Abstract
Birt–Hogg–Dubé syndrome (BHD) is a rare inherited autosomal dominant disorder caused by germline mutations in the tumour suppressor gene FLCN, encoding the protein folliculin. Its clinical expression typically includes multiple pulmonary cysts, recurrent spontaneous pneumothoraces, cutaneous fibrofolliculomas and renal tumours of various histological types. BHD has no sex predilection and tends to manifest in the third or fourth decade of life. Multiple bilateral pulmonary cysts are found on chest computed tomography in >80% of patients and more than half experience one or more episodes of pneumothorax. A family history of pneumothorax is an important clue, which suggests the diagnosis of BHD. Unlike other cystic lung diseases such as lymphangioleiomyomatosis and pulmonary Langerhans cell histiocytosis, BHD does not lead to progressive loss of lung function and chronic respiratory insufficiency. Renal tumours affect about 30% of patients during their lifetime, and can be multiple and recurrent. The diagnosis of BHD is based on a combination of genetic, clinical and/or skin histopathological criteria. Management mainly consists of early pleurodesis in the case of pneumothorax, periodic renal imaging for tumour detection, and diagnostic work-up in search of BHD in relatives of the index patient.
Short abstract
Birt–Hogg–Dubé syndrome is a rare genetic disorder characterised by multiple lung cysts, recurrent pneumothoraces, skin lesions and kidney tumours. As the presenting symptoms may be respiratory, chest physicians should be able to identify this disease. https://bit.ly/2xsOTuk
Introduction
The widespread use of chest high-resolution computed tomography (HRCT) has provided better recognition of elementary lesions known as pulmonary cysts, which consist of well-delimited hyperlucent zones distributed throughout the lung parenchyma. As a result, cystic lung diseases have now become a distinct group of rare lung disorders. Among them, pulmonary lymphangioleiomyomatosis (LAM) and pulmonary Langerhans cell histiocytosis (PLCH) are now more familiar to respiratory physicians. However, the differential diagnosis of cystic lung diseases has substantially expanded in the recent years (table 1), and remains challenging. Birt–Hogg–Dubé syndrome (BHD) is a recently described cause of multiple pulmonary cysts and constitutes one of the three most important causes of cystic lung disease with LAM and PLCH. It is characterised by distinct genetic, clinical and imaging features and may involve several organs including the lung, the skin and the kidney. Knowledge of this syndrome has now become essential for the diagnostic and therapeutic approach to cystic lung diseases by the respiratory physician.
TABLE 1.
Main differential diagnosis of cystic lung diseases
| Frequency # | [Ref.] | |
| Multiple cysts as main feature | ||
| Lymphangioleiomyomatosis (sporadic or associated with tuberous sclerosis) | ∼100% | [1] |
| Pulmonary Langerhans cell histiocytosis¶ | >90% | [2] |
| Birt–Hogg–Dubé syndrome; familial pneumothorax | >80% | [3] |
| Nonamyloid Ig deposition disease | [4] | |
| Pulmonary amyloidosis | [5] | |
| Primary and metastatic neoplasms | Rare | |
| Infections, e.g. Pneumocystis jirovecii | Rare | |
| Other, e.g. Niemann–Pick disease, neurofibromatosis, Ehlers–Danlos syndrome, Proteus syndrome, MALT lymphoma, Castleman disease, congenital pulmonary airway malformation, BPD, fire-eater's lung, hyper-IgE syndrome, Erdheim–Chester disease | ||
| Multiple cysts in interstitial lung disease | ||
| Lymphocytic interstitial pneumonia | >60% | [6, 7] |
| Hypersensitivity pneumonitis (subacute/chronic) | 13–39% | [8, 9] |
| Sjögren syndrome | 14–23% | [10, 11] |
| Desquamative interstitial pneumonia | 32% | [12] |
| Follicular bronchiolitis | [13] | |
| Other, e.g. ankylosing spondylitis, lymphomatoid granulomatosis |
Ig: immunoglobin; MALT: mucosa-associated lymphoid tissue; BPD: bronchopulmonary dysplasia. #: frequency of pulmonary cysts, when available; ¶: in the early stage of pulmonary Langerhans cell histiocytosis, a purely nodular pattern can be seen.
What is BHD syndrome?
BHD is a rare inherited autosomal dominant disorder caused by germline mutations in the tumour suppressor gene FLCN, encoding the protein folliculin. Its clinical expression typically includes cutaneous fibrofolliculomas, multiple pulmonary cysts, recurrent spontaneous pneumothoraces and renal tumours of various histological types. The cutaneous features of the disease and its autosomal dominant inheritance were first described by three Canadian physicians in 1977, from whom its name derives [14]. Thereafter, several case reports suggested an association with renal tumours, pulmonary cysts and spontaneous pneumothoraces [15–18], followed by a more precise description of the syndrome in 1999 [19].
Genetics
The genetic locus involved in BHD was mapped to chromosome 17p11.2 by linkage analyses in 2001 [20, 21]. A year later, the impairment of the FLCN gene, encoding a protein designated as folliculin, was identified as causative of BHD [22]. To date, it remains the only gene involved in this syndrome. Over 200 pathogenic variants have been identified in numerous affected families [23, 24]. The majority of FLCN mutations are protein truncating, including frameshift (small deletions or insertions), nonsense or splice-site variants, which supposedly lead to a loss of function of folliculin [23]. Several pathogenic variants were identified in every coding exon of FLCN. However, the polycytosine tract of exon 11 is thought to represent a mutation hotspot, and almost half of affected individuals harbour either the c.1285delC or the c.1285dupC variants [25]. In addition, large intragenic deletions or duplications were identified in a minority of patients [26, 27]. However, disease-causing missense variants were only rarely reported [23, 28]. Mutations are often inherited from one affected parent, but can also occur de novo in individuals with no prior family history [29].
The penetrance of BHD is considered high, but the expression of the disease varies substantially among family members and between families [25, 30]. Notably, pulmonary cysts and/or relapsing pneumothoraces were reported as the only clinical manifestations in several families carrying FLCN constitutional mutations [31–34]. In this context, it has been suggested to rename BHD “FLCN (folliculin) gene-associated syndrome” or “FLCN syndrome”, which would better reflect the current state of knowledge on the disease [35]. To date, research has not established any clear correlations between the type or the position of FLCN variants and the phenotype [36]. A few studies, however, have suggested some possible genotype–phenotype associations [37–39]. In particular, Toro et al. [37] reported an increased number of pulmonary cysts in individuals harbouring mutations in exon 9, as well as more pneumothoraces in individuals carrying variants located in exons 9 and 12. Another study found a significantly increased risk of pneumothorax for carriers of mutations c.1300G>C (59%) or c.250-2A>G (77%), as compared to those with the hotspot mutation c.1285dupC [39]. Furthermore, the variant c.1285dupC was associated with a significantly higher risk of colorectal cancer than the variant c.610delGGinsTA [38].
Pathogenesis
FLCN is considered a tumour suppressor gene [40], following the two-hit hypothesis defined by Knudson [41]. Indeed, renal tumour cells of patients with BHD were shown to harbour somatic second hits mutations in FLCN or a loss of heterozygosity on the short arm of chromosome 17 [42, 43]. The exact function of folliculin, which is expressed in most tissues, including lung, skin and kidney [44, 45], is not yet completely understood. It is believed to be implicated in the regulation of cell growth, proliferation and survival through interactions with the mechanistic target of rapamycin (mTOR) signalling pathway [46, 47].
The mechanisms leading to the formation of pulmonary cysts following loss of folliculin function remain incompletely resolved. The process is thought to be driven by several dysregulated signalling pathways, including mTOR and 5′AMP-activated protein kinase [48, 49], impaired cell–cell adhesion [50] and alterations in matrix metalloproteinases caused by imbalance in extracellular matrix homeostasis [51]. A recent hypothesis suggests that cysts could arise as a consequence of deficient cell–cell adhesion and repeated stretch-induced stress caused by breathing, thus leading, over the long term, to the expansion of alveolar spaces, predominantly in lung regions where alveolar volume changes during the respiratory cycle are the most important [52]. This “stretch hypothesis” provides an explanation for the predominantly subpleural and basal distribution of pulmonary cysts in BHD. More recent data showed a decreased activity of the WNT signalling pathway in FLCN-deficient mesenchymal-lineage cells via an inhibitory effect of transcription factor TFE3 [53]. These findings suggest that WNT-dependent cell–cell communication during lung development could contribute to the formation of pulmonary cysts in BHD.
Renal cell carcinomas (RCCs) found in BHD patients are clearly different from sporadic RCC and should preferentially be called FLCN-associated RCC. In addition to their distinct histological appearance (mainly chromophobe and mixed oncocytic/chromophobe tumours) that will be discussed later in this review, they carry DNA copy-number abnormalities in addition to FLCN-somatic mutations [54, 55]. Most of the loss of heterozygosity was attributed to uniparental disomy and a specific signature was identified throughout the histological types of the FLCN-associated RCC.
Whereas sporadic RCC usually arise from proximal tubular cells, chromophobe and oncocytic tumours originate from more distal tubular cells. However, the trigger for the second hit in the distal tubules of the nephron that may eventually lead to RCC has not been identified.
Clinical picture
The disease is characterised by a wide phenotypic heterogeneity. Carriers of FLCN gene mutations may be asymptomatic, or exhibit varying degrees of cutaneous, pulmonary or renal features. Typically, affected individuals present with skin lesions and spontaneous recurrent pneumothoraces due to pulmonary cysts. Alternatively, the disease can sometimes manifest only with pulmonary cysts and/or relapsing pneumothoraces in the absence of any cutaneous or renal involvement [27, 31–34, 56]. Unlike LAM, BHD has no sex predilection [57] and can arise at any age, although it tends to emerge in the third or fourth decade of life [58]. Some data suggest a lower incidence of cutaneous and renal manifestations but a higher recurrence rate of pneumothorax in Asian patients compared to Caucasians [27, 56, 59–61].
Pulmonary manifestations
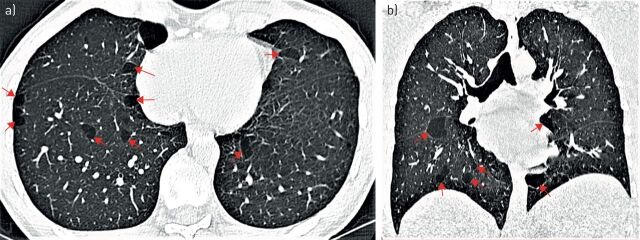
Over 80% of patients with BHD present with multiple bilateral pulmonary cysts (figure 1) [25, 37, 62]. Cysts can be found in young adults [63] but usually tend to manifest in the fourth to fifth decade of life [27, 33]. Due to the propensity of cysts to rupture, affected individuals are predisposed to spontaneous pneumothorax with a high recurrence rate. There is an estimated 50-fold higher risk of pneumothorax in BHD patients than in the general population [62]. This is much lower than in LAM, in which the risk of pneumothorax has been estimated to be 1000-fold higher than in the general female population [64]. Nevertheless, there are considerable differences in the reported prevalence rates of spontaneous pneumothorax in BHD depending on the cohorts analysed [65], with higher rates in pulmonary cohorts (42–76%) [60, 66, 67] compared to renal/dermatologic cohorts (23–38%) [25, 37, 62, 68, 69]. The mean age of occurrence of the first episode of pneumothorax was between 36 and 38 years in three large cohorts [37, 67, 69]. The recurrence rate was 75–82% with an average number of 3.6 episodes [37, 67].
FIGURE 1.
Chest computed tomography in Birt–Hogg–Dubé syndrome. a) A few pulmonary cysts of uneven distribution, size and shape in predominantly basal and paramediastinal location (arrows). b) Frontal plane reconstruction showing multiple cysts adjacent to blood vessels, fissures and visceral pleura, with predominantly basal and paramediastinal location (arrows).
The presence of pulmonary cysts, cysts number, size and total volume, as well as a family history of pneumothorax have been identified as risk factors for the occurrence of pneumothorax in BHD [37, 68]. Pulmonary cysts and/or pneumothorax have no sex predilection and are not associated with smoking or the presence and/or severity of cutaneous and renal involvement [37, 62]. BHD patients also have an increased risk of pneumothorax while diving, as well as during and following air travel, with a flight-related pneumothorax rate ranging from 0.12% to 0.63% per flight [66, 67, 70]. This could be explained by changes in atmospheric pressure in aircraft cabin during flight, which can cause cyst expansion and favour their rupture. Although most pneumothoraces occur in patients with pulmonary cysts [55], they have also been reported in the absence of any obvious cysts on HRCT [71, 72], and in children with BHD [73].
Except for episodes of pneumothorax, pulmonary cysts in BHD are generally asymptomatic or only associated with mild cough and/or exertional dyspnoea, even in patients with extensive lung involvement. Lung function data in BHD have only been reported in a few series [63, 74–78]. A report of baseline lung function in 14 patients showed nearly normal lung volumes and only minimally reduced diffusing capacity of the lung for carbon monoxide (DLCO) [75]. Another report of baseline data in 12 patients found normal lung function in 58% and mild restrictive pattern in 33% [77]. In the only large retrospective series currently available (n=96), mean values of forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), FEV1/FVC ratio and total lung capacity were normal at baseline, whereas mean residual volume was moderately increased to 116% of predicted value, and mean DLCO was moderately decreased to 85% pred at baseline [78]. When adjusted for age, sex, smoking and history of pleurodesis, lung function parameters did not significantly decline over a follow-up period of 6 years [78]. These data suggest that lung involvement in BHD does not usually lead to respiratory insufficiency, in contrast to other cystic lung diseases such as LAM or PLCH.
The occurrence of lung adenocarcinoma, atypical adenomatous hyperplasia or micronodular pneumocyte hyperplasia-like lesions have been reported in patients with BHD [33, 60, 74, 79]. However, a clear association with pulmonary tumours has not been established so far.
Cutaneous manifestations
Skin involvement is common in BHD, at least in Caucasians in whom it is found in about 80% and may be the presenting sign [14, 25, 36, 37, 59, 68, 69, 80]. In Asian patients, skin manifestations seem to be less common [60] and less typical [59, 81]. Characteristic lesions are fibrofolliculomas (figure 2) and trichodiscomas [45]. The presence of at least five such lesions, with histological confirmation in at least one, has been proposed as a major criterion for BHD diagnosis [58]. Fibrofolliculomas and trichodiscomas are considered as hamartomas of the epithelium of the follicular mantle and perifollicular tissue [82]. Acrochordons, also known as skin tags, are the third most common skin lesion in BHD. They present as small, soft, skin-coloured benign tumours with thin necks mainly distributed on the eyelids, neck and axilla. Acrochordons are not specific of BHD and are also frequent in the general population [83].
FIGURE 2.
Fibrofolliculomas in Birt–Hogg–Dubé syndrome. Multiple skin-coloured tiny papules of the paranasal area can be seen.
Skin lesions usually appear during the third to fourth decade in BHD, and occur only exceptionally before 25 years [25, 71]. Both fibrofolliculomas and trichodiscomas, now considered as different evolutionary stages of the same lesion, present as whitish to skin-coloured dome-shaped papules, with a diameter of 2–3 mm and a smooth surface (figure 2) [84]. Predilection sites are the face (especially peri nasal), the retroauricular and nuchal region, and the upper chest [14, 45, 82]. Lesions are typically multiple with sometimes more than 100 lesions present, but their number is highly variable, even within the same family.
Other skin lesions have been occasionally described in BHD patients. A comedonic and cystic variant of fibrofolliculoma has recently been reported [85]. It presents as open comedones centred in skin-coloured to white papules or cysts. In contrast to classical fibrofolliculomas, this variant may present in children and resemble nevus comedonicus [86]. Perifollicular fibromas [68, 87–89], connective tissue nevus [90], multiple angiomatous nodules [91], (angio)lipomas [18], periungual fibromas [92], angiofibromas [68, 92, 93] and intraoral papules [94] have also been described. The latter three may lead to a wrong diagnosis of tuberous sclerosis complex (TSC) [93], another genetic autosomal dominant disorder characterised by facial angiofibromas, ungual fibromas, kidney angiomyolipomas, retinal hamartomas, cortical tubers, subependymal giant cell astrocytomas and other hamartomatous lesions. In women, TSC is frequently associated with pulmonary LAM, another cystic lung disease characterised by recurrent pneumothorax and progressive destruction of the lung parenchyma. However, the other typical skin signs of TSC such as hypomelanotic macules and shagreen patches are absent in BHD. This overlap in symptoms between BHD and TSC may be due to a shared effect of the mutated proteins on signalling through the mTOR complex 1 [95]. Another differential diagnosis is familial trichodiscoma, which tends to start in childhood and is not associated with kidney or pulmonary features [96], and for which the genetic background is currently unclear. Also presenting with similar flesh-coloured facial papules are Spiegler–Brooke–Fend syndrome, Muir–Torre syndrome, Bazex–Dupré–Christol syndrome, Rombo syndrome, Gorlin–Goltz syndrome and PTEN-hamartoma syndrome (mainly Cowden syndrome). However, histopathology and genetic causes of these tumours are different [97, 98].
The above-mentioned tumours seen in BHD are benign. Some data suggest that BHD patients might have an increased risk of melanoma, but this remains controversial. There are case reports of both malignant skin [99–102] and choroidal melanoma [103, 104], which may be familial [102, 105] and/or multiple [102, 105], and even more debated reports of multiple atypical nevi [102]. One small study found a risk of melanoma in confirmed BHD as high as 10%, which is much higher than the 1.8–2.4% risk in the general population [105]. However, more studies are needed to determine whether FLCN mutations are a true risk factor for malignant melanoma.
The identification of fibrofolliculomas at skin examination should raise the suspicion of BHD and prompt further investigations to confirm the diagnosis and screen for renal tumours and pulmonary cysts. However, the finding of other lesions clinically similar to fibrofolliculomas but histologically different does not exclude the diagnosis. In these cases, biopsy of other skin lesions, investigation of other family members, and genetic analyses are important.
Renal manifestations
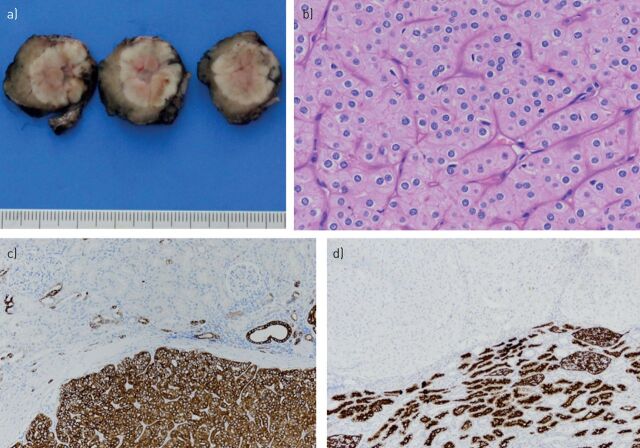
Renal cancer constitutes the most severe manifestation of BHD. Renal tumours develop in about 30% of cases [25, 60, 62, 68, 106] and the risk of developing renal cancer is increased seven-fold in patients with BHD compared to unaffected relatives [62]. Renal tumours occur at a mean age of 50 years (range 31–74 years) [106] but have also been reported in 20-year-old patients [80]. Renal tumours in BHD are multifocal and/or bilateral in more than half of cases [62, 106, 107], and may have a varied and sometimes mixed histological appearance. The malignancy potential of BHD-associated renal tumours also varies, ranging from benign oncocytomas (about 5% of cases) to malignant clear cell renal carcinomas (about 9% of cases) [106–108]. Chromophobe renal cell carcinoma (chRCC) and a mixed pattern of chRCC and oncocytoma, both associated with a low malignant potential, account for more than 70–80% of FLCN-associated renal tumours (figures 3 and 4). This frequency distribution contrasts with the large predominance of clear cell histological subtype observed in sporadic renal tumours [80, 106, 108]. Cases of papillary RCC have also been reported in BHD, as well as more undifferentiated carcinomas [80]. Angiomyolipoma, a benign kidney tumour type often encountered in LAM and TSC, is rare in BHD [75]. Renal cysts have been reported in patients with BHD, but they are also common in the general population, and whether they are really part of the BHD syndrome is currently unclear [19, 71].
FIGURE 3.
Abdominal computed tomography scan of a patient with chromophobe renal cell carcinoma after injection of contrast media. The left kidney shows an irregular edge and a homogenous mass indicated by the arrow. The tumour was removed by robot-assisted laparoscopic surgery.
FIGURE 4.
Example of a chromophobe renal cell carcinoma. a) Macroscopic appearance (scale in centimetres). b) Haematoxylin and Eosin staining (× 400). c) Staining with anti-cytokeratin-7 antibodies (× 100). d) CD10 staining (× 100). All images courtesy of Prof. La Rosa (Lausanne University Hospital, Lausanne, Switzerland)
Identification of RCCs in BHD patients is usually related to pain or macrohematuria, or found incidentally at imaging for abdominal problems or during familial or follow-up screening. In a French series, four patients had metastatic tumours at the time of initial diagnosis or later. The course of the metastatic disease was quite indolent in all patients [80, 109].
Other clinical manifestations
A large variety of benign or malignant tumours, including parotid oncocytoma [110–112], rhabdomyoma [113], parathyroid adenoma [18], breast cancer and others [3, 58], have occasionally been reported in BHD patients, but to date without established causal link with FLCN gene mutations. An initially suspected association between BHD and colorectal polyps or carcinoma [15] has not been confirmed in a series of 45 patients who underwent colonoscopic screening [62]. Nevertheless, there seems to be a genotype–phenotype correlation, as suggested by a recent study showing a significantly higher risk of colorectal cancer in a subset of patients with BHD [38].
Imaging
Chest imaging
HRCT is the imaging modality of choice for cystic lung diseases. Multiple thin-walled bilateral cysts with normal surrounding parenchyma is the characteristic radiological feature of BHD [114]. However, the sole recognition of typical pulmonary cysts on HRCT is not sufficient to confidently diagnose BHD [75]. The size, shape and number of cysts can vary greatly. They most often measure <1 cm in diameter but can range from a few millimetres to ≥2 cm [51]. They usually have visible thin uniform walls with a round, oval, lentiform or irregular shape. The largest cysts generally have a lobulated multiseptated appearance [115]. The number of cysts ranges from a few to more than 400 [37, 75, 114] with a preferential distribution in the basal, subpleural, or paramediastinal regions of the lung (figure 1) [114, 115]. The majority of patients present with <20 cysts [115] and <30% of lung volume involvement [114]. There seems to be an association between an increased risk of pneumothorax and larger cyst size as well as basal location [37, 63, 76].
The main radiological differential diagnosis of BHD is emphysema and other diffuse cystic lung diseases, especially LAM. Some morphological and distribution features are suggestive of BHD, such as large irregular lobulated or multiseptated cysts, especially when located in the subpleural lower lung regions, or the presence of cysts in the immediate vicinity or including the most proximal portion of lower pulmonary vessels [75]. In addition, the predominantly basal and medial distribution of cysts in BHD helps differentiating BHD from the apical predominance of dilated airspaces and blebs found in smoking-related emphysema and primary spontaneous pneumothorax [57]. In contrast to LAM, lung cysts in BHD are usually larger, less circular, fewer in number and with a more predominant basal and paramediastinal distribution [75, 116]. Contrary to LAM, the number and size of cysts in BHD is not thought to substantially increase over time, although data are scarce [114, 117].
Renal imaging
Subtypes of FLCN-associated RCC cannot be differentiated by imaging (figure 3), and needle biopsy and pathological analysis may provide substantial guidance in the management of renal mass in BHD patients, but its role needs to be defined [118, 119]. Regarding staging of renal carcinomas, the same staging system is used for FLCN-associated RCC and sporadic RCC and stands on the TNM staging system.
The sensitivity of various imaging modalities has been tested in a retrospective Dutch study [109]. Among 199 patients diagnosed with BHD, 172 (86%) patients had an initial renal screen. Among these cases, 121 patients were followed-up for an average of 4.2 years and a majority were closely monitored annually (83%) or at least every other year (94%). During the initial or follow-up screens, 38 renal carcinomas were identified in 23 patients at a mean age of 51 years. Ultrasound was performed in 18 of the 38 tumours, and detected tumours of 20 to 120 mm in diameter in nine cases. However, renal ultrasound missed nine small tumours of 7–27 mm in diameter that were discovered by computed tomography (CT) or magnetic resonance imaging (MRI). Of note, four patients presented with metastatic RCC at the time of BHD diagnosis.
Histopathology
Pulmonary features
The histopathological features of ruptured cysts resected as part of the surgical management of spontaneous pneumothorax consist of nonspecific abnormalities that are undistinguishable from emphysema, with the exception of the basal predominance of lesions [120]. Conversely, the examination of unruptured cysts showed epithelial cells lining the inner surface of the cysts, without any associated abnormalities such as aberrant cellular proliferation or atypia, nor inflammatory or fibrosing component [48, 121]. Cysts are located in close vicinity of the interlobular septa and/or visceral pleura, and each lesion merges on one side with interstitial stroma of the interlobular septum and/or pleura, and on the other side with normal alveolar structures.
The predominantly basal distribution of the cysts and the presence of normal surrounding parenchyma without neoplastic cell proliferation or inflammation was recently confirmed in an analysis of 229 cysts from 50 BHD patients [122]. Additionally, the lesions were typically located within the lung parenchyma without obvious connection to the bronchi, frequently abutting interlobular septa and sometimes containing intracystic structures composed of interlobular septa. These findings and the distinctive spatial distribution of the cysts provide additional arguments to support that lung involvement in BHD is different from centrilobular apical emphysema and subpleural bullae.
Renal tumours
Most of the series of FLCN-associated RCC from various countries agree on a variety of histological findings that differs from sporadic RCC. Chromophobe, clear, papillary, oncocytic and sarcomatoid cells have been described among the FLCN-associated RCC, and most of the time a mix of several of these cells coexist. Proportions of the various histological types vary among series, which may be due to a lack of standardisation or difficulties at defining the precise histological type [69]. However, a majority of chromophobe (figure 4), oncocytic or mixed chromophobe/oncocytic cells are encountered. RCC of clear cell type have been described in 9–48% of cases [80, 123]. Even if chromophobe and/or oncocytic type are predominant, and although the BHD Consortium guidelines [58] propose that these types should alert for BHD, the high frequency of clear cell RCC in some BHD series make this recommendation less stringent.
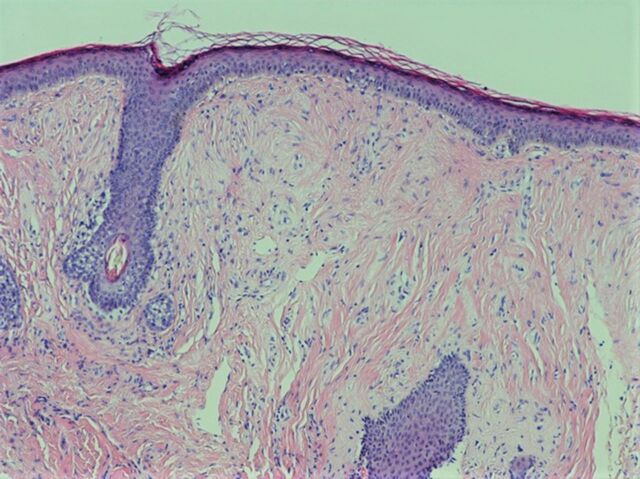
Skin abnormalities
Suspicion of BHD needs histological confirmation if skin lesions are present, which is the case in most families. Only histology can discriminate between fibrofolliculomas, trichodiscomas, perifollicular fibromas [82, 88, 98] or atypical angiofibromas [84, 93], as they are clinically indistinguishable. It is also important to differentiate them from similar lesions such as trichofolliculomas, basaliomas and others. Fibrofolliculomas are centred around a well-developed hair follicle, from which delicate epithelial cords of immature basaloid cells emanate in the loose connective tissue surrounding the central follicle. They anastomose among them and with the epithelium of the central hair follicle, resulting in a retiform pattern [82] (figure 5). Especially in the cystic fibrofolliculoma, the hair follicles appear cystically dilated and contain keratinous debris. In contrast, trichodiscomas are well-delimited lesions composed of a prominent stroma of thin collagen fibres, star-shaped fibrocytes and abundant mucin with, at the lateral margins, a collarette of large lobules of mature sebocytes which appear to embrace the lesion as a mitt or “hand of bananas” [82]. In some cases, a prominent vascular component is seen in the stroma of the lesion, which is then called a perivascular fibroma [82]. Both fibrofolliculomas and trichodiscomas may be present in the same patient, or even in different parts of the same lesion [82, 98], and are thought to belong to the same spectrum [82, 97].
FIGURE 5.
Histopathology of a fibrofolliculoma with fibroblast-rich mesenchymal tissue in the whole dermal space (Haematoxylin and Eosin stain, ×100). Copyright of this figure belongs to D. Hohl.
Diagnosis of BHD
Because of its rarity, BHD is likely underdiagnosed and mistaken for primary spontaneous pneumothorax, emphysema, LAM or another cystic lung disease. Furthermore, its broad spectrum of clinical expression makes it difficult to identify and can delay the diagnosis, sometimes by years [67]. However, an early diagnosis is important to set up screening for renal cancer in patients and affected relatives.
The most frequent expression of the disease leading to the diagnosis of BHD is spontaneous pneumothorax, although generally only after the second episode [67]. BHD is thought to be the cause of 5–10% of apparent primary spontaneous pneumothorax [56, 124–126]. In patients presenting with apparent primary spontaneous pneumothorax, a positive family history of pneumothorax was highly predictive of BHD diagnosis, with prevalence rates of 64–86% [125, 126]. Indeed, BHD appears to be the single most common cause of familial pneumothorax [127]. One study suggested that, in patients presenting with apparent primary pneumothorax, HRCT screening for an underlying diffuse cystic lung disease such as BHD, LAM or PLCH is cost-effective and should be recommended [67]. A simple clinical scoring system has also been proposed to identify patients with BHD with high sensitivity and specificity among those presenting with apparent primary spontaneous pneumothorax, in the absence of HRCT [126]. The role of radiologists in suggesting a diagnosis of BHD based on chest HRCT in the absence of clinical suspicion has also been highlighted [128].
In the case of suspicion of BHD, it is recommended to carefully search for personal and family history of skin lesions, pneumothorax, lung cysts and renal tumours, as they represent prominent diagnostic clues of the disease. If present, further investigations are required, including skin examination by a dermatologist with punch biopsy of suggestive cutaneous lesions, screening for renal tumours with abdominal CT or MRI, chest HRCT with review of cysts distribution and morphology by an expert radiologist, and pulmonary function testing [57]. Finally, a genetic evaluation and counselling for genetic testing should be proposed to confirm the diagnosis.
FLCN sequence analysis of the coding and flanking intronic regions in patients who fulfil the clinical diagnostic criteria for BHD has a diagnostic yield of almost 90% [68, 129]. When no pathogenic variant is detected by sequence analysis, search for a deletion/duplication using other techniques like multiplex ligation-dependant probe should be considered [129]. It is worth noting that a negative FLCN gene testing does not exclude the diagnosis.
Confirmation of BHD diagnosis relies on a combination of clinical features and/or identification of a FLCN germline mutation. Two diagnostic algorithms have been proposed (table 2), but still await formal validation [57, 58]. Regarding kidney involvement, the identification of multifocal or bilateral renal cancer is very suggestive of BHD, and a histological diagnosis of mixed chromophobe and oncocytic tumour is almost pathognomonic of the syndrome.
TABLE 2.
Diagnostic criteria for Birt–Hogg–Dubé (BHD) syndrome
| Diagnostic criteria proposed by Menko [58] |
| Patient should fulfil one major or two minor criteria for diagnosis |
| Major criteria: |
| At least five fibrofolliculomas or trichodiscomas, at least one histologically confirmed, of adult onset |
| Pathogenic FLCN germline mutation |
| Minor criteria: |
| Multiple lung cysts: bilateral basally located lung cysts with no other apparent cause, with or without spontaneous primary pneumothorax |
| Renal cancer: early onset (age <50 years) or multifocal or bilateral renal cancer, or renal cancer of mixed chromophobe and oncocytic histology |
| A first-degree relative with BHD |
| Diagnostic criteria proposed by Gupta [57] |
| Definite pulmonary BHD: |
| Characteristic# or compatible¶ lung HRCT and skin biopsy positive for fibrofolliculoma or trichodiscoma |
| Characteristic or compatible lung HRCT and confirmed family history of BHD in first- or second-degree family member |
| Characteristic or compatible lung HRCT, and tissue confirmation or renal chromophobe adenoma or oncocytoma |
| Characteristic or compatible lung HRCT, and tissue confirmation of genetic testing positive for BHD |
| Probable pulmonary BHD: |
| Characteristic HRCT, exclusion of TSC and LAM, and personal or family history of pneumothorax |
| Compatible HRCT, exclusion of TSC and LAM, and any of the following: |
| Family or personal history of renal tumours |
| Skin angiofibroma |
| Renal angiomyolipoma |
| Possible pulmonary BHD: |
| Compatible or characteristic HRCT |
HRCT: high-resolution computed tomography; TSC: tuberous sclerosis complex; LAM: lymphangioleiomyomatosis. #: multiple thin-walled round, elliptical or lentiform, well-defined air-filled cysts, without internal structure, in a basilar, medial and subpleural predominant distribution, with preserved or increased lung volume, and no other significant pulmonary involvement (specifically no interstitial lung disease); ¶: thin-walled cysts without the more typical elliptical shape or subpleural distribution.
Management and prognosis
Early diagnosis of the disease, early identification and treatment of renal tumours, and prevention of pneumothorax are the main aspects to consider in the management of BHD. Family members at risk should be offered screening for lung and kidney involvement, as pulmonary cysts and renal tumours are highly prevalent in BHD. Diagnostic/presymptomatic genetic testing should also be discussed when the familial mutation is known.
Management of pulmonary involvement
There is currently no specific treatment for BHD-associated cystic lung disease and whether mTOR inhibitors are effective in preventing cysts formation is unknown. Therefore, management of pulmonary involvement is limited to preventing and treating pneumothoraces [57]. Because of the high recurrence rate of pneumothorax, it is recommended to consider pleurodesis after the first episode of spontaneous pneumothorax [57]. In one retrospective series, the risk of relapse was significantly reduced from >60% with conservative treatment to around 30% after pleurodesis [67]. In another retrospective series reporting the efficacy of surgical pleurodesis with a cellulose mesh covering the visceral pleura, total pleural covering was significantly more effective than lower pleural covering, with 0% versus 42% recurrence rate at 7.5 years [130]. It is important to inform patients about the risk and symptoms of pneumothorax, and to recommend medical assessment in case of new respiratory symptoms such as dyspnoea or chest pain. Patients should also be discouraged from diving. In spite of the slightly increased risk of pneumothorax observed during and after a flight, it seems unnecessary to advise against air travel [66]. However, in case of an ongoing or recently treated pneumothorax, patients should be advised to avoid travelling by air. Given that pulmonary function tests are essentially normal and cystic lung disease only rarely impacts lung function, it is not recommended to perform regular follow-up with pulmonary function tests and/or chest HRCT in the majority of patients. However, periodic pulmonary function testing should be provided to patients with extensive cystic lung disease and impaired lung function at baseline [57]. Even if there is no obvious causal association between tobacco and the occurrence of pulmonary cysts, pneumothorax or BHD-associated lung function decline, patients should be discouraged from smoking, and smokers should receive smoking cessation advice or counselling. Pneumococcal vaccination and annual influenza vaccination are recommended.
Management of renal involvement
Screening for renal tumours should be proposed to all BHD patients at diagnosis or starting from the age of 20 years [131]. After initial imaging, lifelong follow-up is recommended every 3 to 4 years to identify any tumour at an early stage. As renal ultrasound may not be sensitive enough to detect small lesions [132] and to avoid the cumulative radiation exposure of repeated CT, MRI is the recommended imaging modality [54, 131], even though no series has prospectively validated this strategy. Most BHD-associated renal tumours have a low malignant potential and a favourable prognosis. As several tumours may develop during lifetime, a delayed nephron-sparing strategy is favoured to preserve kidney function over time [54, 131]. Additionally, prior surgery may complicate subsequent resections and interfere with imaging interpretation. Therefore, if one or more tumours are detected, it is recommended to postpone surgery until the largest mass reaches 3 cm in diameter, with subsequent imaging intervals depending on the type, size and growth rate of the lesions [54, 106, 131, 133]. When surgery is not feasible, radiofrequency ablation or cryotherapy are alternative nephron-sparing techniques. A long-term beneficial effect of everolimus has been reported in one Japanese patient with BHD and metastatic renal cancer [134], but more studies are needed to assess the efficacy of mTOR inhibitors in BHD-associated renal cancer. Metastatic disease is usually treated the same way as other metastatic RCC, even though no prospective studies have specifically addressed this issue.
Management of cutaneous involvement
Skin lesions of BHD do not need therapy, as there is no risk of malignant transformation. For aesthetic reasons however, excision, debulking, ablative laser treatment (CO2 or Erb-Yag laser) [135, 136] or electrodessication can be proposed [58]. However, recurrence may occur. One study failed to demonstrate a significant cosmetic improvement with topical sirolimus [137], in contrast to its effect on angiofibromas in TSC.
Conclusion
As one of the three main causes of cystic lung diseases found at HRCT and present in up to 10% of patients with apparently spontaneous pneumothorax, BHD is now for the respiratory physician an important diagnosis to consider. When BHD is suspected, a multidisciplinary approach involving respiratory physicians, radiologists, geneticists, nephrologists, dermatologists, thoracic surgeons and pathologists is needed to confirm the diagnosis and to implement the appropriate follow-up, especially periodic kidney imaging for early detection of renal cancer. When BHD has been identified in an index patient, a diagnostic work-up of family members is another important step in the management of this genetic disorder with dominant autosomal transmission.
Acknowledgements
The authors acknowledge Stefano La Rosa (Department of Pathology, Lausanne University Hospital, Lausanne, Switzerland) for providing figure 4 and Sibylle Menal for secretarial assistance.
Footnotes
Provenance: Commissioned article, peer reviewed.
Number 1 in the Series “Rare genetic interstitial lung diseases” Edited by Bruno Crestani and Raphaël Borie
Conflict of interest: C. Daccord reports non-financial support from Boehringer-Ingelheim and Roche, outside the submitted work.
Conflict of interest: J-M. Good has nothing to disclose.
Conflict of interest: M-A. Morren has nothing to disclose.
Conflict of interest: O. Bonny has nothing to disclose.
Conflict of interest: D. Hohl has nothing to disclose.
Conflict of interest: R. Lazor reports personal fees and non-financial support from Boehringer-Ingelheim, and non-financial support from Roche and Vifor, outside the submitted work.
References
- 1.Johnson SR, Cordier JF, Lazor R, et al. . European Respiratory Society guidelines for the diagnosis and management of lymphangioleiomyomatosis. Eur Respir J 2010; 35: 14–26. doi: 10.1183/09031936.00076209 [DOI] [PubMed] [Google Scholar]
- 2.Brauner MW, Grenier P, Mouelhi MM, et al. . Pulmonary histiocytosis X: evaluation with high-resolution CT. Radiology 1989; 172: 255–258. doi: 10.1148/radiology.172.1.2787036 [DOI] [PubMed] [Google Scholar]
- 3.Gupta N, Sunwoo BY, Kotloff RM. Birt–Hogg–Dubé syndrome. Clin Chest Med 2016; 37: 475–486. doi: 10.1016/j.ccm.2016.04.010 [DOI] [PubMed] [Google Scholar]
- 4.Colombat M, Stern M, Groussard O, et al. . Pulmonary cystic disorder related to light chain deposition disease. Am J Respir Crit Care Med 2006; 173: 777–780. doi: 10.1164/rccm.200510-1620CR [DOI] [PubMed] [Google Scholar]
- 5.Zamora AC, White DB, Sykes AM, et al. . Amyloid-associated cystic lung disease. Chest 2016; 149: 1223–1233. doi: 10.1378/chest.15-1539 [DOI] [PubMed] [Google Scholar]
- 6.Johkoh T, Muller NL, Pickford HA, et al. . Lymphocytic interstitial pneumonia: thin-section CT findings in 22 patients. Radiology 1999; 212: 567–572. doi: 10.1148/radiology.212.2.r99au05567 [DOI] [PubMed] [Google Scholar]
- 7.Honda O, Johkoh T, Ichikado K, et al. . Differential diagnosis of lymphocytic interstitial pneumonia and malignant lymphoma on high-resolution CT. AJR Am J Roentgenol 1999; 173: 71–74. doi: 10.2214/ajr.173.1.10397102 [DOI] [PubMed] [Google Scholar]
- 8.Franquet T, Hansell DM, Senbanjo T, et al. . Lung cysts in subacute hypersensitivity pneumonitis. J Comput Assist Tomogr 2003; 27: 475–478. doi: 10.1097/00004728-200307000-00003 [DOI] [PubMed] [Google Scholar]
- 9.Silva CI, Muller NL, Lynch DA, et al. . Chronic hypersensitivity pneumonitis: differentiation from idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia by using thin-section CT. Radiology 2008; 246: 288–297. doi: 10.1148/radiol.2453061881 [DOI] [PubMed] [Google Scholar]
- 10.Lechtman S, Debray MP, Crestani B, et al. . Cystic lung disease in Sjögren's syndrome: an observational study. Joint Bone Spine 2017; 84: 317–321. doi: 10.1016/j.jbspin.2016.05.019 [DOI] [PubMed] [Google Scholar]
- 11.Uffmann M, Kiener HP, Bankier AA, et al. . Lung manifestation in asymptomatic patients with primary Sjögren syndrome: assessment with high resolution CT and pulmonary function tests. J Thorac Imaging 2001; 16: 282–289. doi: 10.1097/00005382-200110000-00009 [DOI] [PubMed] [Google Scholar]
- 12.Hartman TE, Primack SL, Swensen SJ, et al. . Desquamative interstitial pneumonia: thin-section CT findings in 22 patients. Radiology 1993; 187: 787–790. doi: 10.1148/radiology.187.3.8497631 [DOI] [PubMed] [Google Scholar]
- 13.Lu J, Ma M, Zhao Q, et al. . The clinical characteristics and outcomes of follicular bronchiolitis in Chinese adult patients. Sci Rep 2018; 8: 7300. doi: 10.1038/s41598-018-25670-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Birt AR, Hogg GR, Dube WJ. Hereditary multiple fibrofolliculomas with trichodiscomas and acrochordons. Arch Dermatol 1977; 113: 1674–1677. doi: 10.1001/archderm.1977.01640120042005 [DOI] [PubMed] [Google Scholar]
- 15.Hornstein OP, Knickenberg M. Perifollicular fibromatosis cutis with polyps of the colon – a cutaneo-intestinal syndrome sui generis. Arch Dermatol Res 1975; 253: 161–175. doi: 10.1007/BF00582068 [DOI] [PubMed] [Google Scholar]
- 16.Binet O, Robin J, Vicart M, et al. . Fibromes perifolliculaires, polypose colique familiale, pneumothorax spontanés familiaux. Ann Dermatol Venereol 1986; 113: 928–930. [Google Scholar]
- 17.Roth JS, Rabinowitz AD, Benson M, et al. . Bilateral renal cell carcinoma in the Birt–Hogg–Dubé syndrome. J Am Acad Dermatol 1993; 29: 1055–1056. doi: 10.1016/S0190-9622(08)82049-X [DOI] [PubMed] [Google Scholar]
- 18.Chung JY, Ramos-Caro FA, Beers B, et al. . Multiple lipomas, angiolipomas, and parathyroid adenomas in a patient with Birt–Hogg–Dubé syndrome. Int J Dermatol 1996; 35: 365–367. doi: 10.1111/j.1365-4362.1996.tb03642.x [DOI] [PubMed] [Google Scholar]
- 19.Toro JR, Glenn G, Duray P, et al. . Birt–Hogg–Dubé syndrome: a novel marker of kidney neoplasia. Arch Dermatol 1999; 135: 1195–1202. [DOI] [PubMed] [Google Scholar]
- 20.Khoo SK, Bradley M, Wong FK, et al. . Birt–Hogg–Dubé syndrome: mapping of a novel hereditary neoplasia gene to chromosome 17p12-q11.2. Oncogene 2001; 20: 5239–5242. doi: 10.1038/sj.onc.1204703 [DOI] [PubMed] [Google Scholar]
- 21.Schmidt LS, Warren MB, Nickerson ML, et al. . Birt–Hogg–Dubé syndrome, a genodermatosis associated with spontaneous pneumothorax and kidney neoplasia, maps to chromosome 17p11.2. Am J Hum Genet 2001; 69: 876–882. doi: 10.1086/323744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nickerson ML, Warren MB, Toro JR, et al. . Mutations in a novel gene lead to kidney tumors, lung wall defects, and benign tumors of the hair follicle in patients with the Birt–Hogg–Dubé syndrome. Cancer Cell 2002; 2: 157–164. doi: 10.1016/S1535-6108(02)00104-6 [DOI] [PubMed] [Google Scholar]
- 23.Lim DH, Rehal PK, Nahorski MS, et al. . A new locus-specific database (LSDB) for mutations in the folliculin (FLCN) gene. Hum Mutat 2010; 31: E1043–E1051. doi: 10.1002/humu.21130 [DOI] [PubMed] [Google Scholar]
- 24.European BHD Consortium. www.europeanbhdconsortium.eu/. Date last accessed: August 15, 2020.
- 25.Schmidt LS, Nickerson ML, Warren MB, et al. . Germline BHD-mutation spectrum and phenotype analysis of a large cohort of families with Birt–Hogg–Dubé syndrome. Am J Hum Genet 2005; 76: 1023–1033. doi: 10.1086/430842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Benhammou JN, Vocke CD, Santani A, et al. . Identification of intragenic deletions and duplication in the FLCN gene in Birt–Hogg–Dubé syndrome. Genes Chromosomes Cancer 2011; 50: 466–477. doi: 10.1002/gcc.20872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kunogi M, Kurihara M, Ikegami TS, et al. . Clinical and genetic spectrum of Birt–Hogg–Dubé syndrome patients in whom pneumothorax and/or multiple lung cysts are the presenting feature. J Med Genet 2010; 47: 281–287. doi: 10.1136/jmg.2009.070565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nahorski MS, Reiman A, Lim DH, et al. . Birt–Hogg–Dubé syndrome-associated FLCN mutations disrupt protein stability. Hum Mutat 2011; 32: 921–929. doi: 10.1002/humu.21519 [DOI] [PubMed] [Google Scholar]
- 29.Menko FH, Johannesma PC, van Moorselaar RJ, et al. . A de novo FLCN mutation in a patient with spontaneous pneumothorax and renal cancer; a clinical and molecular evaluation. Fam Cancer 2013; 12: 373–379. doi: 10.1007/s10689-012-9593-8 [DOI] [PubMed] [Google Scholar]
- 30.Sattler EC, Steinlein OK. Delayed diagnosis of Birt–Hogg–Dubé syndrome due to marked intrafamilial clinical variability: a case report. BMC Med Genet 2018; 19: 45. doi: 10.1186/s12881-018-0558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Graham RB, Nolasco M, Peterlin B, et al. . Nonsense mutations in folliculin presenting as isolated familial spontaneous pneumothorax in adults. Am J Respir Crit Care Med 2005; 172: 39–44. doi: 10.1164/rccm.200501-143OC [DOI] [PubMed] [Google Scholar]
- 32.Painter JN, Tapanainen H, Somer M, et al. . A 4-bp deletion in the Birt–Hogg–Dubé gene (FLCN) causes dominantly inherited spontaneous pneumothorax. Am J Hum Genet 2005; 76: 522–527. doi: 10.1086/428455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gunji Y, Akiyoshi T, Sato T, et al. . Mutations of the Birt–Hogg–Dubé gene in patients with multiple lung cysts and recurrent pneumothorax. J Med Genet 2007; 44: 588–593. doi: 10.1136/jmg.2007.049874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frohlich BA, Zeitz C, Matyas G, et al. . Novel mutations in the folliculin gene associated with spontaneous pneumothorax. Eur Respir J 2008; 32: 1316–1320. doi: 10.1183/09031936.00132707 [DOI] [PubMed] [Google Scholar]
- 35.Cottin V, Cordier JF, Khouatra C, et al. . Multiple cystic lung diseases. In: Cottin V, Cordier JF, Richeldi L, eds. Orphan Lung Diseases: A Clinical Guide to Rare Lung Disease. London, Springer-Verlag, 2015; pp. 253–270. [Google Scholar]
- 36.Schmidt LS, Linehan WM. Molecular genetics and clinical features of Birt–Hogg–Dubé syndrome. Nat Rev Urol 2015; 12: 558–569. doi: 10.1038/nrurol.2015.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Toro JR, Pautler SE, Stewart L, et al. . Lung cysts, spontaneous pneumothorax, and genetic associations in 89 families with Birt–Hogg–Dubé syndrome. Am J Respir Crit Care Med 2007; 175: 1044–1053. doi: 10.1164/rccm.200610-1483OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nahorski MS, Lim DH, Martin L, et al. . Investigation of the Birt–Hogg–Dubé tumour suppressor gene (FLCN) in familial and sporadic colorectal cancer. J Med Genet 2010; 47: 385–390. doi: 10.1136/jmg.2009.073304 [DOI] [PubMed] [Google Scholar]
- 39.Sattler EC, Syunyaeva Z, Mansmann U, et al. . Genetic risk factors for spontaneous pneumothorax in Birt–Hogg–Dubé syndrome. Chest 2020; 157: 1199–1206. [DOI] [PubMed] [Google Scholar]
- 40.Hong SB, Oh H, Valera VA, et al. . Tumor suppressor FLCN inhibits tumorigenesis of a FLCN-null renal cancer cell line and regulates expression of key molecules in TGF-β signaling. Mol Cancer 2010; 9: 160. doi: 10.1186/1476-4598-9-160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Knudson AG J. Mutation and cancer: statistical study of retinoblastoma. Proc Natl Acad Sci USA 1971; 68: 820–823. doi: 10.1073/pnas.68.4.820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Khoo SK, Kahnoski K, Sugimura J, et al. . Inactivation of BHD in sporadic renal tumors. Cancer Res 2003; 63: 4583–4587. [PubMed] [Google Scholar]
- 43.Vocke CD, Yang Y, Pavlovich CP, et al. . High frequency of somatic frameshift BHD gene mutations in Birt–Hogg–Dubé-associated renal tumors. J Natl Cancer Inst 2005; 97: 931–935. doi: 10.1093/jnci/dji154 [DOI] [PubMed] [Google Scholar]
- 44.Warren MB, Torres-Cabala CA, Turner ML, et al. . Expression of Birt–Hogg–Dubé gene mRNA in normal and neoplastic human tissues. Mod Pathol 2004; 17: 998–1011. doi: 10.1038/modpathol.3800152 [DOI] [PubMed] [Google Scholar]
- 45.Adley BP, Smith ND, Nayar R, et al. . Birt–Hogg–Dubé syndrome: clinicopathologic findings and genetic alterations. Arch Pathol Lab Med 2006; 130: 1865–1870. [DOI] [PubMed] [Google Scholar]
- 46.Baba M, Hong SB, Sharma N, et al. . Folliculin encoded by the BHD gene interacts with a binding protein, FNIP1, and AMPK, and is involved in AMPK and mTOR signaling. Proc Natl Acad Sci USA 2006; 103: 15552–15557. doi: 10.1073/pnas.0603781103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hartman TR, Nicolas E, Klein-Szanto A, et al. . The role of the Birt–Hogg–Dubé protein in mTOR activation and renal tumorigenesis. Oncogene 2009; 28: 1594–1604. doi: 10.1038/onc.2009.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Furuya M, Tanaka R, Koga S, et al. . Pulmonary cysts of Birt–Hogg–Dubé syndrome: a clinicopathologic and immunohistochemical study of 9 families. Am J Surg Pathol 2012; 36: 589–600. doi: 10.1097/PAS.0b013e3182475240 [DOI] [PubMed] [Google Scholar]
- 49.Goncharova EA, Goncharov DA, James ML, et al. . Folliculin controls lung alveolar enlargement and epithelial cell survival through E-cadherin, LKB1, and AMPK. Cell Rep 2014; 7: 412–423. doi: 10.1016/j.celrep.2014.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Khabibullin D, Medvetz DA, Pinilla M, et al. . Folliculin regulates cell-cell adhesion, AMPK, and mTORC1 in a cell-type-specific manner in lung-derived cells. Physiol Rep 2014; 2: e12107. doi: 10.14814/phy2.12107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dal Sasso AA, Belem LC, Zanetti G, et al. . Birt–Hogg–Dubé syndrome. State-of-the-art review with emphasis on pulmonary involvement. Respir Med 2015; 109: 289–296. doi: 10.1016/j.rmed.2014.11.008 [DOI] [PubMed] [Google Scholar]
- 52.Kennedy JC, Khabibullin D, Henske EP. Mechanisms of pulmonary cyst pathogenesis in Birt–Hogg–Dubé syndrome: the stretch hypothesis. Semin Cell Dev Biol 2016; 52: 47–52. doi: 10.1016/j.semcdb.2016.02.014 [DOI] [PubMed] [Google Scholar]
- 53.Kennedy JC, Khabibullin D, Hougard T, et al. . Loss of FLCN inhibits canonical WNT signaling via TFE3. Hum Mol Genet 2019; 28: 3270–3281. doi: 10.1093/hmg/ddz158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schmidt LS, Linehan WM. Clinical features, genetics and potential therapeutic approaches for Birt–Hogg–Dubé syndrome. Expert Opin Orphan Drugs 2015; 3: 15–29. doi: 10.1517/21678707.2014.987124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Iribe Y, Yao M, Tanaka R, et al. . Genome-wide uniparental disomy and copy number variations in renal cell carcinomas associated with Birt–Hogg–Dubé syndrome. Am J Pathol 2016; 186: 337–346. doi: 10.1016/j.ajpath.2015.10.013 [DOI] [PubMed] [Google Scholar]
- 56.Ren HZ, Zhu CC, Yang C, et al. . Mutation analysis of the FLCN gene in Chinese patients with sporadic and familial isolated primary spontaneous pneumothorax. Clin Genet 2008; 74: 178–183. doi: 10.1111/j.1399-0004.2008.01030.x [DOI] [PubMed] [Google Scholar]
- 57.Gupta N, Seyama K, McCormack FX. Pulmonary manifestations of Birt–Hogg–Dubé syndrome. Fam Cancer 2013; 12: 387–396. doi: 10.1007/s10689-013-9660-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Menko FH, van Steensel MA, Giraud S, et al. . Birt–Hogg–Dubé syndrome: diagnosis and management. Lancet Oncol 2009; 10: 1199–1206. doi: 10.1016/S1470-2045(09)70188-3 [DOI] [PubMed] [Google Scholar]
- 59.Murakami Y, Wataya-Kaneda M, Tanaka M, et al. . Two Japanese cases of Birt–Hogg–Dubé syndrome with pulmonary cysts, fibrofolliculomas, and renal cell carcinomas. Case Rep Dermatol 2014; 6: 20–28. doi: 10.1159/000358216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Furuya M, Yao M, Tanaka R, et al. . Genetic, epidemiologic and clinicopathologic studies of Japanese Asian patients with Birt–Hogg–Dubé syndrome. Clin Genet 2016; 90: 403–412. doi: 10.1111/cge.12807 [DOI] [PubMed] [Google Scholar]
- 61.Park HJ, Park CH, Lee SE, et al. . Birt–Hogg–Dubé syndrome prospectively detected by review of chest computed tomography scans. PLoS One 2017; 12: e0170713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zbar B, Alvord WG, Glenn G, et al. . Risk of renal and colonic neoplasms and spontaneous pneumothorax in the Birt–Hogg–Dubé syndrome. Cancer Epidemiol Biomarkers Prev 2002; 11: 393–400. [PubMed] [Google Scholar]
- 63.Tomassetti S, Carloni A, Chilosi M, et al. . Pulmonary features of Birt–Hogg–Dubé syndrome: cystic lesions and pulmonary histiocytoma. Respir Med 2011; 105: 768–774. doi: 10.1016/j.rmed.2011.01.002 [DOI] [PubMed] [Google Scholar]
- 64.Gonano C, Pasquier J, Daccord C, et al. . Air travel and incidence of pneumothorax in lymphangioleiomyomatosis. Orphanet J Rare Dis 2018; 13: 222. doi: 10.1186/s13023-018-0964-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cooley J, Lee YCG, Gupta N. Spontaneous pneumothorax in diffuse cystic lung diseases. Curr Opin Pulm Med 2017; 23: 323–333. doi: 10.1097/MCP.0000000000000391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Johannesma PC, van de Beek I, van der Wel JW, et al. . Risk of spontaneous pneumothorax due to air travel and diving in patients with Birt–Hogg–Dubé syndrome. Springerplus 2016; 5: 1506. doi: 10.1186/s40064-016-3009-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gupta N, Kopras EJ, Henske EP, et al. . Spontaneous pneumothoraces in patients with Birt–Hogg–Dubé syndrome. Ann Am Thorac Soc 2017; 14: 706–713. doi: 10.1513/AnnalsATS.201611-886OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Toro JR, Wei MH, Glenn GM, et al. . BHD mutations, clinical and molecular genetic investigations of Birt–Hogg–Dubé syndrome: a new series of 50 families and a review of published reports. J Med Genet 2008; 45: 321–331. doi: 10.1136/jmg.2007.054304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Houweling AC, Gijezen LM, Jonker MA, et al. . Renal cancer and pneumothorax risk in Birt–Hogg–Dubé syndrome; an analysis of 115 FLCN mutation carriers from 35 BHD families. Br J Cancer 2011; 105: 1912–1919. doi: 10.1038/bjc.2011.463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Postmus PE, Johannesma PC, Menko FH, et al. . In-flight pneumothorax: diagnosis may be missed because of symptom delay. Am J Respir Crit Care Med 2014; 190: 704–705. doi: 10.1164/rccm.201404-0698LE [DOI] [PubMed] [Google Scholar]
- 71.Kluger N, Giraud S, Coupier I, et al. . Birt–Hogg–Dubé syndrome: clinical and genetic studies of 10 French families. Br J Dermatol 2010; 162: 527–537. doi: 10.1111/j.1365-2133.2009.09517.x [DOI] [PubMed] [Google Scholar]
- 72.Onuki T, Goto Y, Kuramochi M, et al. . Radiologically indeterminate pulmonary cysts in Birt–Hogg–Dubé syndrome. Ann Thorac Surg 2014; 97: 682–685. doi: 10.1016/j.athoracsur.2013.05.120 [DOI] [PubMed] [Google Scholar]
- 73.Geilswijk M, Bendstrup E, Madsen MG, et al. . Childhood pneumothorax in Birt–Hogg–Dubé syndrome: a cohort study and review of the literature. Mol Genet Genomic Med 2018; 6: 332–338. doi: 10.1002/mgg3.373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ayo DS, Aughenbaugh GL, Yi ES, et al. . Cystic lung disease in Birt–Hogg–Dubé syndrome. Chest 2007; 132: 679–684. doi: 10.1378/chest.07-0042 [DOI] [PubMed] [Google Scholar]
- 75.Tobino K, Hirai T, Johkoh T, et al. . Differentiation between Birt–Hogg–Dubé syndrome and lymphangioleiomyomatosis: quantitative analysis of pulmonary cysts on computed tomography of the chest in 66 females. Eur J Radiol 2012; 81: 1340–1346. doi: 10.1016/j.ejrad.2011.03.039 [DOI] [PubMed] [Google Scholar]
- 76.Skolnik K, Tsai WH, Dornan K, et al. . Birt–Hogg–Dubé syndrome: a large single-family cohort. Respir Res 2016; 17: 22. doi: 10.1186/s12931-016-0339-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lee JH, Jeon MJ, Song JS, et al. . Birt–Hogg–Dubé syndrome in Korean: clinicoradiologic features and long-term follow-up. Korean J Intern Med 2019; 34: 830–840. doi: 10.3904/kjim.2018.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Daccord C, Cottin V, Prévôt G, et al. . Lung function in Birt–Hogg–Dubé syndrome: a retrospective analysis of 96 patients. Orphanet J Rare Dis 2020; 15: 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nishida C, Yatera K, Yamasaki K, et al. . Possible familial case of Birt–Hogg–Dubé syndrome complicated with lung cancer: a possible link between these two disease entities. Respir Med 2015; 109: 923–925. doi: 10.1016/j.rmed.2015.05.005 [DOI] [PubMed] [Google Scholar]
- 80.Benusiglio PR, Giraud S, Deveaux S, et al. . Renal cell tumour characteristics in patients with the Birt–Hogg–Dubé cancer susceptibility syndrome: a retrospective, multicentre study. Orphanet J Rare Dis 2014; 9: 163. doi: 10.1186/s13023-014-0163-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kamada T, Yoshikawa Y, Shirase T, et al. . Perifollicular fibromas associated with Birt–Hogg–Dubé syndrome. J Dermatol 2015; 42: 1194–1195. doi: 10.1111/1346-8138.13091 [DOI] [PubMed] [Google Scholar]
- 82.Requena L, Sangueza O. Fibrofolliculoma and trichodiscoma. Requena L, Sangueza O, eds. In: Cutaneous Adnexal Neoplasms. Cham, Springer, 2017; pp. 503–515. [Google Scholar]
- 83.Luba MC, Bangs SA, Mohler AM, et al. . Common benign skin tumors. Am Fam Physician 2003; 67: 729–738. [PubMed] [Google Scholar]
- 84.Spring P, Fellmann F, Giraud S, et al. . Syndrome of Birt–Hogg–Dubé, a histopathological pitfall with similarities to tuberous sclerosis: a report of three cases. Am J Dermatopathol 2013; 35: 241–245. doi: 10.1097/DAD.0b013e318259b593 [DOI] [PubMed] [Google Scholar]
- 85.Aivaz O, Berkman S, Middelton L, et al. . Comedonal and cystic fibrofolliculomas in Birt–Hogg–Dubé syndrome. JAMA Dermatol 2015; 151: 770–774. doi: 10.1001/jamadermatol.2015.0215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sprague J, Landau JW. Birt–Hogg–Dubé syndrome presenting as a nevus comedonicus-like lesion in an 8-year-old boy. Pediatr Dermatol 2016; 33: e294–e295. doi: 10.1111/pde.12945 [DOI] [PubMed] [Google Scholar]
- 87.Cho S, Hahm JH. Perifollicular fibroma. J Eur Acad Dermatol Venereol 1999; 13: 46–49. doi: 10.1111/j.1468-3083.1999.tb00843.x [DOI] [PubMed] [Google Scholar]
- 88.McKenna DB, Barry-Walsh C, Leader M, et al. . Multiple perifollicular fibromas. J Eur Acad Dermatol Venereol 1999; 12: 234–237. doi: 10.1111/j.1468-3083.1999.tb01034.x [DOI] [PubMed] [Google Scholar]
- 89.Shvartsbeyn M, Mason AR, Bosenberg MW, et al. . Perifollicular fibroma in Birt–Hogg–Dubé syndrome: an association revisited. J Cutan Pathol 2012; 39: 675–679. doi: 10.1111/j.1600-0560.2012.01929.x [DOI] [PubMed] [Google Scholar]
- 90.Weintraub R, Pinkus H. Multiple fibrofolliculomas (Birt–Hogg–Dubé) associated with a large connective tissue nevus. J Cutan Pathol 1977; 4: 289–299. doi: 10.1111/j.1600-0560.1977.tb00920.x [DOI] [PubMed] [Google Scholar]
- 91.Nikolaidou C, Moscarella E, Longo C, et al. . Multiple angiomatous nodules: a novel skin tumor in Birt–Hogg–Dubé syndrome. J Cutan Pathol 2016; 43: 1197–1202. doi: 10.1111/cup.12811 [DOI] [PubMed] [Google Scholar]
- 92.DiCicco B, Johnson W, Allred J, et al. . Koenen's tumor and facial angiofibromas in a case of Birt–Hogg–Dubé syndrome: a cutaneous contribution to growing evidence of a relationship with tuberous sclerosis complex. JAAD Case Rep 2016; 2: 196–198. doi: 10.1016/j.jdcr.2016.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pithadia DJ, Treichel AM, Lee CR, et al. . Birt–Hogg–Dubé syndrome initially diagnosed as tuberous sclerosis complex. JAAD Case Rep 2019; 5: 368–371. doi: 10.1016/j.jdcr.2019.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Nadershahi NA, Wescott WB, Egbert B. Birt–Hogg–Dubé syndrome: a review and presentation of the first case with oral lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997; 83: 496–500. doi: 10.1016/S1079-2104(97)90152-9 [DOI] [PubMed] [Google Scholar]
- 95.Schmidt LS, Linehan WM. FLCN: The causative gene for Birt–Hogg–Dubé syndrome. Gene 2018; 640: 28–42. doi: 10.1016/j.gene.2017.09.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Starink TM, Houweling AC, van Doorn MB, et al. . Familial multiple discoid fibromas: a look-alike of Birt–Hogg–Dubé syndrome not linked to the FLCN locus. J Am Acad Dermatol 2012; 66: 259. doi: 10.1016/j.jaad.2010.11.039 [DOI] [PubMed] [Google Scholar]
- 97.Vincent A, Farley M, Chan E, et al. . Birt–Hogg–Dubé syndrome: a review of the literature and the differential diagnosis of firm facial papules. J Am Acad Dermatol 2003; 49: 698–705. doi: 10.1067/S0190-9622(03)01582-2 [DOI] [PubMed] [Google Scholar]
- 98.Tellechea O, Cardoso JC, Reis JP, et al. . Benign follicular tumors. An Bras Dermatol 2015; 90: 780–796. doi: 10.1590/abd1806-4841.20154114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Welsch MJ, Krunic A, Medenica MM. Birt–Hogg–Dubé syndrome. Int J Dermatol 2005; 44: 668–673. doi: 10.1111/j.1365-4632.2004.02095.x [DOI] [PubMed] [Google Scholar]
- 100.Cocciolone RA, Crotty KA, Andrews L, et al. . Multiple desmoplastic melanomas in Birt–Hogg–Dubé syndrome and a proposed signaling link between folliculin, the mTOR pathway, and melanoma susceptibility. Arch Dermatol 2010; 146: 1316–1318. doi: 10.1001/archdermatol.2010.333 [DOI] [PubMed] [Google Scholar]
- 101.Mota-Burgos A, Acosta EH, Marquez FV, et al. . Birt–Hogg–Dubé syndrome in a patient with melanoma and a novel mutation in the FCLN gene. Int J Dermatol 2013; 52: 323–326. doi: 10.1111/j.1365-4632.2012.05742.x [DOI] [PubMed] [Google Scholar]
- 102.Nowsheen S, Hand JL, Gibson LE, et al. . Melanoma in a patient with previously unrecognized Birt–Hogg–Dubé syndrome. JAAD Case Rep 2019; 5: 947–952. doi: 10.1016/j.jdcr.2019.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fontcuberta IC, Salomao DR, Quiram PA, et al. . Choroidal melanoma and lid fibrofoliculomas in Birt–Hogg–Dubé syndrome. Ophthalmic Genet 2011; 32: 143–146. doi: 10.3109/13816810.2010.544367 [DOI] [PubMed] [Google Scholar]
- 104.Marous CL, Marous MR, Welch RJ, et al. . Choroidal melanoma, sector melanocytosis, and retinal pigment epithelial microdetachments in Birt–Hogg–Dubé syndrome. Retin Cases Brief Rep 2019; 13: 202–206. doi: 10.1097/ICB.0000000000000595 [DOI] [PubMed] [Google Scholar]
- 105.Sattler EC, Ertl-Wagner B, Pellegrini C, et al. . Cutaneous melanoma in Birt–Hogg–Dubé syndrome: part of the clinical spectrum? Br J Dermatol 2018; 178: e132–e133. doi: 10.1111/bjd.15937 [DOI] [PubMed] [Google Scholar]
- 106.Pavlovich CP, Grubb RL 3rd, Hurley K, et al. . Evaluation and management of renal tumors in the Birt–Hogg–Dubé syndrome. J Urol 2005; 173: 1482–1486. doi: 10.1097/01.ju.0000154629.45832.30 [DOI] [PubMed] [Google Scholar]
- 107.Pavlovich CP, Walther MM, Eyler RA, et al. . Renal tumors in the Birt–Hogg–Dubé syndrome. Am J Surg Pathol 2002; 26: 1542–1552. doi: 10.1097/00000478-200212000-00002 [DOI] [PubMed] [Google Scholar]
- 108.Gupta S, Kang HC, Ganeshan D, et al. . The ABCs of BHD: An in-depth review of Birt–Hogg–Dubé syndrome. AJR Am J Roentgenol 2017; 209: 1291–1296. doi: 10.2214/AJR.17.18071 [DOI] [PubMed] [Google Scholar]
- 109.Johannesma PC, van de Beek I, van der Wel T, et al. . Renal imaging in 199 Dutch patients with Birt–Hogg–Dubé syndrome: screening compliance and outcome. PLoS One 2019; 14: e0212952. doi: 10.1371/journal.pone.0212952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lindor NM, Kasperbauer J, Lewis JE, et al. . Birt–Hogg–Dubé syndrome presenting as multiple oncocytic parotid tumors. Hered Cancer Clin Pract 2012; 10: 13. doi: 10.1186/1897-4287-10-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Maffe A, Toschi B, Circo G, et al. . Constitutional FLCN mutations in patients with suspected Birt–Hogg–Dubé syndrome ascertained for non-cutaneous manifestations. Clin Genet 2011; 79: 345–354. doi: 10.1111/j.1399-0004.2010.01480.x [DOI] [PubMed] [Google Scholar]
- 112.Yoshida K, Miyagawa M, Kido T, et al. . Parotid oncocytoma as a manifestation of Birt–Hogg–Dubé syndrome. Case Rep Radiol 2018; 2018: 6265175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Balakumar R, Farr MRB, Fernando M, et al. . Adult-type rhabdomyoma of the larynx in Birt–Hogg–Dubé syndrome: evidence for a real association. Head Neck Pathol 2019; 13: 507–511. doi: 10.1007/s12105-018-0922-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Tobino K, Gunji Y, Kurihara M, et al. . Characteristics of pulmonary cysts in Birt–Hogg–Dubé syndrome: thin-section CT findings of the chest in 12 patients. Eur J Radiol 2011; 77: 403–409. doi: 10.1016/j.ejrad.2009.09.004 [DOI] [PubMed] [Google Scholar]
- 115.Agarwal PP, Gross BH, Holloway BJ, et al. . Thoracic CT findings in Birt–Hogg–Dubé syndrome. AJR Am J Roentgenol 2011; 196: 349–352. doi: 10.2214/AJR.10.4757 [DOI] [PubMed] [Google Scholar]
- 116.Park HJ, Chae EJ, Do KH, et al. . Differentiation between lymphangioleiomyomatosis and Birt–Hogg–Dubé syndrome: analysis of pulmonary cysts on CT images. AJR Am J Roentgenol 2019; 212: 766–772. doi: 10.2214/AJR.18.20232 [DOI] [PubMed] [Google Scholar]
- 117.Johannesma PC, Houweling AC, van Waesberghe JH, et al. . The pathogenesis of pneumothorax in Birt–Hogg–Dubé syndrome: a hypothesis. Respirology 2014; 19: 1248–1250. doi: 10.1111/resp.12405 [DOI] [PubMed] [Google Scholar]
- 118.Ward RD, Tanaka H, Campbell SC, et al. . 2017 AUA Renal mass and localized renal cancer guidelines: imaging implications. Radiographics 2018; 38: 2021–2033. doi: 10.1148/rg.2018180127 [DOI] [PubMed] [Google Scholar]
- 119.Lobo JM, Clements MB, Bitner DP, et al. . Does renal mass biopsy influence multidisciplinary treatment recommendations? Scand J Urol 2020; 54: 27–32. doi: 10.1080/21681805.2019.1703805 [DOI] [PubMed] [Google Scholar]
- 120.Butnor KJ, Guinee DG Jr. Pleuropulmonary pathology of Birt–Hogg–Dubé syndrome. Am J Surg Pathol 2006; 30: 395–399. doi: 10.1097/01.pas.0000183571.17011.06 [DOI] [PubMed] [Google Scholar]
- 121.Koga S, Furuya M, Takahashi Y, et al. . Lung cysts in Birt–Hogg–Dubé syndrome: histopathological characteristics and aberrant sequence repeats. Pathol Int 2009; 59: 720–728. doi: 10.1111/j.1440-1827.2009.02434.x [DOI] [PubMed] [Google Scholar]
- 122.Kumasaka T, Hayashi T, Mitani K, et al. . Characterization of pulmonary cysts in Birt–Hogg–Dubé syndrome: histopathological and morphometric analysis of 229 pulmonary cysts from 50 unrelated patients. Histopathology 2014; 65: 100–110. doi: 10.1111/his.12368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sattler EC, Reithmair M, Steinlein OK. Kidney cancer characteristics and genotype-phenotype-correlations in Birt–Hogg–Dubé syndrome. PLoS ONE 2018; 13: e0209504. doi: 10.1371/journal.pone.0209504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Johannesma PC, Reinhard R, Kon Y, et al. . Prevalence of Birt–Hogg–Dubé syndrome in patients with apparently primary spontaneous pneumothorax. Eur Respir J 2015; 45: 1191–1194. doi: 10.1183/09031936.00196914 [DOI] [PubMed] [Google Scholar]
- 125.Ebana H, Mizobuchi T, Kurihara M, et al. . Novel clinical scoring system to identify patients with pneumothorax with suspicion for Birt–Hogg–Dubé syndrome. Respirology 2018; 23: 414–418. doi: 10.1111/resp.13191 [DOI] [PubMed] [Google Scholar]
- 126.Torricelli E, Occhipinti M, Cavigli E, et al. . The relevance of family history taking in the detection and management of Birt–Hogg–Dubé syndrome. Respiration 2019; 98: 125–132. doi: 10.1159/000498973 [DOI] [PubMed] [Google Scholar]
- 127.Liu Y, Xing H, Huang Y, et al. . Familial spontaneous pneumothorax: importance of screening for Birt–Hogg–Dubé syndrome. Eur J Cardiothorac Surg 2020; 57: 39–45. doi: 10.1093/ejcts/ezz171 [DOI] [PubMed] [Google Scholar]
- 128.Lee E, Sayyouh M, Haggerty JE, et al. . Role of radiologists in the diagnosis of unsuspected Birt–Hogg–Dubé syndrome in a tertiary clinical practice. AJR Am J Roentgenol 2019; 213: 792–797. doi: 10.2214/AJR.19.21176 [DOI] [PubMed] [Google Scholar]
- 129.Sattler EC, Steinlein OK. Birt–Hogg–Dubé syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al., eds.. GeneReviews®. 1993-2020. Seattle, University of Washington, Seattle, 2020. [Google Scholar]
- 130.Mizobuchi T, Kurihara M, Ebana H, et al. . A total pleural covering of absorbable cellulose mesh prevents pneumothorax recurrence in patients with Birt–Hogg–Dubé syndrome. Orphanet J Rare Dis 2018; 13: 78. doi: 10.1186/s13023-018-0790-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Stamatakis L, Metwalli AR, Middelton LA, et al. . Diagnosis and management of BHD-associated kidney cancer. Fam Cancer 2013; 12: 397–402. doi: 10.1007/s10689-013-9657-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Jamis-Dow CA, Choyke PL, Jennings SB, et al. . Small (< or = 3-cm) renal masses: detection with CT versus US and pathologic correlation. Radiology 1996; 198: 785–788. doi: 10.1148/radiology.198.3.8628872 [DOI] [PubMed] [Google Scholar]
- 133.Herring JC, Enquist EG, Chernoff A, et al. . Parenchymal sparing surgery in patients with hereditary renal cell carcinoma: 10-year experience. J Urol 2001; 165: 777–781. doi: 10.1016/S0022-5347(05)66524-X [DOI] [PubMed] [Google Scholar]
- 134.Nakamura M, Yao M, Sano F, et al. . [A case of metastatic renal cell carcinoma associated with Birt–Hogg–Dubé syndrome treated with molecular-targeting agents]. Hinyokika Kiyo 2013; 59: 503–506. [PubMed] [Google Scholar]
- 135.Gambichler T, Wolter M, Altmeyer P, et al. . Treatment of Birt–Hogg–Dubé syndrome with erbium:YAG laser. J Am Acad Dermatol 2000; 43: 856–858. doi: 10.1067/mjd.2000.109294 [DOI] [PubMed] [Google Scholar]
- 136.Truchuelo MT, Alcantara J, Allende I, et al. . Multiple facial papules of Birt–Hogg–Dubé syndrome treated with a CO2 laser. Ann Dermatol 2011; 23: S279–S280. doi: 10.5021/ad.2011.23.S2.S279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gijezen LM, Vernooij M, Martens H, et al. . Topical rapamycin as a treatment for fibrofolliculomas in Birt–Hogg–Dubé syndrome: a double-blind placebo-controlled randomized split-face trial. PLoS ONE 2014; 9: e99071. doi: 10.1371/journal.pone.0099071 [DOI] [PMC free article] [PubMed] [Google Scholar]