Abstract
Background:
Remineralizing agents such as fluoride and casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) are popular treatment choices for incipient enamel lesions. Recently introduced resin infiltration enhances the esthetics of teeth affected by these enamel lesions. Furthermore, few studies reported the utilization of colloidal silica infiltration for the white spot lesions. However, the potency of these materials for treatment in primary teeth necessitates investigation.
Thus, this study evaluated and compared the effectiveness of CPP-ACP fluoride (CPP-ACPF), resin infiltration, and colloidal silica infiltration on surface microhardness in artificial white spot lesions in primary incisors using the Vickers microhardness testing machine.
Materials and Methods:
In this in vitro study, on the labial surface of 45 primary incisors, artificial white spot lesions were created by immersing them in a demineralizing solution. According to the evaluation method, random distribution of specimens into three groups: Group 1: CPP-ACPF, Group 2: resin infiltration, and Group 3: colloidal silica infiltration. Specimens after treatment were stored in artificial saliva, followed by microhardness evaluation using Vickers microhardness. Microhardness readings at baseline, post demineralization, and after treating them with different materials were taken. The level of significance was 0.01.
Results:
Enamel specimens treated with resin infiltration showed a high microhardness mean value compared to CPP-ACPF and colloidal silica infiltration.
Conclusion:
Resin infiltration is a promising and effective treatment option for incipient enamel lesions followed by CPP-ACPF compared to colloidal silica infiltration in primary teeth.
Key Words: Demineralization, dental white spots, icon, infiltration, primary teeth
INTRODUCTION
Dental caries, a widespread disease, involve alterations in the apatite crystals of enamel to create visible white spot lesions or initial enamel caries, followed by dentin involvement and consequently cavitation.[1] These chalky manifestations of initial enamel caries are an irregularity amid the biological mineralization activity presented by the mineral content loss from the enamel subsurface and surface and usually an esthetic concern for patients and parents.[1,2] The primary treatment procedure of initial or noncavitated caries is remineralization. The available treatment options include varnish, pastes, and topical remineralizing methods such as fluoride therapy.[3] However, these treatment alternatives have constraints as no instant results are present, demand patient compliance, and stains from external sources might incorporate into the lesions at remineralization. Furthermore, remineralization occurs superficially, while the lesion internally continues to remain porous, thus revealing unpredictable results and persistent whitish discoloration. The lesions treatment should enhance the esthetics and inhibit caries progression.[4] Conservative esthetic procedures demand no tooth removal, and it is achieved by “minimal intervention dentistry.”[3] This minimal approach defines the least invasive treatment of smooth surface and noncavitated approximal carious lesions.[5] Such microinvasive artificial caries treatment recently has shown a notable reduction in enamel mineral loss following the demineralization and arrest of lesions compared to untreated ones.[6] It can treat caries promptly without drilling.
Increased concentrations of calcium and phosphate ions in casein phosphopeptide-amorphous calcium phosphate (CPP-ACP) complexes stabilize CPP to produce an amorphous nanocomplex that can partially restore the demineralized enamel. In preventive and restorative procedures, intermediary treatment substitutes with low-viscosity light-cure resin infiltration can be assuring for restricting carious enamel lesions in the subsurface lesion. Thus, resin infiltration halts the caries progression by occluding enamel porosities, which serve as pathways for the diffusion of acids and minerals.
Similarly, demineralized dentin treated with colloidal silica nanoparticles depicts a high remineralization potential restoring nearly 20% of the phosphate levels and exhibiting a 16% mineral volume recovery.[4]
The present research compared CPP-ACP fluoride (CPP-ACPF), resin infiltration, and colloidal silica infiltration on surface microhardness of artificial white spot lesions in primary anterior teeth as limited research is available on these product's effects.
MATERIALS AND METHODS
This in vitro study was independently reviewed and approved by the Institutional Ethics Committee of Bharati Vidyapeeth (Deemed to be University), Medical College and Hospital, Sangli.
Materials used in this study are shown in Table 1.
Table 1.
Materials used in the study
| Material | Composition |
|---|---|
| CPP-ACPF(GC tooth mousse plus; GC Corporation, Tokyo, Japan) | CPP-ACP 10%, sodium carboxyl methylcellulose, propylene glycol, silicon dioxide, titanium dioxide, xylitol, flavoring, guar gum, phosphoric acid, zinc oxide, magnesium oxide, ethyl 4-hydroxybenzoate, propyl 4-hydroxybenzoate |
| Resin infiltrate(ICON smooth surface kit; DMG, Hamburg, Germany)- | Icon etch: 15% hydrochloric acid, pyrogenic silicic acid, surface-active substances Icon dry: 99% ethanol Icon infiltrant: Tetraethylene glycol dimethacrylate, initiators, additives |
| Colloidal silica infiltrate(Zephyr Chemicals, Navi Mumbai, Maharashtra) | 29.6 weight percentage suspensionin water pH at 25°C: 10 Average particle diameter: 8.3 nm Stabilizing counter ion: Sodium |
CPP: Casein phosphopeptide, ACP: Amorphous calcium phosphate, ACPF: ACP fluoride,
Methodology with group and subgroups is shown in Figure 1.
Figure 1.
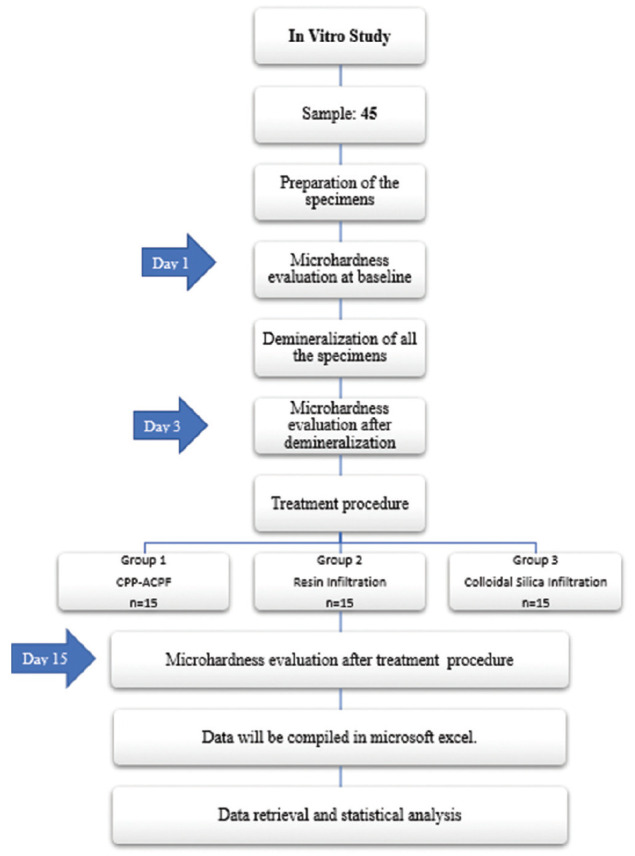
Method with group and subgroups.
Selection of specimen
Forty-five sound human deciduous central incisors indicated for extraction with sound enamel and over-retained incisors were collected and stored in 0.1% thymol solution until further processing. Excluded teeth included carious lesions, discoloration, attrition, restoration, developmental anomalies, hypoplastic defects, fractures, or cracks.
Preparation of the specimen
The teeth were cleaned with pumice slurry and a prophylaxis brush and then decoronated at approximately 1 mm coronal to the cementoenamel junction and embedded with the labial surfaces exposed and parallel to the floor in acrylic resin blocks of 1 × 1 inch diameter and height.
To increase the accuracy of microhardness measurements, smoothening of the enamel surfaces was done with 4000-grit silicon carbide paper, followed by polishing with a 600-grit grinding disk using gamma-alumina polishing gel. All teeth samples were coated with nail varnish, leaving a 2 mm × 2 mm window prepared by placing wax on the buccal surface [Figure 2].
Figure 2.
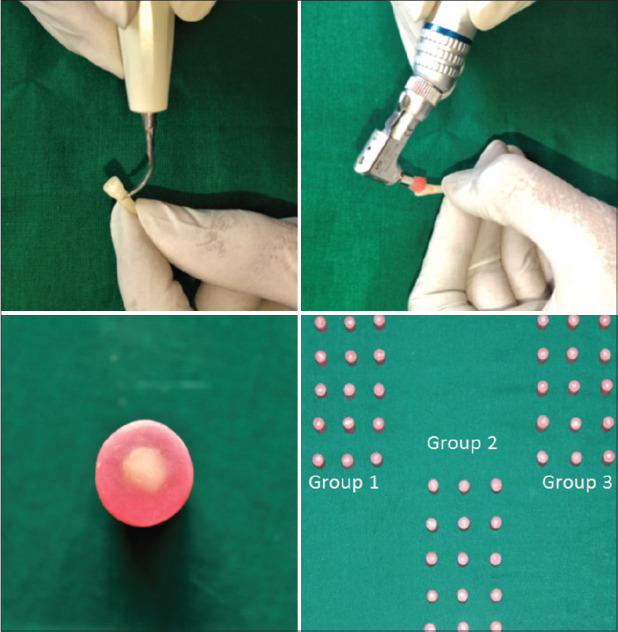
Prepared specimens divided into three groups.
Surface microhardness testing
Vickers microhardness test measured the difference of enamel surface microhardness at baseline and post treatment. The microhardness testing load of 50 g was applied for 10 s as recommended by Prajapati et al.[7] Five indentations, 100 μm apart, were made in the middle of each specimen, and readings noted were averaged. The samples were divided into three groups.
Artificial white spot lesion formation
Artificial lesions formation on enamel specimens was by immersing them in 7.5 ml of lactic acid at 0.1 molar concentration and Carbopol 907 at 0.2%, along with 50% hydroxyapatite saturated in volume, and adjusted to pH 5.0 pH using sodium hydroxide at 37° temperature in an incubator for 72 h, simulating an active area of demineralization.[8] For post demineralization microhardness testing, samples were washed with distilled water and dried. The new measurements were 100 μm below the initial hardness indentations. The average of five indentations with a spacing of 100 μm was considered the final value for surface microhardness post demineralization.
Treatment phase
Group 1 - CPP-ACPF was applied daily to the specimen with a micro brush and kept for 3 min followed by pH cycling.
Group 2 - the specimens were etched with Icon Etch-15% hydrochloric acid gel for 2 min, washed with water spray for 30 s, and dried with icon dry-99% ethanol for 30 s, followed by 10 s of compressed air drying. Icon-infiltrant applied on the specimen's surface for 3 min using an applicator followed by light curing for 40 s. The infiltration application was repeated for 1 min and cured to compensate for the polymerization shrinkage. Finally, the infiltrated specimen's surfaces were polished using the Sof-Lex finishing and polishing kit (3M ESPE, Minnesota, US) to eliminate surface irregularities.
Group 3 - the specimens were immersed in test tubes containing 20 ml of 29.6% colloidal silica suspension for 3 min each daily, followed by pH cycling.
The pH-cycling process [Table 2] was for 15 days with a freshly prepared demineralizing solution. All the specimens were washed with deionized water pre and post demineralization process for 1 min.
Table 2.
pH cycling
| Duration | pH cycling procedure |
|---|---|
| 08.00-09.00 | Demineralization |
| 09.00-09.03 | Treatment materials |
| 09.03-13.00 | Artificial saliva |
| 13.00-14.00 | Demineralization |
| 14.00-14.03 | Treatment materials |
| 14.03-19.00 | Artificial saliva |
| 19.00-20.00 | Demineralization |
| 20.00-20.03 | Treatment materials |
| 20.03-08.00 | Artificial saliva |
On the 15th day, the remineralized specimens' surface microhardness was assessed similarly to the initial microhardness test by considering the five indentations average as the final value for surface microhardness post treatment.
Statistical procedures
Data gathered for surface microhardness were analyzed utilizing IBM SPSS statistics, version 21.0 IBM Corp, Armonk, NY, USA.
For numerical data, descriptive statistics such as mean and standard deviation were used, and the normality of numerical data was verified with the Shapiro–Wilk test. Parametric tests used as data followed a normal curve
Intergroup comparison (>2 groups) done with one-way analysis of variance (ANOVA) followed by pair-wise comparison using post hoc test.
For all the statistical tests, P < 0.05 values were considered significant.
RESULTS
Intergroup comparison of baseline and post demineralization exhibited a statistically nonsignificant difference (P > 0.05) for the values between Group 1 (CPP-ACPF), Group 2 (resin infiltration), and Group 3 (colloidal silica infiltration). The groups, however, recorded an improvement in microhardness following treatment [Table 3]. One-way ANOVA test for intergroup comparison confirmed a statistically significant difference for the values among the three groups (P < 0.01, P < 0.05) post treatment with higher values in Group 2 (resin infiltration) and least in Group 3 (colloidal silica infiltration).
Table 3.
Comparison of mean surface microhardness values
| Variables | Groups | Number of specimens | Mean | SD | F | The P value of one-way ANOVA |
|---|---|---|---|---|---|---|
| Baseline | CPP-ACPF | 15 | 302.230 | 5.664 | 0.630 | 0.538# |
| Resin infiltration | 15 | 304.533 | 6.199 | |||
| Colloidal Silica Infiltration | 15 | 303.843 | 5.409 | |||
| Demineralization | CPP-ACPF | 15 | 174.495 | 1.574 | 0.810 | 0.452# |
| Resin Infiltration | 15 | 174.457 | 1.840 | |||
| Colloidal silica infiltration | 15 | 175.167 | 1.729 | |||
| Post treatment | CPP-ACPF | 15 | 262.938 | 5.152 | 407.951 | 0.000** |
| Resin infiltration | 15 | 283.026 | 6.636 | |||
| Colloidal silica infiltration | 15 | 229.799 | 3.015 |
**Statistically highly significant difference (P<0.01), #Nonsignificant difference (P>0.05). CPP: Casein phosphopeptide, SD: Standard deviation, ACP: Amorphous calcium phosphate, ACPF: ACPF fluoride
The intergroup comparison showed that the resin infiltration group exhibited significantly greater microhardness than the other two groups, i.e., CPP-ACPF and colloidal silica infiltrate [Graph 1].
Graph 1.
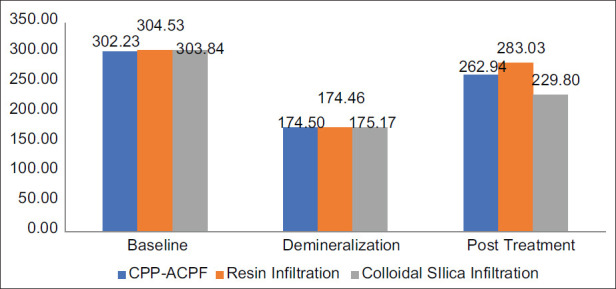
Intergroup comparison of surface microhardness.
DISCUSSION
Preventive procedures for dental decay intend to prevent caries in their initial stages and remineralize the damaged dental surface with materials that decelerate or inhibit cavity development and protect the dental tissue. Thus, fluoride forms the foundation of noninvasive treatment of initial carious lesions; however, its remineralization ability is dependent on the calcium and phosphate ions availability.[9] In a study by Salehzadeh Esfahani et al.,[10] after re-demineralization, the enamel microhardness treated with CPP-ACP denoted significantly higher remineralization than other materials. However, in noncompliant individuals, it is challenging to apply topical fluoride and CPP-ACPF and may cause inadequate mineralization.[1] Therefore, the need for specifically curated treatment regimens is needed to warrant remineralization of initial lesions of enamel and intensify their acid resistance. Thus, considering the association between mineral content and the enamel surface microhardness, the latter can be employed as a criterion to assess the efficiency of various remineralizing materials in preventing the demineralization process and reversing lesions.[9]
Caries infiltration is an innovative procedure alternative intended to bridge the gap in treatable and untreatable procedures.[1] According to Mandava et al.,[4] Kim et al.,[11] and Palmara et al.,[12] the carious lesion's microhardness increased with resin infiltration. Resin infiltration functions by obstructing the enamel diffusion pathways from acids, with a masking effect being an added advantage. Moreover, resin infiltration persevered color stability for nearly 2 months post application.[3] These features indicated resin infiltration as the best-tested technique for the WSLs treatment and are consistent with past studies with effective resistances against further acid challenge and WSLs masking.
Another material studied is the colloidal silica infiltrate. The colloidal silica nanoparticles serve as a scaffold and aid in forming hydroxyapatite crystals and mineralize the dentinal collagen matrix under high pH, thus manifesting mineralization potential. These nanoparticles in the inter- and intrafibrillar collagen spaces diminish the energy barrier, eventually influencing the cluster formation of inorganic ions, enhancing the demineralized specimens after artificial saliva immersion.[4] In a study, Besinis et al.[13] mentioned the higher penetration and remineralization property of colloidal silica nanoparticles due to the tiny particle size compared to nano-hydroxyapatite.
The present study conducted on primary incisors obtained a notable difference in microhardness levels of the three groups. Similarly, in previous research,[10] the mean surface microhardness of samples at baseline and post demineralization was about 303 and 174 VHN, respectively. In other words, although enamels with primary lesions manifested an even surface, their mineral content, and thus microhardness was lower compared to an intact enamel.
The demineralizing formulation used in our study was lactic acid[8] as the ingredients were easily accessible, and also, this step was essential as satisfactory demineralization was a vital requirement for investigating resin infiltration in vitro. Furthermore, to mimic the oral condition, artificial saliva was used as a storage media.[14]
Post treatment, resin infiltration showed a notable improvement in microhardness of lesions followed by CPP-ACPF and least in colloidal silica infiltration. Furthermore, neither treatment material in the current study could restore the surface microhardness of the enamel lesions to the predecalcification levels. The results disagreed with the previous studies.[2,11,12] in which icon resin infiltration restored the artificial enamel lesions' microhardness nearing the sound enamel level. This difference could be due to the effect of pH cycling conducted in our study. Moreover, Uysal et al.[15] reported CPP-ACPF as an effective treatment for remineralizing enamel lesions. Similarly, Srinivasan et al.,[16] Wu et al.,[17] and Jayarajan et al.[18] proved the efficiency of CPP-ACPF in the remineralization of white spot lesions. However, in our study, CPP-ACPF was not as efficient as resin infiltration in restoring the microhardness of the artificial white spot lesions.
In colloidal silica suspension, 24-h sample immersion was done, which clinically is not possible and differs from the method of application of resin infiltration and CPP-ACPF.[19] Based on earlier studies, results[13,19] improved microhardness nearing the baseline values was anticipated with colloidal silica infiltration. However, the difference in composition of colloidal silica may have contributed to the reduced microhardness values that appeared in this study.
Pancu et al.[20] noted maximum microhardness values with icon resin infiltrant than conventional sealants. Moreover, Torres et al.[2] stated that resin infiltration penetrated the residual crystals spaces of the porous carious lesion and the demineralized tissue and thus enhanced the mechanical strength of the infiltrated surface.
Therefore, resin infiltration proves to be a promising noninvasive approach and an option for both nonoperative and operative treatments. The icon resin infiltration obstructs the caries progression in the lesion and improves the dental tissue hardness and resistance to acid attacks. The current research employed an in vitro model of artificial enamel lesions that limited the validity of the oral environment because, under clinical conditions, the carious lesions infiltrated are deeper.[21]
Hence, further researches are required to verify the efficacy of resin infiltration techniques and clinical application of colloidal silica infiltration under clinical conditions.
CONCLUSION
The resin infiltrant (ICON) can improve the microhardness levels compared to CPP-ACPF and colloidal silica infiltration
Resin infiltration technique can alternately be a microinvasive approach in primary incisors
The management of early enamel carious lesions can be done efficiently by resin infiltration.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
REFERENCES
- 1.Abdel-Hakim SM, Metwalli N, El-Askary F, Wassel M. Microhardness, sem and color change analysis of artificial enamel lesions in primary teeth treated with resin infiltration, CPP-ACP or fluoride gel: An in vitro study. Egypt Dent J. 2016;62:3735–44. [Google Scholar]
- 2.Torres CR, Rosa PC, Ferreira NS, Borges AB. Effect of caries infiltration technique and fluoride therapy on microhardness of enamel carious lesions. Oper Dent. 2012;37:363–9. doi: 10.2341/11-070-L. [DOI] [PubMed] [Google Scholar]
- 3.Prasada KL, Penta PK, Ramya KM. Spectrophotometric evaluation of white spot lesion treatment using novel resin infiltration material (ICON®) J Conserv Dent. 2018;21:531–5. doi: 10.4103/JCD.JCD_52_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mandava J, Reddy YS, Kantheti S, Chalasani U, Ravi RC, Borugadda R, et al. Microhardness and penetration of artificial white spot lesions treated with resin or colloidal silica infiltration. J Clin Diagn Res. 2017;11:C142–6. doi: 10.7860/JCDR/2017/25512.9706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yazkan B, Ermis RB. Effect of resin infiltration and microabrasion on the microhardness, surface roughness and morphology of incipient carious lesions. Acta Odontol Scand. 2018;76:473–81. doi: 10.1080/00016357.2018.1437217. [DOI] [PubMed] [Google Scholar]
- 6.Paris S, Schwendicke F, Seddig S, Müller WD, Dörfer C, Meyer-Lueckel H. Micro-hardness and mineral loss of enamel lesions after infiltration with various resins: Influence of infiltrant composition and application frequency in vitro . J Dent. 2013;41:543–8. doi: 10.1016/j.jdent.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Prajapati D, Nayak R, Pai D, Upadhya N, K Bhaskar V, Kamath P. Effect of resin infiltration on artificial caries: An in vitro evaluation of resin penetration and microhardness. Int J Clin Pediatr Dent. 2017;10:250–6. doi: 10.5005/jp-journals-10005-1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gocmen GB, Yanikoglu F, Tagtekin D, Stookey GK, Schemehorn BR, Hayran O. Effectiveness of some herbals on initial enamel caries lesion. Asian Pac J Trop Biomed. 2016;6:846–50. [Google Scholar]
- 9.Mc Donald RE, Avery DR, Stooky GK, Chin JR, Kowolik JK. Dental caries in child and adolescent. In: Dean JA, Mc Donald RE, Avery DR, editors. Dentistry for the Child and Adolescent. 9th ed. St Louis: Mosby; 2011. pp. 179–80. [Google Scholar]
- 10.Salehzadeh Esfahani K, Mazaheri R, Pishevar L. Effects of treatment with various remineralizing agents on the microhardness of demineralized enamel surface. J Dent Res Dent Clin Dent Prospects. 2015;9:239–45. doi: 10.15171/joddd.2015.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim JH, Son HH, Chang J. Color and hardness changes in artificial white spot lesions after resin infiltration, restorative dentistry and endodontics. Restor Dent Endod. 2012;37:90–5. [Google Scholar]
- 12.Palmara JE, Tyas M, Burrow MF. Resin Infiltrated Artificial Caries Lesions Examined by Polarized Microscopy and Microhardness Tests. Hamburg: DMG; 2010. [Google Scholar]
- 13.Besinis A, van Noort R, Martin N. Remineralization potential of fully demineralized dentin infiltrated with silica and hydroxyapatite nanoparticles. Dent Mater. 2014;30:249–62. doi: 10.1016/j.dental.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 14.Mahmoud HA, Elmayad DM, Ghandour IA. Effects of dental bleaching on caries resistance of human enamel. Cairo Dent J. 2009;25:449–55. [Google Scholar]
- 15.Uysal T, Amasyali M, Koyuturk AE, Ozcan S. Effects of different topical agents on enamel demineralization around orthodontic brackets: An in vivo and in vitro study. Aust Dent J. 2010;55:268–74. doi: 10.1111/j.1834-7819.2010.01233.x. [DOI] [PubMed] [Google Scholar]
- 16.Srinivasan N, Kavitha M, Loganathan SC. Comparison of the remineralization potential of CPP-ACP and CPP-ACP with 900 ppm fluoride on eroded human enamel: An in situ study. Arch Oral Biol. 2010;55:541–4. doi: 10.1016/j.archoralbio.2010.05.002. [DOI] [PubMed] [Google Scholar]
- 17.Wu G, Liu X, Hou Y. Analysis of the effect of CPP-ACP tooth mousse on enamel remineralization by circularly polarized images. Angle Orthod. 2010;80:933–8. doi: 10.2319/110509-624.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jayarajan J, Janardhanam P, Jayakumar P. Efficacy of CPP-ACP and CPP-ACPF on enamel remineralization – An in vitro study using scanning electron microscope and DIAGNOdent. Indian J Dent Res. 2011;22:77–82. doi: 10.4103/0970-9290.80001. [DOI] [PubMed] [Google Scholar]
- 19.Gelani R, Zandona AF, Lippert F, Kamocka MM, Eckert G. In vitro progression of artificial white spot lesions sealed with an infiltrant resin. Oper Dent. 2014;39:481–8. doi: 10.2341/13-202-L. [DOI] [PubMed] [Google Scholar]
- 20.Pancu G, Andrian S, Iovan G, Ghiorghe A, Topoliceanu C, Moldovanu A, et al. Study regarding the assessment of enamel microhardness in incipient carious lesion treated by ICON method. Rom J Oral Rehabil. 2011;3:94–100. [Google Scholar]
- 21.Paris S, Meyer-Lueckel H. Inhibition of caries progression by resin infiltration in situ. Caries Res. 2010;44:47–54. doi: 10.1159/000275917. [DOI] [PubMed] [Google Scholar]


