Abstract
Sleep disordered breathing, especially obstructive sleep apnoea (OSA), has a high and increasing prevalence. Depending on the apnoea and hypopnoea scoring criteria used, and depending on the sex and age of the subjects investigated, prevalence varies between 3% and 49% of the general population. These varying prevalences need to be reflected when considering screening for OSA. OSA is a cardiovascular risk factor and patients are at risk when undergoing medical interventions such as surgery. Screening for OSA before anaesthesia and surgical interventions is increasingly considered. Therefore, methods for screening and the rationale for screening for OSA are reviewed in this study.
Short abstract
Screening of patients with simple questionnaires and sleep tests will identify OSA prior to surgery http://ow.ly/4GZl300mXsh
Introduction
Sleep disordered breathing (SDB) presents a group of disorders with its origin during sleep. These can be categorised according to pathophysiology and findings into the following subcategories according to third revision of the International Classification of Sleep Disorders, which are obstructive sleep apnoea (OSA), central sleep apnoea, sleep-related hypoventilations, sleep related hypoxia and isolated symptoms (with snoring and catathrenia) [1].
OSA has a high prevalence, which has increased over past decades [2]. Depending on age, the prevalence of moderate and severe sleep apnoea (AHI ≥15 events per h) among men is 10–17% and among women 3–9%. Using lower AHI thresholds, the prevalence is much higher. Sleep apnoea events are observed in many more subjects. Severe sleep apnoea has been recognised as a risk factor for cardiovascular disorders [3]. Some, but not all, data suggest that treatment of sleep apnoea with continuous positive airway pressure (CPAP) lead to a reduction of cardiovascular risk and mortality in these patients.
Diagnosis of OSA
Diagnosis for OSA and, to a broader extent, SDB is performed either in sleep centres or with home sleep testing (HST) with limited channels. This method is also called “polygraphy”, portable sleep recording or out-of-centre recording. The required procedures and systems that are eligible vary between countries. This is often linked to national reimbursement regulations. For an effective diagnosis of SDB, the criteria have been well described by the SCOPER approach, encompassing the assessment of “sleep”, “cardiovascular”, “oxygen saturation”, “position”, “effort of respiration” and “respiratory flow” [4]. Appropriate sensors are a matter of technology. Technology is improving and, thus, sensors change over time. For reporting SDB, a quality-controlled evaluation is needed. The evaluation depends on criteria set for the scoring of apnoea and hypopnoea events as well as for oxygen desaturation events. Algorithms and scoring methodology differ between systems, and therefore, systematic comparison of methodologies has to be performed in regular intervals.
Screening for OSA
Screening for OSA is different from investigating patients referred to a centre due to suspected OSA, who are likely to represent a group with moderate to high pre-test probability. The goal for screening for a disorder, in general, is to effectively rule in and rule out patients with the highest possible sensitivity and specificity, evaluated against costs. When using systems appropriate for diagnosing OSA based on the SCOPER criteria mentioned above, the most expensive part of SCOPER, the sleep component, is omitted and estimated by reported sleep times instead. As a consequence, the dilution effect is observed [5]. This means that the number of apnoeas identified are divided by a longer total sleep time than actually happened.
Methods used for screening OSA
Methods for screening can be devices that follow the SCOPER criteria as outlined in a comprehensive review [4]. Devices like common six-channel systems (e.g. Embletta (ResMed, San Diego, CA, USA), Somnowatch (SOMNOmedics, Randersacker, Germany) and Nox T3 (Nox Medical, Reykjavik, Iceland)) are able to cover all aspects. Other devices with fewer channels (e.g. Watch-PAT (Itamar Medical, Caesarea, Israel)) try to cover the SCOPER criteria with surrogate parameters derived from other signals. Sleep periods can be derived by actigraphy. Respiration may be derived from variations in pulse wave amplitude and heart rate. Oximetry is usually part of the methods applied to screen for OSA. At the lower end, devices with even fewer channels, usually one to three channels (e.g. ApneaLink (ResMed)) may record respiratory flow or movement, sometimes even without oximetry and pulse rate.
Population-based studies
Epidemiological studies need systems which have a validated sensitivity and specificity. It is of particular importance to define scoring criteria for respiratory events, allowing the results are meaningful and to be compared between different national cohorts. A recent sleep apnoea population screening [6] showed a very high prevalence of sleep apnoea based on the American Academy of Sleep Medicine 2012 scoring criteria [7]. An apnoea–hypopnoea index of ≥5 events per h was recorded in 83.8% of men and in 60.8% of women, whereas an apnoea–hypopnoea index of ≥15 events per h was noted in 49.7% of men and in 23.4% of women. Mild sleep apnoea (AHI 5–15 events per h) was present in 40% of men and in 32% of women <60 years, while in those ≥60 years, it was 25% and 43%, respectively. Moderate sleep apnoea (AHI 15–30 events per h) was present in 25% of men and in 11% of women <60 years, while in those ≥60 years, it was 32% and 21%, respectively. Severe sleep apnoea (AHI ≥30 events per h) was found in 15% of men and in 3% of women <60 years, while in those ≥60 years, it was 31% and 13% respectively.
Compared with women, scores on the apnoea–hypopnoea index were around three times higher in men in the younger age category (≥40 to <60 years) and twice as high in older men (60–85 years). In that study, different scoring criteria were applied in addition and as a result, the prevalence changed dramatically.
High-risk patients
Providing sleep studies in high-risk patients can be very useful in order to identify a cardiovascular risk factor or other consequences of SDB. Subjects for such approach could be patients with a history of previous cardiovascular events (myocardial infarction or stroke) or with cardiovascular risk factors (arterial hypertension or atrial fibrillation). Another group includes subjects with daytime sleepiness and professional drivers should undergo evaluation for SDB, as suggested by the attention given to the problem by the current European Union legislation [8].
Screening for SDB before surgical interventions
As SDB becomes better recognised, the relationship between SDB and complications from anaesthesia and post-operative analgesia has gained wider attention [9–13]. The role of OSA as a risk factor for anaesthetic morbidity and mortality is considerable. The main peri-operative risk factors associated with OSA include upper airway collapse, hypoxaemia and difficult airway control. Stierer et al. identified a difficult upper airway in 21.9% of OSA patients and in 2.6% of the controls, with intubation failure in 5% of the OSA patients [14].
Retrospective studies in a peri-operative setting have reported an increased frequency of respiratory complications in patients with an oxygen desaturation index (ODI) >5 events per h and, in addition, peri-operative complications, especially episodes of oxygen desaturation in patients with OSA [15, 16]. A recent meta-analysis, encompassing nine studies, reported a likelihood of 2.43 to develop a post-operative complication in the presence of OSA [17]. In addition, cardiovascular, gastrointestinal and bleeding abnormalities are over-represented. A high incidence of perioperative pulmonary complications including intubation/mechanical ventilation, aspiration pneumonia and acute respiratory distress syndrome was reported in OSA patients undergoing general surgical or orthopaedic procedures [18–22]. However, there was no correlation between the AHI and rate of complications, suggesting that identification of even mild cases of OSA may be critical prior to major elective surgery [19]. The associated risks involve underlying obesity, abnormal upper airway anatomy and cardiovascular comorbidities.
There is a strong association between OSA and obesity, and the prevalence of OSA is particularly high in patients undergoing gastric bypass surgery [23–26]. Sleep studies are therefore mandated and pre-operative polysomnography could be performed, since it is the most cost-effective strategy for diagnosing OSA [27]. However, urgency of the planned surgical procedure frequently limits a policy of liberally applied pre-operative polysomnography. Pre-operative screening of these patients, by cardiopulmonary polygraphy or even more simplified systems, is a feasible alternative which currently is routinely applied [28].
Increased recognition of the potential threats has therefore slowly modified the way physicians manage patients with a diagnosis of OSA in peri- and post-operative care. New preventive strategies to control peri-operative risk have been introduced [29]. However, given the underdiagnosis of OSA in the general population, screening cannot be extensively applied to all patients awaiting surgery [30, 31]. Based on the recent HypnoLaus study, the prevalence of OSA is very high in the general population [6], even when an AHI cut-off value of ≥15 events per h is used and, consequently, there is a considerable number of patients undergoing elective surgery who exhibit a high risk of OSA. As the time the anaesthetist spends on a pre-operative assessment is brief, it is crucial to have a concise but structured way of identifying patients at risk for OSA. A brief questionnaire is a practical, useful and efficient way to pre-operatively identify patients who are likely to have OSA [32]. Such questionnaires apply often used apnoea-screening questions but it is important to notice that negative answers to these questions or absence of the typical OSA features does not eliminate the possibility of OSA. In patients undergoing elective surgery, procedures may need to be postponed until a proper sleep assessment has been made and, if appropriate, treatment of OSA has been instituted. It follows that all patients should be interviewed for potential apnoea and, if possible, receive an evaluation of the upper airway anatomy. Information from a bed partner at the time of the pre-operative assessment can be extremely useful, since patients often are unaware of snoring and disrupted breathing that may have been noticed by their partner. Some practical guidelines have been developed and updated by a Task Force of the American Society of Anesthesiologists (ASA) and others [28, 29, 33, 34]. Optimal pre-operative benefit of CPAP may require ≥1 month of treatment for oedema in the airway to subside [33]. In cases of urgent surgery, the patient should be assumed to have OSA.
Focused history
Risk stratification and triage of patients referred to sleep facilities is highly desirable, as the diagnostic capacity of sleep centres is limited and waiting lists tend to grow [35]. Relevant clinical information should be obtained by a detailed medical history and careful clinical examination of subjects with suspected SDB. However, there are several caveats to be considered in relation to diagnostic procedures in OSA. First, it may be hard to produce objective, reproducible findings, due to observer and reporter bias. Valuable efforts have been made to increase standardisation. These include the use of questionnaires that allow for both the identification of individuals with a high likelihood of SDB and for triage according to their symptomatology. Questionnaires that make use of isolated symptoms have a limited effectiveness. For instance, snoring is a primary symptom in OSA that has a sensitivity of almost 100% but lacks specificity. Thus, snoring has a low positive predictive value [36]. The report of “breath holding” has a low sensitivity but a high specificity for OSA [36]. The diagnostic performance of the Epworth Sleepiness Scale (ESS) score >10 to predict AHI >5 events per h has a sensitivity of 54% and a specificity of 63% [37]. Moreover, subjective clinical impressions of OSA tend to have inadequate sensitivity (60%) and specificity (63%). Novel clinical prediction models that optimise sensitivity and specificity have therefore been developed. In one such attempt, apnoeas, snoring, excessive sleepiness while driving and sleeping in supine sleep position were combined; however, without beneficial outcome [38].
Pre-operative screening questionnaires and clinical prediction models
Several pre-operative screening questionnaires that incorporate risk factors, clinical symptoms and physical examination parameters have been developed to facilitate the diagnosis of OSA. Several of these have been validated for peri-operative screening: the Berlin Questionnaire [39–41], the ASA checklist [29], the STOP-Bang questionnaire [42] and the Flemons Index (Sleep Apnea Clinical Score (SACS)) [43]. Some of these clinical prediction models have attempted to establish a reliable diagnosis without a simultaneous objective sleep test but these attempts have failed [44]. The oldest of these tests is the Flemons Index, which combines neck circumference, presence or absence of hypertension, and historical features (habitual snoring, partner report of gasping, choking or snorting). The test provides the SACS and it was demonstrated that a SACS ≥15 was associated with a high probability of OSA (OR 5.17 and positive predictive value of 81%) [44]. Moreover, the SACS has been associated with post-anaesthesia care complications [45]. Takegami et al. [46] developed a four-variable screening tool based on sex, BMI, blood pressure and snoring. This tool was highly discriminative but mathematical corrections were needed to calculate an end score; therefore, the utility in the peri-operative period was limited.
The Berlin Questionnaire was the outcome of the Conference on Sleep in Primary Care in April 1996 in Berlin, Germany. The questionnaire has a high specificity for identifying subjects with moderate to severe OSA but rather low specificity. It classifies subjects as low- or high-risk for OSA based on responses in three categories: 1) snoring history, 2) daytime sleepiness and 3) history of hypertension or obesity. When a patient responds positively in two of the categories assessed, he/she can be considered at a high risk for OSA. The Apnea Risk Evaluation System (ARES) combines features of the Berlin Questionnaire, the Flemons' Index and the ESS, and classifies the patient as “no apparent risk”, “low risk” or “high risk”, with a sensitivity of 94% and a specificity of 79% for an AHI >5 events per h. In a cohort of 2877 patients screened with the ARES questionnaire in a pre-operative setting, 23.7% had high risk for OSA (661) and among these, 82% had OSA [47]. Enciso et al. [48] found an increased sensitivity (90.4%) at the expense of a lower specificity (43.2%) to find an AHI ≥15 events per h compared to the Berlin Questionnaire. The ASA OSA scoring checklist combines physical characteristics, history of apparent airway obstruction and somnolence. Its sensitivity is acceptable (72–87%) but its specificity is low (36–38%). The STOP and STOP-Bang questionnaires are self-administered questionnaires that were developed and tested by Chung et al. [42]. STOP is the acronym for four questions addressing the presence of snoring, daytime fatigue (tiredness), observed apnoeas, and arterial hypertension. The STOP-Bang questionnaire is a refinement of the STOP questionnaire, and incorporates questions on BMI (>35 kg·m−2), age (>50 years), neck circumference (>40 cm) and gender (male), with improved sensitivity at the cost of a slightly lower specificity. Both questionnaires have a high sensitivity for identifying subjects with SDB but relatively low specificity. The STOP questionnaire labels a patient with a high risk for SDB if at least two positive answers are present, while the STOP-Bang questionnaire uses a cut-off value of at least three positive answers. Due to its simplicity, STOP-Bang is frequently used to predict severity of underlying OSA and to facilitate triage of patients. In a study comparing STOP, the Berlin Questionnaire and the ASA OSA scoring checklist, the ASA OSA checklist showed the highest sensitivity but the lowest specificity (table 1) [40, 49]. Taken together, the potential usefulness of these tools for prioritisation of an objective diagnostic test is limited. The strongest model so far is the OSA50 questionnaire, which combines a simple questionnaire with oximetry. OSA50 is an acronym for obesity (waist circumference in males >102 cm, females >88 cm), snoring (has your snoring ever bothered other people?), apnoea (has anyone noticed that you stop breathing during your sleep?) and 50 (are you aged 50 years or over?). If the answers are yes, a score of 3, 3, 2 and 2 points, respectively, is assigned. If a cut-off ≥5 out of 10 and ODI ≥16 events per h is applied for OSA, a sensitivity of 97%, a specificity of 87% and a diagnostic accuracy of 83% is reached [50]. The authors reported that they preferred oximetry over nasal pressure for their two-stage model, because the failure rate for the oximetry signal (3%) was one-third of that observed for the nasal pressure signal (9%). Recently, the P-SAP (Perioperative Sleep Apnea Prediction Score) was proposed. This score incorporates six out of eight elements of the STOP-Bang questionnaire and some other common elements used in the standard peri-operative assessment (Mallampati score, presence of diabetes and thyromental distance <6 cm) [51]. 1 point is assigned for each of the nine risk factors (unweighted scale) and scores are summed. This provides a very high sensitivity and a very low specificity in the lower range but a very low sensitivity and very high specificity in the higher range. It was concluded that the score requires further refinement.
TABLE 1.
STOP, the Berlin Questionnaire and the ASA checklist in pre-operative patients
| AHI ≥5 events per h | AHI ≥15 events per h | AHI ≥30 events per h | |
| Sensitivity | |||
| STOP | 66% | 74% | 79% |
| Berlin Questionnaire | 69% | 79% | 87% |
| ASA checklist | 72% | 79% | 87% |
| Specificity | |||
| STOP | 60% | 53% | 49% |
| Berlin Questionnaire | 56% | 50% | 46% |
| ASA checklist | 38% | 37% | 36% |
STOP: snoring, tiredness, observed apnoeas, pressure; ASA: American Society of Anesthesiologists; AHI: apnoea–hypopnoea index.
Practical approach
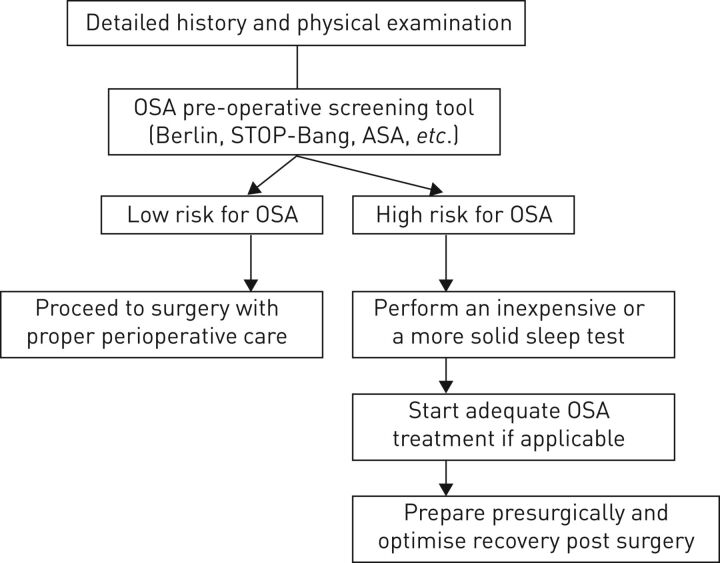
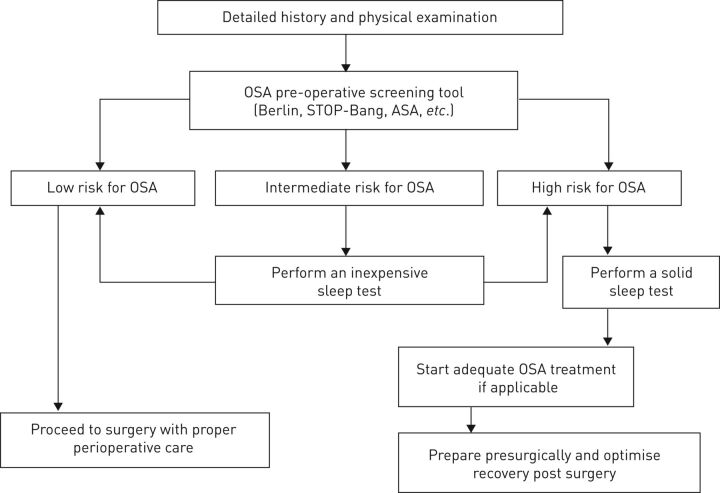
Patients with suspicion of OSA based on focused history and physical examination should be screened with a pre-operative screening tool, such as the Berlin Questionnaire, STOP-Bang, SACS or ASA checklist, in order to classify them as low or high risk for OSA (two-step model) (figure 1). Patients categorised as high risk for OSA should either proceed to surgery as “high risk” for OSA or receive a referral to a sleep specialist for further assessment and treatment. In a three-step model is used (e.g. ARES questionnaire), those classified with an intermediate risk should be screened with an inexpensive sleep test in order to confirm or reject the presence of OSA. When in doubt, it may be advisable to consider a final advanced sleep test to classify breathing during sleep in more detail (figure 2). It should be kept in mind that based on the false-negative rates, it is likely that most clinical screening tests miss a significant proportion of patients with OSA. Finally, the relative urgency of the surgery will determine whether to proceed directly to surgery or to refer the patient for additional assessment in terms of sleep and breathing. It could also be argued whether patients scheduled for ambulatory surgery need such an approach. It was shown that the rate of unplanned hospital admissions (need for invasive procedure, bleeding, pain, nausea/vomiting, prolonged regional blockade, cardiovascular complications, ventilatory support, aspiration, pneumonia and urinary retention) (23.9% versus 18.8%, OR 1.4) and the rate of other adverse events (2.1% versus 1.3%, OR 1.7) between OSA and non-OSA patients were unchanged following such a practice [52]. However, Chung [53] reported that it may be unsafe for patients with untreated severe OSA requiring post-operative narcotics to undergo ambulatory surgery.
FIGURE 1.
Two-stage model. OSA: obstructive sleep apnoea; STOP-Bang: snoring, tiredness, observed apnoeas, pressure, body mass index, age, neck circumference, gender; ASA: American Society of Anesthesiologists.
FIGURE 2.
Three-stage model. OSA: obstructive sleep apnoea; STOP-Bang: snoring, tiredness, observed apnoeas, pressure, body mass index, age, neck circumference, gender; ASA: American Society of Anesthesiologists.
Can pre-operative screening reduce waiting lists?
Anaesthetists need a highly accurate clinical test with a high sensitivity to definitely rule out OSA in a lower-risk population, without a need to depend on a confirmatory polysomnography [54]. However, the need for advanced additional sleep studies depends on the characteristics, specifically sensitivity and specificity of the screening tools used. An ideal diagnostic test should have a relatively high sensitivity with sufficient specificity. Moreover, it should be minimally intrusive and relatively inexpensive, and it should identify patients early in the disease process [55]. Given the high degree of heterogeneity and false negative responses associated with all questionnaires and most clinical prediction models, a significant proportion of patients with OSA will be missed by all questionnaires and most of the clinical models [54]. However, false-positive cases will give rise to a need for confirmation of the suspicion, leading to more sleep studies and longer waiting lists.
It seems that some clinical models can identify the OSA phenotype more robustly than questionnaires alone. This may be cost-effective but so far, their potential use is limited to the prioritisation of an objective diagnostic test. It also needs to be taken into account that prediction models often are derived and validated in high-risk populations, which introduces bias and results in a higher sensitivity compared with when the test is used in a lower-risk population. Theoretically, when the target is to predict severe OSA, it is feasible to use these methods pre-operatively, with a high degree of accuracy. This would certainly reduce the pressure on sleep centres. It should be underlined that the current conclusions only are valid if the national healthcare system accepts an OSA diagnosis based on a simplified tool in order to initiate (CPAP) therapy. If confirmation by a full sleep study is mandatory, this will even extend the waiting lists. As an alternative, home respiratory polygraphy could be considered. Validation of portable monitors has been specifically developed in the context of a high prevalence of comorbid conditions such as obesity, chronic heart failure, type 2 diabetes mellitus, stroke and pulmonary hypertension. The results are similar to those of polysomnography, although a low accuracy in detecting hypopnoeas is a recognised major drawback [56].
Effect of CPAP therapy in the peri-operative setting
Consistent use of CPAP prior to surgery and immediately after surgery appears to hold the best potential for decreasing peri- and post-operative complications [34, 57], and to result in shorter hospital length of stay, compared to untreated patients [19]. A carry-over effect was observed, even though some of these patients did not receive CPAP therapy in the hospital, and may be explained by decreased inflammation and upper airway oedema, decreased tongue volume, as well as increased upper airway dimensions and less collapsibility [58, 59]. Optimal pre-operative benefit of CPAP may require 4–6 weeks of treatment for oedema in the airway to subside [58]. Induction of anaesthesia causes an immediate significant reduction in functional residual capacity of 16–20% in the supine position and up to 20% of lung bases are collapsed soon after induction of anaesthesia [60, 61]. Together with upper airway obstruction, this predisposes patients to hypoxaemia. These problems can be offset by the application of CPAP during pre-oxygenation [62–64]. One of the challenges with pre-operative CPAP therapy is timely pre-operative diagnosis, CPAP titration and final adherence. In fact, a recent study described a 40% adherence with CPAP therapy and median usage of just 2.5 h among users [65]. Patients who have not been using CPAP regularly or for long enough may still have airway oedema. In patients who have severe OSA or a significantly comprised airway, pre-operative intubation and post-operative extubation during wake are highly recommended [66]. Furthermore, the supine position during the peri-operative period may worsen upper airway obstruction. Reduction in anaesthetic dose may also be helpful in patients who have OSA and shorter-acting hypnotics may be preferred [67, 68]. In the post-operative setting, emergence from anaesthesia is a critical period involving removal of artificial airways and reversal of neuromuscular blockade. Applying CPAP when assisting ventilation with bag and mask can be useful to help minimise upper airway obstruction in the peri-operative setting. Few studies describe the impact of post-operative CPAP therapy on adverse outcomes but rendered current guidelines to recommend the use of CPAP therapy. In a small study, Renotte et al. [69] showed a reduction in post-operative complications in patients who used CPAP pre-operatively, on extubation and nearly continuously for up to 48 h after surgery. In a large cohort of 26 842 patients, Abdelsattar et al. [70] reported more unplanned reintubations (OR 2.5) and myocardial infarction (OR 2.6) in untreated OSA compared with treated OSA. However, a recent meta-analysis concluded that there is no significant difference in the post-operative adverse events between CPAP and no CPAP treatment but a trend towards shorter hospital length of stay and potential benefits in the use of CPAP during the peri-operative period [71]. The nonsignificant benefit of CPAP on post-operative adverse events may be explained by a low overall incidence of post-operative complications in this meta-analysis. Nevertheless, the recent findings that diagnosed OSA patients with a CPAP prescription have fewer cardiac complications are substantial and provide a rationale for treating OSA with CPAP during the peri-operative period [71, 72]. Finally, timely diagnosis and treatment led to a reduction of medication usage for the associated medical diseases [73]. CPAP may need to be applied shortly after extubation and therefore necessitates availability of a CPAP device [13]. In those who have not used or been compliant with CPAP previously, or in undiagnosed cases, temporary introduction of CPAP until cessation of narcotic analgesic or sedative drugs is warranted. Oxygen can be added to CPAP treatment, usually via a side port on the CPAP mask, but may mask the presence of obstructive episodes, particularly to an inexperienced observer [13]. Administration of CPAP immediately after extubation maintains spirometric lung function at 24 h after laparoscopic bariatric surgery better than CPAP started in the post-anaesthesia care unit [74–76]. Subjects who had immediate post-extubation CPAP showed an average reduction of 27% in forced vital capacity versus, on average, a 50% reduction 1 h post-operatively in a standard care group. The use of CPAP in the recovery room appears to be too late to restore lost lung volumes. In spite of these potentially beneficial effects, CPAP appears to be underused post-operatively. In one study, the rate of postoperative CPAP use was relatively low (60%), even in OSA patients with previous experience of CPAP. This reflects a lack of hospital policies guiding the routine use of CPAP when such patients are hospitalised [15, 19]. Patients who use CPAP pre-operatively on a regular basis should be advised to bring the device to the hospital for use in the post-operative period [34]. CPAP should be applied at pressures known to be effective in eliminating upper airway obstruction in a particular patient. However, CPAP pressure requirements may change after surgery or with the use of anaesthetic, sedative and analgesic agents [77]. Some practical issues also remain. Patients may be incapable of using CPAP without assistance in the post-operative period. Patients may also be reluctant to use CPAP, because of discomfort, nausea or pain [77]. With better control of post-operative pain and nausea/vomiting, it may improve the compliance with CPAP among OSA patients [71]. Moreover, there is no significant risk of post-operative nausea and vomiting with the use of post-operative CPAP [78]. Finally, OSA presents a dilemma in the peri-operative setting to the treating physician, who must decide either to cancel the surgery and refer the patient for possible CPAP therapy or to proceed, knowing that the risk of complications may be increased [79].
Conclusion
The combination of anaesthesia and undiagnosed OSA can be potentially dangerous, and may place the patients at an increased risk of peri-operative complications and post-operative morbidity. Screening of patients with simple questionnaires and a variety of inexpensive sleep tests will identify patients at risk of OSA, and will provide a necessary first step in arriving at a solid sleep test, identifying patients with OSA prior to surgery. This enables pre-surgical preparations and optimises post-surgical recovery. Pre-screening should be viewed as a necessary step to avoid complications peri-operatively and during recovery time, and provides an opportunity to identify previously undiagnosed medical conditions that, if treated, would likely lead to improvement in overall outcome from any intervention and in overall quality of life.
Disclosures
J. Hedner ERR-0012-2016_Hedner (1.2MB, pdf)
T. Penzel ERR-0012-2016_Penzel (1.2MB, pdf)
Footnotes
Conflict of interest: Disclosures can be found alongside this article at err.ersjournals.com
Provenance: Submitted article, peer reviewed.
References
- 1.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd Edn. Darien, American Academy of Sleep Medicine, 2014. [Google Scholar]
- 2.Peppard PE, Young T, Barnet JH, et al. . Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013; 177: 1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marin JM, Carrizo SJ, Vicente E, et al. . Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 2005; 365: 1046–1053. [DOI] [PubMed] [Google Scholar]
- 4.Collop NA, Tracy SL, Kapur V, et al. . Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clin Sleep Med 2011; 7: 531–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Escourrou P, Grote L, Penzel T, et al. . The diagnostic method has a strong influence on classification of obstructive sleep apnea. Results from the European Sleep Apnoea Database (ESADA). J Sleep Res 2015; 24: 730–738. [DOI] [PubMed] [Google Scholar]
- 6.Heinzer R, Marques-Vidal P, Marti-Soler H, et al. . Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med 2015; 3: 310–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berry RB, Brooks R, Gamaldo CE, et al. . The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. Version 2.1. Darien, American Academy of Sleep Medicine, 2014. [Google Scholar]
- 8.Bonsignore MR, Randerath W, Riha R, et al. . New rules on driver licensing for patients with obstructive sleep apnoea: EU Directive 2014/85/EU. Eur Respir J 2016; 47: 39–41. [DOI] [PubMed] [Google Scholar]
- 9.Hartmann B, Junger A, Klasen J. Anesthesia and sleep apnea syndrome. Anaesthesist 2005; 54: 684–693. [DOI] [PubMed] [Google Scholar]
- 10.Hiremath AS, Hillman DR, James AI, et al. . Relationship between difficult tracheal intubation and obstructive sleep apnoea. Br J Anesth 1998; 80: 606–611. [DOI] [PubMed] [Google Scholar]
- 11.Vasu TS, Grewal R, Doghramji K. Obstructive sleep apnea syndrome and perioperative complications: a systematic review of the literature. J Clin Sleep Med 2012; 8: 199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.den Herder C, Schmeck J, Appelboom DJK, et al. . Risks of general anaesthesia in people with obstructive sleep apnoea. Br Med J 2004; 329: 955–959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hillman DR, Loadsman JA, Platt PR, et al. . Obstructive sleep apnoea and anaesthesiology. Sleep Med Rev 2004; 8: 459–471. [DOI] [PubMed] [Google Scholar]
- 14.Stierer TL, Wright C, George A, et al. . Risk assessment of obstructive sleep apnea in a population of patients undergoing ambulatory surgery. J Clin Sleep Med 2010; 6: 467–472. [PMC free article] [PubMed] [Google Scholar]
- 15.Hwang D, Shakir N, Limann B, et al. . Association of sleep-disordered breathing with postoperative complications. Chest 2008; 133: 1128–1134. [DOI] [PubMed] [Google Scholar]
- 16.Liao P, Yegneswaran B, Vairavanathan S, et al. . Postoperative complications in patients with obstructive sleep apnea: a retrospective matched cohort study. Can J Anesthesiol 2009; 56: 819–828. [DOI] [PubMed] [Google Scholar]
- 17.Kaw R, Chung F, Pasupluleti V, et al. . Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Brit J Anesth 2012; 6: 897–906. [DOI] [PubMed] [Google Scholar]
- 18.Memtsoudis S, Liu SS, Ma Y, et al. . Perioperative pulmonary outcomes in patients with sleep apnea after noncardiac surgery. Anesth Analg 2011; 112: 113–121. [DOI] [PubMed] [Google Scholar]
- 19.Gupta RM, Parvizi J, Hanssen AD, et al. . Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. May Clin Proc 2001; 76: 897–905. [DOI] [PubMed] [Google Scholar]
- 20.De Jesus Danzi-Soares N, Genta PR, Nerbass FB, et al. . Obstructive sleep apnea is common among patients referred for coronary artery bypass grafting and can be diagnosed by portable monitoring. Coron Artery Dis 2012; 23: 31–38. [DOI] [PubMed] [Google Scholar]
- 21.Parikh SN, Stuchin SA, Maca C, et al. . Sleep apnea syndrome in patients undergoing total joint arthroplasty. J Arthroplasty 2002; 17: 635–642. [DOI] [PubMed] [Google Scholar]
- 22.Harrison MM, Childs A, Carson PE. Incidence of undiagnosed sleep apnea in patients scheduled for elective total joint arthroplasty. J Arthroplasty 2003; 18: 1044–1047. [DOI] [PubMed] [Google Scholar]
- 23.Ravesloot MJL, Hilgevoord AA, van Wagensveld BA, et al. . Assessment of the effect of bariatric surgery on obstructive sleep apnea at two postoperative intervals. Obes Surg 2014; 24: 22–31. [DOI] [PubMed] [Google Scholar]
- 24.Morong S, Benoist LB, Ravesloot MJ, et al. . The effect of weight loss on OSA severity and position dependence in the bariatric population. Sleep Breath 2014; 18: 851–856. [DOI] [PubMed] [Google Scholar]
- 25.Young T, Peppard PE, Taheri S. Excess weight and sleep-disordered breathing. J Appl Physiol 2005; 99: 1592–1599. [DOI] [PubMed] [Google Scholar]
- 26.Ling IT, James AL, Hillman DR. Interrelationships between body mass, oxygen desaturation, and apnea-hypopnea indices in a sleep clinic population. Sleep 2012; 35: 89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pietzch JB, Garner A, Cipriano LE, et al. . An integrated health-economic analysis of diagnostic and therapeutic strategies in the treatment of moderate-to severe obstructive sleep apnea. Sleep 2011; 34: 695–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mechanick JI, Youdim A, Jones DB, et al. . Clinical practice guidelines for the perioperative, nutritional, metabolic, and nonsurgical support of the bariatric surgery patient – 2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocr Pract 2013; 19: 337–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gross JB, Benumof JL, Caplan RA. Practice guidelines for the preoperative management of patients with obstructive sleep apnea: a report by the American Society of Anesthesiologists Task Force on Perioperative Management of Patients with obstructive sleep apnea. Anesthesiology 2006; 104: 1081–1093. [DOI] [PubMed] [Google Scholar]
- 30.Kapur V, Strohl KP, Redline S, et al. . Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath 2002; 6: 49–54. [DOI] [PubMed] [Google Scholar]
- 31.Young T, Evans L, Finn L, et al. . Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997; 20: 705–706. [DOI] [PubMed] [Google Scholar]
- 32.Abrishami A, Khajehdehi A, Chung F. A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anaest 2010; 57: 423–438. [DOI] [PubMed] [Google Scholar]
- 33.Seet E, Chung F. Management of sleep apnea in adults – functional algorithms for the perioperative period: Continuing Professional Development. Can J Anesth 2010; 57: 849–864. [DOI] [PubMed] [Google Scholar]
- 34.Adesanya AO, Lee W, Greilich NB, et al. . Perioperative management of obstructive sleep apnea. Chest 2010; 138: 1489–1498. [DOI] [PubMed] [Google Scholar]
- 35.Flemons WW, Douglas NJ, Kuna ST, et al. . Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med 2004; 169: 668–672. [DOI] [PubMed] [Google Scholar]
- 36.Bliwise DL, Nekich JC, Dement WC. Relative validity of self-reported snoring as a symptom of sleep apnea in a sleep clinic population. Chest 1991; 99: 600–608. [DOI] [PubMed] [Google Scholar]
- 37.Martinez D, Breitenbach TC, Lumertz MS. Repeating administration of Epworth Sleepiness Scale is clinically useful. Sleep Breath 2011; 15: 763–773. [DOI] [PubMed] [Google Scholar]
- 38.Deegan P, McNicholas WT. Predictive value of clinical features for the obstructive sleep apnoea syndrome. Eur Respir J 1996; 9: 117–124. [DOI] [PubMed] [Google Scholar]
- 39.Netzer NC, Stoohs RA, Netzer CM, et al. . Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 1999; 131: 485–491. [DOI] [PubMed] [Google Scholar]
- 40.Chung F, Yegneswaran B, Liao P, et al. . Validation of the Berlin Questionnaire and American Society of Anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients. Anesthesiology 2008; 108: 822–830. [DOI] [PubMed] [Google Scholar]
- 41.Chung F, Ward B, Ho J, et al. . Preoperative identification of sleep apnea risk in elective surgical patients, using the Berlin questionnaire. J Clin Anesth 2007; 19: 130–134. [DOI] [PubMed] [Google Scholar]
- 42.Chung F, Yegneswaran B, Liao P, et al. . STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008; 108: 812–821. [DOI] [PubMed] [Google Scholar]
- 43.Flemons WW, Whitelaw WA, Brant R, et al. . Likelihood ratios for a sleep apnea clinical prediction rule. Am J Respir Crit Care Med 1994; 150: 1279–1285. [DOI] [PubMed] [Google Scholar]
- 44.Rowley JA, Aboussouan LS, Badr MS. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep 2000; 23: 929–938. [DOI] [PubMed] [Google Scholar]
- 45.Gali B, Whalen FX, Schroeder DR, et al. . Identification of patients at risk for postoperative respiratory complications using a preoperative obstructive sleep apnea screening tool and postanesthesia care assessment. Anesthesiol 2009; 110: 869–877. [DOI] [PubMed] [Google Scholar]
- 46.Takegami M, Hayashino Y, Chin K, et al. . Simple four-variable screening tool for identification of patients with sleep-disordered breathing. Sleep 2009; 32: 939–948. [PMC free article] [PubMed] [Google Scholar]
- 47.Finkel KJ, Searleman AC, Tymkew H, et al. . Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med 2009; 10: 753–758. [DOI] [PubMed] [Google Scholar]
- 48.Encisco R, Clarck GT. Comparing the Berlin and the ARES questionnaire to identify patients with obstructive sleep apnea in a dental setting. Sleep Breath 2011; 15: 83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.How Ong T, Raudha S, Fook-Chong S, et al. . Simplifying STOP-BANG: use of a simple questionnaire to screen for OSA in an Asian population. Sleep Breath 2010; 14: 371–376. [DOI] [PubMed] [Google Scholar]
- 50.Chai-Coetzer CL, Antic NA, Rowland LS, et al. . A simplified model of screening questionnaire and home monitoring for obstructive sleep apnoea in primary care. Thorax 2011; 66: 213–219. [DOI] [PubMed] [Google Scholar]
- 51.Ramachandran SK, Kheterpal S, Consens F. Derivation and validation of a simple perioperative sleep apnea prediction score. Anesth Analg 2010; 110: 1007–1015. [DOI] [PubMed] [Google Scholar]
- 52.Sabers C, Plevak DJ, Schroeder DR, et al. . The diagnosis of obstructive sleep apnea as a risk factor for unanticipated admissions in outpatient surgery. Anesth Analg 2003; 96: 1328–1335. [DOI] [PubMed] [Google Scholar]
- 53.Chung F. It may be unsafe for patients with untreated severe OSA requiring postoperative narcotic to undergo ambulatory surgery. J Clin Sleep Med 2011; 7: 111–113. [PMC free article] [PubMed] [Google Scholar]
- 54.Ramachandran SK, Josephs LA. A meta-analysis of clinical screening tests for obstructive sleep apnea. Anesthesiology 2009; 110: 928–939. [DOI] [PubMed] [Google Scholar]
- 55.Ross SD, Sheinhait IA, Harrison KJ. Systematic review and meta-analysis of the literature regarding the diagnosis of sleep apnea. Sleep 2000; 23: 519–532. [PubMed] [Google Scholar]
- 56.Chiner E, Sancho-Chust JN, Barbé F. Specific diagnosis and clinical pathways in at-risk populations. In: Barbé F, Pépin J-L, eds. Obstructive Sleep Apnoea (ERS Monograph). Sheffield, European Respiratory Society, 2015; pp. 147–160. [Google Scholar]
- 57.Chung F, Nagappa M, Singh M, et al. . CPAP in the perioperative setting. Evidence of support. Chest 2016; 149: 586–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ryan CF, Lowe AA, Li D, et al. . Magnetic-resonance-imaging of the upper airway in obstructive sleep-apnea before and after chronic nasal continuous positive airway pressure therapy. Am Rev Respir Dis 1991; 144: 939–944. [DOI] [PubMed] [Google Scholar]
- 59.Vroegop AV, Smithuis JW, Benoist LB, et al. . CPAP washout prior to reevaluation polysomnography: a sleep surgeon's perspective. Sleep Breath 2015; 19: 433–439. [DOI] [PubMed] [Google Scholar]
- 60.Hedenstierna G, Edmark L. The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 2005; 31: 1327–1335. [DOI] [PubMed] [Google Scholar]
- 61.Hedenstierna G. Alveolar collapse and closure of airways: regular effects of anaesthesia. Clin Physiol Funct Imaging 2003; 23: 129–129. [DOI] [PubMed] [Google Scholar]
- 62.Coussa M, Proietti S, Schnyder P, et al. . Prevention of atelectasis formation during the induction of general anesthesia in morbidly obese patients. Anesth Analg 2004; 98: 1491–1495. [DOI] [PubMed] [Google Scholar]
- 63.Rusca M, Proietti S, Schnyder P, et al. . Prevention of atelectasis formation during induction of general anesthesia. Anesth Analg 2003; 97: 1835–1839. [DOI] [PubMed] [Google Scholar]
- 64.Herriger A, Frascarolo P, Spahn DR, et al. . The effect of positive airway pressure during pre-oxygenation and induction of anesthesia upon duration of non-hypoxic apnoea. Anaesthesia 2004; 59: 243–247. [DOI] [PubMed] [Google Scholar]
- 65.Guralnick AS, Pant M, Minhaj J, et al. . CPAP adherence in patients with newly diagnosed obstructive sleep apnea prior to elective surgery. J Clin Sleep Med 2012; 8: 501–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lan CK, Rose MW. Perioperative management of obstructive sleep apnea. Sleep Med Clin 2006; 1: 541–548. [Google Scholar]
- 67.Pawlik MT, Hansen E, Waldhauser D, et al. . Clonidine premedication in patients with sleep apnea syndrome: a randomized, double-blind, placebo-controlled study. Anesth Analg 2005; 101: 1374–1380. [DOI] [PubMed] [Google Scholar]
- 68.Liu SS, Chisholm MF, Ngeow J, et al. . Postoperative hypoxemia in orthopedic patients with obstructive sleep apnea. HSS J 2011; 7: 2–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Renotte MT, Baele P, Aubert G, et al. . Nasal continuous positive airway pressure in the perioperative management of patients with obstructive sleep apnea submitted to surgery. Chest 1995; 107: 367–374. [DOI] [PubMed] [Google Scholar]
- 70.Abdelsattar ZM, Hendren S, Wong SL, et al. . The impact of untreated obstructive sleep apnea on cardiopulmonary complications in general and vascular surgery: a cohort study. Sleep 2015; 38: 1205–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nagappa M, Mokhlesi B, Wong J, et al. . The effects of continuous positive airway pressure on postoperative outcomes in obstructive sleep apnea patients undergoig surgery: a systematic review and meta-analysis. Anesth Anal 2015; 120: 1013–1023. [DOI] [PubMed] [Google Scholar]
- 72.Mutter TC, Chateau D, Moffatt M, et al. . A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology 2014; 121: 707–718. [DOI] [PubMed] [Google Scholar]
- 73.Mehta V, Subramanyam R, Shapiro CM, et al. . Health effects of identifying patients with undiagnosed obstructive sleep apnea in the preoperative clinic: a follow-up study. Can J Anaesth 2012; 59: 544–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Neligan PJ, Malhotra G, Fraser M, et al. . Continuous positive airway pressure via the Boussignac system immediately after extubation improves lung function in morbidly obese patients with obstructive sleep apnea undergoing laparascopic bariatric surgery. Anesthesiology 2009; 110: 878–884. [DOI] [PubMed] [Google Scholar]
- 75.Neligan PJ, Malhotra G, Fraser M, et al. . Noninvasive ventilation immediately after extubation improves lung function in morbidly obese patients with obstructive sleep apnea undergoing laparascopic bariatric surgery. Anesth Anal 2010; 110: 1360–1365. [DOI] [PubMed] [Google Scholar]
- 76.Neligan PJ. Metabolic syndrome: anesthesia for morbid obesity. Curr Opin Anesth 2010; 23: 375–383. [DOI] [PubMed] [Google Scholar]
- 77.Meoli AL, Rosen CL, Kristo D, et al. . Upper airway management of the adult patient with obstructive sleep apnea in the perioperative period – Avoiding complications. Sleep 2003; 26: 1060–1065. [DOI] [PubMed] [Google Scholar]
- 78.Meng L. Postoperative nausea and vomiting with application of postoperative continuous positive airway pressure after laparascopic gastric bypass. Obes Surg 2010; 20: 876–880. [DOI] [PubMed] [Google Scholar]
- 79.Memtsoudis SG, Besculides MC, Mazumdar M. A rude awakening – the perioperative sleep apnea epidemic. N Engl J Med 2013; 368: 2352–2353. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
J. Hedner ERR-0012-2016_Hedner (1.2MB, pdf)
T. Penzel ERR-0012-2016_Penzel (1.2MB, pdf)