Abstract
Objectives:
To assess changes in weight-related health behaviors and social determinants of health (SDoH) among youth with overweight/obesity during the coronavirus disease 2019 (COVID-19) pandemic.
Methods:
We assessed weight-related health behaviors (physical activity, screen time, sleep, and diet) and SDoH (food insecurity, income/childcare, and caregivers' perceived stress) before vs. during the pandemic with a survey administered August–October 2020 to caregivers of 2–17-year olds and adolescents 13–17 years old with BMI ≥85th percentile seen in clinic within 6 months prepandemic. We analyzed changes in continuous variables using paired t-tests and categorical variables with McNemar's or Fisher's exact tests, and the influence of social determinants on behavior change using multivariable regression models.
Results:
A total of 129 caregivers and 34 adolescents completed surveys. Compared with prepandemic, caregivers reported youth decreased moderate/vigorous physical activity (−87.4 [205.7] minutes/week, p < 0.001) and increased recreational screen time (2.5 [2.1] hours/day, p < 0.001). Fewer had regular bedtimes (before: 89% and during: 44%, p < 0.001) and more ate most meals with television (before: 16% and during: 36%, p < 0.001). Food insecurity increased from 27% to 43% (p < 0.001), 45% reported reduced household income, and caregivers with moderate/high perceived stress scale scores increased from 43% to 64% (p < 0.001). Moderate/high caregiver stress and food insecurity were associated with greater magnitudes of adverse behavior change.
Conclusion:
Alarming changes in health behaviors among youth with overweight/obesity, particularly among those with stressed caregivers and food insecurity, may increase prevalence of obesity-related comorbidities and exacerbate health disparities. There is an urgent need to expand access to effective interventions for overweight/obesity that address psychosocial stressors.
Keywords: COVID-19 pandemic, obesity, physical activity, screen time, sleep, social determinants of health
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is causing unprecedented disruptions worldwide not only from significant morbidity and mortality from the virus itself but also through economic instability, school closures, and increased stress on families.1 At the same time, the prevalence of obesity continues to rise with a recent national study finding an increase in obesity among youth ages 2–19 years in the United States from 19.3% in 2019 to 22.4% in 2020, as well as a two-fold higher rate of BMI increase during vs. before the pandemic.2,3 Children's daily lives changed drastically due to the pandemic, and there is emerging evidence of negative effects on health behaviors associated with obesity risk and worse cardiometabolic outcomes.4–6
The pandemic may affect some youth and their families more severely due to job loss, food insecurity, loss of schools as the “great equalizer,” and other social determinants of health (SDoH). One recent study among children in Philadelphia suggests a widening of persistent socioeconomic, racial, and ethnic disparities in childhood obesity.7–9
In the United States, studies have found parent-reported declines in physical activity, particularly among those with severe obesity, as well as an increase in snacking and sedentary behaviors.10,11 Data from other countries, including Canada, the Netherlands, China, and Spain, report declines in parent-reported physical activity and higher levels of screen time, with one study from the Netherlands using accelerometry to demonstrate nearly 1 hour/day less physical activity during the pandemic.5,12–14 Studies have separately described adverse changes in well-being, food insecurity, and income loss across different communities, but little is known about the association between these SDoH and health behavior change during the pandemic.
In this study, we sought to examine the extent to which health behaviors of youth with overweight/obesity changed during the first 6 months of the pandemic compared with prepandemic. In exploratory analyses, we evaluated the extent to which SDoH (food insecurity, caregiver stress, income change, and childcare) and demographic characteristics (age and race/ethnicity) modified those behavior changes. Understanding behavior changes affecting youth with overweight/obesity, as well as potential modifiers of these changes, can inform the tailoring of interventions to mitigate the adverse effects of the pandemic on youth and families.
Methods
Study Population
Caregivers of youth 2–17 years old with overweight/obesity (BMI ≥85th percentile), seen September 2019–March 2020 in the Yale Pediatric Primary Care or Endocrinology Clinics, were invited to participate through email. Adolescents 13–17 years old were invited if their caregivers completed the survey and provided their email address to participate. We invited one randomly selected child per household and excluded those without English listed as primary language in the electronic health record (EHR). To limit confounding effects of complex chronic conditions (CCC) on health behaviors and obesity, we identified and excluded children with CCC, including diabetes, defined using the Pediatric Medical Complexity Algorithm and pediatric CCC classification system using EHR problem list and visit diagnosis codes.15,16 All participants received a small incentive (gift card) following survey completion. Yale University's Institutional Review Board approved all protocols.
Survey Design
Study data were collected and managed using REDCap (Research electronic data capture) tools hosted at Yale University. REDCap is a secure, web-based software platform designed to support data capture for research studies.17
The survey assessed health behaviors associated with pediatric obesity (physical activity, screen time, sleep, and dietary habits), as well as relevant SDoH, including food insecurity, changes in income/childcare, perceived stress levels, and race/ethnicity. Caregivers reported on their children's health behaviors, while adolescents reported their own health behaviors. Questions were asked in duplicate to address the prepandemic and during-pandemic periods. The prepandemic period was defined as “the time ‘before COVID-19 school closures' considered to be a typical month, e.g., February 2020 when you/your child was going to school.” Three versions of the survey were developed for the following groups: caregivers of children (2–12 years old), caregivers of adolescents (13–17 years old), and adolescents (13–17 years old). The survey for caregivers of 2–12-year olds included questions regarding childcare. Adolescents were not asked clinical information or questions pertaining to food insecurity and income.
Recruitment
The recruitment period was mid-August to mid-October 2020—approximately 6 months after Connecticut initiated school closures (March 15, 2020) and a state-wide shut down (March 20, 2020). These restrictions were lifted during the summer as community spread declined. School re-openings varied throughout the state with two districts being fully remote in the fall of 2020, including New Haven, and nearly 60% using the hybrid model.18
Measures
Anthropometric data
We extracted height and weight from the EHR and calculated BMI and BMI percentiles using sex- and age-based CDC SAS code.19 Measurements were from the most recent clinic visit between September 2019 and March 2020. We defined overweight as age- and sex-adjusted BMI percentile ≥85 to <95th percentile, and obesity as BMI percentile ≥95. We defined Class 1 obesity as BMI between the 95th percentile and 119% of the 95th percentile, Class 2 obesity as BMI between 120% and 139% of the 95th percentile, and Class 3 obesity as BMI ≥140% of the 95th percentile.20 We utilized BMI expressed as percentage of the 95th percentile (%BMIp95) based on limitations of BMI z-score for children with severe obesity.21
Weight-related behaviors, SDoH, and demographic characteristics
We adapted the Primary Caregivers Questionnaire22 to assess number of days and amount of time spent walking/engaging in moderate/vigorous physical activity (MVPA) during the past 7 days and in the prepandemic period. Screen time was measured using a question from the 2019 to 2020 National Health and Nutrition Examination Survey (NHANES) and was divided into recreational and school related.23 We assessed sleep duration and daytime sleepiness using questions from NHANES 2019–20 and sleep quality with the validated Patient-Reported Outcomes Measurement Information System (PROMIS) sleep disturbance scale short form.24 A t-score ≥66 indicated severe sleep disturbance and was representative of ≥95th percentile for disturbed sleep.25 We assessed dietary changes using questions adapted from a questionnaire used in the Bright Bodies weight management program, NHANES 2019–20, and the validated sugar-sweetened beverage (SSB) screener questionnaire.26,27 We adapted questions to inquire about the time before and since the COVID-19 school closures.
We used the Hunger Vital Sign to assess household food insecurity,28 the Perceived Stress Scale (PSS) for caregiver/adolescent stress,29 and a question from NHANES 2019–20 for caregiver education level. We also questioned caregivers about income and childcare changes associated with the pandemic and extracted children's age and race/ethnicity from the EHR. Supplementary Table S1 details questions and sources utilized.
Statistical Methods
Demographics and sample characteristics were summarized with mean and standard deviation (SD) for continuous variables and frequency and percent for categorical variables. Changes in health behaviors and SDoH were analyzed with paired t-tests for continuous variables, McNemar's paired test for dichotomous variables, and Fisher's exact test for variables with >2 categories.
Linear regression models were used to assess change in continuous variables: physical activity, recreational screen time, sleep duration, intake of sugary beverages (SSB and fruit juice), fruits/vegetables, and chips/foods with added sugar. We also utilized generalized estimating equations to assess the pandemic's impact on binary outcomes: having a regular bedtime, sleep disturbance, and meals with television. Effect modification by SDoH was assessed in separate models, including age (continuous), race/ethnicity (non-Hispanic white vs. other), baseline %BMIp95 (overweight/class 1 obesity vs. class 2/3 obesity), food insecurity status during pandemic, caregiver PSS score during pandemic (moderate/high ≥14 vs. low <14), and changes in childcare and income during vs. prepandemic (decrease vs. increase/no change). The moderation models for continuous variables and for meals with television were adjusted for age, sex, and %BMIp95 before the pandemic.
For other categorical outcomes, the adjusted models failed to converge due to small events by covariates; thus, only results of unadjusted analysis are reported. All statistical analyses were performed using SAS/STAT® Software, version 9.4 (SAS Institute, Inc., Cary, NC). For the primary aim of assessing during-pandemic changes, we used p = 0.001 as the significance cutoff to account for multiple comparisons. Other analyses were exploratory and not interpreted in a confirmatory manner.
Results
Among 1367 caregivers of eligible children and adolescents invited to participate in the study, 129 caregivers (9.4%) completed the survey. Of 48 caregivers of adolescents who gave consent for recruitment, 34 adolescents (71%) responded. The nonresponding caregivers did not significantly differ from responders by youths' age, sex, or %BMIp95, but did differ by race/ethnicity (p < 0.001)—responders had a higher proportion of non-Hispanic white children (36% vs. 17%) than nonresponders (Supplementary Table S2).
Youth in our sample had a mean age of 11 years, a slight female predominance, 32% had severe obesity, 57% had public insurance, 30% were non-Hispanic black, and 30% were Hispanic (Table 1).
Table 1.
Baseline Characteristics of Participants by Caregiver-Proxy Report
| Total caregiver-proxy (n = 129) Mean (SD) or n (%) | Children 2–12 years (n = 78) Mean (SD) or n (%) | Adolescents 13–17 years (n = 51) Mean (SD) or n (%) | |
|---|---|---|---|
| Child/adolescent characteristicsa | |||
| Age, years | 10.9 (4.3) | 8.0 (2.9) | 15.2 (1.5) |
| Sex, female | 77 (60%) | 48 (62%) | 29 (57%) |
| %BMIp95 | 113.3 (20.4) | 109.0 (18.5) | 119.9 (21.6) |
| Obesity class | |||
| Overweight | 49 (38%) | 37 (47%) | 12 (24%) |
| Class 1 | 39 (30%) | 22 (28%) | 17 (33%) |
| Class 2 | 26 (20%) | 13 (17%) | 13 (26%) |
| Class 3 | 15 (12%) | 6 (8%) | 9 (18%) |
| Race/ethnicity | |||
| Hispanic | 38 (30%) | 26 (33%) | 12 (24%) |
| Non-Hispanic white | 46 (36%) | 23 (30%) | 23 (45%) |
| Non-Hispanic black | 38 (30%) | 27 (35%) | 11 (22%) |
| Non-Hispanic multiracial | 4 (3%) | 1 (1%) | 3 (6%) |
| Other/unknown | 3 (2%) | 1 (1%) | 2 (4%) |
| Insurance type | |||
| Medicaid | 73 (57%) | 51 (65%) | 22 (43%) |
| Private | 47 (36%) | 23 (30%) | 24 (47%) |
| Other/unknown | 9 (7%) | 4 (5%) | 5 (10%) |
| Household characteristics | |||
| Household size, number of people | 4.1 (1.5) | 4.2 (1.6) | 4.1 (1.3) |
| <18 years old | 2.3 (1.2) | 2.4 (1.3) | 2.1 (1.2) |
| Adults | 2.0 (0.8) | 1.9 (0.9) | 2.2 (0.7) |
| Had access to an outdoor space for physical activity | 107 (83%) | 65 (83%) | 42 (82%) |
| Had at least one confirmed COVID case in the household | 12 (9%) | 7 (9%) | 5 (10%) |
| Caregiver characteristics | |||
| Caregivers' education level | |||
| Some high school or less | 7 (5%) | 4 (5%) | 3 (6%) |
| High school graduate | 23 (18%) | 13 (17%) | 10 (20%) |
| Some college or more | 99 (77%) | 61 (78%) | 38 (74%) |
| Caregiver BMI | 32.7 (7.1) | 32.8 (7.3) | 32.7 (6.9) |
| Caregiver BMI ≥30 kg/m2 | 79 (61%) | 47 (60%) | 32 (63%) |
| Caregiver partner BMI | 32.5 (6.4) | 33.9 (6.7) | 30.7 (5.6) |
| Caregiver partner BMI ≥30 kg/m2 | 42 (33%) | 28 (36%) | 14 (28%) |
| Marital status | |||
| Not living with a partner | 57 (44%) | 37 (47%) | 20 (39%) |
| Unmarried, living with a partner | 13 (10%) | 9 (12%) | 4 (8%) |
| Married, living with a partner | 59 (46%) | 32 (41%) | 27 (53%) |
Data extracted from EHR.
%BMIp95, percent BMI of the 95th percentile; COVID, coronavirus disease; HER, electronic health record; SD, standard deviation.
Health Behaviors
Prepandemic to during-pandemic changes in health behaviors by caregiver-proxy report are summarized in Table 2. Caregivers reported a mean (SD) reduction of 87.4 (205.7) minutes/week in youths' MVPA (p < 0.001) and 109.7 (255.9) minutes/week in walking time (p < 0.001). School and recreational screen time increased by 2.2 (2.3) and 2.5 (2.1) hours/day, respectively (p < 0.001). The proportion with a regular bedtime decreased from 89% to 44% (p < 0.001). Compared with prepandemic, severe sleep disturbance increased (10% to 29%, p < 0.001). Caregivers reported youth consumed an additional two servings/week of chips/foods with added sugars (p < 0.001) and sugary beverages (p = 0.001), but no significant change in combined fruit/vegetable intake. In addition, more youth watched television with most meals (16% to 36%, p < 0.001) and more families ate 2–3 meals together daily (42% to 57%, p < 0.001).
Table 2.
Changes in Caregiver-Reported Health Behaviors during Pandemic in Youth with Overweight/Obesity
| |
Total caregiver-proxy (n = 129) Mean (SD) or n (%) |
Children 2–12 years (n = 78) Mean (SD) or n (%) |
Adolescents 13–17 years (n = 51) Mean (SD) or n (%) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Health behaviors | Prepandemic | During | Change | p-value | Prepandemic | During | Change | p-value | Prepandemic | During | Change | p-value |
| Physical activity, minutes per week | ||||||||||||
| Walking time | 248.5 (305.1) | 138.8 (184.3) | −109.7 (255.9) | <0.001 | 230.6 (283.5) | 129.8 (145.9) | −100.7 (254.4) | <0.001 | 275.9 (336.6) | 152.5 (232.2) | −123.3 (260.1) | 0.001 |
| Moderate/vigorous physical activity | 213.7 (232.4) | 126.3 (177.4) | −87.4 (205.6) | <0.001 | 208.1 (208.3) | 124.0 (153.4) | −84.1 (211.3) | <0.001 | 222.4 (267.1) | 129.7 (210.5) | −92.6 (198.7) | 0.002 |
| Screen time, hours per day | ||||||||||||
| Recreational screen time | 2.0 (1.5) | 4.4 (2.6) | 2.5 (2.1) | <0.001 | 1.5 (1.0) | 3.9 (2.3) | 2.5 (1.9) | <0.001 | 2.7 (1.9) | 5.1 (2.8) | 2.4 (2.5) | <0.001 |
| School related screen time | 1.3 (1.3) | 3.5 (2.3) | 2.2 (2.3) | <0.001 | 0.9 (1.0) | 2.9 (2.2) | 2.0 (2.3) | <0.001 | 1.9 (1.4) | 4.3 (2.3) | 2.4 (2.4) | <0.001 |
| Sleep | ||||||||||||
| Regular bedtime, n (%) | 115 (89%) | 57 (44%) | −58 (−45%) | <0.001 | 74 (95%) | 42 (54%) | −32 (−41%) | <0.001 | 41 (80%) | 15 (29%) | −26 (−51%) | <0.001 |
| Sleep duration, hours/night | 9.1 (1.6) | 9.0 (2.0) | −0.2 (2.1) | 0.41 | 9.8 (1.2) | 9.2 (1.6) | −0.6 (1.6) | 0.003 | 8.0 (1.7) | 8.5 (2.3) | 0.5 (2.5) | 0.16 |
| Daytime sleepiness, n = 122 | ||||||||||||
| Never/rarely/sometimes | 102 (84%) | 95 (78%) | 7 (6%) | 0.18 | 69 (92%) | 66 (88%) | −3 (−4%) | 0.32 | 33 (70%) | 29 (62%) | −4 (−9%) | 0.35 |
| Often/almost always | 20 (16%) | 27 (22%) | −7 (−6%) | 6 (8%) | 9 (12%) | 3 (4%) | 14 (30%) | 18 (38%) | 4 (9%) | |||
| Sleep disturbance scale, t-score ≥66, yes | 10 (8%) | 29 (23%) | 19 (15%) | <0.001 | 4 (5%) | 17 (22%) | 13 (17%) | <0.001 | 6 (12%) | 12 (24%) | 6 (12%) | 0.03 |
| Diet/nutrition | ||||||||||||
| Sugar-sweetened beverage intake, servings/day | 0.6 (0.9) | 0.8 (1.0) | 0.2 (0.7) | 0.009 | 0.8 (0.9) | 0.9 (1.1) | 0.2 (0.6) | 0.04 | 0.5 (0.8) | 0.6 (1.0) | 0.2 (0.7) | 0.12 |
| Fruit juice, servings/day | 0.8 (1.1) | 1.0 (1.3) | 0.2 (0.7) | 0.005 | 1.0 (1.2) | 1.2 (1.4) | 0.2 (0.6) | 0.03 | 0.5 (0.7) | 0.6 (1.1) | 0.2 (0.7) | 0.08 |
| Fruit | 1.2 (1.0) | 1.3 (1.1) | 0.1 (0.8) | 0.22 | 1.5 (1.1) | 1.6 (1.2) | 0.1 (0.9) | 0.24 | 0.8 (0.7) | 0.8 (0.8) | 0.0 (0.6) | 0.71 |
| Vegetables | 1.1 (0.9) | 1.2 (1.0) | 0.1 (0.7) | 0.20 | 1.1 (1.0) | 1.2 (1.0) | 0.1 (0.7) | 0.52 | 1.0 (0.9) | 1.1 (1.0) | 0.1 (0.7) | 0.22 |
| Chips | 0.5 (0.5) | 0.7 (0.8) | 0.2 (0.5) | <0.001 | 0.6 (0.6) | 0.7 (0.8) | 0.2 (0.5) | 0.005 | 0.5 (0.4) | 0.6 (0.7) | 0.2 (0.6) | 0.05 |
| Food with added sugars | 0.5 (0.5) | 0.7 (0.7) | 0.2 (0.6) | 0.004 | 0.6 (0.6) | 0.8 (0.8) | 0.2 (0.7) | 0.006 | 0.4 (0.3) | 0.5 (0.4) | 0.0 (0.4) | 0.36 |
| Location of meals | ||||||||||||
| Bedroom | 10 (8%) | 20 (16%) | 10 (8%) | 0.02 | 3 (4%) | 12 (15%) | 9 (12%) | 0.007 | 7 (14%) | 8 (16%) | 1 (2%) | 0.71 |
| Living room/den/kitchen/dining room | 119 (92%) | 109 (85%) | −10 (−8%) | 75 (96%) | 66 (85%) | −9 (−12%) | 44 (86%) | 43 (84%) | −1 (−2%) | |||
| Television with meals | ||||||||||||
| Most of the time | 20 (16%) | 46 (36%) | 26 (20%) | <0.001 | 13 (17%) | 28 (36%) | 15 (19%) | <0.001 | 7 (14%) | 18 (35%) | 11 (22%) | 0.002 |
| Sometimes/Rarely/Never | 109 (85%) | 83 (64%) | −26 (−20%) | 65 (83%) | 50 (64%) | −15 (−19%) | 44 (86%) | 33 (65%) | −11 (−22%) | |||
| Meals with family | ||||||||||||
| None | 13 (10%) | 15 (12%) | 2 (2%) | <0.001 | 4 (5%) | 7 (9%) | 3 (4%) | <0.001 | 9 (18%) | 8 (16%) | −1 (−2%) | <0.001 |
| Once | 62 (48%) | 40 (31%) | −22 (−17%) | 33 (42%) | 21 (27%) | −12 (−15%) | 29 (57%) | 19 (37%) | −10 (−20%) | |||
| Two to three times | 54 (42%) | 74 (57%) | 20 (16%) | 41 (53%) | 50 (64%) | 9 (12%) | 13 (26%) | 24 (47%) | 11 (22%) | |||
| Food intake after dinner | ||||||||||||
| 0%–50% | 105 (81%) | 102 (79%) | −3 (−2%) | 0.26 | 61 (78%) | 61 (78%) | 0 (0%) | 1.00 | 44 (86%) | 41 (80%) | −3 (−6%) | 0.18 |
| 51%–100% | 24 (19%) | 27 (21%) | 3 (2%) | 17 (22%) | 17 (22%) | 0 (0%) | 7 (14%) | 10 (20%) | 3 (6%) | |||
Adolescents' self-reported outcomes were in general consistent with caregivers' proxy-reports with decreased frequency of regular bedtime (before: 79% and during: 24%, p < 0.001, p-value of comparison = 0.80) and more often having 2–3 meals daily with family (before: 24% and during: 32%, p < 0.001, p-value of comparison = 0.95). Adolescents reported a smaller degree of increased screen time than their caregivers (adolescents 2.0 [2.5] hours/day vs. caregiver-proxy 2.8 [1.9] hours/day, p-value of comparison = 0.003). Although there was no change in reported sleep disturbance, 18% of adolescents reported severe sleep disturbance both before and during pandemic (Supplementary Table S3).
Social Determinants of Health
Changes in SDoH from prepandemic to during pandemic are summarized in Table 3. Food insecurity increased from 27% to 43% (p < 0.001) and 45% reported reduced household income. The percent of caregivers with moderate/high PSS scores increased from 43% to 64% (p < 0.001); while 65% of adolescents reported prepandemic PSS scores in the moderate/high range, this did not increase significantly.
Table 3.
Changes in the Social Determinants of Health of Youth with Overweight/Obesity during Pandemic by Caregiver Report
| |
Total caregiver-proxy (n = 129) n (%) |
Children 2–12 years (n = 78) n (%) |
Adolescents 13–17 years (n = 51) n (%) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SDoH | Pre | During | Change | p-value | Pre | During | Change | p-value | Pre | During | Change | p-value |
| Moderate/High Parent PSS Score (≥14) | 55 (43%) | 83 (64%) | 28 (22%) | <0.001 | 28 (36%) | 38 (62%) | 20 (26%) | <0.001 | 27 (53%) | 35 (69%) | 8 (16%) | 0.03 |
| Food insecurity | 35 (27%) | 55 (43%) | 20 (16%) | <0.001 | 20 (26%) | 34 (44%) | 14 (18%) | <0.001 | 15 (29%) | 21 (41%) | 6 (12%) | 0.01 |
| Reduced income | 58 (45%) | 41 (53%) | 17 (33%) | |||||||||
| Any childcare | 58 (74%) | 35 (45%) | −13 (−30%) | <0.001 | ||||||||
| Reduced childcare hours | 36 (46%) | |||||||||||
PSS, Perceived Stress Scale; SDoH, social determinants of health.
Association between SDoH and Behavior Changes
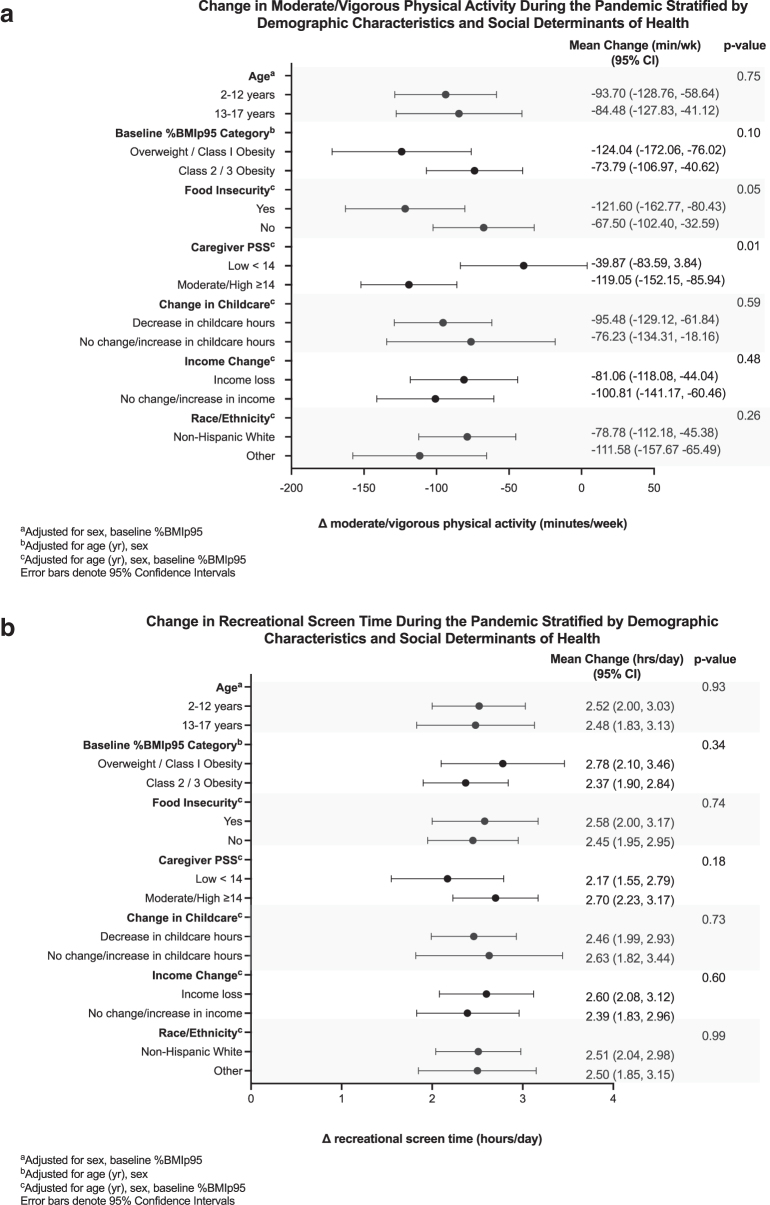
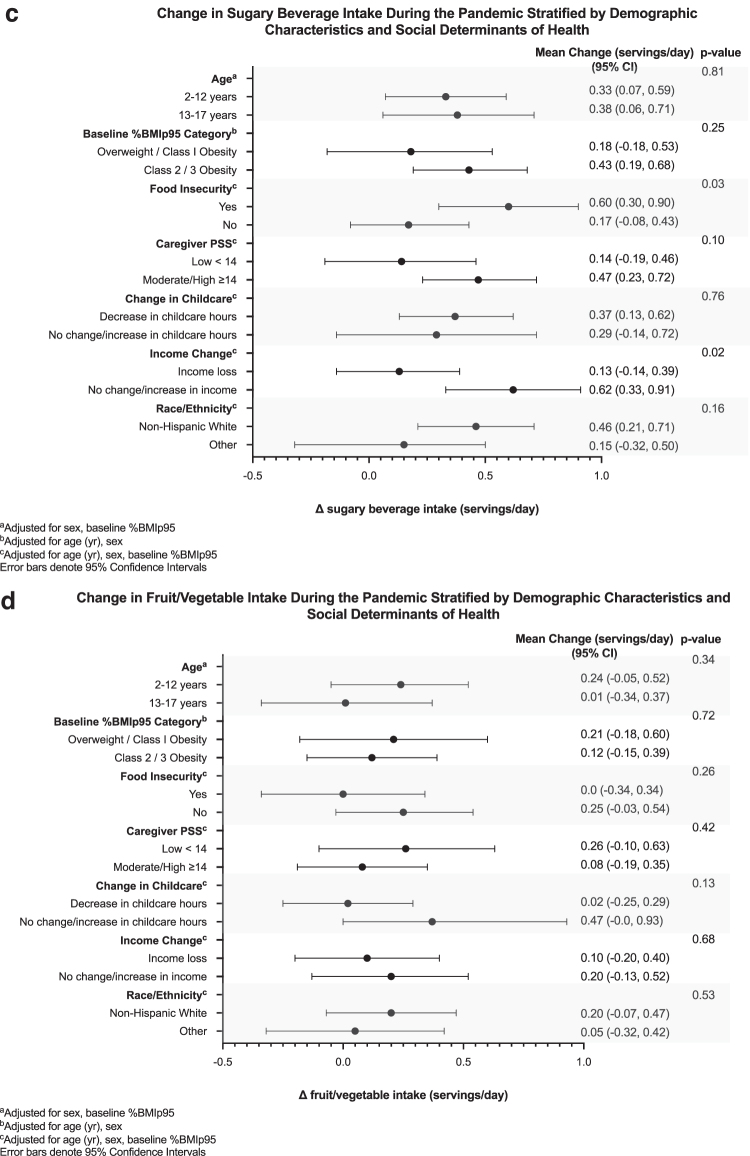
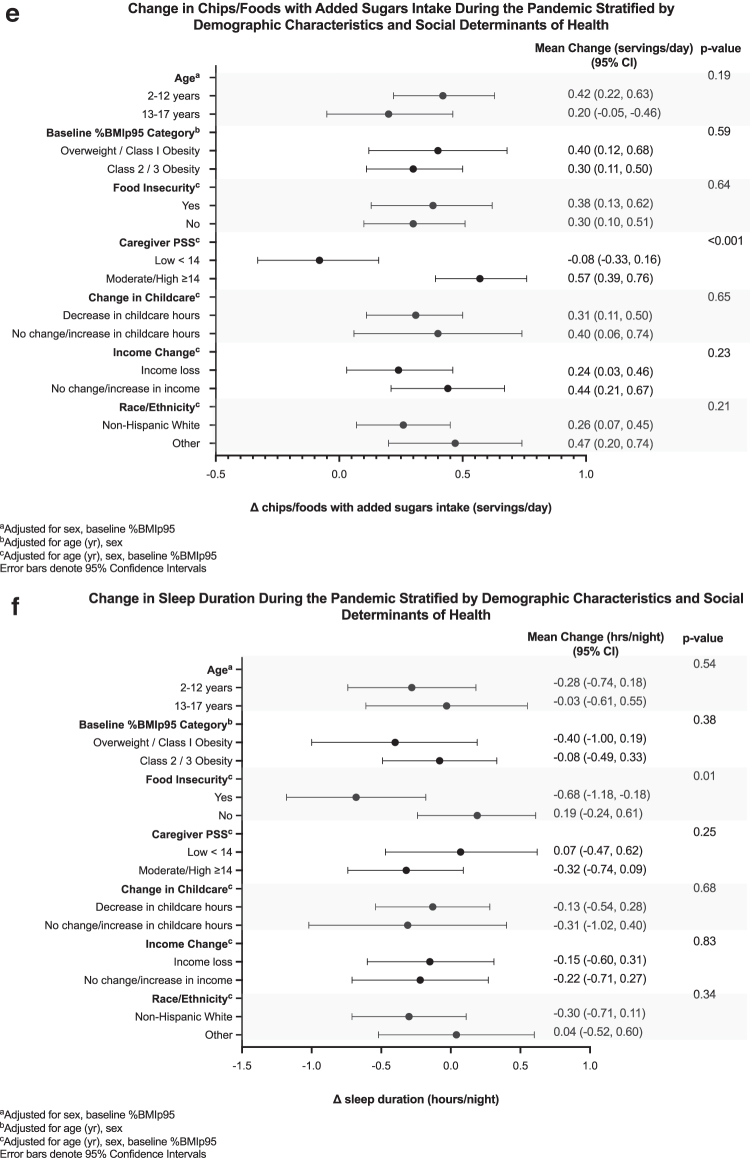
Figure 1 displays associations between SDoH and continuous behavior changes. Children whose caregivers reported moderate/high stress had a higher magnitude of decrease in MVPA (−119.0 [95% confidence interval −152.0, −85.9] vs. −39.9 [−83.6, 3.8] minutes/week, p = 0.01) and higher magnitude of increases in their intake of chips/food with added sugar (0.6 [0.4, 0.8] vs. −0.1 [−0.3, 0.2] servings/day, p < 0.001). Caregiver-reported food insecurity was associated with decrease in sleep duration (−0.7 [−1.2, −0.2] vs. 0.2 [−0.2, 0.6] hours/night, p = 0.01) and a greater increase in sugary beverage intake (0.6 [0.3, 0.9] vs. 0.2 [−0.1, 0.4] servings/day, p = 0.03). Supplementary Table S4 displays additional associations.
Figure 1.
Change in caregiver-reported weight-related behaviors during the pandemic stratified by demographic characteristics and SDoH. (a) Change in moderate/vigorous physical activity during the pandemic stratified by demographic characteristics and SDoH. (b) Change in screen time during the pandemic stratified by demographic characteristics and SDoH. (c) Change in sugary beverage intake during the pandemic stratified by demographic characteristics and SDoH. (d) Change in fruit/vegetable intake during the pandemic stratified by demographic characteristics and SDoH. (e) Change in chips/foods with added sugar intake during the pandemic stratified by demographic characteristics and SDoH. (f) Change in sleep duration during the pandemic stratified by demographic characteristics and SDoH. PSS, Perceived Stress Scale; SDoH, social determinants of health.
Table 4 displays associations between SDoH and categorical behavior changes. Food insecurity was associated with decreased relative risk of having a regular bedtime (RR 0.36 [0.24, 0.54] among food insecure vs. 0.58 [0.47, 0.70] among food secure, p = 0.04). We did not observe significant associations between SDoH and other categorical behavior changes.
Table 4.
Likelihood of Caregiver-Reported Weight-Related Behaviors during vs. Prepandemic Stratified by Demographic Characteristics and Social Determinants of Health
| Regular bedtime (during vs. prepandemic) |
Severe sleep disturbance (during vs. prepandemic) |
Most meals with Television (during vs. prepandemic) |
||||
|---|---|---|---|---|---|---|
| Relative risk (95% CI) | Risk ratio (95% CI) | Relative risk (95% CI) | Risk ratio (95% CI) | Adjusted relative risk (95% CI) | Adjusted risk ratio (95% CI) | |
| Agea (years) | ||||||
| 13–17 | 0.37 (0.24–0.56)f | 0.64 (0.41–1.02) | 2.00 (1.04–3.84)d | 0.47 (0.16–1.38) | 2.57 (1.38–4.81)e | 1.20 (0.55–2.59) |
| 2–12 | 0.57 (0.47–0.69)f | 4.25 (1.80–10.01)f | 2.15 (1.37–3.37)f | |||
| Baseline %BMIp95 categoryb | ||||||
| Overweight/Class I obesity (85%–119% of the 95th percentile) | 4.28 (2.44–7.53)f | 0.61 (0.21–1.76) | 0.90 (0.83–0.97)e | 1.25 (1.01–1.54)d | 2.36 (1.52–3.66) | 1.10 (0.50–2.43) |
| Class 2/3 obesity (≥120th of the 95th percentile) | 7.01 (2.87–17.16)f | 0.72 (0.59–0.88)e | 2.15 (1.11–4.17) | |||
| Food insecurity (yes vs. no)c | ||||||
| Food insecurity Yes | 0.36 (0.24–0.54)f | 0.63 (0.40–0.99)d | 3.40 (1.53–7.53)e | 1.42 (0.50–4.01) | 2.00 (1.26–3.18)e | 0.70 (0.33–1.50) |
| Food insecurity No | 0.58 (0.47–0.70)f | 2.40 (1.23–4.69)d | 2.86 (1.57–5.22)f | |||
| Caregiver PSS (moderate/high vs. low)c | ||||||
| Parent PSS low (<14) | 0.56 (0.43–0.74)f | 1.22 (0.84–1.77) | 4.00 (0.45–35.79) | 1.44 (0.15–13.70) | 2.20 (1.15–4.18)d | 0.94 (0.43–2.06) |
| Parent PSS high (≥14) | 0.46 (0.36–0.59)f | 2.78 (1.65–4.68)f | 2.32 (1.50–3.60)f | |||
| Change in Childcare (no change/increase vs. decrease)c | ||||||
| Childcare hours increase or same | 0.46 (0.36–0.59)f | 0.81 (0.56–1.18) | 2.25 (1.28–3.96)e | 0.41 (0.10–1.62) | 2.29 (1.51–3.46)f | 0.99 (0.42–2.32) |
| Childcare hours decrease | 0.57 (0.43–0.76)f | 5.50 (1.57–19.27)e | 2.31 (1.10–4.88)d | |||
| Income change (no change/increase vs. loss)c | ||||||
| Income increase or same | 0.47 (0.36–0.61)f | 0.89 (0.61–1.29) | 3.50 (1.53–8.01)e | 1.40 (0.48–4.10) | 1.91 (1.18–3.10)e | 0.69 (0.33–1.44) |
| Income decrease | 0.53 (0.40–0.69)f | 2.50 (1.26–4.96)e | 2.77 (1.59–4.83)f | |||
| Race/ethnicity (NHW vs. other)c | ||||||
| Race/ethnicity Other | 0.47 (0.36–0.60)f | 0.85 (0.59–1.23) | 2.75 (1.52–4.97)f | 0.79 (0.21–2.92) | 2.66 (1.63–4.35)f | 1.52 (0.74–3.13) |
| Race/ethnicity NHW | 0.55 (0.42–0.72)f | 3.50 (1.08–11.29)d | 1.75 (1.03–2.96)d | |||
Meals with television model adjusted for sex and baseline %BMIp95.
Meals with television model adjusted for age (year) and sex.
Meals with television model adjusted for age (year), sex, and baseline %BMIp95.
p-value <0.05.
p-value <0.01.
p-value <0.001.
CI, confidence interval; NHW, non-Hispanic white.
Discussion
In this study, we found significant adverse changes in weight-related health behaviors among a sample of youth with overweight/obesity during the COVID-19 pandemic. Recreational and school-related screen time doubled, youth had less physical activity, and unhealthy dietary intake increased. While nearly half of caregivers endorsed moderate/high levels of perceived stress and a quarter food insecurity prepandemic, the proportions increased further during the pandemic. Youth with stressed caregivers and household food insecurity had greater magnitudes of decreased MVPA and increased unhealthy dietary intake. These findings are a call to action to address these modifiable SDoH to mitigate the worsening obesity epidemic and widening disparities that may last long after the COVID-19 pandemic has waned.
By focusing on youth with prepandemic overweight/obesity and examining the relationships between SDoH and adverse behavior changes, our findings add to studies and commentaries drawing attention to the myriad negative impacts the pandemic is having on children, including the emergence of an unprecedented obesogenic environment.30 Studies from all over the world report declines in physical activity and increased screen time.5,6 Rates of BMI increase have increased significantly, particularly for those with prepandemic overweight/obesity.3,31
In our cohort, mean prepandemic MVPA was below CDC recommendations for 60 minutes of MVPA per day, and worsened during the pandemic. Adolescents also reported a similar mean magnitude of change, but we were underpowered to detect statistical significance. Although previous studies report decreased self-reported physical activity during the pandemic, our survey participants reported lower prepandemic MVPA than other studies, which may be explained by our focus on youth with overweight/obesity.5,11 Focusing on opportunities for physical activity in the home or safe outdoor settings may be an effective strategy to improve still limited programmatic options.
The alarming magnitude of increase in screen time in our study and multiple studies internationally speaks the importance of health care providers tailoring anticipatory guidance to caregivers' realities. “The COVID effect” is discussed in mainstream media with online time significantly increased in children 4–15 years old. Health care providers have an opportunity to discuss the risks/benefits of screen time, and the concept that screen time can be harnessed as a positive tool. Early in the pandemic, almost a third of children were using technology to do physical activity.11 Use of technology for play-based physical activity, or “exergaming,” with social interaction and support, has been shown to improve BMI and cardiometabolic health in youth with overweight/obesity.32 Tailoring guidance around technology to the context, rather than promoting dogma of limited screen time, may promote children's access to at-home physical activity when access to school-/outdoor-/facility-based exercise is limited.
Our observations that both moderate/high caregiver PSS and food insecurity were associated with greater changes in weight-related health behaviors during the pandemic underscore the important relationship between psychosocial well-being and weight-related health behaviors. In addition, our adolescent cohort reported baseline moderate/high PSS, which could indicate chronic stress. Prior studies have suggested that both parental and youth stress may be associated with increased BMI in youth and adverse health behaviors such as increased intake of unhealthy comfort foods.33 These similar comfort foods are more feasible to obtain when experiencing food insecurity, given their processed nature and consequent long shelf life. Moreover, uneven school reopenings may put vulnerable children at greater risk as school food is one of the most equitable sources of food access in the country.34
The effect of school closure on overall health is particularly concerning in light of disparate access to in-person learning with racial/ethnic minority students more likely to be in remote school.35 Guidance by the American Academy of Pediatrics speaks to the importance of continuing regular follow-up for obesity and tailoring assessment and counseling to issues exacerbated by the pandemic, including patient/family stress and food insecurity.36
Our communities have reopened and the promise of a new normal is enticing, but postpandemic stress and changes to health behaviors may last years. Clinicians may utilize techniques such as motivational interviewing to provide tailored guidance to address families' heightened psychosocial stressors and barriers to healthy lifestyle routines.37 There is growing evidence of the role for mindfulness to mitigate chronic toxic stress; mindfulness interventions have previously been demonstrated to have beneficial effects on parental emotional eating and child BMI.38 Family-based, high-intensity weight management programs can facilitate healthy BMI change for youth, but access to these programs is limited.39
Telehealth interventions for youth with overweight/obesity show promise for improving access to multidisciplinary weight management programs and require further study.40 More access to green space through the built environment may also impact BMI. Efforts to support innovation in and access to behavioral/lifestyle programs, address food insecurity with access to healthy foods, and expand access to green space in our communities may help mitigate the effects of the current obesogenic climate.
Our study has several limitations, including a low response rate. When comparing demographics for responders vs. nonresponders, the baseline characteristics were similar, although there was a larger response from caregivers of non-Hispanic white youth. We used only electronic surveys due to the pandemic and limited in-person visits, and the survey was only available in English. These factors may limit the generalizability of our findings. Another limitation is the potential for recall bias regarding behaviors that occurred before the pandemic. We also surveyed caregivers as proxies for youth, which may introduce proxy bias. There was variation in responses with large SDs. While we found statistically significant changes, the wide variation may speak to families' varying abilities to engage in healthy behaviors during disruptive events.10
In addition, we tried to balance use of validated surveys with a manageable number of questions to give us a well-rounded sense of weight-related health behaviors. There is also potential for type 1 errors with our exploratory analysis of SDoH and behavior changes, but some of the associations are strongly significant at p-value <0.001.
Conclusion
Mounting evidence suggests that the COVID-19 pandemic will have a long-standing impact on the health and well-being of our communities. This study's findings of adverse changes in health behaviors suggest that youth with overweight/obesity are at risk for worsened health outcomes. Youth with caregivers endorsing higher stress levels and reporting food insecurity appear to be at greater risk for adverse behavior changes, which is alarming in light of persistent and potentially widening disparities in obesity prevalence and severity. Urgent investment is needed to address modifiable SDoH and to expand access to effective interventions that address psychosocial barriers to healthy behaviors in youth.
Supplementary Material
Acknowledgments
We would like to acknowledge Amy Beck, MD, MPH, from University of California San Francisco School of Medicine and Monica Ordway, PhD, APRN, PNP-BC, at Yale School of Nursing, for sharing their experiences with survey measures to capture weight-related health behaviors in youth with overweight/obesity. We would also like to thank the patients and families who participated in this study, for their time and willingness to share their experiences.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Authors' Contributions
Each listed author made substantial contributions to the conception or design of the work and the acquisition, analysis, or interpretation of data for the work. They participated in the drafting of the work and made critical revisions for important intellectual content. They gave final approval of the version to be published. They agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding Information
Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health (NIH) under Award No. R01HL151603 (M.S.), by the National Institute on Minority Health and Health Disparities of the NIH under Award No. R01MD014853 (M.S.), and by CTSA Grant No. UL1 TR001863 from the National Center for Advancing Translational Science (NCATS), a component of the NIH. S.S. was supported by Award No. K12DK094714 from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the NIH. M.V.N. was supported by Award No. K23DK115894 from the NIDDK of the NIH. The study sponsors had no role in study design, collection, analysis, interpretation of data, the writing of the article, and the decision to submit the article for publication.
Author Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. Patrick SW, Henkhaus LE, Zickafoose JS, et al. . Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics 2020;146. [DOI] [PubMed] [Google Scholar]
- 2. Fryar CD. Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2017–2018. NCHS Health E-Stats 2020. 2020.
- 3. Lange SJ, Kompaniyets L, Freedman DS, et al. . Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2–19 years—United States, 2018–2020. MMWR Morb Mortal Wkly Rep 2021;70:1278–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ekelund U, Luan J, Sherar LB, et al. . Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA 2012;307:704–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ten Velde G, Lubrecht J, Arayess L, et al. Physical activity behaviour and screen time in Dutch children during the COVID-19 pandemic: Pre-, during- and post-school closures. Pediatr Obes 2021:e12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beck AL, Huang JC, Lendzion L, et al. Impact of the COVID-19 pandemic on parents' perception of health behaviors in children with overweight and obesity. Acad Pediatr 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agostinelli F. When the Great Equalizer Shuts Down: Schools, Peers, and Parents in Pandemic Times. National Bureau of Economic Research Working Paper Series. 2020; No. 2826. 4. [Google Scholar]
- 8. Hetrick RL, Rodrigo OD, Bocchini CE. Addressing pandemic-intensified food insecurity. Pediatrics 2020;146:e2020006924. [DOI] [PubMed] [Google Scholar]
- 9. Jenssen BP, Kelly MK, Powell M, et al. COVID-19 and changes in child obesity. Pediatrics 2021. [DOI] [PubMed] [Google Scholar]
- 10. Neshteruk C, Zizzi A, Suarez L, et al. . Weight-related behaviors of children with obesity during the COVID-19 pandemic. Child Obes 2021;17:371–378. [DOI] [PubMed] [Google Scholar]
- 11. Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the U.S. BMC Public Health 2020;20:1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents' lifestyle behavior larger than expected. Prog Cardiovasc Dis 2020;63:531–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. López-Bueno R, López-Sánchez GF, Casajús JA, et al. . Health-related behaviors among school-aged children and adolescents during the Spanish Covid-19 confinement. Front Pediatr 2020;8:573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yang S, Guo B, Ao L, et al. . Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin Obes 2020;10:e12416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Feudtner C, Feinstein JA, Zhong W, et al. . Pediatric complex chronic conditions classification system version 2: Updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Simon TD, Haaland W, Hawley K, et al. . Development and validation of the Pediatric Medical Complexity Algorithm (PMCA) Version 3.0. Acad Pediatr 2018;18:577–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harris PA, Taylor R, Thielke R, et al. . Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blanco A. Most Connecticut school districts sticking with hybrid of online and in-person learning; 133 coronavirus cases among students and staff last week. The Hartford Courant. 2020.
- 19. A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 years). National Center for Chronic Disease Prevention and Health Promotion. Available at https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm Published 2019. Updated February 26, 2019.
- 20. Flegal KM, Wei R, Ogden CL, et al. . Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr 2009;90:1314–1320. [DOI] [PubMed] [Google Scholar]
- 21. Freedman DS, Butte NF, Taveras EM, et al. . BMI z-Scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999–2000 to 2013–2014. Obesity (Silver Spring) 2017;25:739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. González-Gil EM, Mouratidou T, Cardon G, et al. . Reliability of primary caregivers reports on lifestyle behaviours of European pre-school children: The ToyBox-study. Obes Rev 2014;15 Suppl 3:61–66. [DOI] [PubMed] [Google Scholar]
- 23. National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Questionnaire 2019-2020 Physical Activity and Physical Fitness (PAQ). Department of Health and Human Services, Centers for Disease Control and Prevention. Available at https://wwwn.cdc.gov/nchs/data/nhanes/2019-2020/questionnaires/PAQ_K.pdf Published 2019.
- 24. Forrest CB, Meltzer LJ, Marcus CL, et al. . Development and validation of the PROMIS Pediatric Sleep Disturbance and Sleep-Related Impairment item banks. Sleep 2018;41. [DOI] [PubMed] [Google Scholar]
- 25. Carle AC, Bevans KB, Tucker CA, Forrest CB. Using nationally representative percentiles to interpret PROMIS pediatric measures. Qual Life Res 2021;30:997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lewis KH, Skelton J, Hsu FC, et al. . Use of electronic health record data to study the association of sugary drink consumption with child weight status. Acad Pediatr 2020;20:767–775. [DOI] [PubMed] [Google Scholar]
- 27. Savoye M, Shaw M, Dziura J, et al. . Effects of a weight management program on body composition and metabolic parameters in overweight children: A randomized controlled trial. JAMA 2007;297:2697–2704. [DOI] [PubMed] [Google Scholar]
- 28. Hager ER, Quigg AM, Black MM, et al. . Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics 2010;126:e26–e32. [DOI] [PubMed] [Google Scholar]
- 29. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–396. [PubMed] [Google Scholar]
- 30. Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health 2020;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Woolford S, Sidell M, Li X, et al. . Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA 2021;326:1434–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Staiano AE, Beyl RA, Guan W, Hendrick CA, et al. . Home-based exergaming among children with overweight and obesity: A randomized clinical trial. Pediatr Obes 2018;13:724–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Baskind MJ, Taveras EM, Gerber MW, et al. . Parent-perceived stress and its association with children's weight and obesity-related behaviors. Prev Chronic Dis 2019;16:E39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Liu J, Micha R, Li Y, Mozaffarian D. Trends in food sources and diet quality among US children and adults, 2003–2018. JAMA Netw Open 2021;4:e215262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Verlenden JV, Pampati S, Rasberry CN, et al. . Association of children's mode of school instruction with child and parent experiences and well-being during the COVID-19 pandemic—COVID Experiences Survey, United States, October 8–November 13, 2020. MMWR Morb Mortal Wkly Rep 2021 2021;70:379–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. AAP. Obesity Management and Treatment During COVID-19 [Interim Guidance]. 2020. Available at https://services.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/obesity-management-and-treatment-during-covid-19 Last accessed December 9, 2020.
- 37. Resnicow K, McMaster F, Bocian A, et al. . Motivational interviewing and dietary counseling for obesity in primary care: An RCT. Pediatrics 2015;135:649–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jastreboff AM, Chaplin TM, Finnie S, et al. . Preventing childhood obesity through a mindfulness-based parent stress intervention: A Randomized Pilot Study. J Pediatr 2018;202:136–142.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. O'Connor EA, Evans CV, Burda BU, et al. . Screening for obesity and intervention for weight management in children and adolescents: Evidence report and systematic review for the US Preventive Services Task Force. JAMA 2017;317:2427–2444. [DOI] [PubMed] [Google Scholar]
- 40. Woo Baidal JA, Chang J, Hulse E, et al. . Zooming toward a telehealth solution for vulnerable children with obesity during coronavirus disease 2019. Obesity (Silver Spring) 2020;28:1184–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.