Abstract
Pulmonary fibrosis is a progressive interstitial lung disease of unknown aetiology with a poor prognosis. Studying genetic diseases associated with pulmonary fibrosis provides insights into the pathogenesis of the disease. Hermansky–Pudlak syndrome (HPS), a rare autosomal recessive disorder characterised by abnormal biogenesis of lysosome-related organelles, manifests with oculocutaneous albinism and excessive bleeding of variable severity. Pulmonary fibrosis is highly prevalent in three out of 10 genetic types of HPS (HPS-1, HPS-2 and HPS-4). Thus, genotyping of individuals with HPS is clinically relevant. HPS-1 tends to affect Puerto Rican individuals due to a genetic founder effect. HPS pulmonary fibrosis shares some clinical features with idiopathic pulmonary fibrosis (IPF), including dyspnoea, cough, restrictive lung physiology and computed tomography (CT) findings of fibrosis. In contrast to IPF, HPS pulmonary fibrosis generally affects children (HPS-2) or middle-aged adults (HPS-1 or HPS-4) and may be associated with ground-glass opacification in CT scans. Histopathology of HPS pulmonary fibrosis, and not IPF, shows vacuolated hyperplastic type II cells with enlarged lamellar bodies and alveolar macrophages with lipofuscin-like deposits. Antifibrotic drugs approved as treatment for IPF are not approved for HPS pulmonary fibrosis. However, lung transplantation has been performed in patients with severe HPS pulmonary fibrosis. HPS pulmonary fibrosis serves as a model for studying fibrotic lung disease and fibrosis in general.
Short abstract
Hermansky–Pudlak syndrome (HPS) is an autosomal recessive disorder characterised by highly prevalent pulmonary fibrosis. HPS pulmonary fibrosis is a rare inherited interstitial lung disease that can serve as a model for studying fibrotic lung disorders. https://bit.ly/2ZWFR2Y
Introduction
Pulmonary fibrosis, a multifactorial, often fatal lung disease with limited treatment, is characterised by deposition of extracellular matrix protein and accumulation of fibroblasts, myofibroblasts and immune cells in the alveolar interstitium, leading to destruction of the pulmonary architecture [1–3]. The aetiology of pulmonary fibrosis is incompletely understood and several hypotheses regarding potential pathogenic mechanisms of disease have been posited [1–4]. Some data suggest that pulmonary fibrosis results from recurrent epithelial injury with aberrant repair or accelerated ageing [1–6]. Type II epithelial cell senescence and functional abnormalities, including endoplasmic reticulum stress, oxidative injury, mitochondrial dysfunction and impaired proteostasis, may alter alveolar homeostasis and contribute to the pathobiology of pulmonary fibrosis [1–4, 6–10]. Proposed mechanisms of disease include release of profibrotic mediators into the extracellular alveolar milieu, recruitment and activation of fibroblasts or myofibroblasts, epithelial–mesenchymal transition, and abnormal extracellular matrix turnover [1–4]. Several cytokines and growth factors are believed to contribute to the pathogenesis of pulmonary fibrosis, including transforming growth factor (TGF)-β, connective tissue growth factor, platelet-derived growth factor, CCL2 (chemokine (C-C motif) ligand 2/monocyte chemoattractant protein-1), galectin-3, matrix metalloproteinases and interleukin-11 [1–4, 11, 12]. Dysregulation of these and other molecules may disrupt lung homeostasis and lead to development of pulmonary fibrosis.
Pulmonary fibrosis is a manifestation of several inherited disorders, including telomere disease, dyskeratosis congenita and Hermansky–Pudlak syndrome (HPS) [13–21]. HPS is a rare autosomal recessive disorder with locus heterogeneity that can serve as a model for investigating the pathogenesis of pulmonary fibrosis. HPS is characterised by oculocutaneous albinism, bleeding diathesis, inflammatory bowel disease and pulmonary fibrosis (figure 1) [16, 17, 22, 23]. HPS was initially described by Frantisek Hermansky and Paulus Pudlak in 1959 [24]. They reported two patients with oculocutaneous albinism, bleeding diathesis due to platelet dysfunction and reticular cells with pigment deposits in the bone marrow. Since the initial report, 10 genetic types of HPS have been identified and each is associated with a defect in biogenesis of lysosome-related organelles complex (BLOC)-1 (HPS-7, HPS-8 and HPS-9), BLOC-2 (HPS-3, HPS-5 and HPS-6), BLOC-3 (HPS-1 and HPS-4) or adapter protein (AP)-3 complex (HPS-2 and HPS-10) (table 1) [17, 22, 25–34]. The worldwide prevalence of HPS is approximately 1–9 per million individuals, but prevalence per HPS genetic type can be different in subpopulations due to genetic founder effects. Four HPS genetic types are associated with the development of interstitial lung disease (ILD) or pulmonary fibrosis. Most middle-aged adults with HPS-1 or HPS-4 and children or young adults with HPS-2 develop progressive and generally fatal pulmonary fibrosis [16, 17, 20, 21, 35]. In addition, one child with HPS-10 was reported to have ILD [33]. Given the high prevalence of fibrotic lung disease, understanding the pathogenesis of pulmonary fibrosis in these HPS genetic types can provide insights into the aetiology of fibrosis, which is incompletely understood. In this review, we summarise the current understanding of the genetics, pathobiology, clinical features and management of HPS pulmonary fibrosis.
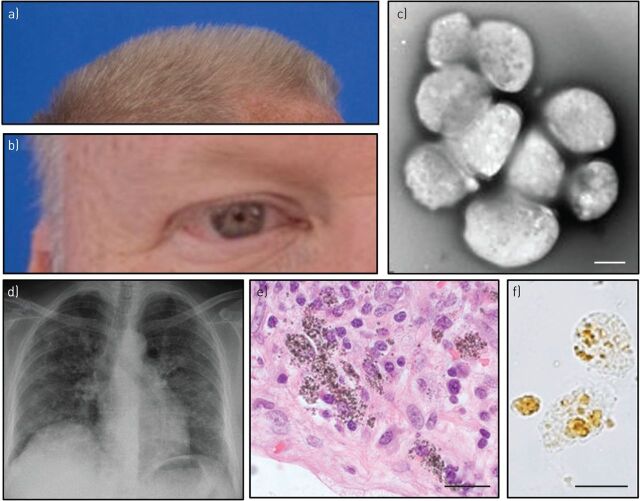
FIGURE 1.
Clinical features of Hermansky–Pudlak syndrome (HPS). a, b) Hypopigmentation of a) hair and b) skin and iris of a Puerto Rican male. c) δ-granules are absent in platelets from a patient with HPS-1 imaged using whole-mount transmission electron microscopy. Scale bar: 2 μm. d) Bilateral interstitial infiltrates are found in a chest radiograph of a 50-year-old female with HPS pulmonary fibrosis. e) Fibrotic lung tissue stained with haematoxylin and eosin and f) unstained renal epithelial cells isolated from urine derived from a subject with HPS-1 show abnormal intracellular deposits. Scale bar: 20 μm.
TABLE 1.
Hermansky–Pudlak syndrome (HPS)-associated genes, loci, proteins and complexes
| HPS type | Gene# | Locus | Protein | Complex |
| HPS-1 | HPS1 | 10q23.1 | HPS1 | BLOC-3 |
| HPS-2 | AP3B1 | 5q14.1 | AP-3 complex β3A subunit | AP-3 |
| HPS-3 | HPS3 | 3q24 | HPS3 | BLOC-2 |
| HPS-4 | HPS4 | 22q11.2–q12.2 | HPS4 | BLOC-3 |
| HPS-5 | HPS5 | 11p15–p13 | HPS5 | BLOC-2 |
| HPS-6 | HPS6 | 10q24.3 | HPS6 | BLOC-2 |
| HPS-7 | DTNBP1 | 6p22.3 | Dysbindin | BLOC-1 |
| HPS-8 | BLOC1S3 | 19q13 | BLOC-1 subunit 3 | BLOC-1 |
| HPS-9 | PLDN | 15q15 | Pallidin | BLOC-1 |
| HPS-10 | AP3D1 | 19p13.3 | AP-3 complex δ1 subunit | AP-3 |
AP: adaptor protein; BLOC: biogenesis of lysosome-related organelles complex. #: see www.genecards.org for aliases.
Genetics of HPS pulmonary fibrosis
10 types of HPS have been identified and each is associated with variants in a specific gene (table 1) [17, 22, 34]. Pulmonary fibrosis develops in individuals with HPS-1 [16], HPS-2 [20, 35] or HPS-4 [21]; ILD was described in a young boy with HPS-10 [33].
HPS-1
The HPS1 gene, identified by positional cloning in 1996 by Oh et al. [36], is 30.5 kb with 20 exons and is found on chromosome 10q24.1–q25.1. HPS1 encodes a 700-amino-acid protein with a molecular weight of 79.3 kDa. HPS1 and HPS4 proteins interact to form BLOC-3 [37, 38]. Although the function of BLOC-3 has not been fully elucidated, BLOC-3 is a Rab32/38 guanine nucleotide exchange factor, and promotes membrane recruitment of Rab32 and Rab38 [39]. BLOC-3 was found to activate Rab32/38, which regulates melanogenesis in melanocytes in vitro [40]. Given that HPS1 and HPS4 proteins are subunits of the same complex, their clinical manifestations are similar, including the development of pulmonary fibrosis in middle-aged adults.
67 HPS1 variants located throughout the entire gene have been reported in association with HPS-1 [34]. The variants include frameshift, missense, nonsense, insertion, deletion and splice site variants. A common HPS1 variant is c.1472_1487dup16-bp. This 16-bp duplication in exon 15 of HPS1 is generally found in affected individuals who originate from the northwest region of Puerto Rico [16]. Due to a genetic founder effect, the prevalence of HPS-1 in northwest Puerto Rico is approximately 1 per 1800 individuals; 1 in 22 Puerto Ricans in the region is a carrier of this HPS1 variant [41]. Approximately 257 individuals with HPS-1 are reported to be Puerto Rican and tend to be homozygous for the c.1472_1487dup16-bp HPS1 variant; many Puerto Rican individuals with HPS-1 are unreported [34].
Notably, HPS-1 also affects individuals of other ethnicities and nationalities. Approximately 129 non-Puerto Rican individuals with numerous variants in HPS1 have been reported; none of these individuals were homozygous for the c.1472_1487dup16-bp HPS1 variant [34]. Genetic isolates of HPS-1 were reported in Japan and Switzerland [42, 43]. Caucasian, African-American, non-Puerto Rican Latino, European, Middle Eastern, Pakistani, Afghan, Ukrainian, Russian, subcontinental Indian and Chinese individuals with HPS-1 have also been reported [34, 44–48]. Although multiple pathogenic HPS1 variants were identified, genotype–phenotype correlations with pulmonary fibrosis or other disease manifestations in HPS-1 have not been reported.
HPS-2
HPS-2 is associated with biallelic variants in AP3B1, located on chromosome 5q14.1 [25]. AP3B1 encodes the β3A subunit of the AP-3 complex, which is involved with membrane formation and intracellular vesicle trafficking. To date, approximately 35 individuals with HPS-2 have been reported in the literature; their ethnicities are varied [34]. No Puerto Rican cases of HPS-2 have been described. 29 pathogenic variants throughout AP3B1 have been reported and there were no founder mutations or frequently occurring AP3B1 variants [34]. Northern blot analysis from tissues with nonsense variants shows absent AP3B1 transcript, consistent with nonsense-mediated mRNA decay [49]. In addition to neutropenia and immunodeficiency, children or young adults with HPS-2 can develop ILD or pulmonary fibrosis [20, 35, 49, 50].
HPS-4
HPS-4 is associated with biallelic pathogenic variants in the HPS4 (also known as BLOC3S2) gene, located on chromosome 22q12.1 [21]. 32 pathogenic variants located throughout HPS4 have been reported [34]. Almost half of these are nonsense variants and result in truncated HPS4 protein [34]. Approximately 36 individuals with HPS-4 have been reported of various ethnicities, including Ashkenazi-Jewish, European, South Asian, Chinese and Japanese [27, 34]. A c.2089_2093dupAAGCA variant in HPS4 was reported in individuals of European descent [21, 27]. HPS4 contains 14 exons and encodes a 76.9-kDa protein, which interacts with the HPS1 protein in BLOC-3 [37, 38]. Reduced levels of the HPS4 protein destabilise BLOC-3 and result in low levels of HPS1 [45, 51]. Clinical manifestations of HPS-4 resemble those of HPS-1, including progressive pulmonary fibrosis [21].
Pathobiology of HPS
Defective formation of lysosome-related organelles and abnormal intracellular vesicle trafficking are mechanisms that contribute to the clinical manifestations of HPS (figure 2) [22, 52]. Each HPS-causing gene encodes a protein which is a subunit of a cytoplasmic complex involved in these functions. Hetero-oligomeric complexes involved in the pathobiology of HPS include BLOC-1, BLOC-2, BLOC-3 and the AP-3 complex. HPS gene products are ubiquitously expressed, and defects in these cellular processes manifest in various cells and organ systems.
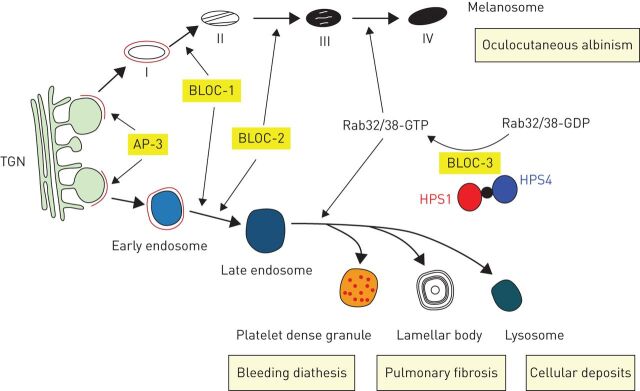
FIGURE 2.
Relationships of protein complexes involved in Hermansky–Pudlak syndrome (HPS), biogenesis of intracellular organelles and clinical manifestations of disease. Four stages (I–IV) of melanosome maturation and platelet δ-granule (dense granule), lamellar body and lysosome formation via the endosomal pathway from the TGN are shown. Defects in these vesicles are associated with oculocutaneous albinism, bleeding diathesis, pulmonary fibrosis and excessive cellular deposits in HPS. Protein complexes associated with HPS, including AP-3, BLOC-1, BLOC-2 and BLOC-3, and a Rab32/38 guanine nucleotide exchange factor comprised of HPS1 and HPS4 protein subunits, are involved in the formation of melanosomes, platelet δ-granules, lamellar bodies and lysosomes. TGN: trans-Golgi network; AP: adaptor protein; BLOC: biogenesis of lysosome-related organelles complex.
Oculocutaneous albinism
Melanosomes are lysosome-related organelles involved in the synthesis and storage of melanin. Melanosomes are found in melanocytes and retinal pigment epithelial cells in the eye, and improper biogenesis of these organelles in HPS causes oculocutaneous albinism. The severity of oculocutaneous albinism is variable and generally dependent upon HPS genetic type [22]. For example, individuals with HPS-1 and HPS-4 typically have pronounced pigment defects. Their skin, hair and eye colour are generally light (figure 1a and b). Visual acuity is poor and many people with HPS-1 are legally blind. In contrast, people with other HPS genetic types have milder oculocutaneous albinism.
Bleeding diathesis
δ-granules are lysosome-related organelles in platelets and their contents (i.e. calcium, ADP, ATP and serotonin) contribute to blood clotting [53]. Specifically, δ-granules are involved in platelet recruitment and the secondary aggregation response, which is abnormal in individuals with platelet δ-granule deficiency. Each platelet generally contains three to eight δ-granules; however, platelets in individuals with HPS are devoid of δ-granules (figure 1c) [54]. The absence of platelet δ-granules in HPS causes easy bruisability and excessive bleeding. Patients with HPS may experience severe or frequent epistaxis, pronounced bleeding with loss of deciduous teeth, menorrhagia in females, haematochezia associated with HPS inflammatory bowel disease and excessive blood loss with clinical biopsies or surgery [55].
Pulmonary fibrosis
In the lung, lamellar bodies in alveolar type II epithelial cells are surfactant-containing lysosome-related organelles, and accumulation of enlarged lamellar bodies in type II cells is a histopathological feature of murine models of HPS and individuals with HPS pulmonary fibrosis [56–58]. Light microscopy analysis of HPS pulmonary fibrosis lung tissue shows foamy-appearing alveolar macrophages and hyperplastic type II cells, and electron microscopy images demonstrate type II cells engorged with several enlarged lamellar bodies. Intracellular ceroid lipofuscin may accumulate in alveolar macrophages, which are found in high concentrations in murine models of HPS and patients with HPS-1 with and without pulmonary fibrosis [19, 59–61]. Foamy alveolar macrophages were also reported in a patient with HPS-5, which is an HPS genetic type that is not known to be associated with pulmonary fibrosis [62].
Macrophages, mast cells and other immune cells may be involved in a distal lung inflammatory response associated with high concentrations of cytokines and chemokines in the alveolar milieu [59–61, 63]. Levels of CCL2, CCL3 (macrophage inflammatory protein-1α) and granulocyte–macrophage colony-stimulating factor are increased in bronchoalveolar lavage (BAL) fluid from patients with HPS-1 with and without pulmonary fibrosis, suggesting that a pro-inflammatory alveolar microenvironment may precede the development of fibrotic lung disease in HPS-1 [61]. Alveolar macrophages isolated from BAL fluid derived from patients with HPS-1 were shown to spontaneously secrete high concentrations of CCL2, CCL3 and CCL5 (RANTES (regulated on activation, normal T-cell expressed and secreted)) [61]. This constitutive activation of HPS-1 alveolar macrophages was downregulated in vitro by pirfenidone, which is an antifibrotic drug approved as treatment for idiopathic pulmonary fibrosis (IPF) [61]. Notably, alterations in the peripheral blood immunome were detected in patients with HPS pulmonary fibrosis, which suggests that dysregulation of the immune system is not restricted to the lung in this disorder [64].
Despite these advances, the mechanisms contributing to HPS pulmonary fibrosis are not fully defined, and it is unclear how intracellular trafficking defects and abnormal biogenesis of lysosome-related organelles cause fibrotic lung disease. It is also unknown why pulmonary fibrosis develops in specific HPS genetic types and not others. However, further investigations into the mechanisms of disease are being facilitated by the development of in vitro type II cell and lung organoid models of HPS, and studies utilising in vivo murine models of HPS and human lung tissue have demonstrated that alveolar type II epithelial cells play a central role in the pathobiology of pulmonary fibrosis [65–68]. Experiments utilising bone marrow transplantation and transgenic type II cell-specific correction of the HPS defect in HPS murine models demonstrated that type II cells are involved with regulation of alveolar macrophage activation and susceptibility to pulmonary fibrosis [67]. In addition, dysregulation of type II cells in murine models of HPS or patients with HPS was reported, including aberrant endoplasmic reticulum stress response, impaired autophagy, defective surfactant secretion and altered phospholipid content [69–72]. Type II cells in HPS also exhibit high expression of CCL2, other cytokines, inducible nitric oxide synthase and galectin-3 [60, 68, 73]. Excessive CCL2 production by type II cells in HPS mice was associated with high concentrations of alveolar macrophages, which produce increased levels of TGF-β, a profibrotic protein. Targeted deletion of CCL2 in type II cells normalised alveolar macrophage concentration, downregulated TGF-β production by macrophages and ameliorated bleomycin-induced pulmonary fibrosis [68]. Galectin-3, a β-galactoside-binding lectin with pleiotropic effects, also has profibrotic effects in HPS, and was shown to promote epithelial apoptosis, fibroblast proliferation and myofibroblast differentiation, and M2-like differentiation of macrophages [74]. In HPS, galectin-3 contributes to exaggerated injury and fibroproliferative repair by altering the effects of chitinase 3-like-1 protein, another mediator of pulmonary fibrosis in HPS [74, 75].
Fibroblasts and myofibroblasts, effector cells capable of secreting extracellular matrix proteins, are not known to contain lysosome-related organelles, but they are involved in the pathogenesis of HPS pulmonary fibrosis. Although the origin of these mesenchymal cells is uncertain, it is postulated that various mechanisms, including epithelial–mesenchymal transformation, proliferation of resident fibroblasts, altered myofibroblast de-differentiation and recruitment of circulating bone marrow-derived fibrocytes, may contribute to expansion of the alveolar interstitial cell population and to maintenance of a profibrotic milieu [76–79]. A cross-sectional study demonstrated high peripheral blood fibrocyte concentrations in patients with HPS pulmonary fibrosis, but not in HPS patients without lung disease or normal controls [79]. A longitudinal study showed that episodic increases in circulating fibrocytes were associated with death from HPS pulmonary fibrosis [79]. These findings indicate that peripheral blood fibrocyte concentration is associated with clinical outcome and suggest that fibrocytes may have a role in the pathobiology of disease. In addition, alterations in levels and activity of matrix metalloproteases in HPS may have a role in dysregulated turnover of extracellular matrix protein in the lung [80].
Clinical features of HPS pulmonary fibrosis
Clinical features
Symptoms of HPS pulmonary fibrosis are similar to those of other fibrotic lung disorders, including IPF. Individuals with HPS pulmonary fibrosis typically present with progressive dyspnoea on exertion or chronic cough [16, 55, 81, 82]. Children with HPS-2 also experience recurrent infections and neutropenia responsive to granulocyte colony-stimulating factor, and may develop spontaneous pneumothorax [17, 20, 35]. Symptoms generally manifest in the fourth decade of life in individuals with HPS-1, in middle-aged adults with HPS-4, or in children or young adults with HPS-2 [16–18, 20, 21, 35, 55, 81]. In contrast, patients with IPF usually present with symptoms of disease when they are older than 50 years of age (table 2) [83–86].
TABLE 2.
Clinical features of Hermansky–Pudlak syndrome (HPS) pulmonary fibrosis and idiopathic pulmonary fibrosis (IPF)
| HPS-1 or HPS-4 pulmonary fibrosis | HPS-2 pulmonary fibrosis | IPF | |
| Onset of pulmonary symptoms | Middle age | Children or young adults | >50 years of age |
| Acute exacerbations | Yes | Unknown | Yes |
| Oculocutaneous albinism | Yes | Yes | No |
| Nystagmus | Yes | Yes | No |
| Excessive bleeding | Yes | Yes | No |
| HRCT scan finding of ground-glass opacification | Yes | Yes | No |
| Type II epithelial cell enlargement | Yes | Yes | No |
| Giant lamellar bodies | Yes | Yes | No |
| Foamy alveolar macrophages | Yes | Unknown | No |
| Ceroid lipofuscin tissue deposition | Yes | Yes | No |
| Pulmonary histopathology | UIP, NSIP, DAD | UIP, NSIP, DIP | UIP |
HRCT: high-resolution computed tomography; UIP: usual interstitial pneumonia; NSIP: nonspecific interstitial pneumonia; DAD: diffuse alveolar damage; DIP: desquamative interstitial pneumonitis.
Physical examination findings include oculocutaneous albinism with variable pigmentation. Horizontal nystagmus, photophobia, iris transillumination and poor visual acuity are present in most patients [55, 82]. Ecchymoses may be found on the extremities, trunk or face. Auscultation of the chest reveals coarse inspiratory bilateral rales initially in the lung bases that progress to involve additional areas. Acrocyanosis and digital clubbing may be found in individuals with severe lung disease.
Lung function testing
Consistent with pulmonary function testing measurements in patients with fibrosing lung disease, lung function values in individuals with HPS pulmonary fibrosis have a broad range and typically correlate with severity of disease [18]. Patients with early HPS pulmonary fibrosis may have normal values. Spirometry in symptomatic patients may show reduced forced vital capacity (FVC) with normal airflow; individuals with coexisting asthma may have small or large airways airflow obstruction responding to an inhaled bronchodilator. Lung volume measurements in individuals with HPS pulmonary fibrosis generally show restriction; diffusing capacity of the lung for carbon monoxide (DLCO) is typically reduced [18, 55]. FVC, forced expiratory volume in 1 s, total lung capacity, vital capacity and DLCO can decrease to similar extents in affected patients [18]. Rate of decline in lung function may initially vary in patients with mild HPS pulmonary fibrosis [87]. However, serial pulmonary function tests in some patients with severe disease receiving placebo in a clinical trial demonstrated progression of disease, with 12–15% annual rates of decline in FVC % pred values [88]. Reduced oxygen saturation with exertion or at rest may be found in patients with severe HPS pulmonary fibrosis [55, 81].
Imaging
HPS pulmonary fibrosis and IPF have some common radiographic features, but some of their findings differ (table 2). In patients with HPS pulmonary fibrosis, chest imaging with conventional or high-resolution computed tomography (HRCT) scans is more sensitive than using chest radiographs; individuals with mild findings of HPS pulmonary fibrosis on HRCT scans had normal findings on chest radiographs [19]. Bilateral reticulonodular interstitial infiltrates, fibrosis and pleural thickening can be found on chest radiographs (figure 1d). Conventional or HRCT scan findings in patients with HPS pulmonary fibrosis can include bilateral reticulations and septal thickening predominantly involving basilar subpleural regions of the lung in early disease and diffusely involving the lung parenchyma in severe disease (figure 3). Other HRCT scan findings include peri-bronchovascular thickening, traction bronchiectasis and honeycombing. Ground-glass opacities, which are generally atypical in IPF, are found in HRCT scan images of patients with HPS pulmonary fibrosis. In a cohort of six children with HPS-2, ground-glass opacities were found in all initial CT scans [35]. Analyses of HPS pulmonary fibrosis HRCT imaging findings and pulmonary function values showed that radiographic scores correlate inversely with FVC [19].
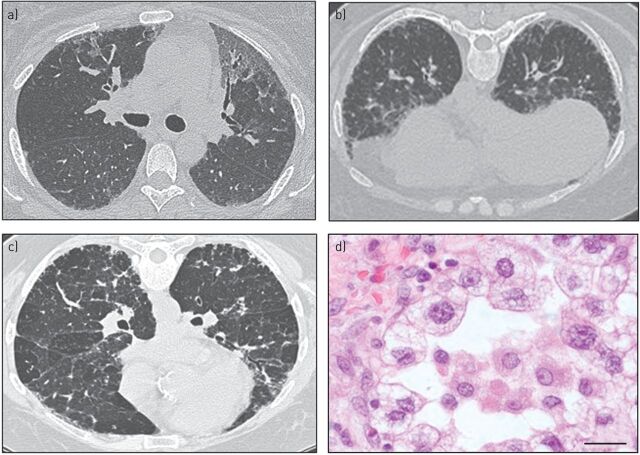
FIGURE 3.
Computed tomography (CT) scan and histopathological images of Hermansky–Pudlak syndrome (HPS) pulmonary fibrosis. a) Supine and b) prone CT scan images of a 47-year-old subject with moderate HPS pulmonary fibrosis show bilateral ground-glass opacities, reticulations and honeycombing. c) CT scan image of a 38-year-old subject with HPS pulmonary fibrosis demonstrates bilateral ground-glass opacities, traction bronchiectasis, reticulations and honeycombing. d) Aggregates of foamy alveolar macrophages, vacuolated hyperplastic type II alveolar epithelial cells containing enlarged lamellar bodies, and interstitial accumulation of cells and extracellular matrix are found in lung tissue from a subject with HPS pulmonary fibrosis. Haematoxylin and eosin staining. Scale bar: 20 μm.
Histopathology
Some histopathology features of HPS pulmonary fibrosis are found in other fibrosing lung disorders, but there are some distinctive histological findings of HPS pulmonary fibrosis. Thickening of the interalveolar septa and alveolar interstitium due to accumulation of extracellular matrix proteins, immune cells, fibroblasts and myofibroblasts is found in HPS pulmonary fibrosis and IPF. In addition, type II cell hyperplasia, fibroblastic foci and temporal heterogeneity are histological features of both disorders [89]. Enlargement of airspaces due to cystic destruction of lung parenchyma and dense fibrosis can also be seen in HPS pulmonary fibrosis and IPF. Usual interstitial pneumonia, a histological hallmark of IPF, and nonspecific interstitial pneumonia histological patterns were reported in patients with HPS-1 and HPS-2; desquamative interstitial pneumonitis was reported in children with HPS-2 [35, 84, 89–93]. However, foamy-appearing alveolar macrophages that sometimes contain ceroid lipofuscin deposits and vacuolated type II cells with enlarged lamellar bodies are characteristics of HPS pulmonary fibrosis (figure 3). Electron microscopy imaging of lung tissue can show multiple giant lamellar bodies in type II cells [58].
Natural history of disease
HPS pulmonary fibrosis is a chronic progressive ILD that often culminates in lung transplantation or death due to respiratory failure, typically in middle-aged adults with HPS-1 or HPS-4, or in children and young adults with HPS-2. Natural history of disease data from individuals with HPS-1 show that pulmonary fibrosis affecting middle-aged adults progresses at variable rates [88]. Cross-sectional analysis of FVC measurements versus age at 5-year intervals demonstrated a bimodal distribution in a cohort of individuals with HPS. Nadirs of FVC were found in patients with HPS at ages 36–40 and 56–60 years, suggesting that some patients progress at an earlier age, and hence more rapidly, than others [16]. However, longitudinal studies comparing rates of disease progression in individuals with HPS pulmonary fibrosis based on age of disease onset are not reported. Data from subjects with HPS pulmonary fibrosis randomised to receive placebo in clinical trials investigating pirfenidone as treatment showed that individuals with mild or moderate disease have inconsistent rates of disease progression [87, 88]. Approximate survival of three individuals 37–47 years of age with severe disease was <20 months after reaching a FVC of 50% predicted [88]. Rapid progression of fibrosis on HRCT scans was reported in children with HPS-2 [35]. Lung transplantations were performed in patients with severe HPS-1 at 27–57 years of age [90, 94–98]. Acute exacerbations of pulmonary fibrosis associated with rapid worsening of dyspnoea, decline in lung function and development of diffuse ground-glass opacities on HRCT scan were reported in some individuals with HPS-1 and HPS-4 [89, 90, 94, 99]. Histopathology of explanted tissue from a lung transplant recipient with HPS-1 who experienced an acute exacerbation revealed usual interstitial pneumonia with diffuse alveolar damage [90].
Diagnosis, management and treatment of HPS pulmonary fibrosis
Diagnosis
The diagnosis of HPS is established in an individual with oculocutaneous albinism and an increased tendency to bleed or easy bruisability who has pathogenic biallelic variants in genes associated with HPS. Targeted genetic sequencing or next-generation sequencing is emerging as a method to identify genetic variants and diagnose HPS in patients with clinical manifestations of disease [34, 47, 62, 100, 101]. Platelet whole-mount electron microscopy demonstrating absent δ-granules is consistent with HPS [16, 54, 82, 102, 103]. Although platelet electron microscopy is used to diagnose HPS, this test requires specialised expertise and is available at limited clinical laboratories [82, 102]. Pulmonary fibrosis in individuals with HPS is diagnosed by CT scan findings. Given the high prevalence of pulmonary fibrosis in HPS, lung biopsy is usually not recommended to establish a diagnosis of HPS pulmonary fibrosis and is relatively contraindicated due to patients' increased tendency to bleed [102]. Although foamy alveolar macrophages are found in patients with HPS, there is generally no role for bronchoscopy in diagnosing HPS pulmonary fibrosis.
Clinical management
Clinical management involves preventive care for asymptomatic individuals with HPS genetic types associated with pulmonary fibrosis, supportive care for those with symptomatic HPS pulmonary fibrosis and lung transplantation for patients with severe disease [55]. Genetic counselling may be beneficial for families affected with HPS.
Individuals with HPS-1, HPS-2, HPS-4 and possibly HPS-10 are at risk for development of pulmonary fibrosis. Avoidance of respiratory irritants, including smoke inhalation, is recommended. Routine maintenance of health, including regular exercise, balanced nutrition, proper weight management, treatment of comorbid illness, and vaccinations against influenza and pneumococcus, is recommended. Lung transplantation is a viable option for individuals with severe HPS pulmonary fibrosis and optimisation of each patient's candidacy as a potential transplant recipient should be pursued throughout their lives [94]. Minimising the risk of skin cancer by avoiding the sun or using high-calibre sunblock as well as routine dermatology evaluations to screen for skin cancer and to remove suspicious lesions are recommended [55, 104]. Alloimmunisation is another potential barrier to lung transplantation for some patients with an increased bleeding tendency [94]. To minimise alloimmunisation, it is preferable to use procoagulant drugs to prevent or treat haemorrhage for mild bleeding if possible. For patients who require platelet or blood transfusion, irradiated single-donor leukoreduced platelets are recommended and, in some instances, human leukocyte antigen-matched platelets may be indicated [94].
Patients with symptomatic HPS pulmonary fibrosis may benefit from pulmonary rehabilitation or supplemental oxygen for hypoxaemia [55]. A 6-min walk test using a portable oximeter should be considered as hypoxaemia may be detected only during exertion in patients with mild HPS pulmonary fibrosis. Overnight pulse oximetry measurements are recommended in patients with moderate HPS pulmonary fibrosis to detect nocturnal hypoxaemia during sleep.
Medical treatment
No medications are currently approved by the US Food and Drug Administration as treatment for HPS pulmonary fibrosis. Corticosteroid drugs have not been shown to be effective and are not recommended for therapy [81]. Two clinical trials investigating pirfenidone, an oral antifibrotic drug approved as treatment for IPF, have been conducted [87, 88, 105–107]. Pirfenidone inhibits TGF-β, and incubation of alveolar macrophages from patients with HPS-1 with pirfenidone significantly reduced inflammatory cytokine secretion and downregulated their constitutive activation [61, 108–110]. The first randomised, placebo-controlled trial showed that pirfenidone slowed the rate of lung function decline in a subset of subjects with mild or moderate HPS pulmonary fibrosis [88]. A second trial was conducted to study the efficacy of pirfenidone in subjects with mild or moderate disease [87]. This randomised, placebo-controlled trial was stopped due to futility and hence was unable to determine whether or not pirfenidone is an effective treatment for HPS pulmonary fibrosis. Pirfenidone was tolerated by most subjects enrolled in these trials, but taken together, results regarding efficacy were inconclusive [87, 88]. Notably, three subjects enrolled in the first protocol elected to receive open-label pirfenidone for several years and longitudinal analyses demonstrated that pirfenidone may have ameliorated their HPS pulmonary fibrosis [111]. Currently, pirfenidone is not approved as treatment for HPS pulmonary fibrosis.
Nintedanib, a tyrosine kinase inhibitor, is an antifibrotic drug approved as treatment for IPF, ILD associated with systemic sclerosis or chronic fibrosing ILD with a progressive phenotype [112–116]. Clinical trials showed that nintedanib reduced the rate of FVC decline in patients with any of these conditions compared with placebo [112–114]. A potential adverse effect of nintedanib is bleeding, which is a theoretical concern for patients with HPS who may experience excessive bleeding due to platelet dysfunction [16, 17]. Although nintedanib is not specifically approved as treatment for HPS pulmonary fibrosis, nintedanib is approved as treatment for patients with progressive fibrotic lung disease caused by different underlying conditions [114, 115].
Lung transplantation
Despite an increased tendency to bleed, patients with HPS pulmonary fibrosis have successfully undergone single- or double-lung transplantation [90–95]. Pre-transplant multidisciplinary planning involves early referral to a regional transplant centre. Consultation with a haematologist is recommended to determine an appropriate management plan to prevent and treat bleeding. Therapeutic options include procoagulant drugs (e.g. desmopressin and aminocaproic acid) and platelet transfusions, and plans should be individualised based on the severity of each patient's platelet dysfunction and their response to procoagulant medications. Consultation with a gastroenterologist is recommended for individuals with coexisting inflammatory bowel disease. Patients with HPS pulmonary fibrosis have progressive disease and mechanical ventilation can be used as a temporising supportive measure in lung transplant candidates with respiratory failure. Extracorporeal membrane oxygenation with full anticoagulation was also successfully employed in patients with end-stage HPS pulmonary fibrosis who were actively listed for lung transplant [90, 94, 97, 98]. Lung transplant recipients with HPS should receive standard of care post-transplant, including immunosuppressive medications and surveillance bronchoscopies with biopsies [94]. However, patients undergoing endoscopic biopsies may need prophylactic treatment against bleeding. Recurrence of pulmonary fibrosis in lung transplant recipients with underlying HPS has not been reported [94].
Future therapy
Future therapy for HPS pulmonary fibrosis may involve antifibrotic drugs or novel approaches to treatment. Antifibrotic therapies are being studied in clinical trials as treatment for IPF and pulmonary fibrosis associated with other underlying conditions, and these drugs are potential candidate medications to investigate as treatment for HPS pulmonary fibrosis. In addition, patients with HPS-1 have variants in the same gene (i.e. HPS1) and many patients originating from Puerto Rico are homozygous for the same c.1472_1487dup16-bp HPS1 variant. Thus, gene therapy and gene editing are potential treatments for HPS. A pre-clinical proof-of-principle study showed that the HPS1 defect in dermal melanocytes from patients with HPS-1 was corrected by transducing the cells with a lentiviral vector containing an HPS1 construct [117]. After transduction, the HPS-1 melanocytes expressed HPS1 protein and pelleted cells became darker, thereby showing molecular and functional correction of the HPS1 gene. Another pre-clinical study involving fibroblasts demonstrated that high levels of galectin-3, a profibrotic protein, in HPS-1 lung fibroblasts normalised following transfection with an HPS1 construct [73]. Furthermore, in vivo transgenic correction of Ap3b1 in type II epithelial cells in mice with an HPS-2 defect conferred protection from bleomycin-induced pulmonary fibrosis [67]. Other investigators demonstrated that gene editing with Streptococcus pyogenes Cas9 nuclease corrected the c.1472_1487dup16-bp HPS1 microduplication variant in HPS-1 B-lymphoblastoid cells [118]. These promising proof-of-principle results suggest that gene therapy and gene editing are possible strategies as future treatment for HPS pulmonary fibrosis.
Conclusions
HPS pulmonary fibrosis is a rare autosomal recessive disorder with an enigmatic and complex pathogenesis of disease. Investigations into the pathobiology of HPS pulmonary fibrosis are facilitated by the availability of in vitro and in vivo pre-clinical models of disease. Pulmonary fibrosis develops in individuals with HPS-1, HPS-2 or HPS-4 and is highly prevalent in individuals with HPS-1, who have pathogenic biallelic variants in HPS1. Given these unique attributes, HPS pulmonary fibrosis serves as a model for studying fibrotic lung disorders and fibrosis in general.
Acknowledgements
We thank our patients who participated in our programme.
Footnotes
Number 4 in the Series “Rare genetic interstitial lung diseases” Edited by Bruno Crestani and Raphaël Borie
Previous articles in the Series: No. 1: Daccord C, Good J-M, Morren M-A, et al. Brit–Hogg–Dubé syndrome. Eur Respir Rev 2020; 29: 200042. No. 2: Hadchouel A, Drummond D, Abou Taam R, et al. Alveolar proteinosis of genetic origins. Eur Respir Rev 2020; 29: 200187. No. 3: Cazzato S, Omenetti A, Ravaglia C, et al. Lung involvement in monogenetic interferonopathies. Eur Respir Rev 2020; 29: 200001.
Provenance: Commissioned article, peer reviewed.
Conflict of interest: T. Yokoyama has nothing to disclose.
Conflict of interest: B.R. Gochuico has nothing to disclose.
Support statement: This study was supported in part by the Intramural Research Program, National Human Genome Research Institute, National Institutes of Health (NIH). The NIH had no role in writing the manuscript. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. N Engl J Med 2018; 378: 1811–1823. doi: 10.1056/NEJMra1705751 [DOI] [PubMed] [Google Scholar]
- 2.Martinez FJ, Collard HR, Pardo A, et al. Idiopathic pulmonary fibrosis. Nat Rev Dis Primers 2017; 3: 17074–17093. doi: 10.1038/nrdp.2017.74 [DOI] [PubMed] [Google Scholar]
- 3.Richeldi L, Collard HR, Jones MG. Idiopathic pulmonary fibrosis. Lancet 2017; 389: 1941–1952. doi: 10.1016/S0140-6736(17)30866-8 [DOI] [PubMed] [Google Scholar]
- 4.Wynn TA. Integrating mechanisms of pulmonary fibrosis. J Exp Med 2011; 208: 1339–1350. doi: 10.1084/jem.20110551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sisson TH, Mendez M, Choi K, et al. Targeted injury of type II alveolar epithelial cells induces pulmonary fibrosis. Am J Respir Crit Care Med 2010; 181: 254–263. doi: 10.1164/rccm.200810-1615OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faner R, Rojas M, Macnee W, et al. Abnormal lung aging in chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2012; 186: 306–313. doi: 10.1164/rccm.201202-0282PP [DOI] [PubMed] [Google Scholar]
- 7.Kropski JA, Blackwell TS. Endoplasmic reticulum stress in the pathogenesis of fibrotic disease. J Clin Invest 2018; 128: 64–73. doi: 10.1172/JCI93560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheresh P, Kim S, Tulasirum S, et al. Oxidative stress and pulmonary fibrosis. Biochim Biophys Acta 2013; 1832: 1028–1040. doi: 10.1016/j.bbadis.2012.11.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malsin ES, Kamp DW. The mitochondria in lung fibrosis: friend or foe? Transl Res 2018; 202: 1–23. doi: 10.1016/j.trsl.2018.05.005 [DOI] [PubMed] [Google Scholar]
- 10.Romero F, Summer R. Protein folding and the challenges of maintaining endoplasmic reticulum proteostasis in idiopathic pulmonary fibrosis. Ann Am Thorac Soc 2017; 14: S410–S413. doi: 10.1513/AnnalsATS.201703-207AW [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishi Y, Sano H, Kawashima T, et al. Role of galectin-3 in human pulmonary fibrosis. Allergol Int 2007; 56: 57–65. doi: 10.2332/allergolint.O-06-449 [DOI] [PubMed] [Google Scholar]
- 12.Strikoudis A, Cieślak A, Loffredo L, et al. Modeling of fibrotic lung disease using 3D organoids derived from human pluripotent stem cells. Cell Rep 2019; 27: 3709–3723. doi: 10.1016/j.celrep.2019.05.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borie R, Le Guen P, Ghanem M, et al. The genetics of interstitial lung diseases. Eur Respir Rev 2019; 28: 190053. doi: 10.1183/16000617.0053-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Courtwright AM, El-Chemaly S. Telomeres in interstitial lung disease: the short and the long of it. Ann Am Thorac Soc 2019; 16: 175–181. doi: 10.1513/AnnalsATS.201808-508CME [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Savage SA. Dyskeratosis congenita. In: Adam MP, Ardinger HH, Pagon RA, et al., eds. GeneReviews [Internet]. Seattle, University of Washington, 2019. [Google Scholar]
- 16.Gahl WA, Brantly M, Kaiser-Kupfer MI, et al. Genetic defects and clinical characteristics of patients with a form of oculocutaneous albinism (Hermansky–Pudlak syndrome). N Engl J Med 1998; 338: 1258–1264. doi: 10.1056/NEJM199804303381803 [DOI] [PubMed] [Google Scholar]
- 17.Huizing M, Malicdan MCV, Gochuico BR, et al. Hermansky–Pudlak syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al., eds. GeneReviews [Internet]. Seattle, University of Washington, 2017. [Google Scholar]
- 18.Brantly M, Avila NA, Shotelersuk V, et al. Pulmonary function and high-resolution CT findings in patients with an inherited form of pulmonary fibrosis, Hermansky–Pudlak syndrome, due to mutations in HPS-1. Chest 2000; 117: 129–136. doi: 10.1378/chest.117.1.129 [DOI] [PubMed] [Google Scholar]
- 19.Avila NA, Brantly M, Premkumar A, et al. Hermansky–Pudlak syndrome: radiography and CT of the chest compared with pulmonary function tests and genetic studies. AJR Am J Roentgenol 2002; 179: 887–892. doi: 10.2214/ajr.179.4.1790887 [DOI] [PubMed] [Google Scholar]
- 20.Gochuico BR, Huizing M, Golas GA, et al. Interstitial lung disease and pulmonary fibrosis in Hermansky–Pudlak syndrome type 2, an adaptor protein-3 complex disease. Mol Med 2012; 18: 56–64. doi: 10.2119/molmed.2011.00198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson PD, Huizing M, Claassen DA, et al. Hermansky–Pudlak syndrome type 4 (HPS-4): clinical and molecular characteristics. Hum Genet 2003; 113: 10–17. doi: 10.1007/s00439-003-0933-5 [DOI] [PubMed] [Google Scholar]
- 22.Huizing M, Gochuico BR, Gahl WA, et al. Molecular genetics of Hermansky–Pudlak syndrome. eLS 2017; 2017: 1–10. doi: 10.1002/9780470015902.a0024328.pub2 [DOI] [Google Scholar]
- 23.Hussain N, Quezado M, Huizing M, et al. Intestinal disease in Hermansky–Pudlak syndrome: occurrence of colitis and relation to genotype. Clin Gastroenterol Hepatol 2006; 4: 73–80. doi: 10.1016/S1542-3565(05)00858-X [DOI] [PubMed] [Google Scholar]
- 24.Hermansky F, Pudlak P. Albinism associated with hemorrhagic diathesis and unusual pigmented reticular cells in the bone marrow: report of two cases with histochemical studies. Blood 1959; 14: 162–169. doi: 10.1182/blood.V14.2.162.162 [DOI] [PubMed] [Google Scholar]
- 25.Dell'Angelica EC, Shotelersuk V, Aguilar RC, et al. Altered trafficking of lysosomal proteins in Hermansky–Pudlak syndrome due to mutations in the β3A subunit of the AP-3 adaptor. Mol Cell 1999; 3: 11–21. doi: 10.1016/S1097-2765(00)80170-7 [DOI] [PubMed] [Google Scholar]
- 26.Anikster Y, Huizing M, White J, et al. Mutation of a new gene causes a unique form of Hermansky–Pudlak syndrome in a genetic isolate of central Puerto Rico. Nat Genet 2001; 28: 376–380. doi: 10.1038/ng576 [DOI] [PubMed] [Google Scholar]
- 27.Suzuki T, Li W, Zhang Q, et al. Hermansky–Pudlak syndrome is caused by mutations in HPS4, the human homolog of the mouse light-ear gene. Nat Genet 2002; 30: 321–324. doi: 10.1038/ng835 [DOI] [PubMed] [Google Scholar]
- 28.Zhang Q, Zhao B, Li W, et al. Ru2 and Ru encode mouse orthologs of the genes mutated in human Hermansky–Pudlak syndrome types 5 and 6. Nat Genet 2003; 33: 145–153. doi: 10.1038/ng1087 [DOI] [PubMed] [Google Scholar]
- 29.Huizing M, Pederson B, Hess RA, et al. Clinical and cellular characterisation of Hermansky–Pudlak syndrome type 6. J Med Genet 2009; 46: 803–810. doi: 10.1136/jmg.2008.065961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li W, Zhang Q, Oiso N, et al. Hermansky–Pudlak syndrome type 7 (HPS-7) results from mutant dysbindin, a member of the biogenesis of lysosome-related organelles complex 1 (BLOC-1). Nat Genet 2003; 35: 84–89. doi: 10.1038/ng1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morgan NV, Pasha S, Johnson CA, et al. A germline mutation in BLOC1S3/Reduced pigmentation causes a novel variant of Hermansky–Pudlak syndrome (HPS8). Am J Hum Genet 2006; 78: 160–166. doi: 10.1086/499338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Badolato R, Prandini A, Caracciolo S, et al. Exome sequencing reveals a pallidin mutation in a Hermansky–Pudlak-like primary immunodeficiency syndrome. Blood 2012; 119: 3185–3187. doi: 10.1182/blood-2012-01-404350 [DOI] [PubMed] [Google Scholar]
- 33.Ammann S, Schulz A, Krägeloh-Mann I, et al. Mutations in AP3D1 associated with immunodeficiency and seizures define a new type of Hermansky–Pudlak syndrome. Blood 2016; 127: 997–1006. doi: 10.1182/blood-2015-09-671636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huizing M, Malicdan MCV, Wang JA, et al. Hermansky–Pudlak syndrome: mutation update. Hum Mutat 2020; 41: 543–580. doi: 10.1002/humu.23968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hengst M, Naehrlich L, Mahavadi P, et al. Hermansky–Pudlak syndrome type 2 manifests with fibrosing lung disease early in childhood. Orphanet J Rare Dis 2018; 13: 42. doi: 10.1186/s13023-018-0780-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oh J, Bailin T, Fukai K, et al. Positional cloning of a gene for Hermansky–Pudlak syndrome, a disorder of cytoplasmic organelles. Nat Genet 1996; 14: 300–306. doi: 10.1038/ng1196-300 [DOI] [PubMed] [Google Scholar]
- 37.Martina JA, Moriyama K, Bonifacino JS. BLOC-3, a protein complex containing the Hermansky–Pudlak syndrome gene products HPS1 and HPS4. J Biol Chem 2003; 278: 29376–29384. doi: 10.1074/jbc.M301294200 [DOI] [PubMed] [Google Scholar]
- 38.Carmona-Rivera C, Simeonov DR, Cardillo ND, et al. A divalent interaction between HPS1 and HPS4 is required for the formation of the biogenesis of lysosome-related organelle complex-3 (BLOC-3). Biochim Biophys Acta 2013; 1833: 468–478. doi: 10.1016/j.bbamcr.2012.10.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gerondopoulos A, Langemeyer L, Liang J, et al. BLOC-3 mutated in Hermansky–Pudlak syndrome is a Rab32/38 guanine nucleotide exchange factor. Curr Biol 2012; 22: 2135–2139. doi: 10.1016/j.cub.2012.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ohishi Y, Kinoshita R, Marubashi S, et al. The BLOC-3 subunit HPS4 is required for activation of Rab32/38 GTPases in melanogenesis, but its Rab9 activity is dispensable for melanogenesis. J Biol Chem 2019; 294: 6912–6922. doi: 10.1074/jbc.RA119.007345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Witkop CJ, Nuñez Babcock M, Rao GH, et al. Albinism and Hermansky–Pudlak syndrome in Puerto Rico. Bol Asoc Med P R 1990; 82: 333–339. [PubMed] [Google Scholar]
- 42.Ito S, Suzuki T, Inagaki K, et al. High frequency of Hermansky–Pudlak syndrome type 1 (HPS1) among Japanese albinism patients and functional analysis of HPS1 mutant protein. J Invest Dermatol 2005; 125: 715–720. doi: 10.1111/j.0022-202X.2005.23884.x [DOI] [PubMed] [Google Scholar]
- 43.Schallreuter KU, Frenk E, Wolfe LS, et al. Hermansky–Pudlak syndrome in a Swiss population. Dermatology 1993; 187: 248–256. doi: 10.1159/000247258 [DOI] [PubMed] [Google Scholar]
- 44.Merideth MA, Vincent LM, Sparks SE, et al. Hermansky–Pudlak syndrome in two African-American brothers. Am J Med Genet A 2009; 149A: 987–992. doi: 10.1002/ajmg.a.32757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carmona-Rivera C, Golas G, Hess RA, et al. Clinical, molecular, and cellular features of non-Puerto Rican Hermansky–Pudlak syndrome patients of Hispanic descent. J Invest Dermatol 2011; 131: 2394–2400. doi: 10.1038/jid.2011.228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vincent LM, Adams D, Hess RA, et al. Hermansky–Pudlak syndrome type 1 in patients of Indian descent. Mol Genet Metab 2009; 97: 227–233. doi: 10.1016/j.ymgme.2009.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wei A, Yuan Y, Bai D, et al. NGS-based 100-gene panel of hypopigmentation identifies mutations in Chinese Hermansky–Pudlak syndrome patients. Pigment Cell Melanoma Res 2016; 29: 702–706. doi: 10.1111/pcmr.12534 [DOI] [PubMed] [Google Scholar]
- 48.Power B, Ferreira CR, Chen D, et al. Hermansky–Pudlak syndrome and oculocutaneous albinism in Chinese children with pigmentation defects and easy bruising. Orphanet J Rare Dis 2019; 14: 52. doi: 10.1186/s13023-019-1023-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huizing M, Scher CD, Strovel E, et al. Nonsense mutations in ADTB3A cause complete deficiency of the β3A subunit of adaptor complex-3 and severe Hermansky–Pudlak syndrome type 2. Pediatr Res 2002; 51: 150–158. doi: 10.1203/00006450-200202000-00006 [DOI] [PubMed] [Google Scholar]
- 50.Gil-Krzewska A, Murakami Y, Peruzzi G, et al. Natural killer cell activity and dysfunction in Hermansky–Pudlak syndrome. Br J Haematol 2017; 176: 118–123. doi: 10.1111/bjh.14390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wei A, Yuan Y, Qi Z, et al. Instability of BLOC-2 and BLOC-3 in Chinese patients with Hermansky–Pudlak syndrome. Pigment Cell Melanoma Res 2019; 32: 373–380. doi: 10.1111/pcmr.12748 [DOI] [PubMed] [Google Scholar]
- 52.Huizing M, Helip-Wooley A, Westbroek W, et al. Disorders of lysosome-related organelle biogenesis: clinical and molecular genetics. Annu Rev Genomics Hum Genet 2008; 9: 359–386. doi: 10.1146/annurev.genom.9.081307.164303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gunay-Aygun M, Huizing M, Gahl WA. Molecular defects that affect platelet dense granules. Semin Thromb Hemost 2004; 30: 537–547. doi: 10.1055/s-2004-835674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Witkop CJ, Krumwiede M, Sedano H, et al. Reliability of absent platelet dense bodies as a diagnostic criterion for Hermansky–Pudlak syndrome. Am J Hematol 1987; 26: 305–311. doi: 10.1002/ajh.2830260403 [DOI] [PubMed] [Google Scholar]
- 55.Seward SL Jr, Gahl WA. Hermansky–Pudlak syndrome: health care throughout life. Pediatrics 2013; 132: 153–160. doi: 10.1542/peds.2012-4003 [DOI] [PubMed] [Google Scholar]
- 56.Lyerla TA, Rusiniak ME, Borchers M, et al. Aberrant lung structure, composition, and function in a murine model of Hermansky–Pudlak syndrome. Am J Physiol Lung Cell Mol Physiol 2003; 285: L643–L653. doi: 10.1152/ajplung.00024.2003 [DOI] [PubMed] [Google Scholar]
- 57.Wang L, Lyerla T. Histochemical and cellular changes accompanying the appearance of lung fibrosis in an experimental mouse model for Hermansky Pudlak syndrome. Histochem Cell Biol 2010; 134: 205–213. doi: 10.1007/s00418-010-0724-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nakatani Y, Nakamura N, Sano J, et al. Interstitial pneumonia in Hermansky–Pudlak syndrome: significance of florid foamy swelling/degeneration (giant lamellar body degeneration) of type-2 pneumocytes. Virchows Arch 2000; 437: 304–313. doi: 10.1007/s004280000241 [DOI] [PubMed] [Google Scholar]
- 59.Young LR, Borchers MT, Allen HL, et al. Lung-restricted macrophage activation in the pearl mouse model of Hermansky–Pudlak syndrome. J Immunol 2006; 176: 4361–4368. doi: 10.4049/jimmunol.176.7.4361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Atochina-Vasserman EN, Bates SR, Zhang P, et al. Early alveolar epithelial dysfunction promotes lung inflammation in a mouse model of Hermansky–Pudlak syndrome. Am J Respir Crit Care Med 2011; 184: 449–458. doi: 10.1164/rccm.201011-1882OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rouhani FN, Brantly ML, Markello TC, et al. Alveolar macrophage dysregulation in Hermansky–Pudlak syndrome type 1. Am J Respir Crit Care Med 2009; 180: 1114–1121. doi: 10.1164/rccm.200901-0023OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stephen J, Yokoyama T, Tolman NJ, et al. Cellular and molecular defects in a patient with Hermansky–Pudlak syndrome type 5. PLoS One 2017; 12: e0173682. doi: 10.1371/journal.pone.0173682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kirshenbaum AS, Cruse G, Desai A, et al. Immunophenotypic and ultrastructural analysis of mast cells in Hermansky–Pudlak syndrome type-1: a possible connection to pulmonary fibrosis. PLoS One 2016; 11: e0159177. doi: 10.1371/journal.pone.0159177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.El-Chemaly S, Cheung F, Kotliarov Y, et al. The immunome in two inherited forms of pulmonary fibrosis. Front Immunol 2018; 9: 76. doi: 10.3389/fimmu.2018.00076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kook S, Qi A, Wang P, et al. Gene-edited MLE-15 cells as a model for the Hermansky–Pudlak syndromes. Am J Respir Cell Mol Biol 2018; 58: 566–574. doi: 10.1165/rcmb.2017-0324MA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Korogi Y, Gotoh S, Ikeo S, et al. In vitro disease modeling of Hermansky–Pudlak syndrome type 2 using human induced pluripotent stem cell-derived alveolar organoids. Stem Cell Reports 2019; 12: 431–440. doi: 10.1016/j.stemcr.2019.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Young LR, Gulleman PM, Bridges JP, et al. The alveolar epithelium determines susceptibility to lung fibrosis in Hermansky–Pudlak syndrome. Am J Respir Crit Care Med 2012; 186: 1014–1024. doi: 10.1164/rccm.201207-1206OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Young LR, Gulleman PM, Short CW, et al. Epithelial–macrophage interactions determine pulmonary fibrosis susceptibility in Hermansky–Pudlak syndrome. JCI Insight 2016; 1: e88947. doi: 10.1172/jci.insight.88947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mahavadi P, Korfei M, Henneke I, et al. Epithelial stress and apoptosis underlie Hermansky–Pudlak syndrome-associated interstitial pneumonia. Am J Respir Crit Care Med 2010; 182: 207–219. doi: 10.1164/rccm.200909-1414OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ahuja S, Knudsen L, Chillappagari S, et al. MAP1LC3B overexpression protects against Hermansky–Pudlak syndrome type-1-induced defective autophagy in vitro. Am J Physiol Lung Cell Mol Physiol 2016; 310: L519–L531. doi: 10.1152/ajplung.00213.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guttentag SH, Akhtar A, Tao JQ, et al. Defective surfactant secretion in a mouse model of Hermansky–Pudlak syndrome. Am J Respir Cell Mol Biol 2005; 33: 14–21. doi: 10.1165/rcmb.2004-0293OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kook S, Wang P, Young LR, et al. Impaired lysosomal integral membrane protein 2-dependent peroxiredoxin 6 delivery to lamellar bodies accounts for altered alveolar phospholipid content in adaptor protein-3-deficient pearl mice. J Biol Chem 2016; 291: 8414–8427. doi: 10.1074/jbc.M116.720201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cullinane AR, Yeager C, Dorward H, et al. Dysregulation of galectin-3. Implications for Hermansky–Pudlak syndrome pulmonary fibrosis. Am J Respir Cell Mol Biol 2014; 50: 605–613. doi: 10.1165/rcmb.2013-0025OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhou Y, He CH, Yang DS, et al. Galectin-3 interacts with the CHI3L1 axis and contributes to Hermansky–Pudlak syndrome lung disease. J Immunol 2018; 200: 2140–2153. doi: 10.4049/jimmunol.1701442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhou Y, He CH, Herzog EL, et al. Chitinase 3-like-1 and its receptors in Hermansky–Pudlak syndrome-associated lung disease. J Clin Invest 2015; 125: 3178–3192. doi: 10.1172/JCI79792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Iwano M, Plieth D, Danoff TM, et al. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J Clin Invest 2002; 110: 341–350. doi: 10.1172/JCI0215518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Willis BC, Liebler JM, Luby-Phelps K, et al. Induction of epithelial-mesenchymal transition in alveolar epithelial cells by transforming growth factor-β1: potential role in idiopathic pulmonary fibrosis. Am J Pathol 2005; 166: 1321–1332. doi: 10.1016/S0002-9440(10)62351-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kato K, Logsdon NJ, Shin YJ, et al. Impaired myofibroblast dedifferentiation contributes to non-resolving fibrosis in aging. Am J Respir Cell Mol Biol 2020; 62: 633–644. doi: 10.1165/rcmb.2019-0092OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Trimble A, Gochuico BR, Markello TC, et al. Circulating fibrocytes as biomarker of prognosis in Hermansky–Pudlak syndrome. Am J Respir Crit Care Med 2014; 190: 1395–1401. doi: 10.1164/rccm.201407-1287OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Summer R, Krishna R, Schriner D, et al. Matrix metalloproteinase activity in the lung is increased in Hermansky–Pudlak syndrome. Orphanet J Rare Dis 2019; 14: 162. doi: 10.1186/s13023-019-1143-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Vicary GW, Vergne Y, Santiago-Cornier A, et al. Pulmonary fibrosis in Hermansky–Pudlak syndrome. Ann Am Thorac Soc 2016; 13: 1839–1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.De Jesus Rojas W, Young LR. Hermansky–Pudlak syndrome. Semin Respir Crit Care Med 2020; 41: 238–246. doi: 10.1055/s-0040-1708088 [DOI] [PubMed] [Google Scholar]
- 83.Olson AL, Gifford AH, Inase N, et al. The epidemiology of idiopathic pulmonary fibrosis and interstitial lung diseases at risk of a progressive-fibrosing phenotype. Eur Respir Rev 2018; 27: 180077. doi: 10.1183/16000617.0077-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med 2018; 198: e44–e68. doi: 10.1164/rccm.201807-1255ST [DOI] [PubMed] [Google Scholar]
- 85.Nalysnyk L, Cid-Ruzafa J, Rotella P, et al. Incidence and prevalence of idiopathic pulmonary fibrosis: review of the literature. Eur Respir Rev 2012; 21: 355–361. doi: 10.1183/09059180.00002512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ley B, Collard HR, King TE Jr. Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2011; 183: 431–440. doi: 10.1164/rccm.201006-0894CI [DOI] [PubMed] [Google Scholar]
- 87.O'Brien K, Troendle J, Gochuico BR, et al. Pirfenidone for the treatment of Hermansky–Pudlak syndrome pulmonary fibrosis. Mol Gen Metabol 2011; 103: 128–134. doi: 10.1016/j.ymgme.2011.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gahl WA, Brantly M, Troendle J, et al. Effect of pirfenidone on the pulmonary fibrosis of Hermansky–Pudlak syndrome. Mol Gen Metabol 2002; 76: 234–242. doi: 10.1016/S1096-7192(02)00044-6 [DOI] [PubMed] [Google Scholar]
- 89.Sugino K, Gocho K, Kikuchi N, et al. Acute exacerbation of combined pulmonary fibrosis and emphysema associated with Hermansky–Pudlak syndrome. Respirol Case Rep 2016; 4: 13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Thompson G, Sekiguchi H, Chen D, et al. A 40-year-old man with albinism and progressive dyspnea. Chest 2018; 154: e143–e146. doi: 10.1016/j.chest.2018.05.032 [DOI] [PubMed] [Google Scholar]
- 91.Katzenstein AL, Myers JL. Idiopathic pulmonary fibrosis: clinical relevance of pathologic classification. Am J Respir Crit Care Med 1998; 157: 1301–1315. doi: 10.1164/ajrccm.157.4.9707039 [DOI] [PubMed] [Google Scholar]
- 92.Katzenstein AL, Zisman DA, Litzky LA, et al. Usual interstitial pneumonia: histological study of biopsy and explant specimens. Am J Surg Pathol 2002; 26: 1567–1577. doi: 10.1097/00000478-200212000-00004 [DOI] [PubMed] [Google Scholar]
- 93.Wuyts WA, Cavazza A, Rossi G, et al. Differential diagnosis of usual interstitial pneumonia: when is it truly idiopathic? Eur Respir Rev 2014; 23: 308–319. doi: 10.1183/09059180.00004914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.El-Chemaly S, O'Brien KJ, Nathan SD, et al. Clinical barriers to lung transplantation in Hermansky–Pudlak syndrome pulmonary fibrosis. PLoS One 2018; 13: e0194193. doi: 10.1371/journal.pone.0194193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lederer DJ, Kawut SM, Sonett JR, et al. Successful bilateral lung transplantation for pulmonary fibrosis associated with the Hermansky–Pudlak syndrome. J Heart Lung Transplant 2005; 24: 1697–1699. doi: 10.1016/j.healun.2004.11.015 [DOI] [PubMed] [Google Scholar]
- 96.Tager AM, Sharma A, Mark EJ. Case 32-2009 – a 27-year-old man with progressive dyspnea. N Engl J Med 2009; 361: 1585–1593. doi: 10.1056/NEJMcpc0905544 [DOI] [PubMed] [Google Scholar]
- 97.Umei N, Ichiba S, Chida M. Successful use of veno-venous extracorporeal membrane oxygenation as a bridge to lung T transplantation in a patient with pulmonary fibrosis. Gen Thorac Cardiovasc Surg 2017; 65: 478–480. doi: 10.1007/s11748-016-0726-0 [DOI] [PubMed] [Google Scholar]
- 98.Sim W, Kim SY, Han J, et al. Extracorporeal membrane oxygenation bridge to lung transplantation in a patient with Hermansky–Pudlak syndrome and progressive pulmonary fibrosis. Acute Crit Care 2019; 34: 95–98. doi: 10.4266/acc.2018.00402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sakata Y, Kawamura K, Ichikado K, et al. Hermansky–Pudlak syndrome type 4 with interstitial pneumonia. Respir Med Case Rep 2013; 9: 38–41. doi: 10.1016/j.rmcr.2013.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.O'Brien KJ, Lozier J, Cullinane AR, et al. Identification of a novel mutation in HPS6 in a patient with hemophilia B and oculocutaneous albinism. Mol Genet Metab 2016; 119: 284–287. doi: 10.1016/j.ymgme.2016.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Han CG, O'Brien KJ, Coon LM, et al. Severe bleeding with subclinical oculocutaneous albinism in a patient with a novel HPS6 missense variant. Am J Med Genet A 2018; 176: 2819–2823. doi: 10.1002/ajmg.a.40514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.El-Chemaly S, Young LR. Hermansky–Pudlak syndrome. Clin Chest Med 2016; 37: 505–511. doi: 10.1016/j.ccm.2016.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Chen D, Uhl CB, Bryant SC, et al. Diagnostic laboratory standardization and validation of platelet transmission electron microscopy. Platelets 2018; 29: 574–582. doi: 10.1080/09537104.2018.1476682 [DOI] [PubMed] [Google Scholar]
- 104.Toro J, Turner M, Gahl WA. Dermatologic manifestations of Hermansky–Pudlak syndrome in patients with and without a 16-base pair duplication in the HPS1 gene. Arch Dermatol 1999; 135: 774–780. doi: 10.1001/archderm.135.7.774 [DOI] [PubMed] [Google Scholar]
- 105.Noble PW, Albera C, Bradford WZ, et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet 2011; 377: 1760–1769. doi: 10.1016/S0140-6736(11)60405-4 [DOI] [PubMed] [Google Scholar]
- 106.King TE Jr, Bradford WZ, Castro-Bernardini S, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med 2014; 370: 2083–2092. doi: 10.1056/NEJMoa1402582 [DOI] [PubMed] [Google Scholar]
- 107.Margaritopoulos GA, Trachalaki A, Wells AU, et al. Pirfenidone improves survival in IPF: results from a real-life study. BMC Pulm Med 2018; 18: 177. doi: 10.1186/s12890-018-0736-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Iyer SN, Gurujeyalakshmi G, Giri SN. Effects of pirfenidone on transforming growth factor-β gene expression at the transcriptional level in bleomycin hamster model of lung fibrosis. J Pharmacol Exp Ther 1999; 291: 367–373. [PubMed] [Google Scholar]
- 109.Conte E, Gili E, Fagone E, et al. Effect of pirfenidone on proliferation, TGF-β-induced myofibroblast differentiation and fibrogenic activity of primary human lung fibroblasts. Eur J Pharm Sci 2014; 58: 13–19. doi: 10.1016/j.ejps.2014.02.014 [DOI] [PubMed] [Google Scholar]
- 110.Jin J, Togo S, Kadoya K, et al. Pirfenidone attenuates lung fibrotic fibroblast responses to transforming growth factor-β1. Respir Res 2019; 20: 119. doi: 10.1186/s12931-019-1093-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.O'Brien KJ, Introne WJ, Akal O, et al. Prolonged treatment with open-label pirfenidone in Hermansky–Pudlak syndrome pulmonary fibrosis. Mol Genet Metab 2018; 125: 168–173. doi: 10.1016/j.ymgme.2018.07.012 [DOI] [PubMed] [Google Scholar]
- 112.Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 2014; 370: 2071–2082. doi: 10.1056/NEJMoa1402584 [DOI] [PubMed] [Google Scholar]
- 113.Distler O, Highland KB, Gahlemann M, et al. Nintedanib for systemic sclerosis-associated interstitial lung disease. N Engl J Med 2019; 380: 2518–2528. doi: 10.1056/NEJMoa1903076 [DOI] [PubMed] [Google Scholar]
- 114.Flaherty KR, Wells AU, Cottin V, et al. Nintedanib in progressive fibrosing interstitial lung diseases. N Engl J Med 2019; 381: 1718–1727. doi: 10.1056/NEJMoa1908681 [DOI] [PubMed] [Google Scholar]
- 115.Wells AU, Flaherty KR, Brown KK, et al. Nintedanib in patients with progressive fibrosing interstitial lung diseases – subgroup analyses by interstitial lung disease diagnosis in the INBUILD trial: a randomised, double-blind, placebo-controlled, parallel-group trial. Lancet Respir Med 2020; 8: 453–460. doi: 10.1016/S2213-2600(20)30036-9 [DOI] [PubMed] [Google Scholar]
- 116.Wollin L, Wex E, Pautsch A, et al. Mode of action of nintedanib in the treatment of idiopathic pulmonary fibrosis. Eur Respir J 2015; 45: 1434–1445. doi: 10.1183/09031936.00174914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ikawa Y, Hess R, Dorward H, et al. In vitro functional correction of Hermansky–Pudlak syndrome type-1 by lentiviral-mediated gene transfer. Mol Genet Metab 2015; 114: 62–65. doi: 10.1016/j.ymgme.2014.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Iyer S, Suresh S, Guo D, et al. Precise therapeutic gene correction by a simple nuclease-induced double-stranded break. Nature 2019; 568: 561–565. doi: 10.1038/s41586-019-1076-8 [DOI] [PMC free article] [PubMed] [Google Scholar]