Abstract
Introduction
School-age children play a key role in the spread of airborne viruses like influenza due to the prolonged and close contacts they have in school settings. As a result, school closures and other non-pharmaceutical interventions were recommended as the first line of defense in response to the novel coronavirus pandemic (COVID-19).
Methods
We used an agent-based model that simulates communities across the United States including daycares, primary, and secondary schools to quantify the relative health outcomes of reopening schools for the period of August 15, 2020 to April 11, 2021. Our simulation was carried out in early September 2020 and was based on the latest (at the time) Centers for Disease Control and Prevention (CDC)’s Pandemic Planning Scenarios released in May 2020. We explored different reopening scenarios including virtual learning, in-person school, and several hybrid options that stratify the student population into cohorts in order to reduce exposure and pathogen spread.
Results
Scenarios where cohorts of students return to school in non-overlapping formats, which we refer to as hybrid scenarios, resulted in significant decreases in the percentage of symptomatic individuals with COVID-19, by as much as 75%. These hybrid scenarios have only slightly more negative health impacts of COVID-19 compared to implementing a 100% virtual learning scenario. Hybrid scenarios can significantly avert the number of COVID-19 cases at the national scale–approximately between 28 M and 60 M depending on the scenario–over the simulated eight-month period. We found the results of our simulations to be highly dependent on the number of workplaces assumed to be open for in-person business, as well as the initial level of COVID-19 incidence within the simulated community.
Conclusion
In an evolving pandemic, while a large proportion of people remain susceptible, reducing the number of students attending school leads to better health outcomes; part-time in-classroom education substantially reduces health risks.
Keywords: Agent-based model, Non-pharmaceutical interventions, Workplace restrictions, K-12 school reopening scenarios, COVID-19
Graphical Abstract
1. Introduction
The novel coronavirus disease (COVID-19) was first identified in Wuhan, China in late December 2019 and subsequently spread worldwide. (ProMED, 2020) By March 11, 2020, when the World Health Organization (WHO) declared COVID-19 as a global pandemic, there were already close to 120,000 confirmed cases and more than 4,300 deaths worldwide. (WHO, 2020) As of August 2022, there are now over 577 million confirmed cases and over 6.4 million deaths worldwide, with over 91 million confirmed cases and over one million deaths in the United States (U.S.). (Worldometer, 2020) The SARS-CoV-2 virus spreads primarily through small droplets and aerosols of saliva or discharge from the nose of an infected person. (Zhang et al) During the early stages of the pandemic, there were no vaccines or large-scale treatments for COVID-19, (Zhang et al) demonstrating the urgent need for non-pharmaceutical approaches to reduce its spread.
Public health officials recommended a range of individual-and-community-level non-pharmaceutical interventions to slow the spread of COVID-19 and mitigate the impact on people, communities, and the healthcare system. (CDC, 2020) Individual measures included personal protective actions, such as applying proper cough etiquette, hand hygiene, wearing face masks, isolating when sick, or quarantining after an exposure to a confirmed case or after residing in/arriving from a community with known widespread transmission. Community measures included social distancing measures such as stay-at-home recommendations, canceling mass gatherings, minimizing face-to-face contact at workplaces, and closing schools or changing school attendance schedules.
One of the most controversial community measures considered to reduce COVID-19 transmission was school closures and reopening strategies. As the cases of COVID-19 in the U.S. started to increase during the early spring of 2020, most of the primary and secondary schools were closed for the remainder of the 2019–2020 school year. (Ballotpeida, 2020) This raised concern about the wellbeing of school children, especially due to educational disparities that have been exacerbated by the pandemic, social isolation, and other unintended consequences such as access to free and subsidized lunches at schools. (Tsai et al., 2017) However, there was anecdotal evidence that reopening schools for the traditional academic year in autumn 2020 in areas experiencing widespread community transmission would provide additional transmission pathways between communities that were otherwise mostly isolated. For example, the Cherokee County School District in Georgia reported 108 confirmed cases of COVID-19 within two weeks of schools reopening, and three out of the six high schools in the district reverted to full remote leaning by the third week. (COVID-19, 2020, CNN.com, 2020) In Mississippi, 71 of the 82 counties reported positive COVID-19 cases within few weeks of schools reopening. (Clarion Ledger, 2020) Similarly, in Tennessee, over 2000 children tested positive for COVID-19 within two weeks of schools reopening (Newsweek, 2020).
To assess the impacts of school closures and reopening strategies on COVID-19 transmission, researchers began to use mathematical and computational models of COVID-19 spread. Several studies had quantified the impact of various non-pharmaceutical interventions in combination with different school reopening strategies and found that reopening schools as normal was likely to increase the number of COVID-19 cases. (Di Domenico et al., 2020, Espana et al., 2020) Other studies found that closing schools and incorporating social distancing measures in classrooms were effective in reducing the spread of COVID-19. (Ferguson et al., 2020) In addition, hybrid (i.e., a combination of in-person and virtual) approaches to learning, such as capping the in-person classroom size, was found to likely be effective in reducing transmission (Espana et al., 2020, Head et al., 2020) and provide a balanced approach between supporting education while limiting the spread of COVID-19.
A critical component to COVID-19 transmission that was absent from previous school closing and reopening simulations was incorporating the transmission pathways and impacts from workplace restrictions. We address this gap by combining personal non-pharmaceutical interventions, school reopening scenarios, and workplace restrictions into an agent-based model, EpiCast, to assess the potential feedbacks on the spread of COVID-19. Using parameters provided by the U.S. Centers for Disease Control and Prevention (CDC) to simulate COVID-19 transmission within the U.S., we explored several school reopening scenarios including virtual learning, in-person learning, and several hybrid options that stratify the student population into cohorts in order to reduce exposure and disease spread. The results of this study can support decisions regarding optimal school reopening strategies that balance education, the wellbeing of children, and the negative health outcomes of COVID-19.
2. Methods
2.1. Agent-based model description
We used an agent-based model, known as Epidemiological Forecasting (EpiCast), originally designed to simulate community-level influenza transmission in the U.S. at the national-scale and adapted it to simulate COVID-19. (Germann et al., 2006) The primary modifications for COVID-19 relate to the disease natural history (as described later) since the transmission mechanisms for COVID-19 are similar to that for influenza. The national-scale simulation model consists of 281 million individuals distributed among 65,334 census tracts to closely represent the actual population distribution according to the 2000 U.S. Census data. (Germann et al., 2006) Each tract is organized into 2,000-person communities resulting in 180,492 model communities. The model combines U.S. Census demographics and worker flow data to generate daytime and evening contact networks based on potential contacts emerging at daycares, schools, workplaces, households, neighborhoods (∼500 people), and communities (e.g., mall, supermarket). (Germann et al., 2006) In each census tract, the synthetic population matches the actual population in several demographic measures including the number of residents and households, the household’s age distribution, the household size and membership distribution, and employment status for working adults. In addition, each workplace is assigned a 3-digit North American Industrial Classification System (NAICS) code based on the proportion of workers in each sector in each county. We used a regional model (∼8.6 million people in the Chicago Metropolitan Statistical Area (MSA)) to explore additional scenarios (given the extensive computational nature of the national model) in order to determine the impact of different assumptions on COVID-19 spread and mitigation strategies.
A new feature of EpiCast, developed for the purpose of this study, is the ability to capture interactions between teachers and students while in school settings. In previous EpiCast simulation studies, (Germann et al., 2006, Germann et al., 2019) school mixing groups accounted only for transmission between students; teachers and staff were not explicitly included. For the present study, we associate a workplace with NAICS Subsector Code 611 (Educational Services) with each school, and account for mixing between the teachers, staff, and school children. Where necessary, we add additional workplace(s) in a community to achieve an average 14:1 student:(teacher/staff) ratio in each school, based on recent statistics from the National Center for Education Statistics. (National Center for Education Statistics, 2020) This is necessary because our community model assumes that elementary and secondary school children attend school in the tract/community in which they reside, not accounting for bussing across Census tract boundaries which the actual employment statistics reflect. Transmission between children in a school mixing group, and between teachers/staff in a workplace mixing group, are unchanged from the original model. For the added mixing, from students to teachers/staff and vice versa, we assume that the individual child-adult contacts are twice the child-child contact rates.
2.2. Epidemiological parameter assumptions
In order to simulate COVID-19 transmission within a community, we used parameter assumptions and model-produced epidemiological data from the CDC’s Pandemic Planning Scenarios released in May 2020 ( Table 1). (CDC, 2020) The disease natural history for COVID-19 was assumed to be as follows: the latent period is drawn from an approximately Gaussian distribution between 1 and 7 days (mean 3.75), with the incubation period lasting one additional day (i.e., between 2 and 8 days). The infectious period is drawn from a similar distribution between 3 and 9 days (mean 5.6). Furthermore, the proportion of infections which remain asymptomatic are assumed to be 40% and the relative infectiousness of asymptomatic or pre-symptomatic individuals is assumed to be 75%. Self-isolation of symptomatic individuals is assumed to be similar to those used for pandemic influenza studies. (CDC, 2020) We assumed levels of reduction in contacts to quantify the impact of social distancing, facemasks, and hygiene ( Table 2). The “reduced” social distancing scenarios assume a 50% reduction in compliance of preschool and elementary school-age children to account for limited facemask or social distancing measures. Finally, long distance travel is assumed to be reduced due to travel and quarantine restrictions implemented across the nation (Table 2). (Travel, 2021) Each county was initialized and calibrated to match the cumulative case counts during the first two weeks of August 2020 as reported by the New York Times COVID-19 repository. (The New York Times COVID-19 Repository, 2020 https://github.com/nytimes. (accessed Aug 13, 2020)). We do not report the number of cases during the model’s 10-day calibration phase and thus assume that the simulation starts on August 15, 2020.
Table 1.
Summary of Key EpiCast model parameters for this study. (CDC, 2020)
| Parameter | Age Group | ||
|---|---|---|---|
| 0–49 | 50–64 | 65+ | |
| Symptomatic case hospitalization rate | 0.017 | 0.045 | 0.074 |
| Symptomatic case fatality rate | 0.0005 | 0.002 | 0.013 |
| Percentage of hospitalized cases requiring treatment in the ICU | 23.6% | 36.2% | 35.1% |
| Percentage of hospitalized cases requiring >=1 day of ventilator use | 11.7% | 21.8% | 21.3% |
Table 2.
Workforce status & reduction in contacts due to social distancing assumptions.
| Working Status |
Reduction in Contacts due to Social Distancing |
Long Distance Travel |
|||||
|---|---|---|---|---|---|---|---|
| Workplace Assumption |
Full Time | Part-time or Shift | Telework Take-up | Laid Off | Workplace | Other non-household | |
| Fewer Open Workplaces | 44% | 32% | 20% | 16% | 10% | 50% | 50% |
| More Open Workplaces | 52% | 32% | 15% | 8% | 10% | 25% | 75% |
Assumptions regarding full time, part-time, the number of individuals teleworking, and employees laid off as a result of the COVID-19 pandemic are shown in Table 2. Although some of these percentages were chosen based on discussions with subject matter experts from the State of New Mexico, similar reductions were observed in other areas. Furthermore, the percentage of individuals teleworking are based on two surveys of the labor market near the beginning of the COVID-19 pandemic in the U.S. from the Bureau of Labor Statistics (BLS). (U.S, 2020) The ability to telework for each 3-digit NAICS sector also comes from the BLS survey and is shown in Table A-1 in the appendix. The model assumptions on working in the workplace versus working from home or being laid off were based on the values in both Table 2 and Table A-1 in the appendix.
2.3. Workplace modeling assumptions
Per the phase guidelines released in Opening Up America Again (Opening up America Again, 2020) in April 2020, we modeled two scenarios: “Fewer Open Workplaces,” similar to Phase 2 of Opening Up America Again, and “More Open Workplaces”, similar to Phase 3. These two scenarios describe different levels of in-person workplace assumptions (Table 2, and Figure A-1 and Table B-1 in the appendix). Specifically, Fewer Open Workplaces encourages telework whenever possible and feasible with business operations as well as limited onsite operations for a small set of businesses. More Open Workplaces assumes staffing of additional worksites with an expanded number of onsite workers. An example is a retail business may be open to 25% customer capacity as per Phase 2 recommendations and the NAICS industry percentage of employees working onsite is 50% (in order to accommodate the workers necessary for the operation of the business) for Fewer Open Workplaces. For More Open Workplaces, this business may have the opportunity to have a 50% customer capacity and the percentage of employees would need to increased to 75%. For a comparison across intervention approaches, we also use a Pre-pandemic Behavior scenario, which assumes that all businesses are open with no capacity or social distancing restrictions.
2.4. School scenarios
We explored the impact of various school reopening scenarios ( Table 3). These scenarios range from 100% virtual learning to 100% in-classroom learning (Baseline). We explored multiple hybrid learning options, where students are separated into cohorts and attend school on alternating days or weeks. We also explored scenarios with 80% in-classroom enrollment and the remaining 20% virtual learning in response to surveys that suggest that at least 20% of parents may not send their children back to school in the 2020–2021 school year. (Barnum and Bryan, 2020) For the regional model, we assume that the 2020–2021 school year for the Chicago Public Schools begins on September 8th, 2020. The national scale model assumes different start dates for the 2020–2021 school year ranging from August 3rd, 2020 (Arizona) to September 16th, 2020 (New York) based on publicly available information from school districts. We assume a 50% reduction in contacts due to social distancing measures implemented at school settings for the Fewer Open Workplaces and a 25% reduction for the More Open Workplaces (Table 2).
Table 3.
Descriptions of school reopening, baseline, and pre-pandemic scenarios.§.
| Scenario Name | Scenario Code | Scenario Description |
|---|---|---|
| Pre-Pandemic Behavior | Pre-Pandemic Behavior | No mitigations, all businesses completely open (i.e., 100% enrollment with no social distancing in place). |
| Baseline | Baseline | All students physically in school with some social distancing (i.e., 100% enrollment). |
| 80% Onsite Learning with Reduced Social Distancing‡ | 80%_ OL_LessSD | All enrolled* students physically in school. |
| 80% Onsite Learning with Ideal Social Distancing† | 80%_OL_SD | All enrolled* students physically in school. |
| 80% Partial Onsite Learning – Alternating Week with Reduced Social Distancing‡ | 40%_POL_ LessSD_Week | Two non-overlapping cohorts of students – 40% of the students attend one week and the other 40% attend the next week. |
| 80% Partial Onsite Learning – Alternating Days with Reduced Social Distancing‡ | 40%_POL_LessSD_2Day | Two non-overlapping cohorts of students – 40% of the students attend for two days/week (Mon/Tue) and the other 40% attend for two days (Thu/Fri). Wednesday off for disinfection. |
| 80% Partial Onsite Learning – Alternating Weeks with Ideal Social Distancing† | 40%_POL_SD_Week | Two non-overlapping cohorts of students – 40% of the students attend one week and the other 40% attend the next week. |
| 80% Partial Onsite Learning – Alternating Days with Ideal Social Distancing† | 40%_POL_SD_2Days | Two non-overlapping cohorts of students – 40% of the students attend for two days/week (Mon/Tue) and the other 40% attend for two days (Thu/Fri). Wednesday off for disinfection. |
| 100% Distance Learning | Offsite | No students physically in school. |
§Note that given the similar results between all the “Less SD” scenarios in the regional simulations, we did not run the Less SD for the nationwide scenarios.
*Note that 80% in-person enrollment was used due to recent surveys that suggest that at least 20% of parents may not send their children back to school. (Opening up America Again, 2020)
†Ideal social distancing assumes 50% reduction in contacts due to students staying 6 ft from other people, increased hygiene, and masks/face coverings.
‡Reduced social distancing assumes 25% reduction in contacts of preschool and elementary school-age children to account for limited facemask use or limited social distancing measures.
3. Results
3.1. Overall national impacts
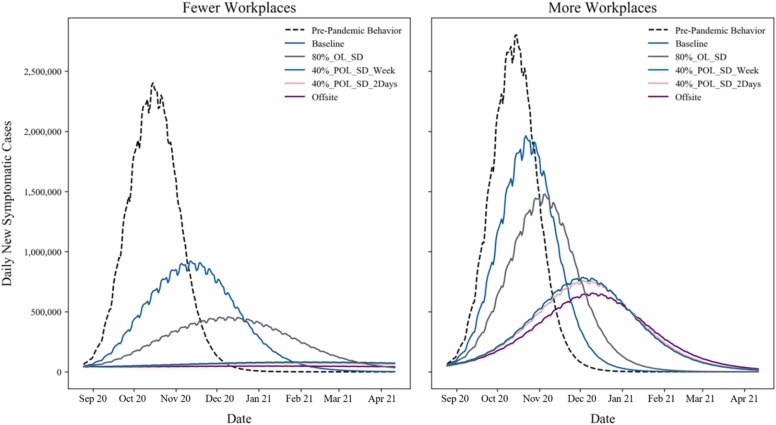
The impacts of school reopening scenarios of six scenarios under Fewer Open Workplaces and More Open Workplaces for the nation are shown in Fig. 1. Note that each regional simulation (i.e., Chicago-area) only takes a few minutes, allowing a wider exploration of scenarios. More specifically the results presented here were obtained in 3-4 min using 4 Intel nodes (with Haswell or Knights Landing processors). In contrast, each national simulation typically required 40–60 min on 16 nodes. To account for the stochastic nature of the simulation model, results for each scenario were averaged over 20 realizations for the regional (Chicago-area) model, and 3 realizations for the national model. The regional results for the Chicago MSA are shown in the appendix (Figure A-2 and Tables B-2 and B-3). In the analysis, only symptomatic cases were reported for easy comparison purposes. Given the similar results between all the reduced social distancing (“Less SD”) scenarios in the Chicago MSA simulations, we did not run the Less SD for the nationwide scenarios. All the hybrid and virtual learning scenarios delay the epidemic peak and flatten the curve for Fewer Open Workplaces, which is consistent with previous studies on school closures (Fig. 1). (Elveback et al., 1976; Espana et al., 2020; Ferguson et al., 2020; Germann et al., 2006) However, for More Open Workplaces, the peak for most scenarios is spread around three weeks regardless of school reopening scenario and the impact of hybrid school reopening scenarios is reduced. Additionally, the reduced social distancing scenario (analyzed only the Chicago MSA region), which accounts for limited compliance in facemask usage and social distancing measures for children in K-8 (i.e., kindergarten through grade 8–see appendix), has a slight but significant decrease in the clinical attack rate (CAR) (i.e., the percentage of the population that has developed or currently has symptoms at the end of the simulation) over the simulated eight-month period. That is, for the Fewer Open Workplaces scenario, the CAR is reduced from 26.3% for the 80% less social distancing scenario to 23.8% for the ideal social distancing scenario. Similarly, the CAR is reduced for the 40% 2-day split cohort scenario from 8.8% to 5.8% for the Fewer Open Workplaces scenarios depending on the ideal or reduced social distancing assumptions, respectively. These results show that reducing the number of students attending in the classroom and splitting the student population into cohorts can reduce the potential negative impacts of COVID-19.
Fig. 1.
National results from the EpiCast model for various school reopening scenarios under Fewer Open Workplaces and More Open Workplaces (simulation period: August 15, 2020 to April 11, 2021).
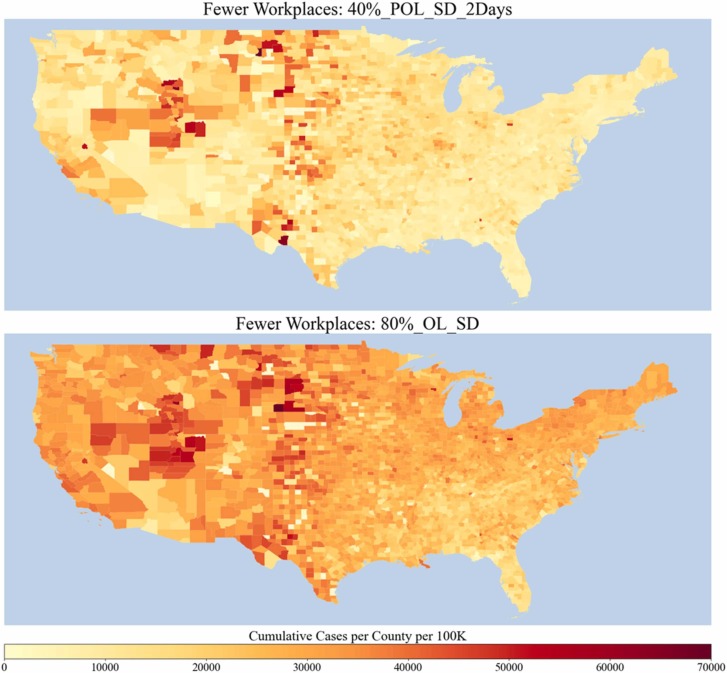
National impacts were spatially heterogeneous, but resulted in the highest incidence throughout the Great Plains and Rocky Mountain Region for both the 40% split cohort attending 2 days a week scenario and the 80% onsite learning scenario ( Fig. 2). The spatial differentiation is due to local demographics and initial conditions. In addition, we provided state level comparisons for 12 representative states (at least one state per U.S. Department of Health & Human Services Regions) in order to show the spatial differentiation for all the scenarios (Figures A-3 to A-12).
Fig. 2.
Simulated results of cumulative cases per county per 100,000 population for (1) two non-overlapping cohorts of 40% of students attending school 2-days a week and (2) 80% of students in-classroom learning (simulation period: August 15, 2020 to April 11, 2021).
Table 4, Table 5 show key results from the model aggregated for the nation. Table 4 shows the total number of symptomatic cases, deaths and hospitalizations for each scenario for the full eight-month simulation period and for the four weeks around the peak of the epidemic. Table 5 shows the peak incidence and prevalence as well as the time to peak and the total CAR for each scenario. Similar impacts as the Chicago MSA model (see appendix) are observed at the national level but the overall attack rate is lower for all scenarios. Specifically, the scenarios with the lowest CARs, despite the number of open workplaces, are the 100% offsite or virtual learning and the 40% 2-day and alternating weeks school scenarios. As noted earlier, the impacts of COVID-19 spread are lower for the Fewer Open Workplaces compared to the More Open Workplaces for all scenarios.
Table 4.
Summary of key EpiCast results for the Nation – Part 1.
| Workplace Assumptions |
Scenario Name |
During Peak 4 Weeks |
Cumulative - August 15, 2020 to April 11, 2021 |
Cases Averted | ||||
|---|---|---|---|---|---|---|---|---|
| Cases | Hospitalized | Deaths | Cases | Hospitalized | Deaths | |||
| Fewer Open Workplaces | Pre-Pandemic Behavior | 59,664,577 | 1798,188 | 107,322 | 110,244,127 | 3370,360 | 230,451 | |
| Baseline | 24,323,551 | 685,746 | 38,649 | 75,049,776 | 2,132,798 | 128,292 | ||
| 80%_OL_SD | 12,346,146 | 354,878 | 20,900 | 55,178,391 | 1,588,821 | 95,848 | 19,871,385 | |
| 40%_POL_SD_Week | 2263,045 | 67,090 | 4108 | 15,922,257 | 466,195 | 27,874 | 59,127,519 | |
| 40%_POL_SD_2Days | 1997,647 | 59,056 | 3624 | 14,457,662 | 424,601 | 25,474 | 60,592,114 | |
| Offsite | 1,336,844 | 39,827 | 2484 | 10,665,240 | 316,245 | 19,169 | 64,384,536 | |
| More Open Workplaces | Pre-Pandemic Behavior | 68,242,756 | 2,064,544 | 120,162 | 116,608,169 | 3,584,053 | 242,236 | |
| Baseline | 49,681,358 | 1,470,601 | 84,679 | 102,532,010 | 3,071,051 | 198,517 | ||
| 80%_OL_SD | 38,469,699 | 1,156,296 | 69,342 | 93,355,312 | 2,830,004 | 184,520 | 9,176,698 | |
| 40%_POL_SD_Week | 21,206,204 | 657,099 | 42,085 | 75,101,132 | 2,331,432 | 154,298 | 27,430,878 | |
| 40%_POL_SD_2Days | 20,479,987 | 636,866 | 41,009 | 73,871,330 | 2,296,792 | 152,097 | 28,660,680 | |
| Offsite | 17,756,292 | 556,366 | 36,073 | 68,375,029 | 2,139,919 | 142,522 | 34,156,981 | |
Table 5.
Summary of key EpiCast results for the Nation – Part 2.
| Workplace Assumptions |
Scenario Name | Peak Incidence (Cases per 1000 Persons) |
Time to Peak Incidence (days) | Peak Prevalence (Cases per 1000 Persons) |
Time to Peak Prevalence (days) |
Peak Date | Clinical Attack Rate (%)* |
|---|---|---|---|---|---|---|---|
| Fewer Open Workplaces |
Pre-Pandemic Behavior | 2,402,432 | 62 | 51 | 66 | 10/20/20 | 42.4 |
| Baseline | 922,097 | 90 | 19 | 94 | 11/17/20 | 28.9 | |
| 80%_OL_SD | 456,896 | 118 | 10 | 122 | 12/15/20 | 21.2 | |
| 40%_POL_SD_Week | 82,209 | 174 | 2 | 178 | 2/9/21 | 6.1 | |
| 40%_POL_SD_2Days | 72,686 | 174 | 2 | 178 | 2/9/21 | 5.6 | |
| Offsite | 50,110 | 8 | 1 | 157 | 1/19/21 | 4.1 | |
| More Open Workplaces |
Pre-Pandemic Behavior | 2,803,605 | 62 | 59 | 65 | 10/19/20 | 44.8 |
| Baseline | 1,963,443 | 69 | 41 | 73 | 10/27/20 | 39.4 | |
| 80%_OL_SD | 1,478,282 | 83 | 31 | 87 | 11/10/20 | 35.9 | |
| 40%_POL_SD_Week | 786,216 | 111 | 17 | 115 | 12/8/20 | 28.9 | |
| 40%_POL_SD_2Days | 758,840 | 111 | 16 | 115 | 12/8/20 | 28.4 | |
| Offsite | 654,784 | 118 | 14 | 122 | 12/15/20 | 26.3 |
Source of Infection
The clinical attack rate is the percentage of the population that develop symptoms at the end of the simulation.
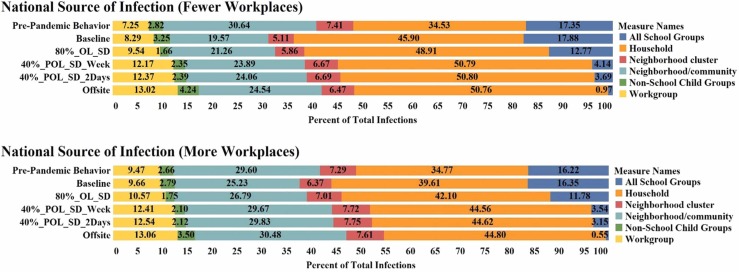
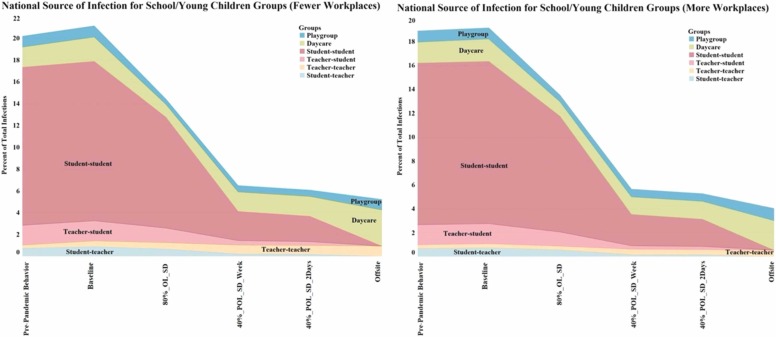
Our results show that the majority of cases are generated at home, followed by neighborhood/community settings ( Fig. 3). The percentage of infection generated in schools and workplaces is correlated with the level of schools/workplaces open. It is important to note that additional infections generated at workplaces are captured under neighborhood/community due to the fact that EpiCast does not explicitly account for customer interactions with workers at workplaces/workgroups. In our model, workgroups only account for infection transmissions generated from employee to employee. Fig. 4 shows the aggregated source of infection for daycares, playgroups, and schools for all the national-level scenarios for Fewer Open and More Open Workplaces. Note that for all the hybrid and in-person school scenarios, the student-student interactions generated the most infections due to the prolonged close contacts in these settings.
Fig. 3.
Source of infection for scenarios aggregated for all states.
Fig. 4.
School-related source of infection breakdown including playgroup, daycare, student-student, teacher- student, student-student. The largest contribution is generated from the student-student interactions.
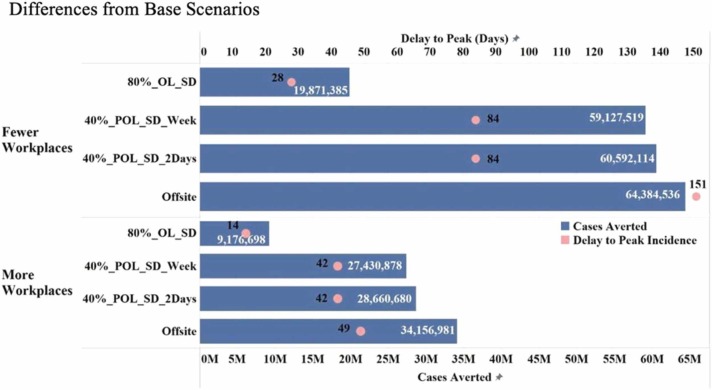
3.2. Cases averted
We estimated the number of cases that may be averted by comparing each of the mitigation scenarios against the Baseline scenario. Fig. 5 shows the cases averted and delay to peak incidence for Fewer Open and More Open Workplaces for all the national-level scenarios. The results show that alternating school cohort scenarios can significantly avert the total number of cases by approximately 60 M and 28 M for the Fewer Open Workplaces and More Open Workplaces, respectively. Furthermore, the offsite or virtual learning scenario provides the largest benefit by averting the greatest number of cases followed by the 40% scenarios. Notably, the 100% distance learning scenario averts nearly 5 million more cases and results in almost twice as long time-to-peak interval compared to the split cohort scenarios. These results demonstrate the positive impacts of non-pharmaceutical interventions in reducing disease burden and flattening the curve.
Fig. 5.
Cases averted and delay to peak incidence in days for all national-level scenarios. Fewer people physically at work and more social distancing along with hybrid school scenarios avert a significant number of cases and delay the peak; fully offsite learning averts even more cases and almost doubles the delay to peak compared to hybrid school scenarios.
3.3. Retrospective analysis performed in july 2021
In the nine months since releasing this study on medRxiv (October 2020 – July 2021), the COVID-19 pandemic caused its so far highest and longest peak in the U.S., vaccines have been approved and distributed, and several new variants have emerged globally. This section provides a brief retrospective analysis, which combines the insight from the modeling with actual profiles observed in the pandemic. It is worth noting that in the U.S., all 50 states and the District of Columbia implemented K-12 school closures by March 24, 2020. During this time, several learning modalities were used including: distance learning, hybrid learning, and full in-person learning. Schools finally reopened across the U.S. in September 2021. In many important respects, the model performed well, but significant differences are apparent. Specifically, approximately 31 million total cases were reported as of April 11, 2021 in the U.S. (Wikipedia, 2021) This is comparable to our model’s projected estimate of 14 million (40%_POL_SD_2Days) to 55 million (80%_OL_SD) cases under the assumption of Fewer Open Workplaces. The peak time for U.S. COVID-19 cases was January 8, 2021, which is also comparable to the range in our model’s projected peak of these two scenarios (December 15, 2020 to February 9, 2021, respectively). Indeed, the reality of this 8-month simulation period arguably lies in-between these two scenarios and it is more aligned with the assumption of Fewer Open Workplaces across the country. The simulated deaths were much lower than what was reported: 555,712 COVID-19 deaths as of April 11, 2021. (Wikipedia, 2021) This is likely a result of us using the latest (at the time) CDC COVID-19 Pandemic Planning Scenarios released in May 2020, (CDC, 2020) which had much lower case-facility ratios by age. However, our projections of deaths and hospitalizations can be easily re-scaled based on more precise estimates of case-fatality and case-hospitalization ratios as they become available.
4. Discussion and conclusions
Non-pharmaceutical interventions such as school closures and other forms of social distancing were implemented globally to mitigate the spread of COVID-19. As the virus transmission was expected to accelerate even further in the U.S. during the winter of 2020–2021, there was a need to assess how to best sustain school activities while reducing the risk of increased transmission. We used an agent-based simulation to assess the impact of several school reopening scenarios in combination with community level transmission that accounts for workplace in-person restrictions.
Our results suggest that reducing the number of students learning in-person by 20% (consistent with the percentage of parents who will likely keep children out of school during the school year 2020/21) (Barnum and Bryan, 2020) reduces the COVID-19 CAR by at least 5% compared to 100% of students learning in-person. Hybrid learning scenarios where split cohorts of 40% of students return to school in non-overlapping formats may result in larger decreases in the CAR, potentially by as much as 75% assuming greater reductions in community business levels. Alternating school cohort scenarios can also significantly avert the total number of cases by approximately 60 M and 28 M for the Fewer Open Workplaces and More Open Workplaces, respectively. These hybrid scenarios assume appropriate non-pharmaceutical interventions such as social distancing and wearing facemasks at school. Our results indicate that implementing smaller classroom sizes and cohorts of students with breaks between in-person school attendance (e.g., two days on, five days off) can have a major impact on the spread of COVID-19 both in terms of total cases and timing of the peak of a given outbreak wave. The hybrid scenarios have impacts which, when plotted, appear only modestly lesser than the 100% offsite or distance learning scenario. However, the 100% distance learning scenario averts nearly 5 million more cases and results in almost twice as long of a time-to-peak interval compared to the split cohort scenario. In general, our findings support strategies that reduce the number of students attending in-person education from a public health perspective but we did not account for the unintended negative consequences of altering school schedules. Our results are consistent with previous studies that have shown that non-pharmaceutical interventions can delay the peak of an outbreak (i.e., flatten the curve) and reduce the total number of cases over the same time frame. (Germann et al., 2019, Courtemanche et al., 2020, Korevaar et al., 2020, Brauner et al., 2020).
The results of our simulations were heavily dependent on the level of adult-to-adult contact in non-school workplaces. Increasing the number of in-person workplaces (i.e., from Fewer Open to More Open Workplaces) increases the overall CAR for all scenarios. For the alternating school cohort scenarios, there is a nearly five-fold increase in the CAR when moving from Fewer Open to More Open Workplaces. Implementing both maximum work-from-home and cohorts in school along with social distancing measures will reduce transmission, hospitalizations, and deaths. We observe significant heterogeneity within the U.S. due to the starting initial conditions of current cases, local demographic drivers (i.e., age distribution), and the number and type of workplaces. Areas with high incidence at the beginning of the simulation have worse outcomes and, generally, earlier peaks. This could mean that timing school reopening to coincide with locally lower incidence rates is important. All scenarios where schools reopen even at the 80% level will result in greater COVID-19 case rates requiring higher levels of hospitalizations, ICU beds needed, and ventilators needed across the U.S. However, implementing cohorts and smaller class sizes result in fewer cases and deaths, while providing important educational opportunities for children. Combining these with social distancing measures including mask wearing, social distancing, and other non-pharmaceutical interventions results in fewer cases.
Due to the detailed dynamics of our simulation, we were able to identify the activities leading to higher number of infections. In particular, our result show that the majority of infections are generated at home followed by neighborhood/community settings. Identifying the source of infection can help develop targeted mitigations aimed at specific settings that are contributing to disease spread.
Our findings should be considered in context of several potential limitations. First, the model assumed the same level of workplace restrictions (namely Fewer Open Workplaces and More Open Workplaces) uniformly across all the states in the U.S. in order to compare the different scenarios under similar conditions. However, there is evidence that each state has implemented different public health actions resulting in drastically distinct operating statuses for businesses that have reopened. (National Governors Association (NGA), 2020) Therefore, incorporating the heterogeneity in state actions may be necessary in order to better quantify the impact of school reopening scenarios on COVID-19 spread. Second, we did not consider testing and contact tracing explicitly in the simulation. Although we assume isolation of symptomatic individuals promptly after symptom onset, we know that effective contact tracing and testing, in combination with hybrid school reopening scenarios and social distancing measures, will be critical for safely reopening schools. Third, we projected epidemic trajectories through the beginning of April 2021 in order to assess the potential impact of school reopening scenarios during the autumn and winter months. However, several studies (Moran and Del Valle, 2016) have shown that behavioral responses to an epidemic or pandemic are highly dependent on the perception of the severity of the disease. Thus, we expect the behavior and compliance to change and fluctuate in the next six months as a result of new public health orders and disease perception; however, we do not have adequate data to predict this, and therefore assume that the same level of restriction and compliance to non-pharmaceutical interventions will remain in place. Specifically, we assumed 50% reduction in social contacts due to social distancing and facemask measures for the Fewer Workplaces Open scenario and 25% for the More Workplaces Open scenario. These assumptions are likely to be higher in school settings where teachers and staff may enforce face coverings and social distancing measures. Fourth, the population distribution in EpiCast is based upon the 2000 U.S. Census data to take advantage of available tract-to-tract work flow data. This is a major limitation for areas that have seen significant population changes in the last two decades. For example, as Table 4B in the Appendix shows, there has been a significant population increase in the age group of over 55 (i.e., 37.3 million increases in 2019 compared to 2000, which accounts for 80% of total population increase). Therefore, the simulation may be conservative in terms of the potential contacts and spread, as well as the projected hospitalizations and deaths due to COVID-19. Also, the epidemiological parameters have spatial and temporal variability during the course of the COVID-19 pandemic. Additional studies are needed in order to quantify the impact of changing these assumptions on the epidemic projections. Fifth, the study did not assume the use or uptake of COVID-19 vaccines. However, the results are still relevant for the 2020 fall school season when vaccines were not available anywhere, as well as presently for any settings where they still may not be widely available. Sixth, our results were not overly sensitive to the assumptions about students to teachers/staff and vice versa, and we note that the numbers of child-child transmissions are still greater than child-adult transmission due to the much larger number of children in a school. Finally, this study took place during the early phases of the COVID-19 pandemic and did not account for the shifts we’ve observed for other variants such as targeting younger populations.
While there is uncertainty in our epidemic projections, our results are consistent with previously published studies (Germann et al., 2019, Courtemanche et al., 2020, Korevaar et al., 2020, Brauner et al., 2020) and are intended to serve as guidance for decision regarding the impacts of different school reopening scenarios in the U.S. Specifically, recent studies have evaluated the impact of non-pharmaceutical interventions (Haug et al., 2020, Banholzer et al., 2021, Liu et al., 2021) and have found that a balanced approach that reduces risk while enabling limited business activity and education can be achieved through careful implementations of non-pharmaceutical interventions. However, we note that the benefits and limitations of scenario analysis will not play out exactly as specified in this study due to heterogeneities in interventions and compliance.
Contributors
TG, MS, LD, MG, CM, and SD conceived and designed the study. LD performed data curation. TG, GF, and CWR performed the computational experiments. MS, LD, and SD analyzed the results. MS and LD visualized the results. TT, JA, DH developed code to analyze and visualize maps. SD and MG led the writing of the initial drafts of the manuscript on which all authors commented, and all authors agreed with the decision to submit. All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors accept responsibility for submitting the article for publication.
Declaration of Competing Interest
The authors declare no competing interest.
Acknowledgments
The authors wish to acknowledge the following collaborators from the Centers for Disease Control and Prevention (CDC): Dr. Amra Uzicanin (Division of Global Migration and Quarantine at CDC) who helped conceive, design, and interpret the scenarios presented in this paper. Additionally, we thank Dr. Matthew Biggerstaff (Influenza Division) and Dr. Rachel Slayton (Division of Healthcare Quality Promotion) who provided insightful information to guide this study. The authors thank Dr. Jee Hwang, economist at the New Mexico Human Services Department for providing useful information to inform workforce assumptions. Additionally, the authors thank the High-Performance Computing team at LANL for their help with the computational infrastructure and for allocating targeted resources to enable COVID-19 modeling efforts.
This work was sponsored by the United States Centers for Disease Control and Prevention (CDC) and the National Institutes of Health/National Institute of General Medical Sciences/Models of Infectious Disease Agent Study under grant R01GM130668. This work was performed at Los Alamos National Laboratory (LANL), an affirmative action/equal opportunity employer, which is operated by Triad National Security, LLC, for the National Nuclear Security Administration of the United States Department of Energy under contract # 19FED1916814CKC. Approved for public release: LA-UR-20–27982.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, the National Institutes of Health, or Los Alamos National Laboratory.
Data sharing
All the data, additional figures and maps will be available here: https://github.com/lanl/covid19-school-reopening-study.
Data availability
A link to the data is included in the manuscript.
References
- BallotpediaSchool responses to the coronavirus (COVID-19) pandemic during the 2019–2020 academic year. 2020. https://ballotpedia.org/School_closures_in_response_to_the_coronavirus_(COVID 19)_pandemic,_2020#School_closures_map. (accessed Aug 22, 2020).
- Banholzer N., van Weenen E., Lison A., et al. Estimating the effects of non-pharmaceutical interventions on the number of new infections with COVID-19 during the first epidemic wave. Plos One. 2021;16(6) doi: 10.1371/journal.pone.0252827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnum M. and Bryan C. Despite stress of closures, most parents wary of rush to return to school buildings, polls show. 2020. https://www.chalkbeat.org/2020/7/14/21324873/school-closure-reopening-parents-surveys. (accessed Aug 22, 2020).
- Brauner J.M., Sharma M., Mindermann S., Stephenson A.B., Gavenčiak T., Johnston D., Ge H. The effectiveness and perceived burden of nonpharmaceutical interventions against COVID-19 transmission: a modelling study with 41 countries. Science. 2020 doi: 10.1126/science.abd9388. [DOI] [Google Scholar]
- CDC. COVID-19 Pandemic Planning Scenarios. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/planning-scenarios-archive/planning-scenarios-2020–05-20.pdf. (accessed Jul 20, 2020).
- CDC. How to Protect Yourself & Others. Coronavirus Disease 2019 (COVID-19). 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html (accessed Aug 22, 2020).
- Clarion Ledger. As Mississippi schools' positive COVID-19 cases surge, more testing coming for teachers. 2020. https://www.clarionledger.com/story/news/politics/2020/08/17/mississippi-71-counties-with-school-coronavirus-cases-covid-19/5600787002/ (accessed Aug 22, 2020).
- CNN.com. Georgia school district reports 108 Covid-19 cases. 2020. https://www.cnn.com/world/live-news/coronavirus-pandemic-08–14-20-intl/h_b38c07ffe8a2c68a27304952b0532b95 (accessed Aug 22, 2020).
- Courtemanche C., Garuccio J., Le A., Pinkston J., Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate: Study evaluates the impact of social distancing measures on the growth rate of confirmed COVID-19 cases across the United States. Health Aff. 2020;2020(39):1237–1246. doi: 10.1377/hlthaff.2020.00608. [DOI] [PubMed] [Google Scholar]
- COVID-19 World News. Georgia school district reports 108 Covid-19 cases. 2020. https://covid19data.com/2020/08/14/georgia-school-district-reports-108-covid-19-cases/ (accessed Aug 22, 2020).
- Di Domenico L., Pullano G., Sabbatini C.E., Boëlle P.Y., Colizza V. Can we safely reopen schools during COVID-19 epidemic? medRxiv. 2020 doi: 10.1101/2020.05.08.20095521. 2020.05.08.20095521. [DOI] [Google Scholar]
- Elveback L.R., Fox J.P., Ackermann E., Langworthy A., Boyd M., Gatewood L. An influenza simulation model forimmunization studies. Am. J. Epidemiol. 1976;103:152–165. doi: 10.1093/oxfordjournals.aje.a112213. [DOI] [PubMed] [Google Scholar]
- Espana G., Cavany S., Oidtman R.J., Barbera C., Costello A., Lerch A., Perkins A. Impacts of K-12 school reopening on the COVID-19 epidemic in Indiana, USA. medRxiv. 2020 doi: 10.1101/2020.08.22.20179960. 2020.08.22.20179960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson N., Laydon D., Nedjati-Gilani G., Imai N., Ainslie K., Baguelin M., Dighe A. Vol. 2020. 2020. Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. (London: Imperial College London). [DOI] [Google Scholar]
- Germann T.C., Kadau K., Longini I.M., Macken C.A. Mitigation strategies for pandemic influenza in the United States. Proc. Natl. Acad. Sci. U. S. A. 2006;103:5935–5940. doi: 10.1073/pnas.0601266103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germann T.C., Gao H., Gambhir M., Plummer A., Biggerstaff M., Reed C., Uzicanin A. School dismissal as a pandemic influenza response: When, where and for how long? Epidemics. 2019;28 doi: 10.1016/j.epidem.2019.100348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haug N., Geyrhofer L., Londei A., et al. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020;1303–1312(4) doi: 10.1038/s41562-020-01009-0. [DOI] [PubMed] [Google Scholar]
- Head J.R., Andrejko K., Cheng Q., Collender P.A., Phillips S., Boser A., Click K. The effect of school closures and reopening strategies on COVID-19 infection dynamics in the San Francisco Bay Area: a cross-sectional survey and modeling analysis. medRxiv. 2020 doi: 10.1101/2020.08.06.20169797. 2020.08.06.20169797. [DOI] [Google Scholar]
- Korevaar H.M., Becker A.D., Miller I.F., Grenfell B.T., Metcalf C.J.E., Mina M.J. Quantifying the impact of US state non-pharmaceutical interventions on COVID-19 transmission. medRxiv. 2020 doi: 10.1101/2020.06.30.20142877. 2020.06.30.20142877. [DOI] [Google Scholar]
- Liu Y., Morgenstern C., Kelly J., et al. The impact of non-pharmaceutical interventions on SARS-CoV-2 transmission across 130 countries and territories. BMC Med. 2021;19:40. doi: 10.1186/s12916-020-01872-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran K.R., Del Valle S.Y. A meta-analysis of the association between gender and protective behaviors in response to respiratory epidemics and pandemics. PLOS ONE. 2016 doi: 10.1371/journal.pone.0164541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Education Statistics. https://nces.ed.gov/programs/digest/current_tables.asp. (accessed Aug 22, 2020).
- National Governors Association (NGA). Summary of State Actions Addressing Busines Reopenings. https://www.nga.org/coronavirus-business-reopenings/ (accessed Aug 22, 2020).
- Newsweek. Over 2,000 Tennessee Children Test Positive For COVID In 2 Weeks As Schools Reopen In State. 2020. https://www.newsweek.com/over-2000-tennessee-children-test-positive-covid-2-weeks-schools-reopen-state-1526200 (accessed Aug 22, 2020).
- Opening up America Again, 2020. https://www.whitehouse.gov/openingamerica/. (accessed Jul 15, 2020).
- ProMED International Society for Infectious Diseases. Undiagnosed Pneumonia – China (Hubei): Request for Information. https://promedmail.org/promed-post/?id=6864153 (accessed Aug 14, 2020).
- The New York Times COVID-19 Repository. 2020. https://github.com/nytimes. (accessed Aug 13, 2020).
- Travel restrictions issued by states in response to the coronavirus (COVID-19) pandemic, 2020–2021. 2021. https://ballotpedia.org/Travel_restrictions_issued_by_states_in_response_to_the_coronavirus_(COVID-19)_pandemic,_2020–2021#Travel_restrictions.2C_advisories.2C_and_recommendations_by_state (accessed Jul 15, 2021).
- Tsai V., Khan N.M., Shi J., Rainey J., Gao H., Zheteyeva Y. Evaluation of unintended social and economic consequences of an unplanned school closure in rural Illinois. J. Sch. Health. 2017;87(7):546–553. doi: 10.1111/josh.12525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. Ability to work from home: evidence from two surveys and implications for the labor market in the COVID-19 pandemic. 2020. Available at: https://www.bls.gov/opub/mlr/2020/article/ability-to-work-from-home.htm. (accessed Aug 22, 2020).
- WHO. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19 –11 March 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed Aug 14, 2020).
- Wikipedia. https://en.wikipedia.org/wiki/COVID-19_pandemic_deaths_in_April_2021.
- Wikipedia. https://en.wikipedia.org/wiki/COVID-19_pandemic_cases_in_April_2021.
- Worldometer. https://www.worldometers.info/coronavirus/country/us/ (accessed Aug 22, 2020).
- Zhang R., Li Y., Zhang A.L., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc. Natl. Acad. Sci. U.S.A. 117: 14857–14863. https://doi.org/10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
A link to the data is included in the manuscript.