for pulmonary hypertension. Chest 2017; 151: 119–126. [DOI] [PubMed] [Google Scholar]
- 36.Bourji KI, Kelemen BW, Mathai SC, et al. Poor survival in patients with scleroderma and pulmonary hypertension due to heart failure with preserved ejection fraction. Pulm Circ 2017; 7: 409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schoenfeld SR, Choi HK, Sayre EC, et al. Risk of pulmonary embolism and deep venous thrombosis in systemic sclerosis: a general population-based study. Arthritis Care Res (Hoboken) 2016; 68: 246–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ungprasert P, Srivali N, Kittanamongkolchai W. Systemic sclerosis and risk of venous thromboembolism: a systematic review and meta-analysis. Mod Rheumatol 2015: 25: 893–897. [DOI] [PubMed] [Google Scholar]
- 39.Chung WS, Lin CL, Sung FC, et al. Systemic sclerosis increases the risks of deep vein thrombosis and pulmonary thromboembolism: a nationwide cohort study. Rheumatology (Oxford) 2014; 53: 1639–1645. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
V. Sobanski V_Sobanski (1.2MB, pdf)
D. Launay D_Launay (1.2MB, pdf)
M. Humbert M_Humbert (1.2MB, pdf)