Abstract
Background:
Although rapid response teams have been widely promoted as a strategy to reduce unexpected hospital deaths, most studies of rapid response teams have not adjusted for secular trends in mortality prior to their implementation. We examined whether implementation of a rapid response team was associated with a reduction in hospital mortality after accounting for pre-implementation mortality trends.
Methods:
Among 56 hospitals in Get With The Guidelines® (GWTG) -Resuscitation linked to Medicare, we calculated annual rates of case-mix adjusted mortality for each hospital during 2000–2014. We constructed a hierarchical log-binomial regression model of mortality over time (calendar-year), incorporating terms to capture the effect of rapid response teams, to determine whether implementation of rapid response teams was associated with reduction in hospital mortality that was larger-than-expected based on pre-implementation trends, while adjusting for hospital case-mix index.
Results:
The median annual number of Medicare admissions was 5214 (range: 408–18,398). The median duration of pre-implementation and post-implementation period was 7.6 years (~2.5 million admissions) and 7.2 years (~2.6 million admissions), respectively. Hospital mortality was decreasing by 2.7% annually during the pre-implementation period. Implementation of rapid response teams was not associated with a change in mortality during the initial year (RR for model intercept: 0.98; 95% CI 0.94–1.02; P= 0.30) or in the mortality trend (RR for model slope: 1.01 per-year; 95% CI 0.99–1.02; P=0.30). Among individual hospitals, implementation of a rapid response team was associated with a lower-than-expected mortality at only 4 (7.1%) and higher-than-expected mortality at 2 (3.7%) hospitals.
Conclusion:
Among a large and diverse sample of U.S. hospitals, we did not find implementation of rapid response teams to be associated with reduction in hospital mortality. Studies are needed to understand best practices for rapid response team implementation, to ensure that hospital investment in these teams improves patient outcomes.
Keywords: Rapid response team, hospital mortality, Medicare
Introduction
In response to the “100,000 Lives Campaign” by the Institute of Healthcare Improvement in 2004,1 many hospitals implemented rapid response teams over the past two decades with the goal of preventing unexpected deaths in hospitalized patients. The foundation of rapid response teams was that prompt evaluation and intervention in patients who experience acute clinical deterioration in hospital wards by a team with critical care expertise could theoretically rescue patients, prevent unexpected deaths, and lower overall hospital mortality.2 However, evidence to support the effectiveness of rapid response teams remains uncertain.
To date, there has been only one randomized controlled trial of rapid response teams. The MERIT trial included 125,132 patients at 23 hospitals in Australia and found no difference in a composite endpoint of unexpected death, cardiac arrest or unplanned ICU admission in hospitals randomized to implement a rapid response team.3 However, the overall effect in the trial may have been attenuated because cardiac arrest (‘code blue’) teams at control hospitals started to function as rapid response teams during the study. While a recent meta-analysis found that rapid response teams were associated with lower hospital mortality, in aggregate,4 large heterogeneity was present. Among individual studies, some found that rapid response teams were associated with a decrease in hospital mortality while others did not.5–9 Importantly, these studies had several methodological limitations. First, most positive studies of rapid response teams compared pre-intervention vs. post-intervention outcomes without accounting for secular trends. As in-hospital mortality has steadily declined at U.S. hospitals over the past decade,10 lack of adjustment for pre-intervention mortality trends may have biased their findings in favor of rapid response teams. Second, a vast majority of prior studies of rapid response teams were conducted in single centers with a short follow-up period and may not be broadly generalizable.
To overcome limitations of prior observational studies of rapid response teams, we evaluated the association between implementation of a rapid response team and hospital mortality in a diverse group of 56 hospitals participating in the Get With The Guidelines® (GWTG)-Resuscitation registry, using a hierarchical log-binomial regression model of mortality over time to explicitly account for pre-implementation trends in hospital mortality.
Methods
The authors are unable to make the data, methods used in the analysis, and materials used to conduct the research available to any researcher for purposes of reproducing the results or replicating the procedure.
Study Design, Setting & Data Sources
Our study was conducted using three data sources. The first is GWTG-Resuscitation - a large, prospective, multisite registry of in-hospital cardiac arrest in the United States that is provided by the American Heart Association.10 In 2015, we assisted GWTG-Resuscitation to conduct a hospital survey to obtain information on the year of implementation of a rapid response team at each participating hospital. This data point was used to determine the onset of exposure to a rapid response team at each hospital. The second data source was Center for Medicare and Medicaid (CMS) Part A files which includes hospitalization data on all Medicare beneficiaries including the annual number of deaths and admissions in Medicare patients at each hospital, which was then used to calculate hospital mortality rates among Medicare beneficiaries. The third data source was annual hospital case-mix index files, which represent a global measure of complexity of admitted patients for a hospital during a given year. These data are publicly available on the CMS website and were used to calculate annual risk-adjusted hospital mortality rates to account for differences in patient case-mix within and across hospitals over time. The study is reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.11
Hospital Mortality in Medicare Patients
For this study, we used 2000–2014 Medicare Part A data which includes data on all admissions among Medicare beneficiaries in the U.S. We excluded Medicare patients younger than 65 years, and hospitalizations at skilled nursing or rehabilitation facilities to focus our study on acute care admissions. Next, we calculated each hospital’s annual mortality rate as the total number of in-hospital deaths during a given year divided by the total number of admissions during that year. To account for between-hospital differences in case-mix, hospital mortality rates were risk-adjusted for its annual case-mix index using random effects logistic regression models.12 Thus, we created a hospital-level dataset that included each hospital’s unique CMS identifier, annual number of admissions, annual number of deaths, annual unadjusted mortality rate, and annual case-mix adjusted mortality rate for each year during 2000 to 2014. This dataset encompassed all acute care hospitals in the United States.
Data Linkage
This hospital-level dataset with annual data on hospital mortality was then linked with GWTG-Resuscitation data by their data analytic center at University of Pennsylvania using a master file that includes a crosswalk between hospital identifiers in the CMS data and GWTG-Resuscitation. Upon completion of the data linkage, a de-identified dataset which only included the GWTG-Resuscitation hospital identifier was provided to our study team for analysis to ensure that the authors remained blinded to the identity of the hospitals.
Study Cohort
Among 89 GWTG-Resuscitation hospitals that provided the start date for rapid response team implementation at their site, 18 hospitals had a start date prior to 2002 (n=16), or after 2012 (n=2). Because we had hospital mortality data from 2000–2014, these hospitals were excluded as they lacked a minimum of 2 years of either pre-intervention or post-intervention follow-up to adequately assess the effect of rapid response team implementation. Of the remaining 71 hospitals, 56 (78.9%) hospitals were successfully linked to CMS hospital-level data. The 15 hospitals without successful linkage did not have a CMS hospital identifier or had an inaccurate identifier that did not provide an exact match to Medicare files.
Study Outcomes & Variables
The primary outcome was risk-adjusted hospital mortality following implementation of a rapid response team at a hospital. Hospital mortality rates were expressed as per-100 admissions, calculated for each year during 2000 to 2014, and adjusted for case-mix index. Hospital variables included census region, number of beds, academic status, urban or rural location, and total number of Medicare admissions.
Statistical Analysis
We used summary statistics to describe characteristics of participating hospitals. Next, we evaluated the association of rapid response team implementation with hospital mortality. Most prior studies have performed aggregate comparison of mortality before and after a rapid response team and did not account for secular trends in decreasing hospital mortality from other interventions during that period. To address this limitation, we fit a hierarchical log-binomial regression model of mortality over time, incorporating terms to capture the effect of rapid response teams. The effect of calendar time was modeled using restricted cubic splines to allow for nonlinear trends (knots were positioned at 2009, 2011 and 2012, selected based on Akaike Information Criterion (AIC)). Furthermore, two additional terms were included to capture the “deflecting” effects of rapid response team on the time trend for each hospital, both at the time of initiation (“instantaneous effect”) and a linear effect over time (“slope effect”). All effects were modeled at the hospital level using random effects, from which population average parameters (fixed effects) were obtained, summarizing the average pre-implementation mortality trends and the average per-year effect of the rapid response team on hospital mortality.
Besides estimating an overall association across the 56 hospitals, we also examined whether rapid response team implementation was associated with a reduction in mortality at any individual hospital by examining the slope and intercept individually at each hospital from the hierarchical model above. We conducted a joint statistical test to determine whether each hospital’s post-implementation intercept or slope was significantly different compared to the pre-implementation trend. In this way, we examined how often implementation of a rapid response team was associated with significantly lower or higher than expected hospital mortality based on pre-implementation trends.
The study was reviewed by the Institutional Review Board at Mid America Heart Institute which waived the requirement for informed consent because the study used deidentified data. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
Results
A total of 56 hospitals were included in our study. Hospital characteristics are summarized in Table 1. Study hospitals were distributed across all five U.S. census regions. Nearly a third of hospitals had ≥500 beds (31%), 58% were teaching hospitals, and 91% hospitals were located in an urban area. Over the study period, the median number of hospital admissions each year was 5214 (range: 408–18,398).
Table 1.
Characteristic of Study Hospitals
| Hospital Characteristics, N (%) | N=56 |
|---|---|
| U.S. Census Region | |
| North Mid-Atlantic | 12 (21.4%) |
| South Mid-Atlantic | 7 (12.5%) |
| North Central | 14 (25.0%) |
| South Central | 13 (23.2%) |
| Mountain/Pacific | 10 (17.9%) |
| Number of Beds* | |
| <200 | 9 (16.4%) |
| 200–499 | 29 (52.7%) |
| ≥500 | 17 (30.9%) |
| Number of ICU beds* | |
| 0 | 2 (3.6%) |
| 1–12 | 10 (17.9%) |
| 13–25 | 17 (30.4%) |
| 26–50 | 16 (28.6%) |
| >50 | 8 (14.3%) |
| Academic Status | |
| Major teaching | 18 (32.1%) |
| Minor teaching | 14 (25.0%) |
| Non-teaching | 24 (42.9%) |
| Location | |
| Urban | 51 (91.1%) |
| Rural | 5 (8.9%) |
| Date of RRT implementation | |
| 2003–2006 | 25 (44.6%) |
| 2007–2009 | 15 (26.8%) |
| 2010–2012 | 16 (28.6%) |
| Annual Medicare Discharges, median (range) | 5214 (408–18,398) |
| <5000 | 25 (44.6%) |
| 5000–7500 | 15 (26.8%) |
| 7500–10000 | 9 (16.1%) |
| >10,000 | 7 (12.5%) |
Abbreviations: ICU: intensive care unit; RRT, rapid response team
Data on number of beds was missing at 1 hospital and ICU beds was missing at 3 hospitals
The date of implementation of each hospital’s rapid response team was distributed across the study period, with 25 (44.6%) implemented between 2003–2006, 15 (26.8%) between 2007–2009, and 16 (28.6%) between 2009–2012. The median duration of the pre-implementation period was 7.6 years (range: 3.5–12.0) among the 56 hospitals comprising approximately 2.5 million hospitalizations, and the median duration of the post-implementation period was 7.2 years (range: 3.0–11.5) comprising approximately 2.6 million hospitalizations.
Association of Rapid Response Team Implementation with Hospital Mortality
Before study hospitals implemented their rapid response team, hospital mortality was decreasing by 2.7% per-year (Figure 1). After accounting for secular trends in hospital mortality in hierarchical regression, implementation of a rapid response team was not significantly associated with a change in expected mortality during the initial year of implementation (relative risk [RR] for change in mortality intercept: 0.98, 95% CI: 0.94–1.02, P=0.30, Table 2). There was also no significant association between rapid response team implementation and change in hospital mortality over the post-implementation period (RR per year post-initiation = 1.01, 95% CI: 0.99–1.02, P=0.30, Table 2). The association between rapid response team implementation and mortality slope at each year during the post-implementation period is also summarized in Table 2, which shows that hospital mortality was not lower than expected at any time point. Lastly, the joint statistical test for a global difference in mortality and slope after rapid response team implementation across the 56 hospitals was not significant (P=0.36).
Figure 1. Risk-adjusted mortality by year of implementation.
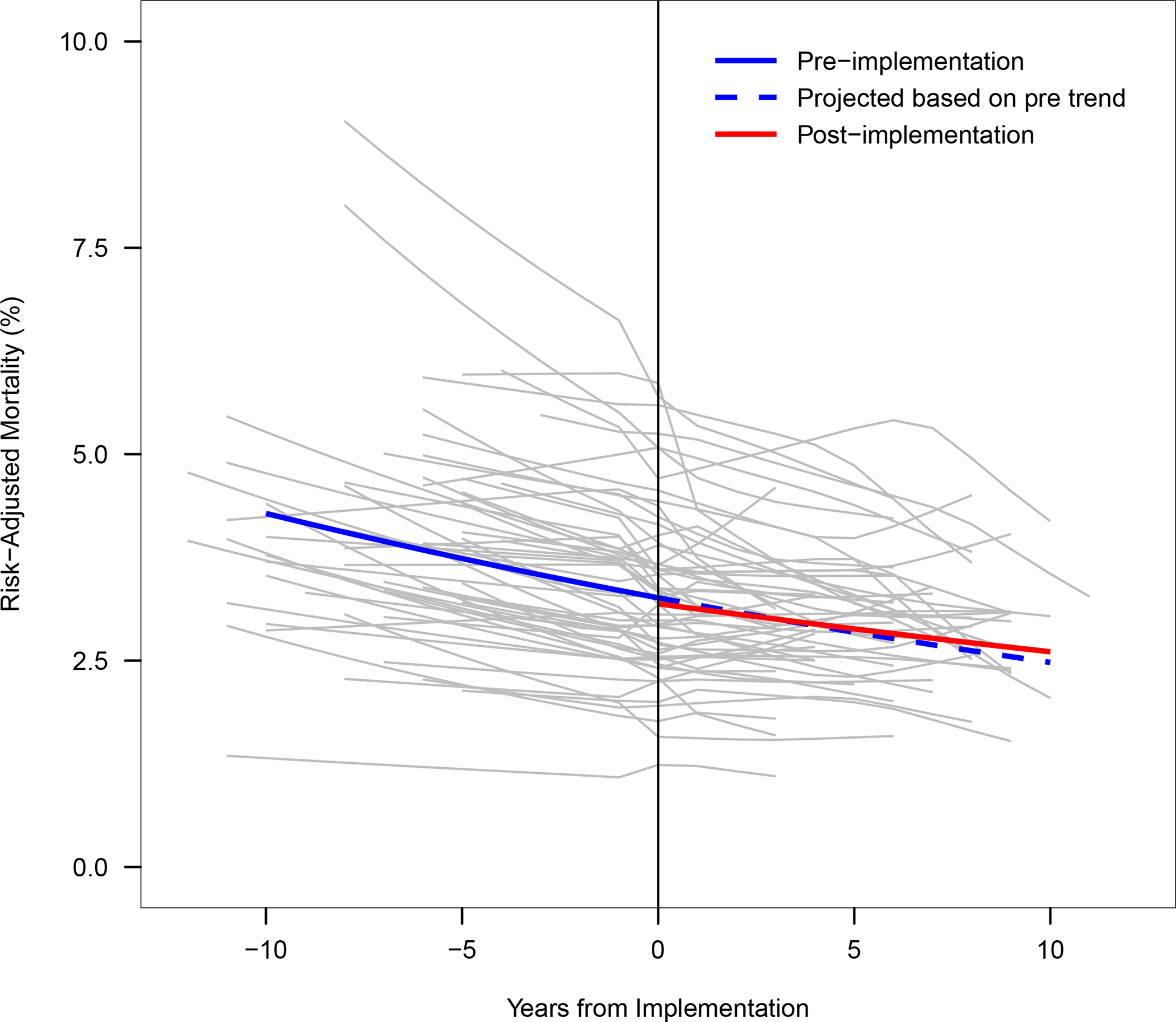
Annual mortality rates are presented by years before, the year of (vertical black line), and years after the implementation of a rapid response team. The lines represent the mean pre-implementation trend in mortality (solid blue line), the projected trend based on pre-implementation data (dashed blue line) and estimated post-implementation trend incorporating the effect of implementation (solid red line).
Table 2. Association of Rapid Response Team Implementation on Hospital Mortality for Overall Cohort of 56 Hospitals.
Estimated derived from hierarchical log-binomial regression model of mortality over time. Implementation of a rapid response team was not associated with lower hospital mortality in the year after implementation (model intercept) or lower than expected mortality during the entire post-implementation period (model slope). Model slope estimates at each post-implementation year are also reported.
| Year After RRT Implementation | RR for Model Slope at each Post-Implementation Year RR (95% CI) | Instantaneous Effect (Model Intercept) RR (95% CI) |
Per-Year Effect (Model Slope) RR (95% CI) |
Global P-value for Overall Effect |
|---|---|---|---|---|
| 0 | 0.98 (0.94, 1.02) | 0.98 (0.94, 1.02) p=0.30 |
1.01 (0.99, 1.02) p=0.30 |
p=0.36 |
| 1 | 0.98 (0.94, 1.03) | |||
| 2 | 0.99 (0.94, 1.04) | |||
| 3 | 1.00 (0.94, 1.06) | |||
| 4 | 1.01 (0.94, 1.08) | |||
| 5 | 1.01 (0.94, 1.10) |
Abbreviations: CI: confidence interval; RR, relative risk; RRT, rapid response team
Figure 2 shows the trends in mortality for each of the 56 study hospitals in relation to their respective year of rapid response team implementation. Consistent with the overall findings, rapid response team implementation was not associated with a change in expected mortality at 50 of the 56 (89.3%) hospitals. At 4 (7.1%) hospitals, implementation of a rapid response team was associated with significantly lower than expected mortality based on pre-implementation trends (panels labelled with a green diamond), whereas 2 (3.6%) hospitals had higher than expected mortality (panels labelled with a red diamond). The model estimates for these 6 hospitals are summarized in Table 3. Of the 4 hospitals with lower-than-expected hospital mortality, all had lower than expected mortality in the year after rapid response team implementation (i.e., a lower model intercept) and 1 also had a sustained year-over-year decrease in hospital mortality than expected (RR of mortality slope: 0.93 [95% CI: 0.89, 0.96]). Of the 2 hospitals with higher-than-expected hospital mortality, both hospitals had a higher-than-expected mortality rate in the year after rapid response team implementation (i.e., a higher model intercept) with no change in the mortality slope over time.
Figure 2. Risk adjusted mortality rates for each hospital by calendar year.
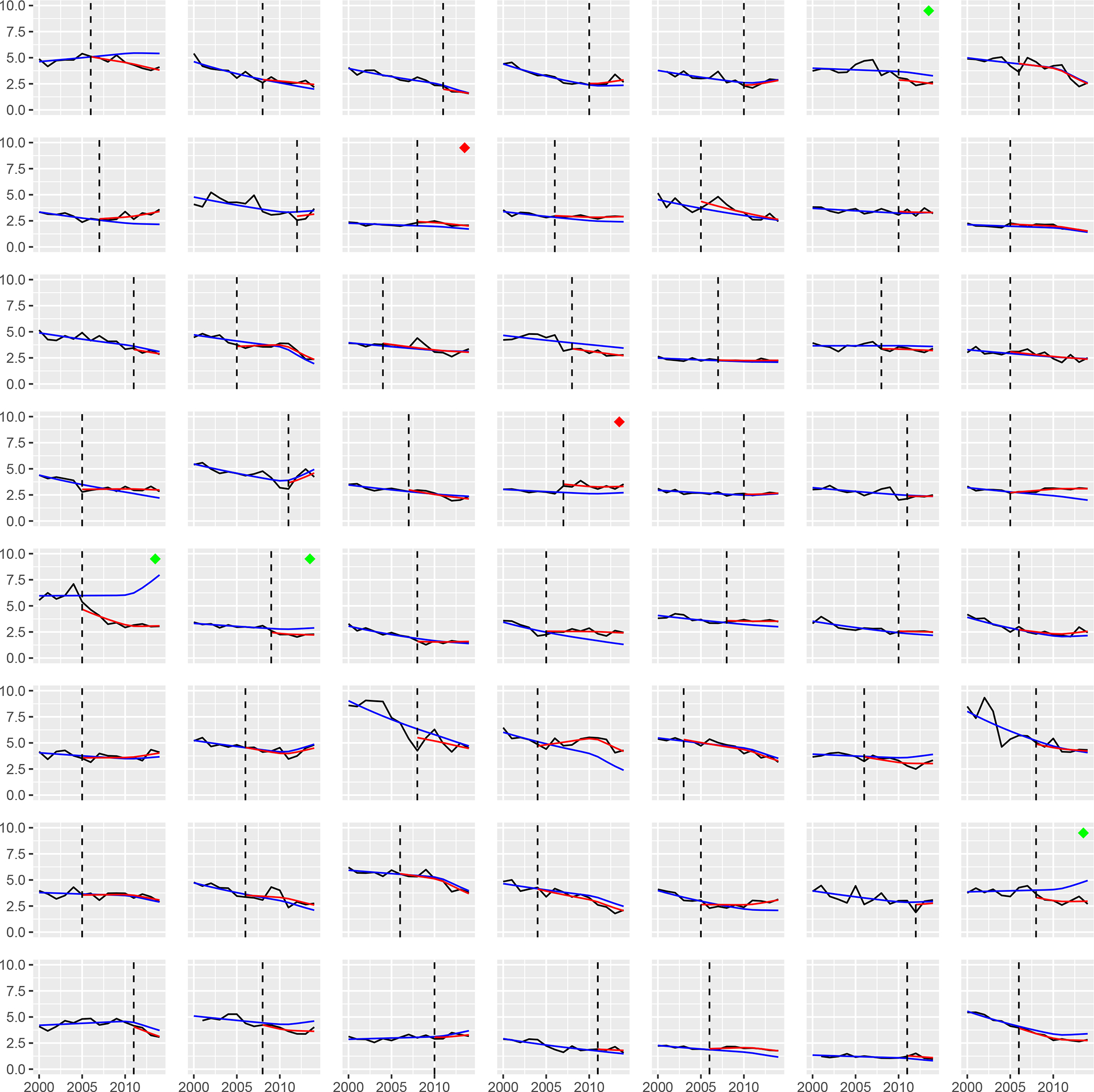
The figure includes 56 panels, each representing a study hospital. The x-axis represents calendar year, and the y-axis represents hospital mortality rate (%). The dashed vertical line represents the year of implementation of rapid response team at that hospital. The solid black line represents actual case mix-adjusted mortality by calendar year. The solid blue line represents the model-predicted mortality trend based on pre-implementation data. The solid red line represents the model-estimated hospital mortality rate after the implementation of the rapid response team, accounting for the effect of implementation on deviation from the projected trend. At 4 hospitals (labelled with a green diamond in the top right corner), implementation of a rapid response team was associated with significantly lower mortality when compared to mortality expected based on pre-implementation trends. At 2 hospitals (labelled with red diamond in the top right corner), implementation of a rapid response team was associated with significantly higher mortality compared to mortality expected based on pre-implementation trends.
Table 3. Model Estimates for Slope and Intercept for Hospitals with a Significant Change in Mortality after Implementation of Rapid Response Team.
Implementation of a rapid response team was associated with lower-than-expected hospital mortality at hospitals 1, 4, 5 and 6 but higher-than-expected hospital mortality at hospitals 2 and 3.
| Site | Instantaneous Effect (Intercept) RR (95% CI) |
Per-Year Effect (Slope) RR (95% CI) |
P-value for Overall Effect |
|---|---|---|---|
| 1 | 0.78 (0.67, 0.91) | 1.00 (0.93, 1.06) | 0.009 |
| 2 | 1.19 (1.05, 1.36) | 1.00 (0.95, 1.05) | 0.02 |
| 3 | 1.29 (1.11, 1.50) | 0.99 (0.95, 1.04) | 0.004 |
| 4 | 0.78 (0.68, 0.90) | 0.93 (0.89, 0.96) | 0.005 |
| 5 | 0.87 (0.78, 0.96) | 0.98 (0.92, 1.03) | 0.04 |
| 6 | 0.83 (0.73, 0.93) | 0.95 (0.90, 1.00) | 0.02 |
Abbreviations: CI: confidence interval; RR: relative risk
Discussion
In this study that included 5.1 million hospitalizations at 56 hospitals over a 15-year period, we found that implementation of a rapid response team was not associated with a significant decrease in hospital mortality overall. Among individual hospitals, a rapid response team was associated with lower-than-expected mortality in only 4 (7.1%) of hospitals. Several of our findings merit further discussion.
Initial studies13, 14 and a highly influential report from the National Academy of Medicine15 highlighted that preventable medical errors account for up to 98,000 hospital deaths each year in the U.S. The disturbingly high frequency of deaths due to medical errors captured the attention of health professionals, policymakers, and the public and led the Institute of Healthcare Improvement in 2004 to recommend rapid response teams as a key patient safety intervention to address preventable deaths.1 Although the rationale for a rapid response team – early intervention in deteriorating patients to prevent unexpected death – makes intuitive sense, evidence supporting their effectiveness in reducing hospital mortality has been mixed, at best, and has largely come from observational studies. 5–9 However, a key limitation of many of these prior studies is that they compared aggregate mortality rates before and after the implementation of a rapid response team and did not account for secular trends in mortality that may have been occurring before their implementation. Given that hospital mortality has decreased during the past two decades,16 such a design likely biased study findings in favor of finding lower hospital mortality rates after implementing a rapid response team. Moreover, small sample size, with limited follow up, and involvement of single center cohorts in a number of these studies raise concerns about chance findings and limit generalizability.17 Additionally, isolated single-center studies risk potential publication bias.
In contrast to many prior studies and meta-analyses, we found no association between implementation of a rapid response team and hospital mortality. Importantly, we addressed key limitations of prior studies in several ways. With linkage of GWTG-Resuscitation with Medicare files, we were able to include 56 hospitals with a total of 5.1 million admissions over a median follow up period of over 7 years, which makes this the largest study to evaluate rapid response teams, to date. For context, the most recent meta-analysis of rapid response teams included data from 29 different studies that collectively represented a total of 2.1 million admissions at 58 hospitals. Importantly, we found that hospital mortality was already decreasing by a relative 2.7% per-year, on average, during the pre-implementation period, highlighting the importance of adjusting for secular trends in obtaining an unbiased estimate of the rapid response team effect on hospital mortality. Our findings are consistent with a recent study of 12 pediatric hospitals that also found no association between implementation of a rapid response team and lower hospital mortality among children after adjusting for secular trends in mortality.18 Moreover, our study avoids possible publication bias in prior studies involving one or a few centers, as the 56 hospitals in this study were an unselected group of hospitals in GWTG-Resuscitation and were included regardless of the effect size of rapid response teams on hospital mortality.
Collectively, our findings suggest that rapid response teams as currently implemented have not resulted in lower hospital mortality. However, it is important to emphasize that unlike biological interventions (e.g., a medication), a rapid response team is a complex intervention comprised of a diverse group of professionals (e.g., nurses, hospitalists, intensivists, and respiratory therapists) and their success depends on a multitude of hospital processes, an effective champion of the team, and institutional leadership, culture, and environment as demonstrated in a recent qualitative study.19 Therefore, while our findings do not show a benefit of rapid response teams in aggregate, it is possible that rapid response teams at some hospitals have been more successful in achieving their goal of lowering hospital mortality as compared with teams at other hospitals. Indeed, we identified 6 (10.2%) hospitals where the rapid response team was associated with a significant change in mortality, and 4 hospitals with lower-than-expected mortality after implementation of their rapid response team, suggesting some heterogeneity of treatment effect. Unfortunately, we lacked detailed information regarding specific hospital protocols and processes of care of each hospital’s rapid response team to further explore how hospital practices and team implementation differed across sites. Given that hospitals devote considerable resources and personnel towards rapid response teams, our findings highlight an urgent need to identify best practices for rapid response teams so that hospitals’ investment in their operation translates into patient benefit.
Prior studies have also examined cardiac arrest incidence on hospital wards as another outcome to evaluate effectiveness of rapid response teams. However, that was not feasible in the current study because Medicare files do not stratify number of hospital admissions by location (ward or intensive care unit). Moreover, other intangible, but important benefits of rapid response teams such as improved staff morale and teamwork, reduced nursing workload, support of bedside nurses due to ready availability of experts who can promptly escalate care of patients in crisis, were not assessed in the current study.20–22
Our study findings should be interpreted considering the following limitations. First, information on date of rapid response team implementation was obtained using a survey of GWTG-Resuscitation hospitals which may have been subject to recall bias. However, the survey was completed by individuals knowledgeable about resuscitation programs at each hospital, typically the Code Blue committee director. Moreover, if there the year of implementation was in error by one or two years in some hospitals, our findings would have been unchanged, given our year-by-year examination of the rapid response team effect on hospital mortality in Table 2. Second, we examined mortality in Medicare beneficiaries; thus, our findings may not be generalizable to hospital-wide mortality. However, there is no reason to believe that hospital processes and mortality outcomes for a rapid response team at a given hospital would differ for Medicare and non-Medicare beneficiaries. Third, a key assumption in evaluating the association between rapid response teams and lower hospital mortality was that pre-implementation trends in mortality would be sustained after the implementation of a rapid response team. Although this assumption is untestable, it is mitigated by the fact that hospitals in our study implemented their rapid response team during different years between 2003 to 2012 so that secular trends in mortality would be largely offset by varying year for team implementation. Fourth, due to lack of data on number of admissions by hospital location, we were unable to evaluate the incidence of cardiac arrest outside the intensive care unit as a potential outcome. However, the latter outcome may be biased if a substantial number of patients arrest soon after transfer to an intensive care unit by a rapid response team.17 Therefore, overall hospital mortality, which comprises all inpatient deaths is less prone to such bias in assessment of rapid response team effectiveness.
In conclusion, we found that the implementation of a rapid response team was not associated with lower hospital mortality. Given that most U.S. hospitals devote considerable resources towards their operation, further studies are needed to understand best practices in rapid response team composition, design, and implementation.
Supplementary Material
What is known
Although rapid response teams have been promoted widely across U.S. hospitals, evidence to support their effectiveness in reducing hospital mortality remains limited.
What this study adds
Using a hierarchical log-binomial regression model of mortality over time (calendar-year) that adjusted for secular trends, we found that implementation of a rapid response team was not associated with a reduction in hospital mortality among a diverse group of 56 hospitals
Future studies are needed to identify best practices of rapid response teams to ensure that hospital investment in these teams improves patients’ survival outcomes. “
Acknowledgment and Authorship:
Dr. Girotra and Dr. Chan had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Girotra also attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Study Concept and design: Girotra, Peberdy, Chan
Acquisition of Data: Girotra, Vaughan-Sarrazin, Chan
Statistical Analysis: Jones, Vaughan-Sarrazin
Analysis and interpretation of data: All Authors
Drafting of the manuscript: Girotra
Critical revision of the manuscript for important intellectual content: All Authors
Study Supervision: Girotra, Chan
Funding:
Dr. Girotra (R56HL158803–01 & R01HL160734–01) and Dr. Chan (R01HL160734–01) receive funding support from the National Institutes of Health.
Abbreviations:
- AIC
Akaike Information Criterion
- CMS
Center for Medicare and Medicaid
- GWTG
Get With The Guidelines
- ICU
Intensive Care Unit
- RR
Relative Risk
- RRT
Rapid Response Team
Appendix:
Author By-line: Besides the study authors, Saket Girotra MD, SM; Mary Ann Peberdy MD; and Paul Chan MD, MSc, Adult Research Task Force members include Anne Grossestreuer PhD; Ari Moskowitz MD; Dana Edelson MD MS; Joseph Ornato MD; Matthew Churpek MD MPH PhD; Michael Kurz MD MS-HES; Monique Anderson Starks MD MHS; Sarah Perman MD MSCE; Zachary Goldberger MD MS
Footnotes
Conflicts of Interest
None
Disclosures:
Dr. Girotra and Dr. Chan have received funding support from the American Heart Association, which currently funds the GWTG-Resuscitation registry. These contents are solely the responsibility of the authors and do not necessarily reflect the views of the American Heart Association, or the Department of Veterans Affairs. None of the other authors have anything to disclose.
REFERENCES
- 1.Berwick DM, Calkins DR, McCannon CJ and Hackbarth AD. The 100,000 lives campaign: setting a goal and a deadline for improving health care quality. JAMA : the journal of the American Medical Association. 2006;295:324–7. [DOI] [PubMed] [Google Scholar]
- 2.Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, Auerbach A, Chen WJ, Duncan K, Kenward G, Bell M, Buist M, Chen J, Bion J, Kirby A, Lighthall G, Ovreveit J, Braithwaite RS, Gosbee J, Milbrandt E, Peberdy M, Savitz L, Young L, Harvey M and Galhotra S. Findings of the first consensus conference on medical emergency teams. Critical care medicine. 2006;34:2463–78. [DOI] [PubMed] [Google Scholar]
- 3.Hillman K, Chen J, Cretikos M, Bellomo R, Brown D, Doig G, Finfer S and Flabouris A. Introduction of the medical emergency team (MET) system: a cluster-randomised controlled trial. Lancet. 2005;365:2091–7. [DOI] [PubMed] [Google Scholar]
- 4.Maharaj R, Raffaele I and Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015;19:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart GK, Opdam H, Silvester W, Doolan L and Gutteridge G. A prospective before-and-after trial of a medical emergency team. The Medical journal of Australia. 2003;179:283–7. [DOI] [PubMed] [Google Scholar]
- 6.Chan PS, Khalid A, Longmore LS, Berg RA, Kosiborod M and Spertus JA. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA : the journal of the American Medical Association. 2008;300:2506–13. [DOI] [PubMed] [Google Scholar]
- 7.Jones D, Opdam H, Egi M, Goldsmith D, Bates S, Gutteridge G, Kattula A and Bellomo R. Long-term effect of a Medical Emergency Team on mortality in a teaching hospital. Resuscitation. 2007;74:235–41. [DOI] [PubMed] [Google Scholar]
- 8.Santamaria J, Tobin A and Holmes J. Changing cardiac arrest and hospital mortality rates through a medical emergency team takes time and constant review. Critical care medicine. 2010;38:445–50. [DOI] [PubMed] [Google Scholar]
- 9.Winters BD, Weaver SJ, Pfoh ER, Yang T, Pham JC and Dy SM. Rapid-response systems as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158:417–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G and Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58 (3):297–308. [DOI] [PubMed] [Google Scholar]
- 11.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP and Initiative S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen LM, Nallamothu BK, Spertus JA, Li Y and Chan PS. Association Between a Hospital’s Rate of Cardiac Arrest Incidence and Cardiac Arrest Survival. JAMA Intern Med. 2013;173:1186–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brennan TA, Leape LL, Laird NM, Hebert L, Localio AR, Lawthers AG, Newhouse JP, Weiler PC and Hiatt HH. Incidence of Adverse Events and Negligence in Hospitalized Patients. New England Journal of Medicine. 1991;324:370–376. [DOI] [PubMed] [Google Scholar]
- 14.Gawande AA, Thomas EJ, Zinner MJ and Brennan TA. The incidence and nature of surgical adverse events in Colorado and Utah in 1992. Surgery. 1999;126(1):66–75. [DOI] [PubMed] [Google Scholar]
- 15.Kohn LT, Corrigan JM and Donaldson MS. To Err is Human: Building a Safer Health System. Committee on Quality of Health Care in America, Institute of Medicine, National Academies Press, Washington DC. 1999. [PubMed] [Google Scholar]
- 16.Hall MJ, Levant S and DeFrances CJ. Trends in inpatient hospital deaths: National Hospital Discharge Survey, 2000–2010. NCHS Data Brief. 2013;Mar(118):1–8. [PubMed] [Google Scholar]
- 17.Chan PS, Jain R, Nallmothu BK, Berg RA and Sasson C. Rapid Response Teams: A Systematic Review and Meta-analysis. Arch Intern Med. 2010;170:18–26. [DOI] [PubMed] [Google Scholar]
- 18.Kutty S, Jones PG, Karels Q, Joseph N, Spertus JA and Chan PS. Association of Pediatric Medical Emergency Teams With Hospital Mortality. Circulation. 2018;137:38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dukes K, Bunch JL, Chan PS, Guetterman TC, Lehrich JL, Trumpower B, Harrod M, Krein SL, Kellenberg JE, Reisinger HS, Kronick SL, Iwashyna TJ, Nallamothu BK and Girotra S. Assessment of Rapid Response Teams at Top-Performing Hospitals for In-Hospital Cardiac Arrest. JAMA Intern Med. 2019;179:1398–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Benin AL, Borgstrom CP, Jenq GY, Roumanis SA and Horwitz LI. Republished: Defining impact of a rapid response team: qualitative study with nurses, physicians and hospital administrators. Postgrad Med J. 2012;88:575–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Astroth KS, Woith WM, Stapleton SJ, Degitz RJ and Jenkins SH. Qualitative exploration of nurses’ decisions to activate rapid response teams. J Clin Nurs. 2013;22:2876–82. [DOI] [PubMed] [Google Scholar]
- 22.Stolldorf DP. Original Research: The Benefits of Rapid Response Teams: Exploring Perceptions of Nurse Leaders, Team Members, and End Users. Am J Nurs. 2016;116:38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


