Abstract
The intravenous iron formulations ferric carboxymaltose (FCM) and ferric derisomaltose (FDI) offer the possibility of administering a large amount of iron in one infusion. This results in faster correction of anemia and the formulations being better tolerated than oral iron formulations. This triad of logistic advantages, improved patient convenience, and fast correction of anemia explains the fact that intravenous iron formulations nowadays are frequently prescribed worldwide in the treatment of iron deficiency anemia. However, these formulations may result in hypophosphatemia by inducing a strong increase in active fibroblast growth factor-23 (FGF-23), a hormone that stimulates renal phosphate excretion. This effect is much more pronounced with FCM than with FDI, and therefore the risk of developing hypophosphatemia is remarkably higher with FCM than with FDI. Repeated use of FCM may result in severe osteomalacia, which is characterized by bone pain, Looser zones (pseudofractures), and low-trauma fractures. Intravenous iron preparations are also associated with other adverse effects, of which hypersensitivity reactions are the most important and are usually the result of a non-allergic complement activation on nanoparticles of free labile iron—Complement Activation-Related Pseudo-Allergy (CARPA). The risk on these hypersensitivity reactions can be reduced by choosing a slow infusion rate. Severe hypersensitivity reactions were reported in < 1% of prospective trials and the incidence seems comparable between the two formulations. A practical guideline has been developed based on baseline serum phosphate concentrations and predisposing risk factors, derived from published cases and risk factor analyses from trials, in order to establish the safe use of these formulations.
Key Points
| Hypophosphatemia, by increasing active FGF-23 concentrations, is an adverse effect of intravenous iron formulations, especially ferric carboxymaltose (FCM). Repeated use of FCM may result in severe osteomalacia. |
| Hypersensitivity reactions are mainly derived from Complement Activation-Related Pseudo-Allergy (CARPA) and may be prevented by a slower infusion rate. The risk of severe hypersensitivity reactions is comparable for all intravenous iron formulations. |
| A practical guideline has been developed, based on serum phosphate concentrations and predisposing risk factors, for the safe use of intravenous iron formulations. |
Introduction
Iron deficiency anemia is a common medical disorder that may be caused by, for instance, gastrointestinal or menstrual blood losses. Besides analysis and treatment of the underlying disorder, treatment with iron supplements is often necessary; however, oral iron formulations are often poorly tolerated, mainly due to gastrointestinal adverse effects. Therefore, 90 years ago, attempts were made to administer iron intravenously but this was discouraged due to its toxicity [1]. The toxicity of these initial iron formulations was confirmed by others [2, 3]; however, in the same report, Nissim reported that intravenous iron was much better tolerated when a solution of saccharated iron oxide was used, created by the dissolution of metallic iron in sucrose [3]. Further experiments by the same group identified that the amount of sugar in the solution, the pH at which precipitation occurred, and the amount of iron administered were critical to prevent toxicity [4]. Further research was aimed at the imitation of ferritin, in which iron oxide was safely encased and transported in the circulation. The protein component of ferritin was replaced by a carbohydrate component because the protein (apoferritin) may have antigenic properties [5]. Indeed, it appeared that the molecular structure of the developed high-molecular-weight iron dextran formulation resembled the molecular structure of ferritin [6].
Nowadays, it is clear that the development of iron salts shielded in a carbohydrate shell had resolved the direct toxicity of free labile iron in the circulation [7]. The first representatives of these carbohydrate formulations on the market were iron dextrans; however, clinical experience with a high-molecular-weight iron dextran (Imferon®, Fisons, UK) revealed life-threatening anaphylactoid reactions [8]. The later-developed low-molecular-weight iron dextran (Infed®, Allergan, USA; and Cosmofer®, Pharmacosmos, Denmark) had a much better safety profile and was generally well tolerated [7, 9, 10] but is less frequently prescribed, at least in Europe [11].
In the late 1990s, two new formulations with comparable characteristics were introduced that were not based on a dextran shell but a smaller carbohydrate core: ferric gluconate (Ferrlecit®, Schein Pharmaceuticals, USA) and iron sucrose (IS; Venofer®, Vifor Pharma, Switzerland; Ferracin®, Acino Pharma AG, Switzerland, and nowadays, also generic). Compared with historical controls, ferric gluconate resulted in fewer allergic reactions than dextrans [12–14], and with regard to an assumed safer risk profile, these formulations replaced the use of dextrans [7].
However, in the smaller carbohydrate shell of IS (or ferric gluconate), iron is less tightly bound compared with low-molecular-weight iron dextran, and therefore only a smaller amount of iron could be administered in one infusion [15]. Hence, repeated administrations were necessary for correction of anemia [16–19].
The introduction of ferric carboxymaltose (FCM; maximum of 1000 mg iron per infusion; Ferinject®, Vifor Pharma, Switzerland; Injectafer®, American Regent, USA) made it possible to administer a significant amount of iron in only one infusion [20–24]. Trials revealed that with FCM, the anemia resolved earlier and that the drug was better tolerated than oral iron [21–23, 25–30]. In addition, the possibility of correcting iron deficiency anemia in only one to two infusions offered great advantages in terms of logistics and patient convenience.
In the same era, ferumoxytol (Feraheme®, AMAG Pharma, USA) was introduced, which is a semi-synthetic carbohydrate-coated superparamagnetic iron oxide nanoparticle [31] that was initially developed to serve as a contrast-enhancing agent for magnetic resonance imaging (MRI), but the fast infusion of this formulation in that setting resulted in a large number of hypersensitivity reactions [7]. However, the release of free labile iron with this formulation is less than with IS or ferric gluconate [31], and a slower infusion rate prevented hypersensitivity reactions [7]. Ferumoxytol is only registered in the US, and the maximum dose per infusion is 510 mg of iron.
The most recently introduced intravenous iron formulation for administering a large amount of iron (up to 20 mg/kg body weight) in one infusion is ferric derisomaltose (FDI [former name iron-isomaltoside]; Monofer®, Pharmacosmos, Denmark) [32–35], which has now been available for about a decade. It was the end product of an ambitious development program to create an efficacious parenteral iron formulation with a favorable safety profile that did not require a test dose. In addition, for the convenience of patients and physicians, it should have optimal dosing flexibility without limitations to correct the iron deficiency in one infusion [35].
Besides the use of these new intravenous iron formulations in iron deficiency anemia, FCM has regained more and more attention in the treatment of heart failure [36–39].
In contrast to the increasing use of intravenous iron formulations, clinically relevant adverse effects are less known, therefore the aim of this guideline was to increase awareness of these adverse effects and to propose a pragmatic protocol for safer use of these formulations.
Hypophosphatemia After Intravenous Iron
Clinical Relevance, Mechanism of Action, and Epidemiology
After the introduction of FCM, an unexpected adverse effect emerged—hypophosphatemia. This adverse effect was initially considered mild, transient, and clinically irrelevant [22, 25], but when this formulation was used more intensively in clinical practice, several case reports showed that hypophosphatemia could be severe, symptomatic, and could persist for months [40–48]. Moreover, patients had to be admitted to the hospital for correction of hypophosphatemia [40, 41, 45–47, 49]. Furthermore, the length of stay of those patients who were admitted for correction of iron deficiency anemia was prolonged by a mean of 7 days due to the occurrence and correction of hypophosphatemia [48].
The incidence of hypophosphatemia differed between the studied populations [50, 51]. The incidence was low (3–4%) in patients with renal insufficiency [20, 27] but increased to more than 70% in patients with menstrual blood losses or in women with iron deficiency and fatigue [25, 52].
From the initial studies by Wolf et al. [53, 54], it appeared that iron deficiency stimulates the production of fibroblast growth factor-23 (FGF-23), a hormone produced and secreted by osteocytes that is known to increase the renal excretion of phosphate. However, recent experiments in mice showed that bone marrow sinusoidal endothelial cells were a site for FGF-23 upregulation during iron deficiency anemia [55].
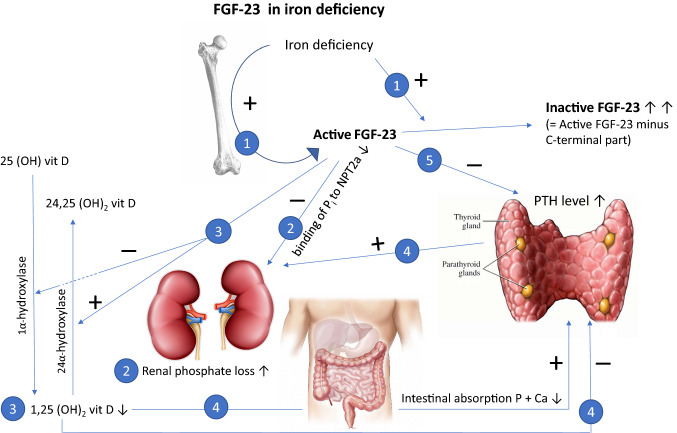
Parallel to the increased production of FGF-23, the degradation of FGF-23 is also increased, which implies that the active level of FGF-23 remains stable and that the phosphate level is not affected. The effects of FGF-23 during iron deficiency are presented in Fig. 1.
Fig. 1.
The physiological effects of FGF-23 during iron deficiency. During iron deficiency, the production of FGF-23 is increased. Recent experiments in mice showed that bone marrow sinusoidal endothelial cells were a site of FGF-23 upregulation [55]; however, at the same time, the increase in active FGF-23 is counterbalanced by the increase in the disintegration of intact (active) FGF-23 (1). This results in normal physiology of FGF-23 and increased concentrations of inactive FGF-23. FGF-23 results in diminished binding of Pi to NPT2A in the proximal tubule in the kidney, resulting in renal phosphate excretion (2). FGF-23 also interferes with vitamin D metabolism. It stimulates the inactivation of active 1.25 (OH)2 vitamin D and inhibits the activation of inactive 25 (OH)vitamin D (3). Less-active vitamin D results in a decrease in intestinal calcium and phosphate absorption. Lower calcium and phosphate concentrations stimulate the release of PTH, and active vitamin D inhibits the production of PTH. The increased production of PTH further stimulates phosphate excretion in the kidney (4). FGF-23 has also a direct blocking effect on the production of PTH by its co-receptor α-Klotho (5). FGF-23 fibroblast growth factor 23, Pi inorganic phosphate, NPT2A sodium-dependent phosphate cotransporter 2A, PTH parathyroid hormone, Vit D vitamin D
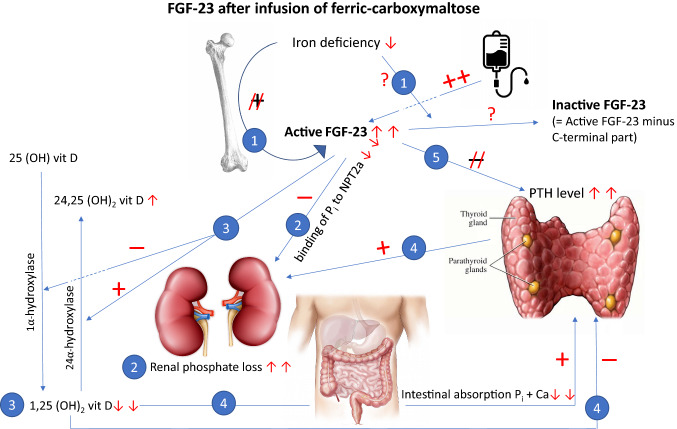
FGF-23 can be measured using different assays. One assay measures the intact and active form and another fits the C-terminal part, which is released from the active form to become inactive. Therefore, the latter assay measures both the active and inactive form of FGF-23. By combining both assays, the exact level of inactivated FGF-23 can be determined by comparing the results of the C-terminal assay with the results of the active assay [53]. In this way, it could be demonstrated that after the administration of FCM, the intact and active level of FGF-23 is markedly increased within 24 h [54, 56–58]. The mechanism behind this increase has not yet been elucidated, however it has been proposed that the carbohydrate shell of FCM might inhibit the cleavage of full-length intact FGF-23, which is upregulated in iron deficiency [53, 54, 56], but an alternative explanation may be the interference with gene expression. The high level of intact FGF-23 results in reduced expression of the sodium-dependent phosphate cotransporter 2A (NPT2A) in the proximal tubule in the kidney, enhancing renal phosphate excretion [59–63].
In addition, active FGF-23 inhibits the production of active vitamin D [1.25(OH)2D] and stimulates the inactivation of active vitamin D. Due to the reduced level of 1.25(OH)2D, the production of parathyroid hormone (PTH) is no longer impaired and the increased level of PTH contributes to the severity and duration of hypophosphatemia [42, 53, 54, 56, 57, 64–66]. The effects of FCM on FGF-23 are presented in Fig. 2.
Fig. 2.
The effects of FGF-23 after infusion of ferric carboxymaltose. Although the iron deficiency-driven stimulus for increased FGF-23 production and the simultaneous inactivation is diminished after iron repletion, the active FGF-23 level is remarkably increased following ferric carboxymaltose infusion. The exact mechanism behind this increase is currently unknown (1). This strongly results in diminished binding to NPT2A in the proximal tubule in the kidney and induces renal phosphate losses (2). In addition, vitamin D metabolism is disturbed by blocking the activation of 25 (OH) vitamin D and stimulating the inactivation of active 1.25 (OH)2 vitamin D (3). The markedly reduced active vitamin D concentrations result in lower intestinal calcium and phosphate absorption. By lower calcium and phosphate concentrations, the secretion of PTH is stimulated. In addition, active vitamin D no longer blocks the secretion of PTH. The substantial increase in PTH further stimulates renal phosphate losses (4). The ongoing stimulus of FGF-23 downregulates the blockade of FGF-23 on PTH secretion, which results in a further increase in PTH concentrations and renal phosphate losses (5). FGF-23 fibroblast growth factor 23, Pi inorganic phosphate, NPT2A sodium-dependent phosphate cotransporter 2A, PTH parathyroid hormone, Vit D vitamin D
In contrast, the risk of hypophosphatemia in the initial studies with FDI appeared relatively low and clinically non-significant [67, 68]. A retrospective analysis in Innsbruck (Austria) showed that the risk of hypophosphatemia indeed seemed lower with FDI than with FCM—4% versus 45%. Severe hypophosphatemia (inorganic phosphate [Pi] below 0.6 mmol/L [1.86 mg/dL]) was only observed in FCM-treated patients (33% of the treated patients) [69].
In recent years, prospective data have been published that compared both formulations. In a study in the US, one dose of 1000 mg FDI was compared with two doses of 750 mg FCM, with an interval of 1 week in two comparable published trials (Phosphare-IDA Study), which included 245 patients in total [56]. The FCM dose was the registered FCM dose in the US. It may be debated that two separate doses or a higher total dose will have influenced the incidence of hypophosphatemia. Nevertheless, hypophosphatemia (Pi < 2 mg/dL [0.65 mmol/L]) occurred in 8% of the FDI-treated patients versus almost 75% of the FCM-treated patients. The lowest level was observed around 14 days after the first infusion. The phosphate concentration decreased remarkably more in the FCM group: mean 1.5 mg/dL (0.48 mmol/L) versus 0.3 mg/dL (0.1 mmol/L) in the FDI group. Severe hypophosphatemia (Pi < 1 mg/dL [0.32 mmol/L]) was exclusively observed in the FCM group (11% of patients). Five weeks after the infusion, hypophosphatemia was still present in 4% of the FCM-treated patients versus 1% of the FDI-treated patients [56].
Another randomized trial in the US that included almost 2000 patients compared two doses of ferumoxytol 510 mg with two doses of FCM 750 mg, both administered on days 1 and 8 [58]. The incidence of hypophosphatemia (Pi < 2 mg/dL [0.65 mmol/L]) with ferumoxytol was 0.9% versus 50.8% with FCM. Severe hypophosphatemia (Pi < 1.3 mg/dL [0.42 mmol/L]) occurred in 0% of patients taking ferumoxytol versus 10% taking FCM. After 5 weeks, at the end of the study period, hypophosphatemia persisted in none of the ferumoxytol-treated patients versus 29% of the FCM-treated patients [58].
In Europe, two prospective studies have been published. The small HOMe aFERs Study compared 26 women with iron deficiency anemia who received one dose of either FCM or FDI 20 mg/kg to a maximum of 1000 mg. Hypophosphatemia (Pi < 2 mg/dL [0.65 mmol/L]) was observed in 75% of the women treated with FCM versus 8% of the women treated with FDI [65]. In 106 evaluable patients with inflammatory bowel disease, a standard dose of 1000 mg, as is common in daily practice, of both drugs was compared. Moderate to severe hypophosphatemia (Pi < 0.65 mmol/L [2 mg/dL]) was observed in 57% of the FCM-treated patients versus 6% of the FDI-treated patients [70]. Comparable results were retrieved from a preliminary analysis of the Phosphare-IBD trial, in which both groups also received 1000 mg of either FCM or FDI. In almost 50 patients in each group, hypophosphatemia occurred in 51% of patients in the FCM group versus 8% in the FDI group [71]. In a recent meta-analysis, hypophosphatemia occurred in 47% of the FCM-treated patients versus 4% of the FDI-treated patients [72].
Prospectively, one single dose of 1000 mg FDI was also compared in over 1500 patients with five consecutive doses of 200 mg IS (Ferwon-IDA trial). Hypophosphatemia was observed in 4% of patients in the FDI group versus 1.5% in the IS group [16]. A smaller comparable trial studying just over 450 patients revealed an incidence of hypophosphatemia of 1.5% with FDI versus 0% with IS [73].
Noteworthy, low-molecular-weight iron dextran is also registered for the correction of total iron deficit in a single infusion (up to 20 mg iron/kg body weight). Nevertheless, in daily practice, at least in Europe, low-molecular-weight iron dextran is less frequently used than FCM or FDI, possibly due to previous reports claiming a substantially higher risk of severe infusion reactions, although these results may be biased due to the combined analysis of high- and low-molecular-weight dextran-based iron formulations [7]. In the initial paper of Wolf et al., low-molecular-weight dextran was compared with FCM [54]. In contrast to FCM, low-molecular-weight dextran did not increase intact FGF-23, and hypophosphatemia did not occur [54]. Another study confirmed the absence of developing hypophosphatemia with low-molecular-weight iron dextran [74].
Risk of Hypophosphatemia
As outlined above, it clearly appears that the risk of hypophosphatemia differs between the different formulations. The risk with FCM is remarkably higher than with FDI, which in turn has a small higher risk than IS or ferumoxytol. A recently published subanalysis of the Phosphare-IDA trial revealed FCM as the strongest risk factor for the development of hypophosphatemia [75], with an odds ratio of 38 versus FDI. The incidences of hypophosphatemia with the different iron formulations are presented in Table 1.
Table 1.
Incidences of hypophosphatemia
| Intravenous iron formulation | Incidence of hypophosphatemia (%) | References |
|---|---|---|
| Ferric carboxymaltose | 47–57 | [70, 72] |
| Ferric derisomaltose | 4–8 | [16, 72] |
| Iron sucrose | 1.5 | [16] |
| Ferumoxytol | 0.9 | [58] |
| Low-molecular-weight iron dextran | 0 | [54, 74] |
The reported incidences of ferric carboxymaltose and ferric derisomaltose are the highest reported in the main prospective trials, taking into account the fact that one dose of the formulation has been administered. The incidence with iron sucrose implies five consecutive administrations and two for ferumoxytol. The total dose of all formulations consists of about 1000 mg of elementary iron. In a meta-analysis, the incidence of hypophosphatemia with either ferric carboxymaltose or ferric derisomaltose was somewhat lower and these incidence rates are also presented [72].
Repeated doses may increase the risk. The American trial with two administrations of FCM [56] revealed a higher incidence than one single dose in the European trial [70]. Repeated doses also increased the duration of hypophosphatemia [76]. In the Phosphare-IBD trial, a second dose was administered after 35 days. The phosphate level after 70 days was lower than the phosphate level after 35 days [71]. Frazier et al. and Wolf et al. showed that intact FGF-23 increased further after administration of a second dose of FCM, and that the Pi-concentration decreased further accordingly [56, 57]. The administered dose also correlates with the nadir of hypophosphatemia—the higher the dose, the lower the nadir [72, 76]. A pooled analysis from 45 trials confirmed that repeated infusions result in deeper and longer-existing hypophosphatemia, and that a higher dose is also associated with an increased risk of developing hypophosphatemia [77].
Moreover, patients who had a relatively low serum phosphate concentration prior to the administration of intravenous iron also had a higher risk of achieving moderate to severe hypophosphatemia [40, 43, 48, 75].
Several other risk factors have been recognized in a variety of case reports and from post hoc analysis of trials. A low level of vitamin D may impair the resorption of phosphate in the gut [40, 46, 47]. In addition, subgroups with a low baseline serum vitamin D concentration had an increase in FGF-23 concentrations [78]. Hyperparathyroidism [40, 46, 75] also increases renal phosphate excretion. Bariatric surgery [40, 79], especially a Roux-Y gastric bypass, may also impair gastrointestinal phosphate resorption or lead to vitamin D deficiency. Patients with gastrointestinal malabsorption or malnutrition, or who have a relatively low body weight [45, 48, 77], may suffer from a phosphate-deficient state. In addition, when intravenous iron is administered with a fixed dose, patients with a low body weight receive a relatively higher dose. Renal transplant recipients [40, 41, 80] often have persistent hyperparathyroidism.
Drugs to treat osteoporosis, such as bisphosphonates or denosumab [81], impair the resolution of phosphate from the bone. Furthermore, denosumab may result in hypocalcemia, which in turn results in secondary hyperparathyroidism [82], increasing renal phosphate losses [81]. In the initial paper about denosumab, hypocalcemia did not occur [83] but data from clinical practice showed incidences of between 4 and 14% [84–87]. Risk factors for developing hypocalcemia were a lower baseline serum calcium concentration [84–86], renal insufficiency [84–87], the use of loop diuretics [86], and a prior high bone turnover state [88].
The risk also increases with increasing age [43, 77], however it may also occur in children [89–92]. The high incidence of vitamin D deficiency in the elderly [93–95], as well as protein-energy malnutrition, which is also a problem in the elderly [96, 97], may lead to a phosphate-deficient state and explain the risk with increasing age. One post hoc analysis also showed an increased risk in Black people [77]. This may perhaps also be influenced by vitamin D, since Black people may have lower vitamin D concentrations when they live at a higher latitude [98].
The lower the ferritin level, as a representation of the severity of the iron deficiency, the higher the risk of developing hypophosphatemia [43, 72, 75, 77]. This may be explained by the fact that iron deficiency upregulates FGF-23 [53, 54, 56]. The increase in active FGF-23, which occurs after the administration of intravenous iron, especially FCM [54, 56–58], may then be more pronounced. This is in concordance with the fact that in patients with autosomal-dominant hypophosphatemic rickets (ADHR), who have a congenital genetic defect that impairs the degradation of intact FGF-23, iron deficiency results in an increase in renal phosphate losses [99, 100]. The predisposing risk factors are summarized in Table 2.
Table 2.
Factors that predispose to, or protect against, the development of hypophosphatemia
| Predisposing factors for the development of hypophosphatemia |
| Dose and number of doses of intravenous iron |
| Severity of iron deficiency, expressed by lower ferritin |
| Pre-existing low serum phosphate concentration |
| Vitamin D deficiency |
| Hyperparathyroidism |
| Bariatric surgery: Roux-Y gastric bypass |
| Malabsorption |
| Malnourishment or relatively low body weight |
| Increasing age |
| Renal transplant |
| Drugs for osteoporosis: denosumab and bisphosphonates |
| Black race |
| Factors for protection against the development of hypophosphatemia |
| Increasing renal insufficiency |
On the other hand, renal insufficiency relatively protects against the development of hypophosphatemia [20, 27, 64, 72, 77] because patients with renal insufficiency deal with disturbed renal phosphate clearance and have a pre-existing increased level of FGF-23. However, FGF-23 also increases further in patients with renal insufficiency [64], and even in patients receiving hemodialysis [101]. Which level of renal insufficiency definitely protects against the risk of hypophosphatemia is currently unknown. Although the risk of hypophosphatemia is reduced in conditions with impaired phosphate excretion (i.e. mainly renal insufficiency), the other biological actions of high FGF-23 levels may be harmful. For instance, FGF-23 has been associated with the development of left ventricular hypertrophy [102] and worse cardiac outcome [103, 104]. In addition, also in renal insufficiency, FGF-23 is associated with worse cardiac outcome [105–108] and mortality [109] and is associated with the progression of renal failure [109, 110]. Furthermore, in hemodialysis, FGF-23 is associated with left ventricular diastolic dysfunction [111], incidence of cardiovascular events [112–115], and mortality [112, 116]. There are indications that not only intact FGF-23 but also the separated C-terminal part is associated with an increased risk of mortality [117].
Osteomalacia
To date, several cases have been published that showed that repeated use of FCM leads to a severe form of osteomalacia, characterized by bone pain, Looser zones (pseudofractures) and low-trauma fractures [66, 118–125]. Similar results have been reported for another intravenous iron formulation, iron-polymaltose (Maltofer®, Vifor Pharma, Switzerland), the use of which is less common [126, 127]. In addition, in Japan, osteomalacia is reported from the use of maltose-enriched ferric oxide, a formulation comparable with IS [128–130]. To date, no cases of osteomalacia have been published with repeated use of FDI. A small study was performed administering FDI every 3 months for up to 1 year to prevent relapse of iron-deficiency anemia in patients with inflammatory bowel disease. The authors reported that hypophosphatemia was not observed [131]; however, since osteomalacia has been reported with a comparable formulation to IS and hypophosphatemia may also occur with FDI, it seems likely that repeated use of FDI may also lead to osteomalacia. One case of osteomalacia induced by FCM has been published, in which FCM was changed to FDI. Unfortunately, no improvement in bone mineral status was observed and even new fractures occurred [66].
A systematic review of reported cases has recently been published [132] in which the authors evaluated 28 case reports, considering 30 cases, of which 18 reported on FCM, 8 reported on saccharated iron oxide, and three reported on iron-polymaltose. In one report, the iron formulation was not mentioned. All but two cases received at least five infusions (median 17, range 2–198). Osteomalacia was characterized by bone pain in almost all cases (Looser zones [pseudofractures] and fractures). Looser zones are the radiological hallmark of osteomalacia. When performed, all cases had an abnormal nuclear bone scan. Alkaline phosphatase was usually, but not always, elevated. The lower limbs, followed by the chest, pelvis, and back, were most frequently affected but osteomalacia may occur in the whole body. Inflammatory bowel disease was the most common underlying disease. Contributing factors in those cases could be malabsorption of calcium and phosphate, vitamin D deficiency, and the use of corticosteroids [132].
The etiology of osteomalacia can be understood from the fact that activation of vitamin D is blocked by FGF-23, and active 1.25(OH)2D gets more rapidly inactivated by FGF-23 [63, 133]. Indirectly, PTH will increase as a result of the loss of active 1.25(OH)2D. Furthermore, FGF-23 may have a direct effect on the bone, where it acts as a mineralization inhibitor by controlling calcium and phosphate metabolism in the bone [59]. Hence, FGF-23 creates severe mineralization disorder of the bone.
A safe time interval between repeated doses of FCM is currently unknown. Biochemically, bone markers have been reported to be normalized approximately 6 months after the administration of FCM [124], suggesting that administration of a second dose of intravenous iron after 6 months seems reasonable. However, FCM-induced hypophosphatemia has been reported to persist up to 48 weeks after the infusion [77], although it is not clear from that study whether this small subset of patients with prolonged hypophosphatemia received either one or more infusions [77].
Hypersensitivity Reactions
Another important factor in deciding which iron formulation will be prescribed is the risk of hypersensitivity reactions. Hypersensitivity may include a broad range of symptoms such as cardiovascular (hypotension, tachycardia), respiratory (dyspnea, bronchospasm), gastrointestinal (abdominal pain, nausea and vomiting), and skin (erythema, urticaria and flushing). Since hypersensitivity reactions are not uncommon, a warning statement has been published in the Summary of Product Characteristics (SmPC) of all intravenous iron formulations.
The etiology of these hypersensitivity reactions is still not fully clarified but cumulative evidence points to the direction of non-allergic, complement-mediated activation by nanoparticles of iron (free or labile iron, which does not bind quickly enough to transferrin)—Complement Activation-Related Pseudo-Allergy (CARPA) [134–136]. Activation of the complement triggers other inflammatory cells, including mast cells and basophils, which produce histamine, among other proinflammatory products [137, 138]. Hence, the clinical picture of CARPA resembles the true immunoglobulin (Ig) E-mediated allergy [137]. CARPA has already been recognized with the use of some monoclonal antibodies, liposomal medication, and chemotherapy [134]. In rare cases, the classical IgE-mediated form of hypersensitivity or anaphylaxis also occurs [134].
A frequently occurring, relatively innocent and relatively quick resolving hypersensitivity reaction, characterized by flushing, pain, or pressure in the chest and/or back, arthralgia and/or myalgia, is known as a Fishbane reaction [137, 139]. The precise pathophysiologic mechanism of a Fishbane reaction has not been resolved but it may be provoked by the release of free labile iron itself and not by complement activation [139].
Hypersensitivity reactions due to CARPA have two important consequences for daily practice. At first, prior sensitization is not required and therefore may occur at the first administration. Second, the complement-mediated reaction is dependent on the infusion rate. Repeated administration of the same drug at a lower infusion rate is usually possible without provoking hypersensitivity reactions [140].
Based on high-quality prospective evidence and meta-analyses, all the formulations appear equal with respect to serious adverse events (SAEs), with incidence rates of approximately 0.2–1.7% [9, 141].
Previous concerns regarding higher SAEs with the use of iron dextran have been questioned and are probably biased by the high-molecular-weight iron dextran formulations, which are no longer available [7]. True anaphylaxis is rare and occurs in approximately 1:250,000 administrations [9, 142].
However, adverse events are usually a secondary outcome parameter and the trials were not powered on infrequent adverse events. Mild to moderate hypersensitivity reactions or other mild adverse events (excluding hypophosphatemia) occur more frequently but the incidence rates vary widely, depending on terminology and the type of intravenous iron formulation [135]. A universal approach with a standardized method grading hypersensitivity reactions in adequately powered prospective studies could provide a more definite answer as to whether the different intravenous iron formulations truly differ in the incidence of adverse events.
In the prospective trials, mild to moderate hypersensitivity reactions were reported in up to 11% of FCM cases, 22% of FDI cases, and 17% of IS cases [56, 73]. In the US trial, severe hypersensitivity reactions were reported in one patient in the FDI group (0.8%) versus two patients in the FCM group (1.7%) [56]. In another trial, skin lesions, which may be classified as hypersensitivity reactions, occurred in 7.5% of cases in the FDI group versus 3.0% of cases in the IS group. Severe hypersensitivity reactions were reported in 0.6% of cases in both groups in that study [73]. A third trial reported severe hypersensitivity reactions of 0.3% in the FDI group versus 0.4% in the IS group [16]. Taken together, from these trials, adverse events, except hypophosphatemia, seem to occur somewhat more often with FDI and IS, but the risk of severe hypersensitivity reactions seems comparable. This risk seems to be approximately, or even below, 1%.
Practical Guidelines
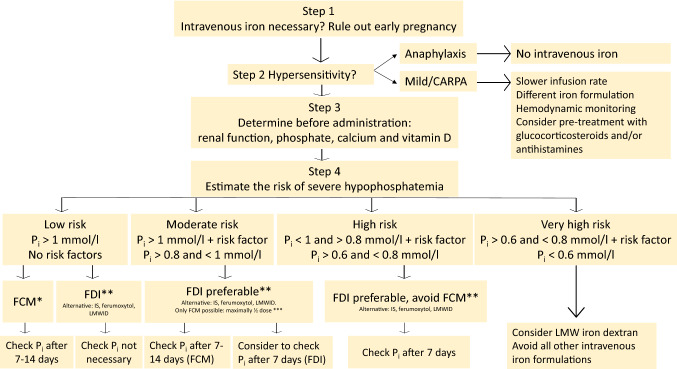
In the interests of patient safety, it is important to obtain tools to support the clinician in making a proper risk–benefit decision. The first step is to consider whether your patient may have an increased risk of developing hypophosphatemia (Table 2). It is also important to check whether previous use of intravenous iron formulations has led to hypersensitivity reactions and which formulation was used in that situation.
Since the mean decrease of phosphate by FCM is about 0.4–0.5 mmol/L (1.24–1.55 mg/dL) [56, 72], a baseline phosphate concentration above 1.0 mmol/L (3.1 mg/dL) is considered relatively safe to prevent severe hypophosphatemia, but the occurrence of severe hypophosphatemia cannot be totally excluded. The best way to prevent hypophosphatemia is the choice of iron formulation (Table 1). A flowchart regarding the safe use of these formulations is presented in Fig. 3.
Fig. 3.
Flowchart for safe use of intravenous iron preparations. The risk of developing hypophosphatemia can be determined by applying the predisposing risk factors from Table 2. When FCM is used, the SmPC advices to measure the serum phosphate concentration before administration and to repeat this after 14 days. However, when only one dose of FCM is administered, the nadir usually occurs after 7 days. A predose serum phosphate concentration of 1 mmol/L is used as a relatively safe border to prevent the development of severe hypophosphatemia, since prospective trials revealed a mean decrease in serum phosphate of 0.4–0.5 mmol/L with the use of FCM. For mg/dL, Pi must be multiplied by 3.1. *Even in low-risk patients, FCM represents a risk of severe hypophosphatemia. The best way to prevent hypophosphatemia is the choice of iron formulation. Local availability, costs, and the risk of other adverse effects will further contribute to the physician’s final decision to choose either FCM or FDI. When iron deficiency anemia cannot be restored by a maximum dose of iron 1000 mg and multiple infusions are likely, FCM should definitely not be used because repeated infusions increase the risk and duration of hypophosphatemia, implying a risk of inducing osteomalacia. An interval of 6 months between dosing may be safe to prevent osteomalacia. **Ferumoxytol and IS have a lower risk of hypophosphatemia than FDI and can also be used, but less iron can be administered in one infusion. Ferumoxytol is only registered in the US. LMWID has not been associated with the development of hypophosphatemia and can therefore also be used. Total correction of the iron deficit is possible using LMWID, but requires a longer infusion rate (4–6 h) and a test dose of 25 mg. ***The use of FCM in this situation is not recommended. In a situation whereby FCM is the only treatment option, use half the maximal dose (500 mg), realizing that iron deficiency cannot be fully restored, and repeated doses are contraindicated. CARPA Complement Activation-Related Pseudo-Allergy, FCM ferric carboxymaltose, SmPC Summary of Product Characteristics, FDI ferric derisomaltose, IS iron sucrose, LMWID low-molecular-weight iron dextran, Pi inorganic phosphate
The treatment schedule of intravenous iron is based on the calculated iron deficiency and the body weight of the patient using Ganzoni’s formula: total iron dose = [actual (lean or ideal) body weight × (15 (or target hemoglobin (Hb) – actual Hb in g/dL)] × 2.4 + iron stores [143]. For mmol/L, the formula has to be changed to: [actual body weight × ((9.3 (or target Hb) – actual Hb) × 1.61)] × 2.4 + iron stores. Two-thirds of body iron is incorporated into Hb and one-third in storage sites [144]. Calculation of the iron stores is an assumption. Various approaches have been used to estimate the iron stores, varying from body weight-dependent calculations (10–15 mg/kg) to a fixed dose of 500–1000 mg (Pharmacoeconomic review report: iron isomaltoside 1000 [Monoferric]; Canadian Agency for Drugs and Technologies in Health]. When a modification of the Ganzoni’s formula with a fixed iron store replacement dose of 500 mg iron was applied to participants from five clinical trials, a mean iron deficit of 1531 mg was calculated [145]; however, when it was applied to two larger randomized trials, the mean iron deficit was calculated to be 1392 mg [145]. Thus, the required dose to replace the iron deficit is usually > 1000 mg. However, in clinical practice, the formula may be considered impractical, and current dosing guidelines in the SmPC for FCM do not refer to this formula. The simplified dosing regimen for FCM resulted in better clinical efficacy and compliance than dosing according to Ganzoni’s formula for IS [146].
The SmPC of FCM advises a maximum dose of iron 1000 mg at a time, in 15 min infusions. When necessary, a second dose may be administered after 1 week. The FDI SmPc refers to a maximum single infusion dose of up to 20 mg/kg body weight. The infusion rate is at least 15 min for doses to 1000 mg and 30 min for doses above 1000 mg. FDI should not be diluted to an iron concentration below 1 mg/mL, or more than 500 ml total volume. Low-molecular-weight iron dextran requires a test dose of 25 mg of iron. Similar to FDI, the maximum single infusion dose consists of up to 20 mg/kg body weight of iron, but it has to be infused more slowly over 4–6 h. The SmPCs can be found at http://www.medicines.org.uk, with the exception of ferumoxytol, which is only licensed in the US.
If acute symptoms develop after an intravenous iron infusion, the infusion should be stopped. Clinical judgment is required to differentiate between true allergy/anaphylaxis (rare) and CARPA (relatively common). If CARPA is considered as the most likely explanation and the symptoms abate, a rechallenge with a slower rate of infusion is usually possible, since CARPA is dependent on the rate of infusion [137–140]. In patients with a history of an infusion reaction, pretreatment with glucocorticosteroids and second- or third-generation antihistamines has been mentioned, in addition to a reduced infusion rate [138, 139]. Alternatively, a different preparation may be considered. To prevent CARPA at the first infusion, it is proposed to use a much slower rate of infusion than is reported in the SmPC, preferably 1–2 h instead of 15–30 min. In the case of severe hypersensitivity reactions or anaphylaxis, the use of the same drug or another intravenous iron formulation is contraindicated [139].
When the risk of hypophosphatemia is increased, choose the drug with the lowest risk of this adverse effect. As learned from the published trials, FDI has a remarkably lower risk than FCM. When using ferumoxytol or IS, the risk is even lower but less iron can be administered in one infusion. The SmPC of FCM has recently changed. Besides a warning for the risk of hypersensitivity reactions, which is true for all intravenous iron formulations, the SmPC of FCM now also points to the risk of hypophosphatemia. In addition, it is strongly advised to measure the serum phosphate concentration before administration and to repeat this after 2 weeks, when the nadir has usually been reached. In the US trial, in which two doses of FCM were used with a 1-week interval, the nadir was indeed reached after 2 weeks [56]; however, when only one dose was used, the nadir occurred earlier and commonly, after 7 days [65, 77]. Furthermore, after one dose of FDI, the nadir was reached after 7 days [56]. Dependent on the preparation used and the considered risk, it is advisable to check the phosphate concentration after 1–2 weeks (Fig. 3). In addition, it is advisable to control the vitamin D status before administration, as well to have a better understanding of the risk of hypophosphatemia. When the risk of hypophosphatemia is moderate, high, or very high, the use of FCM is strongly discouraged (Fig. 3). Considering the limited risk of hypophosphatemia and the higher patient convenience (single infusion vs. multiple infusions, no requirement for a test dose, and the infusion rate), we prefer FDI over low-molecular-weight iron dextran, IS, or ferumoxytol in moderate- and high-risk patients. When the risk of hypophosphatemia is only moderately increased and no other intravenous iron formulation other than FCM is possible, for instance due to adverse effects of alternative formulations, it is advisable to use half the maximal dose (500 mg) of FCM, realizing that this dose is usually insufficient to correct the iron deficit, and repeated doses must be avoided because they increase the risk [147]. When the risk is very high and no oral iron option is available, the use of low-molecular-weight iron dextran is an option because this formulation has no risk of hypophosphatemia [54, 74]. The assumed higher risk of hypersensitivity reactions with dextrans might be biased by the combined analysis with high-molecular-weight iron dextrans [7]. However, one prospective trial did reveal a significantly higher incidence of hypersensitivity reactions with low-molecular-weight iron dextran compared with FCM [74].
Both FCM [148, 149] and FDI [150] have been used in pregnancy with an acceptable safety profile. However, their use is limited to the second and third trimesters, while data on their safe use in the first trimester are lacking. Therefore, to be safe, the use of FCM and FDI in early pregnancy is not recommended.
FCM has been studied in children mostly retrospectively [90–92, 151–153], but also prospectively [154]. FCM appeared effective in correction of anemia, with an acceptable risk profile comparable with adults. Three retrospective studies reported hypophosphatemia, with incidence rates ranging from 14 to 20% [90–92]. To date, no studies of FDI in children have been performed and the SmPC of FDI advises it should not be used in subjects under the age of 18 years because of lack of safety data. Very recently, a prospective trial of FDI in children has been initiated [ClinicalTrials.gov: NCT05179226].
Repeated use of FCM is also not recommended because of the risk of severe bone disturbances. A safe interval for repeated administration is currently unknown, but based on recovery of bone markers, we suggest an interval of at least 6 months [124]. However, in a small subset of patients, hypophosphatemia has been reported to last for up to 48 weeks [77]. Prolonged hypophosphatemia implies an ongoing increased concentration of FGF-23 and ongoing mineralization disorder of the bone, which ideally should be restored before administrating a new dose.
In the case of chronic iron supplementation, consider an oral option whenever possible. When this option is not successful, ferric citrate (Auryxia®, Akebia Therapeutics, USA) may be another option. This iron preparation was introduced as a phosphate binder in patients with renal failure [155], but it appeared to increase the iron stores and to diminish the need for intravenous iron and the use of erythropoietin analogs in patients receiving hemodialysis [156, 157]. Other oral iron formulations usually have little effect on iron stores in dialysis patients [158]. In patients with chronic renal failure, ferric citrate revealed a larger rise of iron parameters than iron sulphate [159]. One ferric citrate tablet contains 210 mg of elementary iron, which is much more than the usual formulations. The precise way in which ferric citrate increases gastrointestinal iron resorption is currently unknown. The higher amount of elementary iron in the tablets does not seem to be the whole explanation [158]. A very recent study in mice showed that ferric citrate absorption is dependent on conventional enterocyte iron transport by ferroportin and that significant paracellular iron absorption does not occur [160]. The common adverse effects of this drug are gastrointestinal disturbances and dark-colored stools in concordance with other oral iron supplements. Unfortunately, this drug is not available in all countries but it may be administered on a compassionate use basis.
Treatment of Hypophosphatemia
In the case of severe hypophosphatemia (Pi <0.35 mmol/L) or sometimes moderate hypophosphatemia (Pi > 0.35 and < 0.65 mmol/L), hospital admission may be necessary to administer phosphate, either intravenously or orally; however, in the case of severe hypophosphatemia, the intravenous route may be preferable [161]. Continuous or repeated supplementation of phosphate might be needed as long as FGF-23 and PTH are high, and may last for up to more than 3 months [48, 72, 162]. Therefore, repeated checks are required. Oral solutions or tablets are safer but the resorption may be unpredictable [161]. Even more so, oral phosphate formulations may result in gastrointestinal disturbances, especially diarrhea [40, 47, 161, 163]. The administration of phosphate formulations, either orally or intravenously, has a risk of more severe adverse effects, and may result in hypocalcemia [161, 163], arrhythmias [161], ectopic calcifications [161, 163], and acute phosphate nephropathy [161, 164]. Therefore, prevention of hypophosphatemia is preferable to treatment and phosphate formulations should be restricted to clinically urgent situations only. In addition, the administration of phosphate formulations stimulates the release of PTH, which in turn may increase renal phosphate losses [165]. Dietary phosphate supplementation increased serum FGF-23 concentrations in healthy men [166, 167]. Whether this also happens in intravenous iron-induced hypophosphatemia is currently unknown, but oral phosphate formulations increased FGF-23 further in patients with X-linked hypophosphatemia (XLH) who suffer from a loss-of-function mutation in the PHEX gene and have increased circulating levels of FGF-23 [165, 168].
Food components may be changed. Protein from dairy products, for instance, is relatively rich in phosphate [161, 163], and Pi compounds are often used for food conservation. An example of this phenomenon is cola. Mild hypophosphatemia may be treated with a phosphate-enriched diet [40, 161].
In addition, activation of vitamin D is disturbed and inactivation of active vitamin D is increased [63, 133]. Hence, it is important to administer active vitamin D compounds (alfacalcidol or calcitriol) to stimulate gastrointestinal phosphate resorption and to control the additional hyperparathyroidism [47, 124]. However, the additionally increased calcium resorption may increase the risk of acute phosphate nephropathy, primarily when the administration of phosphate formulations and active vitamin D compounds are combined [161].
In severe cases, burosumab (Crysvita®, Kyowa Kirin, Japan) may be an option. Burosumab is a monoclonal antibody against FGF-23 and has proven to be effective in patients with XLH [169, 170]. Burosumab also appeared to improve bone status in patients with tumor-induced osteomalacia [171, 172]. In patients with this disease, a mesenchymal tumor produces FGF-23. Recently, burosumab (off-label) has been used successfully in FCM-induced osteomalacia [66].
An alternative additional option may be dipyridamole, which increased the renal phosphate resorption in patients with increased renal phosphate losses [173]. Concordant hyperparathyroidism can be treated with cinacalcet, which lowers the renal phosphate losses by this phenomenon [165, 174]. Be aware that cinacalcet may result in hypocalcemia [165]. Calcitonin may be another additional option; this compound appeared to impair the release of FGF-23 in the osteocyte in patients with XLH [175]. The treatment options are summarized in Table 3.
Table 3.
Treatment options when hypophosphatemia has occurred
| Mild hypophosphatemia: Pi > 0.65 and < 0.80 mmol/L |
| Adapt nutrition: phosphate-enriched diet: dairy products; cola |
| Consider active vitamin D compounds |
| Moderate hypophosphatemia: Pi > 0.35 and < 0.65 mmol/L |
| Adapt nutrition: phosphate-enriched diet: dairy products; cola |
| Active vitamin D compounds |
| Oral phosphate solutions/tablets |
| When symptomatic: intravenous phosphate solutions |
| In the case of accompanying hyperparathyroidism: consider cinacalcet |
| Probable additional alternative options: dipyridamole and calcitonin |
| Severe hypophosphatemia: Pi < 0.35 mmol/L |
| Adapt nutrition: phosphate-enriched diet: dairy products; cola |
| Active vitamin D compounds |
| Intravenous phosphate solutions |
| In the case of accompanying hyperparathyroidism: cinacalcet |
| Insufficient response: burosumab |
| Probable additional alternative options: dipyridamole and calcitonin |
| Osteomalacia |
| Burosumab |
| Active vitamin D compounds |
| Oral phosphate solutions/tablets or intravenous phosphate solutions |
| Adapt nutrition: phosphate-enriched diet: dairy products; cola |
| Accompanying hyperparathyroidism: cinacalcet |
Be aware that the etiologic factor for hypophosphatemia may persist for a remarkable period of time, even more than 3 months. Prevention is therefore preferable to cure.
Pi inorganic phosphate
For mg/dL, Pi must be multiplied by 3.1
Conclusion
The intravenous iron formulations FCM and FDI, which have now been available for more than 10 years, offer the possibility of administering a large amount of iron in one infusion, resulting in faster resolution of anemia. Moreover, FCM and FDI are better tolerated than the oral iron formulations. The triad of logistic advantages, improved patient convenience, and fast correction of anemia explains the fact that intravenous iron formulations nowadays are frequently prescribed worldwide in the treatment of iron deficiency anemia.
An important adverse effect of these formulations is the upregulation of intact active FGF-23, which results in renal phosphate losses and hypophosphatemia. Hypophosphatemia is most frequently and most severely provoked by FCM, but the other formulations, except low-molecular-weight iron dextran, may also result in this adverse effect. For FCM, it is advised nowadays, since the SmPC has been adapted, to check the serum phosphate concentration before and 1–2 weeks after the infusion. Several predisposing risk factors have been recognized, as shown in Table 2. Patients with renal impairment are relatively protected but the upregulation of FGF-23 in these patients may also be harmful. Repeated use may result in severe osteomalacia with bone pain, Looser zones (pseudofractures), and low-trauma fractures. Therefore, repeated use must be prevented as much as possible. When hypophosphatemia has been developed, it may persist for a long time (more than 3 months) and the treatment of hypophosphatemia is quite challenging. Burosumab, a monoclonal antibody against FGF-23, seems a robust compound for the treatment of induced osteomalacia.
Other important adverse effects are hypersensitivity reactions; however, most hypersensitivity reactions are provoked by non-allergic CARPA, induced by the release of free labile iron, and these reactions can be limited by choosing a slow infusion rate. Severe hypersensitivity reactions seem to occur in fewer than 1% of treated patients. Furthermore, the published prospective trials do not reveal remarkable differences between FCM and FDI.
Declarations
Funding
This was a physician-driven report and no funding was received.
Ethics declarations
This manuscript follows all ethical considerations as proposed by the World Health Organization.
Conflicts of interest
Johannes M.M. Boots received lecture fees and participated in advisory boards from Cablon Medical, The Netherlands; Pharmacosmos, Denmark; and Vifor Pharma, The Netherlands. Rogier A.M. Quax has no disclosures with regard to this manuscript.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
The literature was partly taken from a previous publication. We conducted a search of Pubmed for additional literature on specific items to prove our message. In addition, the literature was recognized from references from trials and reviews. We tried to check opinions in reviews as much as possible by analyzing original reports. It was not intended to review all possible literature, since many reports reached the same conclusions and therefore not all reports are incorporated in this manuscript.
Code availability
Not applicable.
Authors’ contributions
This report is driven by the recognition that physicians in clinical practice do not always make a proper risk–benefit analysis when prescribing intravenous iron formulations. Many physicians from diverse specialties, such as internal medicine, gastroenterology, geriatrics, rheumatology, cardiology, gynecology, and even pediatrics, are unaware of the possible adverse effects and may harm their patients. It is intended to develop a practical guideline, based on a thorough evaluation of the literature, which can be implemented in daily practice or electronic prescription modules to prevent further harm in the future. Both authors contributed to the literature search, writing of the manuscript, and designing the figures, and read and approved the final version.
References
- 1.Heath CW, Strauss MB, Castle WB. Quantitative aspects of iron deficiency in hypochromic anemia. (The parenteral administration of iron) J Clin Invest. 1932;11:1293–1312. doi: 10.1172/JCI100478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goetsch AT, Moore CV, Minnich V. Observations on the effect of massive doses of iron given intravenously to patients with hypochromic anemia. Blood. 1946;1:129–142. doi: 10.1182/blood.V1.2.129.129. [DOI] [PubMed] [Google Scholar]
- 3.Nissim JA. Intravenous administration of iron. Lancet. 1947;2(6463):49–51. doi: 10.1016/s0140-6736(47)90053-6. [DOI] [PubMed] [Google Scholar]
- 4.Nissim JA, Robson JM. Preparation and standardisation of saccharated iron oxide for intravenous administration. Lancet. 1949;1(6556):686–689. doi: 10.1016/S0140-6736(49)91958-3. [DOI] [PubMed] [Google Scholar]
- 5.Müller A. Classification and properties of iron preparations. Arzneimittelforschung (Drug Res). 1974;24:880–883. [PubMed] [Google Scholar]
- 6.Theil EC, Sayers DE, Brown MA. Similarity of the structure of ferritin and iron.dextran (Imferon) determined by extended X-ray absorption fine structure analysis. J Biol Chem. 1979;254:8132–8134. doi: 10.1016/S0021-9258(19)86864-3. [DOI] [PubMed] [Google Scholar]
- 7.Auerbach M, MacDougall I. The available intravenous iron formulations: History, efficacy, and toxicology. Hemodial Int. 2017;21(Suppl 1):S83–92. doi: 10.1111/hdi.12560. [DOI] [PubMed] [Google Scholar]
- 8.Hamstra RD, Block MH, Schocket AL. Intravenous iron dextran in clinical medicine. J Am Med Assoc. 1980;243:1726–1731. doi: 10.1001/jama.1980.03300430028018. [DOI] [PubMed] [Google Scholar]
- 9.Avni T, Bieber A, Grossman A, Green H, Leibovici L, Gafter-Gvili A. The safety of intravenous iron preparations: systematic review and meta-analysis. Mayo Clin Proc. 2015;90:12–23. doi: 10.1016/j.mayocp.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Chertow GM, Mason PD, Vaage-Nilsen O, Ahlmén J. On the relative safety of parenteral iron formulations. Nephrol Dial Transplant. 2004;19:1571–1575. doi: 10.1093/ndt/gfh185. [DOI] [PubMed] [Google Scholar]
- 11.Bailie GR, Larkina M, Goodkin DA, Li Y, Pisoni RL, Bieber B, et al. Variation in intravenous iron use internationally and over time: the Dialysis Outcomes and Practice Patterns Study (DOPPS) Nephrol Dial Transplant. 2013;28:2570–2579. doi: 10.1093/ndt/gft062. [DOI] [PubMed] [Google Scholar]
- 12.Michael B, Coyne DW, Fishbane S, Folkert V, Lynn R, Nissenson AR, et al. Sodium ferric gluconate complex in hemodialysis patients: Adverse reactions compared to placebo and iron dextran. Kidney Int. 2002;61:1830–1839. doi: 10.1046/j.1523-1755.2002.00314.x. [DOI] [PubMed] [Google Scholar]
- 13.Coyne DW, Atkinson NF, Jr, Nissenson AR, Fishbane S, Agarwal R, Eschbach JW, et al. Sodium ferric gluconate complex in hemodialysis patients. II. Adverse reactions in iron dextran-sensitive and dextran-tolerant patients. Kidney Int. 2003;63:217–224. doi: 10.1046/j.1523-1755.2003.00703.x. [DOI] [PubMed] [Google Scholar]
- 14.Faich G, Strobos J. Sodium ferric gluconate complex in sucrose: safer intravenous iron therapy than iron dextrans. Am J Kidney Dis. 1999;33:464–470. doi: 10.1016/s0272-6386(99)70183-6. [DOI] [PubMed] [Google Scholar]
- 15.Chandler G, Harchowal J, Macdougall IC. Intravenous iron sucrose: Establishing a safe dose. Am J Kidney Dis. 2001;38:988–991. doi: 10.1053/ajkd.2001.28587. [DOI] [PubMed] [Google Scholar]
- 16.Auerbach M, Henry D, Derman RJ, Achebe MM, Thomsen LL, Glaspy J. A prospective, multi-center, randomized comparison of iron isomaltoside 1000 versus iron sucrose in patients with iron deficiency anemia; the FERWON-IDA trial. Am J Hematol. 2019;94:1007–1014. doi: 10.1002/ajh.25564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kochhar PK, Kaundal A, Ghosh P. Intravenous iron sucrose versus oral iron in the treatment of iron deficiency anemia in pregnancy: a randomized clinical trial. J Obstet Gynaecol Res. 2013;39:504–510. doi: 10.1111/j.1447-0756.2012.01982.x. [DOI] [PubMed] [Google Scholar]
- 18.Schröder O, Mickisch O, Seidler U, de Weerth A, Dignass AU, Herfarth H, et al. Intravenous iron sucrose versus oral iron supplementation for the treatment of iron deficiency anemia in patients with inflammatory bowel disease—a randomized, controlled, open-label, multicenter study. Am J Gastroenterol. 2005;100:2503–2509. doi: 10.1111/j.1572-0241.2005.00250.x. [DOI] [PubMed] [Google Scholar]
- 19.Lindgren S, Wikman O, Berits R, Blom H, Eriksson A, Grännö C, et al. Intravenous iron sucrose is superior to oral iron sulphate for correcting anaemia and restoring iron stores in IBD patients: a randomized, controlled, evaluator blind, multicentre study. Scand J Gastroenterol. 2009;44:838–845. doi: 10.1080/00365520902839667. [DOI] [PubMed] [Google Scholar]
- 20.Charytan C, Bernardo MV, Koch TA, Butcher A, Morris D, Bregman DB. Intravenous ferric carboxymaltose versus standard medical care in the treatment of iron deficiency anemia in patients with chronic kidney disease: a randomized, active-controlled, multi-center study. Nephrol Dial Transplant. 2013;28:953–964. doi: 10.1093/ndt/gfs528. [DOI] [PubMed] [Google Scholar]
- 21.Breymann C, Gliga F, Bejenariu C, Strizhova N. Comparative efficacy and safety of intravenous ferric carboxymaltose in the treatment of postpartum iron deficiency anemia. Int J Gynaecol Obstet. 2008;101:67–73. doi: 10.1016/j.ijgo.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Seid MH, Derman RJ, Baker JB, Banach W, Goldberg C, Rogers R. Ferric carboxymaltose injection in the treatment of postpartum iron deficiency anemia: a randomized controlled clinical trial. Am J Obstet Gynecol. 2008;199(435):e1–7. doi: 10.1016/j.ajog.2008.07.046. [DOI] [PubMed] [Google Scholar]
- 23.Moore RA, Gaskell H, Rose P, Allan J. Meta-analysis of efficacy and safety of intravenous ferric carboxymaltose (Ferinject) from clinical trial reports and published trial data. BMC Blood Disorders. 2011 doi: 10.1186/1471-2326-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barish CF, Koch T, Butcher A, Morris D, Bregman DB. Safety and efficacy of intravenous ferric carboxymaltose (750 mg) in the treatment of iron deficiency anemia: two randomized, controlled trials. Anemia. 2012 doi: 10.1155/2012/172104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van Wyck DB, Mangione A, Morrison J, Hadley PE, Jehle JA, Goodnough LT. Large-dose intravenous ferric carboxymaltose injection for iron deficiency anemia in heavy uterine bleeding: a randomized, controlled trial. Transfusion. 2009;49:2719–2728. doi: 10.1111/j.1537-2995.2009.02327.x. [DOI] [PubMed] [Google Scholar]
- 26.Van Wyck DB, Martens MG, Seid MH, Baker JB, Mangione A. Intravenous ferric carboxymaltose compared with oral iron in the treatment of postpartum anemia: a randomized controlled trial. Obstet Gynecol. 2007;110:267–278. doi: 10.1097/01.AOG.0000275286.03283.18. [DOI] [PubMed] [Google Scholar]
- 27.Qunibi WY, Martinez C, Smith M, Benjamin J, Mangione A, Roger SD. A randomized controlled trial comparing intravenous ferric carboxymaltose with oral iron for treatment of iron deficiency anaemia of non-dialysis-dependent chronic kidney disease patients. Nephrol Dial Transplant. 2011;26:1599–1607. doi: 10.1093/ndt/gfq613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Becuzzi N, Zimmermann R, Krafft A. Long-term efficacy of postpartum intravenous iron therapy. Biomed Res Int. 2014 doi: 10.1155/2014/815437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jose A, Mahey R, Sharma JB, Bhatla N, Saxena R, Kalaivani M, et al. Comparison of ferric carboxymaltose and iron sucrose complex for treatment of iron deficiency anemia in pregnancy-randomised controlled trial. BMC Pregnancy Childbirth. 2019 doi: 10.1186/s12884-019-2200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Onken JE, Bregman DB, Harrington RA, Morris D, Acs P, Akright B, et al. A multicenter, randomized, active-controlled study to investigate the efficacy of intravenous ferric carboxymaltose in patients with iron deficiency anemia. Transfusion. 2014;54:306–315. doi: 10.1111/trf.12289. [DOI] [PubMed] [Google Scholar]
- 31.Balakrishnan VS, Rao M, Kausz AT, Brenner L, Pereira BJG, Frigo TB, et al. Physiochemical properties of ferumoxytol, a new intravenous iron preparation. Eur J Clin Invest. 2009;39:489–496. doi: 10.1111/j.1365-2362.2009.02130.x. [DOI] [PubMed] [Google Scholar]
- 32.Jahn MR, Andreasen HB, Futterer S, Nawroth T, Schunemann V, Kolb U, et al. A comparative study of the physicochemical properties of iron isomaltoside 1000 (Monofer), a new intravenous iron preparation and its clinical implications. Eur J Pharm Biopharm. 2011;78:480–491. doi: 10.1016/j.ejpb.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 33.Wikstrom B, Bhandari S, Barany P, Kalra PA, Ladefoged S, Wilske J, et al. Iron isomaltoside 1000: a new intravenous iron for treating iron deficiency in chronic kidney disease. J Nephrol. 2011;24:589–596. doi: 10.5301/JN.2011.6248. [DOI] [PubMed] [Google Scholar]
- 34.Reinisch W, Staun M, Tandon RK, Altorjay I, Thillainayagam AV, Gratzer C, et al. A randomized, open-label, non-inferiority study of intravenous iron isomaltoside 1,000 (Monofer) compared with oral iron for treatment of anemia in IBD (PROCEED) Am J Gastroenterol. 2013;108:1877–1888. doi: 10.1038/ajg.2013.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kalra PA, Bock K, Meldal M. Iron isomaltoside 1000: a new high dose option for parenteral iron therapy. Port J Nephrol Hypert. 2012;26:13–24. [Google Scholar]
- 36.Anker SD, Colet JC, Filippatos G, Willenheimer R, Dickstein K, Drexler H, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med. 2009;361:2436–2448. doi: 10.1056/NEJMoa0908355. [DOI] [PubMed] [Google Scholar]
- 37.Ponikowski P, van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, et al. Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symtomatic heart failure and iron deficiency. Eur Heart J. 2015;36:657–668. doi: 10.1093/eurheartj/ehu385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Veldhuisen DJ, Ponikowski P, van der Meer P, Metra M, Böhm M, Doletsky A, et al. Effect of ferric carboxymaltose on exercise capacity in patients with chronic heart failure and iron deficiency. Circulation. 2017;136:1374–1383. doi: 10.1161/CIRCULATIONAHA.117.027497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ponikowski P, Kirwan B, Anker SD, McDonagh T, Dorobantu M, Drozdz J, et al. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. Lancet. 2020;396:1895–1904. doi: 10.1016/S0140-6736(20)32339-4. [DOI] [PubMed] [Google Scholar]
- 40.Blazevic A, Hunze J, Boots JM. Severe hypophosphataemia after intravenous iron administration. Neth J Med. 2014;72:49–53. [PubMed] [Google Scholar]
- 41.Mani LY, Nseir G, Venetz JP, Pascual M. Severe hypophosphatemia after intravenous administration of iron carboxymaltose in a stable renal transplant recipient. Transplantation. 2010;90:804–805. doi: 10.1097/TP.0b013e3181f00a18. [DOI] [PubMed] [Google Scholar]
- 42.Schouten BJ, Hunt PJ, Livesey JH, Frampton CM, Soule SG. FGF23 elevation and hypophosphatemia after intravenous iron polymaltose: a prospective study. J Clin Endocrinol Metab. 2009;94:2332–2337. doi: 10.1210/jc.2008-2396. [DOI] [PubMed] [Google Scholar]
- 43.Sáchez González R, Ternavasio-de la Vega HG, Moralejo Alonso L, Ines Revuelta S, Fuertes MA. Intravenous ferric carboxymaltose-associated hypophosphatemia in patients with iron deficiency anemia A common side effect. Med Clin (Barc) 2015;145:108–111. doi: 10.1016/j.medcli.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 44.Barea Mendoza JA, Gredilla Zubiria I, Gonzalez Olmedo J, Mateo AS. Hypophosphatemia, a poorly known adverse reaction of intravenous use of iron. Med Clin (Barc) 2014;143:284–285. doi: 10.1016/j.medcli.2013.11.030. [DOI] [PubMed] [Google Scholar]
- 45.Fierz YC, Kenmeni R, Gonthier A, Lier F, Pralong F, Coti BP. Severe and prolonged hypophosphatemia after intravenous iron administration in a malnourished patient. Eur J Clin Nutr. 2014;68:531–533. doi: 10.1038/ejcn.2014.20. [DOI] [PubMed] [Google Scholar]
- 46.Vandemergel X, Vandergheynst F. Potentially life-threatening phosphate diabetes induced by ferric carboxymaltose injection: A case report and review of the literature. Case Rep Endocrinol. 2014 doi: 10.1155/2014/843689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anand G, Schmid C. Severe hypophosphataemia after intravenous iron administration. BMJ Case Rep. 2017 doi: 10.1136/bcr-2016-219160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fragkos KC, Sehgal V, Rogers J, Arulrajan S, Pavanerathan P, Barragry J, et al. Hypophosphataemia after intravenous iron therapy with ferric carboxymaltose—real world experience from a tertiary centre in the UK. GastroHep. 2020 doi: 10.1002/ygh2.415. [DOI] [Google Scholar]
- 49.Teh KK, Chuah MB, Tay S, Lim AY, Khoo JJ. Severe hypophosphataemia as a complication of parenteral iron replacement. Eur J Case Rep Int Med. 2020 doi: 10.12890/2020_001860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Glaspy JA, Lim-Watson MZ, Libre MA, Karkare SS, Hadker N, Bajic-Lucas A, et al. Hypophosphatemia associated with intravenous iron therapies for iron deficiency anemia: a systematic literature review. Ther Clin Risk Manag. 2020;16:245–259. doi: 10.2147/TCRM.S243462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zoller H, Schaefer B, Glodny B. Iron-induced hypophophatemia: an emerging complication. Curr Opin Nephrol Hypertens. 2017;26:266–275. doi: 10.1097/MNH.0000000000000329. [DOI] [PubMed] [Google Scholar]
- 52.Favrat B, Balck K, Breymann C, Hedenus M, Keller T, Mezzacasa A, et al. Evaluation of a single dose of ferric carboxymaltose in fatigued, iron-deficient women—PREFER a randomized, placebo-controlled study. PLoS ONE. 2014;9(4):e94217. doi: 10.1371/journal.pone.0094217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wolf M, White KE. Coupling fibroblast growth factor 23 production and cleavage: iron deficiency, rickets, and kidney disease. Curr Opin Nephrol Hypertens. 2014;23:411–419. doi: 10.1097/01.mnh.0000447020.74593.6f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wolf M, Koch TA, Bregman DB. Effects of iron deficiency anemia and its treatment on fibroblast growth factor 23 and phosphate homeostasis in women. J Bone Miner Res. 2013;28:1793–1803. doi: 10.1002/jbmr.1923. [DOI] [PubMed] [Google Scholar]
- 55.Li X, Lozovatsky L, Fretz JA, Finberg KE. Bone marrow sinusoidal endothelial cells are a site of Fgf23 upregulation in iron deficiency anemia. Blood. 2021 doi: 10.1182/blood-2021-153329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wolf M, Rubin J, Achebe M, Econs MJ, Peacock M, Imel EA, et al. Effects on iron isomaltoside vs ferric carboxymaltose on hypophosphatemia in iron-deficiency anemia. J Am Med Assoc. 2020;232:432–443. doi: 10.1001/jama.2019.22450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Frazier R, Hodakowski A, Cai X, Lee J, Zakarija A, Stein B, et al. Effects of ferric carboxymaltose on markers of mineral and bone metabolism: a single-center prospective study of women with iron deficiency. Bone. 2020 doi: 10.1016/j.bone.2020.115559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wolf M, Chertow GM, Macdougall IC, Kaper R, Krop J. Randomized trial of intravenous iron-induced hypophosphatemia. JCI Insight. 2018 doi: 10.1172/jci.insight.124486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hu MC, Shi M, Moe OW. Role of alpha-Klotho and FGF23 in regulation of type II Na-dependent phosphate co-transporters. Pflugers Arch. 2019;471:99–108. doi: 10.1007/s00424-018-2238-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shimada T, Yamazaki Y, Takahashi M, Hasegawa H, Urakawa I, Oshima T, et al. Vitamin D receptor-independent FGF23 actions in regulating phosphate and vitamin D metabolism. Am J Physiol Renal Physiol. 2005;289:F1088–F1095. doi: 10.1152/ajprenal.00474.2004. [DOI] [PubMed] [Google Scholar]
- 61.Shimada T, Mizutani S, Muto T, Yoneya T, Hino R, Takeda S, et al. Cloning and characterization of FGF23 as a causative factor of tumor-induced osteomalacia. Proc Nat Acad Sci U S A. 2001;98:6500–6505. doi: 10.1073/pnas.101545198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Larsson T, Mardell R, Schipani E, Ohlsson C, Ljunggren O, Tenehouse HS, et al. Transgenic mice expressing fibroblast growth factor 23 under the controle of the alpha1(I) collagen promoter exhibit growth retardation, osteomalacia, and disturbed phosphate homeostasis. Endocrinology. 2004;145:3084–3086. doi: 10.1210/en.2004-0354. [DOI] [PubMed] [Google Scholar]
- 63.Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi Y, et al. FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res. 2004;19:429–435. doi: 10.1359/JBMR.0301264. [DOI] [PubMed] [Google Scholar]
- 64.Stöhr R, Sandstede L, Heine GH, Marx N, Brandenburg V. High-dose ferric carboxymaltose in patients with HFrEF induces significant hypophosphatemia. J Am Coll Cardiol. 2018;71:2270–2271. doi: 10.1016/j.jacc.2018.03.448. [DOI] [PubMed] [Google Scholar]
- 65.Emrich IE, Lizzi F, Siegel JD, Seiler-Mussler S, Ukena C, Kaddu-Mulindwa D, et al. Hypophosphatemia after high-dose iron repletion with ferric carboxymaltose and ferric derisomaltose - the randomized controlled HOMe aFers study. BMC Med. 2020 doi: 10.1186/s12916-020-01643-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Amarnani R, Travis S, Javaid MK. Novel use of burosumab in refractory iron-induced FGF23-mediated hypophosphataemic osteomalacia. Rheumatology. 2020;59:2168–2170. doi: 10.1093/rheumatology/kez675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kalra PA, Bhandari S. Efficacy and safety of iron isomaltoside (Monofer((R))) in the management of patients with iron deficiency anemia. Int J Nephrol Renovasc Dis. 2016;9:53–64. doi: 10.2147/IJNRD.S89704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dahlerup JF, Jacobsen BA, van der Woude J, Bark L, Thomsen LL, Lindgren S. High-dose fast infusion of parenteral iron isomaltoside is efficacious in inflammatory bowel disease patients with iron-deficiency anaemia without profound changes in phosphate or fibroblast growth factor 23. Scand J Gastroenterol. 2016;51:1332–1338. doi: 10.1080/00365521.2016.1196496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Schaefer B, Würtinger P, Finkenstedt A, Braithwaite V, Viveiros A, Effenberger M, et al. Choice of high-dose intravenous iron preparation determines hypophosphatemia risk. PLoS ONE. 2016 doi: 10.1371/journal.pone.0167146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Detlie TE, Lindstrøm JC, Jahnsen ME, Finnes E, Zoller H, Moum B, et al. Incidence of hypophosphatemia in patients with inflammatory bowel disease treated with ferric carboxymaltose or iron isomaltoside. Aliment Pharmacol Ther. 2019;50:397–406. doi: 10.1111/apt.15386. [DOI] [PubMed] [Google Scholar]
- 71.Zoller H, Wolf M, Blumenstein I, Primas C, Lindgren S, Thomsen LL, et al. Effects of ferric derisomaltose and ferric carboxymaltose on hypophosphatemia in iron-deficiency anaemia due to inflammatory bowel disease: a phase IV randomised clinical trial. https://www.ecco-ibd.eu: Abstract DOP89 ECCO 2021. Accessed 18 Aug 2022. [DOI] [PMC free article] [PubMed]
- 72.Schaefer B, Tobiasch M, Viveiros A, Tilg H, Kennedy NA, Wolf M, et al. Hypophosphataemia after treatment of iron deficiency with intravenous ferric carboxymaltose or iron isomaltoside—a systematic review and meta-analysis. Br J Clin Pharmacol. 2020 doi: 10.1111/bcp.14643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Derman R, Roman E, Modiano MR, Achebe MM, Thomsen LL, Auerbach M. A randomized trial of iron isomaltoside versus iron sucrose in patients with iron deficiency anemia. Am J Hematol. 2017;92:286–291. doi: 10.1002/ajh.24633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hussain I, Bhoyroo J, Butcher A, Koch TA, He A, Bregman DB. Direct comparison of the safety and efficacy of ferric carboxymaltose versus iron dextran in patients with iron deficiency anemia. Anemia. 2013 doi: 10.1155/2013/169107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schaefer B, Zoller HWM. Risk factors for and effects of persistent and severe hypophosphatemia following ferric carboxymaltose. J Clin Endocrinol Metab. 2022;107:1009–1019. doi: 10.1210/clinem/dgab852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hardy S, Vandemergel X. Intravenous iron administration and hypophosphatemia in clinical practice. Int J Rheumatol. 2015 doi: 10.1155/2015/468675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rosano G, Schiefke I, Göhring U, Fabien V, Bonassi S, Stein J. A pooled analysis of serum phosphate measurements and potential hypophosphataemia events in 45 interventional trials with ferric carboxymaltose. J Clin Med. 2020 doi: 10.3390/jcm9113587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Trummer C, Schwetz V, Pandis M, Grübler MR, Verheyen N, Gaksch M, et al. Effects of vitamin D supplementation on FGF-23: A randomized-controlled trial. Eur J Nutr. 2019;58:697–703. doi: 10.1007/s00394-018-1672-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schoeb M, Räss A, Frei N, Aczél S, Brändle M, Bilz S. High risk of hypophosphatemia in patients with previous bariatric surgery receiving ferric carboxymaltose: a prospective cohort study. Obes Surg. 2020;30:2659–2666. doi: 10.1007/s11695-020-04544-x. [DOI] [PubMed] [Google Scholar]
- 80.Sari V, Atiqi R, Hoorn EJ, Heijboer AC, van Gelder T, Hesselink DA. Ferric carboxymaltose-induced hypophosphataemia after kidney transplantation. Neth J Med. 2017;75:65–73. [PubMed] [Google Scholar]
- 81.Smyth B, Ong S. Severe hypocalcaemia and hypophosphataemia following intravenous iron and denosumab: a novel drug interaction. Intern Med J. 2016;46:360–363. doi: 10.1111/imj.13001. [DOI] [PubMed] [Google Scholar]
- 82.Cianciolo G, Tondolo F, Barbuto S, Iacovella F, Zavatta G, Altieri P, et al. Denosumab-induced hypocalcemia and hyperparathyroidism in de novo kidney transplant recipients. Am J Nephrol. 2021;52:611–619. doi: 10.1159/000518363. [DOI] [PubMed] [Google Scholar]
- 83.Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756–765. doi: 10.1056/NEJMoa0809493. [DOI] [PubMed] [Google Scholar]
- 84.Tsvetov G, Amitai O, Shochat T, Shimon I, Akirov A, Diker-Cohen T. Denosumab-induced hypocalcemia in patients with osteoprosis: can you know who will get low? Osteoporos Int. 2020;31:655–665. doi: 10.1007/s00198-019-05261-7. [DOI] [PubMed] [Google Scholar]
- 85.Tanaka S, Mizutani H, Tsuruya E, Fukuda R, Kuge K, Okubo N. Long-term safety and effectiveness of denosumab in Japanese patients with osteoporosis: 3-year post-marketing surveillance study. J Bone Miner Metab. 2021;39:463–473. doi: 10.1007/s00774-020-01180-4. [DOI] [PubMed] [Google Scholar]
- 86.Kim KJ, Hong N, Lee S, Kim M, Rhee Y. A simple-to-use score for identifying individuals at high risk of denosumab-associated hypocalcemia in postmenopausal osteoprosis: a real-world cohort study. Calcif Tissue Int. 2020;107:567–575. doi: 10.1007/s00223-020-00754-8. [DOI] [PubMed] [Google Scholar]
- 87.Huynh ALH, Baker ST, Stewardson AJ, Johnson DF. Denosumab-associated hypocalcaemia: incidence, severity and patient characteristics in a tertiary hospital setting. Pharmacoepidemiol Drug Saf. 2016;25:1274–1278. doi: 10.1002/pds.4045. [DOI] [PubMed] [Google Scholar]
- 88.Ishikawa K, Nagai T, Sakamoto K, Ohara K, Euro T, Ito H, et al. High bone turnover elevates risk of denosumab-induced hypocalcemia in women with postmenopausal osteoporosis. Ther Clin Risk Manag. 2016;12:1831–1840. doi: 10.2147/TCRM.S123172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Harris RE, Armstrong L, Curtis L, Garrick VG, Tayler R, Hansen R, et al. Severe hypophosphataemia following ferric carboxymaltose infusion in paediatric patients with inflammatory bowel disease. Frontline Gastroenterol. 2019;11:324–326. doi: 10.1136/flgastro-2019-101242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cococcioni L, Pensabene L, El-Khouly S, Chadokufa S, McCartney S, Saliakellis E, et al. Ferric carboxymaltose treatment for iron deficiency anemia in children with inflammatory bowel disease: Efficacy and risk of hypophosphatemia. Dig Liver Dis. 2021;53:830–834. doi: 10.1016/j.dld.2021.02.017. [DOI] [PubMed] [Google Scholar]
- 91.Posod A, Schaefer B, Mueller T, Zoller H, Kiechl-Kohlendorfer U. Hypophosphatemia in children treated with ferric carboxymaltose. Acta Paediatr. 2020;109:1491–1492. doi: 10.1111/apa.15178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kirk SE, Scheurer ME, Bernhardt MB, Mahoney DH, Powers JM. Phosphorus levels in children treated with intravenous ferric carboxymaltose. Am J Hematol. 2021;96:E215–E218. doi: 10.1002/ajh.26165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Boettger SF, Angersbach B, Klimek CN, Monteiro Wanderley AL, Shaibekov A, Sieske L, et al. Prevalence and predictors of vitamin D-deficiency in frail and older hospitalized patients. BMC Geriatr. 2018 doi: 10.1186/s12877-018-0919-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Duarte C, Carvalheiro H, Rodrigues AM, Dias SS, Marques A, Santiago T, et al. Prevalence of vitamin D deficiency and its predictors in the Portuguese population: a nationwide population-based study. Arch Osteoporos. 2020 doi: 10.1007/s11657-020-0695-x. [DOI] [PubMed] [Google Scholar]
- 95.Wei J, Zhu A, Ji JS. A comparison study of vitamin D deficiency among older adults in China and the United States. Sci Rep. 2019 doi: 10.1038/s41598-019-56297-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Besora-Moreno M, Llauradó E, Tarro L, Solà R. Social and Economic factors and malnutrition or the risk of malnutrition in the elderly: a systematic review and meta-analysis of observational studies. Nutrients. 2020 doi: 10.3390/nu12030737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Corish CA, Bardon LA. Malnutrition in older adults: screening and determinants. Proc Nutr Soc. 2019;78:372–379. doi: 10.1017/S0029665118002628. [DOI] [PubMed] [Google Scholar]
- 98.Ames BN, Grant WB, Willett WC. Does the high prevalence of vitamin D deficiency in African Americans contribute to health disparities? Nutrients. 2021 doi: 10.3390/nu13020499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Imel EA, Liu Z, Coffman M, Acton D, Mehta R, Econs MJ. Oral iron replacement normalizes fibroblast growth factor 23 in iron-deficient patients with autosomal dominant hypophophatemic rickets. J Bone Miner Res. 2020;35:231–238. doi: 10.1002/jbmr.3878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Menon LP, Weinstein RS. Iron replacement ameliorates hypophosphatemia in autosomal dominant hypophosphatemic rickets: a review of the role of iron. Bone. 2020 doi: 10.1016/j.bone.2019.115137. [DOI] [PubMed] [Google Scholar]
- 101.Takeda Y, Komaba H, Goto S, Fuji H, Umezu M, Hasegawa H, et al. Effect of intravenous saccharated ferric oxide in serum FGF23 and mineral metabolism in hemodialysis patients. Am J Nephrol. 2011;33:421–426. doi: 10.1159/000327019. [DOI] [PubMed] [Google Scholar]
- 102.Faul C, Amaral AP, Oskouei B, Hu M, Sloan A, Isakova T, et al. FGF23 induces left ventricular hypertrophy. J Clin Invest. 2011;121:4393–4408. doi: 10.1172/jci46122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Bergmark BA, Udell JA, Morrow DA, Cannon CP, Steen DL, Jarolim P, et al. Association of fibroblast growth factor 23 with recurrent cardiovascular events in patients after an acute coronary syndrome: a secondary analysis of a randomized clinical trial. JAMA Cardiol. 2018;3:473–480. doi: 10.1001/jamacardio.2018.0653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Parker BD, Schurgers LJ, Brandenburg VM, Christenson RH, Vermeer C, Ketteler M, et al. The associations of fibroblast growth factor 23 and uncarboxylated matrix Gla protein with mortality in coronary artery disease: the Heart and Soul Study. Ann Intern Med. 2010;152:640–648. doi: 10.7326/0003-4819-152-10-201005180-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Scialla JJ, Xie H, Rahman M, Anderson AH, Isakova T, Ojo A, et al. Fibroblast growth factor-23 and cardiovascular events in CKD. J Am Soc Nephrol. 2014;25:349–360. doi: 10.1681/ASN.2013050465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Leifheit-Nestler M, Große Siemer R, Flasbart K, Richter B, Kirchhoff F, Ziegler WH, et al. Induction of cardiac FGF23/FGFR4 expression is associated with left ventricular hypertrophy in patients with chronic kidney disease. Nephrol Dial Transplant. 2016;31:1088–1099. doi: 10.1093/ndt/gfv421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bouma-de Krijger A, Bots ML, Vervloet M, Blankestijn PJ, ter Wee PW, van Zuilen AD, et al. Time-averaged level of fibroblast growth factor-23 and clinical events in chronic kidney disease. Nephrol Dial Transplant. 2014;29:88–97. doi: 10.1093/ndt/gft456. [DOI] [PubMed] [Google Scholar]
- 108.Seiler S, Rogacev KS, Roth HJ, Shafein P, Emrich I, Neuhaus S, et al. Associations of FGF-23 and sKlotho with cardiovascular outcomes among patients with CKD stages 2–4. Clin J Am Soc Nephrol. 2014;9:1049–1058. doi: 10.2215/CJN.07870713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Isakova T, Xie H, Yang W, Xie D, Anderson AH, Scialla J, et al. Fibroblast growth factor 23 and risk of mortality and end-stage renal disease in patients with chronic kidney disease. J Am Med Assoc. 2011;305:2432–2439. doi: 10.1001/jama.2011.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Scialla JJ, Astor BC, Isakova T, Xie H, Appel LJ, Wolf M. Mineral metabolites and CKD progression in African Americans. J Am Soc Nephrol. 2013;24:125–135. doi: 10.1681/ASN.2012070713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sharma S, Hanudel MR, Ix JH, Salusky IB, Ganz T, Nguyen K. Elevated fibroblast growth factor 23 levels are associated with greater diastolic dysfunction in ESRD. Kidney Int Rep. 2019;4:1748–1751. doi: 10.1016/j.ekir.2019.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Komaba H, Fuller DS, Taniguchi M, Yamamoto S, Nomura T, Zhao J, et al. Fibroblast growth factor 23 and mortality among prevalent hemodialysis patients in the Japan dialysis outcomes and practice study. Kidney Int Rep. 2020;5:1956–1964. doi: 10.1016/j.ekir.2020.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nowak A, Friedrich B, Artunc F, Serra AL, Breidthardt T, Twerenbold R, et al. Prognostic value and link to atrial fibrillation of soluble Klotho and FGF23 in hemodialysis patients. PLoS ONE. 2014 doi: 10.1371/journal.pone.0100688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chonchoi M, Greene T, Zhang Y, Hoofnagle AN, Cheung AK. Low vitamin D and high fibroblast growth factor 23 serum levels associate with infectious and cardiac deaths in the HEMO study. J Am Soc Nephrol. 2016;27:227–237. doi: 10.1681/ASN.2014101009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gutiérrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A, et al. Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med. 2008;359:584–592. doi: 10.1056/NEJMoa0706130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Jovanovich A, You Z, Isakova T, Now K, Cheung A, Wolf M, et al. Fibroblast growth factor 23 trajectories in chronic hemodialysis patients: Lessons from the HEMO study. Am J Nephrol. 2019;49:263–270. doi: 10.1159/000497445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Eisenga MF, Emans ME, van der Putten K, Cramer MJ, Diepenbroek A, Velthuis BK, et al. Epoietin beta and c-terminal fibroblast growth factor 23 in patients with chronic heart failure and chronic kidney disease. J Am Heart Assoc. 2019 doi: 10.1161/jaha.118.011130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Schaefer B, Glodny B, Zoller H. Blood and bone loser. Gastroenterology. 2017;152:e5–6. doi: 10.1053/j.gastro.2016.09.050. [DOI] [PubMed] [Google Scholar]
- 119.Callejas-Moraga EL, Casado E, Gomez-Nuñez M, Caresia-Aroztegui AP. Severe osteomalacia with multiple insufficiency fractures secondary to intravenous iron therapy in a patient with Rendu-Osler-Weber syndrome. Bone Rep. 2020 doi: 10.1016/j.bonr.2020.100712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tozzi D, Tozzi J. Osteomalacia and insufficiency fractures secondary to intravenous iron therpay: A case report. J Orthop Case Rep. 2020;10:4–7. doi: 10.13107/jocr.2019.v10.i01.1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Klein K, Asaad S, Econs M, Rubin JE. Severe FGF23-based hypophosphataemic osteomalacia due to ferric carboxymaltose administration. BMJ Case Rep. 2018 doi: 10.1136/bcr-2017-222851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Bartko J, Röscher P, Zandieh S, Brehm A, Zwerina J, Klaushofer K. Hypophosphatemia, severe bone pain, gait disturbance, and fatigue fractures after iron substitution in inflammatory bowel disease: a case report. J Bone Miner Res. 2018;33:534–539. doi: 10.1002/jbmr.3319. [DOI] [PubMed] [Google Scholar]
- 123.Sangrós Sahún MJ, Goñi Gironés E, Camarero Salazar A, Estébanez EC. Symptomatic hypophosphataemic osteomalacia secondary to treatment with ferric carboxymaltose detected in bone scintigraphy. Rev Esp Med Nucl Imagen Mol. 2016;35:391–393. doi: 10.1016/j.remn.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 124.Fang W, McMahon LP, Bloom S, Gargantuas M. Symptomatic severe hypophosphatemia after intravenous ferric carboxymaltose. JGH Open. 2019;3:438–440. doi: 10.1002/jgh3.12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Vilaca T, Velmurugan N, Smith C, Abrahamsen B, Eastell R. Osteomalacia as a complication of intravenous iron infusion: a systematic review of case-reports. J Bone Miner Res. 2022 doi: 10.1002/jbmr.4558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Schouten BJ, Doogue MP, Soule SG, Hunt PJ. Iron polymaltose-induced FGF23 elevation complicated by hypophosphataemic osteomalacia. Ann Clin Biochem. 2009;46:167–169. doi: 10.1258/acb.2008.008151. [DOI] [PubMed] [Google Scholar]
- 127.Bishay RH, Ganda K, Seibel MJ. Long-term iron polymaltose infusions associated with hypophosphataemic osteomalacia: A report of two cases and review of the literature. Thor Adv Endocrinol Metab. 2017;8:14–19. doi: 10.1177/2042018816678363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ishimaru D, Sumi H. A case of insufficiency fracture of the medial proximal tibia secondary to osteomalacia associated with long-term saccharated ferric oxide administration. Case Rep Orthop. 2017 doi: 10.1155/2017/1675654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Yamamoto S, Okada Y, Mori H, Kurozumi A, Torimoto K, Arao T, et al. Iatrogenic osteomalacia: report of two cases. J UOEH. 2013;35:25–31. doi: 10.7888/juoeh.35.25. [DOI] [PubMed] [Google Scholar]
- 130.Sato K, Nohtomi K, Demura H, Takeuchi A, Kobayashi T, Kazama J, et al. Saccharated ferric oxide (SFO)-induced osteomalacia: In vitro inhibition by SFO of bone formation and 1.25-dihydroxy-vitamin D production in renal tubules. Bone. 1997;21:57–64. doi: 10.1016/s8756-3282(97)00084-7. [DOI] [PubMed] [Google Scholar]
- 131.Reinisch W, Altorjay I, Zsigmond F, Primas C, Vogelsang H, Novacek G, et al. A 1-year trial of repeated high-dose intravenous iron isomaltoside 1000 to maintain stable hemoglobin levels in inflammatory bowel disease. Scand J Gastroenterol. 2015;50:1226–1233. doi: 10.3109/00365521.2015.1031168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Vilaca T, Velmurugan N, Smith C, Abrahamsen B, Eastell R. Osteomalacia as a complication of intravenous iron infusion: a systematic review of case reports. J Bone Miner Res. 2022;37:1188–1199. doi: 10.1002/jbmr.4558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Quarles LD. Skeletal secretion of FGF-23 regulates phosphate and vitamin D metabolism. Nat Rev Endocrinol. 2012;8:276–286. doi: 10.1038/nrendo.2011.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Szebeni J, Fishbane S, Hedenus M, Locatelli F, Patni S, Rampton D, et al. Hypersensitivity to intravenous iron: classification, terminology, mechanisms and management. Br J Pharmacol. 2015;172:5025–5036. doi: 10.1111/bph.13268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Rund D. Intravenous iron: do we adequately understand the shirt- and long-term risks in clinical practice? Br J Haematol. 2021;193:466–480. doi: 10.1111/bjh.17202. [DOI] [PubMed] [Google Scholar]
- 136.MacDougall IC, Vernon K. Complement Activation-Related Pseudo-Allergy: a fresh look at hypersensitivity reactions to intravenous iron. Am J Nephrol. 2017;45:60–62. doi: 10.1159/000451069. [DOI] [PubMed] [Google Scholar]
- 137.Rampton D, Folkersen J, Fishbane S, Hedenus M, Howaldt S, Locatelli F, et al. Hypersensitivity reactions to intravenous iron: guidance for risk minimization and management. Haematologica. 2014;99:1671–1676. doi: 10.3324/haematol.2014.111492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Szebeni J. Complement activation-related pseudoallergy: a stress reaction in blood triggered by nanomedicines and biologicals. Mol Immunol. 2014;61:163–173. doi: 10.1016/j.molimm.2014.06.038. [DOI] [PubMed] [Google Scholar]
- 139.Lim W, Afif W, Knowles S, Lim G, Lin Y, Mothersill C, et al. Canadian expert consensus: management of hypersensitivity reactions to intravenous iron in adults. Vox Sang. 2019;114:363–373. doi: 10.1111/vox.12773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Stojanovic S, Graudins LV, Kar Aung A, Grannell L, Hew M, Zubrinich C. Safety of intravenous iron following infusion reactions. J Allergy Clin Immunol Pract. 2021;9:1660–1666. doi: 10.1016/j.jaip.2020.11.028. [DOI] [PubMed] [Google Scholar]
- 141.Achebe M, DeLoughery TG. Clinical data for intravenous iron - debunking the hype around hypersensitivity. Transfusion. 2020;60:1154–1159. doi: 10.1111/trf.15837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Durup D, Schaffalitzky de Muckadell P, Strom CC. Evaluation of the reported rates of hypersensitivity reactions associated with iron dextran and ferric carboxymaltose based on global data from VigibaseTM and IQVIATM MIDAS® over a ten-year period from 2008 to 2017. Expert Revi Hematol. 2020;13:557–564. doi: 10.1080/17474086.2020.1738215. [DOI] [PubMed] [Google Scholar]
- 143.Ganzoni AM. Intravenous iron-dextran: therapeutic and experimental possibilities. Schweiz Med Wochenschr. 1970;100:301–303. [PubMed] [Google Scholar]
- 144.Ganzoni AM. Neue Aspekte des Eisenmangels. Schweiz Med Wochenschr. 1970;100:691–697. [PubMed] [Google Scholar]
- 145.Koch TA, Myers J, Goodnough LT. Intravenous iron therapy in patients with iron deficiency anemia: Dosing considerations. Anemia. 2015 doi: 10.1155/2015/763576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Evstatiev R, Marteau P, Iqbal T, Khalif IL, Stein J, Bokemeyer B, et al. FERGIcor, a randomized controlled trial on ferric carboxymaltose for iron deficiency anemia in inflammatory bowel disease. Gastroenterology. 2011;141:846–53.e2. doi: 10.1053/j.gastro.2011.06.005. [DOI] [PubMed] [Google Scholar]
- 147.Kassianides X, Bhandari S, Edu MC. Hypophosphataemia, fibroblast growth factor 23 and third-generation intravenous iron compounds: a narrative review. Drugs in Context. 2021;10:2020-11-3. doi: 10.7573/dic.2020-11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Froessler B, Collingwood J, Hodyl NA, Dekker G. Intravenous ferric carboxymaltose for anaemia in pregnancy. BMC Pregnancy Childbirth. 2014; http://www.biomedcentral.com/1471-2393/14/115. Accessed 18 Aug 2022. [DOI] [PMC free article] [PubMed]
- 149.Froessler B, Gajic T, Dekker G, Hodyl NA. Treatment of iron deficiency and iron deficiency anemia with intravenous ferric carboxymaltose in pregnancy. Arch Gynecol Obstet. 2018;298:75–82. doi: 10.1007/s00404-018-4782-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Wesström J. Safety of intravenous iron isomaltoside for iron deficiency and iron deficiency anemia in pregnancy. Arch Gynecol Obstet. 2020;301:1127–1131. doi: 10.1007/s00404-020-05509-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Li Nien Tan M, Windscheif P, Thornton G, Gaynor E, Rodrigues A, Howarth L. Retrospective review of effectiveness and safety of intravenous ferric carboxymaltose given to children with iron deficiency anaemia in one UK tertiary centre. Eur J Pediatr. 2017;176:1419–1423. doi: 10.1007/s00431-017-2995-8. [DOI] [PubMed] [Google Scholar]
- 152.Panagopoulou P, Alexiadou S, Ntoumpara M, Papazoglou A, Makis A, Tragiannidis A, et al. Safety of ferric carboxymaltose in children: Report of a case series from Greece and review of the literature. Pediatr Drugs. 2022;24:137–146. doi: 10.1007/s40272-022-00491-5. [DOI] [PubMed] [Google Scholar]
- 153.Powers JM, Shamoun M, McCavit TL, Adix L, Buchanan GR. Intravenous ferric carboxymaltose in children with iron deficiency anemia who respond poorly to oral iron. J Pediatr. 2017;180:212–216. doi: 10.1016/jpeds.2016.09.053. [DOI] [PubMed] [Google Scholar]
- 154.Carman N, Muir R, Lewindon P. Ferric carboxymaltose in the treatment of iron deficiency in pediatric inflammatory bowel disease. Transl Pediatr. 2019;8:28–34. doi: 10.21037/tp.2019.01.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Dwyer JP, Sika M, Schulman G, Chang IJ, Anger M, Smith M, et al. Dose-response and efficacy of ferric citrate to treat hyperphosphatemia in hemodialysis patients: a short-term randomized trial. Am J Kidney Dis. 2013;61:759–766. doi: 10.1053/j.ajkd.2012.11.041. [DOI] [PubMed] [Google Scholar]
- 156.Lewis JB, Sika M, Koury MJ, Chuang P, Schulman G, Smith MT, et al. Ferric citrate controls phosphorus and delivers iron in patients on dialysis. J Am Soc Nephrol. 2015;26:493–503. doi: 10.1681/ASN.2014020212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Umanath K, Jalal DI, Greco BA, Umeukeje EM, Reisin E, Manley J, et al. Ferric citrate reduces intravenous iron and erythopoiesis-stimulating agent use in ESRD. J Am Soc Nephrol. 2015;26:2578–2587. doi: 10.1681/ASN.2014080842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Vaziri ND, Kalantar-Zadeh K, Wish JB. New options for iron supplementation in maintenance hemodialysis patients. Am J Kidney Dis. 2016;67:367–375. doi: 10.1053/j.ajkd.2015.09.031. [DOI] [PubMed] [Google Scholar]
- 159.Womack R, Berru F, Panwar B, Gutiérrez OM. Effect of ferric citrate versus ferrous sulfate on iron and phosphate parameters in patients with iron deficiency and CKD. Clin J Am Soc Nephrol. 2020;15:1251–1258. doi: 10.2215/CJN.15291219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hanudel NR, Czaya B, Wong S, Rappaport M, Namjoshi S, Chua K, et al. Enteral ferric citrate absorption is dependent on the iron transport protein ferroportin. Kidney Int. 2022;101:711–719. doi: 10.1016/kint.2021.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Felsenfeld AJ, Levine BS. Approach to treatment of hypophosphatemia. Am J Kidney Dis. 2012;60:655–661. doi: 10.1053/j.ajkd.2012.03.024. [DOI] [PubMed] [Google Scholar]
- 162.Prats M, Font R, Garcia C, Cabré C, Jariod M, Martinez Vea A. Effect of ferric carboxymaltose on serum phosphate and C-terminal FGF23 levels in non-dialysis chronic kidney disease patients: Post-hoc analysis of a prospective study. BMC Nephrol. 2013. http://www.biomedcentral.com/1471-2369/14/167. Accessed 18 Aug 2022. [DOI] [PMC free article] [PubMed]
- 163.Gaasbeek A, Meinders AE. Hypophosphatemia: An update on its etiology and treatment. Am J Med. 2005;118:1094–1101. doi: 10.1016/j.amjmed.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 164.Riella LV, Rennke HG, Grafals M, Chandraker A. Hypophosphatemia in kidney transplant recipients: Report of acute phosphate nephropathy as a complication of therapy. Am J Kidney Dis. 2011;57:641–645. doi: 10.1053/j.ajkd.2010.11.024. [DOI] [PubMed] [Google Scholar]
- 165.Alon US, Levy-Olomucki R, Moore WV, Stubbs J, Liu S, Quarles LD. Calcimimetics as an adjuvant for familial hypophosphatemic rickets. Clin J Am Soc Nephrol. 2008;3:658–664. doi: 10.2215/CJN.04981107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Antoniucci DM, Yamashita T, Portale AA. Dietary phosphorus regulates serum fibroblast growth factor-23 concentrations in healthy men. J Clin Endocrinol Metab. 2006;91:3144–3149. doi: 10.1210/jc.2006-0021. [DOI] [PubMed] [Google Scholar]
- 167.Ferrari SL, Bonjour J, Rizzoli R. Fibroblast growth factor-23 relationship to dietary phosphate and renal phosphate handling in healthy young men. J Clin Endocrinol Metab. 2005;90:1519–1524. doi: 10.1210/jc.2004-1039. [DOI] [PubMed] [Google Scholar]
- 168.Carpenter TO, Insogna KL, Zhang JH, Ellis B, Nieman S, Simpson C, et al. Circulating levels of soluble klotho and FGF23 in X-linked hypophosphatemia: circadian variance, effects of treatment, and relationship to parathyroid status. J Clin Endocrinol Metab. 2010;95:E352–E357. doi: 10.1210/jc.2010-0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Carpenter TO, Whyte MP, Irmel EA, Boot AM, Högler W, Linglart A, et al. Burosumab therapy in children with X-linked hypophosphatemia. N Engl J Med. 2018;378:1987–1998. doi: 10.1056/NEJMoa1714641. [DOI] [PubMed] [Google Scholar]
- 170.Imei EA, Glorieux FH, Whyte MP, Munns CF, Ward LM, Nilsson O, et al. Burosumab versus conventional therapy in children with X-linked hypophosphataemia: a randomised, active-controlled, open-label, phase 3 trial. Lancet. 2019;393:2416–2427. doi: 10.1016/S0140-6736(19)30654-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.de Beur SMJ, Miller PD, Weber TJ, Peacock M, Insogna K, Kumar R, et al. Burosumab for the treatment of tumor-induced osteomalacia. J Bone Miner Res. 2020 doi: 10.1002/jbmr.4233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Day AL, Gutiérrez OM, Guthrie BL, Saag KG. Burosumab in tumor-induced osteomalacia: a case report. Joint Bone Spine. 2020;87:81–83. doi: 10.1016/j.jbspin.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 173.Prié D, Benqué Blanchet F, Essig M, Jourdain J, Friedlander G. Dipyridamole decreases renal phosphate leak and augments serum phosphorus in patients with low renal phosphate threshold. J Am Soc Nephrol. 1998;9:1264–1269. doi: 10.1681/ASN.V971264. [DOI] [PubMed] [Google Scholar]
- 174.Geller JL, Khosravi A, Kelly MH, Riminucci M, Adams J, Collins MT. Clinical Vignette. Cinacalcet in the management of tumor-induced osteomalacia. J Bone Miner Res. 2007;22:931–937. doi: 10.1359/JBMR.070304. [DOI] [PubMed] [Google Scholar]
- 175.Liu ES, Carpenter TO, Gundberg CM, Simpson CA, Insogna KL. Calcitonin administration in X-linked hypophosphatemia. N Engl J Med. 2011;364:1678–1680. doi: 10.1056/NEJMc1010928. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The literature was partly taken from a previous publication. We conducted a search of Pubmed for additional literature on specific items to prove our message. In addition, the literature was recognized from references from trials and reviews. We tried to check opinions in reviews as much as possible by analyzing original reports. It was not intended to review all possible literature, since many reports reached the same conclusions and therefore not all reports are incorporated in this manuscript.