Abstract
Objectives
Mandible is an integral part of masticatory system, and it is expected that it’s fracture will have a significant impact on occlusal forces, range of motion, muscle activity levels, and occlusion. The main objective of this study was to compare the efficacy of 3-dimensional (3D) miniplate and conventional miniplates for fixation of anterior mandibular fractures on the basis of bite force as a main parameter.
Methods
66 patients having isolated anterior mandibular fractures were randomized into two groups equally: Conventional miniplates and 3D miniplates. The bite force at incisor, canine, and molar regions was measured preoperatively and postoperatively at weekly intervals until the sixth week, and the mean bite force as well as changes in mean bite force were compared between two groups.
Results
An increase in bite force was noted at each subsequent follow up in both the groups across all sites. Statistically significant difference was found in mean bite force values between both the groups during mid-follow up period. The difference in changes in the mean bite force too was observed to be statistically significant during the mid to late follow up period.
Interpretation & conclusion
Bite force is a reliable parameter to assess restoration of masticatory efficiency following open reduction and internal fixation (ORIF). 3D miniplates when used in anterior mandibular fractures management are efficient enough to withstand masticatory forces throughout the healing process, providing better stability of fractured segments against torsional forces during immediate post-operative period.
Keywords: Anterior mandibular fractures, Conventional and 3D miniplate, Maximum bite force, ORIF
1. Introduction
Mandibular fracture is the most common (59.2%) of all maxillofacial traumas due to its prominent position in the facial skeleton. Of about 15.1% of reported cases of anterior mandibular fractures, symphysis and parasymphysis fractures account for 2.85% and 12.16% respectively.1 Treatment methods for mandibular fractures span from non-surgical maxillomandibular fixation to surgical usage of various internal fixation systems. Champy's recommendation of 2 conventional miniplates placement in the anterior mandibular region to nullify the compression and tension forces are sometimes found to be insufficient in stabilizing the fractures against bending and twisting forces and further require inter-maxillary fixation (IMF).2,3 In order to enhance miniplates' resistance to torsional forces, 3D plating system having numerous advantages was introduced in 1992.4,5
Mandible being an essential part of the masticatory system, any fracture of it will drastically affects occlusal forces, cosmesis, speech, mandibular range of motion, muscle activity, and occlusion.6 Damage to masticatory muscles or its protective neuromuscular system causes reduction in biting force.7,8 Bite force is an important determinant of chewing function and it is proven that individuals who produce higher forces during mastication may exhibit greater masticatory efficiency. Therefore, maximum biting force could be utilized as a clinical indicator to assess masticatory function that has been restored following mandibular fracture treatment.7 Hence, this study was carried out to compare and evaluate the efficiency of 2 mm 3D titanium miniplate versus 2 mm conventional titanium miniplates for management of anterior mandibular fractures on the basis of bite force measurements.
2. Materials and method
This prospective randomized comparative study was carried out after obtaining written informed consent of all the patients enrolled, in the Department of Oral and Maxillofacial Surgery with prior permission from the institutional ethics committee. 66 patients who had anterior mandibular fractures were allocated randomly into two groups, Group-I (Control) conventional miniplates and Group-II (Study) 3-D miniplate. After recording detailed history x-ray Orthopantomogram (OPG) and/or Computed Tomography (CT) scans were prescribed.
Inclusion criteria were:
-
•
Age range between 18 to 60 years
-
•
Isolated anterior mandibular fractures (interforaminal region)
-
•
Complete set of dentition
Exclusion criteria were:
-
•
Patients with comminuted/infected mandibular fractures
-
•
Associated dentoalveolar/pan-facial fractures
-
•
Patients with fractured, mobile or carious teeth
-
•
Medical comorbidities
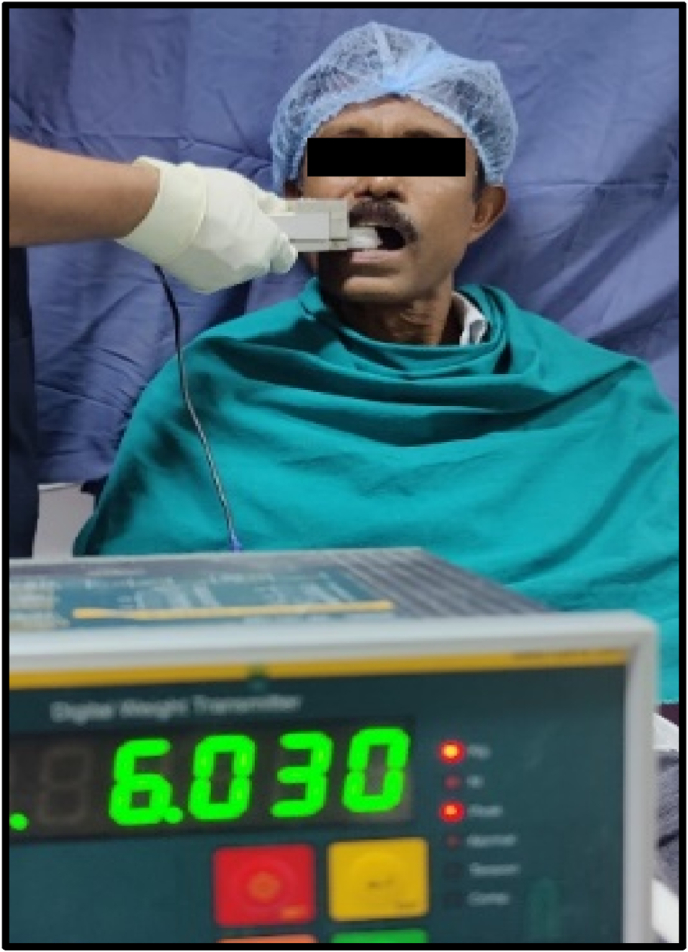
Bite force measurements were recorded preoperatively using gnathodynamometer at three main regions: central incisor, right and left canine, and right and left first molar regions (Fig. 1, Fig. 2). Patients were explained and advised to bite as firmly as they could onto the bite force gauge's pads. To avoid muscular fatigue, the maximum bite force reading on the charge meter display was noted at a time interval of 1 min on each side.
Fig. 1.
Gnathodynamometer.
Fig. 2.
Bite force recording technique.
All patients were operated under general anesthesia by the same surgeon through an intraoral approach. In group-I, two conventional miniplates 2.0 mm 4-hole with gap and in group II, a 3D titanium miniplate was adapted. All plates were fixed using 2 × 8 mm monocortical screws. Subsequent follow-ups were performed every week till the 6th week. Bite force was measured preoperatively and thereafter every week till 6th week postoperatively. Simultaneously, Mouth opening, Duration of surgery, Post-operative Infection, Malunion/Non-union, Hardware failure, Paresthesia, Occlusal status, and Wound dehiscence too were observed.
The data were analyzed and descriptive statistical methods (mean, standard deviation) were used for evaluation of data. Normality assumption was tested using Shapiro-Wilk test and Unpaired t-test was used to compared data.
3. Results
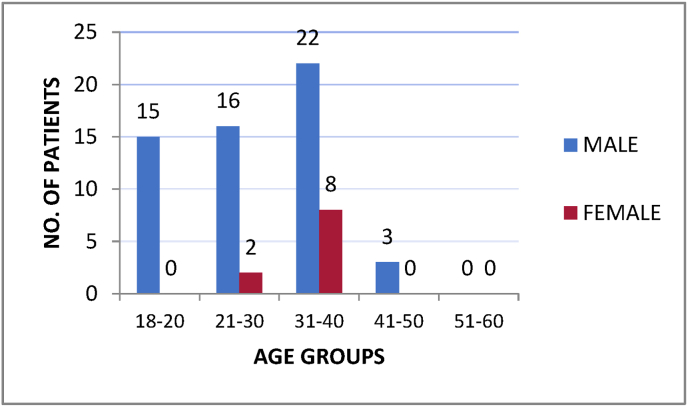
Out of 66 patients enrolled, 56 were male and 10 were female aged 18–60 years with highest number of fractures (45.5%) observed in the third decade of life (Fig. 3). The mean age of patients in the control group was 27.58 ± 7.78 years and that of the study group was 28.55 ± 7.47 years. Fractures of parasymphysis (86%) were observed to be more frequent than that of the symphysis (14%).
Fig. 3.
Age and Gender distribution of study population.
Interincisal measurements were obtained using steel metric ruler preoperatively as well as weekly interval till the 6th week postoperatively. The recorded mean values were found to be lesser preoperatively and during 1st week of follow up whereas gradual progression noted towards the normal mouth opening range at every subsequent follow up in both the groups. There was a significant difference (p < 0.05) observed in the improvement of interincisal mouth opening during the second, third, and fourth weeks of follow-up.
When the mean bite force values were evaluated, there was gradual increase noted on subsequent follow up from 1st week to 6th week in both the group at all the sites and showed statistically significant difference (p < 0.01) between both the groups during 2nd,3rd,4th,5th and 6th week at the incisor region, 3rd week at the right canine region, 2nd and 3rd weeks in the left canine region; 1st,3rd, and 4th weeks at the right molar region, and 2nd and 3rd weeks at the left molar region. Variations in mean biting force values between subsequent follow-ups were calculated for both the groups. With this a comparison of the changes in mean biting force between the two groups was computed. During subsequent weeks’ interval at all the areas, difference in changes in the mean were observed which was statistically significant (p < 0.05) during 2nd, 3rd and 4th weeks at incisor region (Table 1); 3rd and 4th weeks at right canine area (Table 2); from the 1st to 4th weeks at the left canine region (Table 2); 2nd, 3rd and 4th week in the left molar region, and 1st to 5th weeks at right molar region (Table 3).
Table 1.
Comparison of changes in mean incisor bite force between both the groups.
| Follow up (Weekly) | Bite force (kg) Mean ± SD (Group 1) |
Change in bite force Mean ± SD |
Bite force (kg) Mean ± SD (Group 2) |
Change in bite force Mean ± SD |
p value (Changes of mean) |
|---|---|---|---|---|---|
| Pre-op | 1.43 ± 0.44 | – | 1.63 ± 0.45 | – | – |
| 1st | 2.47 ± 0.30 | 1.04 ± 0.36 | 2.64 ± 0.44 | 1.01 ± 0.36 | >0.05 |
| 2nd | 2.87 ± 0.38 | 0.40 ± 0.37 | 3.57 ± 0.56 | 0.93 ± 0.42 | <0.001 |
| 3rd | 3.28 ± 0.54 | 0.41 ± 0.32 | 4.52 ± 0.45 | 0.95 ± 0.45 | <0.001 |
| 4th | 3.59 ± 0.49 | 0.31 ± 0.27 | 5.38 ± 0.57 | 0.86 ± 0.45 | <0.001 |
| 5th | 4.04 ± 0.61 | 0.45 ± 0.40 | 5.72 ± 0.68 | 0.34 ± 0.40 | >0.05 |
| 6th | 4.52 ± 0.62 | 0.48 ± 0.32 | 6.07 ± 0.69 | 0.35 ± 0.19 | >0.05 |
Pre-op = pre-operative, SD = standard deviation.
Table 2.
Comparison of changes in mean canine bite force between both the groups on both the sides.
| Site | Follow up (Weekly) | Bite force (kg) Mean ± SD (Group 1) |
Change in bite force Mean ± SD |
Bite force (kg) Mean ± SD (Group 2) |
Change in bite force Mean ± SD |
p value (Changes of mean) |
|---|---|---|---|---|---|---|
| Right canine area | Pre-op | 3.88 ± 1.14 | – | 3.75 ± 1.12 | – | |
| 1st | 4.18 ± 0.78 | 0.30 ± 0.77 | 4.59 ± 1.09 | 0.84 ± 1.52 | >0.05 | |
| 2nd | 4.78 ± 0.97 | 0.60 ± 0.42 | 5.27 ± 1.09 | 0.68 ± 0.50 | >0.05 | |
| 3rd | 5.31 ± 1.01 | 0.53 ± 0.23 | 6.72 ± 1.12 | 1.45 ± 0.53 | <0.01 | |
| 4th | 6.54 ± 1.20 | 1.23 ± 0.35 | 7.09 ± 1.07 | 0.37 ± 0.30 | <0.01 | |
| 5th | 7.15 ± 1.32 | 0.61 ± 0.61 | 7.73 ± 1.11 | 0.64 ± 0.39 | >0.05 | |
| 6th | 7.68 ± 1.33 | 0.53 ± 0.30 | 8.26 ± 1.06 | 0.53 ± 0.46 | >0.05 | |
| Left canine area | Pre-op | 3.58 ± 1.07 | – | 3.34 ± 0.91 | – | |
| 1st | 4.31 ± 1.12 | 0.73 ± 0.36 | 4.71 ± 1.06 | 1.37 ± 0.60 | <0.001 | |
| 2nd | 4.90 ± 1.21 | 0.59 ± 0.56 | 5.89 ± 1.18 | 1.18 ± 0.47 | <0.001 | |
| 3rd | 5.55 ± 1.34 | 0.65 ± 0.57 | 7.17 ± 1.37 | 1.28 ± 0.53 | <0.001 | |
| 4th | 6.80 ± 1.39 | 1.25 ± 0.71 | 7.38 ± 1.19 | 0.21 ± 0.35 | <0.001 | |
| 5th | 7.33 ± 1.45 | 0.53 ± 0.30 | 7.97 ± 1.14 | 0.59 ± 0.48 | >0.05 | |
| 6th | 8.20 ± 0.99 | 0.87 ± 0.54 | 8.60 ± 0.86 | 0.63 ± 0.44 | >0.05 |
Table 3.
Comparison of changes in mean molar bite force between both the groups on both the sides.
| Site | Follow up (Weekly) | Bite force (kg) Mean ± SD (Group 1) |
Change in bite force Mean ± SD |
Bite force (kg) Mean ± SD (Group 2) |
Change in bite force Mean ± SD |
p value (Changes of mean) |
|---|---|---|---|---|---|---|
| Right molar area | Pre-op | 8.20 ± 0.62 | – | 8.51 ± 0.66 | – | |
| 1st | 8.69 ± 0.35 | 0.49 ± 0.56 | 9.38 ± 0.32 | 0.87 ± 0.43 | <0.05 | |
| 2nd | 9.12 ± 0.42 | 0.43 ± 0.24 | 10.32 ± 0.36 | 0.93 ± 0.44 | <0.001 | |
| 3rd | 9.64 ± 0.59 | 0.52 ± 0.31 | 11.25 ± 0.46 | 0.94 ± 0.26 | <0.001 | |
| 4th | 9.88 ± 0.73 | 0.24 ± 0.39 | 11.83 ± 0.53 | 0.58 ± 0.26 | <0.001 | |
| 5th | 11.54 ± 0.70 | 1.66 ± 0.65 | 11.76 ± 0.58 | 0.07 ± 0.24 | <0.001 | |
| 6th | 12.32 ± 0.75 | 0.78 ± 0.50 | 12.61 ± 0.69 | 0.85 ± 0.48 | >0.05 | |
| Left molar area | Pre-op | 8.33 ± 1.04 | – | 8.37 ± 0.94 | – | |
| 1st | 8.82 ± 0.72 | 0.49 ± 0.68 | 9.18 ± 0.82 | 0.80 ± 0.58 | >0.05 | |
| 2nd | 9.29 ± 0.65 | 0.47 ± 0.23 | 9.97 ± 0.67 | 0.79 ± 0.60 | <0.05 | |
| 3rd | 9.58 ± 0.57 | 0.29 ± 0.31 | 10.75 ± 0.62 | 0.78 ± 0.47 | <0.001 | |
| 4th | 11.33 ± 0.70 | 1.75 ± 0.95 | 11.71 ± 0.89 | 0.96 ± 0.55 | <0.001 | |
| 5th | 11.76 ± 0.69 | 0.43 ± 0.29 | 12.11 ± 0.93 | 0.40 ± 0.33 | >0.05 | |
| 6th | 12.51 ± 0.57 | 0.75 ± 0.39 | 12.80 ± 0.66 | 0.69 ± 0.48 | >0.05 |
There were no cases of non-union, malunion, infection, wound dehiscence or plate fracture in 3D as well as conventional miniplate group recorded. Functional occlusion was achieved in all the patients in both the groups postoperatively, and none of the patient showed neurological deficit. Mean operating time required for surgery was 50.06 ± 5.65 min in study group while in control group it was 64.42 ± 8.57 min. The mean difference between two groups was 14.36 min which was found to be statistically highly significant (<0.001).
4. Discussion
The term Anterior Mandibular Fractures (AMFs) refer to the fractures that occur in the region of bone which is bordered by vertical lines just distal to canine bilaterally and comprises parasymphysis and symphysis fracture of mandible.9 Parasymphysis fracture management is always challenging owing to its unique anatomy, curvature, blood supply, attachments of jaw opening muscles, presence of point of weakness associated with canine roots, proximity to mental foramina and thickness of cortical plates.10 These will have further impact on postoperative outcomes and patient's restoration to normal form and function.
There was ongoing debate on post-operative outcomes offered by 2D and 3D miniplates in the management of anterior mandibular fractures. Each one of them discussed advantages and limitations of both the plating systems in specific situations. Farmand introduced 3D titanium plating system for the management of mandibular fractures for the first time in 1992.5 In 1996, he carried out biomechanical analysis and concluded that the fixation with 3D miniplate would provide greater three-dimensional stability as compared to two conventional miniplates for anterior mandibular fractures.11 However, Jain MK et al. in 2010 reported Champy's miniplate system to be superior compared to 3D miniplate system in one of his studies stating 3D plates were difficult to adapt and unfavourable for use in oblique fractures and fractures involving mental nerve region. At the same time, he also recorded that incorporation of two vertical bars in the design of 3D plates significantly reduces torsional forces and improves stability.12 At times we faced placement and adaptation of 3D plate challenging in certain clinical scenarios such as in cases of:
-
•
Less anterior mandibular height especially in females and in atrophic mandible
-
•
Altered tooth to bone ratio due to larger roots of anterior teeth
-
•
Fracture line is more oblique and in close proximity to the mental foramen
Bite force represents the functional aspects of the mandible and its surrounding musculature. Additionally, it indicates the restoration of masticatory efficiency.13 So, in this study we have used bite force as a main parameter to asses patient's return to normal function following surgical intervention. It can be assumed that postsurgical edema and pain occurring in the early postoperative period can cause abrupt decrease in bite force as well as patient's reluctance or fear of biting hard food after surgery can also be considered as a significant influencing factor. Keeping these observations recorded by previous researchers present study has evaluated biteforce in patients with anterior mandibular fractures treated by 3D plates.
In 2011, Kshirsagar et al.14 has measured bite force in 60 healthy voluntary individuals and compared it with bite forces generated in 6 patients with isolated unilateral parasymphyseal fractures treated using two miniplates at different follow up periods to establish range for biteforce measurements. The values improved till 4–6 weeks and 6–12 weeks at incisor and molar region respectively as compared to that of healthy volunteer group. Fracture at any area can affect the muscle function and masticatory force distribution along the whole mandible. Laterotrusive movements from centric occlusion determine several functional occlusion types amongst which canine guided occlusion states that canines are the most appropriate teeth to guide certain excursive movements of mandible during mastication.15,16 Posterior teeth are better at accepting vertical forces in comparison to lateral forces whereas canines are more adapted to resist lateral forces because of several reasons like their position in the dental arch, possession of good crown-root ratio making them strong enough to withstand higher occlusal forces, and high proprioception.16 There are very few studies available in the literature on bite force measurement after treatment of mandibular fractures and much less for anterior region fractures. Most of the earlier studies measured bite forces to evaluate patient's return to normal masticatory functions only on incisors and molar region.8,14,17, 18, 19 Measurement of bite force at all the three regions i.e., incisor, canine and molar region on both the sides may reflect better distribution of occlusal forces throughout the mandibular arch. All of the aforementioned factors highlight the significance of measuring bite force in all three regions in present study. To the best of our knowledge, only two studies on anterior mandibular fracture management with 3D and conventional miniplates have included bite force measurement at either the canine or premolar region in addition to the molar and incisor region. Jain et al. 201920 had assessed bite force on the incisor, canine, and molar regions; whereas Patel KN et al. 202121 assessed bite force on the incisor, premolar, and molar regions in their comparative studies on anterior mandibular fracture management with 2D Vs 3D miniplates. Thus, limited number of studies contemplated us to compare the bite forces at all the 3 regions generated following fixation of conventional miniplates Vs 3D miniplate group.
When the mean bite force values were compared between both the groups at all the regions the recorded values in the 3D plate group were found to be statistically significant during the mid-follow up period as compared to the conventional miniplate group. This period represents the active healing process of the bone with simultaneous restoration of comfort, nutrition and psychological status of the patient which were disrupted during the early post-operative period. Also, during subsequent follow up, postoperative edema subsides and muscle orientation as well as function restores, which ultimately leads to reduction in trismus and improvement in mouth opening. Kinra et al. in 201722 too noticed significant improvement in bite force at 3rd week of follow up in 3D plate group at incisor, right and left molar region which is consistent with our findings.
In contrast to our findings, Patel KN et al.21 observed that neither group's mean bite force at the incisor area changed significantly between early and late follow-up periods, but they did notice considerable improvement during the mid as well as late follow up period at the right molar region but not the left. Jain et al.20 in his study observed that though bite force was increased at every follow up in both the 3D and conventional groups, no significant difference was recorded between both the groups.
Present study has calculated changes in the mean bite force measurements for both the groups. This enabled us to make further comparison of mean changes between both the groups, providing a better idea of the amount of bite force that is restored. Present study recorded statistically significant difference in changes in the mean of bite forces between both the groups at 3rd and 4th week of follow up in right canine region and 1st to 4th week of follow up in left canine region. The difference we observed in changes in the mean bite force at the incisor region between both the groups during 2nd, 3rd and 4th week of follow up in our study partially correlates with findings of Kinra et al.22 who found it to be significant throughout the follow up (up to 8 weeks) in their study. In this study right and left molar bite force values showed significant difference in the changes in the mean bite force values between both groups during mid-follow up period which was in partial accordance with research carried out by Kinra et al.22 who noticed it to be significant at early follow up period only.
The findings of this study indicate that bite force readings of both the groups increased gradually from preoperative to the sixth postoperative week. It was also observed that during the immediate postoperative period, value of increase in bite force were low in both the groups. However, participants in the 3D group generated more bite force than those in the conventional miniplate group. All above findings prove that the use of 3D miniplates in management of anterior mandibular fracture are efficient enough to withstand masticatory forces during the entire period of fracture healing and most conveniently during immediate postoperative period thereby improving patient's ability to chew and maintain nutrition when it was critical. This can be explained by increase in bite forces and resistance to torsional forces providing better stability of fractured segments even under the fully functional masticatory system by 3D plates.
5. Conclusion
The findings of this study concluded that bite force is a reliable parameter to assess restoration of masticatory efficiency following ORIF. Present study also confirmed that 3D miniplates are more efficacious in the management of anterior mandibular fractures as they can withstand masticatory load efficiently during fracture osteosynthesis which leads to early restoration of chewing efficiency and return of patient to normal daily activities. It was observed that 3D miniplate exceeds conventional miniplate in terms of economic fixation option, ease of surgery, fewer implant materials, and less operating time. 3D miniplate also necessitates shorter surgical exposure of the fracture site, as well as minimal traction of the adjacent soft tissue, resulting in less postsurgical morbidity as an added advantage.
There are certain limitations of this study like: small sample size due to limited number of cases of isolated anterior mandibular fractures we received, individual variations in providing bite force considering age and gender in addition to condition of existing dentition as well as lesser follow up span. We recommend further longitudinal research with a larger sample size and longer duration of follow up with advanced radiographic aids may emphasize the excellent result offered by 3D miniplate in management of anterior mandibular fracture and would definitely prove more enlightening.
Source of funding
None.
Declaration of competing interest
None.
Acknowledgment
We thank Dr. Mayank Patel(biostatistician) for statistical analysis and interpretation of data for the study.
Contributor Information
Shital Patel, Email: drshital_patel@yahoo.com.
Kruna Bhimani, Email: krunabhimani08@gmail.com.
Roma Narsingyani, Email: romsnarsingyani@gmail.com.
Zenish Bhatti, Email: zenish1710@gmail.com.
Rajan Savani, Email: rajan.savani007@gmail.com.
References
- 1.Manodh P., Shankar D.P., Pradeep D., Santhosh R., Murugan A. Incidence and patterns of maxillofacial trauma - a retrospective analysis of 3611 patients - an update. Oral Maxillofac Surg. 2016;20(4):377–383. doi: 10.1007/s10006-016-0576-z. [DOI] [PubMed] [Google Scholar]
- 2.Al-Moraissi E.A., Ellis E. Surgical management of anterior mandibular fractures: a systematic review and meta-analysis. J Oral Maxillofac Surg. 2014;72(12) doi: 10.1016/j.joms.2014.07.042. 2507-e1. [DOI] [PubMed] [Google Scholar]
- 3.Luhr H.G. Vitallium Luhr systems for reconstructive surgery of the facial skeleton. Otolaryngol Clin North AM. 1987;20:573–606. [PubMed] [Google Scholar]
- 4.Gokkulakrishnan S., Singh S., Sharma A., Shahi A.K. An analysis of postoperative complications and efficacy of 3-D miniplates in fixation of mandibular fractures. Dent Res J. 2012;9(4):414. [PMC free article] [PubMed] [Google Scholar]
- 5.Farmand M., Dupoirieux L. The value of 3-dimensional plates in maxillofacial surgery. Maxillofac Surg. 1992;93:353. [PubMed] [Google Scholar]
- 6.Tate G.S., Ellis E., III, Throckmorton G. Bite forces in patients treated for mandibular angle fractures: implications for fixation recommendations. J Oral Maxillofac Surg. 1994;52(7):734–736. doi: 10.1016/0278-2391(94)90489-8. [DOI] [PubMed] [Google Scholar]
- 7.Throckmorton G.S., Ellis E., III, Hayasaki H. Jaw kinematics during mastication after unilateral fractures of the mandibular condylar process. Am J Orthod Dentofacial Orthop. 2003;124(6):695–707. doi: 10.1016/j.ajodo.2003.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Gerlach K.L., Schwarz A. Bite forces in patients after treatment of mandibular angle fractures with miniplate osteosynthesis according to Champy. Int J Oral Maxillofac Surg. 2002;31(4):345–348. doi: 10.1054/ijom.2002.0290. [DOI] [PubMed] [Google Scholar]
- 9.Baiomy A.A., Mohammed A. Efficacy of different fixation techniques in repair of anterior mandibular fractures. Egypt J Oral Maxillofacial Surg. 2018;9(3):109–117. [Google Scholar]
- 10.Mohd Y.Q., Reddy S., Sinha R., Agarwal A., Fatima U., Abidullah M. Three-dimensional miniplate: for the management of mandibular parasymphysis fractures. Ann Maxillofac Surg. 2019;9:333–339. doi: 10.4103/ams.ams_172_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Farmand M. Experiences with the 3-D miniplate osteosynthesis in mandibular fractures. Fortschritte der Kiefer-und Gesichts-chirurgie. 1996;41:85–87. [PubMed] [Google Scholar]
- 12.Jain M.K., Manjunath K.S., Bhagwan B.K., Shah D.K. Comparison of 3-dimensional and standard miniplate fixation in the management of mandibular fractures. J Oral Maxillofac Surg. 2010;68(7):1568–1572. doi: 10.1016/j.joms.2009.07.083. [DOI] [PubMed] [Google Scholar]
- 13.Koc D., Dogan A., Bek B. Bite force and influential factors on bite force measurements: a literature review. Eur J Dermatol. 2010;4:223–232. 02. [PMC free article] [PubMed] [Google Scholar]
- 14.Kshirsagar R., Jaggi N., Halli R. Bite force measurement in mandibular parasymphyseal fractures: a preliminary clinical study. Craniomaxillofacial Trauma Reconstr. 2011;4(4):241–244. doi: 10.1055/s-0031-1293521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clark J.R., Evans R.D. Functional occlusion: I. A review. J Orthod. 2001;28:76–81. doi: 10.1093/ortho/28.1.76. [DOI] [PubMed] [Google Scholar]
- 16.Pasricha N., Sidana V., Bhasin S., Makkar M. Canine protected occlusion. Indian J Oral Sci. 2012;3:13–18. [Google Scholar]
- 17.Giri K.Y., Sahu P., Rastogi S., et al. Bite force evaluation of conventional plating system versus locking plating system for mandibular fracture. J maxillofacial oral surg. 2015;14(4):972–978. doi: 10.1007/s12663-015-0764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pal K., Sushmitha R., Mitra G.V., Motivale T., Tiwari S. Evaluation of post-operative bite force on mandible fractures treated with open and closed reduction. Int J Adv Res. 2017;5(2):1002–1008. [Google Scholar]
- 19.Glória J.C., Fernandes I.A., Silveira E.M., et al. Comparison of bite force with locking plates versus non-locking plates in the treatment of mandibular fractures: a meta-analysis. Int Arch Otorhinolaryngol. 2018;22:181–189. doi: 10.1055/s-0037-1604056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jain M.K., Kerur P. Bite force as a parameter for comparison between three-dimensional and standard titanium miniplates for the management of anterior mandibular fractures: a prospective randomized double-blinded clinical trial. J maxillofacial oral surg. 2019;18(2):249–255. doi: 10.1007/s12663-018-1091-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel K.N.A., Girish G., Sneha T.R., Reddy K.R. Comparative assessment of bite forces in subjects treated for anterior mandibular fractures with 3-dimensional plates and standard miniplates. J Oral Med Oral Surg Oral Pathol Oral Radiol. 2021;7(1):29–36. [Google Scholar]
- 22.Kinra P.K., Jayakumar K., Soumithran C.S., Michael M.J., Passi D., Singh M. Comparative evaluation of bite force analytical study following mandibular osteosynthesis using three dimensional and conventional locking miniplates. Natl J Maxillofac Surg. 2017;8(1):34. doi: 10.4103/njms.NJMS_76_16. [DOI] [PMC free article] [PubMed] [Google Scholar]