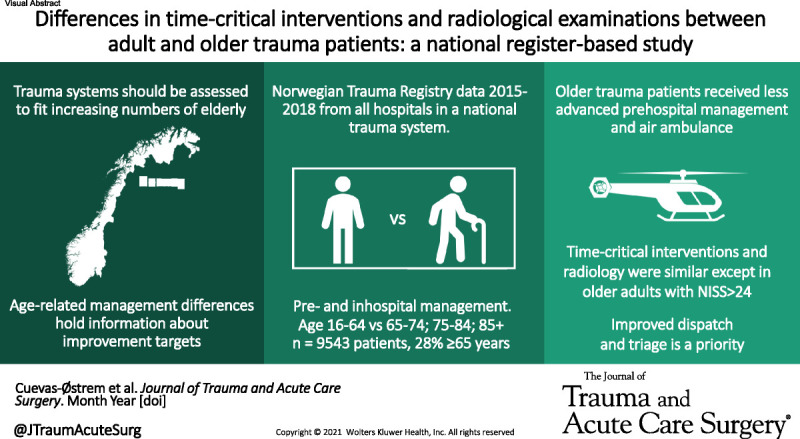
Older trauma patients were less likely to receive advanced prehospital management and air ambulance conveyance, compared to younger adults. The rates of time-critical interventions and radiological examinations were lower only among very severely injured older adults (NISS>24)
KEY WORDS: Trauma, elderly, geriatric, clinical management, prehospital
BACKGROUND
Older trauma patients are reported to receive lower levels of care than younger adults. Differences in clinical management between adult and older trauma patients hold important information about potential trauma system improvement targets. The aim of this study was to compare prehospital and early in-hospital management of adult and older trauma patients, focusing on time-critical interventions and radiological examinations.
METHODS
Retrospective analysis of the Norwegian Trauma Registry for 2015 through 2018. Trauma patients 16 years or older met by a trauma team and with New Injury Severity Score of 9 or greater were included, dichotomized into age groups 16 years to 64 years and 65 years or older. Prehospital and emergency department clinical management, advanced airway management, chest decompression, and admission radiological examinations was compared between groups applying descriptive statistics and appropriate statistical tests.
RESULTS
There were 9543 patients included, of which 28% (n = 2711) were 65 years or older. Older patients, irrespective of injury severity, were less likely attended by a prehospital doctor/paramedic team (odds ratio [OR], 0.64; 95% confidence interval [CI], 0.57–0.71), conveyed by air ambulance (OR, 0.65; 95% CI, 0.58–0.73), and transported directly to a trauma center (OR, 0.86; 95% CI, 0.79–0.94). Time-critical intervention and primary survey radiological examination rates only differed between age groups among patients with New Injury Severity Score of 25 or greater, showing lower rates for older adults (advanced airway management: OR, 0.60; 95% CI, 0.47–0.76; chest decompression: OR, 0.46; 95% CI, 0.25–0.85; x-ray chest: OR, 0.54; 95% CI, 0.39–0.75; x-ray pelvis: OR, 0.69; 95% CI, 0.57–0.84). However, for the patients attended by a doctor/paramedic team, there were no management differences between age groups.
CONCLUSION
Older trauma patients were less likely to receive advanced prehospital care compared with younger adults. Older patients with very severe injuries received fewer time-critical interventions and radiological examinations. Improved dispatch of doctor/paramedic teams to older adults and assessment of the impact the observed differences have on outcome are future research priorities.
LEVEL OF EVIDENCE
Therapeutic/Care Management; Level III.
The burden of geriatric trauma is expected to increase in correlation with aging populations.1,2 Compared with younger adults, older people have a two to four times higher risk of death and are more likely to experience reduced functional outcome after severe injury.3–6 Studies investigating differences in clinical management between age groups have found that older trauma patients receive lower levels of care;5,7 however, detailed descriptions of prehospital and early in-hospital management with a particular focus on time-critical interventions and radiological examinations are lacking. Exposing management variation in the early phases of trauma care is important for trauma system evaluation and can possibly identify improvement targets.
Airway management and chest decompression (CD) are essential time-critical interventions in trauma management.8–10 Both interventions are routinely registered in the Norwegian Trauma Registry (NTR)11 and can be performed basic or advanced reflecting the skills and training of the deployed resources. Chest and pelvic x-rays are part of the primary survey according to the Norwegian adaptation of the Advanced Trauma Life Support (ATLS) guidelines.10 Chest x-ray is one of the earliest checkpoints in the primary survey, serving as a marker of the acuity of care given.10
Previous studies have shown that older adults benefit from improvement of existing trauma system practices.12 Differences in clinical management in disfavor of older patients must be given attention as a possible trauma system improvement opportunity. The aim of this study was to compare prehospital and in-hospital clinical management of adult and older trauma patients, focusing on time-critical interventions and radiological examinations.
MATERIALS AND METHODS
Study Design and Setting
This study conforms with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines and a complete checklist has been uploaded as Supplemental Digital Content (Supplementary Material 1, http://links.lww.com/TA/C347).13 In line with the protocol for the study,14 we performed a retrospective cohort study of all trauma cases in Norway meeting inclusion criteria, between January 1, 2015, and December 31, 2018. Data were extracted from the NTR.
Norway has a population of 5.4 million people, of which approximately 16.5% are 65 years or older.15 The health care system is publicly funded, and a nationwide inclusive trauma system is implemented, describing national field triage criteria (Fig. 1) and uniform requirements to all prehospital services and hospitals.16 Clinical management of severely injured patients in Norway follow an adaptation of the Prehospital Trauma Life Support and ATLS guidelines incorporated in the national trauma plan.16 Trauma patients are managed in trauma centers (TCs) or acute care trauma hospitals (ACTHs) equivalent to American College of Surgeons Committee on Trauma Level I or Level II and Level III TC, respectively.17 All ACTH and TC have 24/7 trauma team availability led by an ATLS educated experienced resident or a surgical consultant. Calls made to the national medical emergency number (113) are evaluated by specially trained emergency medical dispatch center (EMDC) personnel using the “Norwegian Index for Medical Emergencies” (Index), a criteria-based system for dispatch of emergency medical service resources.18 The national trauma field triage criteria are incorporated in the injury chapters. The EMDC operator controls ground ambulance dispatch. Ground ambulances are mainly staffed by emergency medical technicians, paramedics, or nurses. Doctor/paramedic teams are available in a nationwide network. These are manned by an anesthesiologist and a rescue paramedic/nurse, which deploy by helicopter or rapid response cars. No national criteria for doctor/paramedic team dispatch exists.19,20 In all Index chapters, doctor/paramedic team dispatch is suggested for conditions qualifying for the most urgent response. The EMDC operator must recognize a possible need for advanced prehospital care or air transport and involve the on-call prehospital physician.20 All emergency medical services deliver basic interventions (simple airway maneuvers and pharyngeal airways, needle CD), while advanced interventions (advanced airway management [AAM]: supraglottic airway devices, endotracheal intubation/prehospital anesthesia and surgical airway, and chest thoracostomy) are reserved doctor/paramedic teams.
Figure 1.
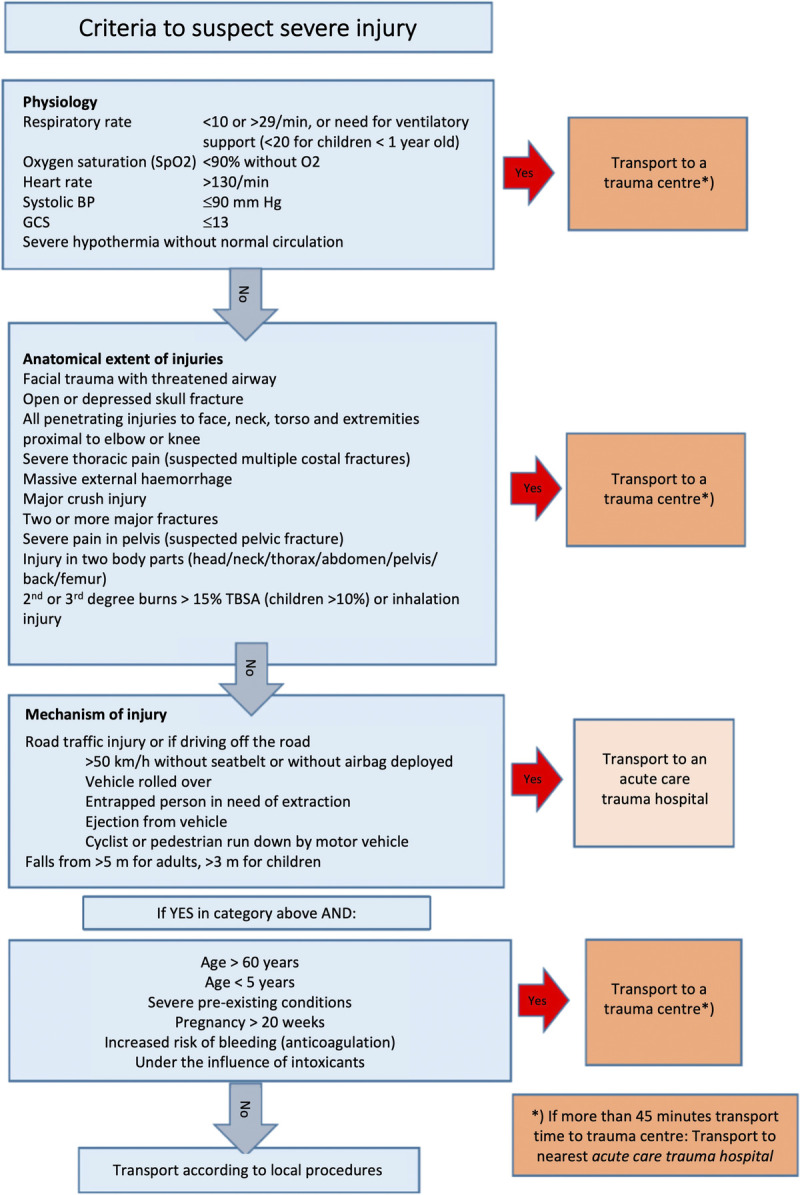
National criteria for field triage of injured people in Norway.
Selection of Participants
In the study period, four TC and 34 ACTH delivered data to the NTR. The NTR holds information about patients who meet the following inclusion criteria: Admitted through trauma team activation (TTA), admitted without TTA but found to have penetrating injuries to head, neck, torso, or extremities proximal to knee or elbow, head injury with Abbreviated Injury Scale (AIS) score of 3 or higher, or New Injury Severity Score (NISS) greater than 12.21 Of patients received by a trauma team, a high coverage is achieved (>95%).21
A total of 33,344 patients were registered in the NTR between 2015 and 2019. Only patients met by a trauma team that were 16 years or older and with NISS ≥9 were included. Patients with missing information about age or AIS or with injuries from drowning, inhalation, hypothermia, and asphyxia without concomitant trauma were excluded (Supplemental Digital Content, Supplementary Fig. 1, http://links.lww.com/TA/C348).
Data Collection and Management
Data collection is based on the Utstein template and includes data from all parts of the treatment chain, from accident site to rehabilitation.11 The NTR's status as a national quality registry has warranted mandatory data delivery since 2006, regulated by law since 2019.22 All patients are registered with a waiver of consent. Injuries are coded according to the AIS manual 2005 version, update 200823 by certified nurse registrars. The AIS and NISS measure injury severity.24
The study population was dichotomized by age into “group 1” (G1) aged 16 years to 64 years and “group 2” (G2) 65 years and older. Prespecified subcategories were defined as age intervals 65 years to 74 years, 75 years to 84 years, and 85 years or older.14 According to the AIS severity description, NISS was grouped into intervals 9 to 14, 15 to 24, and 25 or higher.23 For patients with multiple injuries in the same body region, only the most severe was included in analyses concerning body regions with severe injuries (AIS score, ≥ 3). Glasgow Coma Scale (GCS) was categorized according to Head Injury Severity Scale (HISS).25 Preinjury physical status was defined by the American Society of Anesthesiologists physical status classification system (ASA-PS).26,27 Abbreviated Injury Scale codes for major pneumothorax, tension pneumothorax, hemothorax, and hemopneumothorax (all with AIS severity designation 3–5) were used to assess indication for CD between groups.23
Place of injury is registered as the public municipality number where the injury occurred and is mapped to the Centrality Index of Norway, a continuous variable developed by Statistics Norway grouped into six categories, from highest (1) to lowest (6) centrality.28 Categories 1 through 4 were merged to “Urban Norway” and remaining categories “Remote Norway.” For time analyses, outliers were excluded based on data distribution and insight from clinical practice: For “Prehospital time,” outliers longer than 24 hours were excluded (0.1%) in line with the Utstein template.11 For “Time from admission to x-ray chest,” outliers longer than 90 minutes were excluded (1.6%). For “Time from admission to computed tomography (CT)” outliers less than 10 minutes (0.7%) and longer than 90 min (2.7%) were excluded. A complete list of variables collected from NTR and details about recategorization of selected variables are found as Supplemental Digital Content, Supplementary Material 2 (http://links.lww.com/TA/C349).
Each registry score component has a category for “unknown” information, which was analyzed as “missing.” All variables had 5% missing data or less, except from “prehospital GCS” (17%), “highest level of prehospital care provider” (7%), “time from alarm to hospital arrival” (15%), “emergency department (ED) GCS” (9%), “time from hospital arrival to x-ray chest” (15%), and “Time from hospital arrival to CT” (20%). Details are provided in the tables. No imputation was performed.
Statistics
Continuous data are presented as means with standard deviations (SDs) or medians with interquartile ranges (IQR) and categorical data are reported as numbers and proportions. For continuous data, differences between age groups were evaluated using independent samples t test, unequal variances t test, and Mann-Whitney U test, as appropriate. For categorical data, Pearson's χ2 test or Fisher's exact test were used, and effect size estimated with odds ratios (ORs) with 95% confidence intervals (CIs). A p value less than 0.05 (two-tailed) was considered to indicate significance. Analyses were performed using SPSS v.27 (IBM Corp., Armonk, NY).
Ethics
All patients receive written information about the registry, including the opportunity to access the data recorded and to deny registration. Deidentified data were extracted. Variables with information about five or less patients are not reported, in line with Norwegian data protection standards. The study was approved by the Oslo University Hospital data protection officer (no. 19/16593).
RESULTS
Characteristics of Study Objects
A total of 9543 patients met the inclusion criteria (Supplemental Digital Content, Supplementary Fig. 1, http://links.lww.com/TA/C348), of which 72% were 16 years to 64 years of age (G1) and 28% were 65 years or older (G2). The median age in G1 was 42 years (IQR, 28–53) and 75 years (IQR, 69–82) in G2. Study population demographics, injury characteristics, and outcomes stratified by age are listed in Table 1. Male sex predominated in both groups, although the female proportion increased with increasing age. Patients in G2 had a higher median ASA-PS score (p < 0.001), with 31% classified as ASA-PS 3 or higher, as opposed to 5% in G1 (p < 0.001). Blunt trauma constituted 95% in the study cohort. In G1, traffic-related injuries (TRIs) (46%) and high-energy falls (HEFs) (28%) dominated, while in G2 HEF were most frequent (33%), over TRI (31%), and low-energy falls (LEFs) (28%). The ASA-PS score was significantly higher among G2 patients injured by LEF compared with HEF (ASA-PS ≥ 3: LEF: n = 380 (51.6%); HEF: n = 238 (27.6%), p < 0.001). A higher proportion of patients with NISS of 15 or greater was observed in G2 (p < 0.001). G2 had a higher proportion of severe injuries in AIS body regions Head and Thorax (AIS score ≥ 3), while severe abdominal injuries were more frequent in G1. No difference was seen in the pelvis or lower extremity body region. Moreover, G2 had a higher rate of severe head injuries (AIS head score ≥ 3) through all NISS intervals (NISS, 9–14: G1, n = 232 (7.0%) vs. G2, n = 109 (9.8%); NISS, 15–24: G1, n = 451 (23.7%) vs. G2, n = 281 (32.7%); NISS, ≥ 25: G1, n = 906 (56.8%) vs. G2, n = 529 (71.9%); all p < 0.01). G1 and G2 had similar distributions of urban and remote injury locations. Crude 30-day mortality was 3.0% and 14.8% in G1 and G2, respectively (p < 0.001).
TABLE 1.
Study Population Demographics, Injury Characteristics and Outcome Stratified by Age
| G1: 16–64 y, n = 6832 (72%) | G2: ≥65 y, n = 2711 (28%) | p | 65–74 y, n = 1353 (50%) | 75–84 y, n = 836 (31%) | ≥85 y, n = 522 (19%) | |
|---|---|---|---|---|---|---|
| Age: median (IQR), y | 42 (28–53) | 75 (69–82) | NP | 69 (67–72) | 79 (76–82) | 89 (86–92) |
| Male sex, n (%) | 5294 (77.5) | 1783 (65.8) | <0.001 | 1010 (74.6) | 533 (63.8) | 240 (46.0) |
| Preinjury ASA-PSa, median (IQR) | 1 (1–2) | 2 (1–3) | <0.001* | 2 (1–2) | 2 (2–3) | 3 (2–3) |
| ASA-PS 1, n (%) | 4710 (70.6) | 665 (25.1) | 462 (35.1) | 165 (20.1) | 38 (7.4) | |
| ASA-PS 2, n (%) | 1603 (24.0) | 1152 (43.5) | <0.001 | 556 (42.2) | 380 (46.4) | 216 (42.0) |
| ASA-PS 3**, n (%) | 357 (5.4) | 833 (31.4) | 299 (22.7) | 274 (33.5) | 260 (50.6) | |
| Place of injuryb, n (%) | ||||||
| Urban Norway | 5466 (83.3) | 2192 (83.0) | 0.75 | 1064 (81.3) | 678 (82.8) | 450 (87.5) |
| Remote Norway | 1098 (16.7) | 449 (17.0) | 244 (18.7) | 141 (17.2) | 64 (12.5) | |
| Dominating injury typec, n (%) | ||||||
| Blunt | 6322 (94.0) | 2613 (97.8) | <0.001 | 1291 (97.1) | 817 (98.8) | 505 (97.7) |
| Penetrating | 405 (6.0) | 60 (2.2) | 38 (2.9) | 10 (1.2) | 12 (2.3) | |
| Mechanism of injuryd | ||||||
| Transport-related | 3052 (45.7) | 830 (31.3) | 441 (33.5) | 283 (34.5) | 106 (20.7) | |
| Low-energy fall | 439 (6.6) | 747 (28.2) | <0.001 | 264 (20.0) | 242 (29.5) | 241 (47.1) |
| High-energy fall | 1856 (27.8) | 865 (32.6) | 478 (36.3) | 243 (29.6) | 144 (28.1) | |
| Other | 1336 (20.0) | 208 (7.8) | 135 (10.2) | 52 (6.3) | 21 (4.1) | |
| NISS, median (IQR) | 17 (12–22) | 17 (12–26) | <0.001** | 17 (12–26) | 17 (12–27) | 17 (12–27) |
| 9–14 | 3334 (48.8) | 1115 (41.1) | 562 (41.5) | 330 (39.5) | 223 (42.7) | |
| 15–24 | 1904 (27.9) | 860 (31.7) | <0.001 | 440 (32.5) | 277 (33.1) | 143 (27.4) |
| ≥25 | 1594 (23.3) | 736 (27.1) | 351 (25.9) | 229 (27.4) | 156 (29.9) | |
| AIS score ≥ 3, n (%) | ||||||
| Head | 1614 (23.7) | 921 (34.1) | <0.001 | 407 (30.2) | 301 (36.0) | 213 (40.9) |
| Thorax | 2055 (30.2) | 892 (33.0) | 0.007 | 478 (35.5) | 275 (32.9) | 139 (26.7) |
| Abdomen | 629 (9.2) | 119 (4.4) | <0.001 | 62 (4.6) | 38 (4.6) | 19 (3.6) |
| Lower extremity/pelvis | 978 (14.4) | 357 (13.2) | 0.145 | 167 (12.4) | 111 (13.3) | 79 (15.2) |
| 30-d mortalitye, n (%) | 202 (3.0) | 394 (14.8) | <0.001 | 87 (6.6) | 137 (16.7) | 170 (32.9) |
Missing data for G1 and G2, respectively: a: 2.4% and 2.3%. b: 3.9% and 2.6%. c: 1.5% and 1.4%. d: 2.2% and 2.3%. e: 2.1% and 1.6%.
*Mann-Whitney U test.
**Includes 17 (G1) and 62 (G2) patients with ASA 4. No patients with ASA 5 or 6.
NP, not performed.
Prehospital GCS and Clinical Management
Prehospital GCS was significantly lower in G2 compared with G1, demonstrated by the higher proportions of patients in G2 with GCS less than 9 and less than 14 (p < 0.001) (Table 2). The overall prehospital AAM rate was 6.8% in G1 and 5.5% in G2 (p = 0.02) (Table 2). Approximately 85% of patients receiving AAM had their tracheas intubated and 15% received supraglottic airway device or other, showing no significant difference between groups (p = 0.47). Prehospital doctor/paramedic team attendance and air ambulance transportation increased with increasing injury severity for both groups, although these were observed significantly less frequently in G2, both in the entire cohort, in the subgroup of patients with GCS score less than 9, and across all injury severity subgroups (Table 2, Supplemental Digital Content, Supplementary Table 1, http://links.lww.com/TA/C350). Among patients attended by a doctor/paramedic team, no significant differences between age groups were observed for AAM, both overall and adjusted for GCS score less than 9 and NISS of 25 or greater. Further, no significant differences were observed for CD and direct TC transport. Clinical management of patients attended by a prehospital physician is displayed in Table 3.
TABLE 2.
Prehospital GCS, Clinical Management, and Time-Critical Interventions Stratified by Age
| G1: 16–64 y, n = 6832 (72%) | G2: ≥65 y, n = 2711 (28%) | p/OR With 95% CI | 65–74 y, n = 1353 (50%) | 75–84 y, n = 836 (31%) | ≥85 y, n = 522 (19%) | |
|---|---|---|---|---|---|---|
| GCS scorea, median (IQR) | 15 (14–15) | 15 (14–15) | <0.001* | 15 (14–15) | 15 (13–15) | 15 (12–15) |
| GCS score < 9, n (%) | 575 (10.1) | 246 (11.1) | 109 (9.9) | 80 (11.6) | 57 (13.4) | |
| GCS score 9–13, n (%) | 548 (9.6) | 305 (13.8) | <0.001 | 131 (11.9) | 96 (13.9) | 78 (18.4) |
| GCS score 14–15, n (%) | 4566 (80.3) | 1667 (75.2) | 863 (78.2) | 515 (74.5) | 289 (68.2) | |
| Highest level of prehospital care providerb, n (%) | ||||||
| Physician | 2032 (31.9) | 580 (23.0) | 0.64 (0.57–0.71) | 328 (26.2) | 184 (23.8) | 68 (13.8) |
| Ambulance personnel or other** | 4341 (68.1) | 1940 (77.0) | 924 (73.8) | 590 (76.2) | 426 (86.2) | |
| Physician attendance | ||||||
| If GCS score < 9 | 332 (58.3) | 110 (45.1) | 0.59 (0.43–0.79) | 53 (48.6) | 40 (51.3) | 17 (29.8) |
| If NISS ≥ 15 | 1330 (40.9) | 405 (27.3) | 0.54 (0.47–0.62) | 234 (31.6) | 128 (27.7) | 43 (15.3) |
| AAMc, n (%) | 444 (6.8) | 143 (5.5) | 0.80 (0.66–0.97) | 76 (5.9) | 44 (5.4) | 23 (4.5) |
| AAM in patients with GCS score < 9, n (%) | 305 (53.4) | 101 (41.2) | 0.61 (0.45–0.83) | 51 (46.8) | 32 (40.5) | 18 (31.6) |
| Chest decompressiond, n (%) | 69 (1.1) | 20 (0.8) | 0.72 (0.44–1.19) | 13 (1.0) | NA† | NA† |
| Type of transportatione, n (%) | ||||||
| Air ambulance | 1558 (23.9) | 436 (17.0) | 0.65 (0.58–0.73) | 254 (19.8) | 143 (18.1) | 39 (7.8) |
| Ground ambulance or other‡ | 4957 (76.1) | 2136 (83.0) | 1029 (80.2) | 648 (81.9) | 459 (92.2) | |
| Air ambulance transportation, n (%) | ||||||
| If GCS score < 9 | 211 (37.0) | 66 (26.9) | 0.63 (0.45–0.88) | 32 (29.4) | 26 (32.5) | 8 (14.0) |
| If NISS ≥ 15 | 1023 (30.9) | 303 (20.2) | 0.57 (0.49–0.65) | 182 (24.3) | 99 (21.1) | 22 (7.8) |
| Primary destinationf | ||||||
| Trauma Center, n (%) | 2980 (43.6) | 1083 (39.9) | 0.86 (0.79–0.94) | 547 (40.4) | 325 (38.9) | 211 (40.4) |
| Acute Care Trauma Hospital, n (%) | 3852 (56.4) | 1628 (60.1) | 806 (59.6) | 511 (61.1) | 311 (59.6) | |
| Prehospital timeg: median (IQR), min | 64 (38–99) | 68 (44–105) | NP | 68 (45–105) | 69 (43–107) | 66.5 (44–102) |
| Mean (SD), min | 79 (72) | 89 (89) | <0.001§ | 90 (91) | 89 (87) | 88 (87) |
Missing data for G1 and G2, respectively: a: 17% and 18%. b: 7% and 7%. c: 4% and 3%. d: 4% and 3%. e: 5% and 5%. f: 0%. g: 15% and 16%.
*Mann-Whitney U test.
**“Other” includes 65 (G1) and 12 (G2) patients.
†NA: not reported due to low patient numbers.
‡“Other” includes 197 (G1) and 59 (G2) patients.
§Unequal variances t test.
NA, not applicable; NP, not performed.
TABLE 3.
Emergency Interventions and Transport Destination in the Subgroup of Patients Attended by a Prehospital Physician
| G1: 16–64 y, n = 2032 (78%) | G2: ≥65 y, n = 580 (22%) | OR With 95% CI | 65–74 y, n = 328 (56%) | 75–84 y, n = 184 (32%) | ≥85 y, n = 68 (12%) | |
|---|---|---|---|---|---|---|
| AAMa, n (%) | 384 (18.9) | 122 (21.1) | 1.15 (0.91–1.44) | 66 (20.2) | 38 (20.8) | 18 (26.5) |
| In patients with GCS < 9b | 261 (78.6) | 84 (76.4) | 0.88 (0.53–1.47) | 42 (79.2) | 29 (72.5) | 13 (76.5) |
| In patients with NISS ≥ 25 | 304 (41.0) | 90 (41.7) | 1.03 (0.76–1.40) | 46 (39.7) | 31 (41.9) | 13 (50.0) |
| Chest decompressionc, n (%) | 62 (3.1) | 15 (2.6) | 0.84 (0.45–1.50) | 9 (2.8) | NA* | NA* |
| In patients with NISS ≥ 25 | 53 (7.1) | 10 (4.6) | 0.63 (0.32–1.26) | 6 (5.2) | NA* | NA* |
| Primary destinationd, n (%) | ||||||
| Trauma Center | 1225 (60.3) | 325 (56.0) | 0.84 (0.70–1.01) | 144 (43.9) | 78 (42.4) | 33 (48.5) |
| Acute Care Trauma Hospital | 807 (39.7) | 255 (44.0) | 184 (56.1) | 106 (57.6) | 35 (51.5) |
Missing data for G1 and G2, respectively: a: 0.2% and 0.3%; b (GCS missing): 9.4% and 9.5%; c: 0.2% and 0.3%; d: 0%.
*NA: not reported due to low patient numbers.
NA, not applicable.
Significant difference in AAM rate between G1 and G2 was only observed in the NISS of 25 or greater subgroup (G1, 22.0%; G2, 14.4%; OR, 0.60; 95% CI, 0.47–0.68). As expected, the highest proportions were observed in the subgroup of patients with NISS of 25 or greater and GCS score less than 9, however, at significantly lower rates for G2 (G1, 62.2%; G2, 44.1%; OR, 0.48; 95% CI, 0.33–0.68) (Supplemental Digital Content, Supplementary Table 1, http://links.lww.com/TA/C350). Prehospital CD was performed in approximately 1% of all patients and significant differences between age groups were only observed in the NISS of 25 or greater subgroup (G1, 3.9%; G2, 1.8%; OR, 0.46; 95% CI, 0.25–0.85) (Supplemental Digital Content, Supplementary Table 1, http://links.lww.com/TA/C350). Of the 89 patients receiving prehospital CD, 50 received a chest drain (56%), 21 needle decompression (24%), 13 an incision (15%), and five other or unknown (6%). Indication for CD, defined as relevant AIS codes previously described, did not differ between age groups (G1, n = 483 (7.1%); G2, n = 213 (7.9%); p = 0.182).
Mean time from alarm to hospital arrival was 79 minutes in G1 and 89 minutes in G2 (p < 0.001). G2 patients were less frequently transported to a TC as primary destination (G1, 43.6%; G2, 39.9%; OR, 0.86; 95% CI, 0.79–0.94).
ED Physiologic Variables and Clinical Management
Emergency department GCS was significantly lower in G2 than G1 among patients with NISS of 15 or greater (p = 0.004), demonstrated by the higher proportions of patients with ED GCS score less than 9 and less than 14 (NISS, 15–24: p = 0.03; NISS, ≥ 25: p = 0.006) (Table 4). The proportion of patients with systolic blood pressure (SBP) less than 90 mm Hg was higher in G2, except in the NISS of 25 or greater subgroup where the groups were similar. Emergency department physiologic parameters and clinical management are displayed in Table 4.
TABLE 4.
Emergency Department Physiologic Parameters and Clinical Management Stratified by NISS and Age
| NISS 9 Through 14 | NISS 15 Through 24 | NISS 25 Through 75 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| G1: 16–64 y, n = 3334 (49%) | G2: ≥65 y, n = 1115 (41%) | p/OR With 95% CI | G1: 16–64 y, n = 1904 (28%) | G2: ≥65 y, n = 860 (32%) | p/OR With 95% CI | G1: 16–64 y, n = 1594 (23%) | G2: ≥65 y, n = 736 (27%) | p/OR With 95% CI | |
| GCSa, median (IQR) | 15 (15–15) | 15 (15–15) | 0.11* | 15 (15–15) | 15 (14–15) | 0.004* | 14 (10–15) | 14 (9–15) | 0.004* |
| GCS score <9, n (%) | 68 (2.1) | 17 (1.6) | 52 (2.9) | 29 (3.7) | 287 (22.5) | 151 (24.9) | |||
| GCS score 9–13, n (%) | 163 (5.1) | 71 (6.7) | 0.086 | 138 (7.8) | 85 (10.7) | 0.03 | 205 (16.1) | 127 (21.0) | 0.006 |
| GCS 14–15, n (%) | 2975 (92.8) | 974 (91.7) | 1578 (89.3) | 680 (85.6) | 783 (61.4) | 328 (54.1) | |||
| SBPb: mean (SD), mm Hg | 136.5 (20.7) | 146.4 (29.3) | <0.001** | 133.2 (21.3) | 143.2 (28.3) | <0.001** | 126.7 (29.5) | 141.3 (35.4) | <0.001** |
| <90 mm Hg, n (%) | 44 (1.3) | 36 (3.3) | <0.001 | 39 (2.1) | 35 (4.1) | 0.002 | 153 (9.9) | 57 (8.0) | 0.15 |
| Endotracheal intubationc, n (%) | 120 (3.6) | 37 (3.3) | 0.92 (0.63–1.34) | 124 (6.5) | 50 (5.8) | 0.89 (0.63–1.24) | 359 (22.5) | 131 (17.8) | 0.75 (0.60–0.93) |
| If ED GCS < 9, n (%) | 27 (39.7) | 9 (52.9) | 1.71 (0.59–4.98) | 28 (53.8) | 13 (44.8) | 0.70 (0.28–1.74) | 149 (51.9) | 71 (47.0) | 0.82 (0.55–1.22) |
| ED chest draind, n (%) | 99 (3.0) | 37 (3.4) | 1.13 (0.77–1.66) | 144 (7.7) | 59 (7.0) | 0.90 (0.66–1.23) | 316 (23.5) | 102 (15.7) | 0.61 (0.48–0.78) |
*Mann-Whitney U test.
**Unequal variances t test.
Missing data by increasing NISS interval for G1 and G2, respectively: a: 4%, 7%, 20% and 5%, 8%, 18%; b: 1%, 1%, 4% and 1%, 1%, 3%; c: 0%; d: 1%, 2%, 16% and 2%, 2%, 12%.
Overall, ED intubation rates were 8.8% and 8.0% in G1 and G2, respectively (p = 0.43) (Supplemental Digital Content, Supplementary Table 2, http://links.lww.com/TA/C351). Among patients with NISS less than 25, no significant differences in intubation rates or chest drain insertion rates were observed (Table 4). Among patients with NISS of 25 or greater, G2 patients were less frequently intubated or received chest drain (intubation: G1, 22.5%; G2, 17.8%; OR, 0.75; 95% CI, 0.60–0.93; chest drain: G1, 23.5%; G2, 15.7%; OR, 0.61; 95% CI, 0.48–0.78) (Table 4).
ED Radiological Examinations
X-ray of the chest was performed in more than 90% of patients across age and injury severity groups (Table 5, Supplemental Digital Content, Supplementary Table 3, http://links.lww.com/TA/C352). The median time was 5 minutes from hospital admission (Table 5). X-ray of the pelvis were performed in 71% to 78% of patients, with lowest rates observed for older adults with NISS of 25 or greater (NISS, ≥25: G1, 78.2%; G2, 71.2%; OR, 0.69; 95% CI, 0.57–0.84; Table 4). Emergency department CT was performed in 87% to 90% of patients through both age groups and all injury severity groups with no significant differences observed (Table 5). Among patients with severe injuries (AIS score ≥ 3) in the thorax or the pelvis and lower extremity, G2 patients less frequently received x-ray of the chest and pelvis on admission (thorax, p = 0.001; pelvis and lower extremity, p = 0.031) (Supplemental Digital Content, Supplementary Table 4, http://links.lww.com/TA/C353).
TABLE 5.
Emergency Department Radiological Examinations Stratified by NISS and Age
| NISS 9 Through 14 | NISS 15 Through 24 | NISS 25 Through 75 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| G1: 16–64 y, n = 3334 (49%) | G2: ≥65 y, n = 1115 (41%) | p/OR With 95% CI | G1: 16–64 y, n = 1904 (28%) | G2: ≥65 Years, n = 860 (32%) | p/OR With 95% CI | G1: 16–64 y, n = 1594 (23%) | G2: ≥65 y, n = 736 (27%) | p/OR With 95% CI | |
| X-ray chesta, n (%) | 3014 (90.5) | 1021 (91.7) | 1.16 (0.91–1.47) | 1774 (93.2) | 784 (91.2) | 0.76 (0.56–1.02) | 1505 (94.5) | 665 (90.4) | 0.54 (0.39–0.75) |
| X-ray pelvisb, n (%) | 2541 (76.4) | 854 (76.9) | 1.03 (0.88–1.21) | 1482 (78.0) | 651 (76.0) | 0.89 (0.74–1.08) | 1242 (78.2) | 523 (71.2) | 0.69 (0.57–0.84) |
| CTc, n (%) | 2929 (87.9) | 998 (89.7) | 1.2 (0.96–1.49) | 1745 (91.7) | 778 (90.6) | 0.86 (0.65–1.15) | 1399 (87.8) | 665 (90.4) | 1.30 (0.98–1.73) |
| Time to x-ray chestd: median (IQR), min | 5 (3–9) | 5 (4–9) | NP | 5 (3–8) | 5 (3–8) | NP | 5 (3–8) | 5 (3–8) | NP |
| Mean (SD) | 7.9 (9.6) | 8.9 (11.5) | 0.009* | 7.2 (8.3) | 7.6 (9.4) | 0.42* | 6.4 (6.5) | 7.5 (9.7) | 0.006* |
| Within 15 min (%) | 91.4 | 89.2 | NP | 93.0 | 92.2 | NP | 95.5 | 93.5 | NP |
| Within 60 min (%) | 99.1 | 98.6 | NP | 99.4 | 98.9 | NP | 99.7 | 99 | NP |
| Time to CTe: median (IQR), min | 30 (22–40) | 30 (24–40) | NP | 30 (22–39) | 30 (23–40) | NP | 26 (20–37) | 27 (21–38) | NP |
| Mean (SD) | 32.9 (14.6) | 33.3 (13.9) | 0.50* | 32.6 (14.4) | 34.4 (16.3) | 0.01* | 30.7 (14.6) | 30.8 (14.4) | 0.87* |
Missing data by increasing NISS interval for G1 and G2, respectively: a: 0%; b: 0%; c: 0%; d: 12%, 15%, 21% and 15%, 17%, 17%; e: 23%, 20%, 24% and 24%, 21%, 24%.
*Independent-sample t test.
NP, not performed.
DISCUSSION
The aim of this study was to compare clinical management of adult and older trauma patients, focusing on prehospital and early in-hospital time-critical interventions and admission radiological examinations. Findings showed that, irrespective of injury severity, older patients (≥65 years) received lower rates of prehospital doctor/paramedic team attendance, air ambulance conveyance, and transport directly to a TC. Severely injured older patients (NISS ≥ 25) received prehospital and in-hospital AAM and CD, and primary survey x-ray imaging significantly less frequently than younger adults. We found no significant differences in AAM and CD rates in patients managed by prehospital doctor/paramedic teams. No significant differences in time-critical interventions or radiological examinations were observed among patients with moderate to severe injuries (NISS < 25).
The study population demographics and injury characteristics are in line with previous comparable studies: older adults were more often female, had significant comorbidity, more than 30% had at least one severe head injury, a higher proportion had GCS score less than 9, and mortality was higher (Table 1).4,5,29,30 Noticeably, HEFs and traffic-related injuries were the most common injury mechanisms among older patients. Other studies describe a surge of LEFs in the older population,4,5,29,30 similar to findings in a Norwegian study.31 However, the present study excluded all those not met by a trauma team to enable within-system evaluation of clinical management. This highlights that TTA is still strongly linked to high-energy mechanisms of trauma even for older adults,32,33 despite several publications and ATLS curriculum emphasizing the high risk of severe injuries from LEFs in the elderly.10,34 Additionally, important clinical characteristics warranting high-level care and expedite transport were equally or more frequently present in G2 than in G1, such as higher proportions of patients with AIS head score of 3 or higher, GCS score less than 9, NISS of 15 or greater, or significant comorbidity (Table 1, Table 2). This was not reflected in the prehospital management, where elderly patients were less often attended by a prehospital doctor/paramedic team, conveyed by air ambulance, or transported to TC as primary destination (Table 2, Supplemental Digital Content, Supplementary Table 1, http://links.lww.com/TA/C350). Inadequate activation of the trauma system is the challenge, beginning with dispatch.
Elderly patients are frequently injured by insignificant trauma mechanisms and present with vague symptoms.31,35,36 This increases the risk for the EMDC operator to not recognize or underestimate injury severity, leading to application of nontrauma-specific operative chapters in the Index. This may be one of the reasons why we observed lower rates of doctor/paramedic team attendance, air ambulance conveyance and subsequently prehospital time-critical interventions. A study of all trauma-related emergency calls in South-Eastern Norway reported that operative chapters in the Index containing trauma-specific information was used in 88% of calls,19 suggesting an area for improvement.
The Norwegian criteria for trauma field triage share design characteristics and specific criteria with triage tools associated with undertriage of older patients (Fig. 1).37,38 By design, the Index recommends involving doctor/paramedic teams when patients match field triage criteria (Fig. 1), which older injured patients are less likely to do.35–37 In this study, younger adults showed a mechanism of injury distribution more likely to meet field triage criteria (TRI, HEF, and other), which may have contributed to the higher frequency of doctor/paramedic team attendance and air ambulance conveyance for G1 (Table 1). On the other hand, being older than 60 years, advanced comorbidity, and use of anticoagulants are criteria that lower the threshold for transport to a TC and TTA (Fig. 1). This could have influenced decision to dispatch advanced doctor/paramedic teams to more older adults, although the extent is uncertain as information about comorbidity and medication is not easily accessible for EMDC and prehospital personnel. Geographic location did not significantly differ between the groups and is, therefore, unlikely to have contributed to differences. Besides the convincing evidence that elderly in this study had lower prehospital GCS and, therefore, signs of physiologic derangement, we cannot further assess the influence of physiologic criteria on dispatch differences due to the levels of missing data on other variables (SBP, respiratory rate).
Differences in clinical management, must be given attention as possible improvement targets. We find EMDC triage and dispatch to be the crux of trauma system activation and suggest improvements: first, the Index should better guide operators in injury assessment of elderly, e.g., explicit information about likelihood of severe injuries despite low-energy trauma, and a reminder to consider trauma in acutely unwell elderly patients could be placed in the chapter Unidentified Problem. Second, our findings reveal a need to redefine trauma criteria, especially for elderly patients. This is a matter of great interest internationally, and this includes surveillance of literature and implementation of changes if justified. A recent systematic review of elderly-specific triage criteria found no studies that could demonstrate undertriage levels below the 5% recommended by American College of Surgeons Committee on Trauma.17,37 Third, use of video assisted EMDC triage, recently deployed at most EMDCs in Norway, should be encouraged and assessed according to dispatch precision. Smaller studies show promising results where it is reported to be particularly helpful in situations where no trigger for instant dispatch was met, typically for LEFs.39 Finally, continued efforts to educate personnel in the specific challenges relating to older trauma patients should be a priority for all parts of the trauma treatment chain.
Prehospital time-critical interventions are closely linked to the dispatch of doctor/paramedic teams (Table 2, Table 3). Both G1 and G2 received AAM and CDs at similar rates when attended by a doctor/paramedic team. Griggs et al.40 recently showed that doctor/paramedic team involvement in older trauma patients frequently led to time-critical interventions, particularly prehospital anesthesia and intubation, even among patients with low-energy trauma who did not fulfill the initial criteria for immediate dispatch. This supports our finding that physicians on scene perform advanced interventions also at high age, although likely from a careful selection of cases. To what extent advanced prehospital care and bypass to TC care is beneficial for older adults should be investigated in future studies, as well as the effect changes in dispatch criteria have on dispatch of advanced resources to elderly, the frequency of interventions, and association with outcome.
The key findings from our comparisons of inhospital care were that no significant differences in time-critical interventions or radiological examinations were observed among patients with NISS less than 25, and the median time from hospital admission to chest x-ray was 5 minutes across age groups and injury severity subgroups (Table 4, Supplemental Digital Content, Supplementary Table 3, http://links.lww.com/TA/C352). This shows that the Norwegian trauma system is efficient and responsive for all admitted adult patients. Older patients with NISS of 25 or greater, however, less frequently received prehospital and ED AAM, CD, and admission x-ray imaging (Table 4, Table 5, Supplemental Digital Content, Supplementary Tables 1, http://links.lww.com/TA/C350 and 3, http://links.lww.com/TA/C352). Age and injury severity are known risk factors for a poor prognosis after trauma41 and in line with previous research, our findings show how both are associated with decreasing intervention and examination rates.42 Consequently, the differences in clinical management observed among patients in the highest NISS subgroup (≥25) may be based on sound clinical risk-benefit evaluations leading to limitations or withdrawal of aggressive care where deemed futile or where advance care directives were placed. Unfortunately, this cannot be evaluated based on our data. As injury mechanism and preexisting medical conditions differ between age groups, it would be expected that care given will vary as well.
One of this study's strengths are the analyses of data from all trauma hospitals in a country where a national inclusive trauma system is implemented. Similarities shared between Norway's and other countries' inclusive trauma systems make the findings transferable. There are some limitations to our study, first and foremost related to its retrospective design. We relied on AIS, NISS, and GCS score less than 9 to determine injury severity, although we appreciate that more data about vital signs would bring valuable information. This was not available because of incomplete registration of prehospital data, a challenge for many registries and services.43 The indication for performing or not performing time-critical interventions is not registered in the NTR. Instead, we used measures with a high likelihood of indication for interventions, such as injury stratification and GCS score less than 9 and assessed all AIS codes associated with potential need for CD. The age group 16 years to 64 years was used as the comparator although overtriage in this group would skew the interpretation of our analyses in disfavor of older patients, which we were unable to adjust for. Finally, many of the differences yielded statistical significance, which not necessarily translates to clinical significance.
In summary, older trauma patients, irrespective of injury severity, were less often attended by doctor/paramedic teams, conveyed by air ambulance, or transported directly to a TC compared with younger adults. Time-critical interventions and primary survey x-ray imaging were less often performed on severely injured elderly trauma patients (NISS ≥ 25), although for patients with moderate to severe injuries (NISS < 25), prehospital time-critical interventions and clinical management in the ED showed no significant difference between age groups. When prehospital doctor/paramedic teams were attending the patients, no significant differences in prehospital advanced interventions were found between age groups. Overall, the Norwegian trauma system seems to be efficient, safe, and responsive for adult trauma patients met by a trauma team. However, our findings indicate that older adults are at risk of not receiving advanced prehospital care and that decisions made during dispatch have major consequences for the subsequent course. Improved dispatch of doctor/paramedic teams to older patients may make it more targeted and accessible to all age groups.
Supplementary Material
ACKNOWLEDGMENT
This work was funded by the Norwegian Air Ambulance Foundation.
AUTHORSHIP
M.C.-Ø. and E.J. participated in the acquisition and analysis of the data. M.C.-Ø., T.W., O.R., and E.J. contributed toward the interpretation of data for the article. M.C.-Ø. and E.J. drafted the article. E.J., T.W., and O.R. critically revised the article for intellectual content. All authors made substantial contributions to the conception and design of the work, provided final approval of the version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors attest to meeting the four ICMJE.org. authorship criteria.
DISCLOSURE
The authors declare no conflicts of interest.
Footnotes
Published online: February 7, 2022.
Extracts of this study were presented at the 2021 annual meetings for the Norwegian Society of Anaesthesiology and the Norwegian Orthopaedic Association.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.jtrauma.com).
Contributor Information
Torben Wisborg, Email: torben.wisborg@traumatologi.no.
Olav Røise, Email: olav.roise@medisin.uio.no.
Elisabeth Jeppesen, Email: elisabeth.jeppesen@norskluftambulanse.no.
REFERENCES
- 1.Eurostat . Ageing Europe—looking at the lives of older people in the EU. 2020.
- 2.Callaway DW, Wolfe R. Geriatric trauma. Emerg Med Clin North Am. 2007;25(3):837–860 x. [DOI] [PubMed] [Google Scholar]
- 3.Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. J Trauma. 1998;45(4):805–810. [DOI] [PubMed] [Google Scholar]
- 4.Giannoudis PV, Harwood PJ, Court-Brown C, Pape HC. Severe and multiple trauma in older patients; incidence and mortality. Injury. 2009;40(4):362–367. [DOI] [PubMed] [Google Scholar]
- 5.Spering C, Lefering R, Bouillon B, Lehmann W, von Eckardstein K, Dresing K, Sehmisch S. It is time for a change in the management of elderly severely injured patients! An analysis of 126,015 patients from the TraumaRegister DGU®. Eur J Trauma Emerg Surg. 2019;46:487–497. [DOI] [PubMed] [Google Scholar]
- 6.Gabbe BJ Simpson PM Cameron PA Ponsford J Lyons RA Collie A Fitzgerald M Judson R Teague WJ Braaf S, et al. Long-term health status and trajectories of seriously injured patients: a population-based longitudinal study. PLoS Med. 2017;14(7):e1002322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banerjee J Baxter M Coats T Edwards A Griffiths R Kumar DS Lecky F Sammy I Turpin S Wheldon A, et al. The Trauma Audit and Research Network—major trauma in older people 2017. Report. 2017. [Google Scholar]
- 8.Rehn M, Hyldmo PK, Magnusson V, Kurola J, Kongstad P, Rognas L, Juvet LK, Sandberg M. Scandinavian SSAI clinical practice guideline on pre-hospital airway management. Acta Anaesthesiol Scand. 2016;60(7):852–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crewdson K Lockey D Voelckel W Temesvari P Lossius HM, EHAC Medical Working Group . Best practice advice on pre-hospital emergency anaesthesia & advanced airway management. Scand J Trauma Resusc Emerg Med. 2019;27(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Advanced trauma life support (ATLS). the tenth ed. Chicago: American College of Surgeons’ Committee on Trauma; 2018. [Google Scholar]
- 11.Ringdal KG Coats TJ Lefering R Di Bartolomeo S Steen PA Roise O Handolin L Lossius HM, Utstein TCD expert panel . The Utstein template for uniform reporting of data following major trauma: a joint revision by SCANTEM, TARN, DGU-TR and RITG. Scand J Trauma Resusc Emerg Med. 2008;16:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ringen AH, Gaski IA, Rustad H, Skaga NO, Gaarder C, Naess PA. Improvement in geriatric trauma outcomes in an evolving trauma system. Trauma Surg Acute Care Open. 2019;4(1):e000282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.von Elm E Altman DG Egger M Pocock SJ Gotzsche PC Vandenbroucke JP, STROBE Initiative . Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cuevas-Østrem M, Røise O, Wisborg T, Jeppesen E. Geriatric trauma—a rising tide. assessing patient safety challenges in a vulnerable population using Norwegian Trauma Registry Data and Focus Group Interviews: protocol for a mixed methods study. JMIR Res Protoc. 2020;9(4):e15722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gleditsch RF, Thomas MJ, Syse A. Norway's 2020 population projections. National level results, methods and assumptions. www.ssb.no: Statistics Norway; 2020.
- 16.National traumaplan [in Norwegian]: Norwegian National Advisory Unit on Trauma; 2016. Available at: www.traumeplan.no. Accessed March 17, 2021.
- 17.Rotondo MFC, Smith C, Stephen R. Resources for Optimal Care of the Injured Patient. American College of Surgeons, Committee on Trauma; 2014. [Google Scholar]
- 18.NAKOS . Norwegian Index for Medical Emergencies. Oslo. The Norwegian Directorate of Health; 2018: Available at: https://www.helsedirektoratet.no/veiledere/norsk-indeks-for-medisinsk-nodhjelp/Norsk%20indeks%20for%20medisinsk%20nødhjelp.pdf/_/attachment/inline/c9aa280e-3e84-4197-8743-36f5dd934b8b:f649297bce76e95aed934803c67384569b027d61/Norsk%20indeks%20for%20medisinsk%20nødhjelp.pdf. Accessed December 16, 2021. [Google Scholar]
- 19.Samdal M, Thorsen K, Græsli O, Sandberg M, Rehn M. Dispatch accuracy of physician-staffed emergency medical services in trauma care in South-East Norway: a retrospective observational study. Scand J Trauma Resusc Emerg Med. 2021;29(1):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osteras O, Brattebo G, Heltne JK. Helicopter-based emergency medical services for a sparsely populated region: a study of 42,500 dispatches. Acta Anaesthesiol Scand. 2016;60(5):659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Annual Report for 2019 [in Norwegian] Oslo. Norwegian Trauma Registry; 2020: Available at: https://www.kvalitetsregistre.no/sites/default/files/2021-02/Årsrapport%202019%20Nasjonalt%20traumeregister.pdf. [Google Scholar]
- 22.Ministry of Health, Forskrift om medisinske kvalitetsregistre. Lovdata; 2019. [Google Scholar]
- 23.Gennarelli TA, Wodzin E. Abbreviated Injury Scale 2005: update 2008: Russ Reeder; 2008.
- 24.Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43(6):922–925; discussion 5-6. [DOI] [PubMed] [Google Scholar]
- 25.Stein SC, Spettell C. The Head Injury Severity Scale (HISS): a practical classification of closed-head injury. Brain Inj. 1995;9(5):437–444. [DOI] [PubMed] [Google Scholar]
- 26.ASA Physical Status Classification System American Society of Anesthesiologists; 2019. updated 2019, October 23. Available at: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system.
- 27.Skaga NO, Eken T, Sovik S, Jones JM, Steen PA. Pre-injury ASA physical status classification is an independent predictor of mortality after trauma. J Trauma. 2007;63(5):972–978. [DOI] [PubMed] [Google Scholar]
- 28.Høydahl E. Ny sentralitetsindex for kommunene. www.ssb.no: Statistics Norway; 2017.
- 29.Kojima M, Endo A, Shiraishi A, Otomo Y. Age-related characteristics and outcomes for patients with severe trauma: analysis of Japan’s Nationwide trauma registry. Ann Emerg Med. 2019;73(3):281–290. [DOI] [PubMed] [Google Scholar]
- 30.de Vries R, Reininga IHF, Pieske O, Lefering R, El Moumni M, Wendt K. Injury mechanisms, patterns and outcomes of older polytrauma patients—an analysis of the Dutch Trauma Registry. PLoS One. 2018;13(1):e0190587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cuevas-Ostrem M, Roise O, Wisborg T, Jeppesen E. Epidemiology of geriatric trauma patients in Norway: a nationwide analysis of Norwegian Trauma Registry data, 2015–2018. A retrospective cohort study. Injury. 2020;52:450–459. [DOI] [PubMed] [Google Scholar]
- 32.Kodadek LM, Selvarajah S, Velopulos CG, Haut ER, Haider AH. Undertriage of older trauma patients: is this a national phenomenon? J Surg Res. 2015;199(1):220–229. [DOI] [PubMed] [Google Scholar]
- 33.Staudenmayer KL, Hsia RY, Mann NC, Spain DA, Newgard CD. Triage of elderly trauma patients: a population-based perspective. J Am Coll Surg. 2013;217(4):569–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ayoung-Chee P, McIntyre L, Ebel BE, Mack CD, McCormick W, Maier RV. Long-term outcomes of ground-level falls in the elderly. J Trauma Acute Care Surg. 2014;76(2):498–503; discussion. [DOI] [PubMed] [Google Scholar]
- 35.Rau CS, Wu SC, Chen YC, Chien PC, Hsieh HY, Kuo PJ, Hsieh CH. Effect of age on Glasgow Coma Scale in patients with moderate and severe traumatic brain injury: an approach with propensity score-matched population. Int J Environ Res Public Health. 2017;14(11):1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oyetunji TA, Chang DC, Crompton JG, Greene WR, Efron DT, Haut ER, Cornwell EE, 3rd, Haider AH. Redefining hypotension in the elderly: normotension is not reassuring. Arch Surg. 2011;146(7):865–869. [DOI] [PubMed] [Google Scholar]
- 37.Fuller G, Pandor A, Essat M, Sabir L, Buckley-Woods H, Chatha H, Holt C, Keating S, Turner J. Diagnostic accuracy of prehospital triage tools for identifying major trauma in elderly injured patients: a systematic review. J Trauma Acute Care Surg. 2021;90(2):403–412. [DOI] [PubMed] [Google Scholar]
- 38.Sasser SM Hunt RC Faul M Sugerman D Pearson WS Dulski T Wald MM Jurkovich GJ Newgard CD Lerner EB, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(RR-1):1–20. [PubMed] [Google Scholar]
- 39.Ter Avest E, Lambert E, de Coverly R, Tucker H, Griggs J, Wilson MH, Ghorbangholi A, Williams J, Lyon RM. Live video footage from scene to aid helicopter emergency medical service dispatch: a feasibility study. Scand J Trauma Resusc Emerg Med. 2019;27(1):55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Griggs JE Barrett JW Ter Avest E de Coverly R Nelson M Williams J Lyon RM, Air Ambulance Kent Surrey Sussex . Helicopter emergency medical service dispatch in older trauma: time to reconsider the trigger? Scand J Trauma Resusc Emerg Med. 2021;29(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sammy I, Lecky F, Sutton A, Leaviss J, O’Cathain A. Factors affecting mortality in older trauma patients—a systematic review and meta-analysis. Injury. 2016;47(6):1170–1183. [DOI] [PubMed] [Google Scholar]
- 42.Vassallo J, Fuller G, Smith JE. Relationship between the Injury Severity Score and the need for life-saving interventions in trauma patients in the UK. Emerg Med J. 2020;37(8):502–507. [DOI] [PubMed] [Google Scholar]
- 43.Tonsager K, Kruger AJ, Ringdal KG, Rehn M. Data quality of Glasgow coma scale and systolic blood pressure in scientific studies involving physician-staffed emergency medical services: systematic review. Acta Anaesthesiol Scand. 2020;64:888–909. [DOI] [PubMed] [Google Scholar]


