ABSTRACT
Background
Diaphragmatic dysfunction has been increasingly documented to play a critical role to determine ventilator dependency and failure of weaning.
Objective
The goal was to study the diagnostic accuracy of diaphragmatic rapid shallow breathing index (D-RSBI) as a predictor of weaning outcomes in comparison to RSBI.
Materials and methods
A prospective observational study on consecutively admitted patients who were intubated and mechanically ventilated for a duration of at least 48 hours was carried out. The right hemidiaphragm displacement [diaphragm displacement (DD)] was calculated by M-mode ultrasonography, and respiratory rate (RR) and tidal volume (TV) were documented from the ventilator readings. Rapid shallow breathing index (RSBI) was measured as RR/TV (in liters); D-RSBI was calculated as RR/DD (in millimeters) and expressed as breath/minute/millimeter. Extubation failure was defined as the reinstitution of mechanical ventilation at the end of, or during the spontaneous breathing trial (SBT), re-intubation or the need of noninvasive ventilation (NIV) for the patient within 48 hours of extubation.
Results
Of 101 screened patients, 50 patients met the inclusion criteria, of whom 45 patients had successful SBT, and finally, 41 patients could be successfully extubated. Hence, the overall rate of weaning failure in the study population was 18%. The areas under the receiver operator characteristic (ROC) curves for D-RSBI and RSBI were 0.97 and 0.70, respectively (p <0.0001). The Pearson's correlation among RSBI and D-RSBI was 0.81 (p-value <0.001).
Conclusion
Diaphragmatic rapid shallow breathing index has a positive correlation and greater diagnostic accuracy than RSBI, the conventional weaning index.
How to cite this article
Shamil PK, Gupta NK, Ish P, Sen MK, Kumar R, Chakrabarti S, et al. Prediction of Weaning Outcome from Mechanical Ventilation Using Diaphragmatic Rapid Shallow Breathing Index. Indian J Crit Care Med 2022;26(9):1000–1005.
Keywords: Critical care, Diaphragm, Ultrasonography, Ventilator weaning
Highlight
Diaphragmatic rapid shallow breathing index, which incorporates DD, has a greater diagnostic accuracy of weaning outcome in comparison to RSBI.
Introduction
The current weaning guidelines endorse applying SBT as a tool to predict outcomes. Lately, indices and weaning predictors have been introduced; however, none has shown high prognostic accuracy.1 Weaning failure is determined as either a failure of SBT or clinical worsening needing a re-intubation within 48 hours following extubation.2 Respiratory and cardiac failure are common reasons for weaning failure, while psychological, nutritional-related, or ventilator-related issues can also be contributory. Studies have shown that weaning failure has a prevalence of 20%, but it may vary with the type of patient population being taken care of (e.g., postsurgical versus nonsurgical).2
Diaphragmatic dysfunction has been increasingly documented to play a major role in ventilator dependency and failure of weaning. The diaphragmatic strength evaluation is based on calculating the maximal trans-diaphragm pressure generated by the diaphragm when phrenic nerve stimulation is carried out. The technique is invasive, primarily research-based, and difficult to emulate in daily ICU settings.3 Bedside diaphragmatic ultrasonography is a noninvasive, repeatable, and real-time method to assess patient inspiratory effort during the weaning period using DD in spontaneous or assisted breathing.4 Diaphragmatic dysfunction (less than 10 mm) is a reliable predictor of weaning failure.5,6
The RSBI is the most investigated predictor of weaning outcomes, but it has a wide range of sensitivity and specificity. Diaphragmatic RSBI (D-RSBI) is a novel index, where the DD surrogates the TV.7,8 While calculating RSBI, the role of the active accessory muscles to deliver the TV could bargain its accuracy of successful weaning by concealing the diaphragmatic dysfunction.9 Given limited data, the present study aimed at comparing the diagnostic accuracy of D-RSBI with traditional RSBI to predict weaning outcomes.
Materials and Methods
The current study is a prospective observational study carried out for a period of 18 months, on consecutively admitted critically ill patients in the ICU. Ethical committee approval for the study was taken. Informed consent was obtained from each patient or from the next of kin.
Patients who were intubated and mechanically ventilated for more than 48 hours and who were ready for the first SBT as per the weaning criteria used in the intensive care unit were enrolled for the study. The weaning criteria included: (a) Resolution of acute phase of the disease; (b) Adequate mentation; (c) Systolic blood pressure of 90–160 mm Hg (no or minimal vasopressor); (d) Absence of excessive trachea-bronchial secretion; (e) Stable metabolic status; (f) pH >7.30; (g) PaO2 >60 mm Hg on PEEP <8 cm and FiO2 <0.5; (h) Stable oxygenation: PEEP/FiO2 not increased from last day; (i) Consistent patient triggered breath; (j) Withheld feeding for 2–4 hours; and (k, h) Richmond Agitation and Sedation Scale score measuring between −1 and +1.
The exclusion criteria included: (a) Use of any paralyzing agents in 24 hours before the study; (b) Diagnosis of diaphragm paralysis or paradoxical movement of hemidiaphragm detected on ultrasound; (c) Pregnant patients; (d) Ascites; (e) Age <18 years; (f) Post-thoracotomy; (g) Presence of pneumothorax; (h) Large pleural effusion, subcutaneous emphysema, flail chest, or rib fractures on the right side; and (i) Neuromuscular diseases.1
The clinical data regarding age of patients, acute physiologic and chronic health evaluation II (APACHE II) score, and simplified acute physiologic score (SAPS 2) score on the day of admission to the intensive care unit, total stay in ICU, and duration of mechanical ventilation were recorded. The decision to carry out the SBT, extubate the patient, or consider reinstitution of mechanical ventilation at the end or during the SBT was carried out by the treating physician.
The primary endpoint was the weaning outcome. Successful weaning is defined as when patients could be extubated and were clinically stable for more than 48 hours without any assisted ventilation. Weaning failure is determined if the patient's required restoration of mechanical ventilation under the following circumstances: (a) At the end or during the SBT; (b) Reintubation, or (c) NIV use within 48 hours of extubating.
Study Design
Spontaneous breathing trial was started with the patient in the 30–45° semi-recumbent position using pressure support after ventilation (PSV) mode, set an inspiratory pressure of 5 cm H2O and PEEP of 5 cm H2O. Ultrasonographic scanning of the right hemidiaphragm was carried out in the same posture after a time period of 30 minutes from the beginning of the SBT. Ultrasound scanning was performed earlier than 30 minutes if the patient showed any signs of SBT failure. Signs of SBT failure included the following: (a) Respiratory rate >35/minute; (b) Signs of intolerance – sweating or agitation; (c) Frequent periods of apnea for >15 seconds; (d) SpO2 <90% for >5 minutes; (e) Increase in PaCO2 >10 mm Hg from baseline; (f) pH <7.30; (g) Acute deterioration of mental status; and (h) Features of raised intracranial tension.
Diaphragmatic ultrasonography was performed by a single operator who was adequately trained in the procedure of intensive care ultrasonography. The curvilinear ultrasound probe of 3.5 MHz frequency was used for visualizing the diaphragm and then measuring the diaphragmatic displacement using both B and M modes. Additionally, the high-resolution linear probe of 10 MHz frequency was used for measuring the diaphragmatic thickness during both inspiration and expiration for calculating the diaphragmatic thickness fraction (DTF). The diaphragm could be seen thickening during inspiration due to muscle contraction.
The transducer was placed on the right side of the chest at the anterior subcostal location between the midclavicular line and anterior axillary line. The ultrasound beam would reach the posterior part of the diaphragm at an angle of not less than 70°. The displacement of the diaphragm was visualized when the diaphragm contracts and approaches anteriorly and inferiorly toward the ultrasound probe. This excursion or displacement of the right hemidiaphragm was measured using the M mode scanning as an upward motion. Five such measurements were recorded and averaged, and DD was recorded in millimeters. All measurements were recorded at 6–12 mL/kg during tidal breathing, excluding smaller or deeper breaths.
The following parameters were calculated during the SBT:
(a) Rapid shallow breathing index – RSBI; (b) Diaphragmatic displacement – DD; (c) Diaphragmatic thickness during inspiration and expiration; (d) Diaphragmatic thickness fraction – DTF; (e) Diaphragmatic rapid shallow breathing index – D-RSBI; and (f) Maximum inspiratory pressure – MIP.
The DTF was calculated as: [(Thickness of the diaphragm at end inspiration – Thickness at end-expiration) / Thickness of diaphragm at end expiration] × 100. The ventilatory parameters like TV, minute ventilation, RR, and maximum inspiratory pressure (MIP) were noted from the ventilator display and were recorded. RSBI was calculated as RR/TV (in liters). Diaphragmatic RSBI was calculated as RR/diaphragmatic displacement (in millimeters) and expressed as breath/minute/millimeter.
Patients who developed signs of SBT failure were immediately reconnected to the ventilator. Those who tolerated the SBT got extubated and liberated from a mechanical ventilator. These patients were then monitored closely for the next 48 hours in the ICU for any features of extubation failure.
Statistical Analysis
The statistical analysis was done using GraphPad Prism 8 (GraphPad Software, CA, USA). The Kolmogorov–Smirnov test was used to identify variables with a normal distribution. Data were reported as the mean ± standard deviation (SD) or median along with interquartile range (IQR) for continuous variables. Percentages in the form of frequencies (%) were used for categorical variables. Unpaired Student's t-tests or Mann–Whitney U tests were used as appropriate to compare the various continuous variables in the successful and unsuccessful weaning groups. Chi-square test or the Fisher exact test were used to asses differences in categorized variables. The correlation analysis was calculated using Pearson correlations (Pearson's R2 and p values).
The diagnostic accuracy of D-RSBI and RSBI was evaluated using ROC curves. The positive and negative predictive value (PPV and NPV, respectively), sensitivity, specificity, optimal cut-off point, and the accuracy were calculated for each ROC curve. For all statistical analyses, two-tailed tests were utilized, and p-values equal to or less than 0.05 were taken as statistically significant.
Results
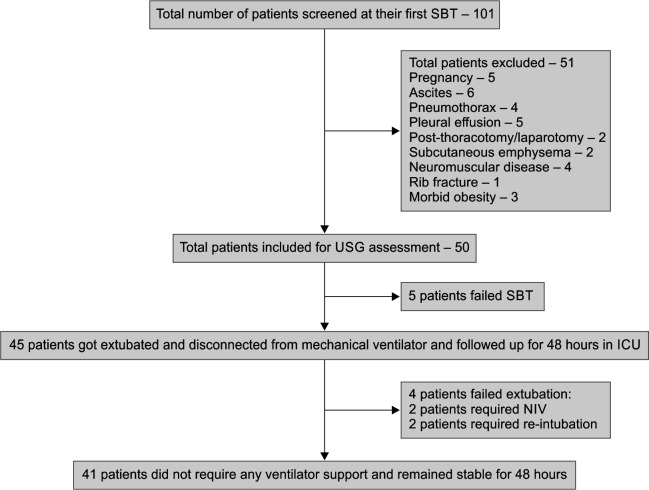
Fifty patients were included in the study after screening 101 consecutive patients (Flowchart 1). There were 29 (58%) male patients with at least one medical comorbid illness present in 58%; majority being diabetes mellitus (38%). The primary indication for ventilation in 27 patients (54%) was a hypercapnic respiratory failure arising in an acute exacerbation of chronic obstructive pulmonary disease, followed by acute respiratory distress syndrome (ARDS) in 11 patients; four hypoxemic respiratory failures due to multilobar pneumonia; three pulmonary edema due to cardiac origin; two massive hemoptysis; two depressed sensorium, and one pulmonary edema due to fluid overload secondary to renal insufficiency. After SBT, 41 were in the “Weaning success” group and nine in the “Weaning failure” group. The baseline clinical characteristics of age, APACHE II, and SAPS II score on the day of ICU admission, the total number of days of ICU stay, and the total duration of mechanical ventilation before the first SBT were not significantly different in the two outcomes groups (Table 1).
Flowchart 1.
Flow diagram of patients recruited in the study
Table 1.
Baseline characteristics of the patients in the outcome groups
| Variable | Success group | Failure group | p-value |
|---|---|---|---|
| Age (years) | 48.9 ± 15.4 | 54.1 ± 12.3 | 0.755 |
| APACHE II | 16.8 ± 5.8 | 17.6 ± 2.34 | 0.302 |
| SAPS | 35.2 ± 10 | 29.4 ± 5.31 | 0.142 |
| Total number of days in ICU | 5.07 ± 2.8 | 6.66 ± 8.2 | 0.834 |
| Total days of mechanical ventilation | 5.14 ± 3.23 | 6.55 ± 8.18 | 0.518 |
APACHE, acute physiologic and chronic health evaluation; ICU, intensive care unit; SAPS, simplified acute physiologic score
Comparison of Various Weaning Parameters among the Study Groups
The MIP, RSBI, DD, DTF, and D-RSBI were compared in the outcome groups, and the difference between the groups was statistically significant (Table 2). The MIP and DD values were statistically correlating with a Pearson's correlation coefficient of 0.65 and p-value <0.001 (Fig. 1). The DTF was 41.6% ± 4.5 in those who were successfully weaned-off when compared to 26.55% ± 4.27 in those who did not (p-value <0.001) (Table 2).
Table 2.
Comparison of various weaning parameters measured in the outcome groups
| Variable | Success group | Failure group | p-value |
|---|---|---|---|
| MIP (cm H2O) | 33.2 ± 5.8 | 22.8 ± 6.2 | <0.001 |
| RSBI | 52.11 ± 15.8 | 70.03 ± 25.4 | 0.008 |
| DD (mm) | 16.1 ± 3.3 | 7.8 ± 1.05 | <0.001 |
| D-RSBI | 1.24 ± 0.37 | 2.69 ± 0.98 | <0.001 |
| DTF | 41.6 ± 4.5 | 26.55 ± 4.27 | <0.001 |
DD, diaphragmatic displacement; DTF, diaphragmatic thickness fraction; D-RSBI, diaphragmatic rapid shallow breathing index; MIP, maximal inspiratory pressure; RSBI, rapid shallow breathing index
Fig. 1.
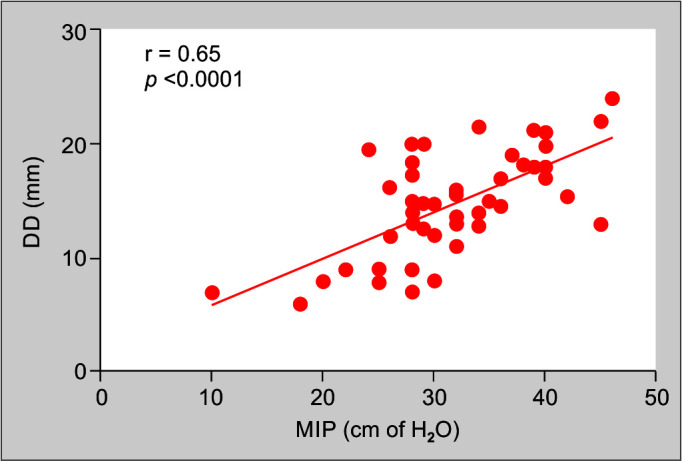
Shows correlation between maximal inspiratory pressure and diaphragmatic displacement. (DD, diaphragmatic displacement; MIP, maximal inspiratory pressure; r, Pearson's correlation coefficient)
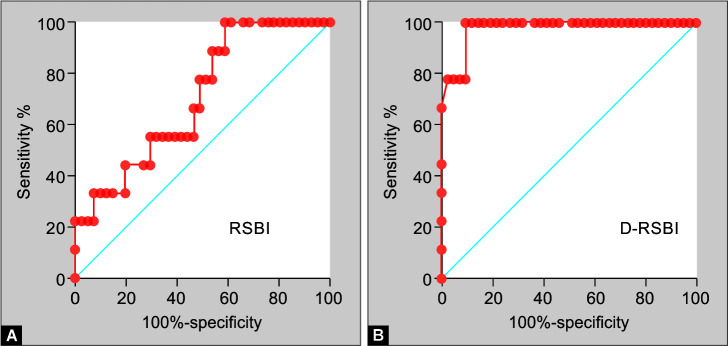
Rapid Shallow Breathing Index and Diaphragmatic RSBI
The RSBI and D-RSBI were differed significantly in the two outcome groups. The AUC for RSBI was 0.7073 with a standard error of 0.08754 (95% confidence interval: 0.5357–0.8789, p-value 0.0534), whereas for D-RSBI, the AUC was 0.977 with a standard error of 0.01853 (95% confidence interval: 0.9406–1.000, p-value <0.0001) which is better than RSBI (Fig. 2). At a cut-off of 1.767 breath/minute/millimeter, D-RSBI had a sensitivity, specificity, PPV, and NPV of 100%, 90.24%, 100%, and 69.23%, respectively (Table 3). The correlation between RSBI and D-RSBI with Pearson's correlation coefficient of 0.81 and p-value <0.001 (Fig. 3).
Figs 2A and B.
ROC curve showing larger area under the curve in case of D-RSBI compared to RSBI. (RSBI, rapid shallow breathing index; D-RSBI, diaphragmatic rapid shallow breathing index)
Table 3.
Comparison of diagnostic accuracy of RSBI and D-RSBI
| RSBI | D-RSBI | |
|---|---|---|
| Threshold | 45.72 | 1.767 |
| Sensitivity (95% confidence interval) | 40.5 (0.2–0.5) | 90.2 (0.7–0.9) |
| Specificity (95% confidence interval) | 100 (0.7–1) | 100 (0.7–1) |
| PPV | 100 | 100 |
| NPV | 26.5 | 69.2 |
| AUR (95% confidence interval) | 0.7 (0.5–0.8) | 0.97 (0.94–1) |
| p-value | 0.05 | <0.001 |
AUR, area under receiver operating characteristic curve; D-RSBI, diaphragmatic rapid shallow breathing index; NPV, negative predictive value; PPV, positive predictive value; RSBI, rapid shallow breathing index
Fig. 3.
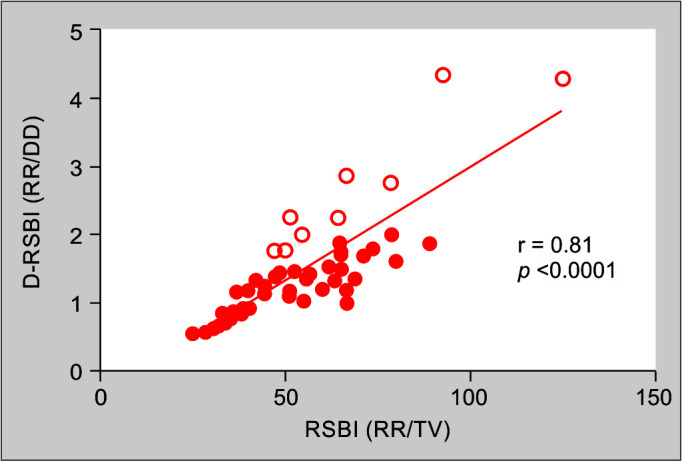
Shows the correlation between RSBI and D-RSBI. (RSBI, rapid shallow breathing index; D-RSBI, diaphragmatic rapid shallow breathing index; RR, respiratory rate; TV, tidal volume; r, Pearson's correlation coefficient)
Discussion
The incidence of weaning failure varies across different studies in the literature and is projected to be around 20%,10 and the weaning outcome in the present study is similar.
The utility of scoring systems at admission in predicting weaning outcomes has in the past shown varied results. Dehghani et al.11 reported the APACHE II score at admission and at first weaning predicted the result of the first weaning of patients from the ventilator. On the contrary, Rojek et al. in the retrospective analysis reported the failure of APACHE II to predict freedom from mechanical ventilation.12 The plausible explanation lies in the advancement and improvement in the management of critically ill patients on a ventilator that the outcome has improved irrespective of the initial severity of the disease as compared to earlier in the past. Other reasons may be related to the heterogeneity of the patients studied; that every scoring system is not universal for all the subjects; as well as differences in the study design. It is a well-known fact that as the length of stay in the ICU is an independent predictor of prolonged hospital stay, higher in-hospital mortality, and reduced long-term survival.13 But the direct relationship between the length of the ICU stay and the outcome of weaning from mechanical ventilators is largely unknown. Muzaffar et al., in multivariate analysis, did not find association of length of ICU stay or days on ventilator as independent predictor of weaning outome.14 The present study reports similar findings.
Maximal inspiratory pressure refers to the maximum pressure the patient can generate against an obstructed airway and it is a marker of inspiratory muscle strength; directly assesses the ability of the respiratory pump to generate and maintain adequate TV to sustain alveolar ventilation. Hence, MIP is one of the main factors of weaning success. Bien et al.15 reported the diagnostic accuracy of MIP in comparison to RSBI, sensitivity of 0.93, specificity of 0.95, positive predictive value of 0.98, negative predictive value of 0.79, and the diagnostic accuracy of 20.85. The current study did not perform comparison between MIP and any other weaning index.
Of all the weaning indices, the RSBI has gained widespread acceptance due to its simplicity and also because it does not require any measurement of complex pulmonary mechanics. It reflects respiratory muscle endurance. But unlike MIP, RSBI does not consider respiratory muscle strength while calculating it. Evidence suggests that a negative RSBI (RSBI ≥105 breaths/min/L) is better at identifying patients who will fail weaning than a positive RSBI (RSBI <105 breaths/min/L) is at identifying patients who can be successfully weaned. At this cut-off of 105 breaths/min/L, it has a positive predictive value, negative predictive value sensitivity, and specificity of 78, 95, 97, and 64%, respectively.16
However, studies that have tested the conventional cut-off of RSBI have suggested an alternative cut-off. A study by Danaga et al. observed that the conventional RSBI cut-off predicted only one-fifth of the patients who were ready for extubation as compared to a cut-off value of 76.5 breaths/min/L which led to an improved sensitivity (66%), with slight decrease in specificity (74%).17 Other studies have also documented a wide range of cut-offs for RSBI, which can be explained by the different study populations, objectives, methodologies, and outcome definitions used.18,19
Ultrasonography of the diaphragm has been evaluated to predict weaning success in multiple studies recently. The diaphragm gets atrophied as the number of days of critical illness and ventilator days increases. Therefore, tracking the diaphragmatic atrophy and diaphragm dysfunction by ultrasonography in patients planned for weaning and difficult to wean cases is an active area of ongoing research.
Diaphragmatic displacement is the measure of diaphragmatic movement or excursion during inspiration measured by ultrasound. Traditionally diaphragmatic excursion is measured on T-piece, however, a recent RCT has demonstrated that it can be accurately measured with low levels of pressure support as was done in the current study.13 Various cut-off values are described in the literature for the normal DD. Theerawit et al. observed that the cut-off value of 12.85 mm for diaphragmatic inspiratory excursion provided a specificity of 55% and a sensitivity of 83% for predicting re-intubation within 48 hours (120). The NPV and PPV of a diaphragmatic inspiratory excursion <12.85 mm were 97 and 17%, respectively. Llamas-Álvarez et al.,20 in a systematic review of 19 studies and 1071 patients, reported diaphragmatic excursion, pooled sensitivity, and specificity of 75%. In the present study, all the patients who had weaning failure had a DD of less than 10 mm.
In the current study, the DTF was an additional parameter and not the part of a research question. Pirompanich and Romsaiyut21 observed that at a cut-off value of DTF of more than or equal to 26%, had the highest sensitivity of 96.0%, specificity of 67.7%, PPV of 88.9%, NPV of 85.7%, and an accuracy of 88.2%. The combination of RSBI and right diaphragm thickening fraction significantly increased the accuracy for weaning success than RSBI alone. Pirompanich and Romsaiyut21 reported for diaphragm thickening fraction, the AUC was 0.87, and diagnostic odds ratio (DOR) was 21 (95% CI, 11–40). The present study also documented significant differences in DTF values among the success and failure groups.
Vivier et al.22 in an observational prospective multicentric study studied 191 at-risk of reintubation patients for over a 20-month period. Among these 191 patients, 33 (17%) were labeled as extubation failures. The proportion of patients who had diaphragmatic dysfunction using diaphragm excursion was similar between successful extubation (46%) and those in whom extubation failed (51%) (p = 0.55). For DTF also, there was no significant difference (71% vs 68%; p = 0.73). Spadaro et al.23 reported that while calculating RSBI, the accessory muscles use could compromise its diagnostic accuracy by masking the underlying diaphragmatic dysfunction. The hypothesis stated that since the accessory muscles are less efficient and get easily fatigued, their exhaustion will lead to an early weaning failure. Hence, the evaluation of diaphragmatic activity was more emphasized than accessory muscles. Thus, substituting the TV with DD in the RSBI, an index known as diaphragmatic RSBI (D-RSBI, RR/DD) was proposed. They compared D-RSBI to the traditional RSBI to predict weaning outcomes. The use of D-RSBI resulted in better diagnostic accuracy (AUROC = 0.89; p <0.0001). Using a cut-off of D-RSBI >1.3 breaths/min/mm yielded a 64.7% specificity, 94.1% sensitivity, 57.1% PPV, and 95.6% NPV. There was a significant correlation between D-RSBI and RSBI (R2 = 0.67; p-value <0.001). They concluded that D-RSBI (RR/DD) is more accurate than the traditional RSBI (RR/VT) with a cut-off of 1.3 having a high sensitivity and specificity.
Furthermore, in a population of COPD patients, Rojek-Jarmuła et al.12 reported a cut-off value of D-RSBI >1.9 breaths/min/mm, PPV, NPV, sensitivity, and specificity of 94.9%, 96%, 84.6%, and 100%, respectively; AUC for D-RSBI and RSBI were 0.97 (p <0.001) and 0.67 (p <0.06), respectively. Mowafy and Abdelgalel13 carried out a randomized trial in 106 mechanically ventilated ready-to-wean patients. The study reported superiority of D-RSBI to traditional RSBI in predicting weaning outcomes with a cut-off value of D-RSBI <1.6 breaths/min/mm monitored at 30 min; yielded sensitivity, specificity, PPV, and NPV of 97.3%, 93.9%, 97.1%, and 93.2%, respectively.
In India, a study in Jharkhand found the speed of diaphragm contraction comparable to RSBI to predict weaning.24 Integrative weaning index has also been tried across the world with the assumption that respiratory physiology parameters including compliance in the index will have a superior but has limited evidence till date.25,26
In our study, the diagnostic accuracy of D-RSBI to predict weaning outcomes was higher for D-RSBI than for RSBI. The sensitivity was increased from 40 to 90% while maintaining the specificity. Thus, demonstrating the increased negative predictive value and diagnostic accuracy of D-RSBI over the RSBI in predicting successful weaning outcomes.
Limitations
It was a single-center study and limited sample size. The correlation between DTF and D-RSBI was not done in the present study. The present study included a heterogeneous patient population, and the pathology of diaphragmatic dysfunction may be different in the different disease states. Hence, the performance of D-RSBI has to be studied separately in individual disease types.
Conclusion
Diaphragmatic rapid shallow breathing index is a novel, ultrasonography-based, noninvasive, and simple bedside predictive tool for weaning guiding intensivists during weaning from mechanical ventilation.
Orcid
Shamil PK https://orcid.org/0000-0002-3326-9976
NK Gupta https://orcid.org/0000-0002-3557-8238
Pranav Ish https://orcid.org/0000-0003-1701-4970
MK Sen https://orcid.org/0000-0002-2681-0381
Rohit Kumar https://orcid.org/0000-0001-6398-7840
Shibdas Chakrabarti https://orcid.org/0000-0002-6334-974X
Nitesh Gupta https://orcid.org/0000-0002-5842-5584
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Schmidt GA, Girard TD, Kress JP, Morris PE, Ouellette DR, Alhazzani W, et al. Liberation from mechanical ventilation in critically ill adults: Executive summary of an Official American College of Chest Physicians/American Thoracic Society Clinical Practice Guideline. Chest. 2017;151(1):160–165. doi: 10.1016/j.chest.2016.10.037. [DOI] [PubMed] [Google Scholar]
- 2.Ghauri SK, Javaeed A, Mustafa KJ, Khan AS. Predictors of prolonged mechanical ventilation in patients admitted to intensive care units: A systematic review. Int J Health Sci (Qassim) 2019;13(6):31–38. PMC6852505 [PMC free article] [PubMed] [Google Scholar]
- 3.Doorduin J, van Hees HW, van der Hoeven JG, Heunks LM. Monitoring of the respiratory muscles in the critically ill. Am J Respir Crit Care Med. 2013;187(1):20–27. doi: 10.1164/rccm.201206-1117CP. [DOI] [PubMed] [Google Scholar]
- 4.Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by M-mode ultrasonography. Chest. 2009;135(2):391–400. doi: 10.1378/chest.08-1541. [DOI] [PubMed] [Google Scholar]
- 5.Kim WY, Suh HJ, Hong SB, Koh Y, Lim CM. Diaphragm dysfunction assessed by ultrasonography: Influence on weaning from mechanical ventilation. Crit Care Med. 2011;39(12):2627–2630. doi: 10.1097/CCM.0b013e3182266408. [DOI] [PubMed] [Google Scholar]
- 6.Farghaly S, Hasan AA. Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients. Aust Crit Care. 2017;30(1):37–43. doi: 10.1016/j.aucc.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 7.Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med. 1991;324(21):1445–1450. doi: 10.1056/NEJM199105233242101. [DOI] [PubMed] [Google Scholar]
- 8.Lee KH, Hui KP, Chan TB, Tan WC, Lim TK. Rapid shallow breathing (frequency tidal volume ratio) did not predict extubation outcome. Chest. 1994;105(2):540–543. doi: 10.1378/chest.105.2.540. [DOI] [PubMed] [Google Scholar]
- 9.Savi A, Teixeira C, Silva JM, Borges LG, Pereira PA, Pinto KB, et al. Weaning predictors do not predict extubation failure in simple-to-wean patients. J Crit Care. 2012;27(2):221.e1–221.e8. doi: 10.1016/j.jcrc.2011.07.079. [DOI] [PubMed] [Google Scholar]
- 10.Shin HJ, Chang JS, Ahn S, Kim TO, Park CK, Lim JH, et al. Clinical factors associated with weaning failure in patients requiring prolonged mechanical ventilation. J Thorac Dis. 2017;9(1):143–150. doi: 10.21037/jtd.2017.01.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dehghani A, Davaridolatabadi E, Abdeyazdan G. Comparison of SOFA and APACHE II scores in predicting weaning of patients from ventilator in the ICU ward of Amin Hospital in Isfahan, Iran. J Med Res Health Sci. 2016;5(9S):128–136. [Google Scholar]
- 12.Rojek-Jarmuła A, Hombach R, Krzych ŁJ. APACHE II score cannot predict successful weaning from prolonged mechanical ventilation. Chron Respir Dis. 2017;14(3):270–275. doi: 10.1177/1479972316687100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mowafy SMS, Abdelgalel EF. Diaphragmatic rapid shallow breathing index for predicting weaning outcome from mechanical ventilation: comparison with traditional rapid shallow breathing index. Egyptian J Anaesth. 2018;35(1):9–17. doi: 10.1016/j.egja.2018.10.003. [DOI] [Google Scholar]
- 14.Muzaffar SN, Gurjar M, Baronia AK, et al. Predictors and pattern of weaning and long-term outcome of patients with prolonged mechanical ventilation at an acute intensive care unit in North India. Rev Bras Ter Intensiva. 2017;29(1):23–33. doi: 10.5935/0103-507X.20170005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bien U dos S, Souza GF, Campos ES, et al. Maximum inspiratory pressure and rapid shallow breathing index as predictors of successful ventilator weaning. J Phys Ther Sci. 2015;27(12):3723–3727. doi: 10.1589/jpts.27.3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karthika M, Al Enezi FA, Pillai LV, Arabi YM. Rapid shallow breathing index. Ann Thorac Med. 2016;11(3):167–176. doi: 10.4103/1817-1737.176876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Danaga AR, Gut AL, Antunes LC, Ferreira AL, Yamaguti FA, Christovan JC, et al. Evaluation of the diagnostic performance and cut-off value for the rapid shallow breathing index in predicting extubation failure. J Bras Pneumol. 2009;35(6):541–547. doi: 10.1590/s1806-37132009000600007. [DOI] [PubMed] [Google Scholar]
- 18.Vallverdu I, Calaf N, Subirana M, Net A, Benito S, Mancebo J. Clinical characteristics, respiratory functional parameters, and outcome of a two hour T-piece trial in patients weaning from mechanical ventilation. Am J Respir Crit Care Med. 1998;158(6):1855–1862. doi: 10.1164/ajrccm.158.6.9712135. [DOI] [PubMed] [Google Scholar]
- 19.Yan S, Lichros I, Zakynthinos S, Macklem PT. Effect of diaphragmatic fatigue on control of respiratory muscles and ventilation during CO2 rebreathing. J Appl Physiol. 1993;75(3):1364–1370. doi: 10.1152/jappl.1993.75.3.1364. [DOI] [PubMed] [Google Scholar]
- 20.Llamas-Álvarez AM, Tenza-Lozano EM, Latour-Pérez J. Diaphragm and lung ultrasound to predict weaning outcome: Systematic review and meta-analysis. Chest. 2017;152(6):1140–1150. doi: 10.1016/j.chest.2017.08.028. [DOI] [PubMed] [Google Scholar]
- 21.Pirompanich P, Romsaiyut S. Correction to: Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients. J Intensive Care. 2018;6:25. doi: 10.1186/s40560-018-0293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vivier E, Muller M, Putegnat JB, Steyer J, Barrau S, Boissier F, et al. Inability of diaphragm ultrasound to predict extubation failure: A multicenter study. Chest. 2019;155(6):1131–1139. doi: 10.1016/j.chest.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 23.Spadaro S, Grasso S, Mauri T, Corte FD, Alvisi V, Ragazzi R, et al. Can diaphragmatic ultrasonography performed during the T-tube trial predict weaning failure? The role of diaphragmatic rapid shallow breathing index. Crit Care. 2016;20(1):305. doi: 10.1186/s13054-016-1479-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Banerjee A, Mehrotra G. Comparison of lung ultrasound-based weaning indices with rapid shallow breathing index: Are they helpful? Indian J Crit Care Med. 2018;22(6):435–440. doi: 10.4103/ijccm.IJCCM_331_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El-Baradey GF, El-Shmaa NS, Ganna SA. Can integrative weaning index be a routine predictor for weaning success? Indian J Crit Care Med. 2015;19(12):703–707. doi: 10.4103/0972-5229.171352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ray A. Integrative weaning index: A few observations. Indian J Crit Care Med. 2017;21(11):805–806. doi: 10.4103/0972-5229.218154. [DOI] [PMC free article] [PubMed] [Google Scholar]