Abstract
Introduction
Hip aspirations are commonly performed for diagnostic purposes using either fluoroscopic or ultrasound guidance. The superiority of one type of image guidance over another for aspiration of a native or replaced hip remains a matter of debate. The questions to be evaluated in this study include 1) to determine if hip aspiration using fluoroscopy or ultrasound guidance more often obtains fluid from native and post-arthroplasty hip joints, and 2) to identify patient-related factors associated with the ability to obtain fluid.
Material and methods
A retrospective analysis of all hip aspirations (433) performed at a single institution was undertaken, with the primary outcome variable being successful attainment of joint fluid. Age, body mass index (BMI), sex, presence of a trainee, presence of an arthroplasty at the time of aspiration on the affected side, amount of fluid collected, and type of image guidance were used as independent variables in regression models.
Results
1) The likelihood of obtaining fluid was approximately 2.1 times greater with ultrasound guidance than fluoroscopy guidance (95% CI = 1.382, 3.117; p < 0.001). 2) Ultrasound guidance and lower BMI were independently associated with a significantly higher likelihood of obtaining fluid. Additionally, one unit decrease in BMI was associated with about a 3% increase in the odds of obtaining fluid (95% CI = 0.950, 0.998; p = 0.033).
Conclusion
This study demonstrates that the use of ultrasound guidance for hip joint aspiration, when compared to fluoroscopic guidance, is more likely to result in a successful aspiration and the acquisition of a greater volume of fluid. Therefore, ultrasound guidance is the preferred method for hip aspiration in both native and replaced hips.
Keywords: Hip joint, Hip replacement, Hip aspiration, Ultrasound, Fluoroscopy
1. Introduction
Hip joint aspirations provide key diagnostic value across a wide variety of suspected diagnoses and are commonly used to evaluate for infection. Successful joint aspiration is helpful in both diagnosis and treatment as it can support a diagnosis of infectious etiology and identify causative pathogens. This procedure is commonly performed in patients with suspected infection before or after hip arthroplasty.1,2 In the past, aspirations have predominantly been performed by using anatomic landmarks or fluoroscopic guidance.3 Ultrasound-guided aspiration is gaining popularity due to its accuracy and increased patient safety related to the absence of ionizing radiation and iodinated contrast agents.4
Multiple studies have been performed in the past independently evaluating the value of fluoroscopy, ultrasound, and computed tomography (CT) imaging modalities for hip aspirations.2,4,5 However, there have not been any studies to date specifically evaluating the success rates of obtaining joint fluid in hip joint aspirations with fluoroscopic versus ultrasound guidance.
The main objective of this study was to identify which type of image guidance technique (fluoroscopy or ultrasound) more often results in the acquisition of fluid from native and post-arthroplasty hip joints for analysis. It was hypothesized that ultrasound guidance would more commonly obtain joint fluid than fluoroscopy given its ability to visualize soft tissue structures and areas of fluid. The secondary aim was to identify potential factors which are predictive of obtaining hip joint fluid, namely age, body mass index (BMI), and presence of an arthroplasty.
2. Material and methods
This study was approved by the primary institution's internal review board (IRB #00071733) as an exempt study given the retrospective, anonymous nature of the review; no informed consent was required. A retrospective review of all hip joint aspirations performed at a single academic institution was performed. All were referred for hip joint aspirations, with most being for the purposes of ruling out infection. They were performed at an outpatient orthopaedic clinic by physicians with fellowship training in musculoskeletal radiology, sports medicine, or pain medicine. All aspirations were performed between May 2014 and February 2021 by a total of 29 different attending physicians. All procedures were performed with either fluoroscopic or ultrasound guidance and only intra-articular aspirations were included (i.e. extra-articular fluid collections were excluded from analysis). The modality of imaging was determined by the treating physician. The demographics of the study group patients are shown in Table 1.
Table 1.
Demographic data for subjects included in the study, n = 433. BMI = body mass index. Fluoro = Fluoroscopy. SD = standard deviation. US = ultrasound. aFrom independent t-test.
| All |
Fluoro |
US |
p value |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | mean | SD | n/mean | %/SD | n/mean | %/SD | |||
| Age | 60.5 | 14.1 | 61.6 | 14.3 | 59.4 | 13.8 | 0.111a | |||
| BMI | 31.0 | 8.2 | 31.7 | 8.9 | 30.3 | 7.5 | 0.082a | |||
| Sex | M | 193 | 44.6% | 97 | 46.0% | 96 | 43.2% | 0.568b | ||
| F | 240 | 55.4% | 114 | 54.0% | 126 | 56.8% | ||||
| Trainee present | Yes | 248 | 57.3% | 129 | 63.6% | 119 | 54.6% | 0.062b | ||
| No | 173 | 40.0% | 74 | 36.4% | 99 | 45.4% | ||||
| Missing | 12 | 2.7% | ||||||||
| Specialty | Sports medicine | 318 | 73.4% | 98 | 46.5% | 220 | 99.1% | <0.001b | ||
| Radiology | 112 | 26.1% | 112 | 55.1% | 1 | 0.45% | ||||
| Pain medicine | 2 | 0.46% | 1 | 0,47% | 1 | 0.45% | ||||
| Fluid appearance | Blood | 27 | 6.2% | 9 | 7.5% | 18 | 12.1% | 0.002b | ||
| Blood-tinged joint fluid | 108 | 24.9% | 48 | 40.0% | 60 | 40.3% | ||||
| Hazy/cloudy | 36 | 8.3% | 8 | 6.7% | 28 | 18.8% | ||||
| Purulent | 14 | 3.2% | 5 | 4.2% | 9 | 6.0% | ||||
| Transparent | 84 | 19.4% | 50 | 41.7% | 34 | 22.8% | ||||
| Arthroplasty | Yes | 300 | 69.3% | 159 | 75.4% | 141 | 63.5% | 0.008b | ||
| No | 133 | 30.7% | 52 | 24.6% | 81 | 36.5% | ||||
| Image guidance | Fluoroscopy | 211 | 48.7% | |||||||
| Ultrasound | 222 | 51.3% |
From χ2 test.
The choice of image guidance technique for aspiration was based predominantly on provider preference. Aspiration was attempted in all cases, even if fluid was not visualized by prior imaging or ultrasound. The aspiration needle was directed, under selected imaging, into an intracapsular location in all cases. Fluid was collected in syringes ranging from 10 to 50 mL, at the physician's discretion for all aspirations. The amount of fluid was recorded by the physician based on the amount aspirated into the syringe. Ultrasound procedures were more common at later dates (point biserial correlation coefficient 0.260, p < 0.001), but date of procedure had no effect on the final regression model (full model explained below). Each of the performing physicians reported whether or not fluid was obtained, the volume of fluid, and the appearance of the fluid. If a patient had missing information about the primary outcome variable, whether fluid was obtained, they were excluded. It was decided a priori to data collection that other missing data points would be deleted pairwise or analysis-by-analysis; in other words, physicians' data would be excluded only from the analyses involving a particular variable for which they had missing data.
2.1. Fluoroscopic aspirations
Fluoroscopic guided aspirations were all performed with the patient in a supine position using an anterolateral approach, aiming for the anterolateral aspect of the femoral head. Local anesthetic was first administered, with the goal of avoiding intra-articular administration of the anesthetic solution. If fluid was obtained immediately, then no contrast material was injected. Multiple attempts were undertaken to obtain fluid; if blood was aspirated, the needle was repositioned. Intra-articular contrast (air or iodinated contrast agent) was occasionally used to verify position after an unsuccessful attempt. In a number of cases (21), a saline flush was injected after unsuccessful aspiration, but these results were deemed unsuccessful attempts, as subsequent aspirations did not provide accurate cell counts.
2.2. Ultrasound aspirations
Most ultrasound-guided aspirations were performed from the anterior aspect of the supine patient. These were generally performed in-plane with a 5-MHz curvilinear probe (which allowed for better visualization at larger depths), though sonographers were free to use a 15-MHz linear probe if desired. Local anesthetic was first administered under ultrasound guidance. Similarly, if initial attempts were unsuccessful, the needle was repositioned, and additional attempts were performed. If only a small amount of blood was obtained, it was considered unsuccessful and additional passes were performed.
The primary outcome variable was successful attainment of hip joint fluid (dichotomous variable), defined as withdrawal of more than 0.1 mL of joint fluid. If a similarly small amount of blood was obtained, this was not deemed to be successful attainment of joint fluid, as this was more likely to be the result of a traumatic aspiration and not synovial fluid. Age, body mass index (BMI), sex, presence of a trainee (defined as a medical student, resident, or fellow who participated in or directly observed the procedure), presence of an arthroplasty at the time of aspiration on the affected side, amount of fluid collected (if any), and type of image guidance were collected. Data collection was performed and stored in a de-identified database to be analyzed by a separate blinded statistician to reduce any potential bias from either the data or data collection methods.
3. Theory/calculation
Statistical analysis was performed by Stata v17.0 (StataCorp, College Station, TX). Descriptive statistics were reported as mean (standard deviation [SD]) for continuous variables and n (%) for categorical variables. Comparisons between patients undergoing fluoroscopic- and ultrasound-guided aspirations were performed with independent t-tests (or Wilcoxon-Mann-Whitney rank-sum tests in case parametric assumptions were not met) for continuous variables, and χ2 tests (there was no cell with an expected frequency smaller than 5) for categorical variables. A logistic regression model was used to identify predictors pertaining to the primary outcome variable, obtaining fluid (dichotomous variable), with the following independent variables: image guidance technique (fluoroscopy vs. ultrasound), presence of a trainee, sex, age, BMI, and presence of an arthroplasty on the affected hip. Linear regression analysis, utilizing the same aforementioned independent variables, was carried out to identify differences in the amount of fluid obtained from the aspirations. Preliminary examination revealed that the outcome variable in the linear regression model, amount of fluid obtained, was positively skewed. Hence, the model was built, using the robust or sandwich estimator of variance.6,7 In both logistic and linear regression models, the interaction between fluoroscopy/ultrasound guidance and BMI was first entered in the model. If the interaction term was not significant, the final model was built without it.
4. Results
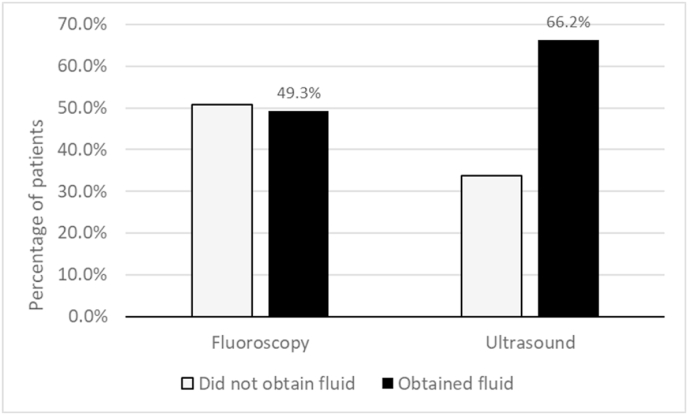
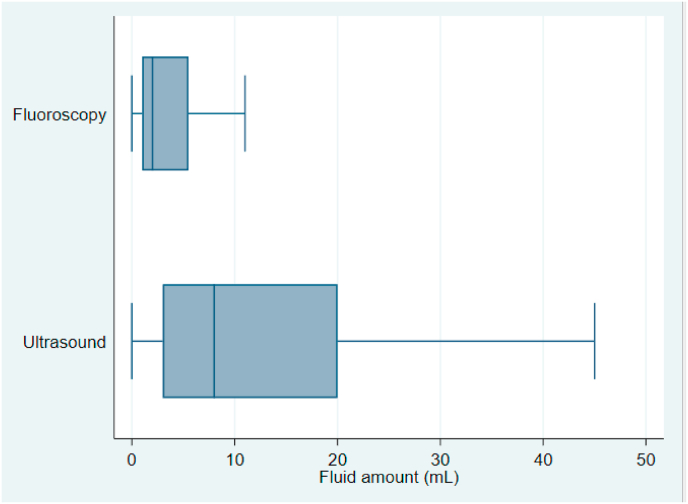
Three hundred attempted aspirations were in patients status-post hip arthroplasty, and 133 were in native hips. Demographic and aspiration information is described in detail in Table 1, with comparisons of patients undergoing aspiration by fluoroscopy or ultrasound. The only significant differences between the groups were specialty (p < 0.001), the presence of an arthroplasty (more common in the fluoroscopy group, p = 0.008) and the appearance of fluid (p = 0.002). When comparing fluoroscopy outcomes between radiologists and sports medicine trained physicians, both equally often obtained fluid (50.9% vs. 48.0%, respectively, p = 0.671). Fig. 1 displays the percentage of patients in whom fluid was obtained based on imaging modality, including all patients. The Wilcoxon-Mann-Whitney rank-sum test showed that a significantly greater volume of fluid was obtained with ultrasound guidance than with fluoroscopic guidance (10.8 ± 17.5 mL vs. 5.9 ± 14.9 mL; p < 0.001; Fig. 2).
Fig. 1.
Percentage of aspirations yielding fluid (n = 433 patients, 211 with fluoroscopic guidance and 222 with ultrasound).
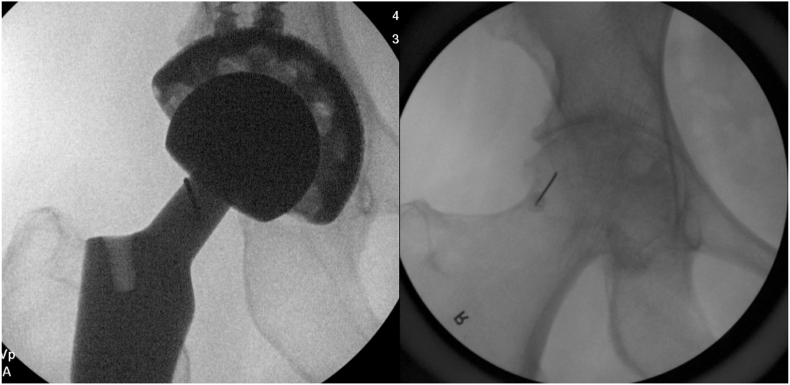
Fig. 2.
Two examples of aspirations under fluoroscopic guidance – the left half demonstrates a hip with prior arthroplasty, while the right represents a native hip. The needles can be visualized in both pictures on the lateral aspect of the femoral head/neck.
The results of the logistic regression analysis are described fully in Table 2. The interaction between fluoroscopic/ultrasound guidance and BMI was not significant (p = 0.982). Consequently, the final model was built without the interaction term. The results showed that ultrasound guidance and lower BMI was significantly associated with a higher likelihood of obtaining fluid, after adjusting for sex, age, trainee present, and arthroplasty (p < 0.05). The odds of obtaining fluid with ultrasound guidance was about 2.1 times greater than the odds for fluoroscopy guidance (OR = 2.075, 95% CI = 1.382, 3.117; p < 0.001). Furthermore, one unit decrease in BMI was associated with about a 3% increase in the odds of obtaining fluid (OR = 0.973, 95% CI = 0.950, 0.998; p = 0.033). It should be noted, however, that OR and its 95% CI were fairly close to 1.00, indicating the minimum effect of BMI. The linear regression model with the robust or sandwich estimator of variance, after excluding the nonsignificant interaction term between fluoroscopic/ultrasound guidance and BMI (p = 0.691), showed that ultrasound guidance and arthroplasty were significantly associated with larger amount of fluid aspirated (p < 0.05). Specifically, ultrasound guidance resulted in about 5.0 mL more fluid being aspirated than fluoroscopic guidance (β = 5.030; 95% CI = 1.051, 9.008; p = 0.013). In addition, history of arthroplasty was associated with about 3.7 mL more fluid being aspirated (β = 3.667; 95% CI = 0.412, 6.922; p = 0.027).
Table 2.
Logistic regression analysis, examining the primary outcome variable, attainment of fluid with hip aspiration (yes/no). BMI = body mass index. CI = confidence interval. OR = odds ratio.
| OR | 95% CI | p | |
|---|---|---|---|
| Ultrasound guidance | 2.075 | 1.382, 3.117 | <0.001 |
| Trainee present | 1.215 | 0.810, 1.824 | 0.347 |
| Female sex | 1.086 | 0.726, 1.624 | 0.690 |
| Age | 1.003 | 0.989, 1.018 | 0.644 |
| BMI | 0.973 | 0.950, 0.998 | 0.033 |
| History of arthroplasty | 1.408 | 0.908, 2.182 | 0.127 |
5. Discussion
Most of the prior literature on this topic has been on hip injections and not aspirations. The literature is contradictory in regards to which imaging modality is more commonly used.8,9 The accuracy when using ultrasound for injections and aspirations ranges from 97 to 100%,10,11 while fluoroscopy is often used as the “gold standard” for ultrasound accuracy studies.11 Both imaging modalities have been shown to have similar accuracy when performed for contrast injection.12 Prior literature has also demonstrated that ultrasound is a superior method for pre-operative identification of periprosthetic hip infection, both in terms of sensitivity/specificity4,13 and cost.13 Ultrasound has also been found to be an effective method for the identification of native hip septic arthritis.14 Although there is evidence to support the use of ultrasound to detect fluid about the hip, no study to date has examined its value in performing a successful aspiration.
There were 433 subjects within this study, providing a large sample size and adequate power. However, there were several limitations. Importantly, any retrospective study lends itself to the related biases. The potential for selection bias is a significant limitation as the involved physicians may have preferentially used one imaging modality over the other for undetermined reasons or personal expertise with a specific imaging modality. All charts reviewed were drawn from a single academic institution's outpatient orthopedic clinic, limiting its generalizability; however, 29 physicians were included. The aspirations were all performed on adults and therefore the findings of our study may not be applicable to the pediatric population. In addition, each of the aspirations examined were performed by physicians with a variety of fellowship training, including musculoskeletal radiology, sports medicine, and pain medicine. This variation in training could represent differences in each physician's ability to successfully utilize ultrasound or fluoroscopy for hip joint aspiration. The choice of fluoroscopy or ultrasound guidance was not truly random and could create a bias that would only be overcome by a randomized prospective trial. Lastly, inherent to any retrospective, observational study, there were potential unobserved covariates that could have influenced the study results but were unable to be included in our statistical models, although we did our best to include important covariates in the models. With the limitations inherent in a retrospective study, the findings of our study should be confirmed with a randomized, controlled trial.
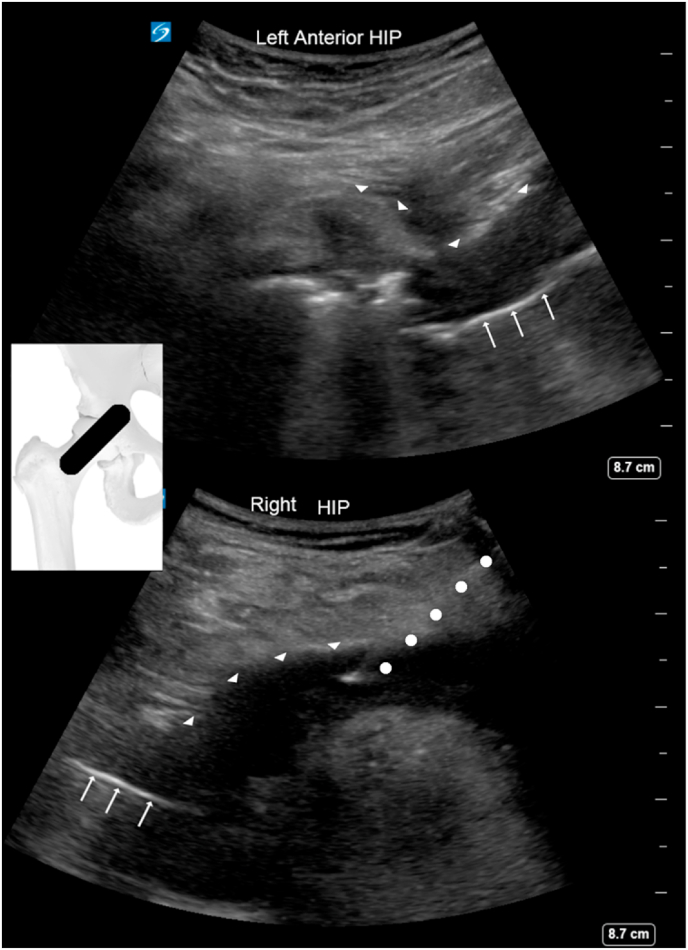
Our study demonstrates that ultrasound-guided aspirations more commonly obtain fluid (approximately twice the odds), and when successful, result in the acquisition of a greater volume of fluid (about 5 additional mL on average). This is likely due to the ability of ultrasound to visualize the targeted fluid (Fig. 3 shows an example of a large hip effusion, visualized with ultrasound), which cannot be seen using fluoroscopy. Furthermore, it is not uncommon for periprosthetic infections to extend beyond the confines of the intracapsular space, which can be readily visualized by ultrasound, but not fluoroscopy. Interestingly, the presence or absence of arthroplasty had no effect on the likelihood of a successful aspiration. This study did not examine other factors related to hip type or morphology such as the presence of dysplasia, presence of avascular necrosis, type of arthroplasty, cam/pincer deformities, or other differences (see Fig. 4).
Fig. 3.
Amount of fluid aspirated from hip joints, based on image guidance technique, n = 433. Outliers are not included. NOTE: OK to be in greyscale.
Fig. 4.
Ultrasound images of large hip effusions in two post-arthroplasty patients. The left aspect is superomedial on both images. The arrows depict the femoral component of the hip arthroplasty, while the ars outline the superficial aspect of the synovium holding the effusion. On the bottom image, the dots represent the trajectory of the needle with the needle tip visible within the fluid collection.
This study found that increased BMI was an independent risk factor in reducing the likelihood of successful aspiration, whereas age, sex, and prior arthroplasty did not show any association. Increased BMI has also been demonstrated to increase radiation dosage received during fluoroscopic-guided injections.15 Possible explanations for the effect of BMI include the increased tissue depth, which increases sonographic attenuation and diminishes visualization of the hip joint and needle tip. Additionally, the needle length is often increased for those with larger BMIs. Needle length has direct implication on the ease of aspiration with shorter needles requiring less pressure to aspirate than longer needles of the same gauge.16
6. Conclusions
In conclusion, the questions to be evaluated in this study included 1) to determine if hip aspiration using fluoroscopy or ultrasound guidance more often obtains fluid from native and post-arthroplasty hip joints, and 2) to identify patient-related factors associated with the ability to obtain fluid. The results demonstrate a statistically-significantly increased likelihood of obtaining fluid with ultrasound guidance when compared to fluoroscopic guidance. Additionally, it revealed that significantly more fluid was aspirated with ultrasound guidance in comparison to fluoroscopic guidance. This study found that increased BMI was an independent risk factor in reducing the likelihood of successful aspiration, whereas age, sex, and prior arthroplasty did not show any association. Given the known cost savings8,13 and absence of radiation exposure with ultrasound,15 it would appear to be the preferred method for performing hip joint aspirations.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Informed consent
Not needed as exempt.
Institutional ethical committee approval
This study was approved by the primary institution's internal review board (IRB #00071733) as an exempt study given the retrospective, anonymous nature of the review; no informed consent was required.
Authors contributions
Conceptualization – AMH, HR, DMC, MT, MA.
Data curation – HR, JP, JF, DMC.
Formal analysis – DMC, MT, MA.
Funding acquisition – N/A.
Investigation – DMC, HR, AMH, MT, AB.
Methodology – DMC, MT.
Project administration – DMC, HR.
Resources – DMC, AMH, MT.
Software – DMC, MT.
Supervision – DMC, AMH.
Validation – DMC, MT, MA.
Visualization – DMC, MT, AMH, MA.
Roles/Writing – original draft – AB, DC, MT.
Writing – review & editing – All authors.
Declaration of competing interest
None.
Acknowledgement
none.
Footnotes
This study was approved by the primary institution's internal review board (IRB #00071733) as an exempt study given the retrospective, anonymous nature of the review; no informed consent was required.
The work was performed at the University of Utah Divisions of Orthopedics and Physical Medicine and Rehabilitation.
Contributor Information
Heather Roesly, Email: hbroesly@gmail.com.
Michael Archibeck, Email: michael.archibeck@hsc.utah.edu.
A. Michael Henrie, Email: Mike.henrie@hsc.utah.edu.
Justin Provo, Email: justin.provo@hsc.utah.edu.
Justin Foley, Email: Justin.foley@hsc.utah.edu.
Andrew Boyer, Email: andrew.boyer@westernu.edu.
Masaru Teramoto, Email: masaru.teramoto@hsc.utah.edu.
Daniel M. Cushman, Email: dan.cushman.work@gmail.com.
References
- 1.Williams J.L., Norman P., Stockley I. The value of hip aspiration versus tissue biopsy in diagnosing infection before exchange hip arthroplasty surgery. J Arthroplasty. 2004;19(5):582–586. doi: 10.1016/j.arth.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 2.Barrack R.L., Harris W.H. The value of aspiration of the hip joint before revision total hip arthroplasty. J Bone Joint Surg Am. 1993;75(1):66–76. doi: 10.2106/00004623-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Phillips W.C., Kattapuram S.V. Efficacy of preoperative hip aspiration performed in the radiology department. Clin Orthop Relat Res. 1983;179:141–146. http://www.ncbi.nlm.nih.gov/pubmed/6617006 [PubMed] [Google Scholar]
- 4.Battaglia M., Vannini F., Guaraldi F., Rossi G., Biondi F., Sudanese A. Validity of preoperative ultrasound-guided aspiration in the revision of hip prosthesis. Ultrasound Med Biol. 2011;37(12):1977–1983. doi: 10.1016/j.ultrasmedbio.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Tomas X., Bori G., Garcia S., et al. Accuracy of CT-guided joint aspiration in patients with suspected infection status post-total hip arthroplasty. Skeletal Radiol. 2011;40(1):57–64. doi: 10.1007/s00256-010-0940-2. [DOI] [PubMed] [Google Scholar]
- 6.Huber P.J. vol. 1. University of California Press; 1967. The behavior of maximum likelihood estimates under nonstandard conditions; pp. 221–233. (Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability). [Google Scholar]
- 7.White H.L.J. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–838. [Google Scholar]
- 8.Henne M., Centurion A., Zeini I.M., Youmans D.H., Osbahr D.C. Trends in utilization of image guidance for hip joint injections. Clin J Sport Med. 2021;31(4):374–378. doi: 10.1097/jsm.0000000000000781. [DOI] [PubMed] [Google Scholar]
- 9.Cushman D.M., Christiansen J., Kirk M., et al. Image guidance used for large joint and bursa injections; a survey study. Physician Sportsmed. 2020;48(2):208–214. doi: 10.1080/00913847.2019.1674122. [DOI] [PubMed] [Google Scholar]
- 10.Finnoff J.T., Hall M.M., Adams E., et al. American medical society for sports medicine position statement. Clin J Sport Med. 2015;25(1):6–22. doi: 10.1097/JSM.0000000000000175. [DOI] [PubMed] [Google Scholar]
- 11.Hoeber S., Aly A.R., Ashworth N., Rajasekaran S. Ultrasound-guided hip joint injections are more accurate than landmark-guided injections: a systematic review and meta-analysis. Br J Sports Med. 2016;50(7):392–396. doi: 10.1136/bjsports-2014-094570. [DOI] [PubMed] [Google Scholar]
- 12.Martínez-Martínez A, García-Espinosa J, Ruiz-Santiago F, Guzmán-Álvarez L, Castellano-García MM. Comparison of ultrasound and fluoroscopic guidance for injection in CT arthrography and MR arthrography of the hip. Radiologí. 58(6):454-459. doi:10.1016/j.rx.2016.07.006. [DOI] [PubMed]
- 13.Randelli F., Brioschi M., Randelli P., Ambrogi F., Sdao S., Aliprandi A. Fluoroscopy- vs ultrasound-guided aspiration techniques in the management of periprosthetic joint infection: which is the best? Radiol Medica. 2018;123(1):28–35. doi: 10.1007/s11547-017-0811-1. [DOI] [PubMed] [Google Scholar]
- 14.Bengtzen R.R., Lee J. Point-of-Care ultrasound and the septic prosthetic hip joint. J Emerg Med. 2019;57(5):701–704. doi: 10.1016/j.jemermed.2019.08.004. [DOI] [PubMed] [Google Scholar]
- 15.Cushman D.M., Mattie R., Clements N.D., McCormick Z.L. The effect of body mass index on fluoroscopic time and radiation dose during intra-articular hip injections. Pharm Manag PM R. 2016;8(9):876–882. doi: 10.1016/j.pmrj.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 16.Haseler L.J., Sibbitt R.R., Sibbitt W.L., Michael A.A., Gasparovic C.M., Bankhurst A.D. Syringe and needle size, syringe type, vacuum generation, and needle control in aspiration procedures. Cardiovasc Intervent Radiol. 2011;34(3):590–600. doi: 10.1007/s00270-010-0011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]