Abstract
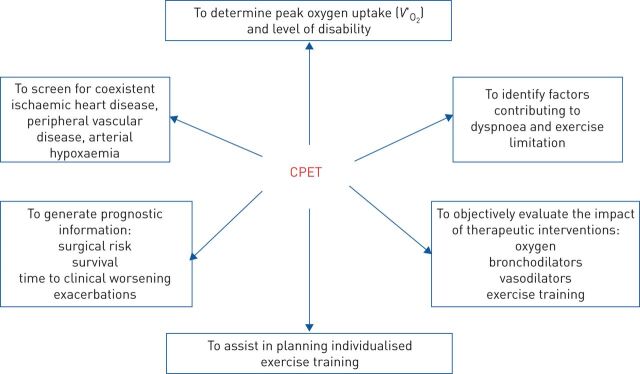
Cardiopulmonary exercise testing (CPET) has long been used as diagnostic tool for cardiac diseases. During recent years CPET has been proven to be additionally useful for 1) distinguishing between normal and abnormal responses to exercise; 2) determining peak oxygen uptake and level of disability; 3) identifying factors contributing to dyspnoea and exercise limitation; 4) differentiating between ventilatory (respiratory mechanics and pulmonary gas exchange), cardiovascular, metabolic and peripheral muscle causes of exercise intolerance; 5) identifying anomalies of ventilatory (respiratory mechanics and pulmonary gas exchange), cardiovascular and metabolic systems, as well as peripheral muscle and psychological disorders; 6) screening for coexistent ischaemic heart disease, peripheral vascular disease and arterial hypoxaemia; 7) assisting in planning individualised exercise training; 8) generating prognostic information; and 9) objectively evaluating the impact of therapeutic interventions.
As such, CPET is an essential part of patients' clinical assessment. This article belongs to the special series on the “Ventilatory efficiency and its clinical prognostic value in cardiorespiratory disorders”, addressed to clinicians, physiologists and researchers, and aims at encouraging them to get acquainted with CPET in order to help and orient the clinical decision concerning individual patients.
Short abstract
Cardiopulmonary exercise testing is an essential part of patient clinical assessment, which also includes prognosis and response to clinical interventions https://bit.ly/2EHXWL2
Introduction
Cardiopulmonary exercise testing (CPET) has long been used as diagnostic tool for cardiac diseases. During recent years CPET has become recognised as a valuable tool in unmasking the mechanisms responsible for unexplained dyspnoea as well as in the follow-up of respiratory diseases [1–5].
Nonetheless, nowadays when asked “What is the clinical value of CPET?”, the vast majority of clinicians will reply as follows: “…to determine peak oxygen uptake and the level of disability”. This is a good answer to start with, but it is incomplete (figure 1).
FIGURE 1.
Clinical utility of cardiopulmonary exercise testing (CPET); reasons for addressing a subject to CPET. V′O2: oxygen uptake.
Exercise intolerance, i.e. the result of the subject's inability to fulfil the energy needs of a particular physical task either imposed or chosen [2, 5], is a cardinal feature of many cardiorespiratory diseases. While exercise intolerance is clearly task specific, CPET typically involves exercising large (lower-extremity) muscle groups to the limit of tolerance on a cycle ergometer with a rapid-incremental (or ramp) format that imposes a smooth progressive stress over an individual's full tolerance range, with high-intensity constant work-rate tests providing a useful adjunct, particularly when assessing interventional change [1–5]. It should be noted that choosing the appropriate test appears to be crucial, as different modalities (cycle, treadmill) as well as the amount of the load increment can affect the CPET results: peak oxygen uptake (V′O2 at peak exercise) is normally independent of work-rate incrementation rate, although unusually rapid or prolonged tests can result in a lower V′O2peak because of difficulties in generating muscular forces to support the high work rates in the former, and of maintaining motivation for prolonged periods in the latter [1–5]. In contrast, the influence of V′O2 response kinetics causes peak work rate to be greater the more rapid the work-rate incrementation rate; it is therefore not a reliable surrogate for V′O2peak [1–5].
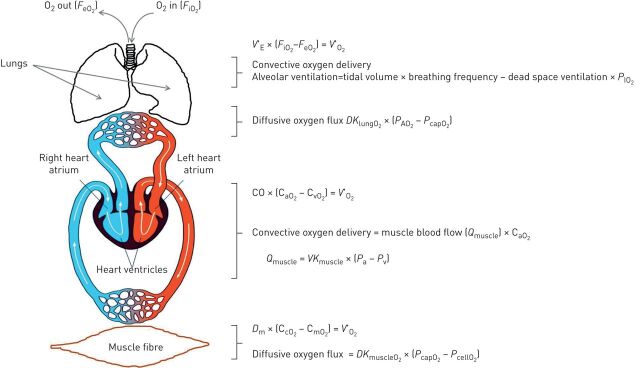
Exercise intolerance may arise from limitation or impairment at the ventilatory level (ventilatory mechanics and pulmonary gas exchange levels), cardio-circulatory level and muscle/metabolic levels, and these specific levels/loci of exercise limitation, alone or in combination, may have an impact on V′O2peak observed during CPET (figure 2) [1, 2, 5].
FIGURE 2.
Delivery of oxygen (O2) from the outside air into the muscle fibre. In this serial system, O2 delivery cannot exceed the capacity of its weakest link. A substantial increase in the function of any one “step” alone may not translate into a corresponding gain in exercise capacity (V′O2max) if the remaining steps of the pathway do not also adapt; this is ultimately how the respiratory system limits exercise tolerance in some elite, aerobically trained athletes. However, in contrast, impairment of any one single step in the O2 transport chain, occuring in heart, lung and/or peripheral vascular disease states, can seriously compromise exercise performance. The oxygen uptake (V′O2) can then be viewed as either the product of minute ventilation (V′E) and the difference between inspired and expired fractions of O2 (FiO2 – FeO2) or the product of cardiac output (CO) and the arterious–venous O2 content difference (CaO2 – CvO2) or the product of muscle diffusion (Dm) and the capillary–mitochondrial O2 content difference (CcO2 – CmO2). PIO2: inspired O2 partial pressure; DKlungO2: diffusive conductance of the lung for O2, where conductance reflects how much movement (e.g. flow) is allowed or permitted; PAO2: alveolar O2 partial pressure; PcapO2: capillary O2 partial pressure; CaO2: arterial blood O2 content (determined by pulmonary gas exchange); VKmuscle: muscle vascular conductance (conductance is the inverse of resistance), for example ↑ conductance, ↑ muscle blood flow due to dilation of resistance vessels and ↓ conductance, ↓ muscle blood flow due to constriction of resistance vessels; Pa: arterial pressure; Pv: venous pressure (the difference or gradient between arterial and venous pressure is an important determinant of skeletal muscle blood flow); DKmuscleO2: diffusive conductance of the muscle for O2; PcellO2: cell O2 partial pressure (the difference or gradient between PcellO2 and PcapO2 is an important determinant of diffusive O2 flux into the muscle, and therefore muscle metabolic and contractile function).
Most cardiorespiratory and peripheral muscle diseases present with decreased physical capacity and exercise tolerance (thus reducing V′O2), which may impact everyday life. This is particularly the case for subjects suffering from respiratory diseases that frequently give rise to symptoms during physical activity, such as dyspnoea, leg fatigue and pain [2, 5]. Dyspnoea is the most common, disabling and cumbersome symptom in cardiorespiratory disorders and it may curtail physical activity in patients with cardiopulmonary disorders [6].
Dyspnoea is often elicited by physical task or exertion (“exertional dyspnoea”) and therefore it is fundamental to understand and explore its mechanisms during exercise with a robust and reliable methodology [6]; CPET provides an excellent tool to identify factors contributing to exertional dyspnoea (unexplained or disproportionate) and exercise limitation, where comprehensive medical evaluation and appropriate additional complementary tests (e.g. resting pulmonary function, arterial blood-gas, acid–base status, haemoglobin, chest radiograph, resting ECG, echocardiography) may fail to predict response to exercise and the associated symptoms [1, 5, 6].
CPET provides the clinician with both objective and subjective information, from ventilatory, gas exchange, circulatory and muscle/metabolic variables to symptom scores. Attention should be paid to how to analyse and interpret these variables and scores. The interpretation requires the combination of CPET results with other clinical and laboratory findings [4, 7]. In addition, verbal information from the patient, including reason for stopping exercise and other sensations that may arise during CPET (e.g. feeling tense or confused, blurred vision, dizzy spells, feelings of anxiety, tingling fingers, bloated feeling in stomach, stiff fingers or arms, tight feelings around mouth, cold hands or feet, chest tightness, increased breathing effort, faster or deeper breathing, unsatisfied inspiration or inability to breathe deeply) can be useful in evaluating exercise limitation and the underpinning mechanisms of exertional dyspnoea [4, 7–9].
Rationale of CPET
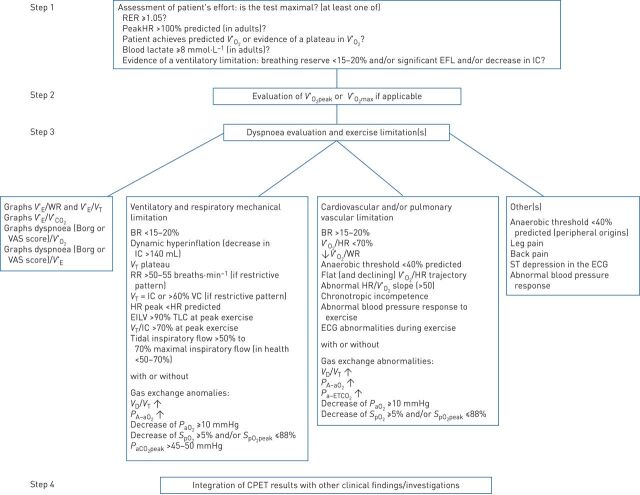
The patient's exercise limitations are investigated using an incremental exercise test [1–5, 7]; before this, it is important to verify that data are technically acceptable and whether the limit of exercise tolerance has been achieved (figure 3).
FIGURE 3.
Interpretation algorithm for cardiopulmonary exercise testing (CPET). This figure provides an outline of a CPET interpretation strategy. Importantly, the data obtained from a CPET test should not be interpreted in isolation, but rather should be integrated with other clinical findings/investigations. RER: respiratory exchange ratio; HR: heart rate; V′O2: oxygen uptake; EFL: expiratory flow limitation; IC: inspiratory capacity; V′E: minute ventilation; WR: work rate; VT: tidal volume; V′CO2: carbon dioxide output; VAS: visual analogue scale; BR: breathing reserve; RR: respiratory rate; VC: vital capacity; EILV: end-inspiratory lung volume; TLC: total lung capacity; VD: dead space volume; PA–aO2: alveolar–arterial oxygen tension difference; PaO2: arterial oxygen pressure; SpO2: pulse-oximeter oxygen saturation; PaCO2: arterial pressure of carbon dioxide; Pa–ETCO2: arterial to end-tidal carbon dioxide pressure difference.
A reduced exercise performance may be due to a single factor, or, most of the time, to the combination of multiple factors such as musculoskeletal, ventilatory, cardiovascular, gas exchange or other anomalies or simply due to deconditioning (sedentarism, for example) or obesity. It is fundamental to differentiate these anomalies from suboptimal effort that can also result in a “false” reduced exercise performance. The definition of V′O2max is not straightforward and V′O2max is often difficult to reach in sedentary or diseased population. Nonetheless V′O2max can be defined as the V′O2 reaching a value beyond which no further (or trivially small) increases in V′O2 occur despite further increases in work rate; this definition calls for a “plateau concept” that is not often attained in a sedentary or diseased population, nor well interpreted or understood by clinicians. That is the reason why it is preferable to refer to V′O2peak rather than V′O2max; a simple definition of “V′O2 plateau” is to consider an increase in V′O2 <2.0 mL·kg−1·min−1 despite an increase in work rate of 5–10% or an increase in V′O2 <150 mL·min−1 during the last work rate compared with the immediately previous one [1–5, 7].
Importantly, it should be kept in mind that there is no gold standard for defining a maximal effort. Criteria to delineate a peak effort are as follows.
A plateau in V′O2 is observed.
Peak exercise minute ventilation (V′Epeak) exceeds 80–85% of directly measured or estimated maximum voluntary ventilation (MVV). Various methods are used to estimate MVV, including forced expiratory volume in 1 s (FEV1)×35, FEV1×40 or disease- or ethnicity-specific equations. Since most laboratories use the equation FEV1×40 to estimate MVV, this equation seems to be appropriate.
More recently, evidence of a ventilatory limitation has been pointed out by the development of significant expiratory flow limitation (EFL; see later) and/or decrease in inspiratory capacity (IC) >140 mL during exercise indicating dynamic lung hyperinflation.
Respiratory exchange ratio at peak of exercise >1.05 would indicate a maximal test across all ages.
The patient achieves a heart rate (HR) at or above calculated HRmax.
V′O2peak exceeds V′O2peak predicted.
Maximum blood lactate ≥8 mmol·L−1 and/or fall in pH of ≥0.04 during the immediate recovery phase.
Ratings of dyspnoea or leg discomfort on a Borg scale indicating 8−10 units or visual analogue scale scale indicating 8−10 cm or even a high score on a similar perceived exertion scale are often used as subjective indicators of peak effort.
Exploring factors explaining exercise limitation: key variables and their interpretation
Figure 3 provides a reporting algorithm for defining a maximal test and starting to delineate the reason(s) for exercise limitation in those in whom an abnormal exercise response is noted [1–5, 7]. The classical criterion for defining exercise intolerance and classifying degrees of impairment is V′O2peak standardised by body mass. Values <40% predicted indicate severe impairment.
Two variables are used to detect exercise intolerance: 1) V′O2peak, which can be compared to normal values, but has the disadvantage of being dependent on subject's motivation as well as their physiological capacity; and 2) the anaerobic threshold (AT), which defines the point at which lactate production exceeds lactate elimination, meaning that above this point exercise cannot be sustained without reliance on anaerobic energy sources. The advantage of AT is that it is effort-independent, but unfortunately its accurate detection depends on specific pattern recognition and experience.
Cardiovascular limitation to exercise is complex and may be defined by certain interrelated variables (figure 3), such as a reduced V′O2 peak, a reduced slope or late plateau of the V′O2 trajectory (i.e. a reduced V′O2/work-rate relationship ≤8), a premature anaerobic threshold (AT <40% pred) or plateau (early or late during exercise) of the oxygen pulse (V′O2/HR ratio), or an abnormal HR/V′O2 slope (>50) may be typical [5, 7].
Pulmonary vascular limitation to exercise is not easy to define and may rely on evidence of increased V′E to carbon dioxide output (V′CO2) slope and ratio at AT in addition to the aforementioned anomalies [10, 11]. Other typical features of pulmonary vascular disease are low levels of end-tidal carbon dioxide pressure (PETCO2) at AT, a physiological dead space (dead space volume (VD)/tidal volume (VT)) which remains stable or increases or fails to decrease from baseline, an arterial carbon dioxide pressure to PETCO2 difference which fails to became negative during exercise and, sometimes, an alveolar to arterial oxygen pressure difference (PA–aO2) which widens on exertion [10, 11] (figure 3). Associated low levels of haemoglobin will enhance oxygen flow deficiency. Ischaemic heart disease or cardiomyopathy may present with electrocardiographic or blood pressure anomalies during CPET [5, 7].
Pulmonary gas exchange limitation to exercise is not straightforward either, and may rely on evidence of inefficient carbon dioxide exchange which can be signalled by high VD/VT and often by high exercise V′E/V′CO2 (figure 3) or (alone or in combination with) inadequate oxygen exchange signalled by low partial pressure of oxygen (PaO2) or, less directly, by desaturation at pulse oximetry [5, 7] and a reduced V′O2peak.
Peripheral muscle limitation to exercise (myopathies and/or deconditioning) can be difficult to detect and some variables may help define it: a reduced V′O2peak, a reduced slope or late plateau of the V′O2 trajectory (i.e. a reduced V′O2/work-rate relationship ≤8), a premature AT <40% pred, and anomalies in blood lactate at peak or during the immediate recovery phase; for example, serum lactate may fail to rise with an undetectable AT in metabolic myopathies such as McArdle disease, while relatively higher serum lactate levels matched for the work rates or the V′O2 could indicate the presence of deconditioning. Ratings of leg discomfort on a Borg scale greater than dyspnoea score at the end of exercise may also be present in a patient limited by locomotor muscle anomalies.
Ventilatory limitation to exercise can also be detected during CPET (figure 3). Beside the well-known breathing reserve, i.e. the comparison of peak V′E to MVV, other indicators of ventilatory limitation to exercise can be appreciated: constraints on dynamic VT expansion relative to resting or dynamic decrease in IC is used to appreciate a critical reduction in inspiratory reserve volume [12–17] (figure 3). More recently, ventilatory limitation has been suggested to occur in the presence of important EFL >25% at peak exercise [1, 2, 18, 19], and some other indicators of mechanical ventilatory limitations to exercise such as end-inspiratory lung volume >90% total lung capacity alone or in combination with VT/IC >70% at peak exercise (figure 3).
Graphic and tabular representations of CPET variables
Graphical representations of CPET variables are crucial; peak V′O2 in an incremental CPET has well-defined normal values; the ventilatory threshold has the advantage of being an effort-independent measure of exercise tolerance. Beside this, the entirety of exercise response (rest to peak exercise and recovery, with data reflecting interval-averaged data of 10–20 s rather than breath-by-breath data, so that “noise” is minimised) should be displayed, not only peak values; it should be highlighted here that an interval average of 30 s may be excessive, as it may underestimate peak values or overestimate AT values. This data display is important for discriminating what is normal from what appears to be abnormal in the exercise response [4, 7]: patterns of ventilatory and gas exchange responses to CPET can be discerned that define specific pathophysiological entities; it can be determined whether exercise is limited by cardiovascular, muscle-metabolic, gas exchange or ventilatory limitation (or a combination of these); additional manoeuvres can be added to the test to clarify pathophysiology, e.g. IC manoeuvres to assess dynamic hyperinflation; some assessments require arterial blood sampling to allow normality or abnormality of VD/VT to be predicted with confidence. Last, but not least, the use of appropriate normal reference values for the CPET variables is crucial.
It goes without saying that the appropriateness or inappropriateness of the response of each variable, compared with the corresponding reference value, is fundamental for discriminating normality or abnormality of exercise response and exploring mechanisms of exertional dyspnoea and exercise limitation. “Discriminating a magnitude or pattern of deviation from the normal response (of the age-, gender- and activity-matched standard subject) and matching the magnitude or pattern of abnormality with that characteristic of particular impairments of physiological system function” is the basis of CPET interpretation [20].
Further clinical applications of CPET
CPET is widely used to objectively evaluate the impact of therapeutic interventions, such as oxygen, bronchodilators, vasodilators, exercise training and others in a wide range of chronic lung and heart diseases characterised by exercise intolerance and dyspnoea [4, 6], such as COPD, interstitial lung disease (ILD), cystic fibrosis (CF), chronic heart failure (CHF) and pulmonary hypertension (PH). In patients with COPD, CPET is increasingly used to evaluate the effects of pharmacological and nonpharmacological interventions aimed at reducing exertional dyspnoea and at improving exercise capacity [3, 6]. Interventions such as bronchodilators and rehabilitation programmes can ameliorate lung mechanics and/or reduce exercise ventilatory demand through a decrease in dynamic lung hyperinflation, an improvement of breathing pattern or an increase in skeletal muscle aerobic capacity [3, 6]. In recent decades, numerous studies have investigated the use of several supplements, including anabolic and growth hormones and nutritional supplements [21–24] as part of nonpharmacological interventions, highlighting their role as adjuncts to possibly enhance the positive effects of exercise training in patients with chronic respiratory disease. Nonetheless, further and longer-term studies are necessary before making a decision on administering these therapies.
All these intervention-related ameliorations occur in the absence of significant effect on FEV1 or other resting pulmonary or cardiac function measurements that define risk stratification of lung and heart disease severity [3, 6].
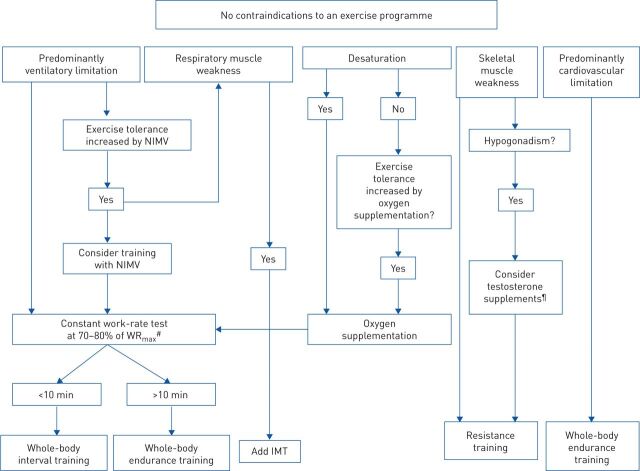
CPET has been proven useful to screen for coexistent ischaemic heart disease, peripheral vascular disease and arterial hypoxaemia [3–6] and to assist in planning individualised exercise training (figure 4). This is a major issue in this field, because CPET can:
Define contraindications to an exercise programme. In the elderly rehabilitation population, comorbidities are common. Cardiac disease is particularly prevalent. An exercise ECG evaluation, complemented by simultaneous gas exchange measurements provides important information as to the safety of an exercise training programme. Cardiac ischaemia, arrhythmias and abnormal blood pressure responses are often present and cannot be predicted from resting measurements.
Determine the need for oxygen supplementation. Oxygen supplementation during exercise improves exercise tolerance and prevents hypoxaemia. The oxygen dose (nasal cannula litre flow) necessary to prevent hypoxaemia cannot be predicted from resting measurements. Exercise desaturation is less likely to occur if the exercise involves cycling rather than walking. Treadmill exercise testing is especially useful to assess need for supplemental oxygen if the exercise training programme involves walking tasks.
Provide an exercise prescription. High-intensity exercise training provides superior physiological training benefits as compared to low-intensity training [25]. An incremental CPET can provide an initial exercise intensity target, measured either as a work-rate target or a heart-rate target.
Measure improvement in exercise tolerance. Constant work-rate exercise testing can provide a sensitive measure of exercise tolerance improvement. However, a necessary prerequisite is that a work rate be individually designed to yield a pre-intervention exercise duration in the range of ∼3–6 min. This can generally be obtained by assigning a work rate equal to ∼70–80% of the peak work rate in a preceding incremental exercise test, although work-rate adjustment may be necessary to obtain an exercise duration in the desired range (figure 4) [1].
FIGURE 4.
Empirical algorithm to help the clinician to prescribe individualised exercise therapy. Based on the exercise limitation of the patient from an incremental exercise test and further clinical findings, different training strategies or combinations can be prescribed. Typical cut-offs are 1) respiratory muscle weakness: maximal inspiratory mouth pressure <60% predicted; 2) hypogonadism: total serum testosterone <400 ng·dL−1; and 3) desaturation: saturation upon exercise <85%. NIMV: noninvasive mechanical ventilation; IMT: inspiratory muscle training; WRmax: peak work rate. #: an exercise performed at 70–80% of the peak work rate from the incremental test; ¶: based on Casaburi et al. [23] and Lewis et al. [24].
Additionally, CPET variables have proven useful in the prognostic assessment of patients with pulmonary and cardiac diseases (e.g. COPD, CF, ILD, CHF and PH) in terms of surgical risk, survival, time to clinical worsening and exacerbations [1]. Table 1 sums up the most useful CPET-derived variables regarded as being good predictors of prognosis in cardiovascular and pulmonary disease patients.
TABLE 1.
Exercise-related indices considered as predictors of prognosis in patients with cardiac and chronic respiratory disorders
| PVD | CHF | ILD | CF | COPD | |
| V′O2peak | + | + | + | + | + |
| Inspiratory capacity | + | ++ | |||
| V′E/V′CO2 | ++ | ++ | ++ | ++ | |
| PaO2-slope (ΔPaO2/ΔV′O2) | + | + | |||
| Arterial desaturation | + | ++ | + | + |
PVD: pulmonary vascular disease; CHF: chronic heart failure; ILD: interstitial lung disease; CF: cystic fibrosis; V′O2peak: oxygen uptake at peak exercise; V′E/V′CO2: ventilatory equivalent for carbon dioxide; PaO2: arterial oxygen partial pressure; +: sensitive; ++: more sensitive.
Despite the relevant advances outlined in this article and in this series, we accept that CPET remains largely unrecognised and, therefore, not used as much as it should be in respiratory medicine. Part of the problem may reside in 1) the lack of standardisation of CPET procedure and protocols, only recently highlighted [7]; 2) the requirement (sometimes the expertise) for excellent knowledge of the integrative mechanisms of physiological adaptations to exercise for correctly interpreting CPET data; 3) lack of access to CPET equipment; and 4) CPET being proposed as a diagnostic tool. These factors have limited the application and the spread of CPET in the past and, unfortunately, may still limit its application and reach in the future.
Clinical perspectives on the utility of CPET
One thing is clear: CPET, in particular, rarely influences diagnosis in patients with pulmonary or cardiac disease, as in most cases the patient to be evaluated has already a primary diagnosis [7]. The utility of CPET in such patients can be: 1) to provide an objective measure of exercise tolerance; 2) to provide information on the locus/loci of exercise limitation; 3) to shed lights upon the potential mechanism(s) contributing to exertional dyspnoea (unexplained or disproportionate); 4) to generate prognostic indices; and 5) to discern patterns of disease progression and the response to a chosen intervention. Importantly, CPET should be viewed as an essential adjunct to a previous thorough medical evaluation comprising medical history, physical examination and appropriate additional complementary exams if needed, such as resting pulmonary and cardiac function, arterial blood-gas, acid–base status, haemoglobin, chest radiograph, and so on [1, 5]. This is in line with the observation that CPET-derived physiological indices have been shown to provide valuable information on functional status and clinical outcomes such as the response to therapeutic interventions and prognosis that are barely addressed by functional measurements at rest such as resting cardiac or pulmonary function tests [4–7].
This article is addressed to clinicians, physiologists and researchers and aims at encouraging them to get acquainted with CPET in order to help and orient clinical decisions concerning individual patients. But this requires a lot of energy, physically and mentally, especially in this era in which each one of us has less time to be devoted to clinical physiology and no sufficient time to teach, learn and explain how to realise and interpret CPET results in a coherent fashion; because as both clinicians and physiologists of the modern era, we are all swamped with our hectic daily work and some other higher priorities. What is the real consequence of this? Alas, only a handful of pulmonologists and clinical physiologists know and perfectly handle CPET, which is becoming available only in specialised centres. What is the solution to this disappointing situation? We urge the recruitment and involvement of younger generations of pulmonologists and clinical physiologists with passion and dedication.
Conclusion
CPET has been proven to be useful for 1) distinguishing between normal and abnormal responses to exercise; 2) determining peak V′O2 and level of disability; 3) identifying factors contributing to dyspnoea and exercise limitation; 4) differentiating between ventilatory (respiratory mechanics and pulmonary gas exchange), cardiovascular, metabolic and peripheral muscle causes of exercise intolerance; 5) identifying anomalies of ventilatory (respiratory mechanics and pulmonary gas exchange), cardiovascular and metabolic systems, as well as peripheral muscle and psychological disorders; 6) screening for coexistent ischaemic heart disease, peripheral vascular disease and arterial hypoxaemia; 7) assisting in planning individualised exercise training; 8) generating prognostic information; and 9) objectively evaluating the impact of therapeutic interventions.
As such, CPET is an essential part of patients’ clinical assessment, which also includes prognosis and response to clinical interventions.
Footnotes
Provenance: commissioned article, peer reviewed.
Number 1 in the Series “Ventilatory efficiency and its clinical prognostic value in cardiorespiratory disorders” Edited by Pierantonio Laveneziana and Paolo Palange
Conflict of interest: P. Laveneziana reports personal fees from Boehringer France, Novartis France and Chiesi France, outside the submitted work.
Conflict of interest: M. Di Paolo has nothing to disclose.
Conflict of interest: P. Palange has nothing to disclose.
References
- 1.Puente-Maestu L, Palange P, Casaburi R, et al. . Use of exercise testing in the evaluation of interventional efficacy: an official ERS statement. Eur Respir J 2016; 47: 429–460. doi: 10.1183/13993003.00745-2015 [DOI] [PubMed] [Google Scholar]
- 2.ERS Task Force, Palange P, Ward SA, et al. . Recommendations on the use of exercise testing in clinical practice. Eur Respir J 2007; 29: 185–209. doi: 10.1183/09031936.00046906 [DOI] [PubMed] [Google Scholar]
- 3.American Thoracic Society/American College of Chest Physicians. ATS/ACCP statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 2003; 167: 211–277. doi: 10.1164/rccm.167.2.211 [DOI] [PubMed] [Google Scholar]
- 4.ERS Task Force on Standardization of Clinical Exercise Testing. Clinical exercise testing with reference to lung diseases: indications, standardization and interpretation strategies. Eur Respir J 1997; 10: 2662–2689. doi: 10.1183/09031936.97.10112662 [DOI] [PubMed] [Google Scholar]
- 5.Palange P, Laveneziana P, Neder JA, et al. . Clinical Exercise Testing (ERS Monograph). Sheffield, European Respiratory Society, 2018. [Google Scholar]
- 6.Laviolette L, Laveneziana P. Dyspnoea: a multidimensional and multidisciplinary approach. Eur Respir J 2014; 43: 1750–1762. doi: 10.1183/09031936.00092613 [DOI] [PubMed] [Google Scholar]
- 7.Radtke T, Crook S, Kaltsakas G, et al. . ERS statement on standardisation of cardiopulmonary exercise testing in chronic lung diseases. Eur Respir Rev 2019; 28: 180101. doi: 10.1183/16000617.0101-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dubé BP, Vermeulen F, Laveneziana P. Exertional dyspnoea in chronic respiratory diseases: from physiology to clinical application. Arch Bronconeumol 2017; 53: 62–70. [DOI] [PubMed] [Google Scholar]
- 9.Laveneziana P, Agostoni P. Exertional dyspnoea in cardiorespiratory disorders: the clinical use of cardiopulmonary exercise testing. Eur Respir Rev 2016; 25: 227–229. doi: 10.1183/16000617.0044-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weatherald J, Boucly A, Montani D, et al. . Gas exchange and ventilatory efficiency during exercise in pulmonary vascular diseases. Arch Bronconeumol 2020; 56: 578–585. 10.1016/j.arbres.2019.12.030. [DOI] [PubMed] [Google Scholar]
- 11.Weatherald J, Sattler C, Garcia G, et al. . Ventilatory response to exercise in cardiopulmonary disease: the role of chemosensitivity and dead space. Eur Respir J 2018; 51: 1700860. doi: 10.1183/13993003.00860-2017 [DOI] [PubMed] [Google Scholar]
- 12.Laveneziana P, Albuquerque A, Aliverti A, et al. . ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J 2019; 53: 1801214. doi: 10.1183/13993003.01214-2018 [DOI] [PubMed] [Google Scholar]
- 13.Laveneziana P, Bruni GI, Presi I, et al. . Tidal volume inflection and its sensory consequences during exercise in patients with stable asthma. Respir Physiol Neurobiol 2013; 185: 374–379. doi: 10.1016/j.resp.2012.08.026 [DOI] [PubMed] [Google Scholar]
- 14.Laveneziana P, Garcia G, Joureau B, et al. . Dynamic respiratory mechanics and exertional dyspnoea in pulmonary arterial hypertension. Eur Respir J 2013; 41: 578–587. doi: 10.1183/09031936.00223611 [DOI] [PubMed] [Google Scholar]
- 15.Laveneziana P, Humbert M, Godinas L, et al. . Inspiratory muscle function, dynamic hyperinflation and exertional dyspnoea in pulmonary arterial hypertension. Eur Respir J 2015; 45: 1495–1498. doi: 10.1183/09031936.00153214 [DOI] [PubMed] [Google Scholar]
- 16.Laveneziana P, Webb KA, Ora J, et al. . Evolution of dyspnea during exercise in chronic obstructive pulmonary disease: impact of critical volume constraints. Am J Respir Crit Care Med 2011; 184: 1367–1373. doi: 10.1164/rccm.201106-1128OC [DOI] [PubMed] [Google Scholar]
- 17.Laveneziana P, Webb KA, Wadell K, et al. . Does expiratory muscle activity influence dynamic hyperinflation and exertional dyspnea in COPD? Respir Physiol Neurobiol 2014; 199: 24–33. doi: 10.1016/j.resp.2014.04.005 [DOI] [PubMed] [Google Scholar]
- 18.Huckstepp RTR, Cardoza KP, Henderson LE, et al. . Distinct parafacial regions in control of breathing in adult rats. PLoS One 2018; 13: e0201485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johnson BD, Weisman IM, Zeballos RJ, et al. . Emerging concepts in the evaluation of ventilatory limitation during exercise: the exercise tidal flow-volume loop. Chest 1999; 116: 488–503. doi: 10.1378/chest.116.2.488 [DOI] [PubMed] [Google Scholar]
- 20.Whipp BJ. Exercise physiology. In: Laurent GJ, Shapiro SD, eds. Encyclopedia of Respiratory Medicine. Boston, Academic Press, 2006; pp. 146–157. [Google Scholar]
- 21.Lewis MI, Horvitz GD, Clemmons DR, et al. . Role of IGF-I and IGF-binding proteins within diaphragm muscle in modulating the effects of nandrolone. Am J Physiol Endocrinol Metab 2002; 282: E483–E490. doi: 10.1152/ajpendo.00191.2001 [DOI] [PubMed] [Google Scholar]
- 22.Urban RJ, Bodenburg YH, Gilkison C, et al. . Testosterone administration to elderly men increases skeletal muscle strength and protein synthesis. Am J Physiol 1995; 269: E820–E826. [DOI] [PubMed] [Google Scholar]
- 23.Casaburi R, Bhasin S, Cosentino L, et al. . Effects of testosterone and resistance training in men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004; 170: 870–878. doi: 10.1164/rccm.200305-617OC [DOI] [PubMed] [Google Scholar]
- 24.Lewis MI, Fournier M, Storer TW, et al. . Skeletal muscle adaptations to testosterone and resistance training in men with COPD. J Appl Physiol 2007; 103: 1299–1310. doi: 10.1152/japplphysiol.00150.2007 [DOI] [PubMed] [Google Scholar]
- 25.Casaburi R, Patessio A, Ioli F, et al. . Reductions in exercise lactic acidosis and ventilation as a result of exercise training in patients with obstructive lung disease. Am Rev Respir Dis 1991; 143: 9–18. doi: 10.1164/ajrccm/143.1.9 [DOI] [PubMed] [Google Scholar]