Abstract
Objective:
To provide state-level estimates of diagnosed attention-deficit/hyperactivity disorder (ADHD) and associated treatment among children in the United States in 2016–2019.
Method:
This study used the National Survey of Children’s Health to produce national and state-level estimates of lifetime diagnosis and current ADHD among all children aged 3–17 years (n=114,476), and national and state-level estimates of medication and behavioral treatment use among children with current ADHD.
Results:
The state-level estimates of diagnosed ADHD ranged from 6.1% to 16.3%. Among children with current ADHD, state-level estimates of ADHD medication usage ranged from 37.8% to 81.4%, and state-level estimates of behavioral treatment ranged from 38.8% to 61.8%.
Conclusion:
There was substantial state-level variation for indicators of ADHD diagnosis and associated treatment. These state-level results can be used by policymakers, public health practitioners, health care providers, and other stakeholders to help address the service needs of children with ADHD in their states.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by symptoms of inattention, hyperactivity, and/or impulsivity that cause impairment in multiple settings (American Psychiatric Association, 2013). ADHD is commonly diagnosed and treated in children and adolescents in the United States, with an estimated 6.1 million U.S. children aged 2–17 years (9.4%) having ever received an ADHD diagnosis as of 2016 and 8.4% of children having current ADHD; 62.0% of children with current ADHD were reported to be receiving medication and 46.7% were receiving behavioral treatment (Danielson et al., 2018). Children and adolescents with ADHD more frequently experience negative outcomes such as school failure, difficult social relationships with peers, conflict with family members, engagement in risky behaviors, and lower health-related quality of life than their peers (Erskine et al., 2016; Faraone et al., 2015; Fleming et al., 2017). ADHD is also recognized as a chronic condition, with many children and adolescents diagnosed with ADHD in childhood continuing to experience symptoms and related functional impairment as adults (Hechtman et al., 2016).
Clinical guidelines for pediatricians recommend treating ADHD with FDA-approved medications and/or behavior therapy, depending on the child’s age and clinical presentation (Subcommittee on Attention-Deficit/Hyperactivity Disorder et al., 2011; Wolraich et al., 2019). For children younger than 6 years, behavior therapy is recommended as the first-line treatment, with medication only being prescribed to young children with ADHD if functional impairment continues after an adequate trial of behavior therapy or if appropriate therapy is not available or accessible. For school-aged children (aged 6–11 years), clinical guidance for pediatricians recommends medication and/or behavior therapy, preferably in combination, and medication treatment is recommended for adolescents (12–18 years), with a preference for the medication to be prescribed in combination with behavior therapy. Clinical guidance for child and adolescent psychiatrists similarly recommends medication and behavior therapy treatment modalities individually and in combination (American Academy of Child and Adolescent Psychiatry, 2007).
Previous studies have shown that there is significant state-level variation in the diagnosis of mental disorders and related treatment among children and adolescents (Bitsko et al., 2022; Whitney & Peterson, 2019), including ADHD (Bozinovic et al., 2021; Centers for Disease Control and Prevention, 2010; Visser et al., 2015; Visser, Blumberg, et al., 2013; Visser et al., 2014). State-level estimates of current ADHD prevalence from the National Survey of Children’s Health (NSCH) collected in 2011–12 ranged from 4% to 15% among children aged 4–17 years, with 2% to 10% of all children receiving current ADHD medication treatment, regardless of ADHD diagnosis status (Visser et al., 2014). The 2011–12 NSCH did not include an indicator to estimate the prevalence of behavior therapy to treat ADHD, but another national survey conducted in 2009–10 about children with special health care needs (CSHCN) provided state-level estimates of past-year behavioral treatment for ADHD that ranged from 33% to 61% of CSHCN with ADHD, compared to 57% to 88% of CSHCN with ADHD who had taken ADHD medication in the past year (Visser et al., 2015). However, approximately 1 out of 8 children with ADHD do not meet special health care need criteria, so these estimates do not capture the full population of children with ADHD (Visser et al., 2015). Studies using health care claims and prescription drug records have similarly shown substantial state-level variation in diagnosis and treatment of ADHD among children and adolescents (Blue Cross Blue Shield, 2019; Board et al., 2020; McDonald & Jalbert, 2013; Piper et al., 2018; Visser et al., 2016).
The objective of this study is to provide state-level estimates of diagnosed ADHD and associated treatment among children and adolescents aged 3–17 years in the United States in 2016–2019. These estimates can serve as a baseline to monitor these indicators in the population over time using the NSCH, an ongoing annual survey that was redesigned in 2016. This study will also be the first to report state-level estimates of behavioral treatment for ADHD among all noninstitutionalized U.S. children with current ADHD using national survey data, providing a more complete understanding of state-level treatment use for ADHD than previous studies that used indicators of ADHD medication usage alone.
Methods
The NSCH is a cross-sectional survey designed to provide national and state-level estimates of health indicators for all noninstitutionalized children aged 0–17 years in the United States (Ghandour et al., 2018). The survey is directed by the Health Resources and Services Administration’s Maternal and Child Health Bureau and administered by the U.S. Census Bureau. The NSCH was previously administered as a telephone survey in 2003, 2007, and 2011–12, but beginning in 2016, the survey was redesigned to be a self-administered mail/online survey with annual data collection. Detailed information about the survey design and methods has been published elsewhere (Ghandour et al., 2018). Briefly, one child in the household was selected to be the focal point of a survey completed by the child’s parent or guardian (hereinafter referred to as the parent) about the child’s health and well-being. The 2016–2019 surveys had annual interview completion rates that ranged from 69.7% to 79.5% among households known to include children and annual overall weighted response rates (probability of screener and interview completion among all sampled addresses) that ranged from 37.4% to 43.1%; annual state-level response rates ranged from 31.5% to 59.8% (United States Census Bureau, 2018a, 2018b, 2019, 2020).
This study describes parent-reported indicators related to the diagnosis and treatment of ADHD among U.S. children aged 3–17 years overall and by state in 2016–2019. The respondent parent was asked whether a doctor or other health care provider had ever told them that their child has attention deficit disorder (ADD) or attention-deficit/hyperactivity disorder (hereafter referred to as ADHD). If yes, the parent was asked whether their child currently had ADHD. Among children with reported current ADHD, the parent was asked if their child was currently taking medication for ADD or ADHD and if their child had received “behavioral treatment for ADD or ADHD such as training or an intervention that [the parent] or [child] received to help with [the child’s] behavior” in the past 12 months. Parents were also asked whether their child had taken medication because of difficulties with their emotions, concentration, or behavior in the past 12 months, or if their child received any treatment or counseling from a mental health professional in the past 12 months.
Weighted prevalence estimates, 95% Clopper-Pearson confidence intervals (using the Korn and Graubard approach (Korn & Graubard, 1998)), and weighted population estimates were calculated for indicators of ever receiving an ADHD diagnosis and current ADHD among all children aged 3–17 years for each state and the District of Columbia as well as for the nation as a whole. State-level and national weighted prevalence estimates for ADHD-specific treatment indicators and 95% Clopper-Pearson confidence intervals were calculated for current use of ADHD medication, past-year receipt of behavioral treatment for ADHD, and receipt of either ADHD medication and/or ADHD behavioral treatment among children with reported current ADHD. Prevalence estimates with 95% confidence intervals for a set of derived indicators that incorporate broader measures of treatment were also calculated: (1) child is currently taking ADHD medication and/or has taken medication for difficulties with emotions, concentration, or behavior in the past 12 months; (2) child had received behavioral treatment for ADHD and/or received treatment or counseling from a mental health professional in the past 12 months; and (3) child received any of the four treatment types (ADHD medication, any medication for difficulties with emotions, concentration, or behavior, behavioral treatment for ADHD, or any treatment or counseling from a mental health professional). All national and state point estimates were evaluated using NCHS standards for precision (Parker et al., 2017) and all estimates met criteria for presentation though the complement for a couple of estimates did not, indicating that nearly all presented estimates can be considered to be stable. Wald F tests were used to test for linear trend in prevalence over the four-year time period for each indicator overall and by state with an α of 0.05. Ranges of state-level estimates, medians, and interquartile intervals (IQIs) are also presented for each indicator to provide detail about the distribution of the state-level estimates. Maps are included to provide a visual illustration of the regional distribution of selected indicators, including symbols to show the states that have estimates that have a statistically significant difference from the rest of the country (p<0.05). The state-level sample size for children aged 3–17 years with valid responses to the ADHD-related questions ranged from 1,947 to 2,532, totaling 114,476 children in the national analytic sample over the study time period. Children with missing responses to either of the ADHD treatment variables were excluded from the analysis of treatment indicators. All analyses were conducted in SAS-callable SUDAAN version 11.0.1 (RTI International; Cary, NC) to account for the complex survey design and to apply sample weights that adjust for probability of selection, non-response, and the underlying distribution of demographic characteristics such as child sex, age, race/ethnicity, special health care need status, family poverty status, household size, and parent education for the target population (United States Census Bureau, 2020).
Results
In 2016–2019, 9.8% of U.S. children aged 3–17 years (approximately 6.0 million) had ever been diagnosed with ADHD based on parent report. The state-level estimates of ever diagnosed ADHD prevalence for this time period ranged from 6.1% to 16.3% (median=10.5%; IQI: 8.7–11.9; Table 1). There were twenty-two states with an ever diagnosed ADHD estimate that was significantly different from the estimate for the rest of the country: seven states had lower estimates than the rest of the country (California, Hawaii, Nebraska, Nevada, New Jersey, New York, South Dakota) and fifteen states had higher estimates than the rest of the country (Alabama, Arkansas, Delaware, Georgia, Indiana, Kentucky, Louisiana, Maine, Mississippi, New Hampshire, North Carolina, Ohio, South Carolina, Tennessee, West Virginia; Figure 1). Among children who had ever received an ADHD diagnosis, most (91.6%) were reported to have current ADHD (range of state-level estimates: 85.0% to 97.1%; data not shown).
Table 1:
Weighted Prevalence Estimates of Parent-Reported Attention-Deficit/Hyperactivity Disorder (ADHD) Diagnosis by a Health Care Provider among U.S. Children aged 3–17 Years by State, National Survey of Children’s Health, 2016–2019
| Ever Received ADHD Diagnosis |
Has Current ADHD |
|||||||
|---|---|---|---|---|---|---|---|---|
| Weighted Population Estimate | Weighted Population Estimate 95% CI | Weighted % | 95% CI | Weighted Population Estimate | Weighted Population Estimate 95% CI | Weighted % | 95% CI | |
|
| ||||||||
| United States | 6,047,000 | (5,800,000, 6,232,000) | 9.8 | (9.4, 10.1) | 5,368,000 | (5,183,000, 5,615,000) | 8.7 | (8.4, 9.1) |
|
| ||||||||
| Alabama | 117,000 | (99,000, 137,000) | 12.7 | (10.7, 14.9) | 112,000 | (94,000, 132,000) | 12.1 | (10.2, 14.3) |
| Alaska | 13,000 | (11,000, 16,000) | 8.6 | (7.0, 10.4) | 12,000 | (10,000, 15,000) | 8.1 | (6.5, 9.9) |
| Arizona | 114,000 | (93,000, 138,000) | 8.2 | (6.7, 10.0) | 107,000 | (86,000, 130,000) | 7.7 | (6.2, 9.4) |
| Arkansas | 76,000 | (65,000, 89,000) | 12.8 | (10.9, 14.9) | 63,000 | (53,000, 73,000) | 10.6 | (9.0, 12.3) |
| California | 464,000 | (365,000, 586,000) | 6.1 | (4.8, 7.7) | 403,000 | (304,000, 510,000) | 5.3 | (4.1, 6.7) |
| Colorado | 93,000 | (75,000, 112,000) | 8.9 | (7.2, 10.8) | 80,000 | (64,000, 99,000) | 7.7 | (6.2, 9.5) |
| Connecticut | 74,000 | (62,000, 87,000) | 11.6 | (9.7, 13.6) | 68,000 | (57,000, 81,000) | 10.7 | (8.9, 12.7) |
| Delaware | 21,000 | (18,000, 24,000) | 12.1 | (10.3, 14.1) | 19,000 | (16,000, 22,000) | 11.1 | (9.4, 13.0) |
| District of Columbia | 9,000 | (7,000, 12,000) | 9.8 | (7.7, 12.3) | 9,000 | (7,000, 11,000) | 9.1 | (7.1, 11.5) |
| Florida | 334,000 | (277,000, 400,000) | 9.5 | (7.9, 11.4) | 313,000 | (256,000, 379,000) | 8.9 | (7.3, 10.8) |
| Georgia | 274,000 | (235,000, 315,000) | 12.7 | (10.9, 14.6) | 242,000 | (205,000, 280,000) | 11.2 | (9.6, 13.1) |
| Hawaii | 17,000 | (13,000, 20,000) | 6.6 | (5.2, 8.1) | 15,000 | (11,000, 18,000) | 5.8 | (4.5, 7.3) |
| Idaho | 31,000 | (26,000, 37,000) | 8.6 | (7.2, 10.2) | 29,000 | (24,000, 35,000) | 8.0 | (6.6, 9.6) |
| Illinois | 226,000 | (188,000, 270,000) | 9.3 | (7.7, 11.1) | 205,000 | (168,000, 248,000) | 8.4 | (6.9, 10.2) |
| Indiana | 153,000 | (131,000, 177,000) | 11.6 | (9.9, 13.4) | 133,000 | (114,000, 157,000) | 10.2 | (8.6, 11.9) |
| Iowa | 63,000 | (53,000, 73,000) | 10.5 | (8.8, 12.3) | 59,000 | (49,000, 69,000) | 9.8 | (8.2, 11.6) |
| Kansas | 64,000 | (53,000, 75,000) | 10.7 | (9.0, 12.6) | 58,000 | (48,000, 69,000) | 9.8 | (8.1, 11.7) |
| Kentucky | 110,000 | (94,000, 129,000) | 13.2 | (11.3, 15.4) | 100,000 | (84,000, 117,000) | 12.0 | (10.2, 14.1) |
| Louisiana | 150,000 | (129,000, 171,000) | 16.3 | (14.1, 18.6) | 128,000 | (110,000, 147,000) | 14.0 | (12.1, 16.0) |
| Maine | 26,000 | (22,000, 30,000) | 12.1 | (10.4, 13.9) | 23,000 | (20,000, 27,000) | 11.1 | (9.5, 12.9) |
| Maryland | 121,000 | (102,000, 143,000) | 10.6 | (8.9, 12.5) | 113,000 | (95,000, 135,000) | 9.9 | (8.3, 11.8) |
| Massachusetts | 123,000 | (104,000, 145,000) | 10.7 | (9.0, 12.6) | 118,000 | (98,000, 140,000) | 10.2 | (8.5, 12.1) |
| Michigan | 197,000 | (163,000, 236,000) | 10.6 | (8.8, 12.7) | 180,000 | (147,000, 217,000) | 9.7 | (7.9, 11.8) |
| Minnesota | 93,000 | (77,000, 112,000) | 8.7 | (7.2, 10.5) | 85,000 | (69,000, 103,000) | 8.0 | (6.5, 9.7) |
| Mississippi | 96,000 | (84,000, 111,000) | 15.8 | (13.7, 18.1) | 88,000 | (75,000, 102,000) | 14.4 | (12.4, 16.7) |
| Missouri | 124,000 | (105,000, 146,000) | 10.9 | (9.2, 12.8) | 118,000 | (98,000, 138,000) | 10.3 | (8.6, 12.1) |
| Montana | 19,000 | (16,000, 23,000) | 10.0 | (8.2, 12.2) | 17,000 | (14,000, 21,000) | 9.1 | (7.2, 11.1) |
| Nebraska | 29,000 | (23,000, 36,000) | 7.5 | (5.9, 9.3) | 26,000 | (21,000, 33,000) | 6.8 | (5.3, 8.6) |
| Nevada | 36,000 | (28,000, 44,000) | 6.3 | (5.0, 7.8) | 32,000 | (26,000, 41,000) | 5.7 | (4.5, 7.2) |
| New Hampshire | 26,000 | (23,000, 30,000) | 11.9 | (10.2, 13.7) | 25,000 | (21,000, 29,000) | 11.2 | (9.6, 13.1) |
| New Jersey | 136,000 | (110,000, 163,000) | 7.9 | (6.4, 9.5) | 117,000 | (93,000, 144,000) | 6.8 | (5.4, 8.4) |
| New Mexico | 34,000 | (28,000, 42,000) | 8.4 | (6.8, 10.3) | 31,000 | (25,000, 38,000) | 7.5 | (6.0, 9.3) |
| New York | 246,000 | (198,000, 300,000) | 7.2 | (5.8, 8.8) | 205,000 | (164,000, 256,000) | 6.0 | (4.8, 7.5) |
| North Carolina | 235,000 | (198,000, 276,000) | 12.1 | (10.2, 14.2) | 222,000 | (185,000, 263,000) | 11.4 | (9.6, 13.5) |
| North Dakota | 13,000 | (10,000, 15,000) | 9.0 | (7.4, 10.8) | 12,000 | (9,000, 14,000) | 8.3 | (6.8, 10.1) |
| Ohio | 256,000 | (216,000, 302,000) | 11.6 | (9.8, 13.7) | 227,000 | (192,000, 269,000) | 10.4 | (8.7, 12.3) |
| Oklahoma | 94,000 | (78,000, 109,000) | 11.7 | (9.8, 13.7) | 86,000 | (72,000, 102,000) | 10.8 | (9.0, 12.8) |
| Oregon | 66,000 | (54,000, 80,000) | 9.1 | (7.4, 11.1) | 63,000 | (51,000, 77,000) | 8.7 | (7.0, 10.7) |
| Pennsylvania | 204,000 | (168,000, 244,000) | 9.1 | (7.5, 10.9) | 179,000 | (146,000, 215,000) | 8.0 | (6.6, 9.6) |
| Rhode Island | 19,000 | (16,000, 23,000) | 11.3 | (9.6, 13.3) | 18,000 | (15,000, 21,000) | 10.6 | (8.9, 12.5) |
| South Carolina | 117,000 | (100,000, 135,000) | 12.7 | (10.9, 14.6) | 102,000 | (87,000, 118,000) | 11.1 | (9.5, 12.9) |
| South Dakota | 13,000 | (11,000, 16,000) | 7.5 | (6.1, 9.1) | 12,000 | (9,000, 14,000) | 6.7 | (5.5, 8.2) |
| Tennessee | 156,000 | (131,000, 182,000) | 12.5 | (10.5, 14.6) | 128,000 | (107,000, 152,000) | 10.4 | (8.7, 12.2) |
| Texas | 620,000 | (516,000, 737,000) | 10.1 | (8.4, 12.0) | 540,000 | (442,000, 644,000) | 8.8 | (7.3, 10.6) |
| Utah | 77,000 | (63,000, 93,000) | 10.0 | (8.2, 12.0) | 72,000 | (58,000, 87,000) | 9.3 | (7.5, 11.3) |
| Vermont | 10,000 | (9,000, 13,000) | 10.6 | (8.7, 12.8) | 9,000 | (7,000, 11,000) | 9.1 | (7.3, 11.2) |
| Virginia | 171,000 | (144,000, 201,000) | 10.8 | (9.1, 12.7) | 146,000 | (120,000, 173,000) | 9.2 | (7.6, 11.0) |
| Washington | 115,000 | (96,000, 137,000) | 8.3 | (6.9, 9.9) | 98,000 | (80,000, 118,000) | 7.1 | (5.9, 8.5) |
| West Virginia | 45,000 | (39,000, 52,000) | 14.6 | (12.5, 16.8) | 40,000 | (34,000, 47,000) | 12.9 | (11.0, 15.1) |
| Wisconsin | 101,000 | (83,000, 121,000) | 9.5 | (7.8, 11.4) | 88,000 | (71,000, 106,000) | 8.3 | (6.8, 10.1) |
| Wyoming | 10,000 | (8,000, 12,000) | 8.7 | (7.2, 10.4) | 9,000 | (7,000, 11,000) | 8.0 | (6.5, 9.7) |
| Range of State Estimates | 6.1–16.3 | 5.3–14.4 | ||||||
| State Estimate Median | 10.5 | 9.2 | ||||||
| State Estimate Interquartile Interval | 8.7–11.9 | 8.0–10.7 | ||||||
CI = Confidence Interval
Figure 1:
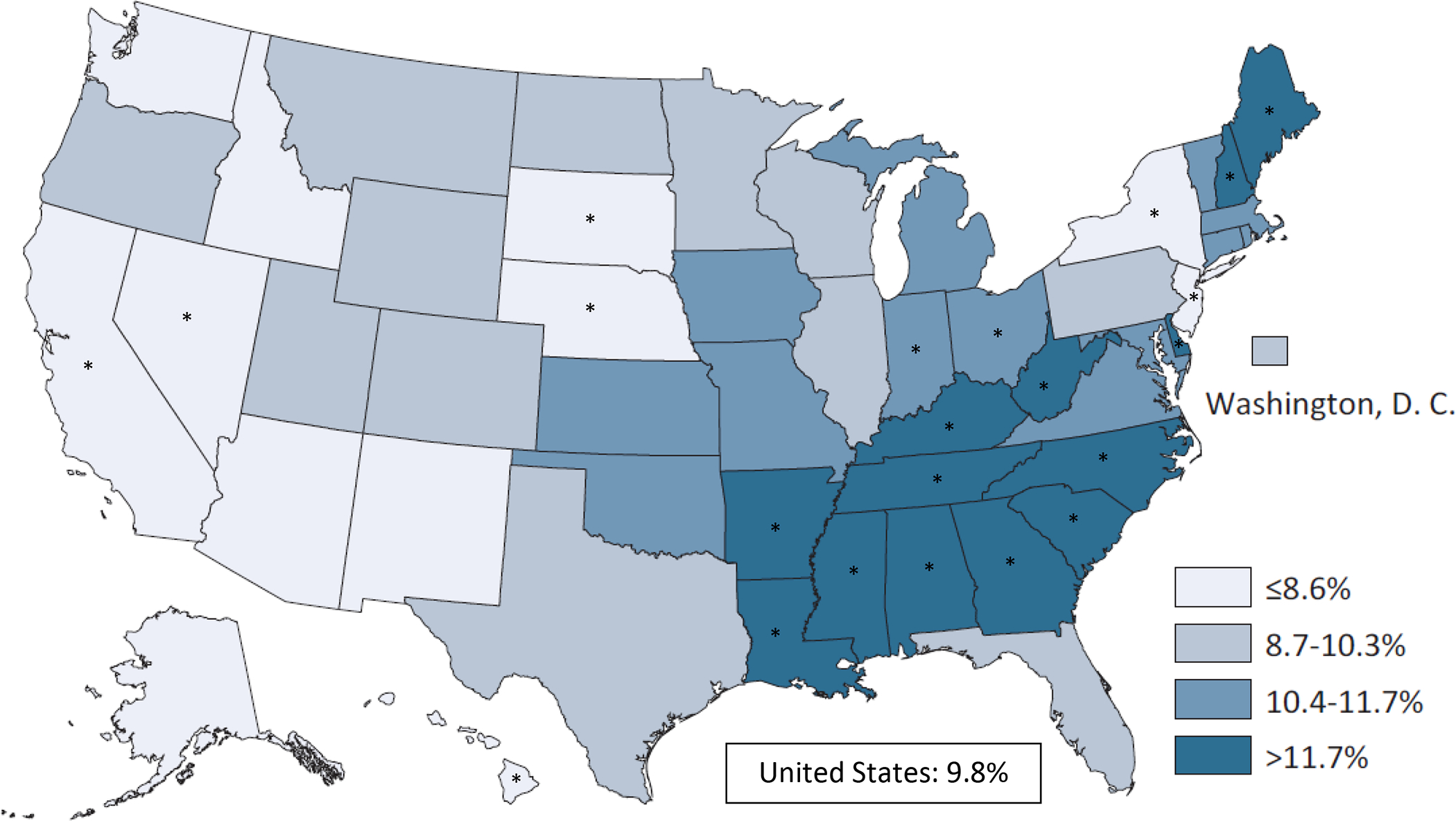
Weighted Prevalence Estimates of Parent-Reported Ever Diagnosed Attention-Deficit/Hyperactivity Disorder (ADHD) among Children/Adolescents Aged 3–17 Years by State, National Survey of Children’s Health, 2016–2019
* Indicates that state estimate has a statistically significant difference (p<0.05) from the estimate for the rest of the country
The overall percentage of U.S. children with current ADHD was 8.7%. The estimates for state-level prevalence of current ADHD among all children aged 3–17 years ranged from 5.3% to 14.4% (median=9.2%; IQI: 8.0–10.7; Table 1). There were twenty-three states with an estimate for current ADHD prevalence that was significantly different from the estimate for the rest of the country: eight states had lower estimates than the rest of the country (California, Hawaii, Nebraska, Nevada, New Jersey, New York, South Dakota, Washington) and fifteen states had higher estimates than the rest of the country (Alabama, Arkansas, Connecticut, Delaware, Georgia, Kentucky, Louisiana, Maine, Mississippi, New Hampshire, North Carolina, Oklahoma, Rhode Island, South Carolina, West Virginia; Figure 2). Trend tests did not detect differences over time in the prevalence of ever diagnosed ADHD or current ADHD overall and for most states; however, the prevalence of ever diagnosed and current ADHD increased in Alabama (p=0.05) and decreased in Wisconsin (p=0.01) over the four-year period (data not shown).
Figure 2:
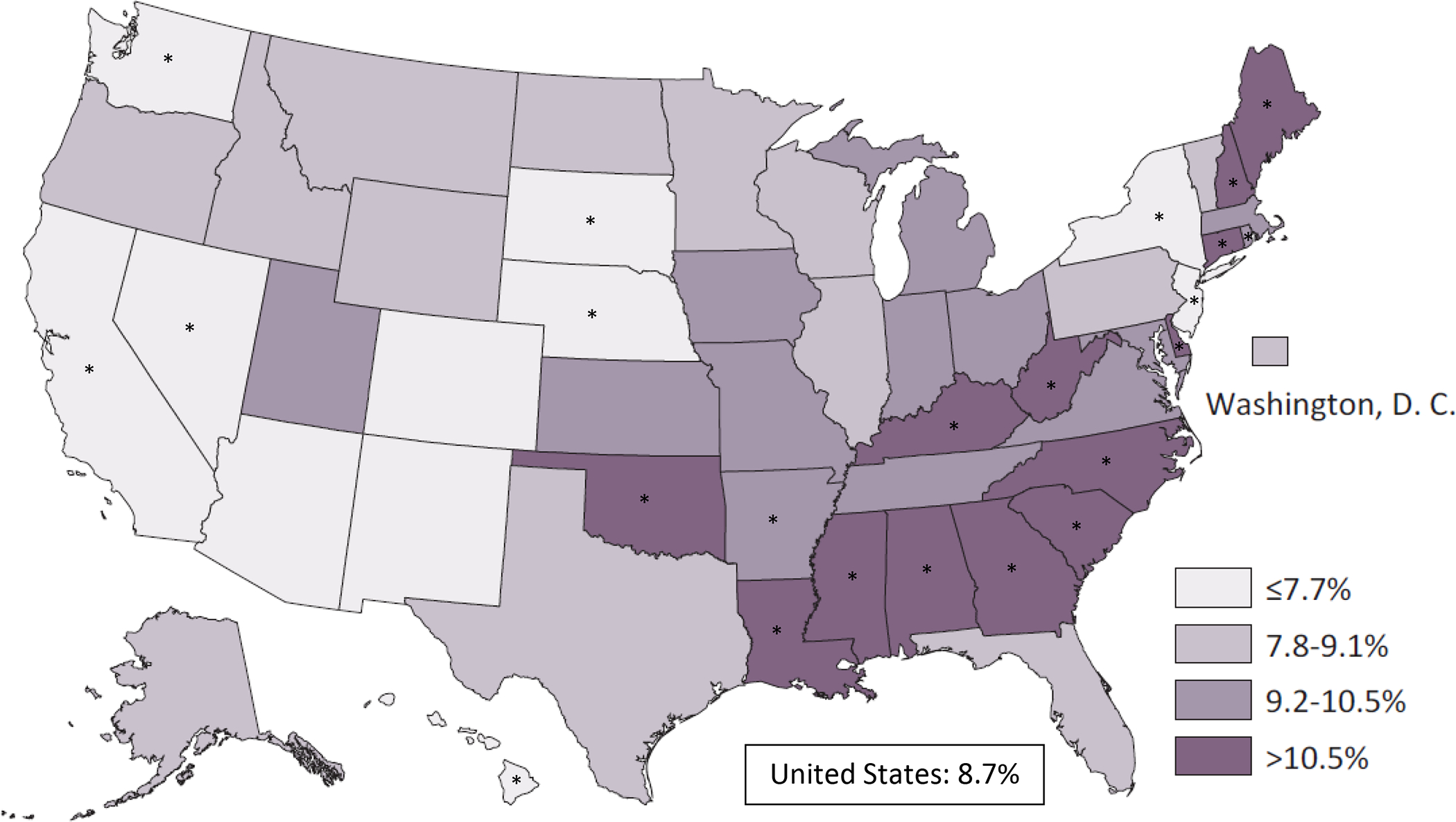
Weighted Prevalence Estimates of Parent-Reported Current Attention-Deficit/Hyperactivity Disorder (ADHD) among Children/Adolescents Aged 3–17 Years by State, National Survey of Children’s Health, 2016–2019
* Indicates that state estimate has a statistically significant difference (p<0.05) from the estimate for the rest of the country
Regarding ADHD-specific treatment, 62.2% of children aged 3–17 years with current ADHD were reported to currently be taking ADHD medication. The associated state-level estimates ranged from 37.8% to 81.4% (median=62.8%; IQI: 56.9–66.1; Table 2). There were twelve states that had an estimate for current ADHD medication use that was significantly different from the estimate for the rest of the country: five states and the District of Columbia had lower estimates than the rest of the country (California, Nevada, New Jersey, Oregon, Washington) and seven states had higher estimates than the rest of the country (Alabama, Delaware, Kentucky, Louisiana, Mississippi, Nebraska, Texas; Figure 3). For most states, there was not a linear trend over time in the percentage of children with current ADHD who were currently taking medication, but there was a significant increase from 2016 to 2019 in Connecticut (from 51.9% to 67.9%, p=0.04) and a significant decrease in New York (from 73.5% to 38.3%, p=0.003; data not shown).
Table 2:
Weighted Prevalence Estimates of Parent-Reported Attention-Deficit/Hyperactivity Disorder (ADHD) Treatment among U.S. Children with Parent Report of Current ADHD Aged 3–17 Years by State, National Survey of Children’s Health, 2016–2019
|
|
||||||
|---|---|---|---|---|---|---|
| Currently Taking ADHD Medication | Received Behavioral Treatment for ADHD in Past 12 Months | Received Medication and/or Behavioral Treatment | ||||
|
|
||||||
| Weighted % | 95% Confidence Interval | Weighted % | 95% Confidence Interval | Weighted % | 95% Confidence Interval | |
|
| ||||||
| United States | 62.2 | (60.3, 64.1) | 47.2 | (45.2, 49.1) | 76.4 | (74.6, 78.1) |
| Alabama | 77.0 | (69.5, 83.4) | 50.6 | (41.2, 59.9) | 84.3 | (77.5, 89.7) |
| Alaska | 61.4 | (51.0, 71.1) | 59.3 | (48.6, 69.4) | 79.4 | (70.6, 86.5) |
| Arizona | 55.2 | (43.8, 66.1) | 51.1 | (40.2, 61.9) | 71.7 | (59.3, 82.1) |
| Arkansas | 62.4 | (54.0, 70.2) | 46.5 | (38.3, 54.8) | 75.6 | (67.8, 82.3) |
| California | 46.4 | (33.6, 59.5) | 49.2 | (36.2, 62.2) | 72.4 | (58.7, 83.6) |
| Colorado | 55.9 | (44.3, 67.0) | 43.0 | (32.2, 54.3) | 69.8 | (57.5, 80.4) |
| Connecticut | 56.9 | (47.4, 66.0) | 54.2 | (44.9, 63.2) | 79.1 | (71.5, 85.5) |
| Delaware | 75.4 | (67.6, 82.1) | 51.7 | (43.0, 60.5) | 85.6 | (78.7, 90.9) |
| District of Columbia | 45.9 | (33.4, 58.8) | 54.1 | (41.1, 66.6) | 65.3 | (51.9, 77.1) |
| Florida | 65.1 | (54.2, 75.0) | 49.2 | (38.9, 59.5) | 75.3 | (63.8, 84.6) |
| Georgia | 69.5 | (61.3, 76.8) | 43.2 | (35.1, 51.5) | 79.5 | (71.7, 85.9) |
| Hawaii | 52.8 | (40.4, 65.0) | 55.7 | (43.5, 67.4) | 75.7 | (63.7, 85.3) |
| Idaho | 58.7 | (49.0, 68.0) | 51.8 | (41.9, 61.5) | 74.7 | (66.4, 81.9) |
| Illinois | 64.6 | (54.0, 74.3) | 58.9 | (49.0, 68.2) | 82.3 | (74.9, 88.3) |
| Indiana | 64.4 | (55.7, 72.4) | 49.9 | (41.4, 58.5) | 79.8 | (72.6, 85.8) |
| Iowa | 65.4 | (56.0, 74.0) | 50.9 | (41.6, 60.2) | 78.3 | (69.4, 85.7) |
| Kansas | 62.8 | (52.8, 72.0) | 42.0 | (33.0, 51.4) | 75.3 | (65.0, 83.8) |
| Kentucky | 73.7 | (65.8, 80.7) | 48.8 | (40.1, 57.5) | 84.0 | (76.4, 89.9) |
| Louisiana | 73.9 | (67.3, 79.9) | 42.1 | (34.7, 49.8) | 82.9 | (77.1, 87.8) |
| Maine | 61.0 | (53.1, 68.4) | 45.4 | (37.6, 53.4) | 76.9 | (69.7, 83.2) |
| Maryland | 68.5 | (59.9, 76.3) | 56.0 | (46.7, 65.1) | 83.9 | (76.7, 89.6) |
| Massachusetts | 57.9 | (48.1, 67.3) | 50.0 | (40.5, 59.5) | 76.4 | (67.5, 83.8) |
| Michigan | 63.4 | (52.5, 73.4) | 44.8 | (34.5, 55.5) | 77.0 | (67.3, 84.9) |
| Minnesota | 64.9 | (53.2, 75.3) | 59.2 | (49.4, 68.6) | 87.6 | (81.5, 92.2) |
| Mississippi | 73.8 | (65.6, 81.0) | 50.1 | (41.9, 58.4) | 82.3 | (74.5, 88.5) |
| Missouri | 62.8 | (53.4, 71.6) | 45.2 | (36.1, 54.5) | 70.2 | (60.6, 78.7) |
| Montana | 65.6 | (54.5, 75.5) | 56.8 | (45.3, 67.7) | 77.3 | (66.6, 85.8) |
| Nebraska | 81.4 | (72.7, 88.3) | 61.8 | (49.7, 72.9) | 91.6 | (85.8, 95.6) |
| Nevada | 37.8 | (27.1, 49.3) | 39.9 | (29.0, 51.7) | 58.8 | (46.0, 70.8) |
| New Hampshire | 65.4 | (57.9, 72.4) | 50.8 | (42.7, 58.9) | 78.9 | (72.4, 84.5) |
| New Jersey | 41.1 | (30.9, 51.9) | 41.7 | (31.1, 52.9) | 58.4 | (46.1, 69.9) |
| New Mexico | 62.1 | (50.8, 72.5) | 47.8 | (36.4, 59.4) | 73.7 | (63.5, 82.4) |
| New York | 54.8 | (43.2, 66.1) | 45.5 | (34.7, 56.7) | 70.5 | (57.5, 81.5) |
| North Carolina | 64.5 | (55.1, 73.1) | 46.2 | (37.0, 55.6) | 78.8 | (70.5, 85.2) |
| North Dakota | 64.0 | (52.9, 74.2) | 50.7 | (40.4, 61.0) | 78.0 | (68.0, 86.1) |
| Ohio | 58.1 | (49.0, 66.9) | 43.5 | (34.7, 52.6) | 75.1 | (66.8, 82.3) |
| Oklahoma | 66.1 | (55.9, 75.3) | 47.9 | (38.5, 57.4) | 79.0 | (70.5, 86.0) |
| Oregon | 50.2 | (39.1, 61.2) | 51.1 | (40.1, 62.1) | 70.2 | (59.4, 79.6) |
| Pennsylvania | 53.9 | (43.7, 63.9) | 54.4 | (44.4, 64.2) | 77.7 | (68.2, 85.4) |
| Rhode Island | 65.8 | (57.1, 73.7) | 48.3 | (39.3, 57.3) | 76.9 | (68.8, 83.8) |
| South Carolina | 64.2 | (56.1, 71.9) | 45.0 | (36.8, 53.4) | 74.1 | (66.2, 81.0) |
| South Dakota | 70.4 | (60.7, 78.9) | 45.2 | (34.7, 56.2) | 76.9 | (67.5, 84.7) |
| Tennessee | 62.8 | (53.4, 71.5) | 38.8 | (30.2, 47.9) | 74.1 | (64.8, 82.0) |
| Texas | 71.8 | (63.5, 79.1) | 40.5 | (31.2, 50.3) | 78.4 | (70.5, 85.0) |
| Utah | 59.5 | (48.0, 70.4) | 40.9 | (30.7, 51.6) | 72.2 | (60.8, 81.8) |
| Vermont | 52.0 | (40.7, 63.2) | 41.1 | (30.2, 52.6) | 65.0 | (53.2, 75.6) |
| Virginia | 62.7 | (52.5, 72.1) | 45.8 | (36.5, 55.3) | 76.9 | (66.7, 85.1) |
| Washington | 47.9 | (38.5, 57.4) | 39.2 | (30.1, 48.9) | 61.5 | (51.8, 70.5) |
| West Virginia | 67.5 | (59.1, 75.0) | 46.5 | (38.0, 55.2) | 76.6 | (69.0, 83.1) |
| Wisconsin | 69.8 | (58.3, 79.7) | 51.3 | (40.7, 61.8) | 81.4 | (70.0, 89.8) |
| Wyoming | 59.8 | (49.3, 69.7) | 54.3 | (43.8, 64.5) | 78.9 | (69.3, 86.6) |
| Range of State Estimates | 37.8–81.4 | 38.8–61.8 | 58.4–91.6 | |||
| State Estimate Median | 62.8 | 48.8 | 76.9 | |||
| State Estimate Interquartile Interval | 56.9–66.1 | 44.8–51.7 | 73.7–79.4 | |||
Figure 3:
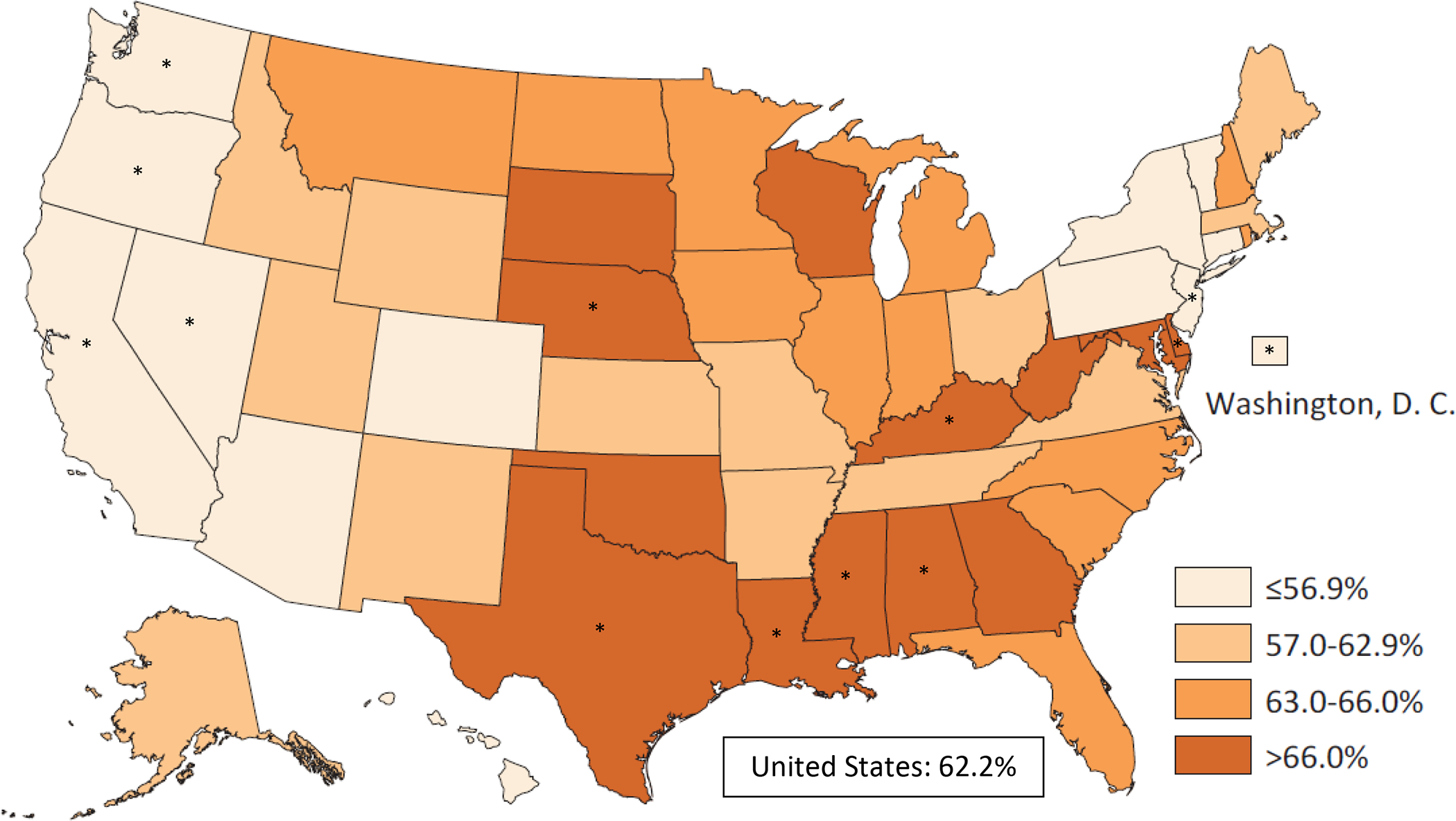
Weighted Prevalence Estimates of Parent-Reported Current Attention-Deficit/Hyperactivity Disorder (ADHD) Medication Treatment among Children/Adolescents Aged 3–17 Years with Current ADHD by State, National Survey of Children’s Health, 2016–2019
* Indicates that state estimate has a statistically significant difference (p<0.05) from the estimate for the rest of the country
A lower percentage of children with current ADHD had received behavioral treatment for ADHD in the past year (47.2%) than who were currently taking ADHD medication (62.2%). The state-level prevalence estimates of children with current ADHD who received behavioral treatment for ADHD in the past year ranged from 38.8% to 61.8% (median=48.8%; IQI: 44.8–51.7; Table 2). There were four states that had an estimate of past year behavioral treatment for ADHD that was significantly higher than the rest of the country (Alaska, Illinois, Minnesota, Nebraska); there were no states that had a significantly lower estimate than the rest of the country (Figure 4). The overall percentage of children with current ADHD who received behavioral treatment increased from 46.4% in 2016 to 51.8% in 2019 (p=0.01); four states (Georgia, Illinois, Iowa, Texas) also had increases over time in the percentage of children receiving behavioral treatment, while Oregon had a decrease over the four-year period (p=0.0001; data not shown).
Figure 4:
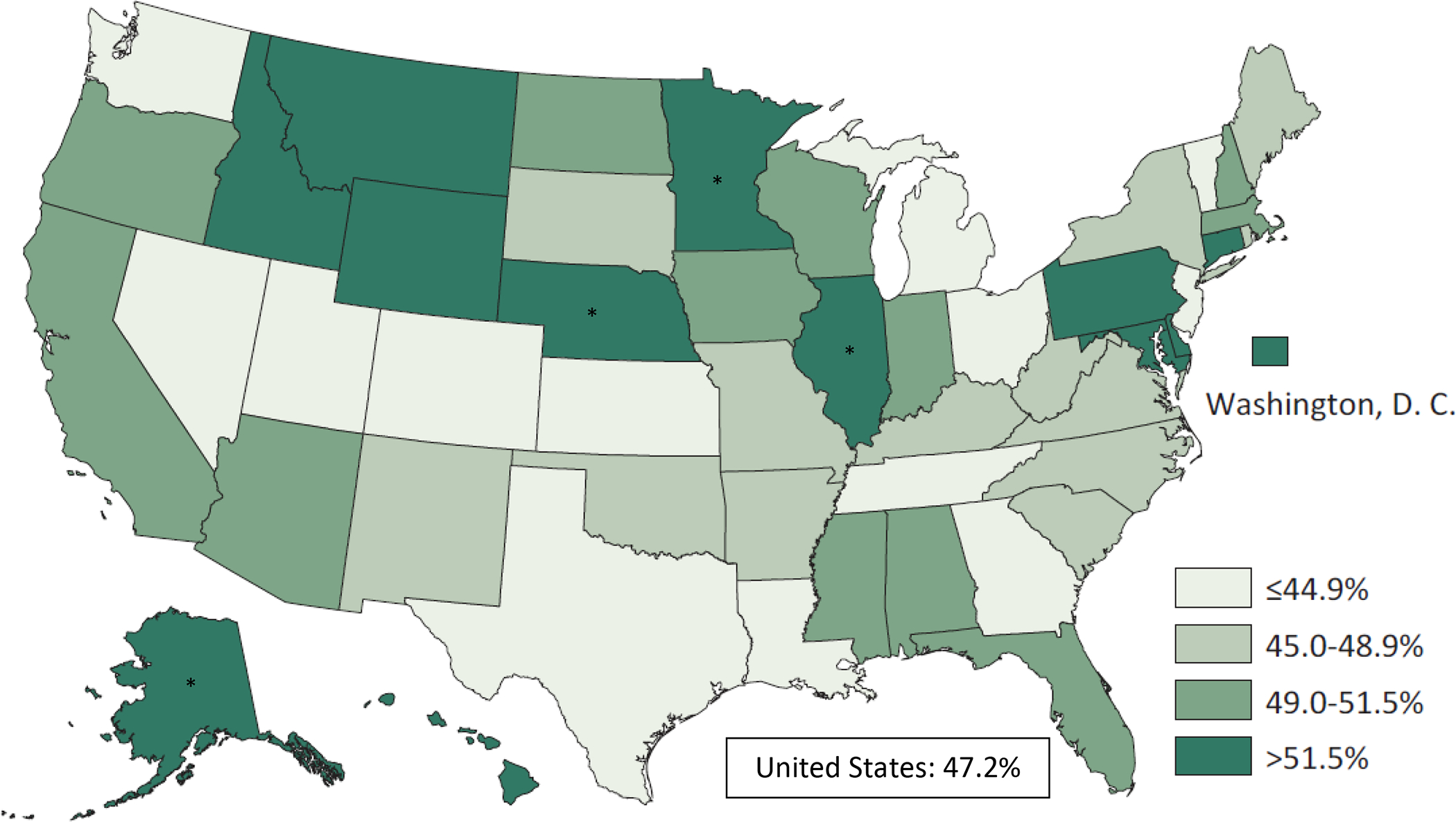
Weighted Prevalence Estimates of Parent-Reported Receipt of Behavioral Treatment for Attention-Deficit/Hyperactivity Disorder (ADHD) in the Past Year among Children/Adolescents Aged 3–17 Years with Current ADHD by State, National Survey of Children’s Health, 2016–2019
* Indicates that state estimate has a statistically significant difference (p<0.05) from the estimate for the rest of the country
In most states, the point estimate for percentage of children with current ADHD receiving medication was higher than the point estimate for percentage of children with current ADHD who had received behavioral treatment for ADHD in the past year (Figure 5), and the correlation between the two treatment indicators across the states was low (r=0.23). There was a moderate positive correlation between state-level prevalence of current ADHD and percentage of children with current ADHD who received ADHD medication (r=0.57), but a small negative correlation between prevalence of current ADHD and percentage of children with current ADHD who received behavioral treatment for ADHD (r=−0.13). The estimated percentage of children with current ADHD who received either medication and/or behavioral treatment ranged from 58.4% to 91.6% (median=76.9%; IQI: 73.7–79.4; Table 2) across states. The percentage of children with current ADHD receiving either treatment increased in two states (Iowa, Minnesota) over the four-year period, and decreased in four states (Massachusetts, New York, North Dakota, Oregon; data not shown).
Figure 5:
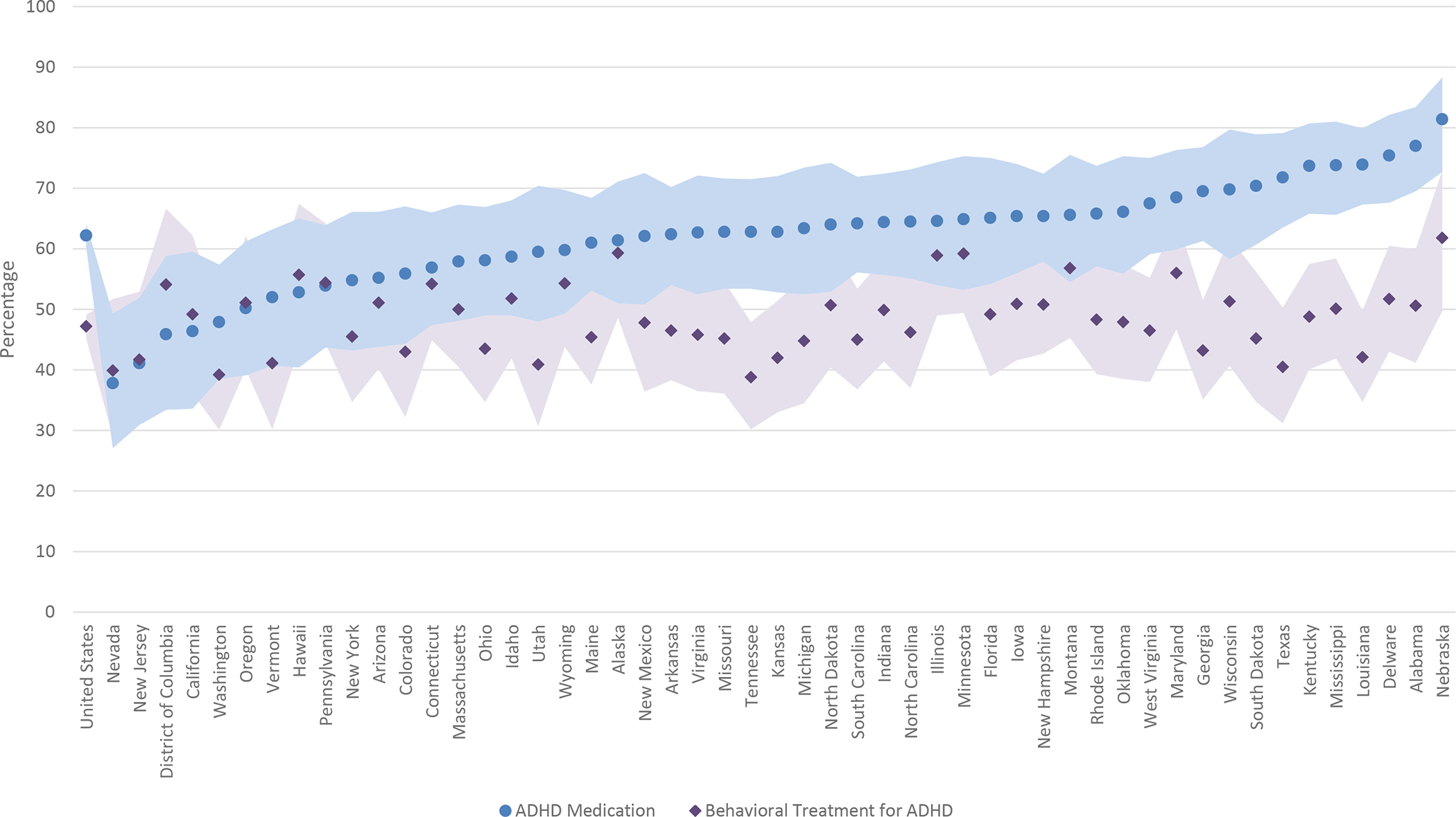
Percentage* of Children/Adolescents Aged 3–17 Years with Current Attention-Deficit/Hyperactivity Disorder (ADHD) Who Are Receiving ADHD Medication and/or Behavioral Treatment for ADHD, National Survey of Children’s Health, 2016–2019
* States are ordered from lowest to highest based on the percentage of children with current ADHD receiving ADHD medication.
Note: Shaded area represents 95% confidence interval for treatment point estimates by state.
As for the broader definitions of treatment, 69.4% of U.S. children with current ADHD were reported to currently be taking ADHD medication and/or have taken any medication for difficulties with emotions, concentration, or behavior in the past year, with state-level estimates ranging from 44.1% to 89.4% (median=71.7%; IQI: 64.9–74.8; Table 3). A lower percentage of U.S. children with current ADHD were reported to have received behavioral treatment for ADHD and/or received any treatment or counseling from a mental health professional in the past year (59.7%) than were reported to be taking medication. State-level estimates for receipt of behavioral treatment for ADHD or any mental health treatment or counseling ranged from 49.0% to 74.8% (median=61.8%; IQI: 56.3–67.5; Table 3). Overall, 82.5% of children with current ADHD had received at least one of the four types of treatment considered in this analysis; the state-level estimates for the any treatment indicator ranged from 65.4% to 94.1% (median=84.9%; IQI: 79.5–87.4; Table 3).
Table 3:
Weighted Prevalence Estimates of Mental Health Treatment among U.S. Children with Parent-Reported Current Attention-Deficit/Hyperactivity Disorder (ADHD) Aged 3–17 Years by State, National Survey of Children’s Health, 2016–2019
| Currently taking ADHD medication or other medication for difficulties with emotions, concentration, or behavior in past 12 months | Received behavioral treatment for ADHD or received any treatment or counseling from a mental health professional in past 12 months | Currently taking ADHD medication or other medication for difficulties with emotions, concentration, or behavior, or received behavioral treatment for ADHD or any treatment or counseling from a mental health professional in past 12 months | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Weighted % | 95% Confidence Interval | Weighted % | 95% Confidence Interval | Weighted % | 95% Confidence Interval | |
|
| ||||||
| United States | 69.4 | (67.5, 71.3) | 59.7 | (57.7, 61.7) | 82.5 | (80.8, 84.1) |
| Alabama | 84.3 | (78.0, 89.3) | 63.6 | (55.0, 71.5) | 91.2 | (86.7, 94.6) |
| Alaska | 72.6 | (63.3, 80.6) | 68.5 | (58.0, 77.8) | 86.7 | (79.8, 91.9) |
| Arizona | 65.1 | (54.7, 74.6) | 62.3 | (50.6, 73.0) | 78.4 | (68.1, 86.7) |
| Arkansas | 70.2 | (61.9, 77.5) | 52.8 | (44.5, 60.9) | 81.0 | (73.5, 87.1) |
| California | 52.4 | (39.1, 65.4) | 59.3 | (45.1, 72.5) | 76.0 | (61.7, 87.0) |
| Colorado | 64.4 | (52.4, 75.2) | 56.3 | (44.5, 67.5) | 76.2 | (63.2, 86.3) |
| Connecticut | 63.5 | (53.9, 72.4) | 70.4 | (62.1, 77.9) | 86.9 | (80.2, 92.0) |
| Delaware | 80.6 | (73.3, 86.6) | 65.3 | (56.8, 73.1) | 87.8 | (81.1, 92.9) |
| District of Columbia | 50.5 | (37.7, 63.3) | 73.5 | (61.6, 83.4) | 79.3 | (67.5, 88.3) |
| Florida | 68.7 | (57.6, 78.4) | 58.9 | (48.3, 69.0) | 78.3 | (66.5, 87.5) |
| Georgia | 76.3 | (68.5, 82.9) | 52.8 | (44.4, 61.0) | 84.9 | (77.5, 90.6) |
| Hawaii | 54.6 | (42.1, 66.7) | 66.2 | (54.1, 76.9) | 79.5 | (67.5, 88.6) |
| Idaho | 68.3 | (58.8, 76.7) | 69.3 | (60.6, 77.1) | 87.2 | (81.1, 91.9) |
| Illinois | 72.9 | (63.1, 81.3) | 74.0 | (65.3, 81.6) | 90.0 | (83.6, 94.5) |
| Indiana | 74.2 | (65.6, 81.6) | 60.6 | (52.5, 68.4) | 86.9 | (81.4, 91.9) |
| Iowa | 77.7 | (69.9, 84.4) | 67.5 | (58.2, 75.8) | 87.8 | (81.4, 92.6) |
| Kansas | 68.3 | (58.1, 77.3) | 61.7 | (52.4, 70.3) | 80.4 | (71.5, 87.5) |
| Kentucky | 80.8 | (73.4, 86.9) | 61.0 | (52.1, 69.3) | 88.2 | (80.8, 93.5) |
| Louisiana | 80.7 | (74.7, 85.8) | 52.0 | (44.4, 59.6) | 88.1 | (82.8, 92.3) |
| Maine | 67.8 | (60.0, 74.9) | 60.4 | (52.2, 68.2) | 85.7 | (79.7, 90.5) |
| Maryland | 74.1 | (65.7, 81.3) | 67.8 | (58.3, 76.4) | 90.5 | (84.1, 94.9) |
| Massachusetts | 61.9 | (55.8, 71.2) | 64.0 | (54.8, 72.5) | 78.8 | (69.9, 86.1) |
| Michigan | 71.7 | (60.7, 81.1) | 59.4 | (48.2, 69.9) | 85.5 | (76.5, 92.0) |
| Minnesota | 70.2 | (58.0, 80.6) | 74.8 | (66.9, 81.7) | 92.4 | (87.1, 96.0) |
| Mississippi | 77.3 | (69.1, 84.2) | 59.1 | (51.0, 66.9) | 85.0 | (77.5, 90.8) |
| Missouri | 72.5 | (63.9, 80.1) | 57.5 | (48.4, 66.4) | 79.9 | (71.3, 86.8) |
| Montana | 77.8 | (68.6, 85.4) | 70.2 | (59.9, 79.3) | 87.4 | (79.4, 93.2) |
| Nebraska | 89.4 | (82.9, 94.0) | 68.9 | (57.2, 79.1) | 94.1* | (88.8, 97.3) |
| Nevada | 44.1 | (32.6, 56.0) | 49.5 | (37.4, 61.7) | 65.4 | (52.1, 77.2) |
| New Hampshire | 71.6 | (64.6, 78.0) | 61.0 | (53.3, 68.4) | 84.9 | (79.2, 89.6) |
| New Jersey | 49.8 | (38.5, 61.2) | 57.6 | (45.5, 69.0) | 67.6 | (54.6, 78.9) |
| New Mexico | 64.9 | (53.6, 75.1) | 63.5 | (52.1, 73.8) | 78.8 | (68.6, 86.9) |
| New York | 60.2 | (48.0, 71.5) | 62.4 | (51.3, 72.6) | 81.6 | (70.8, 89.8) |
| North Carolina | 72.1 | (63.1, 80.0) | 53.5 | (44.3, 62.5) | 81.5 | (73.1, 88.3) |
| North Dakota | 73.4 | (62.2, 82.8) | 66.8 | (57.4, 75.4) | 86.4 | (78.0, 92.6) |
| Ohio | 68.3 | (59.2, 76.4) | 56.0 | (46.6, 65.1) | 84.3 | (77.0, 89.9) |
| Oklahoma | 73.0 | (62.5, 81.9) | 66.9 | (58.0, 75.0) | 88.3 | (80.7, 93.6) |
| Oregon | 58.6 | (47.1, 69.5) | 67.9 | (57.5, 77.2) | 81.1 | (71.0, 88.9) |
| Pennsylvania | 68.9 | (59.0, 77.6) | 65.6 | (55.6, 74.6) | 85.7 | (78.3, 91.3) |
| Rhode Island | 72.4 | (64.1, 79.6) | 62.9 | (53.5, 71.5) | 85.5 | (78.6, 90.8) |
| South Carolina | 73.2 | (65.4, 80.0) | 53.4 | (45.2, 61.4) | 80.9 | (73.2, 87.1) |
| South Dakota | 77.9 | (69.1, 85.1) | 65.5 | (55.9, 74.3) | 84.8 | (76.6, 91.1) |
| Tennessee | 73.2 | (64.3, 80.9) | 55.7 | (46.5, 64.6) | 81.0 | (72.3, 87.9) |
| Texas | 74.3 | (66.1, 81.4) | 53.3 | (43.4, 63.1) | 80.9 | (73.2, 87.2) |
| Utah | 66.2 | (54.0, 77.0) | 49.0 | (38.2, 59.8) | 78.5 | (66.6, 87.7) |
| Vermont | 59.7 | (48.1, 70.5) | 56.0 | (44.5, 67.1) | 75.9 | (63.6, 85.6) |
| Virginia | 75.5 | (67.0, 82.8) | 61.3 | (51.2, 70.7) | 87.2 | (79.7, 92.7) |
| Washington | 58.1 | (48.6, 67.3) | 49.1 | (39.6, 58.6) | 69.5 | (60.0, 78.0) |
| West Virginia | 74.8 | (67.0, 81.6) | 61.8 | (53.2, 69.9) | 84.1 | (77.1, 89.6) |
| Wisconsin | 76.7 | (65.0, 86.0) | 68.5 | (58.4, 77.5) | 87.6* | (77.7, 94.2) |
| Wyoming | 70.4 | (59.9, 79.6) | 71.1 | (62.3, 78.9) | 88.6 | (82.2, 93.3) |
| Range of State Estimates | 44.1–89.4 | 49.0–74.8 | 65.4–94.1 | |||
| State Estimate Median | 71.7 | 61.8 | 84.9 | |||
| State Estimate Interquartile Interval | 64.9–74.8 | 56.3–67.5 | 79.5–87.4 | |||
While the point estimate meets NCHS standards of precision, its complement does not. The complement of this percentage has a relative confidence interval width greater than 130%, indicating that the complementary percentage estimates may be unreliable.
Discussion
Consistent with previous examinations of state-level estimates for ADHD diagnosis and treatment (Blue Cross Blue Shield, 2019; Board et al., 2020; Bozinovic et al., 2021; Centers for Disease Control and Prevention, 2010; McDonald & Jalbert, 2013; Piper et al., 2018; Visser et al., 2015; Visser, Blumberg, et al., 2013; Visser et al., 2014; Visser et al., 2016), data from the 2016–2019 NSCH suggests that there is substantial variation in state-level prevalence of diagnosed ADHD and associated treatment among children and adolescents aged 3–17 years. The percentage of children who ever received an ADHD diagnosis was more than twice as high in the states with the highest prevalence (Louisiana, Mississippi, and West Virginia) than the state with the lowest prevalence (California); most states with high ever diagnosed and current ADHD prevalence estimates were in the South. In 46 states, more than half of children with current ADHD received ADHD medication. The states with the highest percentage of children with current ADHD who received medication were in the Midwest and South, while the states with the lowest percentage of children receiving medication were in the Northeast and West. The percentage of children with current ADHD who received behavioral treatment specifically for ADHD was lower than the percentage who received ADHD medication in 44 states, and in 29 states, less than half of children with current ADHD had received behavioral treatment for ADHD in the past year.
These are the first state-based estimates of behavioral treatment for ADHD among all children with current ADHD including those who do not meet special health care need status, and suggest that some children with ADHD were not receiving behavioral treatment in line with clinical guidelines (American Academy of Child and Adolescent Psychiatry, 2007; Subcommittee on Attention-Deficit/Hyperactivity Disorder et al., 2011; Wolraich et al., 2019). In 16 states, more than a quarter of children with current ADHD were receiving neither ADHD medication nor behavioral treatment for ADHD. It should be noted that the ADHD-specific treatment questions only captured general indicators of medication or behavioral treatment, and it cannot be assumed that all children who received treatment for ADHD were receiving recommended evidence-based treatment based on their age and symptoms. Future research could examine state-level differences in treatment receipt by age to identify states where there is more or less alignment between clinical guidance and broad indicators of actual practice; however, this will require more years of data to produce stable estimates for each age group using the NSCH. The percentage of children receiving any treatment was higher when the broader derived indicators of mental health treatment were incorporated into the analysis, but these indicators may be capturing other treatment modalities that are not specific to address ADHD symptoms and impairment. However, even with the broader treatment indicators, nearly one in five children with current ADHD were reported to not be receiving any treatment.
Though it was not a primary focus of this study, we tested for linear trends over time (2016–2019) for the ADHD diagnostic and treatment indicators. For most states, there were not trends over time detected for the diagnosis or treatment of ADHD, but we did identify a small number of states that showed increases and decreases in estimates over the four-year period, primarily for the treatment indicators. Because these analyses involved a large number of statistical tests (more than 400), it is difficult to distinguish between true changes over time and differences that arose based on Type I error; investigating state-level trends over time as more years of data become available would be an important area of future research. Also, the national percentage of children receiving behavioral treatment for ADHD increased over time; this is another trend that may be important to monitor.
There were some patterns identified regarding the variation of ADHD diagnosis and treatment estimates across states. States with a higher prevalence of current ADHD were more likely to have higher estimates of ADHD medication use, and somewhat less likely to have higher estimates of behavioral treatment for ADHD. There was a small positive correlation between state-level estimates of ADHD medication and behavioral treatment receipt. A number of factors might contribute to the observed variation in ADHD diagnosis and treatment estimates across states. First, differences have been previously documented in the diagnosis and treatment of ADHD by demographic subgroups, such as those based on race/ethnicity or poverty status (Bozinovic et al., 2021; Danielson et al., 2018; Visser et al., 2014), and differences in state-level demographics may be driving the differences in state-level rates of ADHD diagnosis and treatment. State-level educational or health care system policies could also affect the diagnostic and treatment practices for ADHD in a given state. Some examples of such policies include consequential accountability reforms in education (Bokhari & Schneider, 2011; Fulton et al., 2015), special education funding policies (Morrill, 2018), Medicaid policies such as waivers or medication prior authorization (Hulkower et al., 2017; Lindly et al., 2022; Schor & Johnson, 2021), or pharmaceutical detailing policies (Larkin et al., 2017). Variation by state in the characteristics and density of health care providers may also influence state-level rates of ADHD diagnosis and treatment (Andrilla et al., 2018; Fulton et al., 2009; Harati et al., 2020; McBain et al., 2019), as the availability of trained providers could affect families’ ability to get an appropriate ADHD diagnosis or receive certain types of treatment for their children.
State-level estimates are an important component to the surveillance of mental disorders among children. Estimates from smaller geographic areas, such as states, reveal the heterogeneity in prevalence that is smoothed out in a national estimate, which may draw attention to relevant differences in medical and educational practices, state-level policies, and exposures or risk factors that may be potentially related to the development of the disorder of interest (Broder-Fingert et al., 2018). The state-level estimates of diagnosed ADHD prevalence and associated treatment in 2016–2019 provides updated evidence for state-level heterogeneity related to all ADHD indicators (Blue Cross Blue Shield, 2019; Board et al., 2020; McDonald & Jalbert, 2013; Piper et al., 2018; Visser et al., 2015; Visser, Blumberg, et al., 2013; Visser et al., 2014; Visser et al., 2016). Additionally, these state-level estimates can inform state-specific activities, such as surveillance of stimulant medication prescribing in California (Tseregounis et al., 2020), efforts to improve care for ADHD in Louisiana (Kumar & Gleason, 2019), building support for school policies for mental health in South Carolina (Franke et al., 2021), or identification of opportunities to expand availability of ADHD-related diagnosis and treatment services in North Carolina (Canu, 2020). States may use state-level estimates derived from national surveys to develop or supplement other state-based mental health surveillance (Public Health Informatics Institute, 2021) in order to identify areas in need of prevention and intervention activities (Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory, 2021). Additionally, more localized data collected by states or derived from national surveys using small area estimation techniques would further allow for data-driven planning to address community-level disparities (Scally et al., 2017).
This study is subject to at least five limitations. First, these analyses relied on parent-reported data and may be subject to recall or social desirability bias. However, previous work has shown that the prevalence estimates for diagnosed ADHD using national survey data are similar to those obtained from clinical records, indicating convergent validity between the two indictor types (Visser, Danielson, et al., 2013). Second, responses to the ADHD-related indicators have not been validated against clinical judgment or medical or education records, and parents may over- or under-report diagnosis and treatment information based on their understanding of the survey questions relative to their child’s diagnostic and treatment experience. Third, the questions regarding ADHD medication and behavioral treatment for ADHD were broad and did not specify type, quality, duration, or sequencing of treatment. Therefore, we were unable to estimate the percentage of children with ADHD who received evidence-based treatments according to age-specific recommendations from clinical guidelines (Wolraich et al., 2019). Finally, the overall annual response rate for the NSCH was approximately 40%, which may subject the results to non-response bias. However, sample weights were incorporated in the analysis to offset non-response bias and produce geographically-representative estimates, and a U.S. Census Bureau analysis to quantify possible non-response bias found there was no strong or consistent evidence of non-response bias in the 2016 NSCH (U.S. Census Bureau, 2017).
This report describes variation among state-level estimates of the diagnosis and treatment of ADHD among U.S. children and adolescents. These estimates can be used as a baseline to track state-level trends using the redesigned NSCH, which included a shift in mode of administration (from telephone to web-based or paper and pencil) and has had annual data releases beginning with the 2016 survey. This study also provides the first state-level estimates of behavioral treatment among all noninstitutionalized U.S. children with current ADHD, which is significant because clinical practice guidelines recommend behavior therapy in combination with medication for school-aged children and as the first-line treatment for children aged 4–5 years diagnosed with ADHD (Subcommittee on Attention-Deficit/Hyperactivity Disorder et al., 2011; Wolraich et al., 2019). The state-level results provided in this report can be used by state-level policymakers, public health practitioners, health care providers, and other stakeholders to help address the service needs of children and adolescents with ADHD in their state.
Footnotes
Disclaimer:
The views expressed in this article are those of the authors and do not necessarily reflect the official policies of the U.S. Department of Health and Human Services, the Centers for Disease Control and Prevention, or the Health Resources and Services Administration, nor does mention of the department or agency names imply endorsement by the U.S. government.
References
- American Academy of Child and Adolescent Psychiatry. (2007). Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 46(7), 894–921. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, 5th edition. American Psychiatric Association. [Google Scholar]
- Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, & Larson EH (2018). Geographic variation in the supply of selected behavioral health providers. American Journal of Preventive Medicine, 54(6S3), S199–S207. 10.1016/j.amepre.2018.01.004 [DOI] [PubMed] [Google Scholar]
- Bitsko RH, Claussen AH, Lichstein J, Black LI, Everett Jones S, Danielson ML, Hoenig JM, Jack SPD, Brody DJ, Gyawali S, Maenner MJ, Warner M, Holland KM, Meyer LN, Perou P, Crosby AE, Blumberg S, Avenevoli S, Kaminski JW, & Ghandour R (2022). Surveillance of children’s mental health – United States, 2013 – 2019. MMWR Suppl, 71(2), 1–42. 10.15585/mmwr.su7102a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blue Cross Blue Shield. (2019). The impact of attention deficit hyperactivity disorder on the health of America’s children. The Health of America Report. https://www.bcbs.com/sites/default/files/file-attachments/health-of-america-report/Health_of_America_Report-ADHD.pdf
- Board AR, Guy G, Jones CM, & Hoots B (2020). Trends in stimulant dispensing by age, sex, state of residence, and prescriber specialty — United States, 2014–2019. Drug and Alcohol Dependence, 217, 108297. 10.1016/j.drugalcdep.2020.108297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokhari FA, & Schneider H (2011). School accountability laws and the consumption of psychostimulants. Journal of Health Economics, 30(2), 355–372. 10.1016/j.jhealeco.2011.01.007 [DOI] [PubMed] [Google Scholar]
- Bozinovic K, McLamb F, O’Connell K, Olander N, Feng Z, Haagensen S, & Bozinovic G (2021). U.S. national, regional, and state-specific socioeconomic factors correlate with child and adolescent ADHD diagnoses pre-COVID-19 pandemic. Scientific Reports, 11(1), 22008. 10.1038/s41598-021-01233-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broder-Fingert S, Sheldrick CR, & Silverstein M (2018). The value of state differences in autism when compared to a national prevalence estimate. Pediatrics, 142(6). 10.1542/peds.2018-2950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canu W (2020). ADHD in North Carolina: Prevalence, treatment, and looking to the future. North Carolina Medical Journal, 81(2), 122–125. 10.18043/ncm.81.2.122 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2010). Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children — United States, 2003 and 2007. MMWR Morb Mortal Wkly Rep, 59(44), 1439–1443. http://www.cdc.gov/mmwr/pdf/wk/mm5944.pdf [PubMed] [Google Scholar]
- Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, & Blumberg SJ (2018). Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. Journal of Clinical Child & Adolescent Psychology, 47(2), 199–212. 10.1080/15374416.2017.1417860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erskine HE, Norman RE, Ferrari AJ, Chan GCK, Copeland WE, Whiteford HA, & Scott JG (2016). Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: A systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 55(10), 841–850. 10.1016/j.jaac.2016.06.016 [DOI] [PubMed] [Google Scholar]
- Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar J, Ramos-Quiroga JA, Rohde LA, Sonuga-Barke EJS, Tannock R, & Franke B (2015). Attention-deficit/hyperactivity disorder (ADHD). Nature Reviews Disease Primers, 1, 15–27. 10.1038/nrdp.2015.27 [DOI] [PubMed] [Google Scholar]
- Fleming M, Fitton CA, Steiner MFC, McLay JS, Clark D, King A, Mackay DF, & Pell JP (2017). Educational and health outcomes of children treated for attention-deficit/hyperactivity disorder JAMA Pediatrics, 171(7). 10.1001/jamapediatrics.2017.0691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franke KB, Paton M, & Weist M (2021). Building policy support for school mental health in South Carolina. School Psychology Review, 50(1), 110–121. 10.1080/2372966X.2020.1819756 [DOI] [Google Scholar]
- Fulton BD, Scheffler RM, & Hinshaw SP (2015). State variation in increased ADHD prevalence: Links to NCLB school accountability and state medication laws. Psychiatric Services, 66(10), 1074–1082. 10.1176/appi.ps.201400145 [DOI] [PubMed] [Google Scholar]
- Fulton BD, Scheffler RM, Hinshaw SP, Levine P, Stone S, Brown TT, & Modreck S (2009). National variation of ADHD diagnostic prevalence and medication use: Health care providers and education policies. Psychiatric Services, 60(8), 1075–1083. 10.1176/ps.2009.60.8.1075 [DOI] [PubMed] [Google Scholar]
- Ghandour RM, Jones JR, Lebrun-Harris LA, Minnaert J, Blumberg SJ, Fields J, Bethell C, & Kogan MD (2018). The design and implementation of the 2016 National Survey of Children’s Health. Maternal and Child Health Journal, 22, 1093–1102. 10.1007/s10995-018-2526-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harati PM, Cummings JR, & Serban N (2020). Provider-level caseload of psychosocial services for Medicaid-insured children. Public Health Reports, 135(5), 599–610. 10.1177/0033354920932658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hechtman L, Swanson JM, Sibley MH, Stehli A, Owens EB, Mitchell JT, Arnold LE, Molina BS, Hinshaw SP, Jensen PS, Abikoff HB, Perez Algorta G, Howard AL, Hoza B, Etcovitch J, Houssais S, Lakes KD, Nichols JQ, & Group MTAC (2016). Functional adult outcomes 16 years after childhood diagnosis of attention-deficit/hyperactivity disorder: MTA results. Journal of the American Academy of Child & Adolescent Psychiatry, 55(11), 945–952.e2. 10.1016/j.jaac.2016.07.774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulkower RL, Kelley M, Cloud LK, & Visser SN (2017). Medicaid prior authorization policies for medication treatment of attention-deficit/hyperactivity disorder in young children, United States, 2015. Public Health Reports, 132(6), 654–659. 10.1177/0033354917735548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korn EL, & Graubard BI (1998). Confidence intervals for proportions with small expected number of positive counts estimated from survey data. Survey Methodology, 24, 193–201. [Google Scholar]
- Kumar R, & Gleason MM (2019). Pediatric attention-deficit/hyperactivity disorder in Louisiana: Trends, challenges, and opportunities for enhanced quality of care. Ochsner Journal, 19(4), 357–368. 10.31486/toj.18.0103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkin I, Ang D, Steinhart J, Chao M, Patterson M, Sah S, Wu T, Schoenbaum M, Hutchins D, Brennan T, & Loewenstein G (2017). Association between academic medical center pharmaceutical detailing policies and physician prescribing. JAMA, 317(17), 1785–1795. 10.1001/jama.2017.4039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindly OJ, Eaves MC, Xu Y, Tarazi CL, Rao SR, & Kuhlthau KA (2022). Therapy use for U.S. school-aged children with developmental disabilities: State variation and determinants. Disability and Health Journal, 15(1), 101198. 10.1016/j.dhjo.2021.101198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBain RK, Kofner A, Stein BD, Cantor JH, Vogt WB, & Yu H (2019). Growth and distribution of child psychiatrists in the United States: 2007–2016. Pediatrics, 144(6). 10.1542/peds.2019-1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald DC, & Jalbert SK (2013). Geographic variation and disparity in stimulant treatment of adults and children in the United States in 2008. Psychiatric Services, 64(11), 1079–1086. 10.1176/appi.ps.004442012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrill MS (2018). Special education financing and ADHD medications: A bitter pill to swallow. Journal of Policy Analysis and Management, 37(2), 384–402. 10.1002/pam.22055 [DOI] [PubMed] [Google Scholar]
- Parker JD, Talih M, Malec DJ, Beresovsky V, Carroll M, Joe Fred Gonzalez J, Hamilton BE, Ingram DD, Kochanek K, McCarty F, Moriarity C, Shimizu I, Strashny A, & Ward BW (2017). National Center for Health Statistics data presentation standards for proportions. Vital and Health Statistics, Series 2. [PubMed] [Google Scholar]
- Piper BJ, Ogden CL, Simoyan OM, Chung DY, Caggiano JF, Nichols SD, & McCall KL (2018). Trends in use of prescription stimulants in the United States and Territories, 2006 to 2016. PLoS ONE, 13(11), e0206100. 10.1371/journal.pone.0206100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Protecting Youth Mental Health: The U.S. Surgeon General’s Advisory. (2021). https://www.hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf [PubMed]
- Public Health Informatics Institute. (2021). Using data to improve child and adolescent mental health (CAMH): The opening playbook. Retrieved November 4, 2021 from https://phii.org/course/using-data-to-improve-child-and-adolescent-mental-health-camh-the-opening-playbook/ [Google Scholar]
- Scally CP, Pettit KLS, & Arena O (2017). 500 Cities Project: Local data for better health. Urban Institute. https://www.urban.org/sites/default/files/publication/90376/500-cities-project_1.pdf [Google Scholar]
- Schor EL, & Johnson K (2021). Child health inequities among state Medicaid programs. JAMA Pediatrics. 10.1001/jamapediatrics.2021.1082 [DOI] [PubMed] [Google Scholar]
- Subcommittee on Attention-Deficit/Hyperactivity Disorder, Steering Committee on Quality Improvement and Management, Wolraich M, Brown L, Brown RT, DuPaul G, Earls M, Feldman HM, Ganiats TG, Kaplanek B, Meyer B, Perrin J, Pierce K, Reiff M, Stein MT, & Visser S (2011). ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics, 128(5), 1007–1022. 10.1542/peds.2011-2654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tseregounis IE, Stewart SL, Crawford A, Marshall BDL, Cerdá M, Shev AB, & Henry SG (2020). Age- and sex-specific increases in stimulant prescribing rates—California, 2008–2017. Journal of Attention Disorders, 24(2), 205–214. 10.1177/1087054719883008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. (2017). 2016 National Survey of Children’s Health: Nonresponse bias analysis. https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/nonresponse-bias-analysis/NSCH%202016%20Nonresponse%20Bias%20Analysis.pdf
- United States Census Bureau. (2018a). 2016 National Survey of Childrens Health: Methodology report. https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/methodology/2016-NSCH-Methodology-Report.pdf
- United States Census Bureau. (2018b). 2017 National Survey of Children’s Health: Methodology report. https://www.census.gov/content/dam/Census/programs-surveys/nsch/tech-documentation/methodology/2017-NSCH-Methodology-Report.pdf
- United States Census Bureau. (2019). 2018 National Survey of Children’s Health: Methodology report. https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/2018-NSCH-Methodology-Report.pdf
- United States Census Bureau. (2020). 2019 National Survey of Children’s Health: Methodology report. https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/2019-NSCH-Methodology-Report.pdf
- Visser SN, Bitsko RH, Danielson ML, Ghandour RM, Blumberg SJ, Schieve LA, Holbrook JR, Wolraich ML, & Cuffe SP (2015). Treatment of attention deficit/hyperactivity disorder among children with special health care needs. The Journal of Pediatrics, 166(6), 1423–1430.e1422. 10.1016/j.jpeds.2015.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Blumberg SJ, Danielson ML, Bitsko RH, & Kogan MD (2013). State-based and demographic variation in parent-reported medication rates for attention-deficit/hyperactivity disorder, 2007–2008. Preventing Chronic Disease, 10. 10.5888/pcd9.120073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Perou R, & Blumberg SJ (2014). Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry, 53(1), 34–46.e32. 10.1016/j.jaac.2013.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Perou R, & Blumberg SJ (2013). Convergent validity of parent-reported attention-deficit/hyperactivity disorder diagnosis: A cross-study comparison. JAMA Pediatrics, 167(7), 674–675. 10.1001/jamapediatrics.2013.2364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Wolraich ML, Fox MH, Grosse SD, Valle LA, Holbrook JR, Claussen AH, & Peacock G (2016). Vital Signs: National and state-specific patterns of attention deficit/hyperactivity disorder treatment among insured children aged 2–5 years - United States, 2008–2014. MMWR Morb Mortal Wkly Rep, 65(17), 443–450. 10.15585/mmwr.mm6517e1 [DOI] [PubMed] [Google Scholar]
- Whitney DG, & Peterson MD (2019). US national and state-level prevalence of mental health disorders and disparities of mental health care use in children. JAMA Pediatrics. 10.1001/jamapediatrics.2018.5399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, Evans SW, Flinn SK, Froehlich T, Frost J, Holbrook JR, Lehmann CU, Lessin HR, Okechukwu K, Pierce KL, Winner JD, Zurhellen W, & Subcommittee on Children and Adolescents with Attention-Deficit/Hyperactive Disorder. (2019). Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics 144(4), e20192528. 10.1542/peds.2019-2528 [DOI] [PMC free article] [PubMed] [Google Scholar]


