Abstract
Visiting restrictions had to be imposed to prevent the spread of the COVID-19 virus and ensure the safety of long-term care home (LTCH) residents. This mixed method study aimed to explore residents’ and family caregivers’ acceptability of electronic tablets used to preserve and promote contact. Semi-structured individual interviews with 13 LTCH residents and 13 family caregivers were done to study their experiences, as well as the challenges and resources encountered in the implementation and use of videoconferencing. They had to rate, on a scale from 0 to 10, each of the 6 Theoretical Framework of Acceptability’ constructs of the acceptability of the intervention. The results confirm acceptability of videoconferencing, giving residents and caregivers the opportunity to talk to and see each other during the pandemic. Videoconferencing had some benefits, such as being less expensive, and taking less time and effort for family caregivers.
Keywords: Family caregivers, Videoconferencing, Long-term care, Cognitive dysfunction, COVID-19
Introduction
In Canada, long-term care homes saw an unprecedented number of COVID-19 infections and deaths.1 During the first wave of the COVID-19 pandemic, in Quebec for example, almost 80% of COVID-19 deaths across the country were among long-term care residents.2
In an effort to curb the transmission of the virus, authorities imposed significant restrictions on visits, especially in long-term care homes, increasing the feeling of social isolation and loneliness among their residents. Such isolation is associated with the risk of cardiovascular disease, obesity, physical frailty, stroke depression, anxiety, and cognitive decline.3, 4, 5, 6, 7 Lack of stimulation and contact with family and loved ones can be particularly deleterious to cognitively impaired residents, as they are more vulnerable and dependant on their caregivers. It can lead to rapid and severe deterioration in people with Alzheimer's disease and other dementias, whose health is already compromised.8
Family presence plays a vital role in residents’ wellbeing as it improves their quality of life and reduces mortality.9 In Canada, family caregivers provide a wide range of care to their family or friends living with complex conditions, frailty, and impairments,10 , 11 including social, emotional and memory support. Families that were restricted from visiting their relatives during the pandemic were distressed over discontinuation of their care-giving role.12 Some family members were also worried that this situation could affect the ability of residents with dementia to recognize them. The situation was also devastating for family members of residents who died during periods of visit restriction, as they suffered f long-term effects of grief, complicated by being unable to spend their final weeks or months with their loved ones.13
In efforts to mitigate the negative effects of isolation during the pandemic, researchers have suggested the use of technology to preserve residents’ contact with their loved ones as a protective strategy for the maintenance of the mental and physical condition of these older adults.14, 15, 16 To our knowledge, however, an evaluation of the use of technology in long-care facilities to alleviate the negative consequences of isolation on cognitively impaired seniors in Canadian long-term care homes, has yet to be conducted.
The purpose of this study, therefore, is to describe the acceptability of electronic tablets used to preserve and promote contact by cognitively impaired Canadian residents with and their family caregivers.
Material and methods
Study design
In this study, we used a convergent mixed method design. Both quantitative and qualitative approaches were used to collect data, and then integrated them into the interpretation of the overall results.17 This study is part of a larger research project aimed at evaluating the implementation process, viability, and acceptability of interventions aimed at favouring the presence of family caregivers (in person or virtually), as well as the effects on residents and their family caregivers and the related costs.
Setting
In our larger project, we recruited 4 long-term care homes located in the province of Quebec, Canada. Depending on the size of each residence, we recruited convenience samples of 5-10 older residents, as well as one of their family caregivers who regularly communicates with them.
Samples and recruitment
To be eligible to participate, family caregivers must meet the following criteria: (1) Be 18 years of age or older; (2) have a relative with cognitive problems; (3) have a close relative who does not have mental health problems or intellectual disabilities; 4) have a relative who has lived in a long-term care home for at least 1 month. Residents had to satisfy the following criteria: (1) Being cognitively impaired (regardless their stage of cognitive impairment); (2) not being diagnosed with mental health issues or intellectual disabilities; (3) being a resident of the long-term care homes for at least 1 month (4) being able to speak in the region's official language (French).
After identifying potential residents fitting the inclusion criteria, a staff member from every participating LTCF contacted their family caregivers that also fit the inclusion criteria to assess their interest in participating in the research project and being contacted by the research team. A team member followed up to provide them with more details and obtain their consent and a substitute consent for their relatives.
A total of 27 dyads consisting of 27 residents and one of their family caregivers agreed to participate in our larger project. For this analysis, we used data from only 13 dyads from all long-term care homes who chose videoconference as their main method of communication during the period covered by the project. The recruitment of caregivers using videoconference as the main communication mode was very limited, due to the return of in person visits, staffing shortages and work overload in the participating LTCFs.
Intervention
Participating family caregivers who chose to use videoconference as their main communication mode received a document informing them on how to prepare for their meeting with their relative suffering from a neurocognitive disorder.18 In collaboration with family caregivers and facility staff, videoconference meetings were scheduled once a week, with no duration limit and at a time that would be most convenient for all of them.
To be able to use the videoconference, long-term facilities provided residents with electronic tablets. Residents required assistance in many activities of daily living, therefore their care staff (occupational therapist, specialized educator, recreational educator, etc.) were usually involved in organizing and establishing communication with family caregivers. As for family caregivers, they could use the device of their choice to connect to the meetings.
The research team contacted participating caregivers every week to inquire about their videoconference meeting to insure the smooth running of the project.
Data collection
Sociodemographic and clinical data of the participants
Sociodemographic and clinical data of all participants was collected at the beginning of the project. Residents’ sociodemographic and clinical data were collected with the help of staff members. The stage of resident cognitive impairment was assessed by the staff member using the Reisberg scale,19 while functional autonomy was evaluated using the ISO-SMAF score available in each resident's file.20 All scales were completed during the interviews.
Interviews
Following public health recommendations in the context of the COVID-19 pandemic, all interviews were conducted remotely (e.g., by telephone or videoconference).
Semi-structured individual interviews were conducted with 13 dyads using an interview guide inspired by the Theoretical Framework of Acceptability.21 The interviews were designed to uncover the participants’ current experiences in communicating with older adults, as well as the challenges and resources that helped them during the use and implementation of the intervention. Interview guides were presented to three partner caregivers before the beginning of the data collection. Modifications were made following their comments to facilitate participants’ understanding of the questions. The interviews with family caregivers were conducted online and lasted about 1 h. Due to restrictions on visits in long-term care homes, the interviews with residents were conducted face-to face, by staff members who were trained by a member of the research team. Resident interviews lasted a maximum of 10 min. If residents were unable to answer directly, the staff member would describe the residents’ reactions.
Considering the residents’ health condition and cognitive impairment, interviews conducted with them covered only their attitudes and general acceptance of their communication experiences with their family and the videoconferencing intervention. Quantitative data collection on intervention acceptability by family caregivers was conducted at the same time, using the same interview guide as for qualitative data. Family caregivers rated each of the 6 Theoretical Framework of Acceptability’ constructs (Table 1 ) about of the acceptability of the intervention on a scale from 0 to 10, where 10 indicates most favorable acceptability of the intervention (except for the constructs pertaining to cost and burden where the scale is inverted).
Table 1.
Constructs retained in the Theoretical Framework of Acceptability and their definition.21
| Construct | Definition |
|---|---|
| Affective attitude | How an individual feels about the intervention |
| Burden | The perceived amount of effort that is required to participate in the intervention |
| Ethicality | The extent to which the intervention has a good fit with an individual's value system |
| Opportunity costs | The extent to which benefits, profits, or values must be given up when engaging in the intervention |
| Perceived effectiveness | The extent to which the intervention is perceived to be likely to achieve its purpose |
| Self-efficacy | The participant's confidence that they can perform the behaviour(s) required to participate in the intervention |
Data analysis
Qualitative data analysis
This qualitative descriptive study involves both a deductive approach, using intermediate theories and empirical data, and an inductive approach, where residents (n=7) and caregivers (n=6) participated in semi-structured one-on-one interviews. For each interview, the research assistant took detailed notes in the form of real time verbatim. After each interview, a detailed report was written. There was no audio recording of the interviews to provide results in a limited time frame to inform our partners and provide key findings, as required by the terms of funding. We anonymized any identifiable data to protect participants’ privacy.
Using a deductive approach, six constructs from The Theoretical Framework of Acceptability by Sekhon and al. (2017) were used to facilitate the assessment of the intervention's acceptability from the perspectives of participants, based on their experience with the intervention (Table 1): The construct pertaining to intervention coherence was not considered because it did not apply to our intervention (use of tablets). A deductive approach was used to identify emerging themes and subthemes from the narrative data. For calibration, the two research assistants first analyzed a portion of the data independently. They then met with the principal investigator to discuss and agree on the list of themes. A research assistant then analyzed the remaining data, while validating the new themes with the principal investigator and the other research assistant to reach a consensus.
Quantitative data analysis
Quantitative data were analyzed using IBM SPSS Statistics version 28 software. The sociodemographic and construct data were analyzed descriptively, and frequency distributions, means, and medians were calculated.
Mixed methods data analysis
Once the qualitative and quantitative data were analyzed, the findings from both types of analyses (quantitative and qualitative) were merged to observe the convergence and divergence between findings.
Ethical aspects
The study was approved by the CISSS Chaudière-Appalaches Ethics Board (2021-846 - ESMO-ESLD). All participants provided verbal consent to participate in the research project. The information and consent forms were read to the participant who received a copy by email or mail.
In the context where the research team had to recruit people with cognitive problems, the residents’ consent to participate in the project was first obtained from their legal representative. In the absence of a legal representative, the most significant person and capable of consenting to care could provide proxy consent. Once proxy consent was obtained, the care staff had to ensure that verbal or behavioural assent was obtained before asking the resident any questions.
Results
Participants
Ten (10) out of 13 residents of the study were female, with a mean age of 82 years, with moderate to severe cognitive deficit levels (Table 2 ). Iso-SMAF profile scores ranged from 8 to 14, showing significant motor and mental impairment. All participating caregivers were female with a mean age of 60 years. They were mostly family members, mainly residents’ daughters, most of them were retired.
Table 2.
Characteristics of participating residents and their family caregivers.
| Characteristics | Value |
|---|---|
| Residents (n=13) | |
| Age (in years) [mean ± SD (range)] | 81,7 ± 13,4 (58-97) |
| Gender Female [number (%)] |
10 (76,9) |
| Neurocognitive disorders type Alzheimer's disease [number (%)] Mixed dementia [number (%)] Vascular dementia [number (%)] Lewy body Dementia [number (%)] Unspecified dementia [number (%)] |
4 (30,8) 3 (23,0) 1 (7,7) 1 (7,7) 4 (30,8) |
| Functional Autonomy (Iso-SMAF profiles [mean ± SD (range)]) | 10,9 ± 2,2 (8-14) |
| The Global Deterioration Scale (Reisberg Scale) Stage 5 [number (%)] Stage 6 [number (%)] Stage 7 [number (%)] |
3 (23,1) 7 (53,8) 3 (23,1) |
| Time since LTCH admission [Months: mean ± SD (range)] | 31,3 ± 20,9 (7-87) |
| Family caregivers (n = 13) | |
| Age (years) [mean ± SD (range)] | 59,6 ± 10,3 (42-74) |
| Gender Female [number. (%)] |
13 (100) |
| Relationship with the resident Sisterhood/Brotherhood [number. (%)] Daughter/Son [number. (%)] Other [number. (%)] |
2 (15,4) 8 (61,5) 3 (23,1) |
| Education High school diploma [number. (%)] Apprenticeship or other trades certificate [number. (%)] College diploma [number. (%)] Bachelor's degree or higher [number. (%)] No certificate, diploma, or degree [number. %)] |
4 (30,8) 1 (7,7) 3 (23,0) 4 (30,8) 1 (7,7) |
| Job status Employed [number. (%)] Self-employed [number. (%)] Unemployed [number. (%)] Retired [number. (%)] |
3 (23,0) 2 (15,4) 2 (15,4) 6 (46,2) |
Quantitative findings
Quantitative results are shown in Table 3 .
Table 3.
Quantitative results of acceptability of videoconferencing.
| Construct Variables | T2* (n=13) |
|---|---|
| Mean ± Standard Deviation | |
| Affective attitude | 8,6 ± 1,3 |
| Burden | 2,3 ± 2,8 |
| Ethicality | 9,2 ± 1,5 |
| Benefits | 9,1 ± 1,7 |
| Opportunity costs | 1,8 ± 2,4 |
| Perceived effectiveness | 7,1 ± 2,7 |
| Self-efficacy | 8,5 ± 2,7 |
T2 = 3 months after the beginning of the intervention
Family caregivers showed a positive attitude toward the use of videoconferencing (mean score of 8.6 out of 10). The use of tablets had a good fit with their value system (Ethicality mean score 9.2 out of 10), was perceived as an effective tool to establish communication with their loved ones (perceived effectiveness mean score of 7.1 out of 10) and was beneficial (mean score 9.1 out of 10). Moreover, they positively evaluate their capacity for using the tablets (self-efficacy mean score 8.5 out of 10). They perceived that the use of videoconferencing to communicate with residents, required little effort (burden mean score 2.3 out of 10) and was low cost (mean score 1.8 out of 10)
Qualitative findings
Findings are presented below for each theoretical framework of acceptability construct
Attitude
This construct is concerned with residents’ and caregivers’ feelings about using tablets for their communication during a pandemic. Overall, caregivers reported very positive feelings about being able to keep the communication going considering the visiting restrictions imposed due to the pandemic, as expressed by one caregiver:
“We can not go to see her in person, so the tablet allows us to see her. The tablet was a very good idea! She can see us too; it was a great idea. I do not know who had it, but I'm really happy with it.” (LTCH1- Caregiver3)
These feelings were also shared by many residents. When asked about her feelings at the end of the meeting, a resident said:
“I like the little TV because I can see them, and then I can talk to them. I like to talk to my children.” (LTCH1- Resident 5).
Some residents with advanced cognitive deficit, who could not talk, were described by the staff members as reacting positively upon seeing their close relatives on screen or hearing them:
“She smiles, shouts, claps her hands.” (LTCH5-Resident 3).
One of the caregivers added that this means of communication, compared to phone calls, reassured them more about the resident's condition:
“Under the current circumstances, I think it's a very good experience. For my mother, I can not tell, but it is the case for my dad, as well as mine and my siblings… We can see that she's fine. Even if the staff told us she was okay, we would not be able to see her. It makes all the difference to see her. I see how she's dressed, she's clean... Then, I saw a big difference, especially for my dad. They've been married for 70 years, and it's been really good for him. I've seen a difference in his mood.” (LTCH1-Caregiver 4).
Alternatively, some caregivers were happy about the possibility to share photos and videos and show residents familiar things that are not possible in a face-to-face meeting:
“Using the tablet, I can show her my dog. When she used to come to my house, my dog would always lay on top of her. When I showed her my dog, she had a big smile.” (LTCH1-Caregiver 3).
However, the experience was not always pleasant or easy for everyone. Some family members felt that the quality of the virtual communication was not optimal, due to different reasons, such as the short duration of the meetings, the lack of topics of conversation, the poor general health of the residents, generating feelings of sadness:
“I was sad after the call, it reminded me that I could not see them in person.” (LTCH5-Resident 9).
Burden
This construct focuses on the perceived amount of effort that is required to participate in the intervention. According to most caregivers, communicating via tablets can be demanding, especially when the resident is unable to understand or uphold the conversation, due to their condition and the severity of their cognitive deficits:
“It takes a lot of effort. I'm the only one communicating. I keep telling her that I love her, that I think about her every day. It's good to see her, to keep in touch, but it still takes effort because we have to talk a lot on our own.” (LTCH1-Caregiver 1).
The communication might also be more difficult if the meeting environment is noisy:
“There is a lot of noise around, I am always there talking loudly. She understands less, she is less attentive whereas in person, we are in the living room, there are many people. Now it's in the bedroom, so it's better, because it's less noisy.” (LTCH1-Caregiver 6).
Other caregivers pointed out the emotional burden at the end of the call after seeing the resident's state:
“When things do not go so well, we hang up on them, it puts us in a sad state, upset.” (LTCH1-Caregiver 1).
Caregivers highlighted that, depending on the level of functional decline of the residents, it was difficult for them to hold the tablet without the support of staff members. A caregiver suggested adding support to increase their autonomy:
“Be independent with her tablet using ergonomic means. Could initiate the call herself and not have to wait after her call. Depending on someone, sometimes it must be frustrating.” (LTCH4-Caregiver 6).
In addition, sometimes tablets were not optimal to residents’ sensory needs. For example, a caregiver explained how a bigger screen projection could help her father to pay attention to their conversation, compared to the tablets small screen size:
“Using larger screens, such as projecting the meeting onto the television during Zoom meetings, could allow my father to see me in "normal" size, it would be easier to keep his attention.” (LTCH2-Caregiver 2).
Ethicality
This construct centers on the extent to which the use of tablets to maintain communication was perceived to be a good fit with the participants’ ethical values and interests. Upon restrictions on face-to-face meetings, virtual meetings were an alternative for some caregivers to maintain contact with their loved ones. Face-to-face meetings were perceived as more humane and more adapted to interact and take care of the residents.
“In general, I do not like doing facetimes very much since in my opinion, I find it more artificial. Unlike in-person visits, which give opportunities for human interaction. You know I could help her do stuff, comb her hair, etc., but since I can not see her right now, I'm still using FaceTime because there's no other way to talk to her.” (LTCH1-Caregiver 7).
Similarly, some residents preferred the physical presence of their relatives, however they still enjoyed being able to see them.
“I would like better in person but at least with that I see them” (LCTH1-Res 3).
Other caregivers welcomed virtual meetings, focusing on the overall goal, which is to preserve and promote communication, through all possible means:
“The other communication modalities are there when you have no choice. My preferences and values are more related to being present with her in whatever way.” (LTCH1-Caregiver 5).
However, the use of tablets raised privacy issues for some participants. The consistent presence of the staff members during the video calls to ensure a proper functioning of the intervention was reported as uncomfortable:
“It made me uncomfortable that a staff member was standing there while I talked to my mom.” (LTCH2-Caregiver 3).
In response to this, the caregiver made several suggestions for improvement:
“Maybe a stand for the tablet, so the person can not pull the tablet down or push buttons. That way, the tablet would stand on its own, and the staff could leave during the call-I'm uncomfortable, I do not want to talk too long. I always think it's a bad idea to take up staff time like that! So sometimes I limit the amount of time I talk to my mom. Sometimes I could talk to her longer, but I'm uncomfortable! If they had a stand for the tablet to stand on its own, they could just tell us how long we have to make the call and then leave!” (LTCH2-Caregiver 3).
Opportunity cost
This construct is understood as the extent to which the use of tablets was perceived to be advantageous, and to how much time and/or money the participants needed to invest to communicate in this way.
The use of tablets was reportedly perceived as an easier and faster way of communicating. Caregivers were able to have instant access to the call, regardless of the time and place. It also did not generate expenses, as reported by many caregivers. Most of them used their digital devices, such as tablets, laptops, or smartphones to join the videoconference.
Regarding the duration, most caregivers’ virtual meetings did not last longer than their previous face-to-face meetings. However, it was hard for some caregivers to find availability due to conflict between their work schedules and the staff members’ schedule, as well as the resident's care and activities:
“We all have Internet, I had very few drawbacks. The only thing is the availability. It was difficult to get an appointment for the tablet, and it did not last long.” (LTCH5- Caregiver 7).
Perceived effectiveness
This construct refers to the perceived degree of usefulness of the virtual meetings to achieve their purpose of maintaining contact, reducing social isolation, and improving residents’ condition. Most caregivers acknowledged that face-to-face meetings are irreplaceable in terms of quality and effectiveness in communicating with cognitively impaired older adults. For example, one of the participants reported that the resident was more aware and engaged face-to-face compared to videoconference, which lacks the stimulating human contact.
“My in-person visits certainly help to break her isolation, as she is more aware of her physical environment and my presence. In this case, phone calls and video calls are less optimal. Human contact is important. I guess she is more aware when we are there and present than when we make calls.” (LTCH1-Caregiver 6).
Nevertheless, all caregivers agree that during the pandemic, out of all possible options, virtual meetings remain the most effective way to maintain quality contact comparable to face-to-face meetings:
“I think it keeps as much quality contact with the zooms as it does in person. It keeps much better-quality contact than the ones we had over the phone.” (LTCH1-Caregiver 9).
Other caregivers also felt that using the tablets, in the context of visit restrictions, helped to break the isolation that left many residents feeling anxious and lonely:
“It is obvious that during the time of the pandemic the videoconference was a great plus to cut off one's isolation, and even for me and the children I wish it was something that existed even before.” (LTCH5-Caregiver 3).
On the other hand, face-to-face meetings required frequent travels to a long-term care home, which can be physically demanding for some caregivers:
“For sure, my physical movement required more effort to be able to be with him!” (LTCH1-Caregiver 11).
Therefore, tablet use was very much appreciated, especially for caregivers who live in regions far from the facilities and could not visit their relatives frequently:
“I appreciate it because I do not have to move, and I can still see her. I think it's wonderful.” (LTCH4-Caregiver 5).
Self-efficacy
Self-efficacy was defined as participants’ confidence to use tablets and communicate with their relatives. Residents were usually supported by staff members to initiate the call and\or hold the tablets during the meetings. The use of tablets was more complicated for residents suffering from severe cognitive deficits, as it would confuse and irritate some of them. A caregiver described his relative's reactions during the videoconference:
“By video call […] It does not work. He is paralyzed when he sees me. He is lost. He does not understand seeing me on a screen. I wonder if he would get used to it if he tried, but it's too irritating. We waste too much time. It does not work.” (LTCH4-Caregiver 7).
These experiences can impact some caregivers’ confidence in their ability to adopt the required behaviours to communicate with the residents. One caregiver explained how the resident's overall condition created obstacles to providing stimulation and conversing with them:
“Sometimes I'm not sure what to say. Let's say it could not be 1 h, it would be tiring for her, and I run out of ideas.” (LTCH1-Caregiver 1).
Regarding technical aspects of the intervention, many caregivers had used tablets and similar technology in their daily life. However, some older caregivers were unfamiliar with the communication software that was used for virtual meetings, such as Zoom or Teams. A caregiver commented that training might have helped her:
“Maybe have short videos to show them how to use this technology. It would help the staff at the same time. At another facility, people could sign up for classes to learn and create an email address.” (LTCH5-Caregiver 3).
The staff support during virtual meetings increased the sense of competence and confidence of caregivers in this respect. The staff, who often held the tablet for the residents or supervised the operation, would usually interfere to guide caregivers to use the software programs and/or stimulate residents:
“Now I do not feel totally competent, but I'm much more comfortable now than I was before (…) they're dedicated, and they take time, and you do not feel like you're bothering them or that it's asking a lot of them. It's remarkable that they take time like that for me and my mom. They helped me use Zoom, even though we knew a little about it because we've been using Zoom to talk to our children since the pandemic.” (LTCH1-Caregiver 9).
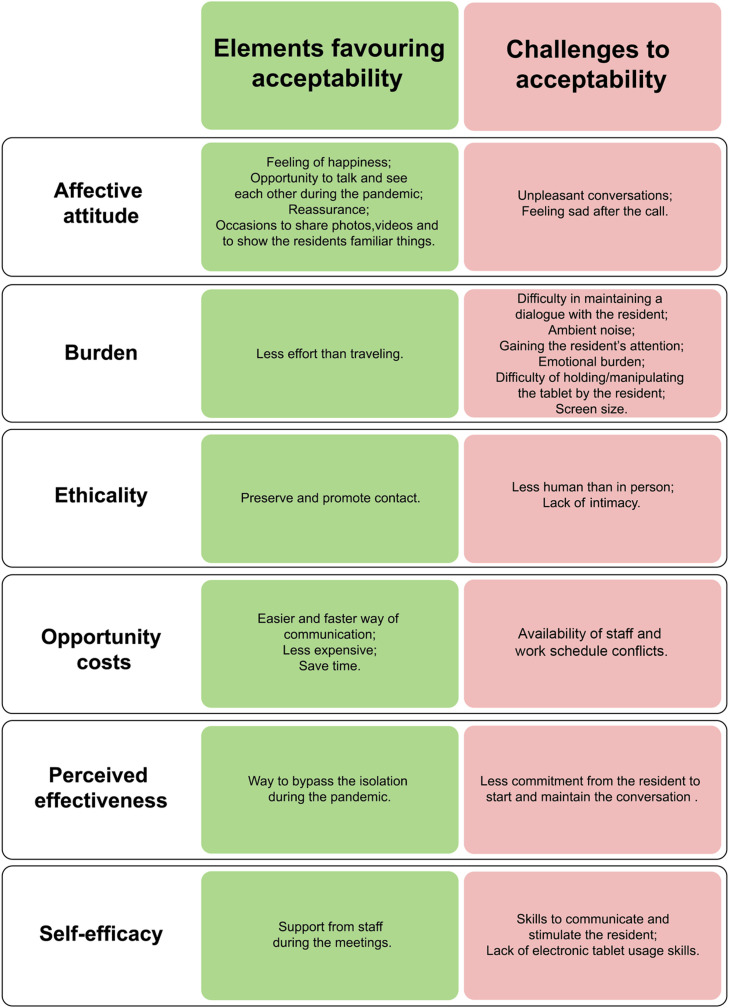
Fig. 1 proposes a summary of the main themes that emerge from the qualitative analysis, including favourable elements and barriers to electronic tablet use acceptability for communication between long-term residents and caregivers.
Fig. 1.
Summary of main findings in relation with the theoretical framework of acceptability constructs.
Discussion
To our knowledge, this is the first study to assess the acceptability of the use of videoconferencing to reduce the feeling of social isolation of older adults with cognitive impairment living in long-term care homes, by maintaining their communication with their caregivers using the theoretical framework of acceptability.21
There is a growing body of international evidence indicating that residents in long-term care homes are particularly vulnerable to social isolation and loneliness.22 However, few studies have been carried out with older adults with moderate to severe cognitive impairment as is the case in the present study. It seems imperative to highlight the vital need for everyone, and especially for older adults with cognitive disorders, to maintain social interactions. The pandemic showed that human care, meeting the fundamental needs of people living in long-term care homes, was neglected, bringing to light crucial elements of the environment in which care is given. Residents of long-term care homes are too often in an environment without sufficient physical stimuli, and without sufficient access to interactions with family caregivers that have personal significance and thus could generate reactions from the residents.
Unfortunately, the pandemic has reduced environmental stimulation. Beyond their cognitive impairments, residents need to be stimulated and to interact socially. We must therefore provide them with the assistance they need to maintain contact with their loved ones. According to family caregivers, videoconferencing allowed opportunities to reduce the residents’ loneliness. It seems to be one of the options to increase older adults’ quality of life by decreasing feelings of isolation and loneliness and increasing feelings of connectedness.23, 24, 25 This is in line with the findings of a systematic review that revealed that videoconferencing could be more effective than telephone calls or written correspondence in reducing the loneliness of older people living in long-term care homes.26 Similarly, out of the context of the pandemic, it can be very useful for families who live far away, or those who are unable to visit, or simply to increase the contact out of their scheduled in-person visits. Some results are consistent with previous research.
In this study, residents and family caregivers showed favourable acceptability and a very positive attitude about being able to communicate by videoconference during the pandemic, as demonstrated by our qualitative and quantitative results. They expressed their satisfaction about their ability to see and talk to their relatives during the pandemic, albeit virtually. These results are consistent with previous research, which reported that older people in long-term care homes were happy and keen to use tablets to talk to their family or friends.27, 28, 29, 30 For example, Boman and colleagues (2014) explored the usability of videophones with older adults with dementia, and revealed positive attitudes towards their use, perceiving them to be worthwhile and enjoyable. Similarly, Siniscarco et al. (2017) concluded that, when in-person visits are limited or impossible, communication via videoconferencing may benefit family or friends living far away to reduce social isolation and mitigate loneliness.
Some family caregivers were pleased to see their resident on video, because it reassured them as to their state of health. The institutionalization of a family member can cause anxiety, and some caregivers would want to verify the quality of care provided to them. They would like to be involved in their care routine and kept up to date as to their condition.23 , 31 They were delighted to be able to show photos and familiar things to residents through the lens of their webcam. Our results are consistent with previous research29 , 32 , 33 among residents showing that videoconferencing gave the opportunity to family members to show familiar elements of their life (e.g., house, pets).
Under regular circumstances, some family caregivers would visit their relatives often. However, some of them would be unable to visit frequently because of other challenges, such as living far away. Moreover, a Canadian survey showed that many family caregivers are also mostly elderly, and traveling frequently to these facilities can be difficult, especially if they are suffering from health issues. Videoconferencing offered family caregivers many benefits such as instant accessibility, ease of activity, affordability, and flexibility. These factors were considered technology-adoption enablers.34 The results support the necessity of exploring new and effective methods to maintain or increase contact between residents and their families and friends, such as videoconferencing, and to maintain these methods well beyond the pandemic.
Some family caregivers experienced technical difficulties during the study, such as weak Wi-Fi and poor image or voice/sound quality. This finding is consistent with the literature.23 , 28 , 33 Similarly, some caregivers reported a certain level of burden associated with the videoconferencing. Some caregivers reported that the tablets that residents used to connect with them were not adapted to their condition. For example, the screen was too small for some visually impaired residents, or the sound was not loud enough. Some residents were unable to hold the electronic tablet without the support of staff members. A solution could be to have the device (iPad or other tablet) supported by a mobile unit, such as that used in another study called ‘Skype on Wheels (SoW) Device’30 in which a familiar telephone handset was also used for sound. A similar installation could be carried out in the long-term care homes and could solve some of these concerns. According to our quantitative results, however, this burden was relatively low.
Finally, although family caregivers and residents seem happy and motivated to meet with each other by videoconference, they reported preferring face-to-face meetings. This means of communication brings different benefits to residents and family caregivers. Regarding the Social Support Behaviors Scale,35 there are four types of social support: Emotional, instrumental, informational, and appraisal. Videoconferencing and in-person visits enable emotional support to residents, and specifically caring, empathy, and love. On the other hand, in-person visits provide instrumental support in terms of concrete assistance. For example, some family caregivers reported that they liked to wash the residents’ hair when they were visiting in person. Thereby, we notice that different types of contact (e.g., virtual, in-person) do not allow for the same levels of social support.
This research has demonstrated the importance of regular contact between family caregivers and residents, regardless of how contact is made. Indeed, the pandemic restricted visits from family caregivers in different ways and levels, which imposed significant impacts on both caregivers and residents. Although face-to-face meetings were perceived as being irreplaceable, it has been revealed that virtual meetings using electronic tablets can be complementary. It is also important to mention that, in most long-term care homes, tablets were not used at all before the pandemic, although videoconferencing is familiar and accessible. The pandemic has highlighted the relevance of videoconference meetings to maintain contact between family caregivers and residents, and to encourage environments to use technology to support caregiving. It offers a novel opportunity to long-term care homes to explore and test how this type of device could be used with residents.
Limitations
Although a sample of 13 dyads was appropriate for a pilot study of a logistically complex intervention, the small sample size may affect the external validity of quantitative data. Moreover, this study was conducted in the context of the COVID-19 pandemic, which constitutes one of its strengths. Yet, the results obtained could differ if a similar study were conducted in a different context, thus limiting the generalizability of the corresponding findings.
Conclusions
This study examined the acceptability among LTCH residents with cognitive disorders and their family caregivers of using electronic tablets to preserve and promote contact in the context of the COVID-19 pandemic. The results suggest that residents and family caregivers appreciated meeting with to each other with videoconferencing. Some challenges were associated with the use of technology, and some adaptations may be needed to make electronic tablets suitable given the physical condition of these residents. Videoconferencing seems to be complementary to face-to-face visits, and we hope that long-term care homes will seize this exceptional opportunity to initiate and expand the use of electronic tablets and of technology in their establishments.
Funding sources
This research project was funded by Canadian Institutes of Health Research with a partnership with Healthcare Excellence Canada (SL3-174031).
Declaration of Competing Interest
There's no conflict of interest to declare.
Acknowledgements
We want to thank Mrs. Micheline Harvey, translator, for the English language review. We would also like to thank Mr. Stéphane Turcotte, biostatistician, for statistical consultation and analysis.
References
- 1.Canadian Institutes for Health Information . CIHI; Ottawa, ON: 2020. Pandemic Experience in the Long- Term Care Sector: How Does Canada Compare with Other Countries?https://www.cihi.ca/sites/default/files/document/covid-19-rapid-response-long-term-care-snapshot-en.pdf [Google Scholar]
- 2.Chouinière, R. Mortalité par COVID-19 au Québec: comparaisons nord-américaines et internationales. Mise à jour du 15 septembre. https://comparaisons-sante-quebec.ca/; 2020.
- 3.Cacioppo J.T., Cacioppo S., Capitanio J.P., Cole S.W. The neuroendocrinology of social isolation. Annu Rev Psychol. 2015;66(1):733–767. doi: 10.1146/annurev-psych-010814-015240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi H., Irwin M.R., Cho H.J. Impact of social isolation on behavioral health in elderly: systematic review. World J Psychiatry. 2015;5(4):432. doi: 10.5498/WJP.V5.I4.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McArthur C., Saari M., Heckman G.A., et al. Evaluating the effect of COVID-19 pandemic lockdown on long-term care residents’ mental health: a data-driven approach in new brunswick. J Am Med Dir Assoc. 2021;22(1):187–192. doi: 10.1016/j.jamda.2020.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Read S., Comas-Herrera A., Grundy E. Social isolation and memory decline in later-life. J Gerontol Ser B. 2020;75(2):367–376. doi: 10.1093/GERONB/GBZ152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simard J., Volicer L. Loneliness and isolation in long-term care and the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21(7):966–967. doi: 10.1016/j.jamda.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Voyer P. 2nd ed. ERPI; Québec: 2013. Soins Infirmiers aux Aînés en Perte D'autonomie. [Google Scholar]
- 9.Tupper S.M., Ward H., Parmar J. Family presence in long-term care during the COVID-19 pandemic: call to action for policy, practice, and research. Can Geriatr J. 2020;23(4):335. doi: 10.5770/CGJ.23.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Statistics Canada. Caregivers in Canada, 2018. https://www150.statcan.gc.ca/n1/daily-quotidien/200108/dq200108a-eng.htm; 2018.
- 11.Parmar J., Brémault-Phillips S., Duggleby W., et al. Caregiver-Centered Care Competency Framework: Education for Health Providers to Support Family Caregivers. 2019 [Google Scholar]
- 12.Hart J.L., Turnbull A.E., Oppenheim I.M., Courtright K.R. Family-centered care during the COVID-19 era. J Pain Symptom Manag. 2020;60(2):e93. doi: 10.1016/J.JPAINSYMMAN.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wallace C.L., Wladkowski S.P., Gibson A., White P. Grief during the COVID-19 pandemic: considerations for palliative care providers. J Pain Symptom Manag. 2020;60(1):e70. doi: 10.1016/J.JPAINSYMMAN.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Noone C., McSharry J., Smalle M., et al. Video calls for reducing social isolation and loneliness in older people: a rapid review. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD013632. Art. No. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsai H.H., Cheng C.Y., Shieh W.Y., Chang Y.C. Effects of a smartphone-based videoconferencing program for older nursing home residents on depression, loneliness, and quality of life: a quasi-experimental study. BMC Geriatr. 2020;20(1):27. doi: 10.1186/s12877-020-1426-2. ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hado E., Friss Feinberg L. Amid the COVID-19 pandemic, meaningful communication between family caregivers and residents of long-term care facilities is imperative. J Aging Soc Policy. 2020;32(4-5):410–415. doi: 10.1080/08959420.2020.1765684. [DOI] [PubMed] [Google Scholar]
- 17.Creswell J.W., Clark V.L.P. 3rd ed. SAGE Publications; Los Angeles: 2018. Designing and Conducting Mixed Methods Research. [Google Scholar]
- 18.CISSS de Chaudière-Appalaches. Aide-mémoire : L'utilisation de la technologie pour communiquer avec votre proche; 2020.
- 19.Reisberg B., Ferris S.H., De Leon M.J., Crook T. The global deterioration scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139:1136–1139. doi: 10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- 20.Hébert R., et al. The functional autonomy measurement system (SMAF) Rev Gériatr. 2003;28:323–336. [Google Scholar]
- 21.Sekhon M., Cartwright M., Francis J.J. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):88. doi: 10.1186/s12913-017-2031-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker S., Warburton J., Waycott J., et al. Combatting social isolation and increasing social participation of older adults through the use of technology: a systematic review of existing evidence. Australas J Ageing. 2018;37(3):184–193. doi: 10.1111/ajag.12572. [DOI] [PubMed] [Google Scholar]
- 23.Demiris G., Oliver D.R., Hensel B., Dickey G., Rantz M., Skubic M. Use of videophones for distant caregiving: an enriching experience for families and residents in long-term care. J Gerontol Nurs. 2008;34(7):50–55. doi: 10.3928/00989134-20080701-02. [DOI] [PubMed] [Google Scholar]
- 24.Sävenstedt S., Brulin C., Sandman P.O. Family members' narrated experiences of communicating via videophone with patients with dementia staying at a nursing home. J Telemed Telecare. 2003;9(4):216–220. doi: 10.1258/135763303322225544. [DOI] [PubMed] [Google Scholar]
- 25.Tsai H.H., Tsai Y.F. Changes in depressive symptoms, social support, and loneliness over 1 year after a minimum 3-month videoconference program for older nursing home residents. J Med Internet Res. 2011;13(4):e93. doi: 10.2196/jmir.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quan N.G., Lohman M.C., Resciniti N.V., Friedman D.B. A systematic review of interventions for loneliness among older adults living in long-term care facilities. Aging Ment Health. 2019;24(12):1945–1955. doi: 10.1080/13607863.2019.1673311. [DOI] [PubMed] [Google Scholar]
- 27.Boman I.L., Lundberg S., Starkhammar S., Nygård L. Exploring the usability of a videophone mock-up for persons with dementia and their significant others. BMC Geriatr. 2014;14:49. doi: 10.1186/1471-2318-14-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siniscarco M.T., Love-Williams C., Burnett-Wolle S. Video conferencing: an intervention for emotional loneliness in long-term care. Act Adapt Aging. 2017;41(4):316–329. doi: 10.1080/01924788.2017.1326763. [DOI] [Google Scholar]
- 29.Tsai H.H., Tsai Y.F. Older nursing home residents' experiences with videoconferencing to communicate with family members. J Clin Nurs. 2010;19(11-12):1538–1543. doi: 10.1111/j.1365-2702.2010.03198.x. [DOI] [PubMed] [Google Scholar]
- 30.Zamir S., Hennessy C.H., Taylor A.H., Jones R.B. Video-calls to reduce loneliness and social isolation within care environments for older people: An implementation study using collaborative action research. BMC Geriatr. 2018;18(1):1–13. doi: 10.1186/S12877-018-0746-Y/TABLES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hertzberg A., Ekman S.L., Axelsson K. Staff activities and behaviour are the source of many feelings: relatives' interactions and relationships with staff in nursing homes. J Clin Nurs. 2001;10(3):380–388. doi: 10.1046/j.1365-2702.2001.00509.x. [DOI] [PubMed] [Google Scholar]
- 32.Hensel B.K., Parker-Oliver D., Demiris G. Videophone communication between residents and family: a case study. J Am Med Dir Assoc. 2007;8(2):123–127. doi: 10.1016/j.jamda.2006.09.01. [DOI] [PubMed] [Google Scholar]
- 33.Mickus M.A., Luz C.C. Televisits: sustaining long distance family relationships among institutionalized elders through technology. Aging Ment Health. 2002;6(4):387–396. doi: 10.1080/1360786021000007009. [DOI] [PubMed] [Google Scholar]
- 34.Lee C., Coughlin J.F. PERSPECTIVE: older adults’ adoption of technology: an integrated approach to identifying determinants and barriers. J Product Innov Manag. 2015;32(5):747–759. doi: 10.1111/JPIM.12176. [DOI] [Google Scholar]
- 35.Langford C.P., Bowsher J., Maloney J.P., Lillis P.P. Social support: a conceptual analysis. J Adv Nurs. 1997;25(1):95–100. doi: 10.1046/j.1365-2648.1997.1997025095.x. [DOI] [PubMed] [Google Scholar]