Abstract
Cavernous nerve injury is an important cause of erectile dysfunction (ED). Although protective nerve technology has been widely used in nerve-sparing radical prostatectomy (nsRP), the incidence of ED is still very high after surgery. The purpose of our study was to evaluate erectile function (EF) and penile length in the non-erectile state (PLNES) following scheduled phosphodiesterase 5 inhibitor (PDE5i), vacuum erectile device (VED) treatment, and combination therapy after nsRP. One hundred patients with localized prostate cancer and normal EF were randomized to scheduled PDE5i group, VED treatment group, a combined treatment group, and the control group without any intervention. The International Index of Erectile Function-5 (IIEF-5) scores and PLNES were evaluated after 6 months and 12 months of treatment. Sexual Encounter Profile (SEP-Question 2 and SEP-Question 3) were evaluated after 12 months of treatment. Ninety-one of the 100 randomized patients completed the study. We found that the 5 mg tadalafil once a day (OaD) combined with VED can help improve IIEF-5 scores in nsRP patients after both 6 months and 12 months. VED alone or combined with tadalafil OaD can help patients maintain PLNES. VED combined with tadalafil OaD can improve the rate of successful penetration (SEP-Question 2) after 12 months. There were no significant differences in the return to target EF after 12 months among the groups. No significant correlation was noted between the variables and return to target EF (IIEF ≥ 17), and between the variables and effective shortening of the patient's penis (shortening ≥ 1 cm) after 12 months of intervention.
Keywords: erectile dysfunction, nerve-sparing radical prostatectomy, penile length, tadalafil, vacuum erectile devices
INTRODUCTION
Cavernous nerve injury is an important cause of erectile dysfunction (ED), which is common after pelvic surgery. Although protective nerve technology has been widely used in nerve-sparing radical prostatectomy (nsRP), the incidence of ED remains very high after surgery, which seriously affects the quality of life of patients and their partners.1 At present, increasing attention is being paid to penile rehabilitation after nsRP. The treatment methods include oral phosphodiesterase 5 inhibitor (PDE5i), vacuum erectile devices (VED), low-energy shock waves, and penile cavernous medicine injections. Although the effective rate in patients after nsRP is significantly lower than that in the general population, PDE5i remains a first-line drug for the treatment of ED after nsRP.2,3 VED is an important method for improving erectile function (EF). This method has no obvious side effects and is relatively simple to perform.4 Studies have found that VED therapy can significantly improve the peak flow velocity and vascular diameter of the cavernous arteries of patients with organic ED and can effectively promote penile rehabilitation in patients with ED.5 It has also been reported in the literature that VED therapy also has a good effect on ED after radical prostatectomy.5,6,7 The purpose of this study was to evaluate EF and penile length in the non-erectile state (PLNES) following scheduled PDE5i, VED treatment, and combination therapy after nsRP.
PATIENTS AND METHODS
This prospective, randomized, single institution trial evaluating EF and PLNES after 5 mg oral tadalafil once a day (OaD) and VED treatment following nsRP was approved by Renji Hospital Ethics Committee, Shanghai Jiao Tong University School of Medicine, Shanghai, China (approval No. [2016]132K). One hundred patients with localized prostate cancer (pT2a–pT2c, Gleason score ≤ 7) who elected to undergo surgical treatment at the Department of Urology and Andrology of Renji Hospital were involved in this study. Patients were counseled and provided informed written consent for participation. Patients with known risk factors for ED and those with health conditions that were potential contraindications for PDE5i therapy were excluded from this study. Patients with known cardiovascular disease, significant renal or hepatic impairment, cerebrovascular disease, poorly controlled hypotension or hypertension, retinitis pigmentosa, a history of bleeding disorders, or active peptic ulcer disease were also excluded. All patients had normal preoperative EF, which was defined as an International Index of Erectile Function-5 (IIEF-5) score ≥ 17. We measured the PLNES before surgery. Patients underwent nsRP using surgical approaches that included laparoscopic radical prostatectomy (LRP) or robot-assisted radical prostatectomy (RRP). The operations were performed by multiple surgeons from our unit. Study accrual occurred from November 2016 to September 2019.
Patients were randomized into the following four groups: patients received 5 mg oral tadalafil OaD (Group T), VED treatment for 15 min twice daily (Group V), and the combination of the two methods (Group T+V) as well as a control group that received no intervention (Group C). Patients began treatment 4 weeks after the operation when all drainage tubes were removed. Patients continued medication use and VED treatment for one calendar year. EF was evaluated using the IIEF-5. Efficacy information was also recorded after each sexual encounter by answering yes/no to questions in their Sexual Encounter Profile (SEP) diaries, including SEP-Question 2 (successful penetration: “were you able to insert your penis into your partner's vagina?”) and SEP-Question 3 (successful intercourse: “did your erection last long enough for you to have successful intercourse?”). The PLNES was measured using an electronic Vernier calliper (Deli Inc., Ningbo, China). Three measurements were obtained and averaged. All patients stopped the use of medication and VED treatment after 12 months. EF and PLNES were evaluated after 6 months and 12 months of treatment. The final assessment was made at 13 months following a 1-month drug washout. At these time points, the self-reported IIEF-5 score and PLNES measurement were obtained and evaluated. The IIEF-5 score was used to provide a subjective assessment of EF. Return to target EF was defined as an IIEF-5 score ≥ 17 (normal or mild ED). Those who met the screening criteria, underwent randomization, and completed follow-up assessment were included in the final study sample.
Data were analyzed using SPSS 21.0 software (SPSS Inc., Chicago, IL, USA). If the data obeyed a normal distribution, they are reported as the mean ± standard deviation, and comparisons between groups were performed by one-way analysis of variance (ANOVA). If the measurement data did not obey a normal distribution, they were reported as the median (lower quartile, upper quartile), and comparisons between groups were performed with the Kruskal–Wallis test at an adjusted test level of α' = 0.0083. Enumeration data were described as frequencies, the Chi-square test was used for comparisons between groups, and the Chi-square split method and the Kruskal–Wallis test were used for pairwise comparisons between groups (α' = 0.0083). Logistic regression analysis was used to measure the correlation between the variables and return to target EF (IIEF ≥ 17), and between the variables and the effective shortening of the penis (shortening ≥ 1 cm) after 12 months of intervention. P < 0.05 indicates statistical significance.
RESULTS
A total of 186 patients were screened for enrolment in this study (Figure 1). Of these patients, 100 met the screening criteria and were randomized. At the 13-month follow-up, 91 patients had completed the study, including 22 (88.0%) in Group C, 24 (96.0%) in Group T, 22 (88.0%) in Group V, and 23 (92.0%) in Group T+V. The evaluation of the randomization process revealed balance across treatment arms in key demographic and clinical patient characteristics (Table 1).
Figure 1.
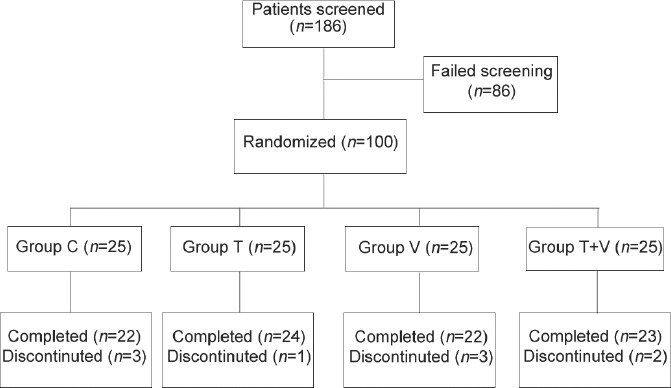
Study design and patient dispositions. One hundred and eighty-six patients were screened for enrolment in this study. One hundred patients met the screening criteria and were randomized. At the 13-month follow-up, 91 patients had completed the study, including 22 in Group C, 24 in Group T, 22 in Group V, and 23 in Group T+V. Group C: control group; Group T: tadalafil 5 mg oral OaD; Group V: vacuum erectile devices treatment for 15 min twice daily; Group T+V: tadalafil 5 mg oral OaD combined vacuum erectile devices treatment for 15 min twice daily. OaD: once a day.
Table 1.
Baseline characteristics of the study population
| Characteristic | Overall (n=100) | Group C (n=25) | Group T (n=25) | Group V (n=25) | Group T + V (n=25) | P |
|---|---|---|---|---|---|---|
| Age (year) | ||||||
| Mean±s.d. | 64.1±6.2 | 67.2±5.1 | 63.6±4.5 | 61.9±6.6 | 63.7±7.4 | 0.019 |
| Median (range) | 64 (49–76) | 65 (60–76) | 63 (54–70) | 63 (49–74) | 63 (50–75) | |
| BMI (kg m−2) | ||||||
| Mean±s.d. | 23.8±2.5 | 23.5±2.5 | 24.8±2.5 | 23.1±1.8 | 23.8±2.9 | 0.102 |
| Median (range) | 23.7 (16.1–30.8) | 23.5 (18.3–30.1) | 24.8 (19.9–30.8) | 22.8 (19.7–27.7) | 23.7 (16.1–30.5) | |
| PSA (ng ml−1) | ||||||
| Mean±s.d. | 10.1±5.1 | 12.1±7.0 | 9.4±4.5 | 10.2±4.0 | 8.8±3.7 | 0.135 |
| Median (range) | 9.0 (3.3–29.9) | 10.1 (3.3–29.9) | 8.3 (5.0–29.4) | 9.5 (5.0–19.5) | 8.0 (4.4–16.6) | |
| Stage, n (%) | ||||||
| T2a | 59 (59.0) | 15 (60.0) | 13 (52.0) | 16 (64.0) | 15 (60.0) | 0.853 |
| T2b | 22 (22.0) | 5 (20.0) | 8 (32.0) | 5 (20.0) | 4 (16.0) | 0.552 |
| T2c | 19 (19.0) | 5 (20.0) | 4 (16.0) | 4 (16.0) | 6 (24.0) | 0.870 |
| Gleason score, n (%) | ||||||
| 6 | 29 (29.0) | 9 (36.0) | 5 (20.0) | 7 (28.0) | 8 (32.0) | 0.637 |
| 7 | 71 (71.0) | 16 (64.0) | 20 (80.0) | 18 (72.0) | 17 (68.0) | 0.637 |
| Type of surgery, n (%) | ||||||
| LRP | 72 (72.0) | 17 (68.0) | 18 (72.0) | 20 (80.0) | 17 (68.0) | 0.755 |
| RARP | 28 (28.0) | 8 (32.0) | 7 (28.0) | 5 (20.0) | 8 (32.0) | 0.755 |
| Baseline IIEF-5 score | ||||||
| Mean±s.d. | 21.6±2.0 | 20.7±1.8 | 21.8±2.0 | 23.5±1.7 | 23.0±2.2 | 0.147 |
| Median (range) | 20 (17–25) | 21 (18–25) | 21 (20–25) | 22 (20–25) | 21 (20–25) | |
| PLNES | ||||||
| Mean±s.d. | 7.7±1.5 | 7.6±1.7 | 8.1±1.1 | 7.5±1.6 | 7.4±1.7 | 0.442 |
| Median (range) | 7.6 (4.5–11.5) | 7.5 (4.6–11.5) | 8.2 (6.2–10.5) | 7.6 (4.5–10.5) | 7.5 (4.8–10.6) |
Group C: control group; Group T: tadalafil 5 mg oral OaD; Group V: vacuum erectile devices treatment for 15 min twice daily; Group T+V: tadalafil 5 mg oral OaD combined vacuum erectile devices treatment for 15 min twice daily, BMI: body mass index; LRP: laparoscopic radical prostatectomy; PLNES: penile length in non-erection state; PSA: prostate-specific antigen; RARP: robot-assisted radical prostatectomy; s.d.: standard deviation; OaD: once a day; IIEF-5: International Index of Erectile Function-5
To compare whether the IIEF-5 scores of the patients in the treatment groups improved after 6 months and 12 months, nonparametric statistical analysis and the Kruskal–Wallis test were used because the values did not conform to a normal distribution. We found that the IIEF-5 scores were significantly different after 6 months and 12 months of intervention in the different treatment groups (6 months, P = 0.002; and 12 months, P < 0.001; Supplementary Table 1). The Mann–Whitney U test was performed to clarify the difference between the groups at an adjusted test level of α' = 0.0083. After 6 months of treatment, the IIEF-5 scores were much higher in Group T+V than those in Group C (P < 0.0001). After 12 months of treatment, the IIEF-5 scores in Group T+V and Group V were much higher than those in control Group C (P < 0.0001). In addition, the IIEF-5 scores of Group T+V were significantly different from those of Group T (P < 0.0001), as shown in Figure 2.
Supplementary Table 1.
International index of erectile function-5 improvement in different groups after 6 and 12 months of intervention (P<0.05)
| IIEF-5 scores | Group C | Group T | Group V | Group T + V | P |
|---|---|---|---|---|---|
| 6 months | |||||
| Mean±s.d. | 4.1±3.4 | 5.7±3.8 | 6.9±3.8 | 8.3±3.9 | 0.002 |
| Median (range) | 5 (0–15) | 5 (0–17) | 5 (0–12) | 7 (5–18) | |
| 12 months | |||||
| Mean±s.d. | 5.6±4.7 | 8.4±5.0 | 12.2±4.7 | 15.5±4.1 | <0.001 |
| Median (range) | 5 (0–17) | 5 (4–19) | 12 (5–19) | 16 (5–21) |
Group C: control group; Group T: tadalafil 5 mg oral OaD; Group V: vacuum erectile devices treatment for 15 min twice daily; Group T+V: tadalafil 5 mg oral OaD combined vacuum erectile devices treatment for 15 min twice daily; SD: standard deviation; EF: erectile function; IIEF-5: International index of EF; OaD: once a day
Figure 2.
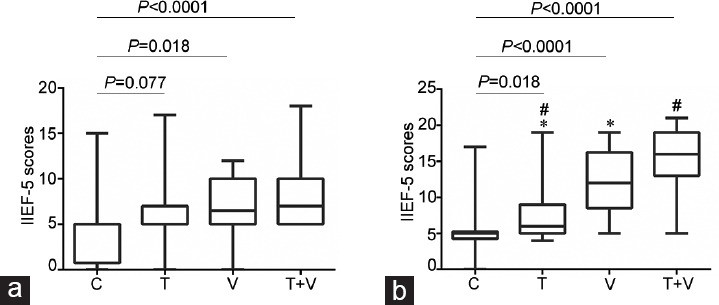
IIEF-5 improvement in different groups after 6 months and 12 months of intervention. The IIEF-5 scores are reported as the median with range. (a) After 6 months of treatment, the IIEF-5 scores were as follows: Group C, 5 (0–15); Group T, 5 (0–17); Group V, 5 (0–12); and Group T+V, 7 (5–18). (b) After 12 months of treatment, the IIEF-5 scores were as follows: Group C, 5 (0–17); Group T, 5 (4–19); Group V, 12 (5–19); and Group T+V, 16 (5–21). C: control group; T: tadalafil 5 mg oral OaD; V: vacuum erectile devices treatment for 15 min twice daily; T+V: tadalafil 5 mg oral OaD combined vacuum erectile devices treatment for 15 min twice daily. *P = 0.004 (Group T vs Group V); #P < 0.0001 (Group T vs Group T+V); Mann–Whitney U test, adjusted test level α' = 0.0083. IIEF-5: International Index of Erectile Function-5; OaD: once a day.
The difference in the PLNES after 6 months and 12 months of treatment in the different groups was compared using one-way ANOVA because the values conformed to a normal distribution. After 6 months and 12 months of treatment, the PLNES of the patients in Group V (6 months, P = 0.005; and 12 months, P < 0.0001) and Group T+V (6 months, P = 0.043; and 12 months, P = 0.001) was much longer than that in Group C. In addition, the PLNES of the patients in Group V (P = 0.003) and Group T+V (P = 0.027) were much longer than that in Group T after 12 months of treatment (Figure 3).
Figure 3.
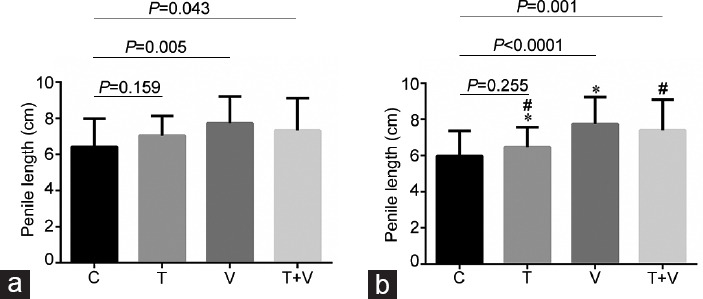
Differences in PLNES in the treatment groups after 6 months and 12 months of intervention. The PLNES were reported as the mean ± s.d. (in cm). (a) After 6 months of treatment, the PLNES values were as follows: Group C, 6.42 ± 1.57; Group T, 7.04 ± 1.10; Group V, 7.72 ± 1.48; and Group T+V, 7.33 ± 1.78. (b) After 12 months of treatment, the PLNES values were as follows: Group C, 5.97 ± 1.40; Group T, 6.45 ± 1.12; Group V, 7.74 ± 1.49; and Group T+V, 7.40 ± 1.69. C: control group; T: tadalafil 5 mg oral OaD; V: vacuum erectile devices treatment for 15 min twice daily; T+V: tadalafil 5 mg oral OaD combined vacuum erectile devices treatment for 15 min twice daily. *P = 0.003 (Group T vs Group V); #P = 0.027 (Group T vs Group T+V), one-way ANOVA, P < 0.05 indicates statistical significant. ANOVA: analysis of variance; PLNES: penile length in the non-erectile state; s.d.: standard deviation; OaD: once a day.
No significant differences in return to the target EF using the IIEF-5 were noted between the groups (P = 0.090; Supplementary Table 2). The proportions of patients with a return to target EF were as follows: 16.7% (Group T), 22.7% (Group V), and 39.1% (Group T+V), versus 9.1% (Group C). SEP-Question 2 (successful penetration) in Group T+V was significantly higher than that in Group C after 12 months (P = 0.015; [Supplementary Table 3). The proportions of patients with successful penetration as measured by a “yes” response to SEP-Question 2 were as follows: 16.7% (Group T), 22.7% (Group V), and 47.8% (Group T+V), versus 9.1% (Group C). The responses to SEP-Question 3 (successful intercourse) did not significantly differ among the groups (P = 0.660; Supplementary Table 4). The proportions of patients with successful intercourse as measured by a “yes” response to SEP-Question 3 were as follows: 12.5% (Group T), 13.6% (Group V), and 21.7% (Group T+V), versus 9.1% (Group C).
Supplementary Table 2.
Number of cases of self-reported International index of erectile function-5 score return to target erectile function (international index of erectile function-5 ≥17) after 12 months treatment in different groups (P=0.090)
| Groups | IIEF5 ≥17 (n) | 0 <IIEF5 <17 (n) | IIEF5 ≥17 (n, %) |
|---|---|---|---|
| C | 2 | 20 | 9.1 |
| T | 4 | 20 | 16.7 |
| V | 5 | 17 | 22.7 |
| T + V | 9 | 14 | 39.1 |
| Sum | 20 | 71 | 22.0 |
Group C: control group; Group T: tadalafil 5 mg oral OaD; Group V: vacuum erectile devices treatment for 15 min twice daily; Group T + V: tadalafil 5 mg oral OaD combined vacuum erectile devices treatment for 15 min twice daily; EF: erectile function; IIEF-5: International index of EF; OaD: once a day
Supplementary Table 3.
Number of cases of answering yes/no about sexual encounter profile Q2 after 12 months treatment in different groups (P=0.015)
| Groups | Yes | No | Yes (n, %) |
|---|---|---|---|
| C | 2 | 20 | 9.1 |
| T | 4 | 20 | 16.7 |
| V | 5 | 17 | 22.7 |
| T + V | 11 | 12 | 47.8 |
| Sum | 22 | 69 | 24.2 |
Group C: control group; Group T: tadalafil 5 mg oral OaD; Group V: vacuum erectile devices treatment for 15 min twice daily; T + V: tadalafil 5 mg oral OaD combined vacuum erectile devices treatment for 15 min twice daily; OaD: once a day
Supplementary Table 4.
Number of cases of answering yes/no about sexual encounter profile Q3 after 12 months treatment in different groups (P=0.660)
| Groups | Yes | No | Yes (n, %) |
|---|---|---|---|
| C | 2 | 20 | 9.1 |
| T | 3 | 21 | 12.5 |
| V | 3 | 19 | 13.6 |
| T + V | 5 | 18 | 21.7 |
| Sum | 13 | 78 | 14.3 |
Group C: control group; Group T: tadalafil 5 mg oral OaD; Group V: vacuum erectile devices treatment for 15 min twice daily; Group T + V: tadalafil 5 mg oral OaD combined vacuum erectile devices treatment for 15 min twice daily; OaD: once a day
No significant correlation was noted between the variables (such as patient age, body mass index [BMI], prostate-specific antigen [PSA], Gleason score, preoperative IIEF-5 score, and PLENS) and return to target EF (IIEF ≥ 17), and between the variables and effective shortening of the patient's penis (shortening ≥ 1 cm) after 12 months of intervention as measured by logistic regression analysis (Table 2).
Table 2.
Correlations between the variables and return to target erectile function (International Index of Erectile Function-5 ≥17), and between the variables and effective shortening of the patient’s penis (shortening ≥1 cm) after 12 months of intervention were analyzed using logistic regression
| Predictor | OR (95% CI) | P |
|---|---|---|
| IIEF-5 ≥17 | ||
| Age (year) | 0.974 (0.886–1.070) | 0.597 |
| BMI (kg m−2) | 1.030 (0.845–1.257) | 0.768 |
| PSA (ng ml−1) | 0.966 (0.858–1.089) | 0.575 |
| Gleason score | 1.362 (0.466–3.983) | 0.573 |
| Baseline IIEF-5 | 1.188 (0.914–1.544) | 0.198 |
| PLNES (cm) | 1.005 (0.704–1.434) | 0.979 |
| Penis shortening ≥1 cm | ||
| Age (year) | 1.056 (0.972–1.148) | 0.199 |
| BMI (kg m−2) | 1.110 (0.926–1.330) | 0.261 |
| PSA (ng ml−1) | 1.054 (0.955–1.163) | 0.297 |
| Gleason score | 1.923 (0.773–4.781) | 0.159 |
| Baseline IIEF-5 | 0.950 (0.783–1.154) | 0.607 |
| PLNES (cm) | 1.245 (0.919–1.687) | 0.157 |
BMI: body mass index; PLNES: penile length in non-erection state; PSA: prostate-specific antigen; CI: confidence interval; IIEF-5: International Index of Erectile Function-5; OR: odds ratio
DISCUSSION
The purpose of penile rehabilitation after nsRP is to improve the oxygen supply and minimize the denervation of the cavernous tissue following vascular and nerve damage through early intervention and prevent penis cavernous fibrosis.8 Ideal penis rehabilitation can help patients regain their erectile function, allowing them to achieve spontaneous erection without relying on drugs, VED or other auxiliary erection treatments.9,10
PDE5i has become the first choice for doctors to perform penis rehabilitation. Patients have good tolerance to PDE5i, which has been shown to be safe in many studies.11,12,13 In our study, no serious adverse reaction occurred following administration of 5 mg oral tadalafil OaD.
However, the results of clinical research on the use of PDE5i for treating ED after nsRP have not been satisfactory. In a prospective, randomized, placebo-controlled clinical trial, there were no findings to support a therapeutic benefit of 50 mg nightly sildenafil in addition to 100 mg on-demand sildenafil compared with on-demand dosing alone.14 Other studies comparing on-demand versus nightly PDE5i include the randomized placebo-controlled trial, which reported the same conclusion.15,16 Based on our single-center study, 5 mg oral tadalafil OaD can improve patients' feelings of penis congestion in the morning. The IIEF-5 score improved, but 12 months of follow-up revealed that 5 mg tadalafil OaD did not improve the percentage of IIEF-5 scores that returned to normal. A 9-month double-blind trial confirmed that long-acting PDE5i tadalafil OaD was currently the most effective penile erectile dysfunction aid.17,18,19 Although tadalafil was significantly better than the placebo in the double-blind treatment period, tadalafil OaD had no significant effect on non-drug-assisted erectile function after a 6-week withdrawal period, and the result did not statistically differ from that obtained with the placebo.
In our study, after treatment with VED for 6 months and 12 months, the penis was prevented from experiencing shortening in the non-erectile state. Penis shortening is a common phenomenon after RP. Shortening of the penis starts approximately 4–8 months after the operation20 and can exceed 1 cm by the 12th month after the operation.21 The gradual shortening of the penis after the operation will affect the patient's standing urination ability and cause a serious psychological burden. Even if the patient has no need for the recovery of erectile function, this can also affect the patient's quality of life. Therefore, maintaining the length of the penis after surgery is also one of the goals of penile rehabilitation. Studies have found that VED therapy can significantly improve the peak flow velocity and vascular diameter of the cavernous arteries of patients with organic erectile dysfunction and prevent penis corpus cavernosum fibrosis.5,6 After 13 months of follow-up, it was found that 5 mg oral tadalafil OaD did not prevent PLNES shortening after RP, and this finding was not significantly different from that in the control group.
We defined EF recovery as a return to a baseline IIEF-5 score ≥ 17, at which point erections are sufficient to maintain sexual intercourse. No significant differences in improvements in effective erections were noted among the three treatment groups with respect to the control group. To compare the difference in erectile function recovery rate, we used the Chi-square test. However, because the minimum frequency within the group was less than 5, nonparametric statistical methods were required, which demonstrated that the difference was not statistically significant. Another study indicated that the percentage of patients who returned to normal EF plateaued approximately 9 months following nsRP.14 Another study reported that recovery can occur up to 24–40 months following surgery, and several authors have suggested a treatment course of up to 24 months.22,23 Longer follow-up is needed to assess long-term recovery in this study.
The limitation of our study was the small sample size. Insufficient attention is given to ED among elderly Chinese patients, especially patients with prostate cancer. More attention is given to the treatment and control of the primary disease but not to the treatment of ED. In particular, elderly female partners have extremely low sexual demands, leading to a low enrolment rate of penile rehabilitation after nsRP.
Male sexual dysfunction associated with prostatectomy can be divided into three main categories: ED and changes in penis size, ejaculation and orgasm dysfunction, and changes in libido and mental health associated with changes in sexual behaviour.24 In this study, we focused on the effectiveness and safety of different rehabilitation treatments in patients with erectile dysfunction and changes in penis size. Given the particularities of the study, the researcher needed to inform the patients in detail about the risks and precautions of different rehabilitation methods. The patients were informed and understood their own rehabilitation treatment methods, that was the reason why the trial could not be double-blind.
CONCLUSIONS
Treatment with 5 mg tadalafil OaD combined with VED can help improve the IIEF-5 score in nsRP patients after 6 months and 12 months. VED treatment alone or combined with tadalafil OaD can help patients maintain PLNES. In addition, the patients in Group T+V reported significantly higher successful penetration. Due to the limitation of the small sample size, there were no significant differences in the return to target EF among the groups after 12 months. According to our study, scheduled PDE5i with VED treatment can improve penile erectile function recovery, whereas VED treatment can prevent penile length shrinkage after nerve-sparing prostatectomy.
AUTHOR CONTRIBUTIONS
MZ and JZC collected the most clinical and follow-up data, wrote and revised the manuscript. MJL and WL designed the study, analyzed the clinical data, and revised the manuscript. YDL, HXW, YPH, and XGL collected partial patients' clinical data and followed up with patients. All authors vouch for the data and analysis. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (No. 81971376 and No. 81800591) and the 3-year action plan to promote clinical skills and clinical innovation in municipal hospitals in Shanghai (No. 16CR3067B), and Shanghai Sailing Program (No. 18YF1412800).
Supplementary Information is linked to the online version of the paper on the Asian Journal of Andrology website.
REFERENCES
- 1.Capogrosso P, Vertosick EA, Benfante NE, Eastham JA, Scardino PJ, et al. Are we improving erectile function recovery after radical prostatectomy? Analysis of patients treated over the last decade. Eur Urol. 2019;75:221–8. doi: 10.1016/j.eururo.2018.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tian D, Wang XY, Zong HT, Zhang Y. Efficacy and safety of short- and long-term, regular and on-demand regimens of phosphodiesterase type 5 inhibitors in treating erectile dysfunction after nerve-sparing radical prostatectomy: a systematic review and meta-analysis. Clin Interv Aging. 2017;12:405–12. doi: 10.2147/CIA.S122273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim S, Sung GT. Efficacy and safety of tadalafil 5 mg once daily for the treatment of erectile dysfunction after robot-assisted laparoscopic radical prostatectomy: a 2-year follow-up. Sex Med. 2018;6:108–14. doi: 10.1016/j.esxm.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raina R, Pahlajani G, Agarwal A, Jones S, Zippe C. Long-term potency after early use of a vacuum erection device following radical prostatectomy. BJU Int. 2010;106:1719–22. doi: 10.1111/j.1464-410X.2010.09360.x. [DOI] [PubMed] [Google Scholar]
- 5.Welliver RC, Jr, Mechlin C, Goodwin B, Alukal JP, McCullough AR. A pilot study to determine penile oxygen saturation before and after vacuum therapy in patients with erectile dysfunction after radical prostatectomy. J Sex Med. 2014;11:1071–7. doi: 10.1111/jsm.12445. [DOI] [PubMed] [Google Scholar]
- 6.Nason GJ, McNamara F, Twyford M, O'Kelly F, White S, et al. Efficacy of vacuum erectile devices (VEDs) after radical prostatectomy: the initial Irish experience of a dedicated VED clinic. Int J Impot Res. 2016;28:205–8. doi: 10.1038/ijir.2016.23. [DOI] [PubMed] [Google Scholar]
- 7.Ismail EA, El-Sakka AI. Innovative trends and perspectives for erectile dysfunction treatment: a systematic review. Arab J Urol. 2016;14:84–93. doi: 10.1016/j.aju.2016.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Segal RL, Cabrini MR, Bivalacqua TJ, Burnett AL. Penile straightening maneuvers employed during penile prosthesis surgery: technical options and outcomes. Int J Impot Res. 2014;26:182–5. doi: 10.1038/ijir.2014.7. [DOI] [PubMed] [Google Scholar]
- 9.Burnett AL, Teloken PE, Briganti A, Whitehurst T, Montorsi F. Intraoperative assessment of an implantable electrode array for cavernous nerve stimulation. J Sex Med. 2008;5:1949–54. doi: 10.1111/j.1743-6109.2008.00865.x. [DOI] [PubMed] [Google Scholar]
- 10.Burnett AL, Goldstein I, Andersson KE, Argiolas A, Christ G, et al. Future sexual medicine physiological treatment targets. J Sex Med. 2010;7:3269–304. doi: 10.1111/j.1743-6109.2010.02025.x. [DOI] [PubMed] [Google Scholar]
- 11.Ficarra V, Novara G, Ahlering TE, Costello A, Eastham JA, et al. Systematic review and meta-analysis of studies reporting potency rates after robot-assisted radical prostatectomy. Eur Urol. 2012;62:418–30. doi: 10.1016/j.eururo.2012.05.046. [DOI] [PubMed] [Google Scholar]
- 12.Garg T, Young AJ, Kost KA, Park AM, Danella JF, et al. Patient-reported quality of life recovery curves after robotic prostatectomy are similar across body mass index categories. Investig Clin Urol. 2017;58:331–8. doi: 10.4111/icu.2017.58.5.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goonewardene SS, Persad R, Gillatt D. Penile rehabilitation for robotic radical prostatectomy: a new game. J Robot Surg. 2016;10:379–80. doi: 10.1007/s11701-015-0548-6. [DOI] [PubMed] [Google Scholar]
- 14.Kim DJ, Hawksworth DJ, Hurwitz LM, Cullen J, Rosner IL, et al. A prospective, randomized, placebo-controlled trial of on-Demand vs. nightly sildenafil citrate as assessed by Rigiscan and the international index of erectile function. Andrology. 2016;4:27–32. doi: 10.1111/andr.12118. [DOI] [PubMed] [Google Scholar]
- 15.Montorsi F, Brock G, Lee J, Shapiro J, Van Poppel H, et al. Effect of nightly versus on-demand vardenafil on recovery of erectile function in men following bilateral nerve-sparing radical prostatectomy. Eur Urol. 2008;54:924–31. doi: 10.1016/j.eururo.2008.06.083. [DOI] [PubMed] [Google Scholar]
- 16.Montorsi F, Wilson TG, Rosen RC, Ahlering TE, Artibani W, et al. Best practices in robot-assisted radical prostatectomy: recommendations of the Pasadena Consensus Panel. Eur Urol. 2012;62:368–81. doi: 10.1016/j.eururo.2012.05.057. [DOI] [PubMed] [Google Scholar]
- 17.Deveci S, Gotto GT, Alex B, O'Brien K, Mulhall JP. A survey of patient expectations regarding sexual function following radical prostatectomy. BJU Int. 2016;118:641–5. doi: 10.1111/bju.13398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emanu JC, Avildsen IK, Nelson CJ. Erectile dysfunction after radical prostatectomy: prevalence, medical treatments, and psychosocial interventions. Curr Opin Support Palliat Care. 2016;10:102–7. doi: 10.1097/SPC.0000000000000195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epifanova MV, Chalyi ME, Gvasaliya BR, Eremin II, Pulin AA, et al. New approaches for recovery of erectile function in patients after radical prostatectomy. Urologiia. 2017;6:138–43. [PubMed] [Google Scholar]
- 20.Raina R, Agarwal A, Ausmundson S, Lakin M, Nandipati KC, et al. Early use of vacuum constriction device following radical prostatectomy facilitates early sexual activity and potentially earlier return of erectile function. Int J Impot Res. 2006;18:77–81. doi: 10.1038/sj.ijir.3901380. [DOI] [PubMed] [Google Scholar]
- 21.Vasconcelos JS, Figueiredo RT, Nascimento FL, Damiao R, da Silva EA. The natural history of penile length after radical prostatectomy: a long-term prospective study. Urology. 2012;80:1293–6. doi: 10.1016/j.urology.2012.07.060. [DOI] [PubMed] [Google Scholar]
- 22.Mulhall JP. The role and structure of a postradical prostatectomy penile rehabilitation program. Curr Urol Rep. 2009;10:219–25. doi: 10.1007/s11934-009-0037-4. [DOI] [PubMed] [Google Scholar]
- 23.Garcia FJ, Brock G. Current state of penile rehabilitation after radical prostatectomy. Curr Opin Urol. 2010;20:234–40. doi: 10.1097/MOU.0b013e3283383b02. [DOI] [PubMed] [Google Scholar]
- 24.Chung E, Van CT, Wilson I, Cartmill RA. Penile prosthesis implantation for the treatment for male erectile dysfunction: clinical outcomes and lessons learnt after 955 procedures. World J Urol. 2013;31:591–5. doi: 10.1007/s00345-012-0859-4. [DOI] [PubMed] [Google Scholar]


