Abstract
Background
As the aging population is increasing significantly, the communication skills training (CST) on transitional care (TC) is insufficient.
Aims
This study aimed to test the effectiveness of an intervention (the online TC CST [OTCCST] and TC) through the perspectives of healthcare providers (HCPs), older patients, and family members.
Methods
A total of 38 HCPs caring for older patients were randomized to the experimental (n = 18) or control groups (n = 20), and 84 pairs of patients and family members were enrolled (experimental: n = 42 vs. control: n = 42). The primary outcome was HCP communication confidence; while secondary outcomes included patient quality of life (QoL), activities of daily living (ADL), rehospitalization counts, and family caregiving burden. Data were collected from HCPs using a scale measuring confidence in communicating with patients. Patient outcomes were assessed using the McGill QoL Questionnaire-Revised and Barthel Index. Family members were assessed with the Caregiver Burden Inventory. Rehospitalization counts were tracked for 3 months post-discharge. Data were analyzed using multiple regression analysis.
Results
Experimental group HCPs showed a significant improvement in communication confidence over the control group (p = 0.0006). Furthermore, experimental group patients had significantly fewer rehospitalization counts within 3-month post-discharge (p < 0.05). However, no significant group differences were found in patient QoL and ADL nor in family caregiver burden.
Conclusion
The OTCCST can effectively improve HCP communication confidence, and the combination of OTCCST and TC can reduce rehospitalization counts for older patients. The OTCCST allows HCPs to learn asynchronously at their convenience, ideal for continuing education, especially during the COVID-19 pandemic.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40520-022-02251-4.
Keywords: Transitional care, Communication skills training, Older adults, Online education, Continuing medical education
Introduction
The global population is aging [1]. Currently, of the approximately 7.8 billion people in the world, 9.3% are over the age of 65 [1]. Disability has increased significantly with aging [2, 3]. Older adults often suffer from multiple chronic diseases and are prone to functional decline. Moreover, due to a lack of disease awareness and inadequate medication use [4, 5], older adults tend to be admitted to hospitals more often, which reflects the importance of transitional care (TC).
TC requires transdisciplinary management designed to enable older patients to receive seamless care after discharge from the hospital [5–7]. Transdisciplinary management is a comprehensive approach that combines disciplinary resources, experience, and techniques to promote individualized care [8]. Although the positive effects of transdisciplinary management were supported by empirical evidence from western countries, such as from older adults with cancer [9], femur fracture [10], and early stage of Alzheimer’s disease [8], its feasibility in clinical practice, especially in Asian countries remains unknown.
Initiating TC at the time of admission is recommended [5, 7]. A previous study verified that TC interventions successfully assist older patients in returning home after hospital discharge [7], which decreases medical costs [11, 12], improves physical function [7], prevents adverse events [13], and reduces the risks of readmission and death [11, 12, 14, 15]. Unfortunately, the effectiveness of TC on patients’ quality of life (QoL) [7, 15, 16] is pending verification [7].
Most randomized clinical trials on TC were performed in Europe and America. Effects were inspected from the patient perspective [7, 15, 17]. Researchers emphasized family members’ need for TC, but most studies did not assess their perspectives on the effectiveness of TC [16, 18]. Although the population of Asia is aging among the fastest globally [19], the capacity to research TC in Asia is far less than in Europe and America [15]. In Asia, older adults usually live with their family members [1]. During the process of admitting older adults or returning them to the community, family members play an important role as caregivers and medical decision-makers. Therefore, the needs of family members cannot be ignored if TC is to be promoted in Asia.
Communication is a critical factor affecting older adults’ transition post-hospitalization [5, 6, 17, 20]. However, communication skills training (CST) or tools designed for healthcare providers (HCPs) specifically to perform TC was not found [17]. Previously, CST mainly focused on issues, such as cancer truth-telling [21–23], shared decision-making [24], advance care planning, and do-not-resuscitate orders [25]. Most trainings targeted a single healthcare profession (e.g., medical students or physicians). The transdisciplinary team training approach is seldom adopted [23].
Based on the transitions framework for gerontological nursing [26, 27] and suggestions from a TC literature review [5, 6, 17, 20], this study designed, implemented, and assessed the effectiveness of an intervention (online TC CST [OTCCST] and TC) through the perspectives of HCPs, older patients, and their family members. This study aimed to 1) test the effectiveness of the OTCCST in improving HCP communication confidence while providing TC and 2) evaluate the effectiveness of the intervention (OTCCST and TC) on improving patient QoL and activities of daily living (ADL), reducing rehospitalization counts, and decreasing family member caregiving burden.
Methods
Study design
This experimental study tested the effectiveness of the OTCCST and TC program. Data were collected between December 1, 2018, and February 28, 2020, at the geriatric, nephrology, infectious diseases, and metabolism departments of a medical center in Taiwan. The primary outcome was HCP communication confidence. The secondary outcomes included patient QoL, ADL, rehospitalization counts, and family member caregiving burden.
Sample
Convenience sampling was used in this study. Selected participants included HCPs, older patients under their care, and family members of these patients. Eligible HCPs were either physicians or nurses who provided direct care and were not absent for over a month during the study period.
Eligible patients were aged ≥ 65 years, hospitalized due to an acute condition, and had a mild-to-moderate disability (ADL scores of 60–95), and clear consciousness (Glasgow coma scores of 15). Patients with severe dementia (Mini-mental state examination < 10) were excluded. Eligible family members were aged ≥ 20 years, stayed with the patient during the hospitalization period the whole day, and assisted with caring for the patient in his/her daily life at home.
Procedure
Data were collected when all HCPs gave written informed consent after the research assistant (RA) fully explained the study’s aim and procedure. HCPs were randomly assigned to either the experimental group (EG) or control group (CG) in a 1:1 ratio using computer-generated assignments. EG HCPs were asked to complete the questionnaire on communication confidence before (T1, pre-test) and immediately after (T2, post-test) the intervention. The CG was not required to undergo the OTCCST and was asked to finish the post-test within 3 days after completing their pre-test.
Once HCPs completed the T2 measures, an invitation card was provided to patients and family members who met the inclusion criteria. If patients and family members were interested in participating, the RA visited them in the ward and explained the study aim and procedure. Those willing, signed an informed consent form. Their allocations followed the assignments of their attending physicians. They did not know their group allocation; however, it was known by the RA, who provided the TC. All patients and family members were asked to complete the questionnaires on QoL, ADL, and caregiver burden during the first 3 days of hospitalization (T1) and one day before discharge (T2). Furthermore, the RA conducted medical chart reviews and telephone follow-ups to collect rehospitalization counts at the third-month post-discharge.
Intervention
The OTCCST for HCPs
The OTCCST is described in detail in Supplementary Table 1. Briefly, the 15-min OTCCST consists of a video lecture and demonstrations on TC communication. The HCPs completed the OTCCST individually at their own suitable time and location. The online link to the OTCCST videos was provided to HCPs in the CG after this study was completed.
TC for patients and family members
This study arranged for a trained RA to perform TC with HCPs. The RA served as a transitional care nurse case manager (TCNCM) during the intervention. The RA is an experienced registered nurse with a public health Ph.D. candidate.
The TC intervention is described in detail in Supplementary Table 2. Briefly, the TC intervention followed 3 steps: identification, first visit, and follow-ups. During identification, the RA identified patients who had a poor prognosis and were candidates to receive TC. During the first visit, the members of the healthcare team met with patients and family members to understand their conditions and preferences for TC. The RA and attending physician then developed an individualized colored health education leaflet for each patient, which described levels of severity of the patient’s disease/condition organized by three flags. Red flag signaled a worsened condition in need of immediate medical action or hospitalization. Yellow flag signaled an unstable condition in need of careful attention from family members. Green flag signaled a stable condition. Each flag was characterized by three common symptoms easily identifiable by patients and family caregivers. Patients received leaflets one day before discharge. During follow-ups, the RA spoke with family members via a phone call or face-to-face services starting within 48 h of discharge and continuing once a week for 1 month (Supplementary Table 2). According to a systemic review, the impact on rehospitalization was largest within 30-day post-discharge [28]. The CG received only routine care.
Outcome measures
Confidence in communicating with patients
A 21-item self-reported scale was used to measure the HCP communication confidence while performing TC [21]. Item responses were rated on a 10-point Likert scale. Higher scores indicate more confidence in communicating. This scale has been widely used in various countries to test the effectiveness of the CST [22]. Here, the Cronbach’s α was 0.981–0.986.
McGill quality of life questionnaire-revised (MQOL-R)
A 14-item self-reported questionnaire was used to measure the patients’ QoL in 4 domains: physical, mental, spiritual, and social well-being [29]. Item responses are rated on a 10-point Likert scale. Higher scores indicate greater QoL. A large study found MQOL-R reliable (Cronbach’s α = 0.94) and valid [30]. Here, the Cronbach’s α of the overall scale and subscales were 0.883–0.904 and 0.741–0.942, respectively.
Barthel index
A 10-item scale was used to measure ADL among older adults [31] with a total score ranging from 0 to 100 points. Higher scores indicate a higher ability to live autonomously. This index has demonstrated high reliability (Cronbach’s α = 0.89–0.98) [32].
Caregiver burden inventory (CBI)
A 24-item scale was used to measure the family members’ caregiving burden in 5 domains: time dependence, development, physical, social, and emotional burden [33]. Item responses are rated on a 5-point Likert scale. Higher scores indicate a higher level of caregiver burden. The CBI has demonstrated high reliability of the overall scale (Cronbach’s α = 0.95) and subscales (Cronbach’s α = 0.73–0.93) [33]. Here, the Cronbach’s α of the overall scale was 0.949–0.951.
Data analysis
Since a lack of studies has examined the benefits of CST in TC for HCPs, older patients, or family members, this study referenced a previous CST study conducted for HCPs and cancer patients, which found that CST had a moderate to high positive effect on HCP communication confidence (Cohen’s d = 0.91–0.65) [23]. The sample size was calculated using G-power 3.1 software and setting power = 0.80, alpha = 0.05, and effect size = (0.91 + 0.65)/2 = 0.78. Given an estimated attrition rate of 30%, 32 HCPs were required for recruitment. Two–three pairs of patients and family members were recruited for each HCP to evaluate the benefits of the intervention from consumer perspectives.
Statistics Analysis System version 9.4 was used for analysis with statistical significance set at p < 0.05. Data were analyzed individually by a Ph.D. student (SYC) trained in both nursing research and biomedical statistic using the intention-to-treat strategy, which analyzes results based on the treatment group to which the participants were initially randomly assigned, regardless of whether they completed the intervention [34]. However, no participants dropped from this study, nor did any violate the initial protocol. For baseline data analysis of HCPs, this study utilized Mann–Whitney test and Fisher’s exact test, while those of patients and family members were analyzed using independent t test and chi-squared test. Those variables, which had significant group differences at T1, were viewed as interfering variables. After controlling for significant interfering variables, multiple regression analysis was used to analyze the effectiveness of the intervention between groups.
Results
Participants’ characteristics
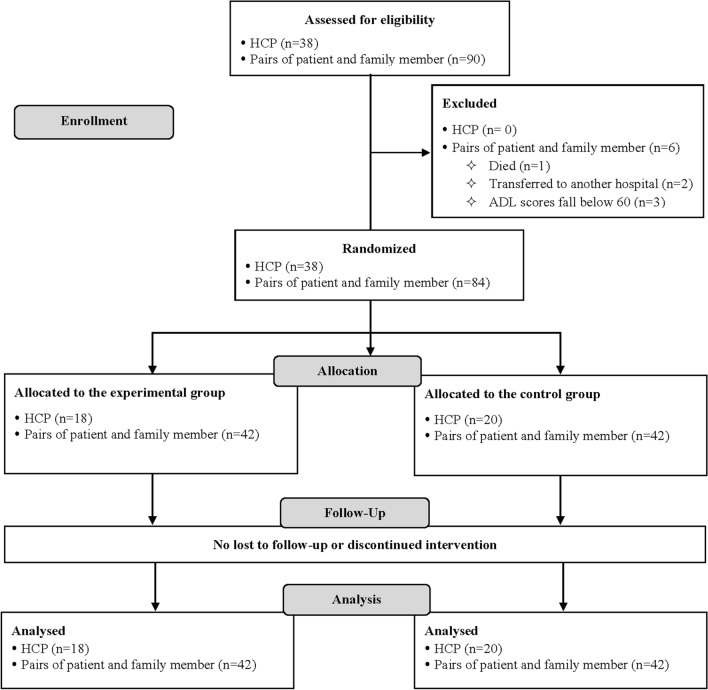
Enrolled were 38 HCPs and 90 pairs of patients and family members. HCPs were randomly assigned to the EG (n = 18) and CG (n = 20). All of them completed this study (Fig. 1). The average age of HCPs was 38.8 ± 11.4 years, and 55.3% were female. Most HCPs had a bachelor’s degree (81.6%), 10 + years of work experience (52.6%), and had not participated in CST before (86.8%). No significant group differences were found in basic characteristics of the HCPs (Supplementary Table 3).
Fig. 1.
Flow diagram of healthcare providers, older patients, and family members
Of 90 patients, one patient died, two were transferred to another hospital, and three fell below the threshold of ADL scores for eligibility. Only 84 patients were assigned to two groups. No one dropped out during follow-up (Fig. 1). Participants who were retained or excluded from this study did not significantly differ in basic characteristics. Patients’ average age was 79.3 ± 10.2 years, and most were male (52.4%), married (56.0%), and had an education level of elementary school (or below) (70.2%). Most patients had ADL 60–90 points (88.1%). Family members in the EG were significantly older than those in the CG (p = 0.03); their financial status was also better than that of the CG (p = 0.05). However, no significant group differences were found in basic characteristics of patients (Supplementary Table 4) and family members (Table 1).
Table 1.
Basic characteristics of family members (N = 84)
| Variables | Experimental group n (%) | Control group n (%) | p |
|---|---|---|---|
| Age (Mean ± SD) | 57.6 ± 15.2 | 50.5 ± 13.4 | 0.03* |
| Gender | |||
| Male | 20 (47.6) | 15 (35.7) | 0.27 |
| Education level | |||
| Elementary (and below) | 6 (14.3) | 7 (16.7) | 0.07 |
| Junior high | 1 (2.4) | 7 (16.7) | |
| High (and above) | 35 (83.3) | 28 (66.6) | |
| Marital status | |||
| Married | 26 (63.4) | 31 (73.8) | 0.31 |
| Single | 15 (35.6) | 11 (26.2) | |
| Financial status | |||
| Poor | 1 (2.4) | 1 (2.4) | 0.05* |
| Fair | 3 (7.1) | 11 (26.2) | |
| Well off | 30 (71.4) | 27 (64.3) | |
| Wealthy | 8 (19.1) | 3 (7.1) | |
| Lives with patient | 30 (71.4) | 30 (71.4) | 1.00 |
SD standard deviation
p < 0.05
Group differences in the primary outcome
Although two groups of HCP did not significantly differ in communication confidence at T1 (p = 0.08); after controlling for the T1 confidence score, confidence at T2 showed a significant group difference (p = 0.0006), demonstrating a moderate effect size (ΔR2 = 0.22) (Table 2).
Table 2.
Group differences in healthcare provider communication confidence in transitional care (N = 38)
| Time points | Experimental group Mean ± SD |
Control group Mean ± SD |
p | ΔR2 |
|---|---|---|---|---|
| T1 | 140.3 ± 37.0 | 163.4 ± 21.3 | 0.08a | 0.22 (R2 = 0.47) |
| T2 | 177.2 ± 19.1 | 167.0 ± 22.4 | 0.0006b*** |
***p < 0.001
HCP, healthcare provider; SD, standard deviation. T1, before OTCCST; T2, immediately after OTCCST
aAnalyzed using Mann–Whitney test
bAdjusted by T1 score and analyzed using multiple regression analysis
Group differences in the secondary outcomes
Concerning patients’ QoL, the EG scored lower than the CG in the total and subscales at T1, but only group differences on the psychological subscale reached statistical significance (p = 0.01). Moreover, groups did not significantly differ in total and subscale scores of QoL at T2. Patients’ ADL showed no significant group differences at T1 and T2. Similar results were also observed for caregiver burden (Table 3); however, the rehospitalization counts of the EG were significantly lower than those of the CG (p < 0.05). (Table 4).
Table 3.
Group differences in patients’ quality of life and activities of daily living and family members’ caregiving burden (N = 84)
| Outcomes | T1 | T2 | ||||
|---|---|---|---|---|---|---|
| Experimental group | Control group | p b | Experimental group | Control group | p c | |
| Overall QoL | 5.0 ± 2.2 | 4.2 ± 2.7 | 0.17 | 6.3 ± 2.1 | 5.5 ± 2.3 | 0.32 |
| Total score | 5.9 ± 1.4 | 6.5 ± 1.6 | 0.33 | 6.4 ± 1.4 | 7.0 ± 1.6 | 0.87 |
| Physical | 4.3 ± 1.8 | 4.9 ± 2.4 | 0.37 | 5.8 ± 1.9 | 6.3 ± 2.5 | 0.82 |
| Psychological | 5.2 ± 2.7 | 7.3 ± 2.4 | 0.01 | 7.0 ± 2.0 | 7.6 ± 2.4 | 0.09 |
| Spiritual | 6.1 ± 1.8 | 6.1 ± 2.1 | 0.97 | 6.7 ± 1.7 | 6.7 ± 1.9 | 0.92 |
| Social | 7.6 ± 1.3 | 7.8 ± 1.8 | 0.71 | 7.5 ± 1.6 | 7.8 ± 1.9 | 0.92 |
| ADL | 76.0 ± 11.9 | 72.1 ± 13.6 | 0.18 | 80.1 ± 12.6 | 76.9 ± 13.4 | 0.90 |
| Caregiver Burdena | 38.2 ± 13.0 | 37.2 ± 15.0 | 0.74 | 37.6 ± 12.4 | 38.4 ± 15.5 | 0.52 |
QoL quality of life, ADL activities of daily living, T1 before intervention, T2 immediately after intervention
aAdjusted by age and financial status
bAnalyzed using independent t test
cAnalyzed using multiple regression analysis
Table 4.
Group differences in rehospitalization counts (n = 84)
| Counts | Experimental group | Control group | pa |
|---|---|---|---|
| n (%) | n (%) | ||
| Never | 31 (73.8) | 24 (57.1) | < 0.05* |
| One time | 5 (11.9) | 13 (31.0) | |
| Two times | 6 (14.3) | 3 (7.1) | |
| Three times | 0 (0.0) | 2 (4.8) |
*p < 0.05
aAnalyzed using chi-square test
Discussion
Due to a lack of previous research on the topic, this study may constitute the first attempt to design, implement, and assess the benefits of a TC intervention from the perspectives of HCPs, patients, and family members in Taiwan. The OTCCST improved HCP communication confidence on TC and the combination of OTCCST and TC reduced rehospitalization counts. However, benefits of the intervention in improving patients’ QoL, ADL, and caregiver burden were not observed.
Group differences in HCP communication confidence
OTCCST can effectively improve HCP communication confidence. This benefit may be attributed to several design-based factors. OTCCST content was based on the literature and reviewed by experts. Furthermore, all content was recorded by a professional videography team with experience producing CST videos for HCP. Scholars have indicated that using quality videos as teaching and learning materials could enhance the quality of clinical skills education [35]. Because the 15-min online video allowed busy HCPs to complete their learning via electronic devices at any time and place, this learning model is appropriate for continuing education. Due to a lack of previous studies on TC CST for HCPs for comparison, further research is needed to validate the benefit of OTCCST.
Group differences in patient QoL, ADL, rehospitalization counts, and family caregiving burden
This study found no significant group differences in patient QoL and ADL, nor family caregiving burden. Concerning patient QoL, Preen et al. observed that older adults who received TC scored higher on the psychological subscale of the MQOL-R 7-day post-discharge [36]. Additionally, Ong et al. discovered that QoL of older heart failure patients, who received TC, had significantly improved 6-month post-discharge [37]. The above finding is different from this study because the post-test of this study only assessed QoL one day before discharge. Therefore, the benefit of the intervention on QoL may not be observed in such a short time. This study cannot capture the long-term benefits of improving patient QoL post-discharge. Longitudinal follow-ups are recommended to understand the short- and long-term benefits of the intervention on patient QoL [26].
Regarding patient ADL, Buurman et al. designed a TC intervention in which patients received home visits by a community nurse for 24-week post-discharge. The patients and their caregivers were provided with geriatric nursing guidance. After 24-week home visits, the study found no significant group difference in ADL scores [38]. However, Courtney et al. found that TC intervention could significantly improve patient ADL at 6-month post-discharge [39], which was different from the finding of Buurman et al. [38]. The reasons could be that besides the regular telephone follow-up or home visits, Courtney et al. provided a personal training plan designed by a physical therapist for older patients during hospitalization and arranged a nurse to confirm patients’ adherence by telephone follow-up after discharge [39] to get better outcomes on patients’ ADL. Therefore, including rehabilitation therapists in TC intervention and incorporating physical training at the early stage of hospitalization is recommended to improve patients’ ADL.
The intervention (OTCCST and TC) could significantly reduce patient rehospitalization counts within 3-month post-discharge. This was like previous studies, which supported that follow-up phone calls, home visits by nurses, and a formal TC program can significantly reduce older patient rehospitalization after discharge [40, 41].
A decline in ADL was identified as a robust risk factor for caregiver burden. However, the study found no significant group differences in caregiver burden [42]. Although Hendrix et al. found that the burden for caregivers of older patients before and after TC essentially remained the same [41], they only designed intra-group comparisons, which is not suitable for comparison with this study. Here, most patients were able to perform their daily activities before acute conditions. It may only be because of their conditions that patients became physically weak and needed assistance. As their condition improved, patient physical well-being was restored. Thus, it was difficult to detect the benefits of TC in reducing caregiver burden. Additionally, caregiver burden was measured one day before the patient’s discharge from the hospital (T2). This measurement point may not capture the full benefit of intervention on caregiver burden post-discharge. This issue may also explain the findings for patient QOL and ADL.
Study limitations
This study has four limitations. First, this study only recruited HCPs from a few specific departments, affecting the generalizability to other departments. Second, the assessment for communication confidence was performed immediately after the OTCCST; thus, this study was unable to observe its long-term benefits. Thus, to better understand the benefits of intervention, future researchers should (1) collect data to capture the long-term effectiveness of the intervention (e.g., one month and six months after the intervention) and (2) recruit participants from different departments to increase the representativeness and size of sample. Third, this study did not collect patient hospitalization information before the intervention, which may limit the study to compare differences between pre- and post-intervention. Therefore, to comprehensively analyze this objective data, it is suggested to collect hospitalization information pre- and post-intervention. Lastly, this study designed a Ph.D. candidate to perform TC. However, TCNCM with this kind of criteria is rare in clinical settings, which may decrease the study application. Nevertheless, past studies reported the TCNCM was essential to facilitate smooth care integration and transition post-discharge [43–45]. Therefore, we highly recommend hospitals arrange a specific TCNCM to help patients during transitional period.
Conclusion
The OTCCST can effectively improve HCP communication confidence in TC and the combination of OTCCST and TC can reduce rehospitalization counts for older patients. The OTCCST allows HCPs to learn asynchronously at their convenience, ideal for continuing education, especially during the COVID-19 pandemic when traditional face-to-face training is restricted. Due to a lack of studies on TC CST for HCPs, research is recommended that applies OTCCST in different settings to validate its effectiveness.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
Conceptualization, design, project administration, and funding acquisition: WRT, JTF, MF; data analysis and interpretation of data: SYC; resources and supervision: JTF, KCL, and CHL; investigation and acquisition of participants: LYY; drafting and critical revision of the manuscript: all authors.
Funding
This work was supported by Chang Gung Memorial Hospital (no. CORPG3H0581) and Chang Gung University (no. BMRP815).
Availability of data and materials
Data are available on request by contacting the corresponding author.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This study has been reviewed and approved by the institutional review board of Chang Gung Memorial Hospital (no. 201801266B0).
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ji-Tseng Fang and Shih-Ying Chen have contributed equally to this study and share the first authorship.
References
- 1.United Nations (2020) World population ageing 2020 highlights. https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/undesa_pd-2020_world_population_ageing_highlights.pdf. Accessed 15 Feb 2021
- 2.Hong J, Kim SW, Joo H, et al. Effects of smartphone mirroring-based telepresence exercise on body composition and physical function in obese older women. Aging Clin Exp Res. 2022;34:1113–1121. doi: 10.1007/s40520-021-02033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tu R, He H, Wang S, et al. The association between healthy aging index and trajectories of disability: a population-based cohort study. Aging Clin Exp Res. 2022;34:1893–1900. doi: 10.1007/s40520-022-02117-9. [DOI] [PubMed] [Google Scholar]
- 4.Arnall AJ, Sayer AA, Clegg A, et al. New horizons in multimorbidity in older adults. Age Ageing. 2017;46:882–888. doi: 10.1093/ageing/afx150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zurlo A, Zuliani G. Management of care transition and hospital discharge. Aging Clin Exp Res. 2018;30:263–270. doi: 10.1007/s40520-017-0885-6. [DOI] [PubMed] [Google Scholar]
- 6.Agomoh CJ, Brisbois MD, Chin E. A mapping review of clinical nurse leader and nurse educator transitional care skills and competencies. Nurs Outlook. 2020;68:504–516. doi: 10.1016/j.outlook.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Hang JA, Naseri C, Francis-Coad J, et al. Effectiveness of facility-based transition care on health-related outcomes for older adults: a systematic review and meta-analysis. Int J Older People Nurs. 2021;16:e12408. doi: 10.1111/opn.12408. [DOI] [PubMed] [Google Scholar]
- 8.Sanz PG, Grasso L, Barrantes FJ. Transdisciplinary assistance and translational research strategies to improve the quality of life of older adults at early stages of Alzheimer disease. Psychol Behav Sci Int J. 2018;9:1–3. doi: 10.19080/PBSIJ.2018.09.555758. [DOI] [Google Scholar]
- 9.Nipp RD, Temel B, Fuh CX, et al. Pilot randomized trial of a transdisciplinary geriatric and palliative care intervention for older adults with cancer. J Natl Compr Canc Netw. 2020;18:591–598. doi: 10.6004/jnccn.2019.7386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Sire A, Invernizzi M, Baricich A, et al. Optimization of transdisciplinary management of elderly with femur proximal extremity fracture: a patient-tailored plan from orthopaedics to rehabilitation. World J Orthop. 2021;12:456–466. doi: 10.5312/wjo.v12.i7.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naylor MD, Hirschman KB, Toles MP, et al. Adaptations of the evidence-based transitional care model in the U.S. Soc Sci Med. 2018;213:28–36. doi: 10.1016/j.socscimed.2018.07.023. [DOI] [PubMed] [Google Scholar]
- 12.Pauly MV, Hirschman KB, Hanlon AL, et al. Cost impact of the transitional care model for hospitalized cognitively impaired older adults. J Comp Eff Res. 2018;7:913–922. doi: 10.2217/cer-2018-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heim N, Rolden H, van Fenema EM, et al. The development, implementation and evaluation of a transitional care programme to improve outcomes of frail older patients after hospitalisation. Age Ageing. 2016;45:643–651. doi: 10.1093/ageing/afw098. [DOI] [PubMed] [Google Scholar]
- 14.Bingham J, Campbell P, Schussel K, et al. The discharge companion program: an interprofessional collaboration in transitional care model delivery. Pharmacy (Basel) 2019;7:68. doi: 10.3390/pharmacy7020068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Le Berre M, Maimon G, Sourial N, et al. Impact of transitional care services for chronically ill older patients: a systematic evidence review. J Am Geriatr Soc. 2017;65:1597–1608. doi: 10.1111/jgs.14828. [DOI] [PubMed] [Google Scholar]
- 16.Aboumatar H, Naqibuddin M, Chung S, et al. Effect of a hospital-initiated program combining transitional care and long-term self-management support on outcomes of patients hospitalized with chronic obstructive pulmonary disease: a randomized clinical trial. JAMA. 2019;322:1371–1380. doi: 10.1001/jama.2019.11982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spencer RA, Singh Punia H. A scoping review of communication tools applicable to patients and their primary care providers after discharge from hospital. Patient Educ Couns. 2021;104:1681–1703. doi: 10.1016/j.pec.2020.12.010. [DOI] [PubMed] [Google Scholar]
- 18.Hansen TK, Pedersen LH, Shahla S, et al. Effects of a new early municipality-based versus a geriatric team-based transitional care intervention on readmission and mortality among frail older patients—a randomised controlled trial. Arch Gerontol Geriatr. 2021;97:104511. doi: 10.1016/j.archger.2021.104511. [DOI] [PubMed] [Google Scholar]
- 19.United Nations (2019) World population ageing 2020 highlights. https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf. Accessed 15 Feb 2021
- 20.Allen J, Hutchinson AM, Brown R, et al. Evaluation of the TRANSITION tool to improve communication during older patients’ care transitions: healthcare practitioners’ perspectives. J Clin Nurs. 2020;29:2275–2284. doi: 10.1111/jocn.15236. [DOI] [PubMed] [Google Scholar]
- 21.Baile WF, Lenzi R, Kudelka AP, et al. Improving physician-patient communication in cancer care: outcome of a workshop for oncologists. J Cancer Educ. 1997;12:166–173. doi: 10.1080/08858199709528481. [DOI] [PubMed] [Google Scholar]
- 22.Fujimori M, Shirai Y, Asai M, et al. Effect of communication skills training program for oncologists based on patient preferences for communication when receiving bad news: a randomized controlled trial. J Clin Oncol. 2014;32:2166–2172. doi: 10.1200/jco.2013.51.2756. [DOI] [PubMed] [Google Scholar]
- 23.Tang WR, Chen KY, Hsu SH, et al. Effectiveness of Japanese SHARE model in improving Taiwanese healthcare personnel's preference for cancer truth telling. Psychooncology. 2014;23:259–265. doi: 10.1002/pon.3413. [DOI] [PubMed] [Google Scholar]
- 24.Hoerger M, Epstein RM, Winters PC, et al. Values and options in cancer care (VOICE): study design and rationale for a patient-centered communication and decision-making intervention for physicians, patients with advanced cancer, and their caregivers. BMC Cancer. 2013;13:188. doi: 10.1186/1471-2407-13-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Romotzky V, Galushko M, Düsterdiek A, et al. "It's Not that Easy"–medical students' fears and barriers in end-of-life communication. J Cancer Educ. 2015;30:333–339. doi: 10.1007/s13187-014-0712-0. [DOI] [PubMed] [Google Scholar]
- 26.Schumacher KL, Jones PS, Meleis AI. Helping elderly persons in transition: a framework for research and practice. In: Meleis AI, editor. Transition theory: Middle-range and situation-specific theories in nursing research and practice. New York: Springer; 2010. pp. 129–144. [Google Scholar]
- 27.Meleis AI (2017) Theoretical Nursing: development and progress. J. B. Lippincott, Philadelphia.
- 28.Fønss Rasmussen L, Grode LB, Lange J, et al. Impact of transitional care interventions on hospital readmissions in older medical patients: a systematic review. BMJ Open. 2021;11:e040057. doi: 10.1136/bmjopen-2020-040057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen SR, Mount BM, Bruera E, et al. Validity of the McGill quality of life questionnaire in the palliative care setting: a multi-centre Canadian study demonstrating the importance of the existential domain. Palliat Med. 1997;11:3–20. doi: 10.1177/026921639701100102. [DOI] [PubMed] [Google Scholar]
- 30.Cohen SR, Sawatzky R, Russell LB, et al. Measuring the quality of life of people at the end of life: the McGill quality of life questionnaire-revised. Palliat Med. 2017;31:120–129. doi: 10.1177/0269216316659603. [DOI] [PubMed] [Google Scholar]
- 31.Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J. 1965;14:61–65. [PubMed] [Google Scholar]
- 32.Gupta A, Rehman A. Measurement scales used in elderly care. Boca Raton: CRC Press; 2017. [Google Scholar]
- 33.Novak M, Guest C. Application of a multidimensional caregiver burden inventory. Gerontologist. 1989;29:798–803. doi: 10.1093/geront/29.6.798. [DOI] [PubMed] [Google Scholar]
- 34.Soares I, Carneiro AV. Intention-to-treat analysis in clinical trials: principles and practical importance. Rev Port Cardiol. 2002;21:1191–1198. [PubMed] [Google Scholar]
- 35.Forbes H, Oprescu FI, Downer T, et al. Use of videos to support teaching and learning of clinical skills in nursing education: a review. Nurse Educ Today. 2016;42:53–56. doi: 10.1016/j.nedt.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 36.Preen DB, Bailey BE, Wright A, et al. Effects of a multidisciplinary, post-discharge continuance of care intervention on quality of life, discharge satisfaction, and hospital length of stay: a randomized controlled trial. Int J Qual Health Care. 2005;17:43–51. doi: 10.1093/intqhc/mzi002. [DOI] [PubMed] [Google Scholar]
- 37.Ong MK, Romano PS, Edgington S, et al. Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: the better effectiveness after transition–heart failure (BEAT-HF) randomized clinical trial. JAMA Intern Med. 2016;176:310–318. doi: 10.1001/jamainternmed.2015.7712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buurman BM, Parlevliet JL, Allore HG, et al. Comprehensive geriatric assessment and transitional care in acutely hospitalized patients: the transitional care bridge randomized clinical trial. JAMA Intern Med. 2016;176:302–309. doi: 10.1001/jamainternmed.2015.8042. [DOI] [PubMed] [Google Scholar]
- 39.Courtney MD, Edwards HE, Chang AM, et al. Improved functional ability and independence in activities of daily living for older adults at high risk of hospital readmission: a randomized controlled trial. J Eval Clin Pract. 2012;18:128–134. doi: 10.1111/j.1365-2753.2010.01547.x. [DOI] [PubMed] [Google Scholar]
- 40.Deniger A, Troller P, Kennelty KA. Geriatric transitional care and readmissions review. J Eval Clin Pract. 2015;11:248–252. doi: 10.1016/j.nurpra.2014.08.014. [DOI] [Google Scholar]
- 41.Hendrix C, Tepfer S, Forest S, et al. Transitional care partners: a hospital-to-home support for older adults and their caregivers. J Am Assoc Nurse Pract. 2013;25:407–414. doi: 10.1111/j.1745-7599.2012.00803.x. [DOI] [PubMed] [Google Scholar]
- 42.van den Kieboom R, Snaphaan L, Mark R, et al. The trajectory of caregiver burden and risk factors in dementia progression: a systematic review. J Alzheimers Dis. 2020;77:1107–1115. doi: 10.3233/jad-200647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen WT, He HG, Chow YL. The evolving roles of nurses providing care at home: a qualitative case study research of a transitional care team. Int J Integr Care. 2022;22:3. doi: 10.5334/ijic.5838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Logan DR. Transition from hospital to home: the role of the nurse case manager in promoting medication adherence in the medicare population. Creat Nurs. 2019;25:126–132. doi: 10.1891/1078-4535.25.2.126. [DOI] [PubMed] [Google Scholar]
- 45.Lovelace D, Hancock D, Hughes SS, et al. A patient-centered transitional care case management program: taking case management to the streets and beyond. Prof Case Manag. 2016;21:277–290. doi: 10.1097/ncm.0000000000000158. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on request by contacting the corresponding author.