ABSTRACT.
To reduce child mortality in children younger than 5 years, Burkina Faso has been offering free care to this population of children since 2016. The free care program is aligned with the Integrated Management of Childhood Illness (IMCI) guidelines. Given that the number of studies that evaluated the competence of health-care workers (HCWs) during the free care program was limited, we assessed the adherence level of HCWs to the IMCI guidelines in the context of free care. This was a secondary data analysis. Data were obtained from a cross-sectional study conducted from July to September 2020 in 40 primary health-care centers and two district hospitals in the Hauts-Bassins region in Burkina Faso. Our analysis included 419 children younger than 5 years old who were consulted according to IMCI guidelines. Data were collected through direct observation using a checklist. The overall score of adherence of HCWs to IMCI guidelines was 57.8% (95% CI, 42.6–73.0). The mean adherence score of the evaluation of danger signs was 71.9% (95% CI, 58.7–85.1). The mean adherence score of following IMCI guidelines was significantly greater in boys (54.2%) compared with girls (44.6%; P < 0.001). Adherence scores of the performance of different IMCI tasks were significantly different across HCW categories. The overall adherence of HCWs to IMCI guidelines in the context of free care was greater than the adherence reported before the implementation of free care in Burkina Faso. However, this assessment needs to be performed nationwide to capture the overall adherence of HCWs to IMCI guidelines in the context of the free care program.
INTRODUCTION
Considerable reductions in mortality in children younger than 5 years have been reported worldwide.1 From 2000 to 2015, the child mortality rate in those younger than 5 years declined by half, from 138 to 72 deaths/1,000 live births, in sub-Saharan African countries.2
In Burkina Faso, the child mortality rate of those younger than 5 years declined from 179.2 to 87.5 deaths/1,000 live births from 2000 to 2020.3 Although substantial progress has been made, Burkina Faso is far from achieving the sustainable development goal 3.2.2 Thus, more focused efforts, such as increasing access to quality health care for children, are needed to reduce child mortality in those younger than 5 years.4
In 1999, the WHO defined the Integrated Management of Childhood Illnesses (IMCI) as the reference for the care of children younger than 5 years.5,6 Since then, the WHO and the United Nations Children’s Fund have promoted IMCI guidelines for use by health-care workers (HCWs) in health facilities to assess, diagnose, and treat children younger than 5 years.5,6 In Burkina Faso, the IMCI strategy was adopted for the care of children younger than 5 years in primary health-care centers called Centres de Santé et de Promotion Sociale (CSPSs). This systematic approach for providing care to children younger than 5 years includes curative actions provided by HCWs in health-care settings and in the community.
The principles of Burkina Faso’s IMCI strategy constitute the basis of the overall services of the free care program for children younger than 5 years. However, HCW adherence to IMCI guidelines prior to the implementation of free care policies was low. In 2013, 20% of nurses working in primary care facilities were trained in IMCI. Of the 28% of children who were assessed for the three danger signs recommended by IMCI, only 15% were classified correctly.7,8 In 2015, the adherence score for trained and untrained HCWs in Boucle du Mouhoun and northern regions in Burkina Faso was 48%.9 In the same two regions, the implementation of IMCI guidelines was improved by the introduction of electronic IMCI guidelines for consultations with children younger than 5 years. Implementing the electronic guidelines increased HCW adherence to IMCI guidelines by 60.8% (from 48% to 79%). The free care program, implemented since 2016, has drastically improved access to care for children younger than 5 years in Burkina Faso.4 There is published literature on the quality of care for children younger than 5 years in the context of free care in Burkina Faso.4 However, care delivery and the provision of health services using a tool such as the IMCI guidelines/booklet were not well studied in the context of free care in Burkina Faso.4,10 Our study is part of a global investigation leading to scientific evidence to facilitate decision making at the national and international levels in the mother-and-child health-care field in Burkina Faso. Our study is the first to report data on adherence to IMCI guidelines in settings where HCW workload increased when more children younger than 5 years were provided with greater access to care. The principal question that the project Production and Analysis of Data in order to Improve Mother and Child Health in Burkina Faso would like to answer is: What is the progress and the effect of interventions related to mother and child health in the context of the free care program in rural and urban areas? Given that all the services of the free care program for children younger than 5 years were based on IMCI principles, our study evaluated HCW adherence to IMCI guidelines in the context of the free care program in Burkina Faso.
METHODS
This was a secondary data analysis. Data were obtained from a main cross-sectional study conducted from July to September 2020 in health-care centers at the first level of Burkina Faso’s health system both in rural and urban areas of the Hauts-Bassins region. This region comprised eight health districts with 188 CSPSs, three medical centers, five medical centers with surgery capacities, and one teaching hospital. The total population of the region was 227,277 inhabitants.11 This region was among the first regions where the free care program was implemented since the piloting period.12 Forty CSPSs were included in the study. Then, two district hospitals were selected for additional data collection. The study included children younger than 5 years who sought care at the health-care centers selected for the study. They were recruited as they attended the health-care facility. Children younger than 5 years seeking outpatient care who were seen by a qualified and IMCI-trained HCW (auxiliary nurse, auxiliary midwives, nurses, and midwives) at health-care centers and whose parent or caregiver provided consent prior to data collection were included in the study.
Children younger than 5 years not present at the health-care facility during field worker visits, children younger than 5 years consulted not according to IMCI guidelines, and children younger than 5 years who were already hospitalized were excluded from this analysis.
The study consisted of an analysis of data obtained from 419 children who were consulted using IMCI guidelines. This sample size represented the total number of children consulted using IMCI guidelines among children younger than 5 years included in a larger cross-sectional study. We included in our analysis 104 children from the Do District, 70 from the Dande District, 60 from the N’Dorola District, 58 from the Dafra District, 50 from the Lena District, 37 from the Hounde District, 30 from the Orodara District, and 10 from the Karangasso Vigue District, resulting in a total of 419 children.
Data collection occurred over a period of 2 months. Data were collected by assistant nurses, nurses, and midwives trained for a better understanding of the study protocol and standard operating procedures for the study implementation. Data were collected on a tablet through direct observation of the consultation of children younger than 5 years. Data collectors used a checklist based on content from the IMCI guidelines to estimate the level of HCW adherence to IMCI guidelines. The checklist comprised four sections: 1) the evaluation of the sick child using IMCI guidelines, 2) the classification of children using the IMCI decision-making chart, 3t The suggested treatment and the reference indication when necessary using the IMCI decision-making chart, 4) the counseling of children’s parents or caregivers, including giving advice on breastfeeding, when to return for follow-up care, the reasons for the reference, how to handle the reference sheet by the patient, and the provision of advice related to medicine intake and a bandage if necessary, all based on the IMCI decision-making chart.
Sociodemographic characteristics were described according to the type of data. Qualitative data were described using percentages and 95% CIs. Age was recorded as mean and SD. Sociodemographic characteristics were also collected per health district and per type of health-care center.
Adherence rates with regard to the following six tasks of IMCI were estimated: danger signs, cough/breathing difficulties, fever or history of fever, anemia, diarrhea, and nutrition. Percentages were computed to estimate scores for the evaluation of adherence per task and for the overall IMCI guidelines. Tasks involving visual checks were difficult to identify by the observer, so they were not included in the computing of the mean adherence score of the evaluation of danger signs.
For each child, for any sub-task, a score of 0 was assigned when the sub-task was not executed; a score of 1 was assigned when the sub-task was accomplished. The final score per sub-task was the proportion of the specific sub-task accomplished among all the children evaluated. The score for a given task corresponded to the mean percentage of all its sub-tasks. The overall score for adherence to all IMCI steps was obtained by estimating the mean percentage of the adherence to all the tasks.
Adherence scores are generally compared with the scores of experts. However, in this study, expert evaluations were not performed. Therefore, the scores were compared with the scores of similar studies for interpretation.
Score comparisons were performed using univariate analysis. A bivariate analysis was used to determine the variation in HCW adherence to IMCI guidelines based on the sociodemographic characteristics of children and professional category. As mentioned, adherence rates with regard to the following six tasks of the IMCI guidelines were estimated: danger signs, cough/breathing difficulties, fever or history of fever, anemia, diarrhea, and nutrition. Data were analyzed using STATA version 14.
The research protocol was approved by the institutional ethics committee of Center Muraz (approval no. 2020-23/MS/SG/INSP/DG/CEI) and the National Ethics Committee for Health Research (approval no. 2020-7-128) prior to implementation of the study. The study was conducted with the approval of the Hauts-Bassins regional health director. No data were collected without written consent from the parents and caregivers of study participants. We ensured the confidentiality of all study participants. No incentive was provided to the study participants, their parents, or the HCWs observed during the consultation.
RESULTS
Sociodemographic characteristics of the study population.
Our study included 419 children whose consultation was performed using IMCI guidelines/booklets and decision-making charts to assist IMCI-trained HWCs. The gender ratio was 1.2% in favor of boys. The mean age was 2.8 years (range, 2.7–2.9 years) and the age group 12 to 23 months was the most represented (25.5%). Most of the children (63.2.%) lived in rural areas (Table 1). Three hundred fifty children (83.5%) were consulted by grade 2 nurses and 46 children (11%) were consulted by grade 1 nurses. Only 23 children (5.5%) were consulted by assistant nurses or assistant midwives. Children were more enrolled in the Do health district (24.8%) compared with other districts. The age groups 0 to 11 months and 48 to 59 months were not represented in the Karangasso Vigue District (Table 1). There was a balance between the proportion of boys and girls throughout all districts (Table 1). Most of children (86.2%) were included in CSPSs, and among them 73.4% lived in rural areas. Only 13.8% of children were recruited in a district hospital, and all of these children lived in urban areas.
Table 1.
Sociodemographic characteristics of children younger than 5 years old visited in health-care centers, stratified by health districts
| Characteristic | Health districts, n (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Dafra | Dande | Do | Karangasso Vigue | Lena | N’Dorola | Orodara | Hounde | Total | ||
| Age, months | ||||||||||
| 0–11 | 10 (11.2) | 13 (14.6) | 14 (15.7) | 0 (0) | 9 (10.1) | 22 (24.7) | 10 (11.2) | 11 (12.4) | 89 (21.2) | |
| 12–23 | 14 (13.1) | 19 (17.8) | 27 (25.2) | 4 (3.7) | 14 (13.1) | 15 (14) | 2 (1.9) | 12 (11.2) | 107 (25.5) | |
| 24–35 | 14. (15.9) | 16 (18.2) | 22 (25) | 4 (4.6) | 13 (14.8) | 10 (11.4) | 4 (4.6) | 5 (5.7) | 88 (21) | |
| 36–47 | 8 (10.7) | 13 (17.3) | 22 (29.3) | 2 (2.7) | 6 (8) | 10 (13.3) | 9 (12) | 5 (6.7) | 75 (17.9) | |
| 48–59 | 12 (20) | 9 (15) | 19 (31.7) | 0 (0) | 8 (13.3) | 3 (5) | 5 (8.3) | 4 (6.7) | 60 (14.3) | |
| Total | 58 (13.8) | 70 (16.7) | 104 (24.8) | 10 (2.4) | 50 (11.9) | 60 (14.3) | 30 (7.2) | 37 (8.8) | 419 (100) | |
| Residential area | ||||||||||
| Rural | 15 (5.7) | 38 (14.4) | 72 (27.2) | 0 (0) | 50 (18.9) | 37 (14) | 25 (9.4) | 28 (10.6) | 265 (63.2) | |
| Urban | 43 (27.9) | 32 (20.8) | 32 (20.8) | 10 (6.5) | 0 (0) | 23 (14.9) | 5 (3.3) | 9 (5.8) | 154 (36.8) | |
| Total | 58 (13.8) | 70 (16.7) | 104 (24.8) | 10 (2.4) | 50 (11.9) | 60 (14.3) | 30 (7.2) | 37 (8.8) | 419 (100) | |
| Gender | ||||||||||
| Male | 29 (12.50) | 38 (16.38) | 59 (25.43) | 7 (3.02) | 30 (12.93) | 31 (13.36) | 15 (6.47) | 23 (9.91) | 232 (55.4) | |
| Female | 29 (15.51) | 32 (17.11) | 45 (24.06) | 3 (1.60) | 20 (10.70) | 29 (15.51) | 15 (8.02) | 14 (7.49) | 187 (44.6) | |
| Total | 58 (13.8) | 70 (16.7) | 104 (24.8) | 10 (2.4) | 50 (11.9) | 60 (14.3) | 30 (7.2) | 37 (8.8) | 419 (100) | |
Adherence of HCWs.
The overall adherence score of HCWs to IMCI guidelines was 57.8% (95% CI, 42.6–73.0; Table 2). HCWs in the Orodara District had the highest adherence score to IMCI guidelines (63.2%; 95% CI, 37.1–89.4). HCWs in the Dafra District had the lowest adherence to IMCI guidelines (31.9%; 95% CI, 9.5–54.4; Table 3).
Table 2.
Health-care worker adherence to Integrated Management of Childhood Illness protocol related to the clinical evaluation of children younger than 5 years old
| Task no. | IMCI algorithm | Question asked to the parent/caregiver and clinical exam to conduct | n | Score (95% CI) | Mean score (95% CI) |
|---|---|---|---|---|---|
| 5 | Danger signs (n = 419) | Ask whether the child is able to drink/breastfeed. | 309 | 0.737 (0.693–0.779) | 0.719 (0.587–0.851) |
| Ask whether the child vomits everything. | 346 | 0.826 (0.786–0.861) | |||
| Ask about recent convulsions. | 249 | 0.594 (0.546–0.642) | |||
| Observe whether the child convulses. | Unable to assess | ||||
| Observe whether the child is lethargic/unconscious. | Unable to assess | ||||
| 6 | Cough/breathing difficulties (n = 419) | Ask about cough. | 340 | 0.811 (0.771–0.848) | 0.38 (0.361–0.399) |
| Ask about difficulty breathing. | 261 | 0.623 (0.575–0.669) | |||
| If cough/difficulty breathing are present, determine duration of cough/difficulty breathing. | 7 | 0.017 (0.007–0.034) | |||
| If cough/difficulty breathing are present, count the number of breaths per minute. | 116 | 0.277 (0.235–0.322) | |||
| If cough/difficulty breathing are present, look for chest indrawing. | 121 | 0.289 (0.246–0,335) | |||
| If cough/difficulty breathing are present, listen for stridor or “wheeze” breathing. | 110 | 0.263 (0.221–0.307) | |||
| 14 | Fever/history of fever (n = 419) | Ask about current fever. | 396 | 0.945 (0.919–0.965) | 0.561 (0.549–0.574) |
| Ask about history of fever. | 342 | 0.816 (0.76–0.852 | |||
| If fever or history of fever is present, determine duration of fever. | 313 | 0.747 (0.703–0.788) | |||
| If fever or history of fever > 7 days is present, ask whether the child has had a fever every day. | 13 | 0.31 (0.017–0.052) | |||
| If fever or history of fever is present, ask whether the child’s urine is dark or not abundant. | 199 | 0.475 (0.426–0.524) | |||
| If fever or history of fever is present, ask about abnormal bleeding. | 139 | 0.332 (0.287–0.379) | |||
| If fever or history of fever is present, ask about history of measles in the past 3 months. | 261 | 0.623 (0.575–0.669) | |||
| If fever or history of fever is present, take the child’s temperature. | 412 | 0.983 (0.966–0.993) | |||
| If fever or history of fever is present, perform a rapid diagnostic test. | 322 | 0.768 (0.725–0.808) | |||
| If fever or history of fever is present, look for neck stiffness. | 220 | 0.525 (0.476–0.574) | |||
| If fever or history of fever is present, take the child’s pulse. | 26 | 0.062 (0.041–0.09) | |||
| If fever or history of fever is present, look for cold hands or feet. | 145 | 0.346 (0.301–– 0.394) | |||
| If fever or history of fever is present, look for jaundice or redness in the eyes. | 376 | 0.897 (0.864–0.925) | |||
| If fever or history of fever is present, look for general rash (undress the child). | 128 | 0.305 (0.262–0.352) | |||
| 5 | Diarrhea (n = 419) | Ask about diarrhea. | 330 | 0.788 (0.745–0.826) | 0.323 (0.303–0.343) |
| If diarrhea is present, determine duration of diarrhea. | 69 | 0.165 (0.13–0.204) | |||
| If diarrhea is present, ask whether there is blood in the stool. | 145 | 0.346 (0.301–0.394) | |||
| If diarrhea is present, offer water to the child. | 3 | 0.007 (0.001–0.021) | |||
| If diarrhea is present, pinch the skin of the abdomen. | 129 | 0.308 (0.264–0.355) | |||
| 1 | Anemia (n = 419) | Look for palmar pallor. | 324 | 0.785 (0.731–0.811) | 0.773 (0.731–0.811) |
| 4 | Nutrition (n = 419) | Look for severe and visible weight loss. | 201 | 0.48 (0.431–0.529) | 0.711 (0.688–0.732) |
| Measure the height of the child. | 226 | 0.539 (0.49–0.588) | |||
| Measure the weight of the child. | 382 | 0.912 (0.88–0.937) | |||
| Measure the perimeter of the child’s arm circumference. | 382 | 0.912 (0.88–0.937) | |||
| Overall score | 0.578 (0.426–0.730) | ||||
IMCI = Integrated Management of Childhood Illness.
Table 3.
Mean adherence scores to Integrated Management of Childhood Illness guidelines per district
| District | Means Adherence scores | |
|---|---|---|
| Score | 95% CI | |
| Dafra | 0.319 | 0.095–0.544 |
| Dande | 0.545 | 0.35–0.74 |
| Do | 0.542 | 0.303–0.781 |
| Karangasso Vigue | 0.441 | 0.285–0.596 |
| Lena | 0.618 | 0.334–0.902 |
| N’Dorola | 0.538 | 0.282–0.794 |
| Orodara | 0.632 | 0.371–0.894 |
| Hounde | 0.55 | 0.298–0.803 |
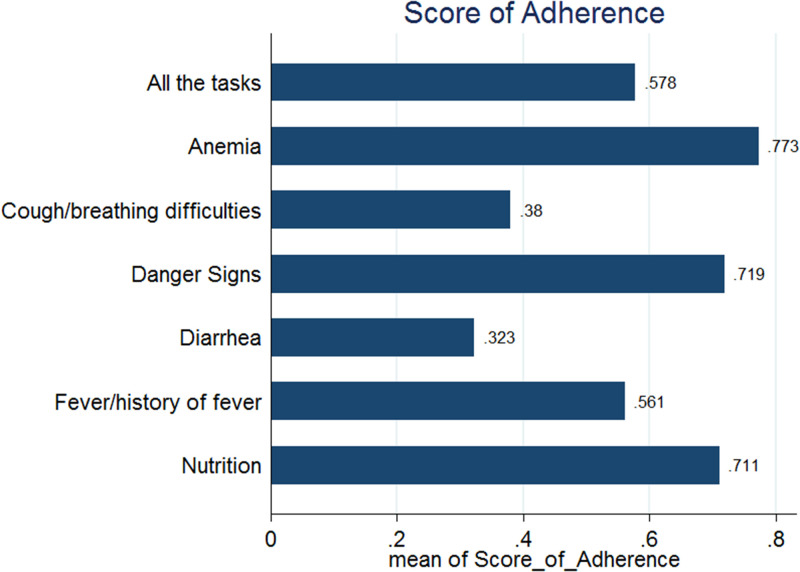
HCWs asked questions about vomiting, the ability to drink, and the presence of convulsions in 82.6% (95% CI, 78.6–86.1), 73.8% (95% CI, 69.3–77.9), and 59.4% (95% CI, 54.6–64.2) of consultations with children, respectively. The mean adherence score for the evaluation of danger signs was 71.9% (95% CI, 58.7–85.1; Figure 1).
Figure 1.
Adherence scores per Integrated Management of Childhood Illness task. This figure appears in color at www.ajtmh.org.
For the evaluation of cough and breathing difficulty, HCWs were more likely to ask whether children had a cough (81.1%; 95% CI, 77.1–84.8) and whether they had breathing difficulty (62.3%; 95% CI, 57.5–66.9). The mean score of the evaluation of cough and breathing difficulty was 38% (95% CI, 36.1–40; Figure 1).
Temperature measurement was the most frequently performed task when evaluating fever (98.3%; 95% CI, 96.6–99.3). The score of fever or history of fever evaluation was 56.1% (range, 54.9–57.4%). For other classifications, the evaluation of anemia had the highest adherence score (77.3%; 95% CI, 73.1–81.1), followed by the adherence score for the evaluation of nutritional status (71.1%; 95% CI, 68.8–73.2). Last, the adherence score for evaluation of diarrhea was the lowest, at 32.3% (95% CI, 30.3–34.3; Figure 1).
Variation of HCW adherence scores according to sociodemographic characteristics of children and professional HCW category.
The mean adherence score to IMCI guidelines in boys (54.2%) was significantly greater than the score obtained in girls (45.3%; P < 0.001). Also, the mean adherence score in children living in rural areas was greater than the mean score obtained during the consultation of children living in urban areas (P < 0.001). However, the difference in scores of different age groups was not significant (P = 0.427; Table 4).
Table 4.
Variation in health-care worker Integrated Management of Childhood Illness guideline adherence score according to the sociodemographic characteristics of evaluated children
| Variable | Global IMCI score | Danger signs | Cough/breathing difficulties | Fever | Diarrhea | Anemia | Nutrition | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | P value | Score | P value | Score | P value | Score | P value | Score | P value | Score | P value | Score | P value | |
| Gender | ||||||||||||||
| Male | 0.542 | < 0.001 | 0.687 | 0.001 | 0.407 | < 0.001 | 0.549 | 0.007 | 0.348 | < 0.001 | 0.767 | 0.486 | 0.5 | 0.001 |
| Female | 0.453 | 0.535 | 0.032 | 0.479 | 0.128 | 0.802 | 0.411 | |||||||
| Age, months | ||||||||||||||
| 0–11 | 0.550 | 0.427 | 0.745 | 0.093 | 0.453 | 0.018 | 0.515 | 0.807 | 0.332 | 0.006 | 0.764 | 0.791 | 0.492 | 0.513 |
| 12–23 | 0.531 | 0.632 | 0.394 | 0.544 | 0.355 | 0.794 | 0.47 | |||||||
| 24–35 | 0.526 | 0.651 | 0.326 | 0.538 | 0.366 | 0.761 | 0.511 | |||||||
| 36–47 | 0.515 | 0.657 | 0.326 | 0.551 | 0.291 | 0.733 | 0.48 | |||||||
| 48–59 | 0.489 | 0.577 | 0.326 | 0.524 | 0.227 | 0.817 | 0.454 | |||||||
| Residential area | ||||||||||||||
| Urban | 0.436 | < 0.001 | 0.539 | < 0.001 | 0.341 | 0.027 | 0.585 | < 0.001 | 0.259 | < 0.001 | 0.604 | < 0.001 | 0.42 | < 0.001 |
| Rural | 0.578 | 0.726 | 0.403 | 0.45 | 0.36 | 0.872 | 0.519 | |||||||
IMCI = Integrated Management of Childhood Illness. Values in bold type are significant.
The mean adherence score to IMCI guidelines in children visited by auxiliary midwives was significantly greater than the score in children consulted by other categories of HCW (78.3%; P = 0.008). Adherence scores of the performance of different IMCI tasks were significantly different across HCW categories except for the evaluation of anemia (Table 5).
Table 5.
Variation in health-care worker adherence score according to professional category
| HCW professional category | Global adherence to IMCI | Danger Signs | Cough/breathing difficulties | Fever | Diarrhea | Anemia | Nutrition | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Score | P value | Score | P value | Score | P value | Score | P value | Score | P value | Score | P value | Score | P value | |
| Grade 1 nurse | 0.533 | 0.008 | 0.685 | 0.002 | 0.393 | 0.004 | 0.544 | 0.016 | 0.331 | 0.008 | 0.431 | 0.11 | 0.494 | 0.031 |
| Grade 2 nurse | 0.444 | 0.519 | 0.252 | 0.455 | 0.218 | 0.822 | 0.4 | |||||||
| Auxiliary midwife | 0.783 | 1 | 0.667 | 0.808 | 0.600 | 1 | 0.625 | |||||||
| Auxiliary nurse | 0.537 | 0.47 | 0.409 | 0.542 | 0.382 | 0.955 | 0.466 | |||||||
HCW = health-care worker; IMCI = Integrated Management of Childhood Illness. Values in bold type are significant.
DISCUSSION
The overall adherence score of HCWs to IMCI guidelines was 57.8%. Many HCWs included in our study have benefited from IMCI initial training, and some of them also received refresher training in the districts where they were appointed. In addition, the introduction of IMCI training in the curriculum of student nurses and student midwives would help establish a cadre of IMCI-trained HCWs. The fact that all HCWs included in our study were trained in IMCI guidelines at least once explained the higher scores found in our study compared with the adherence scores to IMCI guidelines reported before the implementation of the free care program in Burkina Faso.6,13 A previous study reported that the free care program increased the access to health care for children younger than 5 years, leading to an increase in HCW workload.4 The increase in HCW workload may have contributed to the lower than expected scores observed in this study. Despite this, the overall adherence score reported in our study was greater than the result of a recent study conducted in Boucle du Mouhoun and northern regions of Burkina Faso (48%) before the implementation of the free care.9 In addition, the overall score reported in our study was greater than those reported by other studies conducted in Tanzania and Afghanistan, where the adherence rate was only 21% and 24%, respectively.14,15 The observed findings in our study may be the result of a higher quality of care and a high density of HCWs in the Hauts-Bassins region compared with the regions where the adherence score was estimated before the implementation of the free care program. Moreover, observing only the HCWs who used the IMCI guidelines (all trained to IMCI guidelines) could have contributed to high overall adherence scores in our study. HCWs who do not use IMCI guidelines generally have a very low adherence score.9 The evidence attributing of the good adherence scores to the free care program is still inconclusive. Additional studies that take into account other potential confounders, such as interventions that can motivate HCWs in accomplishing their activities, are needed to build the evidence base.
Despite a good overall adherence score, there is existing evidence that suggests an expected 30% increase in adherence score after the implementation of the electronic version of the IMCI guidelines.9 This allowed some districts in other regions of Burkina Faso to reach an adherence score of 100%.15
The medium and low adherences scores observed for fever/history of fever, cough/breathing difficulty, and diarrhea could be the consequence of the high workflow during the rainy season. With an increase in the number of children younger than 5 years seeking care as a result of greater access provided by the free care program, HCWs sometimes skipped parts of the IMCI guidelines to complete their consultations quicker and see more patients. Unfortunately, these results were lower than expected scores.16 Another study also reported a very low adherence score of 9.9% for the evaluation of cough/respiratory difficulty.17 The relatively low adherence score of the evaluation of fever was also reported by El-Ayady et al.18 in Alexandria. In contrast, the fever, cough/respiratory difficulties, and the diarrhea evaluation was performed more effectively in other studies.18,19 This difference may be explained by the greater education level of HCWs included in those studies (physicians).18,19
The adherence score of the evaluation of the danger signs in children younger than 5 years was 71.9%. This high score can result from the fact that we observed only trained HCWs who was using IMCI guidelines. Also, because the presence of danger signs could lead to a bad prognosis for children, HCWs are more inclined to identify them to save children’s lives. This result was similar to the findings of Sarrassat et al.9 in Burkina Faso, who reported a score of 67%. Our result (71.9%) was much higher than those of many studies where adherence scores of danger signs evaluation were less than 33%.8,19,20
We obtained good adherence scores for the evaluation of anemia and malnutrition, at 77.3% and 71.10%, respectively. The high frequency of these syndromes in children younger than 5 years in Burkina Faso led to a good evaluation because HCWs already knew how to assess them. Our results showed a greater adherence score of anemia evaluation in comparison to the findings of Lind et al.,20 who obtain a score of 23.1% despite the implementation of the Algorithm for the Management of Acute Childhood Illnesses intervention. Moreover, the adhesion score for the evaluation of malnutrition was greater than the score of a previous study conducted by Horwood et al.,21 in which, in more than 80% of cases, the adherence score of the evaluation of malnutrition was 60%.
The mean adherence score to IMCI in boys (54.2%) was significantly greater than the score obtained in girls (45.3%). In contrast with another study conducted in Afghanistan,20 there was no difference in the odds of high adherence to IMCI score in girls and in boys (adjusted odds ratio, 0.9; 95%CI, 0.58–1.5).
The low adherence scores of the evaluation of some symptoms such as cough/breathing difficulty and diarrhea has a negative effect on the expected benefit of the IMCI strategy. Therefore, the evaluation of these health conditions should be emphasized during training of HCWs on IMCI guidelines. In addition, coaching, specific supervision, and the scaling up of the electronic version of the IMCI guidelines will contribute to improvements in adherence scores for the evaluation of these health issues.
Our study has some limitations. This evaluation was conducted in only one of the 13 health regions in Burkina Faso. Therefore, it would be relevant to conduct a larger study in many health regions or nationwide to allow for a generalization of the findings to the entire population of children younger than 5 years in Burkina Faso. Some aspects of the evaluation may be disputable because of the data collection method used. Although the observer can easily determine that a question was asked by the HCW, it was more difficult to verify all the visual or manual tasks. In addition, we estimated scores as means of percentages of adherence per task evaluation (given that each task comprises many components). Unfortunately, this approach may lead to the production of some inaccurate numbers. Another limitation is that the scores obtained in the study were not compared with the adherence score obtained by an expert. As result, we only compared our scores with scores obtained from other studies.
CONCLUSION
The overall adherence score of HCWs to IMCI guidelines was relatively high in the Hauts-Bassins region in the context of the free care program for children younger than 5 years. However, the low adherence scores for the evaluation of some IMCI tasks (cough/difficulty breathing and diarrhea) have affected the overall adherence score in our study. The low scores were likely a result of an increase in the workload for HCWs that stems from the demand created when the free care program provided children younger than 5 years with greater access to health-care services. Increasing the density (number of HCWs per health facility) of HCWs in the Hauts-Bassins region will likely lead to greater adherence scores and should be strongly considered. The use of an electronic clinical decision support system developed in line with the IMCI guidelines has been shown to improve how HCWs follow IMCI guidelines.9 Nationwide implementation of the electronic version of the IMCI guidelines should be considered because it is likely to improve adherence scores.
ACKNOWLEDGMENTS
We are grateful to the European Union, the Secretariat Technique - Couverture Sanitaire Universelle, the sexual and reproductive health program of Burkina Faso, and the leaders of public administration. We thank the Production and Analysis of Data in order to Improve Mother and Child Health in Burkina Faso (PAASME) Project National Steering Committee, the members of the study scientific board, the research assistants in charge of data collection, and all participants in this study. We also express our gratitude to the research support staff and the National Observatory of Population Health and the Calculus Center of Centre Muraz/National Public Health Institute.
REFERENCES
- 1.WHO, 2019. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: executive summary. Sex Reprod Heal 2019: 1–12. Available at: https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/.
- 2. Golding N. et al. , 2017. Mapping under-5 and neonatal mortality in Africa, 2000–15: a baseline analysis for the sustainable development goals. Lancet 390: 2171–2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. UN Inter-agency Group for Child Mortality Estimation , 2021. Afghanistan: Under-Five Mortality Rate: Total. Available at: https://childmortality.org/data. Accessed May 4, 2022.
- 4. Matt B, Kiendrébéogo JA, Kafando Y, Tapsoba C, Straubinger S, Metangmo P-M, 2020. Présentation de la Politique de Gratuité au Burkina Faso. pp. 1–75. Available at: https://thinkwell.global/projects/sp4phc/.
- 5. Rakha MA. et al. , 2013. Does implementation of the IMCI strategy have an impact on child mortality? A retrospective analysis of routine data from Egypt. BMJ Open 3: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nguyen DTK, Leung KK, McIntyre L, Ghali WA, Sauve R, 2013. Does Integrated Management of Childhood Illness (IMCI) training improve the skills of health workers? A systematic review and meta-analysis. PLoS One 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kouanda L, Baguiya A, 2013. Evaluation de la Qualite des Soins Prodigues aux Enfants de Moins de Cinq (05) Ans dans les Formations Sanitaires des Regions du Nord et du Centre-Nord du Burkina Faso. Burkina Faso: WHO, UNICEF, UNFPA. [Google Scholar]
- 8.Ministère de la Santé, Direction Générale de la Santé de la Famille, Direction de la Sante de la Mère et de l’Enfant, 2013. Evaluation de la Mise en Oeuvre du Plan de Couverture PCIME 2005–2010 du Burkina Faso. Ouagadougou.
- 9. Sarrassat S, Lewis JJ, Some AS, Somda S, Cousens S, Blanchet K, 2021. An Integrated eDiagnosis Approach (IeDA) versus standard IMCI for assessing and managing childhood illness in Burkina Faso: a stepped-wedge cluster randomised trial. BMC Health Serv Res 21: 354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ouédraogo M, Rouamba T, Samadoulougou S, Kirakoya-Samadoulougou F, 2020. Effect of free healthcare policy for children under five years old on the incidence of reported Malaria cases in Burkina Faso by Bayesian modelling: “not only the ears but also the head of the hippopotamus.” Int J Environ Res Public Health 17: 417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Direction Générale des études et des Statistiques Sectorielles, Ministere de la Sante, 2020. Annuaire Statistiques 2019. Ouagadougou.
- 12. Ridde V, Yaméogo P, 2018. How Burkina Faso used evidence in deciding to launch its policy of free healthcare for children under five and women in 2016. Palgrave Commun 4: 119. [Google Scholar]
- 13. Tawfiq E, Alawi SAS, Natiq K, 2020. Effects of training health workers in integrated management of childhood illness on quality of care for under-5 children in primary healthcare facilities in Afghanistan. Int J Heal Policy Manag 9: 17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bernasconi A, Crabbé F, Raab M, Rossi R, 2018. Can the use of digital algorithms improve quality care? An example from Afghanistan. PLoS One 13: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mitchell M, Getchell M, Nkaka M, Msellemu D, Van Esch J, Hedt-Gauthier B, 2012. Perceived improvement in integrated management of childhood illness implementation through use of mobile technology: qualitative evidence from a pilot study in Tanzania. J Health Commun 17: 118–127. [DOI] [PubMed] [Google Scholar]
- 16. Mitchell M, Hedt-Gauthier BL, Msellemu D, Nkaka M, Lesh N, 2013. Using electronic technology to improve clinical care: results from a before–after cluster trial to evaluate assessment and classification of sick children according to Integrated Management of Childhood Illness (IMCI) protocol in Tanzania. BMC Med Inform Decis Mak 13: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Izudi J, Anyigu S, Ndungutse D, 2017. Adherence to Integrated Management of Childhood Illnesses Guideline in treating south Sudanese children with cough or difficulty in breathing. Int J Pediatr 2017: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. El-Ayady AA, Meleis DE, Ahmed MM, Ismaiel RS, 2015. Primary health care physicians’ adherence and attitude towards Integrated Management of Childhood Illness guidelines in Alexandria governorate in Egypt. Glob J Health Sci 8: 217–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Krüger C, Heinzel-Gutenbrunner M, Ali M, 2017. Adherence to the Integrated Management of Childhood Illness guidelines in Namibia, Kenya, Tanzania and Uganda: evidence from the national service provision assessment surveys. BMC Health Serv Res 17: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lind A. et al. , 2011. Quality of outpatient hospital care for children younger than 5 years old years in Afghanistan. Int J Qual Health Care 23: 108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Horwood C, Vermaak K, Rollins N, Haskins L, Nkosi P, Qazi S, 2009. An evaluation of the quality of IMCI assessments among IMCI trained health workers in South Africa. PLoS One 4: 2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]