Abstract
Background
Neonatal units across the world have altered their policies to prevent the spread of infection during the COVID-19 pandemic. Our aim was to report parental experience in two European neonatal units during the pandemic.
Methods
Parents of infants admitted to each neonatal unit were asked to complete a questionnaire regarding their experience during the COVID-19 pandemic. At King’s College Hospital, UK (KCH), data were collected prospectively between June 2020 and August 2020 (first wave). At the Hospital Clínic Barcelona (HCM), data were collected retrospectively from parents whose infants were admitted between September 2020 and February 2021 (second and third wave).
Results
A total of 74 questionnaires were completed (38 from KCH and 36 from HCM). The parents reported that they were fully involved or involved in the care of their infants in 34 (89.4%) responses in KCH and 33 (91.6%) responses in HCM. Quality time spent with infants during the pandemic was more negatively affected at KCH compared with HCM (n=24 (63.2%) vs n=12 (33.3%)). Parents felt either satisfied or very satisfied with the updates from the clinical care team in 30 (79.0%) responses at KCH and 30 (83.4%) responses in HCM. The parents felt that the restrictions negatively affected breast feeding in six (15.8%) responses at KCH and two (5.6%) responses in HCM. Travelling to the hospital was reported overall to be sometimes difficult (39.2%); this did not differ between the two units (14 (36.8%) respondents at KCH and 15 (41.6%) from HCM). Furthermore, the self-reported amount of time spent giving kangaroo care also did not differ between the two countries.
Conclusion
Restrictive policies implemented due to the COVID-19 pandemic had a negative impact on the perception of quality of time spent by parents with their newborns admitted to neonatal units.
Keywords: COVID-19, neonatology
WHAT IS ALREADY KNOWN ON THIS TOPIC
The COVID-19 pandemic has led to restrictive policies across neonatal units.
Parental policies varied between centres and over time, being stricter at the beginning of the pandemic.
WHAT THIS STUDY ADDS
Despite the restrictive policies implemented, satisfaction with the care that infants received and with medical updates remained positive.
Overall time spent in breast feeding and in kangaroo care was affected by the pandemic but there were no differences between different policies.
The use of face masks generated parental anxiety and difficulties in bonding with their babies.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Neonatal units need to find strategies to mitigate the impact of separation on parental experience and bonding if a similar situation occurs in the future.
Introduction
The COVID-19 pandemic forced healthcare systems worldwide to introduce mitigating measures to reduce the impact of the disease. One of the recommendations was that ‘numbers of visitors and visiting periods should be highly restricted’.1 The Royal College of Paediatrics and Child Health (RCPCH) and the British Association of Perinatal Medicine (BAPM) issued guidance to aid policymakers.2 In response, many neonatal intensive care units amended their unit policies to maintain the safety of infants, parents and clinical staff while continuing to promote family integrated care. The universal responses by most healthcare organisations in imposing restrictions particularly in the early stages, however, often did not consider the unique situation that arises with the mother–baby dyad. Furthermore, restrictions associated with the COVID-19 pandemic in relation to healthcare settings should be taken into account by both health professionals and policymakers as described in a recent global survey.3 A recent review suggested that the restrictions implemented by neonatal units during the COVID-19 pandemic increased parent and infant separation and subsequently reduced the establishment of successful breast feeding.4 Furthermore, a joint UK and US survey of parental perceptions on visiting restrictions during the pandemic highlighted that parents reported reduced involvement and bonding experiences with their infant.5 Those findings, together with baseline risks already associated with the perinatal and postnatal periods, could worsen long-term parental mental health when the heightened general anxiety around the pandemic is considered.6 Indeed, parents report visiting restrictions limit their ability to bond and participate in their infant’s care, with concern expressed about receiving insufficient information and medical updates due to restrictions limiting ward round attendance.5 7 8 Furthermore, parents described having unmet requirements for emotional and psychological support and facing difficulties with transport, work and medical expenses following discharge.9
The aim of this observational study was to demonstrate the difference between how two European neonatal units changed their policies for parents during the pandemic and to describe parental satisfaction during this time. Specifically, we wanted to explore common themes experienced by families with infants admitted to intensive care during the pandemic in two healthcare settings in Europe.
Methods
An observational study was undertaken to describe parental experiences in two European neonatal intensive care units during the COVID-19 pandemic. The study was registered as a service evaluation with the Clinical Governance Department of King’s College Hospital (KCH) National Health Service (NHS) Foundation Trust, London, UK and the Legal Department of Hospital Clinic Barcelona (HCM), Barcelona, Spain.
London (KCH)
The neonatal unit at KCH NHS Foundation Trust (London, UK) is a tertiary medical and surgical neonatal unit with an average of 700 annual admissions. It has a total bed capacity of 36, including 12 intensive care cots (ITUs), 12 high dependency care cots (HDUs), 12 special care cots (SCBUs) and an isolation room. In 2020, there were 4266 births with 575 infants admitted to the neonatal unit (13.4%), which was the lowest admission rate in the last 10 years. Of all the admissions, 194 (33.7%) required intensive care, 261 (45.4%) were preterm <37 weeks and 100 (17.4%) weighed less than 1500 g. Nursing staffing ratio was 1:1 to 1:2 in ITU, 1:2 in HDU and 1:4 in SCBU per shift and medical staffing ratio was 1:4 including middle grade doctors and consultants per weekday shift. Parent facilities on-site include a coffee room and a rest area with one rooming-in room. Pre-pandemic parental policies allowed both parents, grandparents, siblings and other family members to visit, with two adults at the cot side at any one time. Changes to the unit policy at KCH during the COVID-19 pandemic were introduced in March 2020 following recommendations from the RCPCH and BAPM. Only one parent could stay with their baby at a time and no siblings (except twins) or other family members could visit. The parents’ facilities including coffee room, rest area and rooming-in room were closed and parents were advised not to congregate in the reception area. Further, parents were advised to practise social distancing and to always wear face masks as per government guidance. The unit continued to remain open for restrictive parental attendance 24/7. Parents were only able to spend time by their own infant’s cot side and advised to bring a separate shirt with them to the unit for kangaroo care. A maximum of four mothers were allowed in the expressing room. Parental craft skills and care such as kangaroo care, nappy changes, skin care, feeding, bathing the baby and temperature measurements were all still actively encouraged. Furthermore, breastfeeding support continued to be available every day of the week. When parents had to self-isolate, videocalls were arranged daily so they could see their baby. During the study period, there were no COVID-19-positive cases in infants admitted to the unit, but three parents tested positive for coronavirus and had to self-isolate.
Barcelona (HCM)
The neonatal unit at Hospital Clinic - Maternity in Barcelona, Spain (HCM) is a tertiary neonatal unit with an average of 550 annual admissions. It has a total bed capacity of 28 including 8 ITUs, 8 HDUs and 12 SCBUs. In 2020, there were 3295 births with 452 infants admitted to the neonatal unit (13.7%). From all the neonatal admissions, 211 (46.7%) required intensive care, 347 (76.7%) were preterm infants (<37 weeks) and 83 (23.9%) weighed less than 1500 g. Nursing staffing ratio was 1:1 to 1:2 in ITU, 1:2 in HDU and 1:4 in SCBU per shift and medical staffing ratio was 1:4 to 1:4.6 including middle grade doctors and consultants per weekday shift. Parent facilities on-site include a coffee room and rest area and there are 15 live video cameras available in the unit for families to see their infant when unable to attend the unit. Pre-pandemic parental policies allowed both parents, grandparents and siblings to enter the unit in groups of two people each time and the unit remained open 24/7. From March 2020, following the Spanish Society of Neonatology (Sociedad Española de Neonatología) (SENEO) recommendations to prevent the spread of COVID-19 infection, a restrictive parental policy was implemented. Only parents could see their baby, one at a time, and they were required to wear a face mask at all times while on the unit. The parent facilities remained open 24/7 but only one family could use the parent room at any one time. From June 2020, a less restrictive parental policy was implemented and both parents could stay with their baby simultaneously, providing they did not have any coronavirus symptoms and had not been in contact with any person who had tested positive. There were no COVID-19-positive cases in babies admitted to the unit or their parents during the study period.
Questionnaire completion
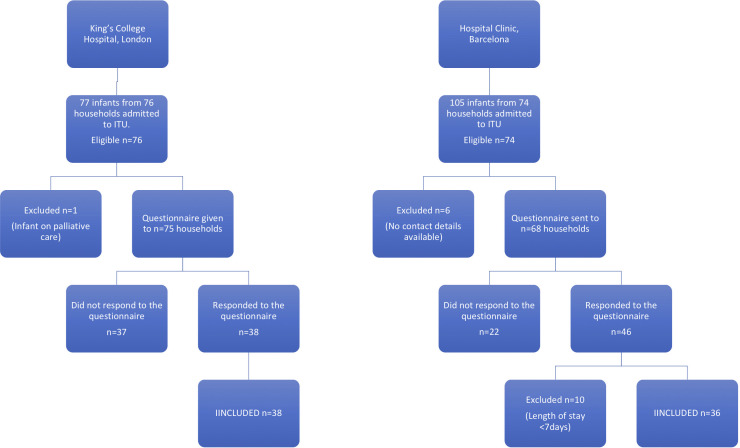
This survey was performed as a service evaluation and improvement project and therefore ethical approval was not sought. Parents were invited to voluntarily participate and understood the aim of the survey. All answers were anonymised, and all patient identifiable information was removed to preserve confidentiality and privacy. The survey was designed by one of the doctors at KCH. A similar neonatal unit in Spain was identified, with the aim to have a broader view of the parental experience during the pandemic. Only one questionnaire was provided per household, so if parents had multiple infants (eg, twins) admitted to the neonatal unit, then they were invited only to participate once. See figure 1 for infant eligibility and inclusion per neonatal unit.
Figure 1.
CONSORT diagram to portray participant inclusion per neonatal unit. CONSORT, Consolidated Standards of Reporting Trials; ITU, intensive care unit.
Parents of infants admitted to KCH neonatal intensive care unit were asked to complete a questionnaire prospectively regarding their experience during the COVID-19 pandemic. The parents were approached by the member of the medical team who was leading the survey, who discussed the aim of the survey with them and, after giving verbal consent, they received a written questionnaire and completed this while their baby was still admitted. Questionnaire responses were anonymised after completion and data collected using a Microsoft Excel spreadsheet.
Families of babies admitted to the HCM in Barcelona are asked to provide contact details and an email address at the beginning of the admission and when they provided it, they consent to be contacted via email. The hospital has a quality and safety management programme (‘ISO 9001’ and ‘UNE179003’) by which questionnaires are sent via the online statistical survey application ‘Lyme Survey’ which meets legal requirements of confidentiality and by completing them, they consent to its final use. Parents of infants admitted to the HCM neonatal intensive care unit were asked retrospectively to complete the same questionnaire used at KCH. One questionnaire was given to each household and completed anonymously.
Parents were eligible to complete the survey if their infant was admitted to the neonatal unit for at least 1 week. Parents of infants receiving palliative care were excluded from the study. The questionnaire contained only six questions aimed at assessing parental experience during the pandemic, and hence would be rapid and burden free for parents to complete. The questionnaire considered specific COVID-19 guidance laid out by the RCPCH, BAPM, SENEO and the neonatal charity Bliss. Furthermore, parents were also requested to give free-text recommendations as to how the service could be improved during the pandemic.
At KCH, data were collected prospectively over a 6-week period, between 25 June 2020 and 5 August 2020 (first wave). At HCM, the data were collected retrospectively from parents whose infants were admitted between 22 September 2020 and 28 February 2021 (second and third wave) and when less restrictive parental policies were in place.
Patient and public involvement
It was not possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research due to the unpredictable nature of the COVID-19 pandemic and associated restrictions.
Results
A total of 74 questionnaires were analysed, 38 from KCH and 36 from HCM. Just over half of the parents felt fully involved with the care of their infant (n=43; 58.1%); however, this was larger in HCM compared with KCH (n=26 (72.2%) vs n=17 (44.7%)). Quality time spent with infants during the pandemic was more negatively affected in KCH compared with HCM (n=24 (63.2%) vs n=12 (33.3%)). For both countries, 44 (59.5%) respondents reported the pandemic did not affect the time spent breast feeding, and 46 (62.2%) reported giving kangaroo care was mostly unchanged. Parents from both units were satisfied with clinical updates from medical and nursing staff throughout the pandemic. Travelling back and forth to the hospital to see their infant was reported overall to be sometimes difficult in 29 responses (39.2%); however, this was no different in either country (14 from KCH vs 15 at HCM). All infants in both cohorts survived to hospital discharge. See table 1 for parental responses as per each neonatal unit.
Table 1.
Parental responses as per each neonatal unit
| KCH (n=38 (%)) | HCM (n=36 (%)) | |
| How involved do you feel with the care of your baby? | ||
| 1=not at all | 0 (0.0) | 0 (0.0) |
| 2=a little involved | 4 (10.5) | 3 (8.3) |
| 3=quite involved | 17 (44.7) | 7 (19.4) |
| 4=fully involved | 17 (44.7) | 26 (72.2) |
| Do you feel that the pandemic has affected the quality of time you spend with your baby? | ||
| 1=disimproved | 24 (63.2) | 12 (33.3) |
| 2=not at all | 13 (34.2) | 19 (52.8) |
| 3=improved | 1 (2.6) | 4 (11.1) |
| 4=not answered | 0 (0.0) | 1 (2.8) |
| Has the pandemic affected the amount of time you spend giving kangaroo care? | ||
| 1=decreased | 13 (34.2) | 6 (16.7) |
| 2=not at all | 21 (55.3) | 25 (69.4) |
| 3=increased | 0 (0.0) | 2 (5.6) |
| 4=not applicable | 4 (10.5) | 0 (0.0) |
| 5=not answered | 0 (0.0) | 3 (8.3) |
| Has the pandemic affected the amount of time you spend breast feeding? | ||
| 1=decreased | 6 (15.8) | 2 (5.6) |
| 2=not at all | 14 (36.8) | 30 (83.3) |
| 3=increased | 0 (0.0) | 1 (2.8) |
| 4=not applicable | 18 (47.4) | 0 (0.0) |
| 5=not answered | 0 (0.0) | 3 (8.3) |
| Are you satisfied with the updates from the medical and nursing staff regarding your baby? | ||
| 1=very unsatisfied | 1 (2.6) | 4 (11.1) |
| 2=unsatisfied | 1 (2.6) | 0 (0.0) |
| 3=moderately satisfied | 6 (15.8) | 2 (5.6) |
| 4=satisfied | 21 (55.3) | 6 (16.7) |
| 5=very satisfied | 9 (23.7) | 24 (66.7) |
| How have you found coming to the hospital to visit your baby? | ||
| 1=very difficult | 5 (13.2) | 5 (13.9) |
| 2=sometimes difficult | 14 (36.8) | 15 (41.7) |
| 3=manageable | 11 (28.9) | 6 (16.7) |
| 4=easy | 8 (21.1) | 9 (25.0) |
| 5=not answered | 0 (0.0) | 1 (2.8) |
Data are expressed as number with % in brackets.
HCM, Hospital Clinic Barcelona; KCH, King's College Hospital.
The questionnaire incorporated a section where parents could write comments about their experience in the neonatal unit, including any suggestions they had to improve this. The results of the survey were shared in both units and acknowledged as part of service improvement.
KCH comments
Many parents expressed concerns over the restrictions as they worried it would impact on how often they would be able to see their baby and bond with them, although they appreciated the reasons for this. Parents said it was ‘difficult with both parents not visiting together’, felt ‘one parent rule was punishing’ and they ‘could not spend time as a family’. There were mothers who described having less time with their baby so that the fathers could also attend; one said it felt ‘rushed and stressful having to leave so the father can see the baby’. Some parents described the impact it had on their emotional well-being as well as mental health. For instance, one of them said she had ‘severe anxiety and was struggling without her partner’s support’ and another parent said it was ‘very difficult to take turns to see our baby when we were under considerable emotional stress’. Difficulties were expressed balancing home life with frequent visits to the hospital, especially with siblings at home, as prior to the pandemic, siblings could be by the cot side or wait with their relatives and use the family facilities with relatives while waiting. One of them said it was ‘incredibly hard with a sibling not allowed in’. Single parents requested being able to nominate a family member to provide additional support. A comment was made that opportunities to express breast milk were affected by limited spaces in the expressing room due to the need for social distancing. One parent also felt that having less time with the baby reduced feeding opportunities. A few parents voiced that although wearing a face mask was understandable, it also made bonding difficult. They expressed feeling ‘sad’ that their baby had never seen them without a mask. Parents worried that not being able to read their facial expressions might have consequences for the baby’s development. A suggestion was made asking if doctors could offer regular conference calls to allow parents to discuss the medical care of their baby together. Parents said they ‘have been very impressed with the care and felt reassured their baby was in the best hands’, ‘nurses and doctors are very helpful’ and ‘staff do a good job with getting parents stuck in with cares and bonding’. Overall, parents were very happy and thankful for the clinical care and continuous support provided, despite the challenges of the pandemic.
HCM comments
The quality of time parents spent with their infant was reported by one family to have been negatively affected by the pandemic, mostly by the wearing of face masks which did not allow the parents to kiss their baby. Furthermore, quality of time was reported to be reduced by not being able to have other family members visit their infant. Parents did however report finding it particularly exciting seeing their infant’s name coloured on the wall next to their incubator and being able to use cameras to see them at any time.
Discussion
We demonstrate that parents reported the overall quality of time spent with their infant to be reduced, especially when more restrictive policies were in place. This may also be related to the difficulties in travel to the hospital. Concerns were highlighted about parental emotional well-being, feelings of anxiety, bonding as a family and lack of support from partners.
We considered why variation in parental satisfaction between the two countries may exist. Anxiety and apprehension during the first wave were high, with rates of major depressive symptoms in pregnant women within the UK peaking at 42%,10 compared with a lower proportion in Spain reporting such symptoms (38%).11 In our study, parents with infants admitted to neonatal intensive care were asked to respond to the questionnaire during different waves of the pandemic. We speculate that the higher levels of self-reported quality time spent with infants and overall greater parental satisfaction in Barcelona than the UK may be secondary to previously reported lower baseline rates of depressive symptoms in pregnancy within the Spanish population. More so, parents in the UK were also asked to complete the questionnaire when visiting was most restrictive. Such differences in self-reported parental satisfaction within our study agree with a recent UK and US survey which explored varying policies between units, with a greater negative parental impact identified during stricter restrictions.8
Muniraman et al conducted a cross-sectional survey of parents impacted by restrictive policies in six tertiary neonatal units, from the UK and the USA assessing their visitation policies and impact on parents’ ability to see, care for and bond with their infants. In a total of 231 responses, they reported that the policies were perceived as restrictive by 62% of the respondents and 41% reporting being unable to bond enough. Mild to severe impact on breast feeding was reported by 36% (75 of 209) of respondents. Our study generally agrees with the above findings and complements the literature by reporting on two separate populations in two European countries with the Barcelona cohort coming later in time in the pandemic (up to February 2021 compared with August in 2020 in Muniraman et al8).
When considering important outcome-related factors, however, our questionnaire highlights that many parents within both the UK and Spain do not report a reduction in time spent breast feeding or provision of kangaroo care. Over half of our respondents felt kangaroo care was not affected during the pandemic, which may be reflective of less strict restrictions. Indeed, this is much higher in comparison with a recent global survey of parental experiences during the pandemic which found only less than half of respondents reported no change to the frequency of kangaroo care; however, this global survey included some units where neither parent was allowed to visit during the restrictions.3 Furthermore, parental satisfaction in receiving medical updates was not affected regardless of which pandemic restriction policy was employed.
Less restrictive measures were in place during completion of the questionnaire in Barcelona, when both parents were able to stay with their infant. Having both parents at the cot side together may have facilitated kangaroo care, family-integrated care and receiving joint medical updates to both parents simultaneously.
There were many comments made in our study regarding the impact on parental emotional well-being. It is crucial that health professionals remain vigilant in identifying parents who require additional emotional support and signposting them to appropriate organisations.
The availability of live video cameras within the neonatal unit in Spain for when parents were unable to see their infant may have been vital in parents feeling more involved with the care of the infant despite not being physically present. Our survey highlights the importance of incorporating different modalities into our clinical care such as telephone conferencing and secure video messaging. Indeed, one study reported that asynchronous video messaging supported models of family integrated care, improved parental experience and emotional closeness to their baby and built strong relationships between families and staff.12 Furthermore, the use of cot-side cameras has been associated with a reduction in parental stress when infant separation occurs.13 Such advancements in technology may thus be beneficial not only during future pandemics, but also in the provision and delivery of universal, sustainable and accessible neonatal care.
Utilisation of digital innovations as a standard of care when considering service provision and redesign of units may indeed remove some of the barriers and obstacles often currently experienced by parents and healthcare workers in being able to provide and promote family integrated care, and thus such advances may be a beneficial side product of the pandemic.14–16
Mask wearing is a highly effective measure in reducing virus transmission at a population level.17 The use of face masks was a recurring theme expressed by parents from both the UK and Spain. Wearing of face masks by parents while with their infant was identified as a particular source of anxiety in both countries with concern over the impact on bonding. Indeed, there is little knowledge of this with respect to the longer-term consequences on infant neurodevelopment. Wearing of face masks may affect attachment processes between parents and their infant within the first few days of life when there is little exposure to and visualisation of parental facial expressions.18 Suggested recommendation from the RCPCH with specific regard to face mask covering is that consideration for removal should be given for asymptomatic parents when providing kangaroo care.19 Furthermore, use of transparent face masks or visors, alongside regularly talking through the mask, should be encouraged to enable bonding and attachment opportunities.20 Balance of risk must be made however between the unknown adverse impact of face covering on infant neurodevelopment with the global benefits of face masks in reducing virus transmission.
The results of this survey were shared among both units and actions including updating unit policies, parents’ facilities, psychological support on-site and communication with parents that have been taken to improve parental experience and service development. To improve care in both units and determine the benefits of differing approaches to the pandemic, it would be interesting in future studies to conduct the same survey and data collection process in the same units over varying time periods during different restrictive measures of the pandemic.
This study has strengths and some limitations. We have surveyed parents from two tertiary neonatal intensive care units in Europe incorporating two different policies on parental restrictions during the COVID-19 pandemic. Answers from both cohorts of parents, with different restrictions, may therefore be useful in guiding further policies in future pandemics to ensure parental satisfaction is taken into consideration. Data were collected from KCH during the first wave of the pandemic when lockdown restrictions were being enforced, thereby capturing an accurate depiction of parental experience in real time. Contrary to this, data from HCM were collected retrospectively and when less restrictive policies were in place, and as such may have positively impacted the reflections of parents who were at home when completing the form, hence the retrospective nature of the Spanish data collection acts as a limitation to the study. As responses from Spain were anonymous, it was not possible to determine how sick the infants were during admission, or how long post-discharge the surveys were completed and how these influences may have further impacted parental views. Information on whether parents from either country were first-time parents was also not collected. Finally, no control group pre-pandemic was included and we did not have survey responses to assess baseline perception involvement in care pre-pandemic; therefore, how self-reported parental satisfaction may have changed within each country when restrictions and policies were implemented could not be elicited.
The long-term impact of the pandemic on parents and infants admitted to neonatal care is not known.
In conclusion, restrictive policies implemented due to the COVID-19 pandemic have affected families with infants admitted to neonatal intensive care. Quality of time spent with the babies was felt to be significantly affected, especially when more restrictive policies were implemented. Parental involvement in the care of their babies and satisfaction with the care that infants received and with medical and nursing updates, however, remained positive. The amount of time spent breast feeding and giving kangaroo care decreased during the pandemic, but was not significantly different between the two units. Neonatal units need to find strategies to mitigate the impact of separation on parental experience and bonding if a similar situation occurs in the future.
bmjpo-2021-001396supp001.pdf (485.5KB, pdf)
bmjpo-2021-001396supp002.pdf (31.9KB, pdf)
Supplementary Material
Footnotes
Contributors: CZ designed the study, and participated in the analysis of data and the writing of the manuscript. EM participated in the design of the study, data acquisition and analysis, and critically revised the manuscript. MT-P acquired the data from HCM, participated in the analysis and critically reviewed the manuscript. EEW participated in the analysis of data and the writing of the manuscript. VA-B acquired the data from HCM, participated in the analysis and critically reviewed the manuscript. RB participated in the design of the study and critically reviewed the manuscript. AH participated in the design of the study and critically reviewed the manuscript. TD participated in the analysis of data and the writing of the manuscript. AG supervised the project, participated in the design and analysis of the study, and critically revised the manuscript. CZ is acting as guarantor.
Funding: This research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at Guy’s and St Thomas' NHS Foundation Trust and King’s College London.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data are available upon requet and in keeping with ICMJE recommendation.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The Health Research Authority Toolkit of the Medical Research Council, UK confirmed that the study would not be considered as research and would not require regulatory approval by a research ethics committee.
References
- 1.Organisation WH . Maintaining essential health services: operational guidance for the COVID-19 conext interim guidance, 2020: 61. [Google Scholar]
- 2.Neonatologia SEd. . Recommendations for management of newborns for SARS-CoV-2 infection, 2020: 16. [Google Scholar]
- 3.Kostenzer J, Hoffmann J, von Rosenstiel-Pulver C, et al. Neonatal care during the COVID-19 pandemic - a global survey of parents' experiences regarding infant and family-centred developmental care. EClinicalMedicine 2021;39:101056. 10.1016/j.eclinm.2021.101056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Veenendaal NR, Deierl A, Bacchini F, et al. Supporting parents as essential care partners in neonatal units during the SARS-CoV-2 pandemic. Acta Paediatr 2021;110:2008–22. 10.1111/apa.15857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown A, Shenker N. Experiences of breastfeeding during COVID-19: lessons for future practical and emotional support. Matern Child Nutr 2021;17:e1388. 10.1111/mcn.13088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ashini A, Alsoufi A, Elhadi M. Parental perception of neonatal ICU visitation during the COVID-19 pandemic. Int J Gynaecol Obstet 2021;153:554–5. 10.1002/ijgo.13650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Darcy Mahoney A, White RD, Velasquez A, et al. Impact of restrictions on parental presence in neonatal intensive care units related to coronavirus disease 2019. J Perinatol 2020;40:36–46. 10.1038/s41372-020-0753-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muniraman H, Ali M, Cawley P, et al. Parental perceptions of the impact of neonatal unit visitation policies during COVID-19 pandemic. BMJ Paediatr Open 2020;4:e000899. 10.1136/bmjpo-2020-000899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fan J, Zhou M, Wei L, et al. A qualitative study on the psychological needs of hospitalized newborns’ parents during COVID-19 outbreak in China. Iran J Pediatr 2020;30:e102748. 10.5812/ijp.102748 [DOI] [Google Scholar]
- 10.Ceulemans M, Foulon V, Ngo E, et al. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic-A multinational cross-sectional study. Acta Obstet Gynecol Scand 2021;100:1219–29. 10.1111/aogs.14092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brik M, Sandonis MA, Fernández S, et al. Psychological impact and social support in pregnant women during lockdown due to SARS-CoV2 pandemic: a cohort study. Acta Obstet Gynecol Scand 2021;100:1026–33. 10.1111/aogs.14073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kirolos S, Sutcliffe L, Giatsi Clausen M, et al. Asynchronous video messaging promotes family involvement and mitigates separation in neonatal care. Arch Dis Child Fetal Neonatal Ed 2021;106:172–7. 10.1136/archdischild-2020-319353 [DOI] [PubMed] [Google Scholar]
- 13.Guttmann K, Patterson C, Haines T, et al. Parent stress in relation to use of bedside telehealth, an initiative to improve family-centeredness of care in the neonatal intensive care unit. J Patient Exp 2020;7:1378–83. 10.1177/2374373520950927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacSween K, Fraser C, Clinton T, et al. Neonatal healthcare workers' perceptions of the impact of the COVID-19 pandemic. Acta Paediatr 2021;110:2814–6. 10.1111/apa.15994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waddington C, van Veenendaal NR, O'Brien K. International Steering Committee for family integrated C. family integrated care: supporting parents as primary caregivers in the neonatal intensive care unit. Pediatr Investig 2021;5:148–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell-Yeo M, Dol J, Richardson B, et al. A co-design of clinical virtual care pathways to engage and support families requiring neonatal intensive care in response to the COVID-19 pandemic (COVES study). J Neonatal Nurs 2021;27:463–70. 10.1016/j.jnn.2021.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Howard J, Huang A, Li Z, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci U S A 2021;118:e2014564118. 10.1073/pnas.2014564118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green J, Staff L, Bromley P, et al. The implications of face masks for babies and families during the COVID-19 pandemic: a discussion paper. J Neonatal Nurs 2021;27:21–5. 10.1016/j.jnn.2020.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Health RCoPaC . BAPM - COVID-19: Frequently asked questions within neonatal services. RCPCH, 2021. [Google Scholar]
- 20.Verd S, Moll P, Serra C, et al. Mothers’ masks should be improved or removed during pandemic as they inhibit bonding with neonates. Acta Paediatr 2021;110:1689. 10.1111/apa.15497 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2021-001396supp001.pdf (485.5KB, pdf)
bmjpo-2021-001396supp002.pdf (31.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data are available upon requet and in keeping with ICMJE recommendation.