African relevance
-
•
Conducted in a regional emergency centre in the Western Cape, South Africa.
-
•
Provides an insight into the prevalence of the palliative care population in an African context, specifically with the high burden of HIV and TB.
-
•
Informs about unique challenges that are faced by emergency centers in the sub Saharan region.
Keywords: Emergency centers, Palliative care, Attendance, Reasons, Diagnoses, Disposition
Abstract
Background
: Globally, emergency centers (ECs) face increasing patients with palliative care (PC) needs. This is also true for South Africa. Factors include an increasingly older population, rising rates of non-communicable and infectious diseases. A paucity of data exists on local rates and reasons for patients with life limiting conditions presenting to ECs. PC and emergency medicine are established specialties, but little is known how they interface in clinical practice. This study describes the contribution of patients with life limiting conditions to the case load of an EC in a regional hospital in the Western Cape.
Methods
: This was a prospective, descriptive study. All patients entering the EC over 3 months were assessed using a validated PC identification tool, developed for low-and-middle-income countries. All patients entering the EC were captured in an electronic database. Those identified to have life limiting illnesses and potential PC needs received a secondary ICD-10 code. These files were extracted and statistically analysed. Variables included diagnosis, demographics, reason for visit, and disposition.
Results
: A total of 426 patient visits (4.24%) were identified. Cancer (25.8%), neurological (19.7%) and HIV (17.4%) were the most frequent diagnoses. Patients with HIV and TB were significantly younger. Physical symptoms were the most common reasons for attendance (87%), followed by social (11%) and system issues (10%). Most patients were discharged home (55%), 26% were admitted, and 13% died in the EC.
Discussion
: ECs in Africa are under-resourced and uncomfortable places for patients with life limiting illnesses. System-related visits could be avoidable, as most were due to patients running out of medication or requiring procedures such as urinary catheter changes, which could be done at the local clinic. Some attended EC due to social reasons, usually due to caregivers feeling overwhelmed. Patients requiring PC make up a significant percentage of EC visits. Optimizing health systems and community home-based care could alleviate EC pressures and improve the illness experience of patients with life limiting conditions.
Background
According to the World Health Organization (WHO), palliative care (PC) aims to improve the quality of life for patients and their relatives that are facing a life limiting illness [1]. Globally, emergency centers (ECs) are facing an increasing population of patients requiring palliative and end of life care [2]. With an increasing world population and increasing life expectancy, the WHO has recognized the lack of PC resources, particularly in developing countries [3].According to the WHO, 78% of patients requiring PC live in low- and middle income countries and that globally only 14% of patients that require PC receive it [1]. In South Africa, rising rates of non-communicable diseases such as hypertension, diabetes, malignancies and infectious diseases like human immunodeficiency virus (HIV) and Tuberculosis (TB) [4] are contributing to the amount of patients that require PC. These diseases are known to cause a prolonged illness experience, unlike for example physical trauma or accidents. A high percentage of these patient will develop life limiting illnesses and have potential PC needs in future. Consequently, ECs are dealing with disproportionally more and more patients. Multiple EC visits by patients at the end of life are considered a marker of poor quality palliative care, resulting in significant distress for both the patient and their care givers [5,6]. Most visits are due to physical symptoms of pain and dyspnea, some of which are potentially avoidable [5,7]. A large proportion of EC visits occur after-hours when they are typically less staffed [6], placing additional stress on the EC team. Numerous perceived or real barriers to palliative care in ECs have been described. It is an uncomfortable environment for dying patients, who are triaged as lower priority than acute care, doctors lacking confidence in palliative care skills, time constraints, discouragement of repeat consultations, and lack of relationship building with patients and families are some of these barriers [7]
Instituting inpatient and outpatient PC services has been shown to decrease both admission rates and length of hospital stay, resulting in significant cost savings [8]. While there is a growing need for PC services in South Africa [9], without data to inform health systems of the actual case load in the EC, planning interventions to improve service delivery remains a challenge. There is a paucity of data both internationally and locally on patient numbers [10], with one international study having found that up to 13% of patients presenting to an EC have palliative symptoms [11]. Apart from work from Nigeria which studied the attendance of patients with advanced chronic kidney disease in an EC [12], there is very little data available on local rates and reasons for patients with potential PC needs visiting ECs.
The aim of this study was to address this knowledge gap and to describe the contribution of patients with life limiting illness that would benefit from PC to the case load of an emergency centre in a large regional hospital in the Western Cape. The objectives included: To estimate the prevalence of patients with potential palliative care needs attending the EC; to describe the patient demographics and diagnoses of these patients; to understand the reasons for EC attendance; and to describe their disposition from the EC.
Methods
Design and setting
This was a single centre prospective, descriptive study. This method was chosen as the authors are familiar with the setting, wanted to obtain baseline data, and wanted to limit bias by doing a prospective (as opposed to a retrospective) study. The study was done at George hospital EC in the Garden Route district of SA. This is a 284-bed regional referral hospital with general specialties. The EC has a dedicated team of 14 doctors and 20 nurses with a specialist emergency medicine physician, and manages 140 patients per 24-h period. The hospital is a referral centre for 10 outlying district hospitals, and is the primary, secondary and tertiary health facility, especially after-hours, for the George sub-district, serving a local population of 200,000 people, together with 10 primary health care clinics. The EC caters for all medical, surgical, psychiatric, paediatric, gynaecologial and forensic emergencies. There is no district hospital or after-hours state health care in the George sub-district. There is a private hospital and a non-governmental organization (NGO) step-down care facility in George. Some home based care (HBC) exists through three NGOs, which provide palliative care services in the community.
Study population, sampling and data collection
All patients entering the EC during the three-month study period from November 2020 to January 2021 were assessed for inclusion into the study by a shift doctor using the shortened Palliative Care Identification tool [13]. This tool was developed and validated for low and middle income countries like South Africa, that have a high burden of HIV and TB. It is based on the GSF-PIG (Gold Standards Framework Prognostic Indicator Guidance) identification tool and aids clinicians to identify patients that have a high risk for death in the next twelve months and a potential PC need. The shortened PC identification tool asks the question, “would you be surprised if the patient were to die in the next year?” and includes seven criteria [13]. (see Appendix A). This tool was chosen as it has been validated for the South African context, has a simple checklist format which makes it easy to use for non-PC trained practitioners and includes both non-communicable and communicable diseases such as HIV and TB. Patients were included if they were over the age of 18 years and met the criteria of the screening tool.
As part of routine practice in the EC, all patients attending the EC are entered into an online electronic EC patient information system called “Hospital and Emergency Centre Tracking Information System” (HECTIS). All patients receive a primary ICD-10 diagnosis and secondary diagnosis (including palliative care) where appropriate, prior to their dispositon.
The Division of Epidemiology and Biostatistics in the Faculty of Health Sciences at Stellenbosch University helped to calculate the sample size. A minimum sample size of 270 cases would give the study 80% power to detect a difference in proportions of more than 30% between two subgroups of equal size, using a significance level of 5%.
In order to sensitise the EC team to PC, training by a doctor experienced in PC was provided to all the doctors working in the unit. This was during weekly group discussions and included simulations using the shortened PC tool. Training was done prior to study commencement and was ongoing for the duration of the study. Study reminders were done twice daily during handover ward rounds to the EC team on shift, to reduce the number of potentially missed eligible patients. Doctors were asked to code any patient that they saw who met the shortened PC criteria and to document in their notes the diagnosis (which made them meet the criteria) and why the patient had come to the unit. This was for both patients with a known diagnosis and those that had been diagnosed during the consultation or admission.
Once patients were identified, their electronic patient records, as captured on the Enterprise Content Management (ECM) system, were reviewed to validate that they met the Shortened PC tool criteria. The following variables were extracted from their records: 1. Diagnosis, categorized as either one of the following: Cancer, Cardiovascular, HIV, Renal, Respiratory, Neurological, Dementia/frail or other (Peripheral vascular disease, end stage liver disease etc.); 2. Demographics (age, gender); 3. Reason for EC visit, categorized as: physical symptoms (particularly pain/dyspnoea), psychological distress, health system (for example running out of medication/access to medications) and social/family reasons; 4. Disposition, categorized as: Discharge home, admit to a ward, died in EC, or refer to a care facility.
Patients were excluded if they did not meet the shortened PC tool criteria. This included patients who had, on folder review, been found to be inappropriately coded during the initial consultation; age less than 18 years and patients coded as requiring PC but with insufficient medical records/information. A waiver of consent was requested and granted from the Higher Research Ethics Committee of the University of Stellenbosch.
The study was done over a three month period, to compensate for seasonal variation. During the study period, South Africa experienced a wave of SARS-CoV-2 infections. In order to maintain external validity, diagnosis of SARS-CoV-2 was not included as a criteria for identifying patients with a potential PC need.
Analysis
The principal investigator accessed the HECTIS database and filtered out all patient records during the study period with a palliative care ICD-10 code. Data were extracted from HECTIS and captured in an Excel spreadsheet and checked for errors and ommisions. Data were analysed with the help of the Statistical Package for the Social Sciences (SPSS) software, version 26©.
Means and standard deviations were used to describe continuous variables that are normally distributed (e.g. age) and medians and interquartile ranges were used to describe continuous data that are not normally distributed. Categorical data were analysed using frequencies and percentages.
For comparison between variables the following general analysis guidelines were followed: for comparison of two continuous variables, Pearson's correlation coefficient was used if data was normally distributed and Spearman's rank order of correlation if data were non-normally distributed. Comparing two categorized variables was performed by means of Pearson's Chi-squared test with Fischer's exact test if small expected frequencies were observed. In comparing a continuous variable with a binary variable, a T- test was used if data were normally distributed and a Mann-Whitney U test if data were non-normally distributed. In comparing a continuous variable with a categorical variable an ANOVA was used if data were normally distributed and a Kruskal-Wallis test if data were non-normally distributed. Post hoc test with Bonferroni adjusted p-values was performed when significant results were obtained. A p-value of <0.05 represented statistical significance.
To ensure internal validity of the sampling, 100 patient files from the total EC visits for November 2020 were randomly selected and reviewed for the relevant visit to EC to determine if they met criteria for requiring PC and were missed. Of the 100 visits, six were correctly identified as requiring PC and were coded as such, forming part of our data. The remaining folders did not meet criteria and were thus correctly omitted from the data set. This allows us to assume a 90% accuracy in the sampling.
Ethics approval
Ethics approval was obtained from the Higher Research Ethics Committee of the University of Stellenbosch (Ref. No. N20/08/081), as well as the Western Cape Department of Health (Ref. No. WC_202109_030) and the management and Ethics committee of George Hospital.
Results
A total of 458 patient visits were identified as having potential palliative care needs over the three-month study period on HECTIS. Following the folder review, to ensure that identified patients met the study criteria, 32 patient visits were excluded (under 18 years old (one) and not meeting the shortened PC screening tool criteria (31). This left a total of 426 patient visits which amounted to 4.24% of the total patient visits to the EC (N = 10 049). This was broken down as follows: November 190 of 4101 (4.6%); December 146 of 3374 (4.3%) and January 90 of 2574 (3.5%).
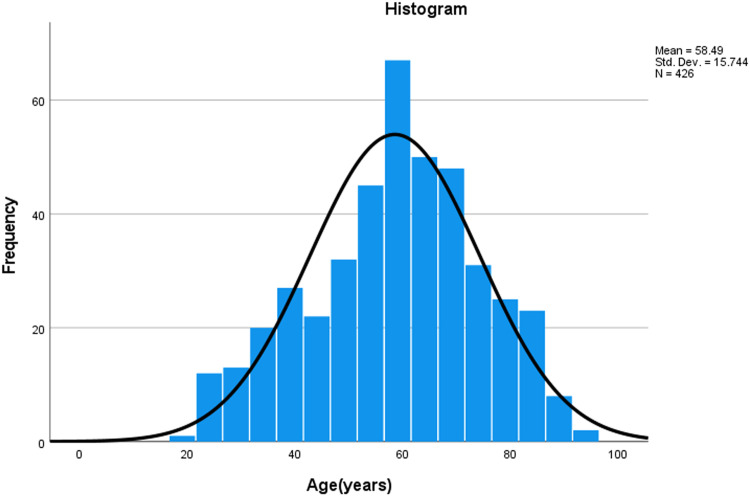
The mean age was 58 years (range 19-96, median 60) with a normal distribution (See Fig. 1). Females were identified more frequently, making up 55.2% of the patient visits. The mean ages of patients with a cardiac, neurological or dementia diagnosis were higher than the average (64, 63 and 72 respectively) while those with HIV or TB diagnosis were younger (40 and 38 respectively)
Fig. 1.
Ages of patients attending the EC who needed palliative care.
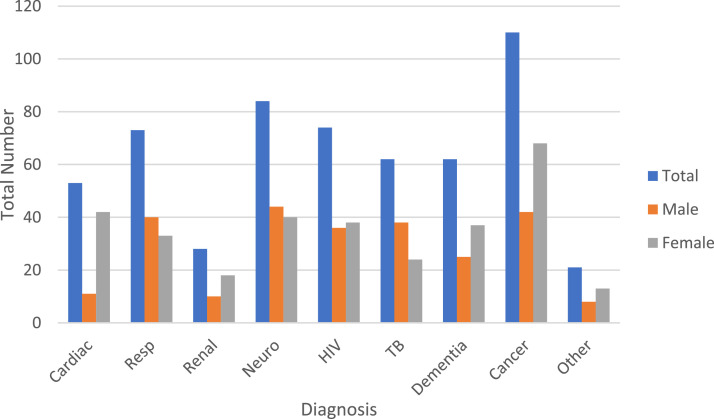
The diagnoses were divided into cardiac, respiratory, renal, neurological, HIV, TB, Dementia/ frailty, cancer and other (including peripheral vascular disease and end-stage liver disease). Several patients had more than one diagnosis meeting the shortened PC tool criteria. The top three diagnoses were cancer (25.8%), neurological disease (19.7%) and HIV (17.4%) which together made up more than half the cases (See Table 1). The gender distribution of patients with a cardiac diagnosis was statistically significant favouring females (p < 0,001) while more males had a TB diagnosis (p = 0,005) (See Fig. 2). There was no significant difference between genders for the other diagnoses.
Table 1.
Diagnoses of patients needing palliative care visiting the EC.
| Frequency | Percentage of total | |
|---|---|---|
| Cardiac | 53 | 12.4 |
| Respiratory | 73 | 17.1 |
| Renal | 28 | 6.6 |
| Neurological | 84 | 19.7 |
| HIV | 74 | 17.4 |
| TB | 62 | 14.6 |
| Dementia/ frail | 62 | 14.6 |
| Cancer | 110 | 25.8 |
| Other (e.g. peripheral vascular disease, end stage liver disease) | 21 | 4.9 |
Fig. 2.
Diagnosis according to gender.
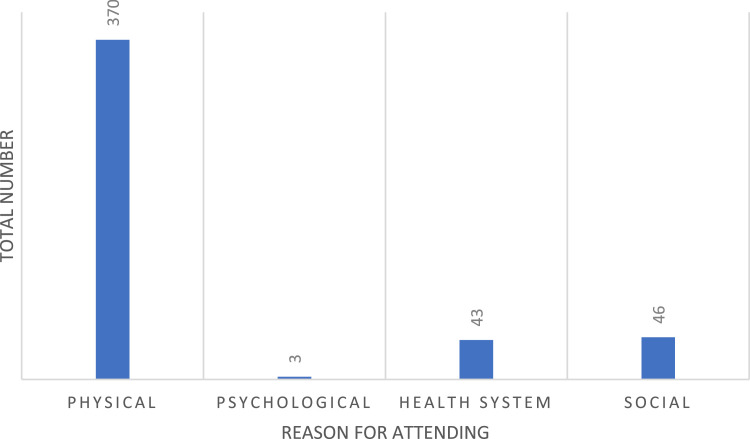
In terms of understanding the reasons for EC attendance of patients needing PC, physical symptoms were the most common (n = 370 (87%)), of which pain and dyspnea were most frequently reported, followed by social (46 (11%)) and health systems (43 (10%)) reasons (See Fig. 3). Some patients had more than one reason for attending the EC. Most of the patients with social reasons for attending had caregiver fatigue or absent support structures, needing placement. Health system reasons included catheter changes or running out of medication at home.
Fig. 3.
Reasons for EC attendance.
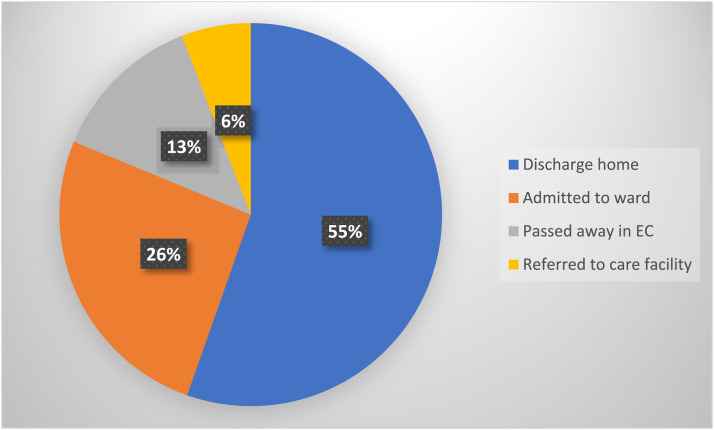
Regarding disposition from the EC, the majority were discharged home (55.0%) while 26.0% of visits resulted in hospital ward admissions. Fifty-five (13.1%) patients demised in the EC and 25 (5.9%) were referred to a step-down care facility (See Fig. 4).
Fig. 4.
Disposition of patients needing palliative care who attended the EC.
Discussion
The main findings of this pilot study were that almost 5% of EC visits were by patients with potential palliative care needs. While this is less than previously reported internationally [11], these patients often have difficult to manage symptoms or have social concerns and contribute to the EC workload and utilization of resources. It also represents an opportunity to initiate PC in this group of patients. The mean age of 58 years was slightly older than a study done in a similar regional centre, which also had a female predominance [13]. PC is most often associated with cancer [14] and while it was the most frequent diagnosis, the combination of the other non-communicable illnesses of cardiac, renal, respiratory and neurological made up more than double the number of cancer patients. Many patients had more than one non-communicable diagnosis, making management complex. Patients with HIV and TB were found in a younger age group than patients with other diseases. At the mean age of 40 and 38 respectively, these patients should usually be part of the workforce and often still have young dependents. Anti-retroviral and anti-tuberculosis treatment is both readily available in the South African public service and very effective, making both HIV and TB treatable diseases and therefore present a good opportunity to decrease their burden on primary and palliative care. .
The main reason for EC attendance of patients needing palliative care was physical, which included pain, shortness of breath, etc. This is not unlike what has been described elsewhere, where pain and dyspnea were the two most common reasons for attendance [7]. Other studies also confirm this, with 23% of EC visits classified as avoidable, with pain (36%) being the most common complaint [5]. Our study found that 10% of EC visits by patients with potential PC needs were system related, such as the need for urinary catheter replacements and running out of medication. This is a function of the local primary health care facilities and therefore could potentially have been avoided. A number of patients attended EC due to social reasons, usually because of the care givers feeling overwhelmed or unable to continue caring for their relatives and requesting respite admissions.
ECs are considered uncomfortable settings by patients with life limiting conditions and their caregivers [15]. It is busy, noisy and overwhelming [16], usually without appropriate space for care and consultation with the dying patient or to talk about end-of-life matters. This is particularly true for ECs in sub-Saharan Africa which are mostly overwhelmed and resource limited, without sufficient staff to offer these patients good PC. Patients with life limiting conditions usually triage as a lower priority to patients with acute life-threatening conditions, and therefore are subjected to long EC waiting times [17]. EC staff find it difficult to care for these patients due to lack of continuity of care, with subsequent inability to build long-lasting relationships, which makes formulating and implementing a palliative care plan difficult [18]. Some EC clinicians might also doubt their abilities and skills for managing patients in need of palliative care. However, many patients with PC needs will still present to the EC as their symptoms cannot be addressed in the community health setting [18] and EC doctors and nurses need skills and experience to continuously shift between emergency care heuristics and palliative care thinking [15]. Failing to do this efficiently and effectively tends to lead to over investigations and inappropriate treatment of patients needing palliative care, without sometimes addressing the real reasons for EC attendance [15].
More than 50% of the patients with palliative care needs who visited the EC were discharged home. This contrasts with previous work which described a 76-94% hospital admission rate [6,7].It has been found that the presence of a community palliative care hospice or HBC services provided an effective strategy to support such patients [19]. However, a systematic review of EC interventions for patients needing PC showed no evidence that EC-based PC affected patient outcomes, except for one study which showed no association with 90-day hospital readmission, but a possible reduction in length of stay if integrated palliative care was introduced early in the EC rather than after hospital admission [18]. Thirteen percent of patients passed away in the EC. This is often considered as a palliative care failure, since most patients would prefer to die at home [18].
Recently, a rural model for palliative care has been described for the Garden Route district in SA. This model emphasizes the integration of hospital care with primary health care (PHC) and home-based care (HBC) as a continuum in a rural setting [20]. For example, when patients with PC needs are visiting the hospital, the attending doctor or nurse ensures a care plan is completed and sent to the PHC services, which in turn connects the patient and family with the HBC services in the community. The idea is to offer a patient-centered quality palliative care service to the patient, while reducing EC visits and consequently reducing emergency services pressures.
Limitations
Limitations were related to both external and internal circumstances. As the study period started (November 2020), George and then South Africa moved into the second wave of infections due to the SARS-CoV-2 virus (COVID-19). The exact impact of this on patient numbers can only be speculated, however it was the feeling of the authors that this resulted in less patient visits to the EC, as the population requiring palliative care are at particular risk to severe SARS-CoV-2 infection and were strongly advised by local and national health departments to avoid hospital contact. This is supported by the total EC visits decreasing over the three-month period from 4101 in November 2020 to 3374 in December 2020 and 2574 in January 2021. While a number of the patients identified as requiring palliative care tested positive for SARS-CoV-2 infection (n = 36, of N = 426), and for some this was the reason for attending EC, SARS-CoV-2 infection was not used as an inclusion criterion.
As potential patients for inclusion were identified by extracting data from the HECTIS database, it was possible that not all patients with PC needs attending the EC were identifiable in HECTIS. This could have biased the results. However, the sample size was large enough to sufficiently address the aim and objectives for this descriptive study. The PC tool used in this study did not make provisions for patients with severe infections (.e. SARS-CoV-2) or trauma, which could have excluded eligible study participants.
Internal limitations were the change-over of EC staff over the study period. Intern doctors rotating through the department for after-hour shifts were trained in the use of the shortened palliative care identification tool [13]. As they only did limited shifts during that time, they would possibly not have been as sensitised in identifying potential patients for the study. In January 2021 there was a change in the community service medical officers in the EC. While the medical officers manage most of the EC patients, the new community service medical officers, who were also trained in the study objectives, might have been less sensitised to identifying patients requiring PC. This could have resulted in identifying lower than actual numbers of patients needing PC attending the EC. The training of the EC team by a doctor experienced in PC to identify appropriate patients for the study could have influenced the care of these patients in the EC. This may have influenced the results, for example disposition, but this was not a major study outcome.
Conclusion
The aim of this study was to describe the contribution of patients with life limiting conditions to the case load of an EC in a large regional hospital in the Western Cape. Almost 5% of EC visits were by patients requiring palliative care, contributing significantly to the EC workload. Pain and dyspnoea were the most common reasons for EC attendance. More than half of patients were discharged home. A functioning community-based palliative care service facilitated this disposition. Further studies exploring the reasons for patients with palliative care needs attending hospital ECs, together with more advocacy for well-functioning home-based palliative care, could alleviate palliative care pressures on ECs and allow for better patient-centred palliative care.
Dissemination of results
The results of this study will be shared with the management team of the George Regional Hospital as well as with the staff involved in the study. This will be done via an informal presentation.
Author contributions
All three authors conceptualised the research and contributed to various drafts of the manuscript. CS collected and analysed the data and drafted the first manuscript. CS, ND and LJ contributed to the final manuscript. CS contributed 50%, LJ contributed 30% and ND contributed 20%. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgements
The authors thank the Emergency Department at George Hospital, specifically the team of dedicated doctors for their continual commitment to and support of the project. Thank you also to Dr F Erasmus for providing PC training and to Ms T. Esterhuizen of the Biostatistics Unit at Stellenbosch University for her support with the data analysis.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.afjem.2022.08.006.
Appendix. Supplementary materials
References
- 1.World Health Organization. Palliative Care 2020, August 5 [04/02/2022]. Available from: https://www.who.int/health-topics/palliative-care.
- 2.Reville B, Foxwell AM. The global state of palliative care-progress and challenges in cancer care. Ann Palliat Med. 2014;3(3):129–138. doi: 10.3978/j.issn.2224-5820.2014.07.03. [DOI] [PubMed] [Google Scholar]
- 3.Sepulveda C, Marlin A, Yoshida T, Ullrich A. Palliative care: the World Health Organization's global perspective. J Pain Symptom Manage. 2002;24(2):91–96. doi: 10.1016/s0885-3924(02)00440-2. [DOI] [PubMed] [Google Scholar]
- 4.M-AD EM, T Mosidi, Nt Zinyakatira, Krish Vallabhjee western cape burden of disease: western cape department of health; 2019 [Available from: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwiL2K2bqe_qAhXkuXEKHXMpBSgQFjAAegQIBBAB&url=https%3A%2F%2Fwww.westerncape.gov.za%2Fassets%2Fdepartments%2Fhealth%2Fburden_of_disease_report_2020.pdf&usg=AOvVaw1z6RXaQ_2pidjl24KO9yW7.
- 5.Delgado-Guay MO, Kim YJ, Shin SH, Chisholm G, Williams J, Allo J, et al. Avoidable and unavoidable visits to the emergency department among patients with advanced cancer receiving outpatient palliative care. J Pain Symptom Manage. 2015;49(3):497–504. doi: 10.1016/j.jpainsymman.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Wallace EM, Cooney MC, Walsh J, Conroy M, Twomey F. Why do palliative care patients present to the emergency department? Avoidable or unavoidable? Am J Hosp Palliat Care. 2013;30(3):253–256. doi: 10.1177/1049909112447285. [DOI] [PubMed] [Google Scholar]
- 7.Verhoef MJ, de Nijs E, Horeweg N, Fogteloo J, Heringhaus C, Jochems A, et al. Palliative care needs of advanced cancer patients in the emergency department at the end of life: an observational cohort study. Support Care Cancer. 2020;28(3):1097–1107. doi: 10.1007/s00520-019-04906-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Desrosiers T, Cupido C, Pitout E, van Niekerk L, Badri M, Gwyther L, et al. A hospital-based palliative care service for patients with advanced organ failure in sub-Saharan Africa reduces admissions and increases home death rates. J Pain Symptom Manage. 2014;47(4):786–792. doi: 10.1016/j.jpainsymman.2013.05.021. [DOI] [PubMed] [Google Scholar]
- 9.Drenth C, Sithole Z, Pudule E, Wust S, GunnClark N, Gwyther L. Palliative care in South Africa. J Pain Symptom Manage. 2018;55(2S) doi: 10.1016/j.jpainsymman.2017.04.024. S170-S7. [DOI] [PubMed] [Google Scholar]
- 10.Wong J, Gott M, Frey R, Jull A. What is the incidence of patients with palliative care needs presenting to the Emergency Department? A critical review. Palliat Med. 2014;28(10):1197–1205. doi: 10.1177/0269216314543318. [DOI] [PubMed] [Google Scholar]
- 11.Kostenberger M, Neuwersch S, Weixler D, Pipam W, Zink M, Likar R. Prevalence of palliative care patients in emergency departments. Wien Klin Wochenschr. 2019;131(17-18):404–409. doi: 10.1007/s00508-019-1530-5. [DOI] [PubMed] [Google Scholar]
- 12.Bello BT, Ojo OE, Oguntunde OF, Adegboye AA. Chronic kidney disease in the emergency centre: a prospective observational study. Afr J Emerg Med. 2018;8(4):134–139. doi: 10.1016/j.afjem.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raubenheimer PJ, Day C, Abdullah F, Manning K, Cupido C, Peter J. The utility of a shortened palliative care screening tool to predict death within 12 months - a prospective observational study in two south African hospitals with a high HIV burden. BMC Palliat Care. 2019;18(1):101. doi: 10.1186/s12904-019-0487-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murray SA, Kendall M, Mitchell G, Moine S, Amblas-Novellas J, Boyd K. Palliative care from diagnosis to death. BMJ. 2017;356:j878. doi: 10.1136/bmj.j878. [DOI] [PubMed] [Google Scholar]
- 15.Lawson BJ, Burge FI, McIntyre P, Field S, Maxwell D. Palliative care patients in the emergency department. J Palliat Care. 2008;24(4):247–255. [PMC free article] [PubMed] [Google Scholar]
- 16.Green E, Ward S, Brierley W, Riley B, Sattar H, Harris T. They shouldn't be coming to the ED, should they?": a descriptive service evaluation of why patients with palliative care needs present to the emergency department. Am J Hosp Palliat Care. 2017;34(10):984–990. doi: 10.1177/1049909116676774. [DOI] [PubMed] [Google Scholar]
- 17.Hjermstad MJ, Kolflaath J, Lokken AO, Hanssen SB, Normann AP, Aass N. Are emergency admissions in palliative cancer care always necessary? Results from a descriptive study. BMJ Open. 2013;3(5) doi: 10.1136/bmjopen-2012-002515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.da Silva Soares D, Nunes CM, Gomes B. Effectiveness of Emergency Department Based Palliative Care for Adults with Advanced Disease: A Systematic Review. J Palliat Med. 2016;19(6):601–609. doi: 10.1089/jpm.2015.0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mahony SO, Blank A, Simpson J, Persaud J, Huvane B, McAllen S, et al. Preliminary report of a palliative care and case management project in an emergency department for chronically ill elderly patients. J Urban Health. 2008;85(3):443–451. doi: 10.1007/s11524-008-9257-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Source: Raubenheimer PJ, Day C, Abdullah F, Manning K, Cupido C, Peter J. The utility of a shortened palliative care screening tool to predict death within 12 months - a prospective observational study in two south African hospitals with a high HIV burden. BMC Palliat Care. 2019;18(1):101. doi: 10.1186/s12904-019-0487-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.