Abstract
The global burden of neurologic disorders is a leading cause of disability and death worldwide and has increased the demand for treatments and rehabilitation. Our proposed integrated osteopathic-neurologic examination (ONE) provides the physician with expanded diagnostic and point-of-care treatment modalities while allowing the physician to make a more tangible effect in patient care. By incorporating the osteopathic structural somatic examination with the complete neurologic evaluation, somatic dysfunction, occurring as a consequence or independent of neurologic injury, can be identified and treated using osteopathic manipulative techniques at time of visit. Using the proposed integrated examination, the physician can determine the interplay between structural and neurologic findings to identify patterns of change that coincide with more specific diagnoses and the chronicity of a condition. Tangible benefits from the ONE approach translate to more accurate clinical assessment and enhanced patient and physician satisfaction.

Recognizing all medical problems do not have a pharmacologic or surgical remedy, a safer structural remedy may provide symptom relief. We propose the osteopathic-neurologic examination (ONE) approach, which provides enhanced overall patient care by incorporating osteopathic structural examination elements with the complete neurologic examination to assess somatic dysfunction. Somatic dysfunction is defined as impairment or altered function of related body structural components characterized by changes in tissue texture, symmetry, motion, and tenderness specific to injury duration.1
Our intent is not to overstate the ONE approach, rather to fundamentally broaden clinical neurologic training and practice to include evaluation of somatic dysfunction.1 The global systematic analysis of 2016 identified a rising burden of neurologic disease despite increased efforts to prevent and slow their progression.2 Misdiagnosis, underdiagnosis, and over or inappropriate treatment of neurologic symptoms, including pain, increase the disease burden. Osteopathic manipulative treatment (OMT) at the point of care offers distinctive therapeutic relief by improving quality of life, decreasing length of hospitalizations, and complementing treatment plans.3-5
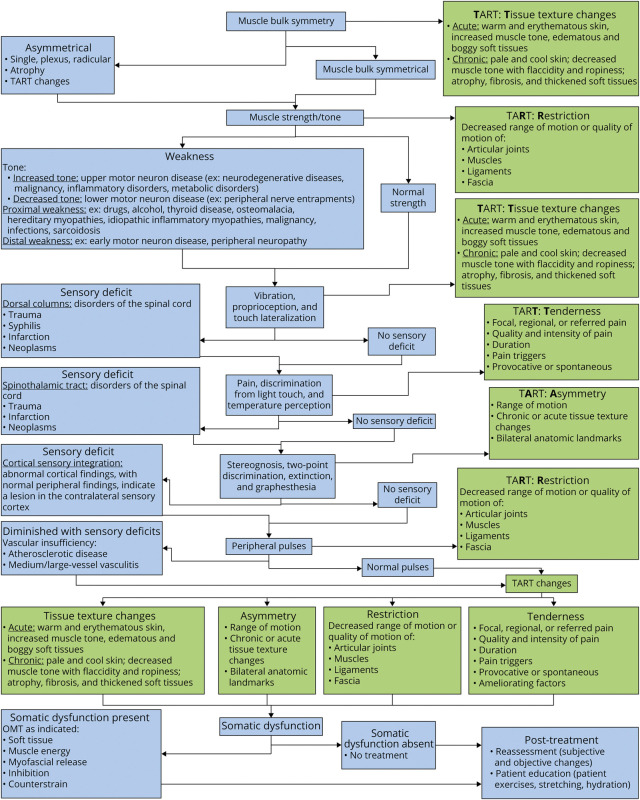
The ONE approach involves obtaining a comprehensive history and performing a complete or focused neurologic examination with a focused osteopathic structural examination, then tailoring OMT to maximize both effectiveness and safety. The osteopathic structural examination assesses for tenderness, asymmetry, range of motion (ROM), and tissue texture (TART) changes. Abnormalities thereof indicate not only presence of somatic dysfunction, but also indicate presence of somatic dysfunction, distinguishes acute from chronic changes, and can be performed by uninitiated physicians with additional training. The primary focus of this article was the biomechanical-structural and neurologic aspects of patient care. Utilization of the ONE approach may enable physicians to make more tangible effect on patient care.
Step 1: Physical Examination and Osteopathic Screening
Osteopathic Screening Examination
An osteopathic structural somatic examination directs attention to altered structural elements that correlate with and may induce gross symptoms and related functional disability. Screening focuses on 3 objective TART elements: tissue texture abnormalities, disparate asymmetry, and tissue restrictions that require a developed level of palpatory skills. Tenderness is a subjective finding that can only be determined from appropriate communication with the patient. These objective palpatory findings may correlate with both motor and sensory changes and extend beyond findings from the traditional neurologic examination.6
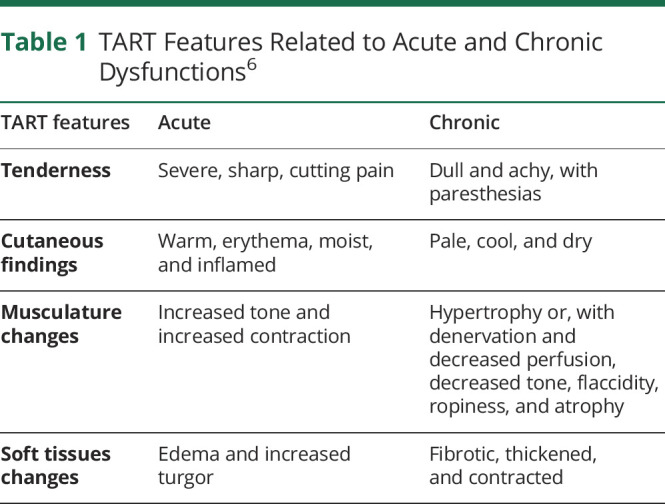
TART: Tenderness and Texture Changes
Palpatory changes are used to verify the patient's complaint and identify dysfunction not discernible by other means. Tenderness and changes in tissue texture present with predictable findings dependent on the chronicity of the dysfunction. Differences in presentation allow the physician to determine whether the dysfunction is acute or chronic (Table 1). Acute injuries incite TART changes, such as postinjury guarding, which are meant to result in tissue healing. However, excessive modification within the neural circuitry evoked by nociception and altered proprioception involved in injury and healing processes can result in pathologic changes and chronic pain patterns. Because patients are exposed to chronic dysfunction for greater lengths of time, peripheral and central neural sensitization mechanisms are continually stressed, resulting in more difficult reversal of the dysfunction and additional physiologic changes including brain reorganization and psychosocial consequences.6 Although acute and chronic changes can be defined by specified lengths of time, physical findings are more accurate and appropriate to determine the palpatory findings correlating with acuity and chronicity. Accurate identification can further guide differential diagnosis and osteopathic treatment. Acute dysfunctions should be treated with more gentle treatment techniques to avoid adverse tissue reactions. Alternatively, chronic dysfunctions should be treated with modalities that directly address the dysfunction and compensatory changes that have developed.6
Table 1.
TART Features Related to Acute and Chronic Dysfunctions6
TART: Asymmetry and Restricted Motion
Restriction, “a resistance or impediment to movement,” can be categorized by the tissue or structure primarily responsible for regional dysfunction, including articular joints, muscles, ligaments, and fascia.6 Restriction frequently results in an asymmetric alteration of morphologic, positional, or motions of body segments or regions. Asymmetry may be assessed visually and confirmed by palpation. Minor anatomic asymmetry is the rule, rather than the exception. Although most individuals have minor asymmetry, assessment of bilateral landmarks, tissue changes, and ROM can allow for early detection of dysfunction. Regional dysfunction may occur in the presence of acute trauma, sustained hypertonic muscles, microtrauma from repetitive motion, or contracture of fascia and ligaments and warrants evaluation of the anatomic cause for restriction. Trauma often produces soft tissue injuries inducing apprehensive muscular splinting and protective guarding. Because of the attachment of musculature to the skeleton, acute or chronic muscular hypertonicity can reduce joint motion and cause anatomic asymmetry.6
Reduced ROM and contracture produces a similar pattern of restriction, altering mobility. Edema may prevent full motion, resulting from pain, stretching fascia, and the fluid itself distorting tissues.6 Assessment of restriction includes observing active and passive ROM to differentiate patient-limited motions from anatomically limited motions. Changes in range and quality of motion result from many neurologic disorders and trauma, including stroke and movement disorders.7 Identification of tension at the end of passive ROM (end feel) is useful when identifying restriction and may provide additional information regarding the etiology of dysfunction. The end feel related to edema feels mushy or sponge-like, whereas hypertonic muscles produce a stretchy or rubbery feeling. Articular dysfunctions present with solid end feel and loss of elasticity. Ligamentous or fascial restrictions have abrupt and hard end feel with significant loss of tissue elasticity.6
Motor
A complete neurologic examination must include an evaluation of motor function beginning with inspection of the area of interest. Careful observation may identify asymmetry in muscle bulk (atrophy, hypertrophy, or pseudohypertrophy), presence of fasciculations, or tremor, followed by muscle strength and fine coordination testing. Observing gait and mobility, both with the patient unaware and while formally tested, provides critical information that may require additional study. Abnormalities in muscle tone along with reflex changes define upper or lower motor neuron deficits.8
Sensory
In addition to a motor evaluation, sensory testing of both primary and cortical sensation and cerebellar evaluation are also essential. Evaluation of the peripheral pulses, if diminished, is indicative of local ischemia and may be causative of sensory and motor abnormalities. Neurologic deficits can have drastic effects on the osteopathic structural somatic examination. In upper and lower neuron (UMN, LMN) disease, regional neurologic deficits give rise to specific TART changes. In UMN disease, tissue texture signs such as spastic weakness are present.9 Sensory, motor, and reflex asymmetries manifest as specific TART changes (Figure). In both UMN and LMN diseases, muscle denervation may increase restriction of myofascial elements, and compensatory dysfunction may occur in other body regions.
Figure. Integrated Osteopathic-Neurologic Examination Enhancing Patient Care: The Osteopathic-Neurologic Examination Approach.
.
Integrating an osteopathic structural somatic examination may further augment the sensory examination through localizing patterns of pain, thus expanding both treatment options and improving precision. Focal points of tenderness can arise because of facilitation, in which a pool of neurons is at a constant state of elevated sensitivity due to a reduced action potential threshold, often resulting in chronic allodynia and hyperalgesia.6,10,11 Once other sources of sensory abnormalities are ruled out, focal points of tenderness may be treated with OMT.
Step 2: Objective Findings
Structural objective findings may be identified using several methods to include examination by body region and discerning a pattern of injury. A complete screen for any TART abnormalities is commonly performed by initially addressing the area of complaint or performed systematically from caudal to cranial for the axial skeleton and then to the extremities. With a pattern of injury approach, a physician can validate the cause and resultant consequences of the injury. Although cohesively interdependent, the summation of neurologic and structural findings refines the diagnosis and leads to individualized treatment. By using a methodical examination approach, with the focus on both biomechanical and neurologic manifestations, related behavioral issues and metabolic consequences are assessed to the degree they contribute to the individual patient complaints.6
Treatment Techniques
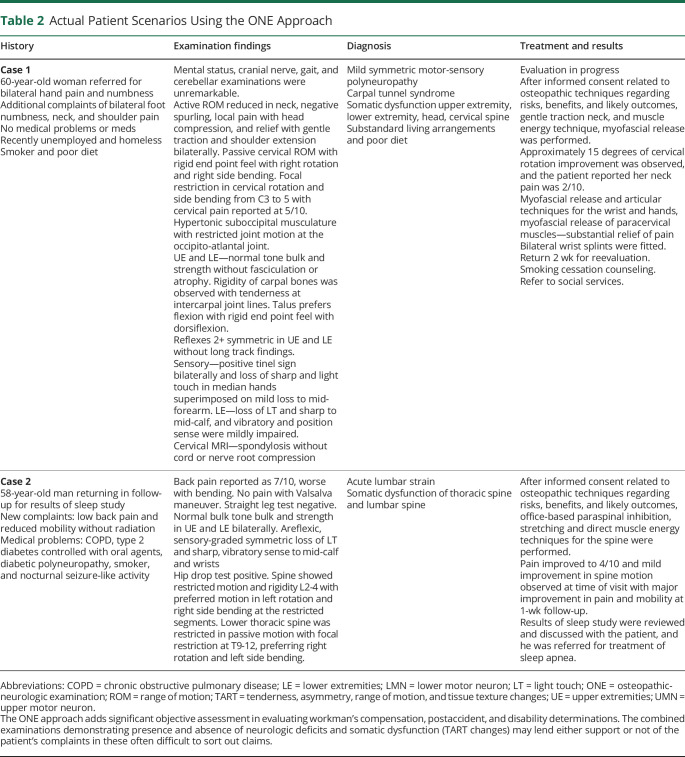
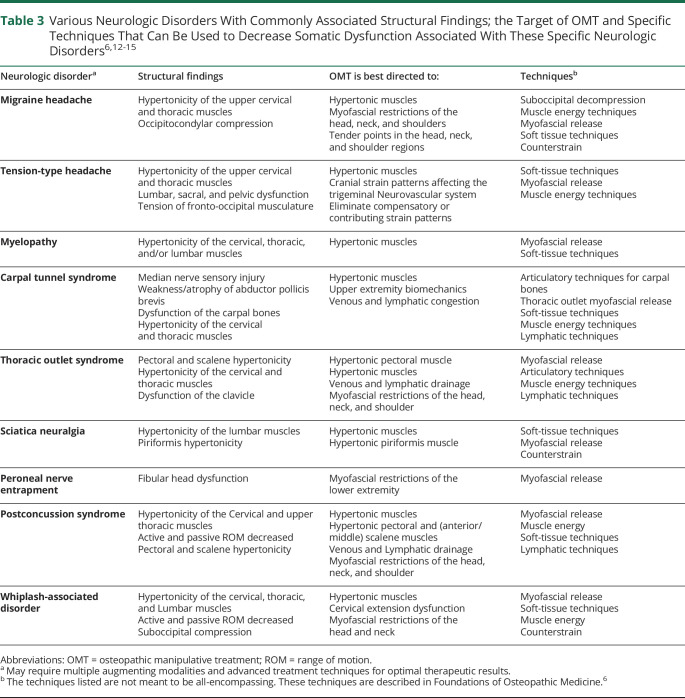
There are numerous osteopathic techniques that can be used to treat specific somatic dysfunctions and can be readily learned by practicing neurologists to help restore biomechanical normalcy and physiologic homeostasis in affected body regions. Examples of common patient presentations and subsequent treatment using the ONE approach are described in Table 2. Common neurologic conditions and indicated OMT treatments are listed in Table 3.
Table 2.
Actual Patient Scenarios Using the ONE Approach
Table 3.
Conclusion
The ONE approach in a neurologic setting can improve patient outcome and enhance physician satisfaction because objective and symptomatic improvements are directly observed. Osteopathic examination and treatment, in addition to improving outcomes, will aid in differentiating functional from identifiable organic causes of patient complaints. Advanced training in defining somatic dysfunction will enhance patient care both diagnostically and therapeutically and reduce dependency on pharmacologic treatments, including opiates, nerve stabilizers, and other drugs with significant side effect profiles. The resulting spectrum of serious medication side effects, and possibility of suboptimal surgical outcomes, contributes to the upswing of physician burnout and patient dissatisfaction with resulting demand for effective low-risk treatment options. With appropriate documentation and coding, the additional time spent in refining the diagnosis and learning treatment techniques is directly remunerative to the physician (eAppendix A, links.lww.com/CPJ/A311). The issues presented in this article mandate alterations in training to include somatic screening in conjunction with neurologic evaluation (for a video demonstrating the ONE approach).16 Physicians wishing to use the ONE approach may expand their skills in osteopathic techniques through available CME accredited workshops (eAppendix A, links.lww.com/CPJ/A311).
Acknowledgment
The authors wish to thank Christopher Breedlove for his assistance in producing the video in reference 16, links.lww.com/CPJ/A311.
Appendix. Authors
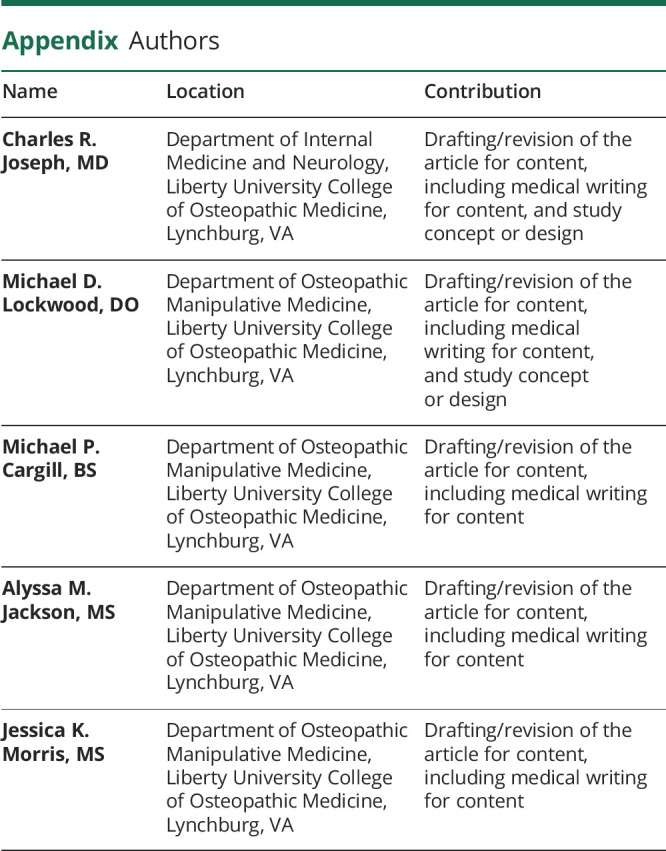
Contributor Information
Michael D. Lockwood, Email: mdlockwood@liberty.edu.
Michael P. Cargill, Email: mpcargill@liberty.edu.
Alyssa M. Jackson, Email: awilson97@liberty.edu.
Jessica K. Morris, Email: jmorris64@liberty.edu.
Study Funding
The authors report no targeted funding.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Giusti R. Lossary of Osteopathic Terminology. 3rd ed. American Association of Colleges of Osteopathic Medicine; 2017. [Google Scholar]
- 2.Cerritelli F, Ruffini N, Lacorte E, Vanacore N. Osteopathic manipulative treatment in neurological diseases: systematic review of the literature. J Neurol Sci. 2016;369:333-341. [DOI] [PubMed] [Google Scholar]
- 3.Voigt K, Liebnitzky J, Burmeister U, et al. Efficacy of osteopathic manipulative treatment of female patients with migraine: results of a randomized controlled trial. J Altern Complement Med. 2011;17(3):225-230. [DOI] [PubMed] [Google Scholar]
- 4.Noll DR, Degenhardt BF, Johnson JC. Multicenter osteopathic pneumonia study in the elderly: subgroup Analysis on hospital length of stay, ventilator-dependent respiratory failure rate, and in-hospital mortality rate. J Am Osteopath Assoc. 2016;116(9):574-587. [DOI] [PubMed] [Google Scholar]
- 5.Fleming RK, Snider KT, Blanke KJ, Johnson JC. The effect of osteopathic manipulative treatment on length of stay in posterolateral postthoracotomy patients: a retrospective case note study. Int J Osteopath Med. 2015;18:88-96. [Google Scholar]
- 6.Seffinger MA. Foundations of Osteopathic Medicine. 4th ed. Wolters Kluwer; 2018. [Google Scholar]
- 7.Shahrokhi M, Asuncion RMD. Neurologic Exam. StatPearls. Accessed November 17, 2020. ncbi.nlm.nih.gov. [PubMed] [Google Scholar]
- 8.Swartz MH. Textbook of Physical Diagnosis: History and Examination, 8th ed. Elsevier; 2021. [Google Scholar]
- 9.Kingsley RE, Gable SR, Kingsley TR. Concise Text of Neuroscience. Williams & Wilkins; 1996. [Google Scholar]
- 10.Sandkühler J. Models and mechanisms of hyperalgesia and allodynia. Physiol Rev. 2009;89(2):707-758. [DOI] [PubMed] [Google Scholar]
- 11.Sandkühler J, Gruber-Schoffnegger D. Hyperalgesia by synaptic long-term potentiation (LTP): an update. Curr Opin Pharmacol. 2012;12(1):18-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wells MR, Giantinoto S, D'Agate D, et al. Standard osteopathic manipulative treatment acutely improves gait performance in patients with Parkinson's disease. J Am Osteopath Assoc. 1999;99(2):92-98. [DOI] [PubMed] [Google Scholar]
- 13.Wolf K, Krinard T, Talsma J, Pierce-Talsma S. OMT for patients with multiple sclerosis. J AM Osteopath Assoc. 2017;117(12):e141. [DOI] [PubMed] [Google Scholar]
- 14.Chappell C. 2017. OMT in post-concussion syndrome. Presented at the 122nd Annual Osteopathic Medical Conference and Exposition, Philadelphia. [Google Scholar]
- 15.Genese JS. Osteopathic manipulative treatment for facial numbness and pain after whiplash injury. J Am Osteopath Assoc. 2013;113(7):564-567. [DOI] [PubMed] [Google Scholar]
- 16.Joseph CR, Cargill M, Jackson AM, Morris JK, Lockwood ML. The “ONE” Approach; LUCOM Vimeo 2021. Accessed August 4, 2021. https://vimeo.com/537769267/064fca792c