Abstract
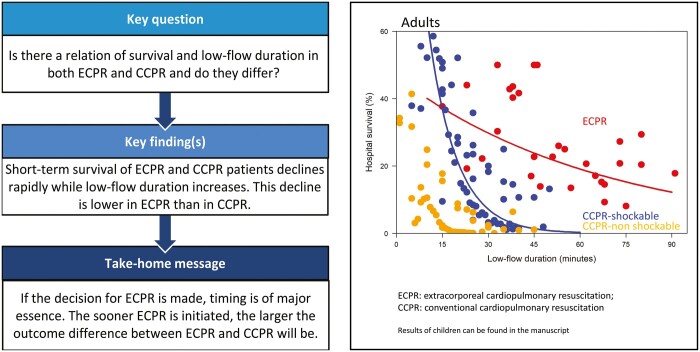
OBJECTIVES
After cardiac arrest, a key factor determining survival outcomes is low-flow duration. Our aims were to determine the relation of survival and low-flow duration of extracorporeal cardiopulmonary resuscitation (ECPR) and conventional cardiopulmonary resuscitation (CCPR) and if these 2 therapies have different short-term survival curves in relation to low-flow duration.
METHODS
We searched Embase, Medline, Web of Science and Google Scholar from inception up to April 2021. A linear mixed-effect model was used to describe the course of survival over time, based on study-specific and time-specific aggregated survival data.
RESULTS
We included 42 observational studies reporting on 1689 ECPR and 375 751 CCPR procedures. Of the included studies, 25 included adults, 13 included children and 4 included both. In adults, survival curves decline rapidly over time (ECPR 37.2%, 29.8%, 23.8% and 19.1% versus CCPR-shockable 36.8%, 7.2%, 1.4% and 0.3% for 15, 30, 45 and 60 min low-flow, respectively). ECPR was associated with a statistically significant slower decline in survival than CCPR with initial shockable rhythms (CCPR-shockable). In children, survival curves decline rapidly over time (ECPR 43.6%, 41.7%, 39.8% and 38.0% versus CCPR-shockable 48.6%, 20.5%, 8.6% and 3.6% for 15, 30, 45 and 60 min low-flow, respectively). ECPR was associated with a statistically significant slower decline in survival than CCPR-shockable.
CONCLUSIONS
The short-term survival of ECPR and CCPR-shockable patients both decline rapidly over time, in adults as well as in children. This decline of short-term survival in relation to low-flow duration in ECPR was slower than in conventional cardiopulmonary resuscitation.
Trial registration
Prospero: CRD42020212480, 2 October 2020.
Keywords: Heart arrest, Cardiac arrest, Cardiopulmonary resuscitation, Extracorporeal cardiopulmonary resuscitation, Survival
Despite mounting research, cardiac arrest remains a major cause of death worldwide [1].
INTRODUCTION
Despite mounting research, cardiac arrest remains a major cause of death worldwide [1]. Although improvements have been seen in the conventional cardiopulmonary resuscitation (CCPR), in the education of laypersons to perform basic life support, and in the use of defibrillators or automated external defibrillators, survival outcomes after cardiac arrest remain poor. Previous studies have shown that various prognostic factors are associated with short-term survival, including age, initial cardiac rhythm, time to return of spontaneous circulation (ROSC), whether or not bystanders attempt basic life support, and how quickly this basic life support is provided [2–4]. Of these prognostic factors, time to ROSC has a major influence on this short-term survival and—unlike factors such as age—is also a factor over which we have some control [5].
One way of shortening the low-flow duration could be the use of extracorporeal cardiopulmonary resuscitation (ECPR). ECPR involves applying an extracorporeal membrane oxygenator during CPR and can be used in both out-of-hospital cardiac arrest (OHCA) and in-hospital cardiac arrest (IHCA). Due to transportation times, the use of ECPR in OHCA patients can be more challenging, whilst most hospitals use maximum low-flow durations in order to be eligible for ECPR. Despite the possible advantages of the use of ECPR to shorten low-flow duration and improve outcomes, one should take into account that this therapy is expensive and could result in severe complications.
The low-flow duration is defined as the elapsed interval from resuscitation until one of 3 endpoints: ROSC, artificial return of circulation using ECPR or death. ECPR treatment is used to limit ischaemic damage and buy time to resolve the cause of cardiac arrest. In a randomized controlled trial, survival outcome of ECPR patients was much higher than in CCPR patients [6]. Two recent meta-analyses have shown the potential benefit on short-term survival of adding ECPR to CCPR [7, 8]. It is clear that the longer the low-flow state is present, the poorer the survival outcome will be [9–11]. The most recent meta-analysis showed that a shorter low-flow duration in ECPR is associated with improved survival [8]. Previously propensity-matched observational studies show different results ranging from improved outcomes for ECPR to no difference in outcomes for ECPR and CCPR [12–17].
Information regarding low-flow duration and survival will contribute to organize ECPR treatment as efficient as possible. Therefore, the aims of this systematic review and meta-analysis were therefore to determine (i) the relation of survival and low-flow duration of both ECPR and CCPR and (ii) if ECPR and CCPR have different survival curves in relation to low-flow duration. We intended to stratify these analyses for adults and children and for OHCA and IHCA.
MATERIALS AND METHODS
This systematic review and meta-analysis are performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [18] and it is listed in the PROSPERO register with registration number CRD42020212480. Study eligibility criteria, search study selection, data extraction and risk of bias assessment are described in detail in the Supplementary Material, Appendix S1. In short, a systematic search in Embase, Medline, Web of Science and Google Scholar was performed from inception up to April 2021. All studies including at least 20 OHCA or IHCA patients treated with ECPR or CCPR were included. Two researchers screened and included the studies and performed data extraction, including study characteristics, patient characteristics, clinical characteristics and outcomes.
Statistical analysis
The study characteristics, patient characteristics, clinical characteristics and outcomes were described for each study. The studies were grouped by adults, children or both. We report continuous variables using mean and standard deviation (SD) or median and interquartile ranges (IQR) where applicable. We report categorical variables using numbers and percentages.
As primary outcome, we studied the relation of short-term survival and low-flow duration. As secondary outcome, the short-term survival in relation to low-flow duration of ECPR and CCPR were compared. Outcome measures differed by study. Studies in which hospital survival was mentioned, this was used as the primary outcome parameter. For studies in which only neurologically intact survival was mentioned, or 30-day, 90-day or 1-year survival: all these outcome parameters were considered as ‘hospital survival’. Including all of these patients will result in a lower short-term survival rate than the actual survival rate and therefore this will be an underestimation of short-term survival. Actual numbers would be higher. If only intensive care unit survival was mentioned in the study, these studies were excluded. In case no individual data were available, we contacted the authors for the exact low-flow durations, followed by a reminder after 1 month if necessary. If we received no response or if the data were not available, we used the time intervals of low-flow duration.
In order to be able to analyse the data of the studies which reported individual data, we had to cluster the low-flow durations with a minimum of 5 events per group. For the studies of which only low-flow duration intervals were available, we calculated the average value of every time interval per study, as this was the best possible approximation for the value of each individual patient. Next, for the maximum values, mostly a value ‘higher than’ (>) a specific value was mentioned. We approximated this value by calculating the mean (SD) and determined low-flow duration belonging to the 87.5 percentile. If there was no mean value mentioned in the articles, we used the median (IQR).
Linear mixed effect (LME) models were used to describe the course of survival over time in relation to ECPR versus CCPR, while accounting for clustering of data within a study. The 2log probability of survival was modelled as a function of time, based on study- and time-specific aggregated survival data, which were weighed according to the inverse variance method. Results are presented as exponential functions. We analysed data of adults and children separately. In adults and in children, we combined shockable and non-shockable initial cardiac rhythm for ECPR patients due to the limited amount of data. For CCPR patients, shockable initial cardiac rhythm (CCPR-shockable) and non-shockable initial cardiac rhythm (CCPR-non-shockable) were analysed separately. We compared ECPR patients to CCPR-shockable patients as shockable rhythm is usually an inclusion criterion for ECPR. Also, ECPR patients are mostly selected based on patient criteria which increase the chances of favourable outcome, as CCPR-shockable patients are the patients with expected better outcomes than in CCPR-non-shockable patients. By selecting the CCPR-shockable patients, mostly patients with cardiac cause of arrest will be included. In case studies including CCPR patients in which initial cardiac rhythm was not classified, were excluded for the analysis.
RESULTS
Study selection
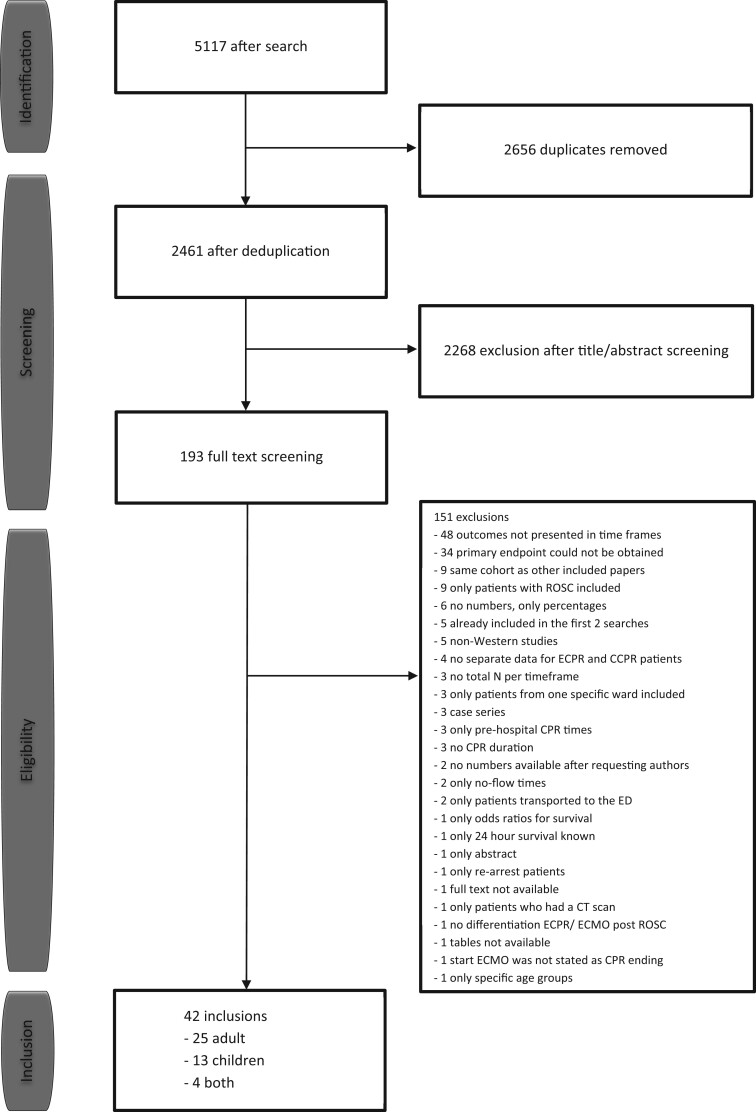
We identified 5117 studies with our search, after removing duplicates, there were 2461 studies remaining. After title and abstract screening, 193 studies were selected for full-text screening. Of those, 48 were excluded because the outcomes were not presented in time intervals, 34 were excluded because the primary endpoint could not be obtained, 9 were excluded because of multiple studies in the same cohort, 9 studies were excluded because these only included patients achieving ROSC and 51 were excluded for other reasons, as shown in Fig. 1. Finally, we included 42 studies (N = 417,133) [9, 11, 14, 19–57], of which 25 studies included only adult patients, 13 studies included only children and 4 studies included both.
Figure 1:
Flowchart of study selection using the PRISMA guidelines.
Characteristics
Table 1 shows the study characteristics and a more detailed description is shown in Supplementary Material, Table S100. Three of the adult studies included patients treated with ECPR or CCPR, 11 studies included only patients treated with ECPR and 10 included only patients treated with CCPR. In the studies in children, 1 study included patients treated with ECPR or CCPR, 5 studies included only patients treated with ECPR and 7 studies included only patients treated with CCPR. In the studies including both adults and children, 1 study included patients treated with ECPR or CCPR, 2 studies included only patients treated with ECPR and 1 study included only patients treated with CCPR.
Table 1:
Study characteristics
| No | Study | Year | Adults/Children/Both | Study design | Inclusion period | Setting (single/multi-centre) | Maximum follow-up duration | ECPR/CCPR/both | Patient number | Follow-up duration included in analyses | Mean low-flow duration (min) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Studies in adults | |||||||||||
| 1 | Adnet [9] | 2017 | Adults | Descriptive | 2011–2015 | Multi | 30 days | CCPR | 27 301 | 30 days | 30.0 (10.0–50.0) |
| 2 | Bartos [51] | 2020 | Adults | Case-control | 2015–2019 | Multi | Hospital stay | Both | 1134 | Hospital stay | ECPR 60.0 ± 1.0 |
| CCPR 35.0 ± 1.0 | |||||||||||
| 3 | Chen [21] | 2008 | Adults | Descriptive | 1994–2005 | Single | 5 years | ECPR | 135 | Hospital stay | 52.8 ± 37.2 |
| 4 | Chou [22] | 2014 | Adults | Case-control | 2006–2010 | Single | Hospital stay | Both | 66 | Hospital stay | ECPR 59.7 ± 34.1 |
| CCPR 49.4 ± 34.6 | |||||||||||
| 5 | Dumot [23] | 2001 | Adults | Descriptive | 1994–1995 | Single | Hospital stay | CCPR | 445 | Hospital stay | NR |
| 6 | Ferguson [24] | 2008 | Adults | Descriptive | 2001–2005 | Single | 6 months | CCPR | 256 | Hospital stay | NR |
| 7 | Fjolner [45] | 2017 | Adults | Descriptive | 2011–2015 | Single | Hospital stay | ECPR | 21 | Hospital stay | 121.0 (55.0–192.0) |
| 8 | Goldberger [25] | 2012 | Adults | Descriptive | 2000–2008 | Multi | Hospital stay | CCPR | 64 339 | Hospital stay | 17.0 (10.0–26.0) |
| 9 | Grunau [27] | 2018 | Adults | Descriptive | 2007–2011 | Multi | Hospital stay | CCPR | 5674 | Hospital stay | 13.0 (7.2–20.8) |
| 10 | Haneya [47] | 2012 | Adults | Descriptive | 2007–2012 | Single | Hospital stay | ECPR | 85 | Hospital stay | 51.0 ± 35.0 |
| 11 | Kim [14] | 2014 | Adults | Cohort | 2006–2013 | Single | 3 months | Both | 499 | 3 months | ECPR 62.0 (47.0–89.0) |
| CCPR 35 (21.0–50.0) | |||||||||||
| 12 | Mandigers [55] | 2021 | Adults | Descriptive | 2010–2020 | Single | Hospital stay | ECPR | 84 | Hospital stay | 51.0 (37.0–80.0) |
| 13 | Murakami [52] | 2020 | Adults | Descriptive | 2010–2015 | Single | 30 days | ECPR | 1630 | 30 days | NR |
| 14 | Nagao [34] | 2016 | Adults | Descriptive | 2005–2012 | Multi | 30 days | CCPR | 28 2183 | 30 days | NR |
| 15 | Otani [35] | 2018 | Adults | Descriptive | 2009–2017 | Single | Hospital stay | ECPR | 135 | Hospital stay | 47.0 (43.0–57.0) |
| 16 | Park [50] | 2019 | Adults | Descriptive | 2013–2016 | Multi | Hospital stay | ECPR | 689 | Hospital stay | NR |
| 17 | Pionkowski [36] | 1983 | Adults | Descriptive | 1978–1982 | Single | Hospital stay | CCPR | 565 | Hospital stay | NR |
| 18 | Pound [53] | 2020 | Adults | Descriptive | 2017–2018 | Multi | Hospital stay | CCPR | 152 | Hospital stay | 6.0 (2.0–18.0) |
| 19 | Reynolds [38] | 2016 | Adults | Descriptive | 2007–2010 | Multi | Hospital stay | CCPR | 11 368 | Hospital stay | 20.0 (12.0–27.3) |
| 20 | Rosenberg [39] | 1993 | Adults | Descriptive | 1988–1989 | Multi | Hospital stay | CCPR | 300 | Hospital stay | NR |
| 21 | Siao [57] | 2020 | Adults | Descriptive | 2012–2017 | Single | Hospital stay | ECPR | 112 | Hospital stay | 46.0 (35.0–57.0) |
| 22 | Valentin [48] | 1995 | Adults | Descriptive | 1989–1991 | Single | Hospital stay | CCPR | 253 | Hospital stay | 30.7 (SD/IQR not mentioned) |
| 23 | Wang [42] | 2014 | Adults | Cohort | 2007–2012 | Single | Hospital stay | ECPR | 230 | Hospital stay | OHCA 67.5 ± 30.6 |
| IHCA 44.4 ± 24.7 | |||||||||||
| 24 | Wengenmayer [11] | 2017 | Adults | Cohort | 2010–2016 | Single | Hospital stay | ECPR | 133 | Hospital stay | 59.6 ± 5.0 |
| 25 | Yukawa [44] | 2017 | Adults | Descriptive | 2011–2015 | Single | Hospital stay | ECPR | 79 | Hospital stay | 45.0 (40.0–56.5) |
| Studies in children | |||||||||||
| 26 | Bembea [19] | 2013 | Children | Descriptive | 2000–2014 | Multi | Hospital stay | ECPR | 593 | Hospital stay | 48.0 (28.0–70.0) |
| 27 | Ganesan [46] | 2018 | Children | descriptive | 2012–2014 | Single | Hospital stay | CCPR | 137 | Hospital stay | 20.0 (SD/IQR not mentioned) |
| 28 | Goto [26] | 2016 | Children | Descriptive | 2005–2012 | Multi | 30 days | CCPR | 12 877 | 30 days | NR |
| 29 | Innes [49] | 1993 | Children | Descriptive | 1990–1991 | Single | 1 year | CCPR | 41 | 30 days | NR |
| 30 | Kalloghlian [29] | 1998 | Children | Descriptive | 1989–1992 | Single | Hospital stay | CCPR | 234 | Hospital stay | NR |
| 31 | Kramer [54] | 2020 | Children | Descriptive | 2005–2016 | Single | Hospital stay | ECPR | 72 | Hospital stay | 60.0 (42.0–80.0) |
| 32 | Lopez [31] | 2004 | Children | Descriptive | 1998–1999 | Multi | 1 year | CCPR | 283 | 1 year | NR |
| 33 | Lopez [30] | 2013 | Children | Descriptive | 2007–2009 | Multi | Hospital stay | CCPR | 502 | Hospital stay | NR |
| 34 | Matos [32] | 2013 | Children | Descriptive | 2000–2009 | Multi | Hospital stay | Both | 3419 | Hospital stay | NR |
| 35 | Meert [56] | 2019 | Children | Descriptive | 2009–2015 | Multi | 1 year | ECPR | 147 | 1 year | NR |
| 36 | Morris [33] | 2004 | Children | Cohort | 1995–2002 | Single | Hospital stay | ECPR | 64 | Hospital stay | 50.0 (SD/IQR not mentioned) |
| 37 | Rathore [37] | 2016 | Children | Descriptive | 2011–2012 | Single | 1 year | CCPR | 314 | Hospital stay | 10.0 (3.0–30.0) |
| 38 | Sivarajan [41] | 2011 | Children | Descriptive | 1990–2006 | Single | 2 year | ECPR | 37 | Hospital stay | 30.0 (15.0–50.0) |
| Studies in adults and children | |||||||||||
| 39 | Chen [20] | 2016 | Both | Descriptive | 2012 | Single | Hospital stay | Both | 382 | Hospital stay | 28.0 (10.0–50.0) |
| 40 | Hendrick [28] | 1990 | Both | Cohort | 1986–1988 | Single | 1–18 months | CCPR | 90 | Hospital stay | NR |
| 41 | Shinn [40] | 2009 | Both | Descriptive | 2004–2006 | Single | Hospital stay | ECPR | 50 | Hospital stay | 51.1 ± 27.8 |
| 42 | Younger [43] | 1999 | Both | Descriptive | 1991–1998 | Single | Hospital stay | ECPR | 23 | Hospital stay | NR |
Study characteristics of the included papers.
CCPR: conventional cardiopulmonary resuscitation; ECPR: extracorporeal cardiopulmonary resuscitation; IHCA: in-hospital cardiac arrest; IQR: interquartile range; OHCA: out-of-hospital cardiac arrest; SD: standard deviation.
Patient and clinical characteristics are shown in Supplementary Material, Table SA. For the adult studies, 1470 patients treated with ECPR and 375 751 patients treated with CCPR were included. For the studies in children, 1140 patients treated with ECPR and 17 653 patients treated with CCPR were included. For the studies including both adults and children, 111 patients treated with ECPR and 436 patients treated with CCPR were included.
Quality assessment
All available studies had an observational design: therefore, the overall quality of evidence was low. With respect to this low quality of evidence, we used the Newcastle-Ottawa Scale (NOS) to distinguish of quality within the included studies (Supplementary Material, Table SB).
Outcomes
The short-term survival percentages we present are calculated using the following LME models. In adult ECPR patients (combining shockable and non-shockable initial cardiac rhythms): Hospital survival (%) = 2(5.5383–(0.02139*time)), time is being given in min of low-flow time. In adult CCPR-shockable patients: Hospital survival (%) = 2(7.5645–(0.1574*time)). Due to one highly influencing study, no LME model could be created for adult CCPR-non-shockable patients. In paediatric ECPR patients (combining shockable and non-shockable initial cardiac rhythms): Hospital survival (%) = 2(5.5139–(0.00442*time)). In paediatric CCPR-shockable patients: Hospital survival (%) = 2(6.8488–(0.08312*time)). In paediatric CCPR-non-shockable patients: Hospital survival (%) = 2(4.4677–(0.0598*time)). In order to compare the ECPR and CCPR-shockable patients, we first arbitrarily determined a difference of 5% survival as clinically relevant. Next, we tested if there is any statistical difference between the course of the LME of ECPR and CCPR-shockable patients.
In 39 of the 42 studies, short-term survival was available, the remaining 3 studies 3 months/1 year survival was included as short-term survival. The survival outcomes are shown in Table 2. In adults, short-term survival ranged from 9.3% to 46.4% in ECPR, and from 5.4% to 39.5% in CCPR. In children, short-term survival ranged from 34.4% to 40.6% in ECPR, and from 9.1% to 46.3% in CCPR. In the studies including both adults and children, short-term survival ranged from 19.4% to 36.0% in ECPR, and from 11.0% to 16.5% in CCPR. In Supplementary Material, Table S500, we summarized the outcomes stratified for OHCA and IHCA patients, for the studies in which this information was available.
Table 2:
Outcomes
| No | Study | Short-term survival (hospital/30 day) |
Long-term survival (3 months/6 months/1 year) |
Survival with CPC score ≤2 |
|||
|---|---|---|---|---|---|---|---|
| ECPR | CCPR | ECPR | CCPR | ECPR | CCPR | ||
| Studies in adults | |||||||
| 1 | Adnet | 1482 (5.4) | 1249 (4.5) | ||||
| 2 | Bartos | 52 (39.0) | 148 (23.0) | 52 (39.0) | 52 (39.0) | 148 (23.0) | |
| 3 | Chen | 46 (34.1) | 43 (31.9) | 41 (30.4) | |||
| 4 | Chou | 15 (34.9) | 5 (21.7) | ||||
| 5 | Dumot | 104 (23.0) | |||||
| 6 | Ferguson | 32 (13.0) | 16 (6.0) | 15 (5.9) | |||
| 7 | Fjolner | 7 (33.3) | 7 (33.3) | ||||
| 8 | Goldberger | 9912 (15.4) | 7034 (10.9%, 1188 missings) | ||||
| 9 | Grunau | 690 (12.2) | 292 (5.1%, 306 missings) | ||||
| 10 | Haneya | 29 (34.1) | 27 (31.7) | ||||
| 11 | Kim | 9 (16.4) | 86 (19.4) | 8 (14.5) | 44 (9.9) | 8 (14.5) | 36 (8.1) |
| 12 | Mandigers | 24 (28.6) | |||||
| 13 | Murakami | 32 (37.6) | 14 (16.5) | ||||
| 14 | Nagao | 21,658 (7.7) | 9669 (3.4) | ||||
| 15 | Otani | 34 (25.0) | 22 (16.3) | ||||
| 16 | Park | 13 (9.3) | 7 (5.0) | ||||
| 17 | Pionkowski | 262 (46.4) | |||||
| 18 | Pound | 60 (39.5) | 43 (28.3) | ||||
| 19 | Reynolds | 1232 (10.8) | 905 (8.0) | ||||
| 20 | Rosenberg | 82 (23.5) | |||||
| 21 | Siao | 45 (40.2) | 41 (36.6) | 34 (30.4) | |||
| 22 | Valentin | 50 (19.8) | 44 (17.4) | ||||
| 23 | Wang | 74 (32.2) | 58 (25.2) | ||||
| 24 | Wengenmayer | 19 (14.3) | |||||
| 25 | Yukawa | 17 (21.5) | 11 (13.9) | ||||
| Studies in children | |||||||
| 26 | Bembea | 241 (40.6) | 108 (18.2%, 125 missings) | ||||
| 27 | Ganesan | 27 (19.7) | 21 (15.3) | ||||
| 28 | Goto | 1167 (9.1) | 325 (2.5) | ||||
| 29 | Innes | 19 (46.3) | 16 (39) | ||||
| 30 | Kalloghlian | 66 (28.2) | |||||
| 31 | Kramer | 26 (36.1) | 22 (30.6) | 19 (26.4) | |||
| 32 | Lopez | 98 (34.6) | 94 (33.2) | ||||
| 33 | Lopez | 197 (39.2) | 104 (88.9) | ||||
| 34 | Matos | 78 (34.4) | 876 (27.4) | ||||
| 35 | Meert | 32 (22.1) | 39 (30.5) | ||||
| 36 | Morris | 23 (35.9) | 26 (35.6) | 5 (50.0%, 3 missings) | |||
| 37 | Rathore | 44 (14.0) | 35 (11.1) | 27 (8.6) | |||
| 38 | Sivarajan | 14 (37.8) | 12 (32.4) | 4 (10.8) | |||
| Studies in adults and children | |||||||
| 39 | Chen | 7 (19.4) | 38 (11.0) | ||||
| 40 | Hendrick | 15 (16.5) | |||||
| 41 | Shinn | 16 (32.0) | |||||
| 42 | Younger | 9 (36.0) | |||||
Survival outcome and neurologic favourable outcome for all included studies. Values are presented as number (%).
CCPR: conventional cardiopulmonary resuscitation; CPC: cerebral performance category; ECPR: extracorporeal cardiopulmonary resuscitation.
Primary and secondary outcome
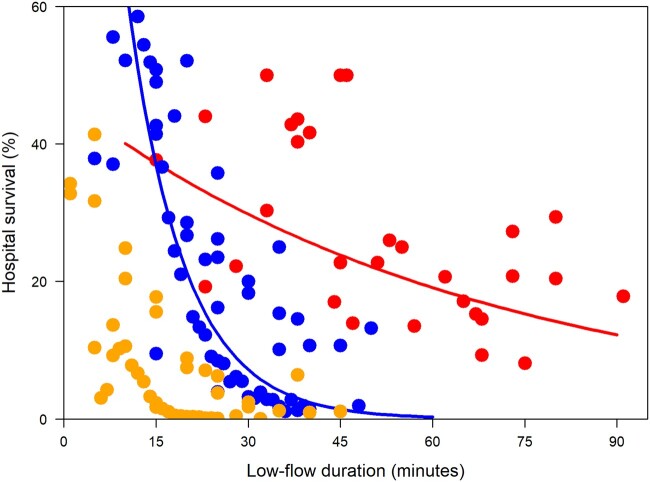
In adults, both survival curves of ECPR patients and CCPR-shockable patients showed a decline in survival with increase of low-flow duration. When comparing the survival curves of adults, the decline in survival outcome for increasing low-flow duration was significantly slower (P < 0.01) in patients treated with ECPR than in CCPR-shockable patients, as shown in Fig. 2. Short-term survival at 15 min low-flow duration was 37.2% in ECPR and 36.8% in CCPR-shockable. In ECPR, short-term survival declined, from 34.5% at 20 min to 29.8% at 30 min, 23.8% at 45 min and 19.1% at 60 min. In CCPR-shockable, short-term survival declined, from 21.4% at 20 min to 7.2% at 30 min, 1.4% at 45 min and 0.3% at 60 min. The difference in survival outcome was at least 5% higher in ECPR than in CCPR-shockable starting from 16.5 min. This difference increased to 22.6% at 30 min and 18.8% at 60 min low-flow duration. Unfortunately, we were unable to estimate a linear mixed model for CCPR-non-shockable patients due to major influence of one study.
Figure 2:
Relation between low-flow duration in minutes and hospital survival in percentage in adult patients treated with extracorporeal cardiopulmonary resuscitation (ECPR, red diagonal line: Hospital survival (%) = 2(5.5383–(0.02139*time (in min)))), conventional cardiopulmonary resuscitation (CCPR) due to shockable initial cardiac rhythms (blue parabole: Hospital survival (%) = 2(7.5645–(0.1574*time (in min)))), CCPR due to non-shockable initial cardiac rhythms (yellow dots no line). Calculated using LME models shown above. Due to one highly influencing study, no LME model could be created for CCPR patients with non-shockable cardia rhythm. LME: linear mixed effect (A color version of this figure appears in the online version of this article).
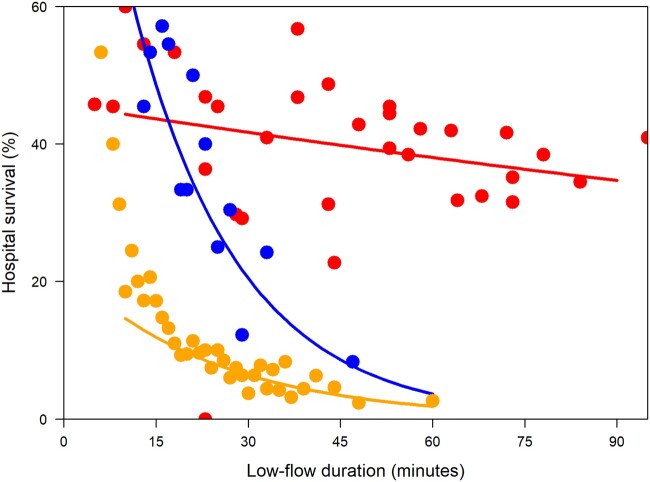
In children, all of the survival curves of ECPR patients, CCPR-shockable patients, and CCPR-non-shockable patients showed a decline in survival with increase of low-flow duration. When comparing the survival curves of children, the decline in survival outcomes for increasing low-flow duration was significantly slower (P < 0.01) in patients treated with ECPR than in CCPR-shockable patients, as shown in Fig. 3. In ECPR, short-term survival declined from 43.6% at 15 min to 41.7% at 30 min, 39.8% at 45 min and 38.0% at 60 min. In CCPR-shockable patients, short-term survival declined from 48.6% at 15 min to 20.5% at 30 min, 8.6% at 45 min and 3.6% at 60 min. In CCPR-non-shockable patients, short-term survival declined from 11.9% at 15 min to 6.4% at 30 min, 3.4% at 45 min and 1.8% at 60 min. The short-term survival was at least 5% higher in ECPR than in CCPR-shockable patients starting from 19.2 min. This difference increased to 21.2% at 30 min, and 34.4% at 60 min low-flow duration.
Figure 3:
Relation between low-flow duration in minutes and hospital term survival in percentage in children treated with extracorporeal cardiopulmonary resuscitation (ECPR, red upper diagonal line: Hospital survival (%) = 2(5.5139–(0.00442*time (min)))), conventional cardiopulmonary resuscitation (CCPR) due to shockable initial cardiac rhythms (blue, parabole line: Hospital survival (%) = 2(6.8488–(0.08312*time (min)))), CCPR due to non-shockable initial cardiac rhythms (yellow lower diagonal line: Hospital survival (%) = 2(4.4677–(0.0598*time (min)))). Calculated using LME models shown above. LME: linear mixed effect (A color version of this figure appears in the online version of this article).
DISCUSSION
The results of our systematic review and meta-analysis show a decline in survival with increase of low-flow duration in both ECPR and CCPR patients. This decline in short-term survival for increasing low-flow duration is significantly slower in patients treated with ECPR than in CCPR-shockable patients, for both adults as children.
The fact that we found a slower decline in survival for increasing low-flow duration in favour of ECPR in both adults and children is in line with the findings of a previous study by Bartos et al. [51]. They recently compared survival outcomes of adults treated with ECPR and CCPR for increasing low-flow durations and found the decline in neurologically favourable survival to be slower in ECPR than in CCPR [51]. Although this study was performed in a smaller group of patients and used a slightly different outcome (neurologically favourable survival rather than just survival), the slower decline in survival for ECPR was similar to that seen in our results. This difference in the decline of short-term survival implies that the sooner ECPR is performed, the greater the chances of a favourable outcome.
The finding in our study that survival outcomes in ECPR are higher than those of CCPR is generally in line with the results of previous studies [7, 8]. In the first randomized controlled trial comparing ECPR to CCPR, Yannopoulos et al. [6] found a short-term survival rate of 43% in ECPR patients and 7% in CCPR patients. Previous systematic reviews comparing patients treated with ECPR and patients treated with CCPR have also shown higher survival outcomes [7, 8] and better neurological outcomes [8] in favour of ECPR. While 2 other recent systematic reviews did not observe this beneficial result for ECPR in OHCA patients, they did observe such a benefit in IHCA patients [58, 59]. Unfortunately, due to a lack of data, we were not able to analyse the outcomes for OHCA and IHCA separately. However, as indicated by Holmberg et al. [59], OHCA patients most likely experience longer low-flow durations than IHCA patients. The outcome difference of OHCA and IHCA is most probably caused by the difference in low-flow duration, the cause of the arrest and the primary rhythm.
With this study, we emphasize the importance of limiting the low-flow duration in both ECPR and CCPR patients. However, in most of the ECPR cases, low-flow durations shorter than 30 min are not always feasible. Especially in OHCA patients, the time until arrival to the hospital varies worldwide between 30 and 60 min [60–62]. Based on our results, we would suggest start preparing for ECPR—retrieve vascular access without dilatation—could be started before cannulation. Definitive cannulation could be started at 20 min low-flow duration. Worldwide, there are limited centres providing ECPR in the field [62], all others can only start ECPR after hospital arrival. Therefore, exploring the means for rapid transportation to the hospital or the ability to perform ECPR in the field is important in an attempt to decrease the low-flow duration. Several studies are recruiting patients or extending their study to research ECPR in the pre-hospital setting [6, 63, 64]. However, the possibilities of these special programmes, are not available globally.
Limitations
This study has some limitations. First, all studies that we included are influenced by confounding by indication. There is still no worldwide consensus regarding which patients are eligible for ECPR. Second, because of the lack of individual patient data we were not able to analyse OHCA and IHCA patients separately. When we stratified the data for ECPR and CCPR in time intervals and tried to stratify for OHCA and IHCA, the amount of data per cell was too limited to analyse. Due to the different causes of cardiac arrest in these 2 groups and the expected difference in the delay before starting CPR, this factor will probably influence the prognosis. Third, a large limitation is the heterogeneity of the study. Despite attempts of reducing this heterogeneity (especially follow-up duration and survival versus neurological favourable outcome), these data were also too limited to analyse. We included a table in the Supplementary Material (Table SE) mentioning the included data. By combining survival outcomes with favourable neurological outcomes in cases where raw survival outcomes were not given, some of the used data will be an underestimation of the survival outcomes. We included these outcomes as short-term survival in order to avoid overestimating. Fourth, all of the available studies are observational studies which hampers strong recommendations based on this study. Fifth, there might be differences in: willingness to start CPR by bystanders, use of automatic external defibrillators and transport times to the nearest hospital, which could not be taken into account. Finally, since we could not include all of the individual patient data, we had to determine average low-flow durations in order to pool the survival data. To overcome such a limitation in future meta-analysis—for example including the randomized controlled trials comparing ECPR and CCPR that are currently being conducted—these data should be pooled based on individual low-flow durations. This will allow for a more accurate comparison between the 2 groups.
CONCLUSION
The short-term survival of ECPR and CCPR-shockable patients both decline rapidly over time, in adults as well as in children. This decline of short-term survival in relation to low-flow duration in ECPR was lower than in CCPR.
SUPPLEMENTARY MATERIAL
Supplementary material is available at ICVTS online.
Supplementary Material
ACKNOWLEDGEMENTS
The authors want to thank Dr W. M. Bramer for his help with the systematic search.
Conflict of interest: Dinis dos Reis Miranda declares having received speaker fees from Xenios GmbH and HillRom GmbH. Diederik Gommers is a member of the medical advisory board of Xenios GmbH and received travel expenses and speaker fees from Xenios and Maquet GmbH. Roberto Lorusso is consultant for Medtronic and Livanova, and member of the medical advisory board of Eurosets srl (Medolla, Italy). Mirko Belliato is a member of the medical advisory board of Eurosets srl (Medolla, Italy) and congress speaker for Hamilton Medical (Bonaduz, Swiss).
Contributor Information
Loes Mandigers, Department of Adult Intensive Care, Erasmus University Medical Center, Rotterdam, Netherlands; Department of Cardiology, Maasstad Hospital, Rotterdam, Netherlands.
Eric Boersma, Department of Cardiology, Erasmus University Medical Center, Rotterdam, Netherlands.
Corstiaan A den Uil, Department of Adult Intensive Care, Erasmus University Medical Center, Rotterdam, Netherlands; Department of Cardiology, Erasmus University Medical Center, Rotterdam, Netherlands; Department of Intensive Care, Maasstad Hospital, Rotterdam, Netherlands.
Diederik Gommers, Department of Adult Intensive Care, Erasmus University Medical Center, Rotterdam, Netherlands.
Jan Bělohlávek, Department of Cardiovascular Medicine, 2nd Faculty of Medicine, Charles University in Prague, Prague, Czech Republic.
Mirko Belliato, UOC Anestesia e Rianimazione 2 Cardiopolmonare, Fondazione IRCC Policlinico San Matteo, Pavia, Italy.
Roberto Lorusso, Cardio-Thoracic Surgery Department, Heart & Vascular Centre, Maastricht University Medical Centre, Cardiovascular Research Institute Maastricht, Maastricht, Netherlands.
Dinis dos Reis Miranda, Department of Adult Intensive Care, Erasmus University Medical Center, Rotterdam, Netherlands.
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.
Author contributions
Loes Mandigers: Conceptualization; Data curation; Formal analysis; Methodology; Writing—original draft. Eric Boersma: Conceptualization; Data curation; Formal analysis; Methodology; Software; Supervision; Writing—review & editing. Corstiaan A. den Uil: Conceptualization; Supervision; Writing—review & editing. Diederik Gommers: Conceptualization; Writing—review & editing. Jan Bělohlávek: Conceptualization; Writing—review & editing. Mirko Belliato: Conceptualization; Writing—review & editing. Roberto Lorusso: Conceptualization; Writing—review & editing. Dinis dos Reis Miranda: Conceptualization; Data curation; Methodology; Supervision; Validation; Writing—review & editing.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Carlos A. Mestres and the other anonymous reviewer(s) for their contribution to the peer review process of this article.
REFERENCES
- 1.World Health Organisation. 2020. https://www.who.int/ (1 February 2020, date last accessed).
- 2. Fernando SM, Tran A, Cheng W, Rochwerg B, Taljaard M, Vaillancourt C. et al. Pre-arrest and intra-arrest prognostic factors associated with survival after in-hospital cardiac arrest: systematic review and meta-analysis. BMJ 2019;367:l6373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patz T, Stelzig K, Pfeifer R, Pittl U, Thiele H, Busch HJ. et al. Age-associated outcomes after survived out-of-hospital cardiac arrest and subsequent target temperature management. Acta Anaesthesiol Scand 2019;63:1079–88. [DOI] [PubMed] [Google Scholar]
- 4. Zhang Q, Qi Z, Liu B, Li C.. Predictors of survival and favorable neurological outcome in patients treated with targeted temperature management after cardiac arrest: a systematic review and meta-analysis. Heart Lung 2018;47:602–9. [DOI] [PubMed] [Google Scholar]
- 5. Lee SH, Jung JS, Lee KH, Kim HJ, Son HS, Sun K.. Comparison of extracorporeal cardiopulmonary resuscitation with conventional cardiopulmonary resuscitation: s extracorporeal cardiopulmonary resuscitation beneficial? Korean J Thorac Cardiovasc Surg 2015;48:318–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA. et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet 2020;396:1807–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ouweneel DM, Schotborgh JV, Limpens J, Sjauw KD, Engstrom AE, Lagrand WK. et al. Extracorporeal life support during cardiac arrest and cardiogenic shock: a systematic review and meta-analysis. Intensive Care Med 2016;42:1922–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Twohig CJ, Singer B, Grier G, Finney SJ.. A systematic literature review and meta-analysis of the effectiveness of extracorporeal-CPR versus conventional-CPR for adult patients in cardiac arrest. J Intensive Care Soc 2019;20:347–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Adnet F, Triba MN, Borron SW, Lapostolle F, Hubert H, Gueugniaud PY. et al. Cardiopulmonary resuscitation duration and survival in out-of-hospital cardiac arrest patients. Resuscitation 2017;111:74–81. [DOI] [PubMed] [Google Scholar]
- 10. Martinell L, Nielsen N, Herlitz J, Karlsson T, Horn J, Wise MP. et al. Early predictors of poor outcome after out-of-hospital cardiac arrest. Crit Care 2017;21:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wengenmayer T, Rombach S, Ramshorn F, Biever P, Bode C, Duerschmied D. et al. Influence of low-flow time on survival after extracorporeal cardiopulmonary resuscitation (eCPR). Crit Care 2017;21:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blumenstein J, Leick J, Liebetrau C, Kempfert J, Gaede L, Groß S. et al. Extracorporeal life support in cardiovascular patients with observed refractory in-hospital cardiac arrest is associated with favourable short and long-term outcomes: a propensity-matched analysis. Eur Heart J Acute Cardiovasc Care 2016;5:13–22. [DOI] [PubMed] [Google Scholar]
- 13. Choi DS, Kim T, Ro YS, Ahn KO, Lee EJ, Hwang SS. et al. Extracorporeal life support and survival after out-of-hospital cardiac arrest in a nationwide registry: a propensity score-matched analysis. Resuscitation 2016;99:26–32. [DOI] [PubMed] [Google Scholar]
- 14. Kim SJ, Jung JS, Park JH, Park JS, Hong YS, Lee SW.. An optimal transition time to extracorporeal cardiopulmonary resuscitation for predicting good neurological outcome in patients with out-of-hospital cardiac arrest: a propensity-matched study. Crit Care 2014;18:535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lasa JJ, Rogers RS, Localio R, Shults J, Raymond T, Gaies M. et al. Extracorporeal Cardiopulmonary Resuscitation (E-CPR) during pediatric in-hospital cardiopulmonary arrest is associated with improved survival to discharge: a report from the American Heart Association's Get with the Guidelines-Resuscitation (GWTG-R) Registry. Circulation 2016;133:165–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Maekawa K, Tanno K, Hase M, Mori K, Asai Y.. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: a propensity-matched study and predictor analysis. Crit Care Med 2013;41:1186–96. [DOI] [PubMed] [Google Scholar]
- 17. Patricio D, Peluso L, Brasseur A, Lheureux O, Belliato M, Vincent JL. et al. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: a retrospective propensity score matched study. Crit Care 2019;23:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bembea MM, Ng DK, Rizkalla N, Rycus P, Lasa JJ, Dalton H. et al. ; American Heart Association’s Get With The Guidelines—Resuscitation Investigators. Outcomes after extracorporeal cardiopulmonary resuscitation of pediatric in-hospital cardiac arrest: a report from the get with the guidelines-resuscitation and the extracorporeal life support organization registries. Crit Care Med 2019;47:e278–85. [DOI] [PubMed] [Google Scholar]
- 20. Chen CT, Chiu PC, Tang CY, Lin YY, Lee YT, How CK. et al. Prognostic factors for survival outcome after in-hospital cardiac arrest: an observational study of the oriental population in Taiwan. J Chin Med Assoc 2016;79:11–6. [DOI] [PubMed] [Google Scholar]
- 21. Chen YS, Lin JW, Yu HY, Ko WJ, Jerng JS, Chang WT. et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: an observational study and propensity analysis. Lancet 2008;372:554–61. [DOI] [PubMed] [Google Scholar]
- 22. Chou TH, Fang CC, Yen ZS, Lee CC, Chen YS, Ko WJ. et al. An observational study of extracorporeal CPR for in-hospital cardiac arrest secondary to myocardial infarction. Emerg Med J 2014;31:441–7. [DOI] [PubMed] [Google Scholar]
- 23. Dumot JA, Burval DJ, Sprung J, Waters JH, Mraovic B, Karafa MT. et al. Outcome of adult cardiopulmonary resuscitations at a tertiary referral center including results of "limited" resuscitations. Arch Intern Med 2001;161:1751–8. [DOI] [PubMed] [Google Scholar]
- 24. Ferguson RP, Phelan T, Haddad T, Hinduja A, Dubin NH.. Survival after in-hospital cardiopulmonary resuscitation. South Med J 2008;101:1007–11. [DOI] [PubMed] [Google Scholar]
- 25. Goldberger ZD, Chan PS, Berg RA, Kronick SL, Cooke CR, Lu M. et al. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet 2012;380:1473–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Goto Y, Funada A, Goto Y.. Duration of prehospital cardiopulmonary resuscitation and favorable neurological outcomes for pediatric out-of-hospital cardiac arrests: a nationwide, population-based cohort study. Circulation 2016;134:2046–59. [DOI] [PubMed] [Google Scholar]
- 27. Grunau B, Puyat J, Wong H, Scheuermeyer FX, Reynolds JC, Kawano T. et al. Gains of continuing resuscitation in refractory out-of-hospital cardiac arrest: a model-based analysis to identify deaths due to intra-arrest prognostication. Prehosp Emerg Care 2018;22:198–207. [DOI] [PubMed] [Google Scholar]
- 28. Hendrick JM, Pijls NH, van der Werf T, Crul JF.. Cardiopulmonary resuscitation on the general ward: no category of patients should be excluded in advance. Resuscitation 1990;20:163–71. [DOI] [PubMed] [Google Scholar]
- 29. Kalloghlian AK, Matthews NT, Khan BA.. Outcome of in-hospital pediatric cardiac arrest. Ann Saudi Med 1998;18:208–11. [DOI] [PubMed] [Google Scholar]
- 30. Lopez-Herce J, Del Castillo J, Matamoros M, Canadas S, Rodriguez-Calvo A, Cecchetti C. et al. ; Iberoamerican Pediatric Cardiac Arrest Study Network RIBEPCI. Factors associated with mortality in pediatric in-hospital cardiac arrest: a prospective multicenter multinational observational study. Intensive Care Med 2013;39:309–18. [DOI] [PubMed] [Google Scholar]
- 31. Lopez-Herce J, Garcia C, Dominguez P, Carrillo A, Rodriguez-Nunez A, Calvo C. et al. Characteristics and outcome of cardiorespiratory arrest in children. Resuscitation 2004;63:311–20. [DOI] [PubMed] [Google Scholar]
- 32. Matos RI, Watson RS, Nadkarni VM, Huang HH, Berg RA, Meaney PA. et al. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation 2013;127:442–51. [DOI] [PubMed] [Google Scholar]
- 33. Morris MC, Wernovsky G, Nadkarni VM.. Survival outcomes after extracorporeal cardiopulmonary resuscitation instituted during active chest compressions following refractory in-hospital pediatric cardiac arrest. Pediatr Crit Care Med 2004;5:440–6. [DOI] [PubMed] [Google Scholar]
- 34. Nagao K, Nonogi H, Yonemoto N, Gaieski DF, Ito N, Takayama M. et al. Duration of Prehospital resuscitation efforts after out-of-hospital cardiac arrest. Circulation 2016;133:1386–96. [DOI] [PubMed] [Google Scholar]
- 35. Otani T, Sawano H, Natsukawa T, Nakashima T, Oku H, Gon C. et al. Low-flow time is associated with a favorable neurological outcome in out-of-hospital cardiac arrest patients resuscitated with extracorporeal cardiopulmonary resuscitation. J Crit Care 2018;48:15–20. [DOI] [PubMed] [Google Scholar]
- 36. Pionkowski RS, Thompson BM, Gruchow HW, Aprahamian C, Darin JC.. Resuscitation time in ventricular fibrillation–a prognostic indicator. Ann Emerg Med 1983;12:733–8. [DOI] [PubMed] [Google Scholar]
- 37. Rathore V, Bansal A, Singhi SC, Singhi P, Muralidharan J.. Survival and neurological outcome following in-hospital paediatric cardiopulmonary resuscitation in North India. Paediatr Int Child Health 2016;36:141–7. [DOI] [PubMed] [Google Scholar]
- 38. Reynolds JC, Grunau BE, Rittenberger JC, Sawyer KN, Kurz MC, Callaway CW.. Association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation 2016;134:2084–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rosenberg M, Wang C, Hoffman-Wilde S, Hickam D.. Results of cardiopulmonary resuscitation. Failure to predict survival in two community hospitals. Arch Intern Med 1993;153:1370–5. [DOI] [PubMed] [Google Scholar]
- 40. Shinn SH, Lee YT, Sung K, Min S, Kim WS, Park PW. et al. Efficacy of emergent percutaneous cardiopulmonary support in cardiac or respiratory failure: fight or flight? Interact CardioVasc Thorac Surg 2009;9:269–73. [DOI] [PubMed] [Google Scholar]
- 41. Sivarajan VB, Best D, Brizard CP, Shekerdemian LS, d'Udekem Y, Butt W.. Duration of resuscitation prior to rescue extracorporeal membrane oxygenation impacts outcome in children with heart disease. Intensive Care Med 2011;37:853–60. [DOI] [PubMed] [Google Scholar]
- 42. Wang CH, Chou NK, Becker LB, Lin JW, Yu HY, Chi NH. et al. Improved outcome of extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest—a comparison with that for extracorporeal rescue for in-hospital cardiac arrest. Resuscitation 2014;85:1219–24. [DOI] [PubMed] [Google Scholar]
- 43. Younger JG, Schreiner RJ, Swaniker F, Hirschl RB, Chapman RA, Bartlett RH.. Extracorporeal resuscitation of cardiac arrest. Acad Emerg Med 1999;6:700–7. [DOI] [PubMed] [Google Scholar]
- 44. Yukawa T, Kashiura M, Sugiyama K, Tanabe T, Hamabe Y.. Neurological outcomes and duration from cardiac arrest to the initiation of extracorporeal membrane oxygenation in patients with out-of-hospital cardiac arrest: a retrospective study. Scand J Trauma Resusc Emerg Med 2017;25:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Fjølner J, Greisen J, Jørgensen MRS, Terkelsen CJ, Ilkjaer LB, Hansen TM. et al. Extracorporeal cardiopulmonary resuscitation after out-of-hospital cardiac arrest in a Danish health region. Acta Anaesthesiol Scand 2017;61:176–85. [DOI] [PubMed] [Google Scholar]
- 46. Ganesan RG, Das S, Parameswara N, Biswal N, Pabhu A.. Survival after in-hospital cardiac arrest among paediatric patients—a descriptive study. J Clin Diagn Res 2018;12:SC04–9. [Google Scholar]
- 47. Haneya A, Philipp A, Diez C, Schopka S, Bein T, Zimmermann M. et al. A 5-year experience with cardiopulmonary resuscitation using extracorporeal life support in non-postcardiotomy patients with cardiac arrest. Resuscitation 2012;83:1331–7. [DOI] [PubMed] [Google Scholar]
- 48. Valentin A, Karnik R, Donath P, Winkler WB, Slany J.. Outcome of cardiopulmonary resuscitation in hospitalized patients. Resuscitation 1995;30:217–21. [Google Scholar]
- 49. Innes PA, Summers CA, Boyd IM, Molyneux EM.. Audit of pediatric cardiopulmonary-resuscitation. Arch Dis Child 1993;68:487–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Park JH, Song KJ, Shin SD, Ro YS, Hong KJ.. Time from arrest to extracorporeal cardiopulmonary resuscitation and survival after out-of-hospital cardiac arrest. Emerg Med Australas 2019;31:1073–81. [DOI] [PubMed] [Google Scholar]
- 51. Bartos JA, Grunau B, Carlson C, Duval S, Ripeckyj A, Kalra R. et al. Improved survival with extracorporeal cardiopulmonary resuscitation despite progressive metabolic derangement associated with prolonged resuscitation. Circulation 2020;142(11):877–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Murakami N, Kokubu N, Nagano N, Nishida J, Nishikawa R, Nakata J. et al. Prognostic impact of no-flow time on 30-day neurological outcomes in patients with out-of-hospital cardiac arrest who received extracorporeal cardiopulmonary resuscitation. Circ J 2020;84:1097–104. [DOI] [PubMed] [Google Scholar]
- 53. Pound G, Jones D, Eastwood GM, Paul E, Hodgson CL; ANZ-CODE Investigators. Survival and functional outcome at hospital discharge following in-hospital cardiac arrest (IHCA): a prospective multicentre observational study. Resuscitation 2020;155:48–54. [DOI] [PubMed] [Google Scholar]
- 54. Kramer P, Mommsen A, Miera O, Photiadis J, Berger F, Schmitt KRL.. Survival and mid-term neurologic outcome after extracorporeal cardiopulmonary resuscitation in children. Pediatr Crit Care Med 2020;21:e316–24. [DOI] [PubMed] [Google Scholar]
- 55. Mandigers L, den Uil CA, Bunge JJH, Gommers D, Dos Reis Miranda D.. Initial arterial pCO2 and its course in the first hours of extracorporeal cardiopulmonary resuscitation show no association with recovery of consciousness in humans: a single-centre retrospective study. Membranes (Basel) 2021;11:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Meert KL, Guerguerian AM, Barbaro R, Slomine BS, Christensen JR, Berger J. et al. ; Therapeutic Hypothermia After Pediatric Cardiac Arrest (THAPCA) Trial Investigators. Extracorporeal cardiopulmonary resuscitation: one-year survival and neurobehavioral outcome among infants and children with in-hospital cardiac arrest. Crit Care Med 2019;47:393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Siao FY, Chiu CW, Chiu CC, Chang YJ, Chen YC, Chen YL. et al. Can we predict patient outcome before extracorporeal membrane oxygenation for refractory cardiac arrest? Scand J Trauma Resusc Emerg Med 2020;28:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chen Z, Liu C, Huang J, Zeng P, Lin J, Zhu R. et al. Clinical efficacy of extracorporeal cardiopulmonary resuscitation for adults with cardiac arrest: meta-analysis with trial sequential analysis. Biomed Res Int 2019;2019:6414673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Holmberg MJ, Geri G, Wiberg S, Guerguerian AM, Donnino MW, Nolan JP. et al. ; International Liaison Committee on Resuscitation’s (ILCOR) Advanced Life Support and Pediatric Task Forces. Extracorporeal cardiopulmonary resuscitation for cardiac arrest: a systematic review. Resuscitation 2018;131:91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Funada A, Goto Y, Tada H, Teramoto R, Shimojima M, Hayashi K. et al. Duration of cardiopulmonary resuscitation in patients without prehospital return of spontaneous circulation after out-of-hospital cardiac arrest: Results from a severity stratification analysis. Resuscitation 2018;124:69–75. [DOI] [PubMed] [Google Scholar]
- 61. Gregers E, Kjærgaard J, Lippert F, Thomsen JH, Køber L, Wanscher M. et al. Refractory out-of-hospital cardiac arrest with ongoing cardiopulmonary resuscitation at hospital arrival—survival and neurological outcome without extracorporeal cardiopulmonary resuscitation. Crit Care 2018;22:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Lamhaut L, Hutin A, Puymirat E, Jouan J, Raphalen JH, Jouffroy R. et al. A pre-hospital extracorporeal cardio pulmonary resuscitation (ECPR) strategy for treatment of refractory out hospital cardiac arrest: an observational study and propensity analysis. Resuscitation 2017;117:109–17. [DOI] [PubMed] [Google Scholar]
- 63. Singer B, Reynolds JC, Davies GE, Wrigley F, Whitbread M, Faulkner M. et al. ; International ECMO Network (ECMONet). Sub30: protocol for the Sub30 feasibility study of a pre-hospital Extracorporeal membrane oxygenation (ECMO) capable advanced resuscitation team at achieving blood flow within 30 min in patients with refractory out-of-hospital cardiac arrest. Resusc Plus 2020;4:100029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. DdR M. ON-SCENE Initiation of Extracorporeal CardioPulmonary Resuscitation During Refractory Out-of-Hospital Cardiac Arrest (ON-SCENE). Clinicaltrials.gov 2020. https://clinicaltrials.gov/ct2/show/NCT04620070 (1 February 2020, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.