Abstract
Background
The neglected tropical disease (NTD) sector is adapting to the uncertain circumstances of coronavirus disease 2019 (COVID-19). The development of the Risk Assessment and Mitigation Action (RAMA) tool was driven by partners of the programme Accelerating the Sustainable Control and Elimination of NTDs (hereafter called Ascend) to enable countries to recommence NTD activities following the World Health Organization advisories of April and July 2020. This article explores the advantages of the RAMA process for NTD delivery.
Methods
The analysis used interview transcripts with NTD practitioners in Cote d'Ivoire, Guinea, Liberia and Nigeria and results from the monitoring of compliance with COVID-19 mitigation measures in Nigeria.
Results
Three themes emerged from the results: adaptability and innovation, collaboration and government ownership and preparedness.
Conclusions
The advantages of the RAMA tool suggest its importance in mitigating the transmission of COVID-19 during NTD delivery. There is the potential for the tool to be adapted for use throughout future pandemics.
Keywords: COVID-19, mitigation, NTDs, risk assessment, transmission
Introduction
Following the World Health Organization (WHO) advisory in April 2020 recommending that neglected tropical disease (NTD) activities be postponed until further notice due to the risks associated with coronavirus 2019 (COVID-19), governments paused activities. This decision was a concern for NTD programmes as interruptions to programmes would delay the achievement of 2030 elimination targets.1 While the underlying epidemiology of each disease, period of delay and implementation of remedial strategies will all influence the ultimate impact of postponement on the progress of NTD programmes towards elimination,2 some—such as schistosomiasis—have greater transmissibility. Delays in interventions will therefore have an even more profound impact. When resurgence of NTDs is rapid in high-transmission areas, it takes longer to get back on track.3,4 Forty-four percent of the 109 countries that responded to the last WHO pulse survey on continuity of essential health services during the COVID-19 pandemic reported disruptions to NTD services, with 60% reporting disruptions to large-scale NTD preventative chemotherapy campaigns.5 The longer-term implications of COVID-19 for NTD elimination and control will be unclear for years to come.6 In July 2020, WHO guidance advised that activities could resume with mitigation measures in place.7 The WHO guidance outlined a decision-making framework for the implementation of mass drug administration (MDA), active case-finding activities and population-based surveys for NTDs in the context of the COVID-19 pandemic and suggested mitigation measures to be considered to decrease the risk of transmission of COVID-19. The WHO also published a mass gathering COVID-19 risk assessment tool for generic events.8 This served as guidance for authorities and event organisers when planning mass gatherings and assisted in identifying risks and appropriate mitigation measures.
While the WHO provides technical leadership for health programmes, the mass gathering tool was for generic, non-health-specific events, so the risks and mitigations were not always applicable to NTD activities such as MDA. Therefore, in response to the WHO guidance and tool, the Ascend programme—alongside national ministries of health (MoHs) in project-supported countries—adapted the WHO mass gathering tool for generic events into a tool that addressed considerations for NTDs. This became the Risk Assessment and Mitigation Action (RAMA) tool.9 Three tools were developed for MDA, disease-specific assessments (DSAs) and surgeries with the objective of preparing national programmes to respond to the pandemic while ensuring the resumption of NTD activities and protection of communities from COVID-19. The RAMA tool lists NTD activity-specific risks (Annex 1) and mitigation measures (Annex 2) to be considered by national programmes based on the WHO guidance of July 2020. The targeted regions and districts are listed in the tool and the overall risk score calculated through a decision matrix.
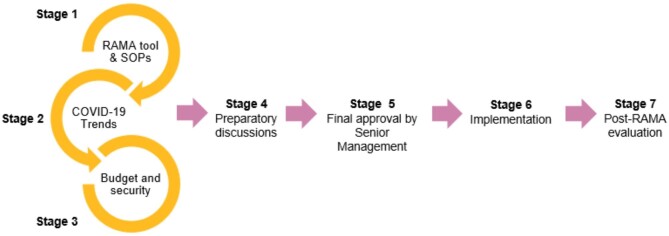
Following a piloting stage, the tool was updated based on learning from initial use and embedded into a risk management process (Figure 1) to ensure compliance with WHO guidance. Alongside the tool, the process includes the monitoring of COVID-19 trends, the technical verification of written COVID-19 standard operating procedures (SOPs), the confirmation of costs associated with mitigation measures such as personal protective equipment (PPE)10 and a security assessment that details risks—aside from COVID-19–that are associated with the operational environment. As part of stage 7 of the RAMA process, programmes have been encouraged to monitor adherence to the COVID-19 SOPs by implementers by using monitoring and evaluation (M&E) tools (Annex 3). Stage 7 also includes a post-activity follow-up, consisting of the submission of updated COVID-19 figures and responses to six follow-up questions (Annex 4) by the team responsible for completing the RAMA process. See Annex 5 for a more detailed summary of stages 1–7.
Figure 1.
Seven stages of the RAMA process.
Developing the RAMA process provided a means by which national programmes, communities, partners and donors could be reassured that programmes were being supported to resume activities safely. However, the RAMA tool and process were produced at a time when COVID-19 case and death rates in NTD-endemic areas were high, national risk mitigation measures were more stringent and the risk appetite of national NTD programmes was lower. As the pandemic has progressed, case and death rates have stabilised, Africa's capacity to manage COVID-19 cases has gradually improved and public health measures have relaxed.11 Nonetheless, application of the RAMA tool and process remains relevant, as it is adaptable to the local COVID-19 situation within the administrative divisions of each country. The RAMA process provides a framework for adaptation by programmes and is not a one-size-fits-all approach. The RAMA process will remain dynamic as the pandemic progresses.
This article documents an evaluation of the RAMA process through semistructured interviews and results from the monitoring of compliance with COVID-19 SOPs to assess how the RAMA process has assisted countries to resume implementation of activities within the confines of COVID-19 restrictions. It explores how the learnings may benefit NTD programmes and other health programmes in the future, beyond COVID-19.
Methods
Semistructured interviews with MoHs
Four semistructured interviews were conducted with key informants within the NTD team of the MoHs in Cote d'Ivoire, Guinea, Liberia and Nigeria in November 2020. The interviews employed a blend of closed- and open-ended questions (Annex 6). Semistructured interviews are recommended when examining unchartered territory and are suitable to this subject matter.12 The interviews were transcribed and key messages grouped into themes for ease of analysis. Transcription provided qualitative evidence of the successes and challenges involved with applying the RAMA process.
Stage 7 of the RAMA process, Nigeria
Monitoring of compliance with COVID-19 SOPs developed through the RAMA process in Nigeria
CommCare, a mobile health application, was utilised by supervisors across Nigeria throughout MDA for schistosomiasis (SCH) and soil-transmitted helminths (STH) in three states and onchocerciasis (OV) and lymphatic filariasis (LF) in seven states to monitor compliance with COVID-19 SOPs by teachers, who were distributing medicine during the SCH/STH MDA and community drug distributors (CDDs) during the OV/LF MDA.
CommCare can be used offline on an Android smartphone with no internet and plots the Global Positioning System location of each entry. The standard community MDA checklist was adapted to include questions on the COVID-19 SOPs (Annex 7). Supervisors used the app to ask questions requiring binary responses (yes or no) and observed practices during MDA to record compliance with the SOPs, entering responses and free-text observations into the digital checklist. The number of days for the training of CDDs was extended to allow time for the recording of compliance with COVID-19 SOPs and observations by supervisors. Each state deployed 21–35 supervisors, depending on the number of local government areas (LGAs) targeted for MDA and the available budget. Benue deployed 21 supervisors, Kogi 34, Kebbi 28, Kwara 35, Sokoto 34, Kaduna 33 and Zamfara 31.
The results from CommCare have helped to determine the level of preparedness of NTD programmes to implement activities safely after completing the RAMA process. Within this article, the results from stage 7 have been presented and discussed for Nigeria only, as the use of CommCare by the NTD programme eased data collection and analysis.
Six post-activity follow-up questions completed by RAMA team members in Nigeria
Annex 4 lists the questions posed to the RAMA team members after the conclusion of the MDA. Information gathered through CommCare helped to respond to these questions. The responses to these questions helped to identify challenges in implementing the COVID-19 SOPs throughout the activities and whether any COVID-19 cases were attributed to the MDA. For this study, the WHO definition of a confirmed COVID-19 case was used.13
Results
Results from semistructured interviews
The results from the semistructured interviews highlighted three key themes: adaptability and innovation, collaboration and government ownership, and preparedness.
Adaptability and innovation
Interviewees highlighted that the RAMA tool enabled programmes to pre-emptively focus on crowd management mitigations. In Liberia, one of the challenges of social distancing was resolved by positioning one dose pole vertically against a wall to measure the dose per patient and promote physical distance between CDDs and community members instead of the usual method of the CDD holding the dose pole next to the patient.
Recognising the additional constraints that COVID-19 placed on CDDs, countries sometimes extended the treatment period of an MDA to accommodate the need to sanitise dose poles, wash and sanitise hands and maintain physical distancing throughout the MDA. Increasing the number of CDDs during an MDA has depended on need due to the increasing burden on CDDs caused by COVID-19 risk mitigation measures. In Nigeria, the recommended ratio is 1 CDD per 200 community members. While this recommendation has not changed throughout the pandemic, there were cases of communities and health facilities asking for more CDDs due to a heavy burden on existing CDDs caused by the need to adhere to the COVID-19 prevention measures. In these cases, additional CDDs were identified. It should be noted that increasing the number of CDDs per community to reduce workload was a recommendation of the community-directed treatment with ivermectin approach prior to the pandemic. However, in some cases the changing operational environment brought on by COVID-19 has highlighted the importance of this approach.
In Nigeria, the maximum number of trainees at each CDD training session was reduced from 50 to 20 to increase social distancing. The rationale behind this was that 20 trainees could be comfortably seated in the classroom or health centre while adhering to the physical distancing requirement of 2 m. The decreased number of trainees per day increased the total number of training days by two or three, depending on the total number of CDDs to be trained. Similarly in Guinea, due to COVID-19 restrictions, it was necessary to add one additional training day.
In addition to innovative solutions to the changed operational environment of COVID-19, some MDA recommendations that existed prior to COVID-19 have proven to be especially effective in the context of the pandemic. For example, in Liberia, throughout MDA, a disposable spoon was used to limit physical contact when administering tablets to community members. This was as opposed to the CDD placing the tablet into the hand of the community member directly.
Community engagement and awareness-raising around COVID-19 mitigation measures was an ongoing effort. In Guinea, CDDs and supervisors spoke to households about COVID-19 safety measures both at the start and end of each MDA. This enhanced community buy-in. During the RAMA process in Cote d'Ivoire, a guide was developed for implementers indicating measures such as compulsory mask wearing, hand hygiene, social distancing and ventilation of indoor spaces. The NTD programme has been able to raise awareness of COVID-19, helped by widespread knowledge of COVID-19 thanks to government communication efforts.
In Nigeria, advocacy and sensitisation helped people understand COVID-19-related risks, as some communities do not believe that COVID-19 exists. State- and LGA-level coordinators engaged with local communities to inform them of the cause of the hiatus in MDA. The NTD programme supported COVID-19 awareness and sensitisation activities in order that communities understood preventative measures. The programme also engaged communities during religious gatherings.
Collaboration and government ownership
Collaboration was facilitated through the introduction of online meetings in addition to physical ones, during which people were able to exchange information. These meetings included national NTD programme managers and coordinators, district health directors and Sightsavers. There were hybrid meetings with some attendees meeting in person and others joining online due to COVID-19 restrictions. In Liberia and Nigeria, due to low internet coverage in most of the communities, CDDs, teachers and health workers were not included in online meetings. However, in-person meetings at the start of MDA involved CDDs and health workers. In Guinea, district health directors shared information from meetings with CDDs and health workers at the subdistrict level, while some health workers attended online meetings.
In all countries, NTD activities were able to restart due to careful planning, facilitated by the RAMA process. In the case of Guinea, coordination was a major challenge after the introduction of the RAMA process due to the large number of information sources required to complete the documentation. However, regular communication between the MoH and partners improved mutual understanding and facilitated completion of the process. The programme has experienced improvements in national coordination and community engagement since, with a renewed commitment to ensure meaningful participation by community members. Despite uncertainty and challenges, the national NTD programme in Guinea gained support from implementing partners to resume MDA across multiple districts by using the RAMA tool.
In Nigeria, regular engagement and communication with the Nigeria Centre for Disease Control meant that partners could have access to the most up-to-date COVID-19 information and guidance to restart NTD activities. The NTD programme relied on information from other public health programmes to understand any challenges associated with restarting a programme during a pandemic. For example, the NTD programme engaged with malaria programmes to understand how they were carrying out their programmes, what types of materials and PPE were being used and how trainings were run.
There was close collaboration between the NTD programme and COVID-19 response teams during the RAMA process and NTD activities. In Liberia, the COVID-19 response team developed strategic documents, including COVID-19 SOPs, to guide NTD activities. During the RAMA process for the MDA, the NTD programme engaged with the COVID-19 response team to plan surveillance, contact tracing, COVID-19 risk communication and community engagement. The COVID-19 response team facilitated COVID-19 awareness training in the five counties targeted for MDA. In Guinea, daily restitution meetings were conducted between the NTD programme and COVID-19 response team to discuss the safety of beneficiaries. In Nigeria, some NTD programme personnel were drafted into the COVID-19 response team to provide support throughout the pandemic. This assisted the national programme when writing the COVID-19 SOPs and providing COVID-19 updates at stages 1, 2 and 7 of the RAMA process.
Preparedness
There was consensus that the RAMA process has improved preparedness to implement programmes in the COVID-19 context. In Cote d'Ivoire and Nigeria, the RAMA process improved guidance for implementers, covering all key mitigation activities while causing no negative impact to local communities. In Guinea, before completing the RAMA process, implementers in the field were fearful of activities restarting. After completing the RAMA process, information on COVID-19 and preventative measures was shared with households. The interview with the programme in Nigeria emphasised the usefulness of the RAMA process in providing the guidance needed to mitigate COVID-19 risks. The interviewee from the programme in Cote d'Ivoire stated that the RAMA tool was easy to complete and adaptable to each country context.
The national NTD programme in Guinea completed the RAMA tool before undertaking integrated research for leprosy, Buruli ulcer and NTDs, separate from the Ascend programme. The programme also completed the RAMA process for MDA, with distribution being successfully carried out in the Nzérékoré region of Guinea. The RAMA process ensured the involvement of local authorities in NTD control activities and proper orientation for health centre workers and CDDs despite the COVID-19 context.
In Liberia, lessons learned from the Ebola epidemic in 2014–2015 have been carried over to the response to COVID-19. Training of health workers, community engagement and the existing Incident Management System were noted for their significance.
Challenges
A key challenge identified from the interviews was the significant amount of time and effort required to complete the RAMA process. The programme in Cote d'Ivoire suggested reducing the number of steps and shortening the timeframe for stakeholder responses. In Nigeria, the RAMA process was difficult for state-level implementing partners to complete and they asked for additional guidance. It was suggested that there is a need for greater sensitisation of the relevant people and authorities on the RAMA process further ahead of implementation. The programme in Cote d'Ivoire suggested that learnings can be gained from other partners and their tools. However, in Nigeria, Guinea and Liberia, the interviewees stated that the RAMA tool was the only risk assessment tool in operation for NTD programmes.
In Liberia and Cote d'Ivoire, despite the RAMA process, there were risks of mistrust and misinformation relating to COVID-19. Some communities were afraid of the spread of COVID-19 during MDA. Thus there was a need for community engagement and awareness-raising when responding to health issues.
Other non-COVID-19-related challenges mentioned include security threats such as kidnapping and armed robbery, which often complicate implementation in Nigeria.
Results from monitoring of compliance with COVID-19 SOPs developed through the RAMA process
CommCare was deployed in Nigeria to monitor the preparedness of CDDs and teachers to comply with COVID-19 SOPs. This section details the data and summarises the behaviours of CDDs and teachers as observed and recorded by supervisors during MDA. The quantitative results from the CommCare app are shown in Table 1.
Table 1.
Quantitative results from the CommCare app used during school-based SCH/STH and community-based OV/LF MDA
| Teachers who complied with SOPs during SCH/STH MDA, % | CDDs who complied with SOPs during OV/LF MDA, % | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Result | Kaduna n=752 | Niger n=659 | Zamfara n=342 | Taraba n=147 | Niger n=1334 | Kogi n=1240 | Kwara n=826 | Kebbi n=1510 | Sokoto n=2723 | Zamfara n=1420 |
| Correct use of PPE | 99 | 99 | 89 | 99 | 99 | 95 | 95 | 98 | 93 | 93 |
| Complied with social distancing | 99 | 99 | 92 | 97 | 100 | 92 | 90 | 98 | 95 | 91 |
| Knowledge of who to contact in the event of an emergency relating to COVID-19 | 95 | – | 99 | – | – | 92 | 97 | 93 | 89 | 95 |
| Disinfected equipment before use | 97 | – | 98 | – | – | 95 | 98 | 97 | 95 | 94 |
| Administered drugs outdoors | 23 | – | 23 | 12 | 28 | 66 | 69 | 45 | 48 | 45 |
| Used handwashing facilities | 99 | 84 | 92 | 98 | 91 | 93 | 92 | 98 | 93 | 92 |
| Used hand sanitiser | 99 | 95 | 92 | 98 | 96 | 93 | 92 | 98 | 93 | 92 |
In general, during the SCH/STH and OV/LF MDAs, there was high compliance with the SOPs. CDDs and teachers at the community level were provided with PPE. Across the states, 84–99% of CDDs used handwashing facilities, 90–100% complied with social distancing and 89–99% showed correct use of PPE. Throughout the SCH/STH MDA, pupils remained at their desks and took turns walking to the front of the classroom where their height was measured and the appropriate dose of praziquantel was administered. All pupils received the same dose of albendazole. Teachers were educated on the signs and symptoms of COVID-19 and were provided with phone numbers to call in the event of suspected cases. However, across the states, 12–69% of teachers or CDDs administered drugs outside—relatively low rates compared with the other protocols listed in Table 1.
It is important to mention that some indicators were not reported on by state programmes in Niger and Taraba states, managed by the same partner. Further inquiries revealed that the OV/LF programmes in both states did not feel the need to include the indicator on knowledge of who to contact in the event of an emergency relating to COVID-19 or the indicator relating to disinfection of equipment, as these were included in the training of CDDs and thus it was not thought to be necessary to include them. In Niger state, the SCH/STH programme decided not to include the indicator relating to administering drugs outdoors for the same reason.
Results from the six post-activity follow-up questions with RAMA team members
Responses to the post-activity follow-up questions reveal that misinformation and mistrust were a concern. In Kaduna, Kogi, Sokoto and Kwara, there was a notion among community members that COVID-19 did not exist or was political propaganda. Thus community members were not willing to use face masks, despite owning them. A few teachers were seen to be wearing face masks incorrectly or putting them in their pockets. These behaviours were corrected by supervisors. In rural areas of Sokoto, some pupils chose not to use face masks due to the religious belief that nothing would happen to them except what was predestined by God. In Kwara and Zamfara, some did not have access to hand sanitiser due to how much it cost. However, most demonstrated good knowledge of handwashing. Enquiry revealed that the school authority provided face masks for all pupils.
No cases of COVID-19 were attributed to any of the NTD-related activities. No participant was reported to have been affected by COVID-19 during or after the implementation of MDA. In Kaduna, at the start of the MDA, the cumulative COVID-19 figure stood at 228 and rose to 766 at the end of the week. However, CDDs tested negative prior to the training and PPE was provided for all staff, including health workers, CDDs and teachers. Temperature checks were completed by all participants and documented on the attendance sheet. In Niger, there were no COVID-19 cases before MDA. However, during the MDA period, 3 of the 23 LGAs reported two cases each and 3 reported one case each. After MDA, five LGAs reported one case, although these could not be directly linked to the implementation. In Kwara, there was a significant decrease from 111 cases in 2–15 March 2021 across 14 LGAs to 2 in 13–26 April 2021 in 1 LGA. The decrease could be attributed to sensitisation of preventive measures. In Sokoto, Kebbi and Kogi, COVID-19 transmission in the targeted locations remained unchanged and no cases were recorded. No participant was reported to have been affected by COVID-19 during or after implementation.
Discussion
The RAMA process has encouraged programmes to evaluate risk and suggest solutions to enable a continuation of interventions. The results reveal the advantages of the risk assessment process to mitigate the transmission of COVID-19 during NTD delivery.
Advantages
For national programmes, this different operational environment has meant rethinking how to distribute medicines safely. Thus it has been essential for programmes to utilise a strong risk assessment process to resume activities.6 RAMA has strengthened mobilisation, as programmes needed to raise awareness with partners and within communities to overcome hostility and fears of COVID-19. These mechanisms for engaging with communities existed prior to the pandemic but were of particular advantage to the NTD programme during the pandemic for the communication of risks, mitigations and updates on treatments. The RAMA tool encourages community leaders to promote prevention behaviours and combat stigma, discrimination and false information related to COVID-19.
Working under the constraints of COVID-19 generated opportunities for enhanced collaboration. Completing the RAMA process required dedicated time and diverse stakeholders working together. It has encouraged coordination across multiple levels. For example, it requires the MoHs to complete documents with up-to-date national, regional and district-level COVID-19 information. This requires frequent communication between partners and governments at the national and subnational level and information sharing between the national NTD programmes and COVID-19 response teams. The necessity for governments to lead in the completion of the RAMA process shows that national ownership is, by design, central to the process. Inclusion of health workers in online meetings in Guinea encouraged collaboration and information sharing when preparing for NTD activities.
Each of the RAMA tools sets out a rigorous set of questions to be answered by regional technical teams and MoHs. They are asked to identify risk factors, consider how routine activities are to be adapted and review the financial implications of working in a different way. While non-governmental organisation (NGO) partners have adopted the tools as part of larger internal review processes, the tool and process provide a formal mechanism between government and their partners to rigorously assess and restart critical outreach work collaboratively. Such an approach complements overall approaches to strengthening health systems, building resilience and facilitating integration and cross-sector collaboration.
While COVID-19 created uncertainty, the RAMA process has prepared programmes to implement activities in a precarious context. In Nigeria, teams have been able to monitor the SOPs and identify challenges via CommCare. The monitoring results show high levels of programme preparedness among implementers and within communities and a willingness to comply with the mitigation measures. There is demonstrated evidence that the MDAs did not contribute to the spread of COVID-19. Instead, the SOPs created opportunities for participants to be safeguarded. The CommCare app has improved remote supervision and the results show that the RAMA process contributed to the reduction in risk of transmission of COVID-19.
In Nigeria, prior to the COVID-19 pandemic and introduction of the RAMA process, the use of handwashing facilities was not highly prioritised, despite the presence of water, sanitation and hygiene (WASH) campaigns and interventions. This was due to a lack of access to water points in the communities. The consideration of COVID-19 risk mitigation measures has encouraged programmes to make provisions for handwashing facilities and hand sanitiser and has improved coordination between WASH actors, the COVID-19 response team and Sightsavers, with many NTD officers being drafted into the COVID-19 response team across states.
The RAMA tool provides a common standard across countries yet is adaptable to country needs depending on the COVID-19 situation, public health measures or security context. It also draws attention to the geographical specificity of risk at the community level. This adaptability will continue to be important as the pandemic develops.
Challenges and limitations
Despite its advantages, the RAMA process requires time and resources at a time when both are scarce. Challenges include the lack of reliable COVID-19 case records at the district and regional level, the additional workload involved in the completion of the RAMA documentation and challenges in engaging governments in the process.
Low to absent COVID-19 testing capacity and poor reporting systems14 mean that it is difficult to know the true extent of infections within countries.15 It is therefore difficult to know for certain whether COVID-19 cases are attributable to NTD activities. While there are challenges in the validity of information sources, it is important to remain open to non-traditional sources.16 However, some programmes rely on measures such as temperature checks and symptom screening of patients and CDDs, which are less reliable methods of detection than COVID-19 tests.17 It is also challenging when government willingness to promote safe practices during a pandemic is weak. The operational environment in Tanzania18 meant that it was not possible to collect data on COVID-19 cases. This did not match up with the requirements of the RAMA process, so some proxy indicators were put in place on which partners reported.
As mobile platforms such as the CommCare app allow supervisors to correct deviations immediately, this may have resulted in higher reported rates of compliance. For example, a supervisor may have observed more people not wearing masks, but having corrected the behaviour, entered into the app that there was high compliance with use of PPE when at first there was not. It is therefore not clear whether the data reflect deviations that supervisors may have subsequently corrected.
Outdoor administration of drugs was particularly low for the school-based SCH/STH MDA, as classrooms were used. However, the classrooms were well-ventilated and social distancing was encouraged. Overall, there was more outdoor administration throughout the community-based OV/LF MDA. However, there were some instances when the administration occurred within the compound perimeter and was therefore referred to as indoor, despite being outdoors. In some cases, the female religious practice of purdah and consideration for the elderly influenced whether drugs were administered indoors or outdoors. Further investigation into the reasons for low rates of outdoor drug administration is recommended.
Table 1 shows the behaviours as seen and recorded by supervisors during MDA. However, data on the knowledge acquired by the teachers and CDDs throughout the training before the drug distribution were not available and thus it was not possible to compare the levels of understanding of the teachers and CDDs after the training with their observed behaviours during the distribution.
Mitigation measures can be difficult to apply. A wider analysis of the compliance with COVID-19 mitigation measures is needed across other countries. Results vary across different country contexts and there is variation in the challenges encountered depending on the capacity to monitor and levels of sensitisation within communities.
Digital remote supervision tools are not yet available in all countries and so paper-based checklists are relied upon. This does not allow for sophisticated analysis.
The semistructured interviews were conducted in November 2020, when countries were amid an emergency COVID-19 response. It would be valuable to repeat the interviews for an updated reflection of the RAMA process.
The seven-stage RAMA process suited the needs of Sightsavers as the lead partner throughout the Ascend programme. Therefore, while the RAMA tool itself is standardised, it should be expected that different processes will have emerged within other organisations that may have used the RAMA tool. Analyses of the advantages of other risk assessment processes will be useful. There are other risk assessment tools not evaluated within this article. The Cote d'Ivoire programme mentioned the risk assessment tool shared by the US Agency for International Development, which was useful due to its focused design.
Beyond COVID-19 and NTDs
As stated by the programme in Guinea, ‘last time it was Ebola, this time it is COVID’. COVID-19 provides an opportunity to strengthen the health system as a whole and improve collaboration between the government and NGO supporting partners in advancing long-term measures to ensure essential services to eliminate disease can continue safely and to a high standard. The next step will be to take RAMA out of the NTD sector and develop it into a tool that will be used to inform future pandemic mitigation strategies. The WHO COVID-19 Mass Gatherings Technical Expert Group sees potential to take into consideration the specific learnings from the RAMA tool and adapt the original WHO mass gathering risk assessment tool into a tool that could be used by other health sectors that involve mass administration of consumables, such as malaria bed nets.
The structure of the RAMA tool can be applied to other subject matter. A Leave No One Behind Assessment Tool for NTD events has been drafted by Sightsavers alongside a Leave No One Behind toolkit. This aims to provide instructions for service delivery for populations at a higher risk of being excluded because of geography, disability, gender or other inequities. This follows a similar structure to the RAMA tool and reflects WHO guidance for assessing who is being left behind and why.
While the COVID-19 situation across Africa stabilises, it will be important for countries to remain cautious.19 The impact of COVID-19 on public health activities will continue. National programmes should clearly and strategically communicate their COVID-19 guidance and rationale for resuming public health activities with communities and health workers to gain their confidence, support and engagement in adopting various frameworks, processes and tools.
It will be important to update the RAMA process to reflect the improving COVID-19 situation and relaxation of public health measures across countries. A review of the seven-stage process will ensure that it is reflective of these developments. An updated RAMA process should be streamlined while not compromising safety.
Conclusions
COVID-19 risks undermining efforts to eliminate NTDs.20 The RAMA process was developed thanks to global collaboration and has resulted in the safe resumption of NTD activities. Millions of MDA treatments, as well as surgeries and surveys, have safely resumed despite the persisting risks of COVID-19. The effectiveness of its application is a testament to the leadership, relationships and motivation of national NTD programmes.
The challenges of implementing NTD programmes in the context of COVID-19 have necessitated new methods of delivery. The RAMA process has helped guide programmes to conduct activities safely and given the opportunity to think innovatively and ‘outside the box’.
The advantages of the RAMA process are wide-reaching and impactful in building resilience in health systems. It will be important for governments to continue to implement activities while mitigating risk. In many countries, the COVID-19 situation will remain volatile into the future.21 Close collaboration and monitoring of COVID-19 trends going forward will continue to be important. Timely delivery of and equal access to COVID-19 vaccines in African nations remain concerns. Though efforts are under way to improve this,22,23 slow rollout of vaccines creates an environment in which the virus can replicate and evolve, producing variants of concern.24. Thus NTD programmes will continue to use RAMA and assist national governments to integrate the tool into their standard approach to strengthen epidemic preparedness and response for future pandemics. This will significantly avoid delays in delivering much needed treatments.
Sustained collaboration with the WHO is recommended to continue to share experiences from the application of the RAMA tool to inform future risk assessments.
Annex 1
Risks associated with treatment distribution as assessed by the RAMA tool for MDA, disease-specific assessments and surgeries
Will the [NTD activity] be conducted in districts where active community transmission (outbreaks with the inability to relate confirmed cases through chains of transmission) or unexpected deaths have recently been documented?
Will those implementing [NTD activity] in the targeted/assessed regions and districts move outside of those areas during the activity (which may then involve travel between cities/villages within the country that may have local transmission)?
Will supervisors come from districts or cities that have documented active local transmission (community spread)?
Will [NTD activity] include people at higher risk of severe disease (e.g. age ≥60 years or with pre-existing medical conditions such as cardiovascular disease, hypertension, diabetes mellitus, chronic lung disease, cancer, cerebrovascular disease of immunosuppression)?
Will [NTD activity] and associated trainings include practices that increase contact between more than 10 people at a time, including increased touching or shaking of hands, touching of shared materials (dose pole, cups etc) reduced ability to maintain physical distancing or increased verbal interactions?
Will components of the [NTD activity], including training and treatment distribution, be held indoors?
Annex 2
Mitigation actions, as recommended in the RAMA tool for MDA
For the areas being assessed, is there a decision-making authority/body and an agreed procedure to modify, restrict, postpone or cancel the treatment distribution due to the evolving COVID-19 outbreak?
Have MDA organisers and staff undergone additional training and exercises on personal safety procedures and emergency mitigation measures (including those specifically listed in this checklist)?
Is there established collaboration and coordination between organisers, local public health sector, security sectors and other necessary sectors critical to the safety of MDA participants?
Has the national NTD programme notified WHO and/or partner public health authorities, including development agencies, about proposed treatment activities to ensure adequate mobilization of human and financial resources?
Are there agreed, clear and easily understood processes in place for coordination with multiple sectors for disseminating risk communication messages for COVID-19?
Have the relevant organisers and responsible staff been informed on the most up-to-date COVID-19 outbreak guidance? And are the relevant organisers and responsible staff committed to following the available guidance?
Are organisers aware of global and local situation reports as provided by the WHO or local public health authorities?
Do organisers and responsible staff understand the nature of COVID-19, its risks and transmission routes, clinical signs and symptoms, vulnerable population groups and the steps that can be taken by organisers and attendees to limit spread and transmission, the recognised best practices (including respiratory etiquette, hand hygiene, public physical distancing, use of PPE where required, etc) and the travel restrictions adopted by different districts and regions that may affect the MDA?
Have SOPs been adopted for treatment distributions to optimise physical distancing and maximise safety for drug distributors and MDA participants? This plan should also include criteria for limiting the size and number of attendees at trainings, maintaining physical distancing, infection control and criteria for cancellation of the MDA (refer to Command and Control questions).
Have organizers confirmed the availability and willingness of supervisors and community drug distributors to participate in the MDA, verifying that drug distributors and supervisors are not providing emergency services (e.g. for COVID-19 or other outbreaks).
-
Have the MDA organisers acquired/do they have a supply plan for the following supplies to help reduce transmission risk?
PPE: disposable surgical masks and gloves (Recommendations for PPE specific to activities or job tasks may change depending on geographic location, local policy, updated risk assessments for workers and information on PPE effectiveness in preventing the spread of COVID-19).
-
Masks:
In areas without community transmission: use of masks is not required.
In areas with community transmission or with unknown transmission scenario: consider wearing a cloth facial covering.
-
Gloves:
Gloves are required only if direct contact is expected with blood or other body fluids, including secretions or excretions, mucous membranes or broken skin, as in the case of surveys that require finger prick blood or intravenous blood draws.
Gloves should be changed after any interaction in which the distributor touches the skin of another person. Used gloves should be disposed of appropriately in a bin with a lid.
For trainings and meetings: consider supporting them virtually if possible. Where person-to-person trainings are required, limit the number of participants and hold training outdoors while still respecting social distancing guidance. Whether or not disposable masks are used, maximum compliance with hand hygiene and other infection, prevention and control measures is critical to prevent human-to-human transmission of COVID-19.
Hand hygiene (performed frequently): Hand sanitiser and rubs/gels (60–80% alcohol), tissues, frequently replaced soap canisters, paper towels and closed bins for disposing of hygiene products are available for trainings; hand washing stations and associated products are available to drug distributors and recipients during treatment distribution.
Cleaning and disinfection: cleaning materials and disinfectants for dose poles, training materials, cups etc. are available during the implementation of activities.
-
Have organisers made plans to accommodate the following to help reduce transmission risk?
Have organisers introduced exclusionary criteria or exclusive/dedicated sessions to reduce the risk of transmission and minimise risk to vulnerable populations?
Have organisers updated and provided training materials to support the introduction of the new SOPs?
Have organisers provided a cleaning schedule to ensure the venues, vehicles, materials used during trainings and treatment distributions are clean and hygienic? Wiping surfaces and any non-disposable materials and equipment regularly with disinfectant is strongly recommended (before, during and after the MDA and between each community MDA). Also consider environmental measures such as room ventilation and humidification.
Are there established screening measures and procedures (e.g. temperature checks, screening for COVID-19 symptoms) in place for attendees/participants at training venues or community distributions (please explain in the comments section)?
Are hand hygiene protocols in place to protect community members and community drug distributors during MDA? Please describe protocol in comments.
Are digital formats (i.e. WhatsApp, SMS, call back) being used to transfer part or all of community treatment reports?
Have community and local leaders been consulted to ensure physical distancing is followed while conducting house-to-house distribution in order to prevent transmission (e.g. maintain social distancing from health workers, avoid communion vessels for drinking water)?
Are there measures in place to prevent touching and other forms of physical contact between community health workers and household members (especially shaking or touching hands) so that the risk of transmission is reduced during the administration of medicine?
Venue: Ensure administration of treatment is conducted outdoors.
Are there measures in place to reduce intracountry movements of personnel, in particular restricting healthcare providers from travelling outside of the assessed region or district(s)?
Has the time frame for implementing the treatment distribution been increased or the number of health staff or community health workers increased to compensate for delays due to physical distancing and other mitigation actions?
Is there a risk communication strategy in place about physical and social distancing for side events andlcoverage assessments (consolidation and reporting of treatments at health facilities, drug audits, census update, data quality assessments, coverage tools and evaluations, etc)?
Have supervisory tools been adapted to enhance remote supervision by higher levels (district, regional and national teams)? A feedback mechanism should be established with the aim of identifying, reporting and correcting any problems occurring during the planned NTD activity.
MDA coverage: Have local supervisors been trained in the use of supervisory coverage tools for in-process monitoring/reporting by field teams during MDA to identify and address low coverage to avoid mop-up campaigns? For example, daily treatment summary calls with supervisors to monitor daily progress towards achieving distribution goals or the adaption of supervisory checklists on to established apps.
Monitoring of mitigation measures: Have local supervisors been trained in the use of supervisory tools to monitor and correct application of the mitigation strategies?
Is there a risk communication strategy for supervisors and health workers regarding COVID-19? Verify with local authorities whether CDDs and supervisors are not at increased risk by communities who might be hostile to those from COVID-19-affected areas and do not pose a risk of stigmatising communities by their presence.
Are health workers well identified and provided with credentials and/or written authorization to implement/participate in the MDA if approached by security forces?
Do the social mobilisation platforms used to mobilise and inform communities about MDA (television, radio, local dramas, town criers) have the capacity to broadcast information about MDA at this time?
Is there a designated person(s) to lead media activities and be tasked with managing all external communications with national and international government officials, the general public and the media? If yes, please identify the spokesperson in comments and what protocols are in place.
Has public health advice been shared as part of training of all supervisors, community health workers and personnel of all relevant stakeholders before and during the MDA on the following: clinical features of COVID-19, preventive and mitigation measures (especially respiratory etiquette), hand hygiene practices, physical distancing and the meaning of the following measures: quarantine, self-isolation and self-monitoring?
Has information on the COVID-19 at-risk populations been provided to all supervisors, health workers and personnel so they may make an informed decision on their attendance due to the personal risks?
Have organisers/public health authorities reached out to community leaders to promote positive healthy and prevention behaviours and combat stigma, discrimination and false information related to COVID-19?
-
If a person feels unwell/is considered to be a suspected case of an acute respiratory infection (or COVID-19) during training or treatment distribution:
Are measures in place to conduct daily health checks with health workers?
Are there procedures that clearly identify who should be contacted if an attendee/participant shows symptoms of COVID-19? Examples include how attendees should interface with the local healthcare system: a hotline/helpline, mobile applications, outpatient clinics and designated medical facilities that manage patients with COVID-19 infection, their location and contacts mapping, etc.
Is there an agreed protocol on who supervisors or community drug distributors should contact to report suspected cases?
Does the country conduct COVID-19 laboratory diagnostic tests? Is testing available for all MDA health workers if indicated? If yes, please specify in comments the type of COVID-19 diagnostic test(s) your country uses.
-
Are there any surge mechanisms and/or sources in place in the event of a public health emergency during the MDA (i.e. are suspected and confirmed cases of COVID-19 reported in connection with the treatment distribution)?
Do COVID-19 surge arrangements include funding for additional mitigation measures, including a supply plan for health emergencies with suspected and confirmed cases of COVID-19 reported in connection with the treatment distribution?
Do COVID-19 surge arrangements include additional training for organisers and supervisors on COVID-19 clinical features, testing, diagnostics, how to use and utilise PPE and employing isolation measures in case of COVID-19 contact, etc?
Have other community-based health campaigns or schools restarted in the country? Have SOPs been adopted for these activities to optimise physical distancing and maximise the safety of health workers and communities? What is the command and control structure that is in place for these other health campaigns (please provide details under source of verification)?
-
Are health facilities in the targeted implementation unit (IUs) prepared for preventing and managing transmission of COVID-19?
Have health facilities in the targeted IUs been given SOPs for COVID-19 preparedness and prevention in health facilities? These include patients being screened for symptoms of COVID-19 at the entrance of health facilities before being allowed into facilities; where patients become crowded, a triage being set up to quickly identify and separate probable cases for further assessment; health workers wearing protective equipment (face masks and gloves); at least 2 m (arm's length) being maintained between health workers and patients and between patients. Please reference the title of the SOP under Source of Verification.
Do health facilities in the targeted IUs have infrastructure and materials to respond to and manage COVID-19 cases? These include health facilities in the targeted areas having daily preparatory and response checklists; providing well-ventilated waiting areas; information, education and communication materials on COVID-19 being clearly displayed on the walls in the local language; protective equipment and other supplies being in stock; handwashing facilities (running water and soap) being placed strategically within and outside the facility; a garbage bin with lid being available and accessible to patients; at the end of clinic sessions, surfaces and floors being wiped with disinfectants; having an area designated to hold suspected cases outside the health facility; state COVID-19 helpline numbers being displayed in a visible part of the building; and ambulance drivers being trained in how to handle and evacuate suspected cases.
Do health workers at health facilities in the targeted IUs have the capacity to manage COVID-19 cases? This includes facility health workers understanding the major risk factors for the disease and the preventive measures needed to avoid contracting the disease; health workers being aware of the current situation in the country and the IU in which she/he resides and her/his community. Health workers at health facilities should be aware of national guidelines for public health workers on the COVID-19 response.
Annex 3
Recommended methods for the monitoring and evaluation of adherence to COVID-19 SOPs
Semistructured interviews
COVID-19 mitigation supervisory checklist
COVID-19 response monitoring checklist app (CommCare)
Third-party monitoring
WhatsApp
Pre- and post-training knowledge tests
Health facility assessment survey
Daily meetings
Annex 4
Post-activity follow-up questions
To what extent were the key COVID-19 prevention measures (social distancing, mask wearing, handwashing, house-to-house delivery etc.) followed by [health workers] during [NTD activity]?
What, if any, were the key changes/deviations from the recommended SOPs?
What were the barriers or challenges in implementing the revised SOPs?
Did revised SOPs affect the quality of [NTD activity]? In what way? For MDA, evaluate coverage compared with previous rounds.
If there were COVID-19 cases in the community or among [health workers] during the NTD activity, how useful were the revised SOPs in identifying signs and symptoms?
Were there any changes in the transmission category for COVID-19 in the targeted area following [NTD activity]? If so, what factors contributed to the change?
Annex 5
Components of the seven stages of the RAMA process
Stage 1
The appropriate RAMA tool template is completed and submitted for MDA, DSA or surgery. The COVID-19 SOPs are completed in collaboration with the national NTD programme. These include appropriate mitigation measures for health workers to follow during the NTD activity. The RAMA tool and SOPs are reviewed by a technical adviser with expertise in the diseases targeted by the activity in question (e.g. onchocerciasis MDA, or trichiasis surgery).
Stage 2
Up-to-date COVID-19 figures for the previous 14 days for the regions and districts targeted by the NTD activity are submitted.
Stage 3
An activity budget is submitted and reviewed, including a confirmation of costs associated with mitigation measures such as PPE. A security risk assessment is submitted and reviewed. This details risks—aside from COVID-19—that are associated with the operational environment, such as crime, road safety or terrorist threats.
Stage 4
There is a call between the country team, the technical adviser and the COVID-19 coordinator during which outstanding issues and safety concerns are discussed in preparation for stage 5.
Stage 5
This includes the presentation by the country team of the RAMA tool score, COVID-19 situation, COVID-19 SOPs, budget and security situation. Based on the information presented, the activity receives technical approval to proceed in the COVID-19 context.
Stage 6
The NTD activity is implemented, during which time the regional and district-level COVID-19 figures are monitored.
Stage 7
Programmes are encouraged to monitor adherence to the COVID-19 SOPs by implementers by using monitoring and evaluation tools such as COVID-19 supervisory checklists. Stage 7 also includes a post-activity follow-up consisting of the submission of updated COVID-19 figures and responses to six follow-up questions by the team responsible for completing the RAMA process. Stage 7 helps to identify the challenges and successes associated with implementing an NTD activity in the context of COVID-19.
Annex 6
Semi-structured interview questions
How has the RAMA process supported the resumption of the NTD programme?
At what stage is the national NTD programme starting to resume programme activities?
What elements of the RAMA tool did you find the most challenging to complete and why?
Do you feel that there is a good level of understanding of the RAMA tool among the key stakeholders involved?
What do you think is required to address this issue?
What was your experience in completing the tools?
What do you think the perception of the RAMA tool has been among key stakeholders?
What could we learn from other sectors in supporting tools to develop and document risk mitigation strategies?
How do you think the RAMA process will help the national NTD programme to build back better and come back stronger than it was before?
Have you identified any improvements to the programme as a result of completing the RAMA process?
What are some of the challenges in implementing NTD programme activities due to COVID-19 now that you are resuming your activities?
Can you describe how the national NTD programme is being delivered differently from how it was before COVID-19? For example, are there social distancing measures in place when conducting MDAs?
What changes are now required to implement safely?
What do you think that this will mean for the future of NTD implementation?
Is there anything else that you would like to share about your experiences with the RAMA tool and process?
Annex 7
Questions from the digital checklist on CommCare app
| Supervision questions | Options for selection | |
|---|---|---|
| RECORDS | Indicate (Yes/No) | |
| 1 | Is there a community/school-based treatment register available and easily accessible? | Yes or No |
| 2 | Are entries in the community/school-based treatment register correct? | Yes or No |
| 3 | Has the census been updated for this calendar year? | Yes or No |
| TRAINING | ||
| 4 | How many trained CDDs/teachers are in this community/school? | ______ |
| 5 | Have you been trained this year? | Yes or No |
| INTERVENTION SUPPLIES | ||
| 6 | Do you have dose poles for treatment? (If yes, verify) | Yes or No |
| 7 | Is the dose pole properly calibrated (verify using tape measurement)? | Yes or No |
| 8 | Does CDD/teacher know how to use dose pole to determine dosage? Ask to demonstrate. | Yes or No |
| 9 | Did you miss anybody because you did not have a sufficient quantity of drugs? | Yes or No |
| 10 | Which drugs are not sufficient? | 1. PZQ, 2. IVM, 3. ALB, 4. MEB, 5. AZT TAB, 6. AZT POS, 7. TEO |
| 11a | Did anybody complain of side effects when you distributed? | Yes or No |
| 11b | If yes, what type of side effects? (Multiple selection response) | 1. Headache, 2. Vomiting, 3. Diarrhoea, 4. Dizziness, 5. Others) |
| FIELD IMPLEMENTATION – COVID-19 | ||
| 12 | Does the CDD/teacher use personal protective equipment (face masks, hand sanitisers, surface disinfectants) during distribution? | Yes or No |
| 13 | Does the CDD/teacher maintain social distancing of 1–2 m during distribution? | Yes or No |
| 14 | Does the CDD/teacher have an agreed protocol of who to contact to report suspected cases of COVID-19? | Yes or No |
| 15 | Is equipment (e.g. dose poles, registers, drugs, other distribution materials) adequately cleaned and disinfected before and after use? | Yes or No |
| 16 | Age group of respondent (CDD/teacher) | 18–30 y, 31–45 y, 46–59 y, ≥60 y |
| 17a | Did the CDD/teacher receive any of the following items? | 1. Dispensing spatulas/spoons, 2. Dispensing tray, 3. None |
| 17b | If none in 17a, have you set an action point to ensure this is provided? | Yes or No |
| 18 | Do pupils/community members wash or sanitise their hands before receiving medicine? | Yes or No |
| 19 | If treatment happened in school, where did pupils get water for treatment? | 1. Home, 2. School |
| 20 | Are CDD/teachers administering drugs to households/pupils indoors or outdoors? | 1. Indoors, 2. Outdoors |
| 22 | Are there other health campaigns occurring in the community/school with associated COVID-19 risk mitigation strategies in place? | Yes or No |
| 23 | Are you supported by community/school in cash or kind for distributing the drugs? | Yes or No |
| Household survey | ||
| 24 | Sample 10 households to assess community awareness of key COVID-19 messages and MDA (ask at least the household head or any other adult). | |
| 25 | Did members of your household swallow medicine? | Yes or No |
| 26 | Do members of your household use face masks? | Yes or No |
| 27 | Do members of your household practise regular handwashing or sanitising? | Yes or No |
| School pupils survey | ||
| 28 | Sample 10 children to assess their awareness of key COVID-19 messages and MDA (at least two from each class). | |
| 29 | Was the child wearing a face mask at the time of the visit? | Yes or No |
| 30 | Ask the child to mention at least one COVID-19 preventive measure. Then choose from the options provided (multiple selection response). | 1. Social distancing, 2. No sharing of items, 3. Wearing of face mask, 4. Regular handwashing |
| 31 | Can this child demonstrate handwashing correctly? | Yes or No |
| 32 | Did the child swallow the medicine? | Yes or No |
Contributor Information
Ioasia Radvan, Sightsavers, Haywards Heath, RH16 3BZ, UK.
Folake Oluwayemisi Aliu, Sightsavers, Kaduna, P.O. Box 503, Nigeria.
Anthony Bettee, Neglected Tropical Diseases, Ministry of Health, Monrovia, P.O. Box 10-9009, Liberia.
Abdourahim Cisse, Sightsavers, 5673 Conakry, Guinea.
Sonnie Ziama Gbewo, Health Services, Ministry of Health, Monrovia, P.O. Box 10-9009, Liberia.
Nicholas Olobio, Public Health, Federal Ministry of Health, Abuja 900104, Nigeria.
Michel Sagno, National Program Against Neglected Tropical Diseases, Ministry of Health, Conakry, BP 585, Republic of Guinea.
Authors’ contributions
IR conceived the study. IR, FOA, AB, AC, SZG, NO and MS developed and wrote the manuscript. IR edited the manuscript and coordinated edits of the other authors. All authors read and approved the final manuscript.
Acknowledgements
We acknowledge Albi Knight for coordinating the four semistructured interviews.
Funding
This paper was published as part of a supplement financially supported by the UK Foreign, Commonwealth and Development Office (FCDO) (contract number 205249) and Sightsavers. The content of this paper relates to activities supported by FCDO and implemented by Sightsavers and partners as part of the Accelerating the Sustainable Control and Elimination of Neglected Tropical Diseases (Ascend) programme, West and Central Africa Lot.
Competing interests
None declared.
Ethical approval
Not required.
Data availability
The data underlying this article will be shared upon reasonable request to the corresponding author.
References
- 1. World Health Organization . Ending the neglect to attain the sustainable development goals. Available from: https://www.who.int/neglected_diseases/Ending-the-neglect-to-attain-the-SDGs–NTD-Roadmap.pdf [accessed 4 October2021]. [Google Scholar]
- 2. World Health Organization . Impact of the COVID-19 pandemic on seven neglected tropical diseases: a model-based analysis. Available from: https://apps.who.int/iris/bitstream/handle/10665/343993/9789240027671-eng.pdf?sequence=1&isAllowed=y [accessed 4 October2021]. [Google Scholar]
- 3. Hollingsworth TD, Mwinzi P, Vasconcelos Aet al. Evaluating the potential impact of interruptions to neglected tropical disease programmes due to COVID-19. Trans R Soc Trop Med Hyg. 2021;115(3):201–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization . NTDs: countries must adapt and innovate to mitigate COVID-19 disruptions. Available from: https://www.who.int/news/item/20-10-2021-ntds-countries-must-adapt-and-innovate-to-mitigate-covid-19-disruptions [accessed 25 October2021]. [Google Scholar]
- 5. World Health Organization . Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1 [accessed 25 October2021]. [Google Scholar]
- 6. Molyneux DH, Aboe A, Isiyaku Set al. COVID-19 and neglected tropical diseases in Africa: impacts, interactions, consequences. Int Health. 2020;12(5):367–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization . Considerations for implementing mass treatment, active case-finding and population-based surveys for neglected tropical diseases in the context of the COVID-19 pandemic. Available from: https://apps.who.int/iris/bitstream/handle/10665/333499/WHO-2019-nCoV-neglected_tropical_diseases-2020.1-eng.pdf?sequence=1&isAllowed=y [accessed4 October 2021]. [Google Scholar]
- 8. World Health Organization . WHO mass gathering COVID-19 risk assessment tool – generic events. Available from: https://www.who.int/publications/i/item/10665-333185 [accessed 14 October2021]. [Google Scholar]
- 9. Sightsavers . NTD Open Resource Portal. Available from: https://ntd-sightsavers.hub.arcgis.com/ [accessed 28 February2022]. [Google Scholar]
- 10. World Health Organization . Use of medical and non-medical/fabric masks for community outreach activities during the COVID-19 pandemic, based on current WHO guidance. Available from: https://apps.who.int/iris/bitstream/handle/10665/341570/WHO-2019-nCoV-IPC-Masks-Comm-health-care-2021.1-eng.pdf?sequence=1&isAllowed=y [accessed 4 October2021]. [Google Scholar]
- 11. United Nations Africa Renewal . Africa on track to control COVID-19 pandemic in 2022. Available from: https://www.un.org/africarenewal/magazine/february-2022/africa-track-control-covid-19-pandemic-2022#:∼:text=Almost%20two%20years%20after%20Africa,that%20continued%20vigilance%20is%20key [accessed 20 April2022]. [Google Scholar]
- 12. Adams W. Conducting semi-structured interviews. In: Wholey J, Hatry H, Newcomer K, editors. Handbook of practical program evaluation. Hoboken, NJ: John Wiley & Sons; 2015:492–505. [Google Scholar]
- 13. World Health Organization . WHO COVID-19: case definitions. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-Surveillance_Case_Definition-2020.2 [accessed 28 February2022]. [Google Scholar]
- 14. Rutayisire E, Nkundimana G, Mitonga HKet al. What works and what does not work in response to COVID-19 prevention and control in Africa. Int J Infect Dis. 2020;97:267–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chitungo I, Dzobo M, Hlongwa Met al. COVID-19: unpacking the low number of cases in Africa. Public Health Pract. 2020;1:100038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Callaway D, Runge J, Mullen Let al. Risk and the Republican National Convention: application of the novel COVID-19 operational risk assessment. Disaster Med Public Health Prep. 2021;doi: 10.1017/dmp.2020.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nuertey BD, Ekremet K, Haidallah ARet al. Performance of COVID-19 associated symptoms and temperature checking as a screening tool for SARS-CoV-2 infection. PLoS One. 2021;16(9):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Buguzi S. COVID-19: counting the cost of denial in Tanzania. BMJ. 2021;373:n1052. [DOI] [PubMed] [Google Scholar]
- 19. United Nations . Africa experiencing longest-running decline in COVID-19 infections. Available from: https://news.un.org/en/story/2022/04/1116262 [accessed 20 April2022]. [Google Scholar]
- 20. Martínez-Juárez LA, Álvarez-Hernandez DA, Sedas ACet al. Defeating neglected tropical diseases in our new world living with COVID-19. Ther Adv Infect Dis. 2020;7:2049936120971975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tessema SK, Nkengasong JN.. Understanding COVID-19 in Africa. Nat Rev Immunol. 2021;21(8):469–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aborode AT, Olofinsao OA, Osmond Eet al. Equal access of COVID-19 vaccine distribution in Africa: challenges and way forward. J Med Virol. 2021;93(9):5212–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bright B, Babalola CP, Agudu NASet al. COVID-19 preparedness: capacity to manufacture vaccines, therapeutics and diagnostics in sub-Saharan Africa. Global Health. 2021:17:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wilkison E, Giovanetti M, Tegally Het al. A year of genomic surveillance reveals how the SARS-CoV-2 pandemic unfolded in Africa. Science. 2021;374(6566):423–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared upon reasonable request to the corresponding author.