Abstract
Background:
To consciously select an appropriate dental cement for each type of intracanal post.
Materials and Methods:
An electronic search was carried out (1970 to 2020) through Medline, PubMed, Scopus, and Google Scholar. The following keywords were searched in title, abstract, or keywords with different combinations: endodontically treated tooth, root canal therapy, dental posts, post and core, prefabricated posts, custom posts, dental cement, resin cements, cement selection, cement, and adhesive resin cement.
Results:
Evaluating full texts, 146 articles were selected to review the types of posts and cements, selection criteria of appropriate cement for each type of post, and compare the results obtained by different cements.
Conclusion:
Dental cements affect the survival rate, durability, and success rate of postbased treatments. Considering special characteristics and application of each type of intracanal post, conscious selection of cement is an important determining factor in long-lasting success. Choosing an appropriate cement has a key role in success and durability of dowel posts-based fixed restorations.
Key Words: Dental cement, glass ionomer cements, post-core technics, zinc phosphate cement, resin cement
INTRODUCTION
One of the most prevalent methods for restoring an endodontically treated tooth (ETT) with inadequate remaining structure is to use dowel post and core complex. The concept of using a root canal to provide retention for core material was the first expressed in 1700s by Pierre Fauchard,[1,2] who suggested to use metallic “tenons” posts screwed into root canal.[3] In 1800>s, several researches focused on increasing crown retention by posts application.[1] Posts, generally, could be classified to prefabricated or custom-made, and metallic or nonmetallic with their related subcategories. Prefabricated metallic posts, the oldest version of intracanal posts, had some limitation in esthetic zone,[4] as well as the risk of toxicity, the possibility of corrosion, and allergic reactions;[5,6] nonmetallic posts were introduced to overcome these deficiencies.[7] However, several failures in the treatment of endodontically treated teeth in the current century[1] put a significant question mark in front of the applications of dowel post. Some studies claimed posts could concentrate stress, and lead to root fracture.[8,9,10,11] Other reported gingivitis,[12,13] periodontal disease,[14] fracture of core,[12] fracture of post,[12] loss of retention,[14,15] and caries[14,16] as the complications of post-based treatment, and introduced gingivitis,[12] and root fracture[15] as the most prevalent complications.
Although some treatment alternative namely “Richmond crown”[1,17] and “Endocrown” were introduced in 19th and 20th centuries, post-based restorative options are still among the most prevalent treatment options used in every day dentistry. The improvement in scientific criteria resulted in an ever-increasing introduction of different materials and methods for post fabrication to maximize the profits, and minimize the potential risks. However, long-term successful results, and predictable retention without stress concentration inside the remaining root structure mainly return to appropriate cement selection. Considering the varieties of available cements with special characteristics [Table 1], the present review focuses on comparing different types of dental cement, according to their selection and application criteria for different types of posts.
Table 1.
Properties of different types of cement
| Cements | Chemical content | Compressive strength | Tensile strength | Solubility (weight% at 24 h) | Setting time (min) | Modulus of elasticity (GPa) | Bond to tooth | Mikroleakage | Retention | Film thickness |
|---|---|---|---|---|---|---|---|---|---|---|
| Zinc phosphate | Phosphoric acid liquid + zinc oxide and magnesium oxide powder[18] | 62-101 MPa[18] | 5-7 MPa[18] | 0.2[19] | 5-9[19] | 13[19] | No[18,19] | High[7,18] | Moderate[7,18] | <25[7,18] |
| Zinc polycarboxylate | Polyacrylic acid + zinc oxide and magnesium oxide powder[18] | 67-91 MPa[18] | 8-12 MPa[18] | 0.0619 | 7-9[19] | 5-6[19] | Moderate chemical[19,22] | High to very high[7,18] | Low to moderate[7,18] | <25[7,18] |
| GI | Aluminosilicates in the powder + polyacrylic acid and tartaric acid[18] | 85-126 MPa[18] | 6-7 MPa[18] | 1[19] | 6-8[19] | 7-8[19] | Chemical[19] | Low to very high[7,18] | Moderate to high[22] | <25[7,18] |
| Resin-modified GI | Resin and GI[18] | 93-226 MPa[18] | 13-24 MPa[18] | 0.7-0.4[19] | 5.5-6[19] | 2.5-7.8[19] | Chemical[19] | Very low[7,18] | Medium[22,23] | >25[7,18] |
| RC | Diluted composite resin + additive adhesive monomers | 179-250 (high[24]) | High[24] | 0.05[19] | 4+[19] | 4-6[19] | Micro-mechanical[19] | Very low[7,18] | High[22] | <25[25] |
GI: Glassionomer; RC: Resin cement
MATERIALS AND METHODS
An electronic search was carried out (1970 to 2020) through Medline, PubMed, Scopus, and Google Scholar. The following keywords were searched in title, abstract, or keywords with different combinations: ETT, root canal therapy, dental post, post and core, prefabricated post, custom post, dental cement, resin cement, cement selection, cement*, adhesive resin cement. Using reference management software (Endnote X8, Thomson Reuters), duplicated studies were eliminated, and the most relevant articles were chosen based on inclusion criteria: English articles focusing on different types of posts and dental cements, and selecting appropriate cement for each type of post. The studies addressed extra canal posts, or other characteristics of intracanal posts were excluded, as well as studies on other direct or indirect restorations.
RESULTS
The numbers of search results for the selected keywords were 1580 (PubMed), 18,000 (Google scholar) and 3105 (Scopus). After duplicate removal and title/abstract analysis, 317 studies were selected for full-text review. Finally, 146 studies met the requirement of inclusion/exclusion criteria and were included to be discussed.
Dental cements provide retention for indirect restorations by chemical or mechanical bonding, or simply, filling the space between the restoration and tooth structure, physically.[26] Intra canal posts provide retention for core materials; however, its own retentiveness should be passively provided by dental cements. Different dental cements are available with varieties of properties to be used:
Zinc phosphate cement (ZP), introduced in 1800s, is the oldest luting cement.[19,27] Low tensile strength,[18,19] high degree of solubility (0.36%),[19] high compressive strength, and elastic modulus,[18] low cost, and early strength are among the properties. After 1 h, ZP has the lowest PH (about 1.2),[18,19] that increases to 5.5 after 24 h.[18] In patients with acid reflux problems, and in vital teeth with low residual dentin thickness, this cement should be used carefully.
Zinc polycarboxylate cement (ZPC), introduced in 1968,[28] was the first cement that exhibited chemical bond to tooth structure, and according to increasing pH after mixing, it was very biocompatible.[22] However, weak bond to enamel and dentin,[18] and low compressive and tensile strength,[18,20] make it inappropriate for single-unit restorations or long-span fixed partial dentures.[18]
Glass ionomer cement (GI) was introduced in 1969 under the name of aluminosilicate polyacrylic acid.[19] Enamel and dentin adhesion, fluoride release, low bonding strength, moderate compressive strength, low tensile strength, and high solubility are among the properties.[18,19] GI could be indicated in varieties of restoration namely all-metal/PFM crowns, short span fixed partial denture, alumina/zirconium-based all-ceramic restorations, and Metal post and core.
Resin-modified GI (RMGI) was introduced to overcome GI sensitivity to early moisture contamination and high solubility rate. In this combination of resin and conventional GI,[21] adhesion to tooth structure was improved as well as compressive/tensile strength, solubility, and post-cementation sensitivity.[29] RMGI has a wide range of applications; however, in traditional feldspathic or pressable ceramic restorations should be used with caution.[18]
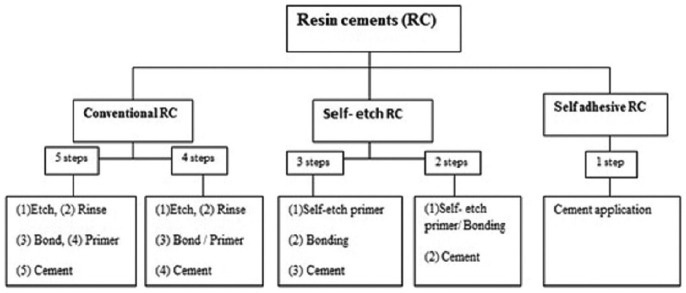
Resin cement (RC) was introduced in mid-1970s as an acid-base reaction cement.[30] High compressive, tensile, and bonding strength, esthetics, and low solubility, candidate this cement for esthetic or compromised situations.[31] RCs could be classified to conventional, self-etch, and self-adhesive types [Figure 1].[7,32] In conventional (total etch or etch-and-rinse) RC, etching process happens as a separate stage, and after rinsing, adhesive, or primer-adhesive is applied on tooth structure before cement application. Self-etch primer, used in self-etch RC, is a combination of acidic monomers, phosphate esters, and primer. These cements might be used in 2 or 3 steps. Self-adhesive (all-in-one) RC combined all the steps in one tube to reduce the technical sensitivity, and facilitate the process. However, the research reported lower bond strength for this type.[33,34,35,36]
Figure 1.
Resin cements classification.
Appropriate cement selection calls for knowing the cements properties [Table 2], and posts requirements. For bonding a post to root canal using RC, the cement has to be bonded to dentin structure. Conventional RC reported to provide high, predictable, and durable bond strength to enamel,[55,56,57] while bonding to dentin represents a greater challenge.[58] Dentin is a wet organic tubular tissue that communicates with dental pulp. All RCs have been reported to cause marginal leakage when used on this dynamic structure.[58] Micromechanical retention of RC to dentin is provided by the formation of hybrid layer between demineralized collagen fibers and cement, and also resin tags. The quality (thickness and uniformity) of hybrid layer determines the bond strength. Unlike self-etch RC, conventional RC proved to provide a thick uniform hybrid layer.[59] On the other hand, self-etch RC penetrates deeper into the dentin compared to self-adhesive type.[60] Morphological imaging has demonstrated a thin hybrid layer formation in self-etch RC, but no hybrid layer or resin tag in self-adhesive type.[33,61,62,63,64,65,66]
Table 2.
Advantages and disadvantages of available dental cements
| Cement | Advantages | Disadvantages |
|---|---|---|
| ZP | Nonexpensive[37] | Does not adhere to tooth or post[37] |
| Easy to manipulate[37] | Brittle[37] | |
| Quick to use[37] | Soluble in time[19,37] | |
| Relatively no technical sensitivity[37] | Vulnerable to microleakage[17,37,38,39] | |
| Reliable retention[37] | Does not release fluoride[37] | |
| Weak enough to remove the post if necessary[37] | ||
| Easy clean-up of excess cement[37] | ||
| GI | Adhere to dentine[37] | Vulnerable to dehydration and elution of calcium and |
| Release fluorid[19,37] | aluminum ions in exposure to excess moisture[37,38] | |
| Nonexpensive[37] | Brittle[37] | |
| Easy to manipulate[37] | Retention of post might be unreliable[37] | |
| Low film thickness[17,37] | ||
| Easily cleanable for excess cement[37] | ||
| Proper choice for patients with gastric reflux problems or want their teeth to be bleached[40,41] | ||
| Resin-modified GI cements | Increased retention[18,14,37] | More expensive than ZP or GI cements[37] |
| Adherence to metallic posts and root dentin[37] | Calls for application of primer or adhesive[37] | |
| Fluoride release[37] | Difficult or impossible to remove post, if required[37] | |
| Easily cleanable for excess cement[37] | ||
| Conventional RCs (etch and rinse) | Highest bond strengths to enamel[42] | High technique sensitivity[42,43,44,45,46] |
| High bond strengths to dentin[43] | Possibility of postoperative sensitivity of tooth[47,48] | |
| Selfadhesive resin cements | Higher bond strengths to dentin[36] | Lower bond strength to enamel compared to etch and rinse system[51] |
| Easy to use and fewer steps requirement[49] | ||
| Low technical sensitivity[50] | ||
| Selfetch resin cements | Lower technique sensitivity[51,53] | Lower bond strength[33,34,35,36] |
| Fewer steps are required[50,51,52,53] | Low rigidity and viscoelasticity[20] | |
| No pre-treatment is required[54] |
ZP: Zinc phosphate; GI: Glassionomer; RCs: Resin cements
However, there are controversial results on preferred RC for dentin bonding. Some studies indicated self-etch cement as the preferred RC for dentin bonding,[57,66,67] while others gave more priority to self-adhesive RC.[68,69,70] It has been reported that in the presence of smear layer, self-adhesive RC provides a weak bond with dentin,[68] and self-etch cement is preferred under such situation to provide an acceptable bond with smear layer, improve fluid content of dentinal tubules, and reduce the amount of dentin decalcification.[51] In spite of all of these controversies, all types of RC, including self-adhesive types, produce adequate bonds to dentin.[51] Bond strength of etch and rinse cements (20–35 Mpa), self-etch (10–35), and self-adhesive (20–30 Mpa) are all in acceptable clinical ranges.[59]
The type of restoration also plays an important role. Total-etch RC is often preferred in indirect restorations especially in the presence of large areas of enamel, while self-etch adhesives are recommended for direct restorations, and predominantly on dentinal bed.[58] According to these controversies, more clinical long-term evaluations are needed.
DISCUSSION
Selecting a proper dowel post depends on various factors namely the amount of remaining tooth structure, tooth anatomy, position, functional requirements, root length, width, and configuration, potential torquing force, dowel post design and material, bonding capability, esthetics, and restoration type.[71,72]
Prefabricated posts and recommended cements
Prefabricated posts are indicated when sufficient width and length of root structure has been preserved, the root has circular cross-section, and severe root canal undercuts prevent cast posts application.[73] Metallic prefabricated posts could be routinely cemented by conventional cements.[73,74,75,76] However, dual-cure RCs have been recommended for nonmetallic types,[67,77] or when higher retention is desired.
-
Metallic post has been using during the past 20 years, and divides into three subgroups based on material type: titanium, stainless steel, or brass. Conventional permanent cement (ZP and GI) could be used for these posts.[73] However, there are controversies in comparison between ZP and RC. Some studies reported better retention for RC,[78] while the others gave more priority to ZP in these posts;[74,75,76] there are other studies not recommend RC for clinical application in posts.[73]
-
Nonmetallic posts are either made from ceramics (zirconia or alumina),[80] or a combination of resin matrix and reinforcing fibers (carbon, glass, or quartz).[81] They were introduced to provide more favorable esthetics,[82] or close elastic modulus to dentine compared to metallic dowel posts[81] to reduce the risk of root fracture and increase the survival rate.[83]
- Zirconia post, composed of zirconium oxide, is an all-ceramic post with high flexural strength, elastic modulus,[84] and toughness.[85,86,87] It could be indicated in esthetic area;[32,88] however, inherent brittleness, limitates its application.[89] There is inherent deficiency in retention of these posts considering the smooth surface,[78] and insufficient bonding to RCs.[90,91,92,93,94] However, RC provides higher bond strength compared to GI cement,[95] and the RC with phosphate monomer content, proved to be more reliable for bonding zirconia[96]
-
Fiber reinforced posts show high success rate with reduced risk of root fracture by their close toughness to dentine.[97] Self-adhesive RC has been suggested as the cement of choice for fiber posts with high bond strength.[97] However, other researches proved better results using etch-and-rinse dual curing adhesive system, compared to self-adhesive or self-etch RC or GI cements.[98,99,100,101,102] A company have suggested dual-cure flowable hybrid composite for cementation of fiber posts.[103]
- Fiber reinforced resin-based composite (FRC) post reduces the risk of toxicity,[31,104] and by their close modulus of elasticity to dentine,[105,106,107] reduces the possibility of root fracture. Moreover, FRC posts can be removed easily for retreatment if necessary.[88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108] Bonding with tooth structure causes good distribution of occlusal forces.[109] However, FRC post has low physical strength. The most reliable cement for this group of posts is etch-and-rinse dual-cure RCs.[110]
- Polyethylene fiber post (PFP), introduced as an alternative to stainless steel and zirconia posts with less micro-leakage,[111] is made from ultrahigh molecular weight polyethylene woven fiber ribbons.[112] Tooth structure protection, and reduced risk of root fracture have been mentioned as advantages.[106] Eskitaşcioğlu et al. reported minimum stress within PFP compared to cast post and core system; and suggested these posts for restoration of apically resected teeth[113]
- Glass fiber (GF) post is made from silicate glass (electrical, or high-strength glass), or quartz fibers,[116,117] and different types of matrices (polymethylmethacrylate or epoxy resin).[118] Silicate glass ceramic post has better esthetic, that could even be enhanced by using epoxy resin as matrix.[88] Quartz (Glass) fiber post could be preferred over CFP for ease of application and removing, and clinicians preferred to use them because of their esthetic biocompatibility.[119] Self-adhesive RCs have been recommended by some companies[120] One study claim that RMGI could be indicated for GF posts.[37] Table 3 summarizes the recommendations of different companies for selecting proper type of cement for each type of posts.
Table 3.
Manufacturers’ recommendations for proper type of cement in each type of post
| Classification of posts | Manufacture of posts | Recommended type of cement |
|---|---|---|
| Metallic prefabricated | ||
| Titanium | A-UCR-330EX(Sweden and martina implantology)[121] | Self-etch RC[122] |
| ParaPost X Posts(Coltene/Whaledent)[122] | Self-adhesive RC[124,125] | |
| Dentatus Classic Surtex®Posts(Dentatus)[123] | Self-curing GI cement[126] | |
| Stainless steel | Parapost(Coltene/Whaledent)[122] | |
| Brass | Dentatus Classic Surtex®Posts(Dentatus)[123] | |
| Nonmetallic prefabricated | ||
| Fiber reinforced posts | TENAX®Fiber Trans(Coltene/Whaledent)[127] | Self-adhesive RC[103,124,127,132] |
| Para post Fiber Lux(Coltene/Whaledent)[127] | self-etching RCs[103] | |
| Para post Taper Lux(Coltene/Whaledent)[127] | Dual-and self-cure RCs[127] | |
| RelyX™ Fiber Post(3M ESPE)[128] | Light-curing RC[127] | |
| EZ-Fit Translucent(Essential dental system)[129] | ||
| DT Posts(VDw Dental)[130] | ||
| Zirconia | Cosmopost(Vivadent)[131] | |
| Snow post(Snow post)[7,133] | ||
| FRC | Marco-lock(RTD dental)[103] | |
| Glass-fiber | FibreKor Posts(Pentron)[133] | |
| Lucent anchor(Dentatus)[122] | ||
| Quartz fiber | Aesthetic-Plus(RTD/Bisco)[7,133] | |
| D.T. Light-Post(RTD/Bisco)[7,133] | ||
| Carbon fiber | C-Post(RTD/Bisco)[7,133] |
GI: Glassionomer; RCs: Resin cements
Custom posts
Custom posts are indicated when moderate-to-severe coronal structure has been lost, root canal has noncircular cross section,[72] the core has different angle to the post, core retention on post is compromised duo to tooth size, and when multiple post and core are to be made in the same patient.[72] A company recommended self-adhesive RC for metallic customize posts;[134] however, considering the adaptation of these types of posts to the root canal, all types of cements could be used for custom posts.[22,135] One study found ZP and GI to be more retentive than ZPC or even RC.[75] Another study claimed that GI is inappropriate for casted intracanal posts considering the insufficient strength.[136]
-
Metallic custom post is a very strong and retentive choice especially for small tooth, as the core is an inherent part of the component. Poor esthetics, risk of corrosion and fabrication inaccuracy, and difficult retrieval could be mentioned as disadvantages.[73]
- Nonprecious alloy posts include the posts fabricated from nickel–chrome, chrome-cobalt, and nonprecious gold color alloy (NPG). Nickel–chrome alloy might be electrolytically etched to enhance micro-mechanical bonding for RCs.[139] NPG alloy with its golden color has been introduced as an alternative for precious alloys with lower cost.[26] It has been claimed to have acceptable durability and thermal resistance, excellent fit, good biocompatibility, and easy adjustability, soldering, and finishing capacity.[26] However, it shows high corrosion susceptibility,[25] that might lead to significant discoloration, and potential cell toxicity.[80]
Nonmetallic all-ceramic custom post, made from high-toughness ceramic materials such as alumina or zirconia, is very biocompatible, does not exhibit galvanic corrosion, and provides significantly enhanced esthetic; but it has low fracture strength and toughness.[80] Dual-cure adhesive RCs have been recommended for this type of posts.[131] Self-curing RC and conventional cements (ZP, GI, RMGI) could also be used for ceramic custom posts.[131] Self-adhesive RC has been suggested for these posts; with higher bond strength compared to conventional cements.[126,134,140] Table 4 summarizes the characteristics of different types of post.
Table 4.
Characteristics of different type of intracanal posts
| Type | Subcategory | Advantages/indications | Disadvantages/contraindications |
|---|---|---|---|
| Prefabricated posts | Metallic | ||
| Titanium | Preservation of tooth structure[141] | Possibility of corrosive or allergic reactions[5,6] | |
| Stainless steel | Same radiodensity as Gutta-Percha[7] | ||
| Brass | Low fracture strength(titanium)[4,7,104,142] | ||
| Nonmetallic | Contraindicated in thin canal[7] | ||
| Esthetic | |||
| Ceramic posts | |||
| Zirconia | Esthetic[32,88,143] | Weaker than metallic posts[7] | |
| High fracture toughness[76] | Less conservative of tooth structure[7] | ||
| Excellent resistance to corrosion[76] | Endanger the core retention[30,144] | ||
| High flexural strength[76,88] | Poor resin-bonding capability[93,145] | ||
| High elastic modulus[84] and toughness[85-87] | |||
| Good chemical stability | |||
| Good biocompatibility | |||
| Fiber reinforced posts | |||
| Polyethylene | Decrease possibility of root fracture[146,147] | Very expensive[112] | |
| Less microleakage than zirconia and stainless-steel posts[112] | |||
| Indicated in teeth with apical resection[146,147] | |||
| High elastic coefficient[146,147] | |||
| High resistance to stretch and distortion[147] | |||
| FRC | Reduced risk of toxicity[31,104] | Low physical strength[104] | |
| Close modulus of elasticity to dentine[105,106,107] | |||
| Can be used in esthetic zone[104] | |||
| Easy to remove and retreat[88,108] | |||
| Good bonding with tooth structure[109] | |||
| Glass-fiber | |||
| Silicate | Better esthetic than quartz fiber posts[88] | Esthetically weaker than FRC posts[88] | |
| Biocompatibility[88] | Low strength[88] | ||
| Dentin bonding[88] | Debonding[88] | ||
| Uncertain clinical performance[88] | |||
| Quartz | Easy to use and manipulation[88] | Debonding[88] | |
| Easy to remove for retreatment[88] | Moderate strength[88] | ||
| Nonesthetic | |||
| Carbon fiber | Close modulus of elasticity to dentine[7,88,148] | Should not be used in esthetic zone[7,88,148] | |
| Reduce the possibility of root fractures[7,82,148] | |||
| Easy to remove[149] | |||
| Reduce the risk of toxicity[31] | |||
| High tensile strength[88] | |||
| Customize posts | Metallic | ||
| Nonprecious alloy | |||
| Nickel-cobalt | High success rate[150,151] | Contraindicated in high esthetic zone[4,7] | |
| Good choice for misaligned, or small teeth[7] | More time and cost[7] | ||
| Easy to remove[7] | Possibility of allergic reactions[5,6] | ||
| Chrome-cobalt | |||
| NPG color alloy | Cost effect[26,152] | High corrosion reaction[26] | |
| High durability[26,152] | Uncertain and insufficient documented evidence | ||
| High thermal strength[26,152] | |||
| Excellent fit[26,152] | |||
| Easy soldering[26,152] | |||
| Biocompatibility[26,152] | |||
| Precious alloy | |||
| Platin-palladium | Highly biocompatible[138] | Expensive | |
| Palladium-silver | Suitable for hypersensitive patients[138] | ||
| Gold | Repair option[138] | ||
| Nonmetallic | |||
| All ceramic | Excellent aesthetics[73] | Brittle[73] | |
| Excellent biocompatibility[73,80] | Not appropriate for bruxism patients[73] | ||
| Low fracture strength and toughness[80] | Very rigid[73] | ||
| No galvanic corrosion[80] | High possibility of root fracture[73] | ||
| Good radioopacity[73] |
NPG: Nonprecious gold; FRC: Fiber reinforced resin-based composite
Cement selection criteria
Dental cement in indirect restorations could be considered as an important determining factor affects retention, stability, survival, esthetic, and also patient satisfaction. The selection of appropriate cement could even be more important in intracanal posts; as in post-based restorations, not only the durability of intracanal posts but also the survival and durability of restorative treatments depend on post retention. There are a wide range of prefabricated or custom posts types/materials introduced in an ever-increasing manner in the last decade. The same varieties exist in available cements, especially when it comes to resin luting cements.
Conventional or resin cements?
In general, when an intracanal post has high degrees of adaptation in the root prepared canal (custom post), or the strength of post is not affected by bonding to tooth structure (e.g., metallic post), or esthetic is not a determining factor, conventional cements namely GI and ZP might provide acceptable retention.[8,19,29] RMGI could provide higher retention,[8,15,37] and ZPC cement could be indicated for situations where retrievability is predicted in dowel post-based treatments.[7,18] These conventional well-known cements with a long history of application, are easily accessible, less expensive, and less technique sensitive that candidate them for routine dental applications.[37] However, there are situations where higher retention, strength, or esthetic call for the application of RCs. Considering the variety of types and characteristics of these cements, conscious selection is important to guarantee the long-lasting success.
Which type of resin cements?
Some RC proved to provide higher and more durable retention (total etch cements),[51] while the others could facilitate the cement application in cementing a dowel post intra root canal (self-adhesive cements),[153] or control the acid penetration or dentin desiccation during cementing process (self-etch cements).[51] Some RC provide immediate and predictable complete polymerization (light-cure RC), while the others could be used when full light penetration is not assured (dual- or self-cure RC).[51] The selection between these cement types call for knowing the characteristic of different dowel posts, and clinical requirements.
The present review tried to provide a document-based information to select an appropriate cement based on dowel post material/type classifications. Long-term studies focused on the changes that occur in cement characteristics over the time, and the behavior of different cements under challenging conditions (e.g., short roots, abnormal dentin structure, excessive applied forces, or potential material deteriorations) are suggested to provide sound and reliable choice of cements for different types of dowel posts. Table 5 summarizes outcomes of studies on different cements.
Table 5.
Outcome of some studies on different cements retention for post and cores
| Author | Type of post | Compared cements | Conclusion |
|---|---|---|---|
| Habib et al., 2005[154] | Custom cast posts | ZP and self-etch dual RC | ZP had higher retentive values compared to RC |
| Duncan and Pameijer, 1998[155] | Parallel titanium posts | RC, ZP, GI, and RMGI | RC provided higher retention than others |
| Chan et al., 1993[156] | Stainless steel paraposts | ZP, ZPC, GI, RC | Stainless steel posts cemented with RC exhibited higher resistance to dislodgement by vertical tensile forces |
| Cohen et al., 1999[157] | Stainless steel posts | RC and ZP | Stainless steel dowels have been shown to be more retentive thancarbon fiber posts when cemented with either RC or ZP cement |
| Lencioni et al., 2010[158] | Pure titanium posts | Self-etch RC, self-adhesive RC, ZP | Posts fixed with self-adhesive RC presented superior bond strength compared to ZP and self-etch cements |
| Ubaldini et al., 2018[159] | Fiber posts | Etch and rinse RC and self-etch adhesive RC | Etch and rinse RC provided higher retention for fiber posts |
| Radke RA, 1988[74] | Cast gold posts | ZP, GI, ZPC | ZP and GI cements were found to be more retentive than ZPC |
| Sahmali et al., 2004[160] | Ceramic posts and carbon fiber posts | Self-etch RC, RMGI, GI | Self-etch RC had significantly higher bond strength than two other cements |
| Hagge et al., 2002[161] | Prefabricated post(paraposts) | Self-etch RC, ZP | Self-etch RC demonstrated higher retention than ZP |
| Bonfante et al., 2007[37] | Glass fiber posts | RMGI, dualcure RC | RC provided higher tensile bond strength for glass fiber posts |
| Menani et al., 2008[162] | Cast posts(gold alloypure titanium) | ZP, RC | Both cements provided similar mean tensile retention |
| Cohen et al., 1998[163] | Flexi-post, access post, titanium post | Composite cement, ZP, advance, duet, and GI | Composite cement provided higher retention for all types of posts |
| Sen et al., 2004[164] | Prefabricated posts(ParaPost, Flexi-Post) | Etch and rinse RC, ParaPost Cement, Flexi-Flow Natural, and ZP | Flexi-post showed significantly higher retentive strengths compared to non-threaded posts RC significantly increased the dowel retention compared to ZP |
| Ertugrul and Ismail, 2005[76] | Cast metal posts | RC, ZP | ZP cement provided greater tensile bond strength than RC with and without silane coating agent |
ZP: Zinc phosphate; GI: Glassionomer; RC: Resin cement; RMGI: Resin-modified glass ionomer
CONCLUSION
Considering the limitation of this review, the following conclusions could be derived:
Conventional cements could be used safely for metallic prefabricated posts; in nonmetallic posts, or in situations with extensive coronal destruction, or higher retentive demands, dual-cure RCs have been recommended as appropriate alternative
Etch-and-rinse RC provides higher retention with predictable durability, but the retention provided by self-etch or self-adhesive RCs could still be acceptable in normal clinical situations
RCs containing functional phosphate monomer are the most appropriate adhesive cement for zirconia prefabricated or custom posts
Considering the perfect adaptation, all types of cements could be used for custom posts; however, conventional cements are preferred for metallic, and adhesive resin for ceramic posts.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
REFERENCES
- 1.Al-Dhalaan R Prosthodontic Management of Endodontically Treated Teeth; Factors Determining Post Selection, Foundation Restorations and Review of Success Failure Data. Was available on 12 May 2020 from: https://www.endoexperience.com/documents/prosthodonticmanagementofendodonticallytreatedteeth.pdf .
- 2.Terry DA, Swift EJ. Post-and-cores: Past to present. Dent Today. 2010;29:132–5. [PubMed] [Google Scholar]
- 3.Smith CT, Schuman NJ, Wasson W. Biomechanical criteria for evaluating prefabricated post-and-core systems: A guide for the restorative dentist. Quintessence Int. 1998;29:305–12. [PubMed] [Google Scholar]
- 4.Meyenberg KH, Lüthy H, Schärer P. Zirconia posts: A new all-ceramic concept for nonvital abutment teeth. J Esthet Dent. 1995;7:73–80. doi: 10.1111/j.1708-8240.1995.tb00565.x. [DOI] [PubMed] [Google Scholar]
- 5.Hayashi Y, Nakamura S. Clinical application of energy dispersive x-ray microanalysis for nondestructively confirming dental metal allergens. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1994;77:623–6. doi: 10.1016/0030-4220(94)90323-9. [DOI] [PubMed] [Google Scholar]
- 6.Kedici SP, Aksüt AA, Kílíçarslan MA, Bayramoğlu G, Gökdemir K. Corrosion behaviour of dental metals and alloys in different media. J Oral Rehabil. 1998;25:800–8. doi: 10.1046/j.1365-2842.1998.00305.x. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: A literature review. J Endod. 2004;30:289–301. doi: 10.1097/00004770-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Guzy GE, Nicholls JI. In vitro comparison of intact endodontically treated teeth with and without endo-post reinforcement. J Prosthet Dent. 1979;42:39–44. doi: 10.1016/0022-3913(79)90328-7. [DOI] [PubMed] [Google Scholar]
- 9.Trope M, Maltz DO, Tronstad L. Resistance to fracture of restored endodontically treated teeth. Endod Dent Traumatol. 1985;1:108–11. doi: 10.1111/j.1600-9657.1985.tb00571.x. [DOI] [PubMed] [Google Scholar]
- 10.Morgano SM. Restoration of pulpless teeth: Application of traditional principles in present and future contexts. J Prosthet Dent. 1996;75:375–80. doi: 10.1016/s0022-3913(96)90028-1. [DOI] [PubMed] [Google Scholar]
- 11.Heydecke G, Butz F, Strub JR. Fracture strength and survival rate of endodontically treated maxillary incisors with approximal cavities after restoration with different post and core systems: An in-vitro study. J Dent. 2001;29:427–33. doi: 10.1016/s0300-5712(01)00038-0. [DOI] [PubMed] [Google Scholar]
- 12.Imran M, Shahid R, Hussain M, Jawaid M, Khan M. Complications after post and core treatment. Pak Oral Dent J. 2015;35:546–9. [Google Scholar]
- 13.Jung RE, Kalkstein O, Sailer I, Roos M, Hämmerle CH. A comparison of composite post buildups and cast gold post-and-core buildups for the restoration of nonvital teeth after 5 to 10 years. Int J Prosthodont. 2007;20:63–9. [PubMed] [Google Scholar]
- 14.Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications in fixed prosthodontics. J Prosthet Dent. 2003;90:31–41. doi: 10.1016/s0022-3913(03)00214-2. [DOI] [PubMed] [Google Scholar]
- 15.Said Y, Sahib D The Use of Post and Core in Public and Private Swedish Dental Care: A Questionnaire Study; 2018. [Last accessed on 2020 May 12]. Was available on from: http://urn.kb.se/resolve?urn=urn: nbn: se: umu: diva-143912 .
- 16.De Backer H, Van Maele G, De Moor N, Van den Berghe L. An up to 20-year retrospective study of 4-unit fixed dental prostheses for the replacement of 2 missing adjacent teeth. Int J Prosthodont. 2008;21:259–66. [PubMed] [Google Scholar]
- 17.Smith CT, Schuman N. Prefabricated post-and-core systems: An overview. Compend Contin Educ Dent. 1998;19:1013–8, 1020. [PubMed] [Google Scholar]
- 18.Yu H, Zheng M, Chen R, Cheng H. Proper selection of contemporary dental cements. Oral Health Dent Manag. 2014;13:54–9. [PubMed] [Google Scholar]
- 19.Hill EE. Dental cements for definitive luting: A review and practical clinical considerations. Dent Clin North Am. 2007;51:643–58, vi. doi: 10.1016/j.cden.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 20.Craig RG. Restorative Dental Materials. 14th ed. 13. St. Louis, Missouri: Mosby; 2019. p. 282. [Google Scholar]
- 21.Peutzfeldt A. Compomers and glass ionomers: Bond strength to dentin and mechanical properties. Am J Dent. 1996;9:259–63. [PubMed] [Google Scholar]
- 22.Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: A review of the current literature. J Prosthet Dent. 1998;80:280–301. doi: 10.1016/s0022-3913(98)70128-3. [DOI] [PubMed] [Google Scholar]
- 23.Christensen GJ. Reducing the confusion about resin cements. Clin Rep. 2008;1:1–3. [Google Scholar]
- 24.O'Brien WJ. Dental Materials and Their Selection. 4th ed. 8. Canada: Quintessence; 2002. p. 218. [Google Scholar]
- 25.Bagheri R. Film thickness and flow properties of resin-based cements at different temperatures. J Dent (Shiraz) 2013;14:57–63. [PMC free article] [PubMed] [Google Scholar]
- 26.Vaidyanathan TK, Vaidyanathan J. Recent advances in the theory and mechanism of adhesive resin bonding to dentin: A critical review. J Biomed Mater Res B Appl Biomater. 2009;88:558–78. doi: 10.1002/jbm.b.31253. [DOI] [PubMed] [Google Scholar]
- 27.Ames WB. A new oxyphosphate for crown setting. Dent Cosmos. 1892;34:392–3. [PMC free article] [PubMed] [Google Scholar]
- 28.Smith DC. A new dental cement. Br Dent J. 1967;123:540–1. [PubMed] [Google Scholar]
- 29.Xu X, Burgess JO. Compressive strength, fluoride release and recharge of fluoride-releasing materials. Biomaterials. 2003;24:2451–61. doi: 10.1016/s0142-9612(02)00638-5. [DOI] [PubMed] [Google Scholar]
- 30.Butz F, Lennon AM, Heydecke G, Strub JR. Survival rate and fracture strength of endodontically treated maxillary incisors with moderate defects restored with different post-and-core systems: An in vitro study. Int J Prosthodont. 2001;14:58–64. [PubMed] [Google Scholar]
- 31.Bearden LJ, Cooke FW. Growth inhibition of cultured fibroblasts by cobalt and nickel. J Biomed Mater Res. 1980;14:289–309. doi: 10.1002/jbm.820140310. [DOI] [PubMed] [Google Scholar]
- 32.Ahmad I. Yttrium-partially stabilized zirconium dioxide posts: An approach to restoring coronally compromised nonvital teeth. Int J Periodontics Restorative Dent. 1998;18:454–65. [PubMed] [Google Scholar]
- 33.De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater. 2004;20:963–71. doi: 10.1016/j.dental.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Hikita K, Van Meerbeek B, De Munck J, Ikeda T, Van Landuyt K, Maida T, et al. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater. 2007;23:71–80. doi: 10.1016/j.dental.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 35.Abo-Hamar SE, Hiller KA, Jung H, Federlin M, Friedl KH, Schmalz G. Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin Oral Investig. 2005;9:161–7. doi: 10.1007/s00784-005-0308-5. [DOI] [PubMed] [Google Scholar]
- 36.Bouillaguet S, Degrange M, Cattani M, Godin C, Meyer JM. Bonding to dentin achieved by general practitioners. Schweiz Monatsschr Zahnmed. 2002;112:1006–11. [PubMed] [Google Scholar]
- 37.Bonfante G, Kaizer OB, Pegoraro LF, do Valle AL. Tensile bond strength of glass fiber posts luted with different cements. Braz Oral Res. 2007;21:159–64. doi: 10.1590/s1806-83242007000200011. [DOI] [PubMed] [Google Scholar]
- 38.Um CM, Oilo G. The effect of early water contact on glass-ionomer cements. Quintessence Int. 1992;23:209–14. [PubMed] [Google Scholar]
- 39.White SN, Yu Z, Tom JF, Sangsurasak S. In vivo microleakage of luting cements for cast crowns. J Prosthet Dent. 1994;71:333–8. doi: 10.1016/0022-3913(94)90090-6. [DOI] [PubMed] [Google Scholar]
- 40.Yu H, Li Q, Cheng H, Wang Y. The effects of temperature and bleaching gels on the properties of tooth-colored restorative materials. J Prosthet Dent. 2011;105:100–7. doi: 10.1016/S0022-3913(11)60007-3. [DOI] [PubMed] [Google Scholar]
- 41.Yu H, Buchalla W, Cheng H, Wiegand A, Attin T. Topical fluoride application is able to reduce acid susceptibility of restorative materials. Dent Mater J. 2012;31:433–42. doi: 10.4012/dmj.2011-106. [DOI] [PubMed] [Google Scholar]
- 42.Sanvin JF, de Rijk WG. Dental cements. Inside Dent. 2006;2:42–7. [Google Scholar]
- 43.Casselli DS, Martins LR. Postoperative sensitivity in Class I composite resin restorations in vivo . J Adhes Dent. 2006;8:53–8. [PubMed] [Google Scholar]
- 44.Frankenberger R, Krämer N, Petschelt A. Technique sensitivity of dentin bonding: Effect of application mistakes on bond strength and marginal adaptation. Oper Dent. 2000;25:324–30. [PubMed] [Google Scholar]
- 45.De Munck J, Shirai K, Yoshida Y, Inoue S, Van Landuyt K, Lambrechts P, et al. Effect of water storage on the bonding effectiveness of 6 adhesives to Class I cavity dentin. Oper Dent. 2006;31:456–65. doi: 10.2341/05-57. [DOI] [PubMed] [Google Scholar]
- 46.Van Meerbeek B, Van Landuyt K, De Munck J, Hashimoto M, Peumans M, Lambrechts P, et al. Technique-sensitivity of contemporary adhesives. Dent Mater J. 2005;24:1–13. doi: 10.4012/dmj.24.1. [DOI] [PubMed] [Google Scholar]
- 47.Christensen GJ. Solving the frustrations of crown cementation. J Am Dent Assoc. 2002;133:1121–2. doi: 10.14219/jada.archive.2002.0339. [DOI] [PubMed] [Google Scholar]
- 48.Christensen GJ. Should resin cements be used for every cementation? J Am Dent Assoc. 2007;138:817–9. doi: 10.14219/jada.archive.2007.0271. [DOI] [PubMed] [Google Scholar]
- 49.Trajtenberg CP, Caram SJ, Kiat-amnuay S. Microleakage of all-ceramic crowns using self-etching resin luting agents. Oper Dent. 2008;33:392–9. doi: 10.2341/07-101. [DOI] [PubMed] [Google Scholar]
- 50.Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, et al. Adhesion to enamel and dentin; 2003. Oper Dent 2003;28:215-35; pp. 215–35. [PubMed] [Google Scholar]
- 51.Seggara M, Seggara A. Practical Clinical Guide to Resin Cements. 1, 2, 3, 4. Heidelberg, Berlin: Springer; 2015. [Last accessed on 2022 Jan 12]. Was available on from: https://link.springer.com/book/10.1007/978-3-662-43842-8 . [Google Scholar]
- 52.Kishimoto M, Shillingburg HT, Jr, Duncanson MG., Jr Influence of preparation features on retention and resistance Part I: MOD onlays. J Prosthet Dent. 1983;49:35–9. doi: 10.1016/0022-3913(83)90234-2. [DOI] [PubMed] [Google Scholar]
- 53.Edelhoff D, Liebermann A, Beuer F, Stimmelmayr M, Güth JF. Minimally invasive treatment options in fixed prosthodontics. Quintessence Int. 2016;47:207–16. doi: 10.3290/j.qi.a35115. [DOI] [PubMed] [Google Scholar]
- 54.Carvalho RM, Pegoraro TA, Tay FR, Pegoraro LF, Silva NR, Pashley DH. Adhesive permeability affects coupling of resin cements that utilise self-etching primers to dentine. J Dent. 2004;32:55–65. doi: 10.1016/j.jdent.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 55.Simon JF, De Rijk WG. Dental cements. Inside Dent. 2006;2:42–7. [Google Scholar]
- 56.Swift EJ, Jr, Bayne SC. Shear bond strength of a new one-bottle dentin adhesive. Am J Dent. 1997;10:184–8. [PubMed] [Google Scholar]
- 57.Peumans M, Kanumilli P, De Munck J, Van Landuyt K, Lambrechts P, Van Meerbeek B. Clinical effectiveness of contemporary adhesives: A systematic review of current clinical trials. Dent Mater. 2005;21:864–81. doi: 10.1016/j.dental.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 58.Perdigão J, Frankenberger R, Rosa BT, Breschi L. New trends in dentin/enamel adhesion. Am J Dent. 2000;13:25D–30D. [PubMed] [Google Scholar]
- 59.Asthana G, Parmar G. Hybrid layer: Foundation of dental bonding. J Gov Dent Coll Hosp. 2014;01:46–50. [Google Scholar]
- 60.de Oliveira Ferraz LC, Ubaldini AL, de Oliveira BM, Neto AM, Sato F, Baesso ML, et al. Analytical method to estimate resin cement diffusion into dentin. J Biomed Opt. 2016;21:55003. doi: 10.1117/1.JBO.21.5.055003. [DOI] [PubMed] [Google Scholar]
- 61.Radovic I, Monticelli F, Goracci C, Vulicevic ZR, Ferrari M. Self-adhesive resin cements: A literature review. J Adhes Dent. 2008;10:251–8. [PubMed] [Google Scholar]
- 62.Vaz RR, Hipólito VD, D'Alpino PH, Goes MF. Bond strength and interfacial micromorphology of etch-and-rinse and self-adhesive resin cements to dentin. J Prosthodont. 2012;21:101–11. doi: 10.1111/j.1532-849X.2011.00794.x. [DOI] [PubMed] [Google Scholar]
- 63.Aguiar TR, Andre CB, Arrais CA, Bedran-Russo AK, Giannini M. Micromorphology of resin-dentin interfaces using self-adhesive and conventional resin cements: A confocal laser and scanning electron microscope analysis. Int J Adh Adhes. 2012;38:69–74. [Google Scholar]
- 64.Aguiar TR, Vermelho PM, André CB, Giannini M. Interfacial ultramorphology evaluation of resin luting cements to dentin: A correlative scanning electron microscopy and transmission electron microscopy analysis. Microsc Res Tech. 2013;76:1234–9. doi: 10.1002/jemt.22290. [DOI] [PubMed] [Google Scholar]
- 65.Al-Assaf K, Chakmakchi M, Palaghias G, Karanika-Kouma A, Eliades G. Interfacial characteristics of adhesive luting resins and composites with dentine. Dent Mater. 2007;23:829–39. doi: 10.1016/j.dental.2006.06.023. [DOI] [PubMed] [Google Scholar]
- 66.Bitter K, Perdigão J, Exner M, Neumann K, Kielbassa A, Sterzenbach G. Reliability of fiber post bonding to root canal dentin after simulated clinical function in vitro . Oper Dent. 2012;37:397–405. doi: 10.2341/11-066-L. [DOI] [PubMed] [Google Scholar]
- 67.Ozer F, Blatz MB. Self-etch and etch-and-rinse adhesive systems in clinical dentistry. Compend Contin Educ Dent. 2013;34:12–4, 16, 18. [PubMed] [Google Scholar]
- 68.Zorba YO, Erdemir A, Turkyilmaz A, Eldeniz AU. Effects of different curing units and luting agents on push-out bond strength of translucent posts. J Endod. 2010;36:1521–5. doi: 10.1016/j.joen.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 69.Radovic I, Mazzitelli C, Chieffi N, Ferrari M. Evaluation of the adhesion of fiber posts cemented using different adhesive approaches. Eur J Oral Sci. 2008;116:557–63. doi: 10.1111/j.1600-0722.2008.00577.x. [DOI] [PubMed] [Google Scholar]
- 70.Bitter K, Meyer-Lueckel H, Priehn K, Kanjuparambil JP, Neumann K, Kielbassa AM. Effects of luting agent and thermocycling on bond strengths to root canal dentine. Int Endod J. 2006;39:809–18. doi: 10.1111/j.1365-2591.2006.01155.x. [DOI] [PubMed] [Google Scholar]
- 71.Fernandes AS, Dessai GS. Factors affecting the fracture resistance of post-core reconstructed teeth: A review. Int J Prosthodont. 2001;14:355–63. [PubMed] [Google Scholar]
- 72.Dangra Z, Gandhewar M. All about dowels – A review part I. Considerations before cementation. J Clin Diagn Res. 2017;11:ZG06–11. doi: 10.7860/JCDR/2017/26472.10518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Garg A, Garg N. Textbook of Endodontics. 4th ed. 27. India, New Delhi: Japee Brothers Medical Publishers; 2018. pp. 406–27. [Google Scholar]
- 74.Radke RA, Barkhordar RA, Podesta RE. Retention of cast endodontic posts: Comparison of cementing agents. J Prosthet Dent. 1988;59:318–20. doi: 10.1016/0022-3913(88)90181-3. [DOI] [PubMed] [Google Scholar]
- 75.Schwartz RS, Murchison DF, Walker WA., 3rd Effects of eugenol and noneugenol endodontic sealer cements on post retention. J Endod. 1998;24:564–7. doi: 10.1016/S0099-2399(98)80079-4. [DOI] [PubMed] [Google Scholar]
- 76.Ertugrul HZ, Ismail YH. An in vitro comparison of cast metal dowel retention using various luting agents and tensile loading. J Prosthet Dent. 2005;93:446–52. doi: 10.1016/j.prosdent.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 77.Panavia TM. F2.0. Kuraray Noritake. Germany, Hattersheim: 2020. Was available on 12 January 2022 from: https://www.kuraraynoritake.eu/en/panavia-f-2-0 . [Google Scholar]
- 78.Baba NZ, Golden G, Goodacre CJ. Nonmetallic prefabricated dowels: A review of compositions, properties, laboratory, and clinical test results. J Prosthodont. 2009;18:527–36. doi: 10.1111/j.1532-849X.2009.00464.x. [DOI] [PubMed] [Google Scholar]
- 79.Ricketts D, Bartlett DW. 7. Edinburgh, New York: Elsevier; 2011. Advanced Operative Dentistry: A Practical Approach; p. 96. Was available on 12 January 2022 from: https://www.elsevier.com/books/advanced-operative-dentistry/9780702031267 . [Google Scholar]
- 80.Koutayas SO, Kern M. All-ceramic posts and cores: The state of the art. Quintessence Int. 1999;30:383–92. [PubMed] [Google Scholar]
- 81.Ferrari M, Vichi A, Mannocci F, Mason PN. Retrospective study of the clinical performance of fiber posts. Am J Dent. 2000;13:9B–13B. [PubMed] [Google Scholar]
- 82.Bandéca MC, El-Mowafy O, Shebl A, Porto-Neto SD. Nonmetallic post-endodontic restorations: A systematic review. Int J Dent. 2010;9:57–62. [Google Scholar]
- 83.Mannocci F, Ferrari M, Watson TF. Intermittent loading of teeth restored using quartz fiber, carbon-quartz fiber, and zirconium dioxide ceramic root canal posts. J Adhes Dent. 1999;1:153–8. [PubMed] [Google Scholar]
- 84.Standlee JP, Caputo AA, Hanson EC. Retention of endodontic dowels: Effects of cement, dowel length, diameter, and design. J Prosthet Dent. 1978;39:400–5. doi: 10.1016/s0022-3913(78)80156-5. [DOI] [PubMed] [Google Scholar]
- 85.Hulbert SF, Morrison SJ, Klawitter JJ. Tissue reaction to three ceramics of porous and non-porous structures. J Biomed Mater Res. 1972;6:347–74. doi: 10.1002/jbm.820060505. [DOI] [PubMed] [Google Scholar]
- 86.Porter DL, Heuer AH. Mechanisms of toughening partially stabilized zirconia (PSZ) J Am Ceram Soc. 1977;60:183–4. [Google Scholar]
- 87.Ichikawa Y, Akagawa Y, Nikai H, Tsuru H. Tissue compatibility and stability of a new zirconia ceramic in vivo . J Prosthet Dent. 1992;68:322–6. doi: 10.1016/0022-3913(92)90338-b. [DOI] [PubMed] [Google Scholar]
- 88.Nasser SA, Moaleem MM, Hussain AA. Tooth colored post system; review of literature. Int J Contemp Dent. 2013;4:50–6. [Google Scholar]
- 89.Raigrodski AJ, Chiche GJ, Potiket N, Hochstedler JL, Mohamed SE, Billiot S, et al. The efficacy of posterior three-unit zirconium-oxide-based ceramic fixed partial dental prostheses: A prospective clinical pilot study. J Prosthet Dent. 2006;96:237–44. doi: 10.1016/j.prosdent.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 90.Al-harbi F, Nathanson D. In vitro assessment of retention of four esthetic dowels to resin core foundation and teeth. J Prosthet Dent. 2003;90:547–55. doi: 10.1016/j.prosdent.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 91.Perdigão J, Geraldeli S, Lee IK. Push-out bond strengths of tooth-colored posts bonded with different adhesive systems. Am J Dent. 2004;17:422–6. [PubMed] [Google Scholar]
- 92.Cohen BI, Pagnillo MK, Newman I, Musikant BL, Deutsch AS. Retention of a core material supported by three post head designs. J Prosthet Dent. 2000;83:624–8. [PubMed] [Google Scholar]
- 93.Dietschi D, Romelli M, Goretti A. Adaptation of adhesive posts and cores to dentin after fatigue testing. Int J Prosthodont. 1997;10:498–507. [PubMed] [Google Scholar]
- 94.Usumez A, Hamdemirci N, Koroglu BY, Simsek I, Parlar O, Sari T. Bond strength of resin cement to zirconia ceramic with different surface treatments. Lasers Med Sci. 2013;28:259–66. doi: 10.1007/s10103-012-1136-x. [DOI] [PubMed] [Google Scholar]
- 95.Marchan S, Coldero L, Whiting R, Barclay S. In vitro evaluation of the retention of zirconia-based ceramic posts luted with glass ionomer and resin cements. Braz Dent J. 2005;16:213–7. doi: 10.1590/s0103-64402005000300008. [DOI] [PubMed] [Google Scholar]
- 96.Subaşı MG, Inan Ö. Influence of surface treatments and resin cement selection on bonding to zirconia. Lasers Med Sci. 2014;29:19–27. doi: 10.1007/s10103-012-1221-1. [DOI] [PubMed] [Google Scholar]
- 97.Bergoli CD, Amaral M, Boaro LC, Braga RR, Valandro LF. Fiber post cementation strategies: Effect of mechanical cycling on push-out bond strength and cement polymerization stress. J Adhes Dent. 2012;14:471–8. doi: 10.3290/j.jad.a28389. [DOI] [PubMed] [Google Scholar]
- 98.Amaral M, Santini MF, Wandscher V, Amaral R, Valandro LF. An in vitro comparison of different cementation strategies on the pull-out strength of a glass fiber post. Oper Dent. 2009;34:443–51. doi: 10.2341/08-113. [DOI] [PubMed] [Google Scholar]
- 99.Bitter K, Paris S, Pfuertner C, Neumann K, Kielbassa AM. Morphological and bond strength evaluation of different resin cements to root dentin. Eur J Oral Sci. 2009;117:326–33. doi: 10.1111/j.1600-0722.2009.00623.x. [DOI] [PubMed] [Google Scholar]
- 100.Marques de Melo R, Galhano G, Barbosa SH, Valandro LF, Pavanelli CA, Bottino MA. Effect of adhesive system type and tooth region on the bond strength to dentin. J Adhes Dent. 2008;10:127–33. [PubMed] [Google Scholar]
- 101.Valandro LF, Filho OD, Valera MC, de Araujo MA. The effect of adhesive systems on the pullout strength of a fiberglass-reinforced composite post system in bovine teeth. J Adhes Dent. 2005;7:331–6. [PubMed] [Google Scholar]
- 102.Wang Z, Ji Y, Zhang F. Bond strengths of an epoxy resin-based fiber post with four adhesive systems. Quintessence Int. 2010;41:e173–80. [PubMed] [Google Scholar]
- 103.Catalogue of Restorative Products. RDT Dental. France: 2020. [Last accessed on 2020 May 12]. p. 12, 28. Was available on from: https://www.rtddental.com/media/files/documents/RTD-Catalog2020_DIGITAL-version.pdf . [Google Scholar]
- 104.Cheung W. A review of the management of endodontically treated teeth.Post, core and the final restoration. J Am Dent Assoc. 2005;136:611–9. doi: 10.14219/jada.archive.2005.0232. [DOI] [PubMed] [Google Scholar]
- 105.Sirimai S, Riis DN, Morgano SM. An in vitro study of the fracture resistance and the incidence of vertical root fracture of pulpless teeth restored with six post-and-coresystems. J Prosthet Dent. 1999;81:262–9. doi: 10.1016/s0022-3913(99)70267-2. [DOI] [PubMed] [Google Scholar]
- 106.Newman MP, Yaman P, Dennison J, Rafter M, Billy E. Fracture resistance of endodontically treated teeth restored with composite posts. J Prosthet Dent. 2003;89:360–7. doi: 10.1067/mpr.2003.75. [DOI] [PubMed] [Google Scholar]
- 107.Schmitter M, Huy C, Ohlmann B, Gabbert O, Gilde H, Rammelsberg P. Fracture resistance of upper and lower incisors restored with glass fiber reinforced posts. J Endod. 2006;32:328–30. doi: 10.1016/j.joen.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 108.Cormier CJ, Burns DR, Moon P. In vitro comparison of the fracture resistance and failure mode of fiber, ceramic, and conventional post systems at various stages of restoration. J Prosthodont. 2001;10:26–36. doi: 10.1111/j.1532-849x.2001.00026.x. [DOI] [PubMed] [Google Scholar]
- 109.Sorrentino R, Salameh Z, Zarone F, Tay FR, Ferrari M. Effect of post-retained composite restoration of MOD preparations on the fracture resistance of endodontically treated teeth. J Adhes Dent. 2007;9:49–56. [PubMed] [Google Scholar]
- 110.Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: A systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies) Quintessence Int. 2008;39:117–29. [PubMed] [Google Scholar]
- 111.Usumez A, Cobankara FK, Ozturk N, Eskitascioglu G, Belli S. Microleakage of endodontically treated teeth with different dowel systems. J Prosthet Dent. 2004;92:163–9. doi: 10.1016/j.prosdent.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 112.Almohareb T. Sealing ability of esthetic post and core systems. J Contemp Dent Pract. 2017;18:627–32. doi: 10.5005/jp-journals-10024-2096. [DOI] [PubMed] [Google Scholar]
- 113.Eskitaşcioğlu G, Belli S, Kalkan M. Evaluation of two post core systems using two different methods (fracture strength test and a finite elemental stress analysis) J Endod. 2002;28:629–33. doi: 10.1097/00004770-200209000-00001. [DOI] [PubMed] [Google Scholar]
- 114.Zalkind M, Hochman N. Direct core buildup using a preformed crown and prefabricated zirconium oxide post. J Prosthet Dent. 1998;80:730–2. doi: 10.1016/s0022-3913(98)70062-9. [DOI] [PubMed] [Google Scholar]
- 115.Michalakis KX, Hirayama H, Sfolkos J, Sfolkos K. Light transmission of posts and cores used for the anterior esthetic region. Int J Periodontics Restorative Dent. 2004;24:462–9. doi: 10.11607/prd.00.0599. [DOI] [PubMed] [Google Scholar]
- 116.Akkayan B. An in vitro study evaluating the effect of ferrule length on fracture resistance of endodontically treated teeth restored with fiber-reinforced and zirconia dowel systems. J Prosthet Dent. 2004;92:155–62. doi: 10.1016/j.prosdent.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 117.Rosato DV, Rosato DV. Reinforced Plastics Handbook. 3rd ed. 2. UK, Kidlington: Elsevier; 2004. p. 41. [Google Scholar]
- 118.Lamichhane A, Xu C, Zhang FQ. Dental fiber-post resin base material: A review. J Adv Prosthodont. 2014;6:60–5. doi: 10.4047/jap.2014.6.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Jain M, Vinayak V. Post-endodontic rehabilitation using glass fiber non metallic posts: A review. Indian J Stomatol. 2011;2:117–9. [Google Scholar]
- 120.Catalogue of GC America INC. Product. Camerica. America: 2019. p. 55. Was available on 12 January 2022 from: https://www.gcamerica.com/catalog/2022/GCA_Catalog_2022.pdf . [Google Scholar]
- 121.Catalogue of PREMIUM. Sweden and Martina Implantology. Germany: 2007. p. 70. Was available on 12 January 2022 from: https://www.sweden-martina.com/articms/admin/reserved_area_file/129/c-imp-premium-usa%20rev. 01-16%20LR.pdf . [Google Scholar]
- 122.Catalogue of ParaPost System. ColtèneWhaledent Inc. Switzerland/Altstätten: 2022. p. 8, 15. Was available on 12 January 2022 from: https://nam.coltene.com/pim/DOC/BRO/docbro31575a-03-19-en-parapost-x-system-brochuresenaindv1.pdf . [Google Scholar]
- 123.Catalogue of Dentatus Classic Surtex Dental Posts. Dentatus. Sweden: 2018. [Last accessed on 2022 Jan 12]. p. 1. Was available on from: https://dentatus.com/products/post-systems/surtex . [Google Scholar]
- 124.Panavia TM. F 2.0. Kuraray Noritake. Germany, Hattersheim: 2020. Was available on 12 January 2022 from: https://www.kuraraynoritake.eu/en/panavia-f-2-0 . [Google Scholar]
- 125.Catalogue of G-CEM™ Capsule. CG America. America: 2008. Was available on 12 January 2022 from: https://www.gcamerica.com/products/operatory/G-CEM_Capsule/ [Google Scholar]
- 126.Catalogue of Multilink Spee. Ivoclar Vivadent. Liechtenstein, Schaan. [Last accessed on 2020 May 12]. Was available on from: http://asia.ivoclarvivadent.com/en-as/all-products/products/luting-material/self-adhesive-resin-cement/multilink-speed .
- 127.Catalogue of TENAX® Fiber Trans. ColtèneWhaledent. Switzerland, Altstätten: 2017. p. 82, 87. Was available on 12 January 2022 from: https://global.coltene.com/pim/DOC/IFU/docifu11-18-30004079d-tenax-fiber-trans-ifu-ltsallaindv1.pdf . [Google Scholar]
- 128.Catalogue of RelyX™ Fiber Post. 3MESPE. USA: 2013. p. 3. Was available on 12 January 2022 from: https://multimedia. 3m.com/mws/media/1146520O/3m-relyx-fiber-post-3d-glass-fiber-post-technical-data-sheet.pdf . [Google Scholar]
- 129.Catalogue of EZ-Fit Translucent. Essential Dental System. New York, America: [Last accessed on 2020 May 12]. Was available on from: http://edsdental.com/ez-fit_translucent/index.htm . [Google Scholar]
- 130.Catalogue of the VDW Endo-System. Vdw-dental. Germany: 2020. p. 53. Was available on 12 January 2022 from: https://www.vdw-dental.com/fileadmin/Dokumente/Service/Informationsmaterial/Kataloge-Broschueren/VDW-Dental-Product-Catalogue-EN.pdf . [Google Scholar]
- 131.Catalogue of CosmoPost Instructions for Use. Ivoclarvivadent. US: 2003. p. 6. Was available on 12 January 2022 from: https://ivodent.hu/__docs/837_b6cd89809faeb9bdb722ae84b8fb4f07.pdf . [Google Scholar]
- 132.Shetty T, Bhat SG, Shetty P. Aesthetic postmaterials. J Indian Prosthodont Soc. 2005;5:122–5. [Google Scholar]
- 133.Catalogue of PinPost. Darby Dental Supply. Penetron: 2016. [Last accessed on 2020 May 12]. p. 657. Was available on from: https://www.darbydental.com/printCatalog/657.pdf . [Google Scholar]
- 134.Catalogue of Dual-Cure Resin Cement/Darby Dental Supply LLC/US (Jerich, NY); 2020. [Last accessed on 2020 May 12]. Was available on from: https://www.darbydental.com/categories/Cements/Permanent/Dual-Cure-Resin-Cement/9430075 .
- 135.Ladha K, Verma M. Conventional and contemporary luting cements: An overview. J Indian Prosthodont Soc. 2010;10:79–88. doi: 10.1007/s13191-010-0022-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Jivraj SA, Kim TH, Donovan TE. Selection of luting agents, part 1. J Calif Dent Assoc. 2006;34:149–60. [PubMed] [Google Scholar]
- 137.Rosenstiel S, Land M. Contemporary Fixed Prosthodontics. 19. Missouri, St. Louis: Mosby; 2015. p. 605, 606. [Google Scholar]
- 138.Catalogue of Gold Standards for Individual Requirements. Degu Dent GmbH. Germany: 2010. [Last accessed on 2020 May 12]. p. 15. Was available on from: https://www.dentsplysirona.com/content/dam/dentsply/pim/manufacturer/Prosthetics/Fixed/Alloys/High_Gold_Alloys/Degunorm/Degunorm-0qbtb5r-en-1402 . [Google Scholar]
- 139.Isidor F, Hassna NM, Josephsen K, Kaaber S. Tensile bond strength of resin-bonded non-precious alloys with chemically and mechanically roughened surfaces. Dent Mater. 1991;7:225–9. doi: 10.1016/S0109-5641(05)80019-3. [DOI] [PubMed] [Google Scholar]
- 140.Ozkurt Z, Işeri U, Kazazoğlu E. Zirconia ceramic post systems: A literature review and a case report. Dent Mater J. 2010;29:233–45. [PubMed] [Google Scholar]
- 141.Goerig AC, Mueninghoff LA. Management of the endodontically treated tooth. Part I: Concept for restorative designs. J Prosthet Dent. 1983;49:340–5. doi: 10.1016/0022-3913(83)90274-3. [DOI] [PubMed] [Google Scholar]
- 142.Sabak SA. Prefabricated post and core material versus custom cast post and core in a maxillary first premolar tooth: Review of literature and management of a clinical case. Cairo Dent J. 1998;14:23–6. [Google Scholar]
- 143.Vichi A, Ferrari M, Davidson CL. Influence of ceramic and cement thickness on the masking of various types of opaque posts. J Prosthet Dent. 2000;83:412–7. doi: 10.1016/s0022-3913(00)70035-7. [DOI] [PubMed] [Google Scholar]
- 144.Dilmener FT, Sipahi C, Dalkiz M. Resistance of three new esthetic post-and-core systems to compressive loading. J Prosthet Dent. 2006;95:130–6. doi: 10.1016/j.prosdent.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 145.Hedlund SO, Johansson NG, Sjögren G. Retention of prefabricated and individually cast root canal posts in vitro . Br Dent J. 2003;195:155–8. doi: 10.1038/sj.bdj.4810405. [DOI] [PubMed] [Google Scholar]
- 146.Vitale MC, Caprioglio C, Martignone A, Marchesi U, Botticelli AR. Combined technique with polyethylene fibers and composite resins in restoration of traumatized anterior teeth. Dent Traumatol. 2004;20:172–7. doi: 10.1111/j.1600-4469.2004.00201.x. [DOI] [PubMed] [Google Scholar]
- 147.Karbhari VM, Strassler H. Effect of fiber architecture on flexural characteristics and fracture of fiber-reinforced dental composites. Dent Mater. 2007;23:960–8. doi: 10.1016/j.dental.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 148.Ricketts DN, Tait CM, Higgins AJ. Post and core systems, refinements to tooth preparation and cementation. Br Dent J. 2005;198:533–41. doi: 10.1038/sj.bdj.4812300. [DOI] [PubMed] [Google Scholar]
- 149.de Rijk WG. Removal of fiber posts from endodontically treated teeth. Am J Dent. 2000;13:19B–21B. [PubMed] [Google Scholar]
- 150.Weine FS, Wax AH, Wenckus CS. Retrospective study of tapered, smooth post systems in place for 10 years or more. J Endod. 1991;17:293–7. doi: 10.1016/S0099-2399(06)81870-4. [DOI] [PubMed] [Google Scholar]
- 151.Walton TR. An up to 15-year longitudinal study of 515 metal-ceramic FPDs: Part 2. Modes of failure and influence of various clinical characteristics. Int J Prosthodont. 2003;16:177–82. [PubMed] [Google Scholar]
- 152.Gholami F, Kohani P, Aalaei S. Effect of nickel-chromium and non-precious gold color alloy cast posts on fracture resistance of endodontically treated teeth. Iran Endod J. 2017;12:303–6. doi: 10.22037/iej.v12i3.10586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pegoraro TA, da Silva NR, Carvalho RM. Cements for use in esthetic dentistry. Dent Clin North Am. 2007;51:453–71, x. doi: 10.1016/j.cden.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 154.Habib B, von Fraunhofer JA, Driscoll CF. Comparison of two luting agents used for the retention of cast dowel and cores. J Prosthodont. 2005;14:164–9. doi: 10.1111/j.1532-849X.2005.00349.x. [DOI] [PubMed] [Google Scholar]
- 155.Duncan JP, Pameijer CH. Retention of parallel-sided titanium posts cemented with six luting agents: An in vitro study. J Prosthet Dent. 1998;80:423–8. doi: 10.1016/s0022-3913(98)70006-x. [DOI] [PubMed] [Google Scholar]
- 156.Chan FW, Harcourt JK, Brockhurst PJ. The effect of post adaptation in the root canal on retention of posts cemented with various cements. Aust Dent J. 1993;38:39–45. doi: 10.1111/j.1834-7819.1993.tb05449.x. [DOI] [PubMed] [Google Scholar]
- 157.Cohen BI, Pagnillo M, Musikant BL, Deutsch AS. Comparison of the retentive and photoelastic properties of two prefabricated endodontic post systems. J Oral Rehabil. 1999;26:488–94. doi: 10.1046/j.1365-2842.1999.00420.x. [DOI] [PubMed] [Google Scholar]
- 158.Lencioni KA, Menani LR, Macedo AP, Ribeiro RF, de Almeida RP. Tensile bond strength of cast commercially pure titanium dowel and cores cemented with three luting agents. J Prosthodont Res. 2010;54:164–7. doi: 10.1016/j.jpor.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 159.Ubaldini AL, Benetti AR, Sato F, Pascotto RC, Medina Neto A, Baesso ML, et al. Challenges in luting fibre posts: Adhesion to the post and to the dentine. Dent Mater. 2018;34:1054–62. doi: 10.1016/j.dental.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 160.Sahmali S, Demirel F, Saygili G. Comparison of in vitro tensile bond strengths of luting cements to metallic and tooth-colored posts. Int J Periodontics Restorative Dent. 2004;24:256–63. [PubMed] [Google Scholar]
- 161.Hagge MS, Wong RD, Lindemuth JS. Retention strengths of five luting cements on prefabricated dowels after root canal obturation with a zinc oxide/eugenol sealer: 1. Dowel space preparation/cementation at one week after obturation. J Prosthodont. 2002;11:168–75. [PubMed] [Google Scholar]
- 162.Menani LR, Ribeiro RF, Antunes RP. Tensile bond strength of cast commercially pure titanium and cast gold-alloy posts and cores cemented with two luting agents. J Prosthet Dent. 2008;99:141–7. doi: 10.1016/S0022-3913(08)60030-X. [DOI] [PubMed] [Google Scholar]
- 163.Cohen BI, Pagnillo MK, Newman I, Musikant BL, Deutsch AS. Retention of three endodontic posts cemented with five dental cements. J Prosthet Dent. 1998;79:520–5. doi: 10.1016/s0022-3913(98)70172-6. [DOI] [PubMed] [Google Scholar]
- 164.Sen D, Poyrazoglu E, Tuncelli B. The retentive effects of pre-fabricated posts by luting cements. J Oral Rehabil. 2004;31:585–9. doi: 10.1111/j.1365-2842.2004.01276.x. [DOI] [PubMed] [Google Scholar]